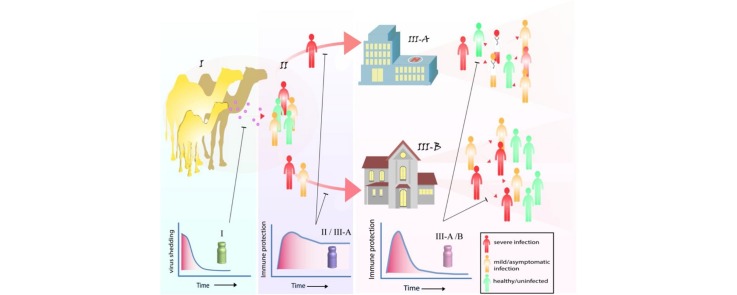
Graphical abstract
MERS-CoV vaccine target groups and the desired vaccine induced immunological response for each group. I: camels; II: camel contacts; III-A: healthcare workers and patients; III-B: house-hold contacts and MERS cases.
Highlights
-
•
MERS-CoV vaccines for dromedary camels and their human contacts can potentially stop virus transmission in the community.
-
•
Both neutralizing antibody and T-cell responses are required for protection
-
•
MERS-CoV vaccines should aim at inducing (long term) mucosal immunity in the different target populations.
-
•
The spike protein induces both neutralizing antibodies and T-cell responses and is the main target of the current vaccine candidates.
-
•
Epitope-based vaccines, focusing at (cross)-protective epitopes, could induce higher and/or broader responses.
Abstract
Middle East respiratory syndrome coronavirus (MERS-CoV) is a cause of severe respiratory infection in humans, specifically the elderly and people with comorbidities. The re-emergence of lethal coronaviruses calls for international collaboration to produce coronavirus vaccines, which are still lacking to date. Ongoing efforts to develop MERS-CoV vaccines should consider the different target populations (dromedary camels and humans) and the correlates of protection. Extending on our current knowledge of MERS, vaccination of dromedary camels to induce mucosal immunity could be a promising approach to diminish MERS-CoV transmission to humans. In addition, it is equally important to develop vaccines for humans that induce broader reactivity against various coronaviruses to be prepared for a potential next CoV outbreak.
Current Opinion in Virology 2017, 23:49–58
This review comes from a themed issue on Preventive and therapeutic vaccines
Edited by Rino Rappuoli and Gerd Sutter
For a complete overview see the Issue and the Editorial
Available online 13th April 2017
http://dx.doi.org/10.1016/j.coviro.2017.03.007
1879-6257/© 2017 The Authors. Published by Elsevier B.V. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/).
Introduction
Coronaviruses are the largest positive sense single stranded RNA viruses. There are six human coronaviruses (HCoV) to date; HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, severe acute respiratory syndrome (SARS)-CoV, and Middle East respiratory syndrome (MERS)-CoV. Prior to the SARS-CoV epidemic in 2002–2003, CoVs were known to cause mild respiratory infections in humans. SARS-CoV, on the other hand, infected around 8000 cases causing severe respiratory disease with a 10% fatality rate [1]. Ten years later, MERS-CoV emerged in the human population also to cause severe respiratory infection [2]. In contrast to the SARS-CoV epidemic, which was contained within one year, MERS-CoV still continues to cause outbreaks with increasing geographical distribution, four years after its first identification. As of March 2nd 2017, 1905 cases in 27 countries have been reported to the WHO with 677 deaths accounting for a 35% case fatality rate (http://www.who.int/emergencies/mers-cov/en/). Like SARS-CoV, MERS-CoV emerged as a result of zoonotic introduction to the human population. Despite its close genome similarity with bat coronavirus HKU4 and HKU5 [2], accumulating serological and molecular evidence pointed to dromedary camels as the most probable reservoir for MERS-CoV [3, 4, 5]. This poses a continuous risk of virus spill-over to people in contact with camels, such as those working in slaughter houses and animal farms, evidenced by the presence of MERS-CoV antibodies in sera of those individuals [6, 7]. Nosocomial transmission, however, accounts for the majority of MERS-CoV cases reported in outbreaks [8, 9, 10], although a substantial part of infections that occur result in unrecognized asymptomatic or mild illnesses [11]. Thus, in addition to camel contacts, other highly-at-risk groups are healthcare workers and patient household contacts [8, 12, 13]. Considering the ongoing MERS-CoV outbreaks, it is crucial to develop intervention measures among which vaccines play an important role. Despite the fact that the emergence of MERS-CoV and SARS-CoV has dramatically changed the way we view CoVs, there is no licensed CoV vaccine or therapeutic drug available to date [14, 15].
Immune correlates of protection
A cornerstone for rational vaccine design is defining the determinants of immune protection. Accumulating data from studies done so far on MERS-CoV and other coronaviruses revealed that a combination of both virus-specific humoral and cellular immune responses is required for full protection against coronaviruses. Especially neutralizing antibodies are considered key players in the protective immunity against CoVs. Neutralizing monoclonal antibodies (Mabs) reduced viral loads in MERS-CoV receptor-transduced mice, rabbits and macaques [16, 17, 18, 19]. Similarly, convalescent camel sera increased virus clearance and decreased lung pathological outcomes in mice with an efficacy directly proportional to anti-MERS-CoV-neutralizing antibody (Nab) titers [20]. Also polyclonal sera produced in transchromosomic bovines protected mice against MERS-CoV challenge [21].
Evidence for the protective role of antibodies also comes from recent studies analyzing immune responses in patients that survived or succumbed to MERS-CoV. Although neutralizing antibodies were only weakly inversely correlated to viral loads, serum antibody responses were higher in survivors compared to fatal cases but viral RNA was not eliminated from the lungs [22, 23]. Administration of convalescent sera, however, did not lead to significant reduction in viral loads [22, 24]. The presence of mucosal IgA Abs, on the other hand, was found to influence infectious virus isolation [25].
