Abstract
Middle East Respiratory Syndrome Coronavirus (MERS-CoV) is an emerging disease with a relatively high case fatality rate. Most cases have been reported from Saudi Arabia, and the disease epidemic potential is considered to be limited. However, human–human transmission has occurred, usually in the context of healthcare facility-associated outbreaks. The scientific and medical community depends on timely publication of epidemiological information on emerging diseases during outbreaks to appropriately target public health responses. In this review, we considered the academic response to four MERS CoV outbreaks that occurred in Al-Hasa in 2013, Jeddah in 2014 and Riyadh in 2014 and 2015. We analysed 68 relevant epidemiology articles. For articles for which submission dates were available, six articles were submitted during the course of an outbreak. One article was published within a month of the Al-Hasa outbreak, and one each was accepted during the Jeddah and Riyadh outbreaks. MERS-CoV epidemiology articles were cited more frequently than articles on other subjects in the same journal issues. Thus, most epidemiology articles on MERS-CoV were published with no preferential advantage over other articles. Collaboration of the research community and the scientific publishing industry is needed to facilitate timely publication of emerging infectious diseases.
Keywords: Middle East Respiratory Syndrome Coronavirus, Outbreak, Epidemiology, Publication, Saudi Arabia, MERS-CoV
Introduction
Emerging infectious diseases are a growing cause of major concern worldwide in terms of public health [1]. The importance of immediate collection of reliable epidemiological information, appropriate analysis, and rapid dissemination to relevant stakeholders during an outbreak, is well-recognised in terms of the public health response and containment of the outbreak [2], [3]. Information on the causative agent, likely routes of transmission and prediction of how the outbreak might spread, diagnostic criteria, and possible treatments are all relevant. Such information allows public health experts in both national and international agencies and in research settings to formulate and implement prevention policies and strategies based on updated evidence. Dissemination of public health information can be achieved by a number of methods such as online, specialised peer reviewed papers or, for example, on the World Health Organization (WHO) website [4]. However, the primary method for communicating research findings is through the medium of journal articles [5].
One example of a recent emerging infectious disease is the Middle East Respiratory Syndrome Coronavirus (MERS-CoV), a betacoronavirus, which can cause acute respiratory illness in humans, with clinical presentation ranging from asymptomatic to death [6], [7]. It was first observed in a 60-year old man with acute pneumonia and subsequent renal failure, who died in a hospital in Jeddah, Saudi Arabia in 2012 [8]. The first human cluster of eleven cases was confirmed retrospectively in a public hospital in Jordan in April 2012 [9]. To date, WHO has been notified of 1800 laboratory-confirmed cases from 27 countries, and of 640 deaths [10]. Most outbreaks have occurred in the Arabian Peninsula, in particular in Saudi Arabia, with occasional spread to other countries, including an outbreak in Korea in 2015 [6]. There have been numerous outbreaks in Saudi Arabia, for example 25 cases in Al-Hasa between April 1st and May 23rd 2013 [11], 255 patients in Jeddah between January 1st and May 16th, 2014 [12], [13], 45 patients between March 29th and May 21st, 2014 in King Fahad Medical City in Riyadh, Prince Sultan Military Medical City, between March and April 2014 [14], [15], and 130 MERS cases at King Abulaziz Medical City in Riyadh in June–August 2015 [16].
Comparison of queries of the online clinical decision support resource UpToDate with reports of cases was recently shown to be helpful in detection and monitoring of outbreaks of MERS-CoV in Saudi Arabia [17]. Another study examining data related to MERS on the internet-based participatory surveillance system HealthMap suggested that such resources can be helpful in outbreak monitoring [18].
In this review, we analysed the academic publications to four outbreaks that occurred in Saudi Arabia: Al-Hasa 2013, Jeddah 2014 and Riyadh 2014 and 2015. A similar analysis of two outbreaks of severe acute respiratory syndrome (SARS) showed that most articles were published after the outbreaks had ended, even though they had direct public health relevance during the outbreaks [5]. Our analysis included the epidemiology categories and research domains in which journal articles on the four MERS-CoV outbreaks were published; the methodological characteristics of studies in terms of type, design, case definition, and setting; the timeline of publication of studies in relation to the time of the outbreak; and the scientific impact of MER-CoV articles, in terms of level of citations compared to simultaneously published control articles.