Besides humoral immunity, cellular immune responses are also considered to play a crucial role in protection against coronaviruses. While B-cell deficient mice were able to clear MERS-CoV, those lacking T-cells failed to eliminate the virus, pointing out the crucial role of T-cells in viral clearance [26]. This is supported by the observation that T-cells were able to protect aged mice against SARS-CoV infection [27••] and the fact that a reduced T-cell count was associated with enhanced disease severity in SARS patients [28]. Along with other studies, these data highlight the importance of T-cells for virus clearance and protection against MERS-CoV [26, 27••] and SARS-CoV [29, 30]. It is also noteworthy to mention that while neither antibodies nor memory B cells were detectable 6-years post-infection [31], SARS-CoV-specific memory T-cells, despite being low in frequency, persisted up to 11 years post-recovery [32]. Nonetheless, the protective capacity of such memory response is not known. Hence, taking into account the waning of virus-specific humoral responses, generating a long-lived memory T cell response through vaccination could be favorable, but as proper B- and T-cell immune responses are required for efficient protection, vaccination should target the induction of both. At the moment we lack information concerning the longevity of anamnestic immune responses following MERS-CoV infection, except for a recent study showing that antibody responses, albeit reduced, persisted up to 34 months post-infection [33]. The role of immune responses in protection is also in line with the observed increased fatality among the aged population following MERS-CoV infection. Retrospective studies on MERS-CoV patients from Saudia Arabia and South Korea have found a significant correlation between old age and mortality [8, 13, 34, 35, 36], a pattern that has been also reported for other respiratory viruses such as SARS-CoV [1] and influenza virus [37]. This is most likely caused by immunosenescence; a failure to produce protective immune response to new pathogens in elderly due to impaired antigen presentation, altered function of TLRs, and a reduced naïve B and T cell repertoire [38]. This age-related increase in mortality was also reported in SARS-CoV laboratory-infected animals, that is, mice and nonhuman primates (NHPs) [39, 40], and was associated with low neutralizing antibodies and poor T-cell responses [41, 42, 43•]. Several factors that play a role in T-cell activation were also found to be dysregulated in an age-related manner. Age-related increase in phospholipase A2 group IID (PLA2G2D), and prostaglandinD2 in the lungs contributed to a diminished T-cell response and severe lung damage through diminishing respiratory dendritic cell (DC) migration [44, 45]. Likewise, adoptive transfer of T-cells to mice enhanced viral clearance and survival [29], highlighting the contribution of a reduced T-cell response in severe disease outcome. These observations also highlight the need for more effective preventive measures for the elderly. In this sense, induction of a potent airway T-cell response may be crucial to protect against CoVs [27••]. Thus, a promising approach to protect against MERS-CoV-induced fatality is to enhance virus-specific tissue (airway) resident memory T-cell responses through intranasal vaccination.
Current MERS-CoV vaccine candidates
Although the MERS-CoV genome encodes for 16 non-structural proteins (nsp1-16) and four structural proteins, the spike (S), envelope (E), membrane (M), and nucleocapsid (N) [46], the viral structural proteins, S and N, show the highest immunogenicity [47]. While both S and N proteins can induce T-cell responses, neutralizing antibodies are almost solely directed against the S protein, with the receptor binding domain (RBD) being the major immunodominant region [48]. Thus, current MERS-CoV vaccine candidates mainly employ the spike protein or (parts of) the gene coding for this glycoprotein.
These MERS-CoV vaccines candidates were developed using a wide variety of platforms, including whole virus vaccines, vectored-virus vaccines, DNA vaccines, (Table 1 ) and protein-based vaccines (Table 2 ). Although live attenuated vaccines produce the most robust immune responses, they pose a risk from reversion to virulence. Inactivated virus vaccines may cause harm due to incomplete attenuation or the capacity to induce lung immunopathology [49]. Viral-vector-based vaccines, on the other hand, provide a safer alternative and have been developed using modified vaccinia virus Ankara (MVA) [50, 51, 52••], adenovirus (AdV) [53, 54], measles virus (MeV) [55], rabies virus (RABV) [56], and Venezuelan equine encephalitis replicons (VRP) [26, 57], all expressing MERS-S/S1 proteins. Additionally, VRP expressing the N protein have also been developed [27••]. A major hurdle facing these viral-vector-based platforms is preexisting immunity in the host which potentially can impair the vaccine efficacy. However, this can be prevented by using virus strains not circulating in the targeted population or immunization strategies involving heterologous prime-boost immunization, for example, MVA and AdV. Although plasmid DNA vaccines are considered to be of low immunogenicty in humans, current versions developed seem to induce potent immune responses. DNA-based vaccines directed at inducing anti S responses were also shown to exert protection in NHPs [58, 59]. Noteworthy to mention is that a combination of DNA (S) and recombinant protein (S1) in a heterologous prime-boost immunization strategy induced higher immune response (Nab) compared to each component alone [58]. Additionally, protein-based vaccines were developed in various platforms as virus-like particles (VLPs) [60], nanoparticles [61], peptide-based [62], and subunit vaccines directed against various regions of the spike protein S1 [58], the N-terminal domain [63], and the RBD [48, 64, 65, 66, 67, 68, 69, 70]. Those vaccines have the highest safety profile among vaccine platforms but confer variable degrees of immunogenicity which need adjustment for the dose, adjuvants, and site of administration to get optimal protective responses. Adjuvants influence the type and magnitude of immune response produced by vaccines, and thus the doses used [61, 65, 68]. Additionally, the route of administration is a determining factor for the type of vaccine-induced immune response produced in the host. While intranasal (i.n.) vaccination with SARS-N produced a protective airway T-cell response against SARS-CoV in mice, subcutaneous (s.c.) vaccination, inducing systemic T-cell responses, did not [27••]. Likewise, i.n. vaccination with MERS-RBD induced a significantly higher neutralizing and IgA antibody responses in the mice airways compared to s.c. vaccination [70]. This is important because mucosal immunity and airway memory T-cell responses are crucial players in protection against respiratory viruses, since these areas are the first to encounter the virus. Therefore, along with selecting antigens for a vaccine, the route of vaccination and adjuvants are key players that cannot be neglected in vaccine design.
Table 1.
Virus and DNA-based MERS-CoV vaccine candidates
| Vaccine platform | Vaccine candidate | Target antigen | Animal model | Route; adjuvant | Immunological response |
Efficacy | Reference | ||
|---|---|---|---|---|---|---|---|---|---|
| Nab | T-cell | ||||||||
| Live attenuated vaccine | rMERS-CoV-ΔE | MERS-CoV | ND | – | ND | ND | ND | [81] | |
| Inactivated whole virus | Whole inactivated virus (WIV) | MERS-CoV | hDPP4 Tg-mice | i.m.; alum/MF59 | + | ND | Protectiveb | [49] | |
| Recombinant Viral vectors | MVA | MVA-S | S | Ad/hDPP4-mice | 2x i.m./s.c.c | + | + | Protective | [51] |
| camel | 2x i.n. + i.m. | +; Mucosal | + | Protective | [52••] | ||||
| Adenovirus | Ad5-S/S1 | S/S1 | mice | 1:i.m.; 2: i.n. | + | + | ND | [53] | |
| Ad5-S/Ad41-S | S | mice | intragastric | + | – | ND | [54] | ||
| i.m. | + | + | ND | [54] | |||||
| Measles | MVvac2-MERS-S/solS | S/solS | Ad/hDPP4-micea | 2x i.p. | + | + | Protective | [55] | |
| Venezuelan equine encephalitis virus | VRP-N | N | Ad/hDPP4-mice | 2x i.n. | – | Airway | Protective | [27••] | |
| VRP-S | S | Ad/hDPP4-mice | 2x footpad | + | + | Protective | [26] | ||
| VRP-S | S | 288/330+/+mice | 2x footpad | + | ND | Protective | [57] | ||
| Rabies virus | BNSP333-S1 | S1 | Ad/hDPP4-mice | 3x i.m. | + | ND | Protective | [56] | |
| DNA Vaccines | VRC8400-S | S | NHP | 3x i.m. + EP | + | ND | Protective | [58] | |
| mice | 3x i.m. + EP | + | ND | ND | [58] | ||||
| pVax1-S | S | NHP | 3x i.m. + EP | + | + | Protective | [59] | ||
| camel | 3x i.m. + EP | + | ND | ND | [59] | ||||
| mice | 3x i.m. + EP | + | + | ND | [59] | ||||
| DNA + rProtein | S DNA (VRC8400-S)/S1 protein | S/S1 | NHPs | 2x S-DNA: i.m + e.p.; 1x S1 Protein: i.m. | + | ND | Protective | [58] | |
Ad, adenovirus; Ad/hDPP4-mice, mice transduced with hDPP4 in an adenoviral vector; alum, aluminum hydroxide; E, envelope protein; EP, electroporation; hDPP4, human dipeptidyl peptidase 4; i.m., intramuscular; i.n., intranasal; i.p., intraperitoneal; MERS-CoV, Middle East respiratory syndrome coronavirus; MVA, modified vaccinia virus Ankara; N, nucleocapsid protein; Nab, neutralizing antibodies; ND, not done; NHP, non-human primate; rMERS-CoV, recombinant Middle East respiratory syndrome coronavirus; S, spike protein; S1, S1 domain of spike protein; solS, spike protein lacking transmembrane domain; Tg-mice, transgenic mice; VRP, virus replicon particle.