Materials and methods
Literature review
We searched the MEDLINE database for all published articles on epidemiology of the MERS-CoV outbreaks in Al-Hasa in 2013 [11], Jeddah in 2014 [12], [13], and Riyadh in 2014 [14], [15] and 2015 [16]. We searched for all journal articles written in English in which the main subject studied was one of the above MERS-CoV outbreaks. The searches focused on journal articles published during each outbreak to the present. Outbreak dates were taken based on the WHO and the Saudi Ministry of Health (MOH). These dates were (1) April 1st and May 23rd 2013 for the Al-Hasa outbreak, (2) January 1st and May 16th, 2014 for the Jeddah outbreak, (3) March 29th and May 21st, 2014 for the Riyadh 2014 outbreak and (4) June–September 28th 2015 for the Riyadh 2015 outbreak [11], [12], [13], [16]. The literature search was carried out in September 2016. Separate searches were carried out for each outbreak. The following search equation was initially used for the Al-Hasa outbreak to maximise retrieval of potentially relevant articles and to exclude publication types other than journal research articles:
Search strategy: [Middle East Respiratory Syndrome coronavirus OR MERS-CoV] AND All fields: [Al-Hasa OR Al-Ahsa] AND Publication type: [Journal article] AND Language: [English] AND Date-publication [2013/04/01-Present].
The search was modified with respect to the location and the start date depending on the outbreak under consideration. Thus for the Jeddah outbreak, [Al-Hasa OR Al-Ahsa] was replaced by [Jeddah] and the Date-publication was changed to [2014/01/01-Present], and for the Riyadh 2014 and 2015 outbreaks, [Al-Hasa OR Al-Ahsa] was replaced by [Riyadh] and the Date-publication was changed to [2014/03/29-Present], covering both Riyadh outbreaks. Searches excluded articles with the following exclusion criteria, adapted from Xing et al. [5]: (1) The main study objective was not MERS-CoV; (2) The data analysed in the study were not collected from the relevant outbreak(s), for example for outbreaks in other countries or different outbreaks in Saudi Arabia, or it was unclear from which outbreak the data had been gathered, as no dates were given; (3) The data analysed in the study were related to a subject other than epidemiology of the relevant outbreak(s), such as feasibility studies for proposed therapies, animal studies on viral effects; (4) The article was not an original study, for example a review or a letter; (5) The study was carried out using only qualitative methodology; (6) The study sample size was <3 cases.
Further searches were carried out using the Web of Science Core Collection, in order to collect any relevant articles not detected in MEDLINE searches. The search equation used for the Al-Hasa outbreak was: Title: [Middle East Respiratory Syndrome coronavirus OR MERS-CoV] AND Topic: [Al-Hasa OR Al-Ahsa]. The search was refined to include only references from 2013 to the present, in English, in the categories Public Environmental & Occupational Health and Infectious Diseases. For the other outbreaks, [Al-Hasa] was changed to [Jeddah] or [Riyadh] accordingly, and the start date changed to 2014 or 2015 as appropriate.
In order to compare the timeline for publication dates in academic research journals to publication of public health bulletins, we also searched public health bulletins for any relevant outbreaks from the start of the earliest outbreak (Al-Hasa, 01/04/2014) to the present. We searched Morbidity and Mortality Weekly Report (MMWR) from the Centers for Disease Control and Prevention (CDC), and the World Health Organization (WHO) Weekly Epidemiological Report (WER) and monthly Bulletin of the World Health Organization. At the time of the literature review and spanning the time of the MERS-CoV outbreaks, the Saudi Epidemiology Bulletin was inaccessible for the relevant time period, with issues only available online up to 2012 [http://fetp.edu.sa/Bulletin.html, accessed 31.08.2016].
Data analysed
Articles were classified as in Xing et al. [5] according to four categories (1) investigation and surveillance; (2) case management; (3) prevention and control; and (4) psychobehavioural aspects. Details for each study were recorded in a data-collection grid including authors, study title and journal, volume and date of publication, study design and type, domain, setting, and study characteristics, such as sample size (initial and final if applicable for study design), case definition criteria, location of patient recruitment and type of data collection. We also recorded where possible statistical analyses information, and data quality assurance processes, such as use of double-data entry, double blinding, or checking data for errors, if described in material and methods section.
Publication timeline and MERS-CoV study citations
We determined the timeline for publication and citation of retained articles, where submission, acceptance and publication dates were known. Submission and acceptance dates were derived from the journals or MEDLINE records, while publication date was taken as when the article was first became available in full text format; when both a print and an online publication dates were available, the publication date was taken as the earlier of the two. If only a publication month was available, the date was assumed to be the 15th of the month. Number of citations for an article on a particular outbreak was based on the Web of Science (Thomas Reuters) record on 7th September 2016 (https://apps.webofknowledge.com/). The impact factor of the journal in which each retained article was published was noted from the Journal of Citation Reports database for 2015 (Thomas Reuters). The impact factors for articles published within one year of the relevant outbreak were compared to the impact factors for articles published thereafter. To provide a control sample of articles, the submission-to-acceptance and acceptance-to-publication sequences and the citation number within six months and thereafter was also recorded for two articles within the same journal issue as each MERS-CoV article being analysed. This would allow us to determine if the MERS-CoV articles were cited more frequently than articles on other subjects published in the same journal issues. In each case, we selected control articles that either immediately preceded or immediately followed the relevant MERS-CoV article. The selection depended on the pagination in the particular journal issue. For example, if the MERS-CoV article was the first article in an issue, we chose the two following articles (of the same type) as the controls, but if it was the last article we picked the two preceding articles (of the same type) as controls. If the MERS-CoV article was somewhere in the middle, we picked the article immediately before and the article immediately after as controls.
Statistical analyses
Data were analyzed using Excel (Microsoft Corporation, Redmond, WA, USA) with Real Statistics add-ins (http://www.real-statistics.com/) and/or Social Science Statistics (http://www.socscistatistics.com/Default.aspx). Kruskan–Wallis analysis was carried out to compare medians for submission-acceptance and acceptance-publication times and numbers of citations between MERS-CoV and control articles and for the articles submitted during any of the four outbreaks to all other articles for which data was available for journal impact factors, numbers of citations and time period between submissions to publication. A p ≤ 0.05 was taken as significant. Kaplan–Meier curves were generated and log-rank test analyses were carried out to compare proportions of MERS-CoV versus control articles under review (submission-acceptance) or under publication (acceptance-publication) for time periods from 0 to 400 days. A p ≤ 0.05 was accepted as significant.
Results
Literature review
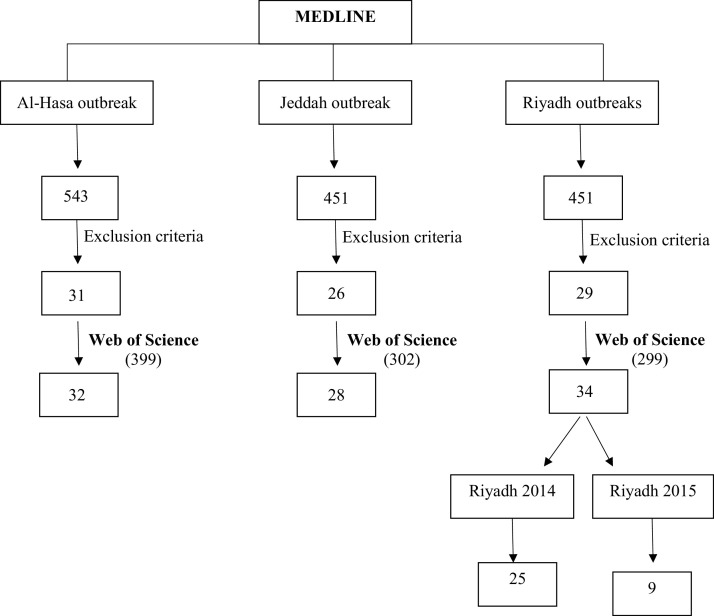
The initial MEDLINE searches produced 543 articles for Al-Hasa, 451 articles for Jeddah, and 451 articles for Riyadh. Most articles were retrieved in more than one of the searches, and in some cases an article retrieved in a particular search proved to be more relevant to another outbreak. For the Web of Science searches, there were 399 articles for Al-Hasa, 302 for Jeddah and 299 for Riyadh. There was substantial overlap with the MEDLINE results. Fig. 1 shows a flow diagram for selection of the final 68 unique articles after exclusion criteria were applied and articles were combined from MEDLINE and Web of Science searches [11], [12], [13], [14], [15], [16], [17], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79]. When these 68 articles (Supplementary Appendix 1) were assigned to the most relevant outbreak, sixteen of the 68 articles were common to two, three or all outbreaks, covering for example evolutionary analyses in which sequences of viruses from more than one of the outbreaks were used, or epidemiology of the whole country (Table 1 ). The final result, when these sixteen articles were distributed, was that the Al-Hasa outbreak featured in 32 articles, either alone or in combination with other outbreaks, the Jeddah outbreak in 28 articles, the Riyadh 2014 outbreak in 25 articles and the Riyadh 2015 outbreak in nine articles (Table 1, Table 2).