Ad/hDPP4-IFNAR −/− -CD46Ge mice.
Neutralizing antibody and protection against viral infection was found in WIV preparation with and without adjuvant but hypersensitivity-type lung reaction was produced post-challenge.
S.c. vaccination was less immunogenic at lower virus doses.
Table 2.
MERS-CoV protein-based vaccine candidates
| Vaccine platform | Vaccine candidate | Target antigen | Animal model | Route; adjuvant | Immunological response |
Efficacy | Reference | ||
|---|---|---|---|---|---|---|---|---|---|
| Nab | T-cell | ||||||||
| Virus-like particles | MERS-CoV VLPs | S,M,E | NHP | 4x i.m.;alum | + | + | ND | [60] | |
| Nanoparticle vaccine | S | S | mice | 2x i.m.;alum/Matrix M1 | + | ND | ND | [61] | |
| Recombinant proteins | S1 | S1 | S1 | mice | 2x i.m. | + | ND | ND | [58] |
| NHP | 2x i.m. | + | ND | protective | [58] | ||||
| RBD Subunit Vaccines | RBD-Fc | S358-588 | Rabbit | i.m.; incomplete Freund’s | + | ND | ND | [48] | |
| rRBD | S367-606 | NHP | 3x i.m.; alum | + | + | Protective | [64] | ||
| rRBD | S367–606 | mice | 3x i.m.;alum/CpG ODNa | ++ | + | ND | [65] | ||
| RBD-Fc | S377-588b | Ad/hDPP4-mice | 3x s.c. +MF59c | + | + | protective | [66, 67, 68] | ||
| Trimer RBD-Fc | S377-588 | Ad/hDPP4-mice | 2x i.m. + alum | + | ND | Protective | [69] | ||
| RBD-Fc | S377-662 | mice | 5x i.n.; Poly(I:C)d | + | + | ND | [70] | ||
| Extra-RBD targets | rNTD | S18-353 | Ad/hDPP4-mice | 3x i.m.;alum + CpG | + | + | Protective | [63] | |
| SP3 | S736–761-KLH | Rabbit | Prime: CFA; 3x boost: incomplete Freund’s | + | ND | [62] | |||
Ad/hDPP4-mice, mice transduced with hDPP4 in an adenoviral vector; alum, aluminum hydroxide; E, envelope protein; hDPP4, human dipeptidyl peptidase 4; i.m., intramuscular; i.n., intranasal; M, matrix protein; MERS-CoV, Middle East respiratory syndrome coronavirus; Nab, neutralizing antibodies; ND, not done; NHP, non-human primate; rNTD, recombinant N-terminal domain; RBD, receptor-binding domain; rRBD, recombinant RBD; RBD-Fc, RBD fused to the antibody crystallizable fragment of human IgG; S, spike protein; S1, S1 domain of spike protein; S367–606, amino acid residues 367–606 of the S protein; S736–761-KLH, peptide S736–761 coupled to keyhole limpet haemocyanin; s.c., subcutaneous; VLPs, Virus-like particles;
i.m.;alum/CpG ODN produced higher neutralizing antibody responses than s.c.; IFA/CpG ODN.
S350-588-Fc, S358-588-Fc, S367-588-Fc, S367-606-Fc, and S377-588-Fc were tested and S377-588-Fc had the highest Nab titers although some produced equal S1 IgG response [66].
MF59 produced the highest immunogenicity at low doses of antigen compared to S377-588-Fc only, or with Freund’s/Alum/mPLA-SM/ISA51/MF59. [67] 1 mg of antigen with MF59 was sufficient to produce humoral and cellular immune responses similar to higher doses (5 mg or 20 mg) [68].
i.n. + poly(I:C) vaccination induced stronger systemic cellular responses and higher local immune responses in mice lungs (IgA and neutralizing antibody titers) than s.c. + Montanide ISA51 vaccination.
Challenges and novel approaches for CoV vaccines
Because the spike protein and more specifically the S1 domain, is highly divergent among different CoVs, neutralizing antibodies only provide homotypic protection. Thus far, the variability in the amino acid sequence of the spike protein observed among MERS-CoV strains is low [71], and circulating MERS-CoV strains did not show any significant variation in the serological reactivity [25, 59], implying that the development of a vaccine that is effective against one strain is likely to be protective against all circulating strains. Another risk posed from the development of antibody escape variants is still present [72, 73], although this is not likely to happen as mutations in two epitopes may be required, and mutants that develop may have reduced viral fitness [73, 74].
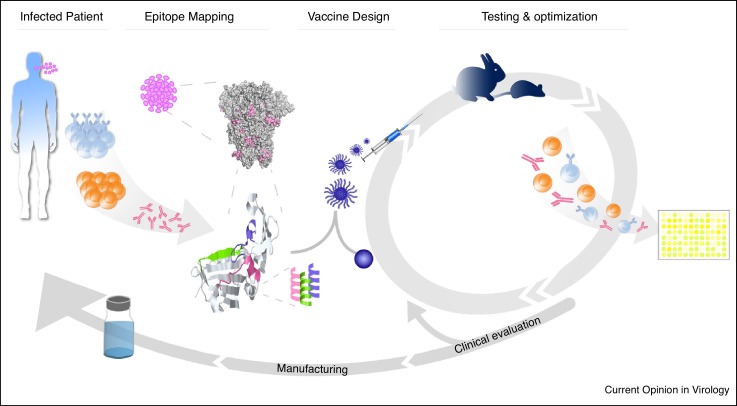
While the RBD is considered an ideal vaccine candidate for MERS-CoV, the spike S2 domain and N protein are more conserved, and thus adaptive immune response directed against these proteins can potentially lay the basis for a more broadly acting coronavirus vaccine. However, evidence for cross reactive immune responses against different CoVs is limited to a few studies. Convalescent SARS-CoV patient sera weakly neutralized MERS-CoV [75] and SARS-S reactive antisera showed low level neutralization of MERS-CoV [61]. Extra-RBD S1 or S2 epitopes could be responsible for this effect, as some neutralizing epitopes have been identified in these regions of the S protein [58, 62]. These may not be as immunodominant as the RBD epitopes but could provide a rationale for the development of a cross protective CoV epitope-focused vaccine. A recent study also demonstrated the potential role of adaptive response against N protein in protection against MERS-CoV infection as this vaccine candidate produced a protective T-cell response against MERS-CoV challenge which was also partially protective against SARS-CoV [27••]. Moreover, infection of mice with SARS-CoV reduced MERS-CoV titers 5 days p.i. upon challenge suggesting the development of a cross reactive T-cell response [26]. Thus, mapping and focusing the immune response towards these critical neutralizing and T-cell epitopes, which could be subdominant, may provide a way to induce immune responses with a broader activity against different CoVs. Immune focusing may also be beneficial for the generation of a robust virus-specific immune response. As during vaccine preparation, some epitopes which are normally hidden in the full length protein structure get exposed. Some epitopes could be immunodominant and have a negative contribution on the overall neutralization capacity produced by the vaccine [76•]. This also holds true for some non-neutralizing immunodominant epitopes, as S1-based vaccines induced slightly higher neutralization than whole S ectodomain-based ones [58, 53]. Additionally, the RBD induced higher neutralizing antibodies compared to an S1 subunit vaccine [48], and shorter regions of RBD induced even higher neutralization responses [66], indicating that additional regions inducing non-neutralizing antibodies may contribute negatively to the overall neutralization response produced. Additionally, antibody-dependent enhancement of the viral infection by non-neutralizing antibodies [77, 78, 79], despite not being reported so far for MERS-CoV, needs also to be taken into consideration when developing a coronavirus vaccine. One approach to enhance the efficacy of subunit vaccines is to mask those negatively-contributing epitopes through glycosylation [76•]. Other approaches are immunefocusing and epitope-based vaccines, all aiming at narrowing the immune response to target only critical or beneficial epitopes to produce a stronger protective response. A prerequisite to reach that goal is to map epitopes targeted by the immune system and identify their biological role as being neutralizing, non-neutralizing, infection enhancing, containing a T-cell epitope, and so on. This can be achieved by analyzing the activity and fine specificity of convalescent patient sera, infected animal polyclonal sera, monoclonal antibodies, animal and human PBMCs. Subsequently the predicted epitopes can also provide a basis for potential vaccine candidates when produced as nanoparticles or VLPs. Further characterization of the immune responses induced by these vaccine candidates when evaluated in an animal model may be utilized to optimize the vaccines for efficacy (Figure 1 ). This epitope-focused vaccine approach may allow for targeting less immunodominant B- and T-cell epitopes having broader protection, avoid eliciting immune responses against epitopes playing no role in protection or having a negative or harmful role. In addition to better targeting of protective immunodominant epitopes, a combination of those epitopes, B- and T-cell epitopes targeting different viral proteins, could be used to produce a broader and stronger protective immune response for both strain-specific and universal CoV vaccines.
Figure 1.
Epitope-based vaccine design. Following a virus infection, potential protective B- and T-cell epitopes are mapped. Peptides or proteins containing promising epitopes are produced and formulated using a suitable platform, for example, nanoparticles and tested for immunogenicity and efficacy in animals. Follwing several cycles of testing and optimization, a final vaccine suitable for human use may be produced.
Target populations for MERS-CoV vaccines
Next to the choice of the MERS-CoV vaccine candidate, it is also important to take into account the target population that needs to be protected through vaccination. Populations at risk of MERS-CoV infection include camel contacts, healthcare workers and patient contacts. The latter two groups could benefit from the rapid onset of immunity though passive immunization using Mabs or convalescent sera, provided that it is given in time. Another alternative strategy for short-term protection is the use of vaccines capable of rapidly inducing high titers of neutralizing antibodies. This will provide a short-term immunity beneficial to protect those highly-at-risk groups when a new case is identified, to prevent outbreaks. To prevent virus infection of primary cases, vaccination of the dromedary camels may also be considered. So far, among the available vaccine candidates, only two have been tested in dromedary camels, pVax1-S and MVA-S. pVax1-S, a DNA-based vaccine, induced neutralizing antibodies in two of three camels tested so far, but has not been tested for efficacy [59]. The other candidate MVA-S, a viral-vector-based vaccine, induced systemic neutralizing antibodies and mucosal immunity which conferred protection against MERS-CoV challenge and reduced virus shedding in vaccinated camels [52••] Therefore, this vaccine candidate may provide a means to prevent zoonotic transmission of the virus to the human population. For camel contacts and healthcare workers in endemic areas, being at a continuous risk of MERS-CoV infection either from infected camels or patients, respectively, it would be beneficial to induce a longer-term (mucosal) protection. While these could be rewarding approaches to stop MERS-CoV outbreaks, it is still worthwhile to develop platforms and vaccines that aim to induce more broad protection against different related CoVs, that could potentially cause future outbreaks.
Knowledge gaps and future prospective
Learning from previous epidemics, the WHO issued a list of priority pathogens posing a risk to the human population and requiring urgent research and development (R&D) for intervention measures, among which MERS-CoV and highly pathogenic CoVs are of high priority. The lack of intervention measures along with the increase in geographical area and ongoing MERS-CoV cases, raise worries for the future occurrence of larger epidemics as a result of virus adaptation in the human population and more efficient human-to human transmission. Further development of MERS-CoV and other CoV vaccines thus needs proactive collaborative efforts from researchers filling knowledge gaps, and market stakeholders providing funding for this costly process. The latter can be insufficient and/or unsustainable, therefore hindering development of even some promising candidates. In an initiative aiming at accelerating vaccine R&D process by providing sustained funding to be prepared for future epidemics, the World Economic Forum launched the Coalition for Epidemic Preparedness Innovations (CEPI) [80]. CEPI is an international non-profit association aiming at removing barriers facing vaccine development for epidemic infections and getting ready for future epidemics, including MERS-CoV. However, we still face a number of challenges despite the fact that various promising MERS-CoV vaccine candidates are currently available. There is a lack of animal models mimicking the disease in humans in which vaccine platforms can be tested prior to human use. We need to take into account the populations to target with vaccination, with camels and camel handlers being the most relevant ones. The lack of full understanding of the pathogenesis and immune responses to the virus in humans and camels, which is crucial for vaccine development, also needs further investments. In addition, the longevity of immune responses post-vaccination has not been evaluated for vaccine candidates, which is important for the vaccination scheme development and for the choice of the best candidates for further development. Lastly, most of the vaccine candidates are developed against the highly variable spike protein and thus may not be able to provide protection against CoV strains evolving in the future. A more targeted vaccination approach aiming at conserved epitopes should be considered for the development of a more broadly-acting CoV vaccine. Given the propensity of CoVs to jump the species barrier, current efforts to develop a MERS-CoV vaccine may also be of benefit to prepare for potential novel CoVs that may emerge in the future.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Acknowledgements
This work was supported by the Zoonoses Anticipation and Preparedness Initiative (ZAPI project; IMI grant agreement no. 115760), with the assistance and financial support of IMI and the European Commission, in-kind contributions from EFPIA partners.