Fig. 1.
Flow diagram for article selection process.
Table 1.
Breakdown of selected articles.
| Outbreak(s) | Number of articles |
|---|---|
| Al-Hasa only | 23 |
| Al-Hasa + Jeddah | 2 |
| Al-Hasa + Jeddah + Riyadh 2014 | 3 |
| Al-Hasa + Riyadh 2014 | 1 |
| Jeddah only | 13 |
| Jeddah + Riyadh 2014 | 5 |
| Jeddah + Riyadh 2015 | 1 |
| Jeddah + Riyadh 2014 and 2015 | 1 |
| Riyadh 2014 only | 12 |
| Riyadh 2015 only | 4 |
| All outbreaks | 3 |
| Total | 68 |
Table 2.
Distribution of articles by outbreak.
| Outbreak | Number of article |
||
|---|---|---|---|
| Alone | Combination | Total | |
| Al-Hasa | 23 | 9 | 32 |
| Jeddah | 13 | 15 | 28 |
| Riyadh 2014 | 12 | 13 | 25 |
| Riyadh 2015 | 4 | 5 | 9 |
| Total | 52 | 42 | 94 |
Total of 94 arises from the sum of articles considering each outbreak alone and in combination with other outbreak(s), thus few of the 68 articles (Table 1) are counted more than once.
The public health bulletins searches of MMWR, WER and the monthly Bulletin of the WHO revealed few articles specific to any of the outbreaks and none were published during the relevant outbreaks. In MMWR, a search of ‘Middle East Respiratory Syndrome coronavirus OR MERS-CoV’ covering from the start of the Al-Hasa outbreak (April 1st 2013) to the present uncovered seven articles, in which two (June 14th 2013 and September 27th 2013) specifically mentioned the Al-Hasa outbreak while one (February 19th 2016) specifically mentioned the Riyadh 2015 outbreak. Five records in the WER for the same time period referenced MERS-CoV, but were not specific to the relevant outbreaks. The articles focused for example on prevention and control guidelines, including travel advice for Hajj pilgrims. In the same period, the Bulletin of the World Health Organization included six MERS-CoV articles, including Public Health Round-ups, and article on pilgrims returning from Hajj, and an article on steps that should be taken regarding surveillance, awareness raising and diagnostic testing capacity, but none specific to any of the outbreaks in this review. The Ministry of Health for Kingdom of Saudi Arabia portal provides daily reports on new cases as they arise, including the cases in the relevant outbreaks [http://www.moh.gov.sa/].
Study characteristics
The articles were divided into four categories, which could be further divided into research domains, as shown in Table 3 . Where an article contained elements of more than one category, it was categorised into the category that dominated the subject matter of the article. Supplementary Appendix 1 shows the categorisation of each of the 68 final articles according to study characteristics. The majority of articles were in the ‘Investigation and surveillance’ category (57.4%), with 33.8% of articles mainly concerned with aspects of viral transmission. And 29.4% of the articles were in the ‘Case management’ category, 10.3% in ‘Prevention and control’ and 2.9% in ‘Psychobehavior’ (Table 3).