References
- 1.Chen J., Subbarao K. The Immunobiology of SARS*. Annu. Rev. Immunol. 2007;25:443–472. doi: 10.1146/annurev.immunol.25.022106.141706. [DOI] [PubMed] [Google Scholar]
- 2.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 3.Haagmans B.L., Al Dhahiry S.H., Reusken C.B., Raj V.S., Galiano M., Myers R., Godeke G.J., Jonges M., Farag E., Diab A. Middle East respiratory syndrome coronavirus in dromedary camels: an outbreak investigation. Lancet Infect. Dis. 2014;14:140–145. doi: 10.1016/S1473-3099(13)70690-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alagaili A.N., Briese T., Mishra N., Kapoor V., Sameroff S.C., Burbelo P.D., de Wit E., Munster V.J., Hensley L.E., Zalmout I.S. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. MBio. 2014;5:e00884–00814. doi: 10.1128/mBio.00884-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reusken C.B., Haagmans B.L., Muller M.A., Gutierrez C., Godeke G.J., Meyer B., Muth D., Raj V.S., Smits-De Vries L., Corman V.M. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect. Dis. 2013;13:859–866. doi: 10.1016/S1473-3099(13)70164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reusken C.B., Farag E.A., Haagmans B.L., Mohran K.A., Godeke G.J., Raj S., Alhajri F., Al-Marri S.A., Al-Romaihi H.E., Al-Thani M. Occupational exposure to dromedaries and risk for MERS-CoV infection, Qatar, 2013–2014. Emerg. Infect. Dis. 2015;21:1422–1425. doi: 10.3201/eid2108.150481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muller M.A., Meyer B., Corman V.M., Al-Masri M., Turkestani A., Ritz D., Sieberg A., Aldabbagh S., Bosch B.J., Lattwein E. Presence of Middle East respiratory syndrome coronavirus antibodies in Saudi Arabia: a nationwide, cross-sectional, serological study. Lancet Infect. Dis. 2015;15:559–564. doi: 10.1016/S1473-3099(15)70090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korea Centers for Disease Control and Prevention Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res. Perspect. 2015;6:269–278. doi: 10.1016/j.phrp.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chowell G., Abdirizak F., Lee S., Lee J., Jung E., Nishiura H., Viboud C. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cauchemez S., Nouvellet P., Cori A., Jombart T., Garske T., Clapham H., Moore S., Mills H.L., Salje H., Collins C. Unraveling the drivers of MERS-CoV transmission. Proc. Natl. Acad. Sci. U. S. A. 2016;113:9081–9086. doi: 10.1073/pnas.1519235113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alraddadi B.M., Al-Salmi H.S., Jacobs-Slifka K., Slayton R.B., Estivariz C.F., Geller A.I., Al-Turkistani H.H., Al-Rehily S.S., Alserehi H.A., Wali G.Y. Risk factors for Middle East respiratory syndrome coronavirus infection among healthcare personnel. Emerg. Infect. Dis. 2016;22:1915–1920. doi: 10.3201/eid2211.160920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drosten C., Meyer B., Muller M.A., Corman V.M., Al-Masri M., Hossain R., Madani H., Sieberg A., Bosch B.J., Lattwein E. Transmission of MERS-coronavirus in household contacts. N. Engl. J. Med. 2014;371:828–835. doi: 10.1056/NEJMoa1405858. [DOI] [PubMed] [Google Scholar]
- 13.Saad M., Omrani A.S., Baig K., Bahloul A., Elzein F., Matin M.A., Selim M.A., Al Mutairi M., Al Nakhli D., Al Aidaroos A.Y. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int. J. Infect. Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Doremalen N., Munster V.J. Animal models of Middle East respiratory syndrome coronavirus infection. Antiviral Res. 2015;122:28–38. doi: 10.1016/j.antiviral.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baseler L., de Wit E., Feldmann H. A comparative review of animal models of Middle East respiratory syndrome coronavirus infection. Vet. Pathol. 2016;53:521–531. doi: 10.1177/0300985815620845. [DOI] [PubMed] [Google Scholar]
- 16.Johnson R.F., Bagci U., Keith L., Tang X., Mollura D.J., Zeitlin L., Qin J., Huzella L., Bartos C.J., Bohorova N. 3B11-N, a monoclonal antibody against MERS-CoV, reduces lung pathology in rhesus monkeys following intratracheal inoculation of MERS-CoV Jordan-n3/2012. Virology. 2016;490:49–58. doi: 10.1016/j.virol.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agrawal A.S., Ying T., Tao X., Garron T., Algaissi A., Wang Y., Wang L., Peng B.H., Jiang S., Dimitrov D.S. Passive transfer of a germline-like neutralizing human monoclonal antibody protects transgenic mice against lethal Middle East respiratory syndrome coronavirus infection. Sci. Rep. 2016;6:31629. doi: 10.1038/srep31629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Houser K.V., Gretebeck L., Ying T., Wang Y., Vogel L., Lamirande E.W., Bock K.W., Moore I.N., Dimitrov D.S., Subbarao K. Prophylaxis with a Middle East respiratory syndrome coronavirus (MERS-CoV)-specific human monoclonal antibody protects rabbits from MERS-CoV infection. J. Infect. Dis. 2016;213:1557–1561. doi: 10.1093/infdis/jiw080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pascal K.E., Coleman C.M., Mujica A.O., Kamat V., Badithe A., Fairhurst J., Hunt C., Strein J., Berrebi A., Sisk J.M. Pre- and postexposure efficacy of fully human antibodies against Spike protein in a novel humanized mouse model of MERS-CoV infection. Proc. Natl. Acad. Sci. U. S. A. 2015;112:8738–8743. doi: 10.1073/pnas.1510830112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao J., Perera R.A., Kayali G., Meyerholz D., Perlman S., Peiris M. Passive immunotherapy with dromedary immune serum in an experimental animal model for Middle East respiratory syndrome coronavirus infection. J. Virol. 2015;89:6117–6120. doi: 10.1128/JVI.00446-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luke T., Wu H., Zhao J., Channappanavar R., Coleman C.M., Jiao J.A., Matsushita H., Liu Y., Postnikova E.N., Ork B.L. Human polyclonal immunoglobulin G from transchromosomic bovines inhibits MERS-CoV in vivo. Sci. Transl. Med. 2016;8:326ra321. doi: 10.1126/scitranslmed.aaf1061. [DOI] [PubMed] [Google Scholar]
- 22.Min C.K., Cheon S., Ha N.Y., Sohn K.M., Kim Y., Aigerim A., Shin H.M., Choi J.Y., Inn K.S., Kim J.H. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci. Rep. 2016;6:25359. doi: 10.1038/srep25359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corman V.M., Albarrak A.M., Omrani A.S., Albarrak M.M., Farah M.E., Almasri M., Muth D., Sieberg A., Meyer B., Assiri A.M. Viral shedding and antibody response in 37 patients with Middle East respiratory syndrome coronavirus infection. Clin. Infect. Dis. 2016;62:477–483. doi: 10.1093/cid/civ951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park W.B., Perera R.A., Choe P.G., Lau E.H., Choi S.J., Chun J.Y., Oh H.S., Song K.H., Bang J.H., Kim E.S. Kinetics of serologic responses to MERS coronavirus infection in humans, South Korea. Emerg. Infect. Dis. 2015;21:2186–2189. doi: 10.3201/eid2112.151421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muth D., Corman V.M., Meyer B., Assiri A., Al-Masri M., Farah M., Steinhagen K., Lattwein E., Al-Tawfiq J.A., Albarrak A. Infectious Middle East respiratory syndrome coronavirus excretion and serotype variability based on live virus isolates from patients in Saudi Arabia. J. Clin. Microbiol. 2015;53:2951–2955. doi: 10.1128/JCM.01368-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao J., Li K., Wohlford-Lenane C., Agnihothram S.S., Fett C., Zhao J., Gale M.J., Jr., Baric R.S., Enjuanes L., Gallagher T. Rapid generation of a mouse model for Middle East respiratory syndrome. Proc. Natl. Acad. Sci. U. S. A. 2014;111:4970–4975. doi: 10.1073/pnas.1323279111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27••.Zhao J., Zhao J., Mangalam A.K., Channappanavar R., Fett C., Meyerholz D.K., Agnihothram S., Baric R.S., David C.S., Perlman S. Airway memory CD4(+) T cells mediate protective immunity against emerging respiratory coronaviruses. Immunity. 2016;44:1379–1391. doi: 10.1016/j.immuni.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows the efficacy of an anti-nucleocapsid vaccine for MERS-CoV, T-cell mediated protection and potential cross protection, and the role of route of administration in protection.
- 28.Wong R.S., Wu A., To K.F., Lee N., Lam C.W., Wong C.K., Chan P.K., Ng M.H., Yu L.M., Hui D.S. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ. 2003;326:1358–1362. doi: 10.1136/bmj.326.7403.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao J., Zhao J., Perlman S. T cell responses are required for protection from clinical disease and for virus clearance in severe acute respiratory syndrome coronavirus-infected mice. J. Virol. 2010;84:9318–9325. doi: 10.1128/JVI.01049-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Channappanavar R., Fett C., Zhao J., Meyerholz D.K., Perlman S. Virus-specific memory CD8 T cells provide substantial protection from lethal severe acute respiratory syndrome coronavirus infection. J. Virol. 2014;88:11034–11044. doi: 10.1128/JVI.01505-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang F., Quan Y., Xin Z.T., Wrammert J., Ma M.J., Lv H., Wang T.B., Yang H., Richardus J.H., Liu W. Lack of peripheral memory B cell responses in recovered patients with severe acute respiratory syndrome: a six-year follow-up study. J. Immunol. 2011;186:7264–7268. doi: 10.4049/jimmunol.0903490. [DOI] [PubMed] [Google Scholar]
- 32.Ng O.W., Chia A., Tan A.T., Jadi R.S., Leong H.N., Bertoletti A., Tan Y.J. Memory T cell responses targeting the SARS coronavirus persist up to 11 years post-infection. Vaccine. 2016;34:2008–2014. doi: 10.1016/j.vaccine.2016.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Payne D.C., Iblan I., Rha B., Alqasrawi S., Haddadin A., Al Nsour M., Alsanouri T., Ali S.S., Harcourt J., Miao C. Persistence of antibodies against Middle East respiratory syndrome coronavirus. Emerg. Infect. Dis. 2016;22:1824–1826. doi: 10.3201/eid2210.160706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cauchemez S., Fraser C., Van Kerkhove M.D., Donnelly C.A., Riley S., Rambaut A., Enouf V., van der Werf S., Ferguson N.M. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect. Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Majumder M.S., Kluberg S.A., Mekaru S.R., Brownstein J.S. Mortality risk factors for Middle East respiratory syndrome outbreak, South Korea, 2015. Emerg. Infect. Dis. 2015;21:2088–2090. doi: 10.3201/eid2111.151231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feikin D.R., Alraddadi B., Qutub M., Shabouni O., Curns A., Oboho I.K., Tomczyk S.M., Wolff B., Watson J.T., Madani T.A. Association of higher MERS-CoV virus load with severe disease and death, Saudi Arabia, 2014. Emerg. Infect. Dis. 2015;21:2029–2035. doi: 10.3201/eid2111.150764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thompson W.W., Shay D.K., Weintraub E., Brammer L., Cox N., Anderson L.J., Fukuda K. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 38.Del Giudice G., Weinberger B., Grubeck-Loebenstein B. Vaccines for the elderly. Gerontology. 2015;61:203–210. doi: 10.1159/000366162. [DOI] [PubMed] [Google Scholar]
- 39.Nagata N., Iwata N., Hasegawa H., Fukushi S., Harashima A., Sato Y., Saijo M., Taguchi F., Morikawa S., Sata T. Mouse-passaged severe acute respiratory syndrome-associated coronavirus leads to lethal pulmonary edema and diffuse alveolar damage in adult but not young mice. Am. J. Pathol. 2008;172:1625–1637. doi: 10.2353/ajpath.2008.071060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smits S.L., de Lang A., van den Brand J.M., Leijten L.M., van I.W.F., Eijkemans M.J., van Amerongen G., Kuiken T., Andeweg A.C., Osterhaus A.D. Exacerbated innate host response to SARS-CoV in aged non-human primates. PLoS Pathog. 2010;6:e1000756. doi: 10.1371/journal.ppat.1000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao J., Zhao J., Van Rooijen N., Perlman S. Evasion by stealth: inefficient immune activation underlies poor T cell response and severe disease in SARS-CoV-infected mice. PLoS Pathog. 2009;5:e1000636. doi: 10.1371/journal.ppat.1000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sheahan T., Whitmore A., Long K., Ferris M., Rockx B., Funkhouser W., Donaldson E., Gralinski L., Collier M., Heise M. Successful vaccination strategies that protect aged mice from lethal challenge from influenza virus and heterologous severe acute respiratory syndrome coronavirus. J. Virol. 2011;85:217–230. doi: 10.1128/JVI.01805-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43•.Channappanavar R., Zhao J., Perlman S. T cell-mediated immune response to respiratory coronaviruses. Immunol. Res. 2014;59:118–128. doi: 10.1007/s12026-014-8534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]; Review on the role of T-cells in protection against respiratory coronaviruses.