Table 3.
Research domains for selected articles.
| Category | Research domain | Number of articles |
|---|---|---|
| 1. Investigation and surveillance | Description of outbreak (location, time, patients) | 6 |
| Causative agent (identification, characteristics) | 1 | |
| Transmission (modes, routes, probability, future outbreak trends) | 23 | |
| Risk factors | 9 | |
| Sub-total | 39 | |
| 2. Case management | Clinical presentation | 11 |
| Treatments/medical interventions (efficacy, adverse events) | 7 | |
| Prognosis (patient outcomes) | 2 | |
| Sub-total | 20 | |
| 3. Prevention and control | Prevention and control measures- use, effectiveness, monitoring | 7 |
| 4. Psychobehavior | Awareness, risk perception, personal attitudes, preventive measures | 2 |
| Total | 68 | |
In terms of the study types, they were either descriptive epidemiology (60.3%) or analytic epidemiology (39.7%) (studies to quantify the association between exposures and outcomes and/or establish causal relationships). Studies were retrospective cohort studies (52.9%), prospective cohort studies (11.8%) or descriptive (longitudinal) cohort studies (14.7%) (Supplementary Appendix 1). The remainder studies were mathematical modelling studies (16.2%) or case control-studies (4.4%). The majority of recruitment occurred in hospitals/primary healthcare centres (76.5%), the community (7.4%), laboratory (5.9%) or college (1.5%), with 8.8% not specified/applicable. In most cases, data was used that was initially collected for other purposes, in particular hospital, medical or exposure records (58.8%; including three where biological specimens were also collected and one where interviews were also performed) or secondary data re-analysis from other studies (5.9%), while the remainder was from biological specimen collection (16.2%), questionnaires (8.8%), sequence data (5.9%; including two where biological specimens were also collected), or was not specified (4.4%). In most studies, MERS-CoV was confirmed by means of PCR (75%), as recommended by the CDC and WHO, sometimes in combination with clinical signs and once with western blotting (Supplementary Appendix 1). Presence of anti-MERS-CoV protein antibodies was included in three studies (4.4%). Nine studies (13.2%) included awareness, emotional responses or guidelines arising from an outbreak, and in five studies it was not specified (7.4%) (Supplementary Appendix 1). Sample size was reported in 61 studies (89.7%), with a median of 105 cases. In studies with no sample size, the studies were revision of infection prevention and control standards or correlation of online reports with reported cases (Supplementary Appendix 1).
In terms of data quality assurance/control, there were few studies that specified which processes were applied. In six studies, there was some form of double-data entry and/or double-blinding, while in eight studies there was some element of checking data for errors (Supplementary Appendix 1).
Journals publishing MERS-CoV articles
The 68 selected articles were published in 40 different journals. Some journals published more than one article. Seven articles were published in Emerging Infectious Diseases (10.3%) and six in the International Journal of Infectious Diseases (8.8%), four each were published in Lancet Infectious Diseases and in Clinical Infectious Diseases (5.9% each) and three (4.4%) each in the American Journal of Roentgenology, Eurosurveillance and mBio. Two (2.9%) were published in each of Epidemics, Lancet, New England Journal of Medicine and PLoS Current Outbreaks. The median impact factor for the 40 journals publishing the 68 retained articles was 3.44 (Interquartile range (IQR) 5.88).