- 44.Zhao J., Zhao J., Legge K., Perlman S. Age-related increases in PGD(2) expression impair respiratory DC migration, resulting in diminished T cell responses upon respiratory virus infection in mice. J. Clin. Invest. 2011;121:4921–4930. doi: 10.1172/JCI59777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vijay R., Hua X., Meyerholz D.K., Miki Y., Yamamoto K., Gelb M., Murakami M., Perlman S. Critical role of phospholipase A2 group IID in age-related susceptibility to severe acute respiratory syndrome-CoV infection. J. Exp. Med. 2015;212:1851–1868. doi: 10.1084/jem.20150632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Boheemen S., de Graaf M., Lauber C., Bestebroer T.M., Raj V.S., Zaki A.M., Osterhaus A.D., Haagmans B.L., Gorbalenya A.E., Snijder E.J. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. MBio. 2012;3 doi: 10.1128/mBio.00473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agnihothram S., Gopal R., Yount B.L., Jr., Donaldson E.F., Menachery V.D., Graham R.L., Scobey T.D., Gralinski L.E., Denison M.R., Zambon M. Evaluation of serologic and antigenic relationships between middle eastern respiratory syndrome coronavirus and other coronaviruses to develop vaccine platforms for the rapid response to emerging coronaviruses. J. Infect. Dis. 2014;209:995–1006. doi: 10.1093/infdis/jit609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mou H., Raj V.S., van Kuppeveld F.J., Rottier P.J., Haagmans B.L., Bosch B.J. The receptor binding domain of the new Middle East respiratory syndrome coronavirus maps to a 231-residue region in the spike protein that efficiently elicits neutralizing antibodies. J. Virol. 2013;87:9379–9383. doi: 10.1128/JVI.01277-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Agrawal A.S., Tao X., Algaissi A., Garron T., Narayanan K., Peng B.H., Couch R.B., Tseng C.T. Immunization with inactivated Middle East respiratory syndrome coronavirus vaccine leads to lung immunopathology on challenge with live virus. Hum. Vaccines Immunother. 2016;12:2351–2356. doi: 10.1080/21645515.2016.1177688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Song F., Fux R., Provacia L.B., Volz A., Eickmann M., Becker S., Osterhaus A.D., Haagmans B.L., Sutter G. Middle East respiratory syndrome coronavirus spike protein delivered by modified vaccinia virus Ankara efficiently induces virus-neutralizing antibodies. J. Virol. 2013;87:11950–11954. doi: 10.1128/JVI.01672-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Volz A., Kupke A., Song F., Jany S., Fux R., Shams-Eldin H., Schmidt J., Becker C., Eickmann M., Becker S. Protective efficacy of recombinant modified vaccinia virus ankara delivering Middle East respiratory syndrome coronavirus spike glycoprotein. J. Virol. 2015;89:8651–8656. doi: 10.1128/JVI.00614-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52••.Haagmans B.L., van den Brand J.M., Raj V.S., Volz A., Wohlsein P., Smits S.L., Schipper D., Bestebroer T.M., Okba N., Fux R. An orthopoxvirus-based vaccine reduces virus excretion after MERS-CoV infection in dromedary camels. Science. 2016;351:77–81. doi: 10.1126/science.aad1283. [DOI] [PubMed] [Google Scholar]; Investigation of a MERS-CoV vaccine for camels, showing a potential protective efficacy.
- 53.Kim E., Okada K., Kenniston T., Raj V.S., AlHajri M.M., Farag E.A., AlHajri F., Osterhaus A.D., Haagmans B.L., Gambotto A. Immunogenicity of an adenoviral-based Middle East respiratory syndrome coronavirus vaccine in BALB/c mice. Vaccine. 2014;32:5975–5982. doi: 10.1016/j.vaccine.2014.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guo X., Deng Y., Chen H., Lan J., Wang W., Zou X., Hung T., Lu Z., Tan W. Systemic and mucosal immunity in mice elicited by a single immunization with human adenovirus type 5 or 41 vector-based vaccines carrying the spike protein of Middle East respiratory syndrome coronavirus. Immunology. 2015;145:476–484. doi: 10.1111/imm.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Malczyk A.H., Kupke A., Prufer S., Scheuplein V.A., Hutzler S., Kreuz D., Beissert T., Bauer S., Hubich-Rau S., Tondera C. A highly immunogenic and protective Middle East respiratory syndrome coronavirus vaccine based on a recombinant measles virus vaccine platform. J. Virol. 2015;89:11654–11667. doi: 10.1128/JVI.01815-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wirblich C., Coleman C.M., Kurup D., Abraham T.S., Bernbaum J.G., Jahrling P.B., Hensley L.E., Johnson R.F., Frieman M.B., Schnell M.J. One-health: a safe, efficient, dual-use vaccine for humans and animals against Middle East respiratory syndrome coronavirus and rabies virus. J. Virol. 2017;91 doi: 10.1128/JVI.02040-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cockrell A.S., Yount B.L., Scobey T., Jensen K., Douglas M., Beall A., Tang X.C., Marasco W.A., Heise M.T., Baric R.S. A mouse model for MERS coronavirus-induced acute respiratory distress syndrome. Nat Microbiol. 2016;2:16226. doi: 10.1038/nmicrobiol.2016.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang L., Shi W., Joyce M.G., Modjarrad K., Zhang Y., Leung K., Lees C.R., Zhou T., Yassine H.M., Kanekiyo M. Evaluation of candidate vaccine approaches for MERS-CoV. Nat. Commun. 2015;6:7712. doi: 10.1038/ncomms8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Muthumani K., Falzarano D., Reuschel E.L., Tingey C., Flingai S., Villarreal D.O., Wise M., Patel A., Izmirly A., Aljuaid A. A synthetic consensus anti-spike protein DNA vaccine induces protective immunity against Middle East respiratory syndrome coronavirus in nonhuman primates. Sci. Transl. Med. 2015;7:301ra132. doi: 10.1126/scitranslmed.aac7462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang C., Zheng X., Gai W., Zhao Y., Wang H., Wang H., Feng N., Chi H., Qiu B., Li N. MERS-CoV virus-like particles produced in insect cells induce specific humoural and cellular imminity in rhesus macaques. Oncotarget. 2016 doi: 10.18632/oncotarget.8475. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coleman C.M., Liu Y.V., Mu H., Taylor J.K., Massare M., Flyer D.C., Glenn G.M., Smith G.E., Frieman M.B. Purified coronavirus spike protein nanoparticles induce coronavirus neutralizing antibodies in mice. Vaccine. 2014;32:3169–3174. doi: 10.1016/j.vaccine.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang Y., Deng Y., Wen B., Wang H., Meng X., Lan J., Gao G.F., Tan W. The amino acids 736-761 of the MERS-CoV spike protein induce neutralizing antibodies: implications for the development of vaccines and antiviral agents. Viral Immunol. 