Publication timeline
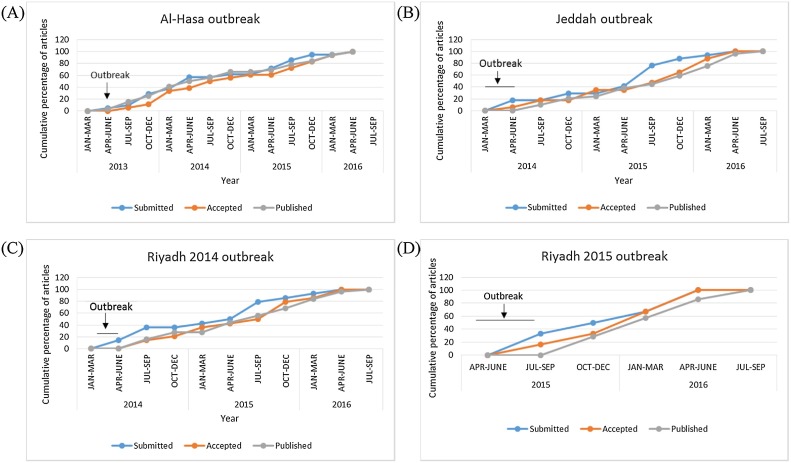
When dates were available, we derived the publication timelines for the retained articles for each of the four outbreaks. Fig. 2 shows the cumulative percentages of articles submitted, published and accepted for each outbreak, from the beginning of the relevant outbreak to the present, Fig. 2A: Al-Hasa (21 articles), Fig. 2B: Jeddah (17 articles), Fig. 2C: Riyadh 2014 (14 articles), Fig. 2D: Riyadh 2015 (7 articles). The timing of the outbreak is indicated on each graph to illustrate that submission, acceptance and publication of the majority of articles occurred after the outbreaks. One of the retained articles was submitted during the Al-Hasa outbreak and published within a month [41], two were submitted and one accepted during the Jeddah outbreak [19], [45], one was submitted for the Riyadh 2014 outbreak [78], and two articles were submitted and one accepted during the Riyadh 2015 outbreak [44], [51] (Fig. 2). This left insufficient numbers of articles to compare impact factors, submission timelines and numbers of citations for articles submitted, accepted or published during any particular outbreak to those submitted, accepted or published after the same outbreak.
Fig. 2.
Cumulative percentages of submitted, accepted and published articles for each outbreak.
The information on submission date was obtained directly from the journals or medline records (Section 2.3 of the materials and methods section).
(A) Al-Hasa; (B) Jeddah; (C) Riyadh 2014; (D) Riyadh 2015.
MERS CoV article characteristics compared to control articles
We determined if there were any differences in timelines from submission-to-acceptance or acceptance-to-publication, or number of article citations, for articles published on any of the MERS-CoV outbreaks compared to control articles on other subjects in the same journal issue.
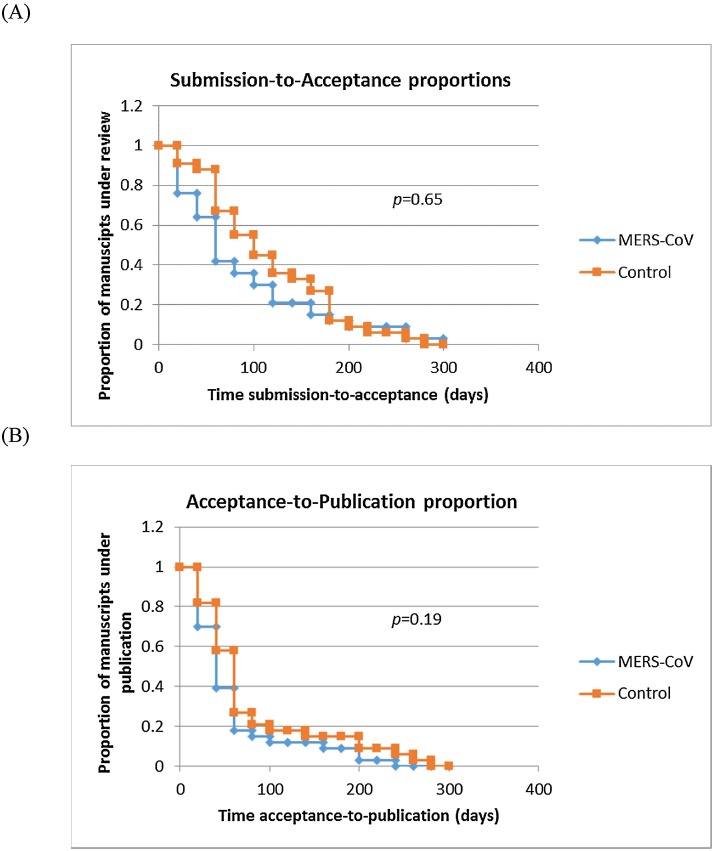
Fig. 3 shows Kaplan–Meier curves representing the proportion of articles under submission/review (Fig. 3A), and the proportion of articles under publication (accepted) for time periods from 0 to 400 days for MERS-CoV versus control articles (Fig. 3B). Log-rank analyses showed no significant difference in hazard rates for submission-to-acceptance (z = 0.45, p = 0.65) or acceptance-to-publication (z = 1.3, p = 0.19) for MERS-CoV versus control articles. There was no statistical difference in the median time of submission-acceptance for MERS-CoV articles and control articles (median 57.5 vs. 83.5 days) (p = 0.065). Likewise, there was no significant difference between the median acceptance-publication times for MERS-CoV versus control articles (medians 34.5 and 43 days respectively; p = 0.132). However, the median citation numbers for MERS-CoV was significantly higher for MERS-CoV articles vs. Controls (medians 6.5 and 1 respectively; p = 0.012).