2014;27:543–550. doi: 10.1089/vim.2014.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jiaming L., Yanfeng Y., Yao D., Yawei H., Linlin B., Baoying H., Jinghua Y., Gao G.F., Chuan Q., Wenjie T. The recombinant N-terminal domain of spike proteins is a potential vaccine against Middle East respiratory syndrome coronavirus (MERS-CoV) infection. Vaccine. 2017;35:10–18. doi: 10.1016/j.vaccine.2016.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lan J., Yao Y., Deng Y., Chen H., Lu G., Wang W., Bao L., Deng W., Wei Q., Gao G.F. Recombinant receptor binding domain protein induces partial protective immunity in rhesus macaques against middle east respiratory syndrome coronavirus challenge. EBioMedicine. 2015;2:1438–1446. doi: 10.1016/j.ebiom.2015.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lan J., Deng Y., Chen H., Lu G., Wang W., Guo X., Lu Z., Gao G.F., Tan W. Tailoring subunit vaccine immunity with adjuvant combinations and delivery routes using the Middle East respiratory coronavirus (MERS-CoV) receptor-binding domain as an antigen. PLoS One. 2014;9:e112602. doi: 10.1371/journal.pone.0112602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ma C., Wang L., Tao X., Zhang N., Yang Y., Tseng C.T., Li F., Zhou Y., Jiang S., Du L. Searching for an ideal vaccine candidate among different MERS coronavirus receptor-binding fragments—the importance of immunofocusing in subunit vaccine design. Vaccine. 2014;32:6170–6176. doi: 10.1016/j.vaccine.2014.08.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang N., Channappanavar R., Ma C., Wang L., Tang J., Garron T., Tao X., Tasneem S., Lu L., Tseng C.T. Identification of an ideal adjuvant for receptor-binding domain-based subunit vaccines against Middle East respiratory syndrome coronavirus. Cell Mol. Immunol. 2016;13:180–190. doi: 10.1038/cmi.2015.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tang J., Zhang N., Tao X., Zhao G., Guo Y., Tseng C.T., Jiang S., Du L., Zhou Y. Optimization of antigen dose for a receptor-binding domain-based subunit vaccine against MERS coronavirus. Hum. Vaccines Immunother. 2015;11:1244–1250. doi: 10.1080/21645515.2015.1021527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tai W., Zhao G., Sun S., Guo Y., Wang Y., Tao X., Tseng C.K., Li F., Jiang S., Du L. A recombinant receptor-binding domain of MERS-CoV in trimeric form protects human dipeptidyl peptidase 4 (hDPP4) transgenic mice from MERS-CoV infection. Virology. 2016;499:375–382. doi: 10.1016/j.virol.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ma C., Li Y., Wang L., Zhao G., Tao X., Tseng C.T., Zhou Y., Du L., Jiang S. Intranasal vaccination with recombinant receptor-binding domain of MERS-CoV spike protein induces much stronger local mucosal immune responses than subcutaneous immunization: implication for designing novel mucosal MERS vaccines. Vaccine. 2014;32:2100–2108. doi: 10.1016/j.vaccine.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Drosten C., Muth D., Corman V.M., Hussain R., Al Masri M., HajOmar W., Landt O., Assiri A., Eckerle I., Al Shangiti A. An observational, laboratory-based study of outbreaks of middle East respiratory syndrome coronavirus in Jeddah and Riyadh, kingdom of Saudi Arabia, 2014. Clin. Infect. Dis. 2015;60:369–377. doi: 10.1093/cid/ciu812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sui J., Deming M., Rockx B., Liddington R.C., Zhu Q.K., Baric R.S., Marasco W.A. Effects of human anti-spike protein receptor binding domain antibodies on severe acute respiratory syndrome coronavirus neutralization escape and fitness. J. Virol. 2014;88:13769–13780. doi: 10.1128/JVI.02232-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tang X.C., Agnihothram S.S., Jiao Y., Stanhope J., Graham R.L., Peterson E.C., Avnir Y., Tallarico A.S., Sheehan J., Zhu Q. Identification of human neutralizing antibodies against MERS-CoV and their role in virus adaptive evolution. Proc. Natl. Acad. Sci. U. S. A. 2014;111:E2018–E2026. doi: 10.1073/pnas.1402074111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tai W., Wang Y., Fett C.A., Zhao G., Li F., Perlman S., Jiang S., Zhou Y., Du L. Recombinant receptor-binding domains of multiple MERS-coronaviruses induce cross-neutralizing antibodies against divergent human and camel MERS-coronaviruses and antibody-escape mutants. J. Virol. 2016;91(Dec 16 (1)) doi: 10.1128/JVI.01651-16. pii: e01651-16. Print 2017 Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chan K.H., Chan J.F., Tse H., Chen H., Lau C.C., Cai J.P., Tsang A.K., Xiao X., To K.K., Lau S.K. Cross-reactive antibodies in convalescent SARS patients’ sera against the emerging novel human coronavirus EMC (2012) by both immunofluorescent and neutralizing antibody tests. J. Infect. 2013;67:130–140. doi: 10.1016/j.jinf.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76•.Du L., Tai W., Yang Y., Zhao G., Zhu Q., Sun S., Liu C., Tao X., Tseng C.K., Perlman S. Introduction of neutralizing immunogenicity index to the rational design of MERS coronavirus subunit vaccines. Nat. Commun. 2016;7:13473. doi: 10.1038/ncomms13473. [DOI] [PMC free article] [PubMed] [Google Scholar]; Using epitope masking as an approach for immunefocusing and production of robust (stronger) immune responses.
- 77.Yip M.S., Leung N.H., Cheung C.Y., Li P.H., Lee H.H., Daeron M., Peiris J.S., Bruzzone R., Jaume M. Antibody-dependent infection of human macrophages by severe acute respiratory syndrome coronavirus. Virol. J. 2014;11:82. doi: 10.1186/1743-422X-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jaume M., Yip M.S., Kam Y.W., Cheung C.Y., Kien F., Roberts A., Li P.H., Dutry I., Escriou N., Daeron M. SARS CoV subunit vaccine: antibody-mediated neutralisation and enhancement. Hong Kong Med. J. 2012;18(Suppl 2):31–36. [PubMed] [Google Scholar]
- 79.Wang S.F., Tseng S.P., Yen C.H., Yang J.Y., Tsao C.H., Shen C.W., Chen K.H., Liu F.T., Liu W.T., Chen Y.M. Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem. Biophys. Res. Commun. 2014;451:208–214. doi: 10.1016/j.bbrc.2014.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vaccine initiative marks bold resolution. Nature 2017, 541:436. [DOI] [PubMed]
- 81.Almazan F., DeDiego M.L., Sola I., Zuniga S., Nieto-Torres J.L., Marquez-Jurado S., Andres G., Enjuanes L. Engineering a replication-competent, propagation-defective Middle East respiratory syndrome coronavirus as a vaccine candidate. MBio. 2013;4:e00650–00613. doi: 10.1128/mBio.00650-13. [DOI] [PMC free article] [PubMed] [Google Scholar]