Fig. 3.
Comparison of publication interval between MERS CoV and control articles. (A) Submission to acceptance proportions (B) acceptance to publication proportions. Kaplan–Meier curves and log-rank analyses for the submission-to-acceptance (A) and acceptance-to-submission times for MERS-CoV versus control articles.
Discussion
Immediate and reliable collection, analysis and dissemination of epidemiological information during infectious disease outbreaks are critical for filling in the knowledge gaps [2], [3], [4]. The primary method for communicating research findings in the medical and scientific community is via journal articles [5]. However, the results of our study show that the majority of publications on epidemiology of MERS-CoV outbreaks in Al-Hasa, Jeddah and Riyadh occurred after the outbreaks had ended. Submission-to-acceptance or acceptance-to-publication times were not significantly different for articles on MERS-CoV outbreak epidemiology compared to control articles. Articles that were eventually published were dominated by descriptive epidemiology and were mainly in the investigation and surveillance domain. Most epidemiology articles on MERS-CoV were published with no preferential advantage over other articles indicating non-expedited review and publication time.
There are various factors that contribute to delayed publication of articles, including author-related and journal-related factors [5]. Input from the epidemiological research community and the scientific publishing industry would be important to facilitate timely publication of emerging infectious diseases. Author-related factors that can result in submission and publication delays include: the time needed to prepare and disseminate protocols, questionnaires and surveys, as well as to prepare the publication for initial submission, choose an appropriate journal, and prepare further submissions necessitated by rejection by the first-choice journal [5]. Publisher-related delays can relate to identification of appropriate reviewers, waiting for reviews, deciding on whether to publish on the basis of the reviews and technical aspects of journal preparation [5]. Publication likelihood can be influenced by factors including geographical location of the researchers, study domain, the disease under consideration, the novelty of the study and positive or negative results [80], [81].
It is important to ensure the quality of studies by a robust peer-review process. However, there are developments in the medical and scientific publishing industry that may help in expediting the process of article publication in future emerging infectious diseases. It is important to minimise the delay between generating and publishing research, by streamlining peer-review process, and targeting specific research audiences. It is also important to offer fast-track and rapid publication options, particularly to advanced online publication. Publication costs and fees can be a barrier to researchers, particularly in developing countries. For epidemiology research, standardization of protocols and questionnaires, and greater accessibility of real-time online information systems, would be of assistance to researchers for rapid collection, analysis and dissemination of research. The need for better data management was identified as an issue in the recent Ebola outbreak [82]. An example of this need is in terms of improved data harmonization and access to application tools. Standardization of protocols would assist in timely production of epidemiological studies. The European Centre for Disease Prevention and Control (ECDC) has published a comprehensive handbook on methods and applications in monitoring of data quality and evaluation of surveillance systems [83], [84].
Other means of communication of information on outbreak epidemiology and other aspects of emergin infectious diseases may include social media networks among healthcare professionals [85]. Access to online resources and internet-based participatory surveillance system such as HealthMap could be useful in detection and monitoring outbreaks [17], [18]. However, presentation of epidemiological information that has been collected and analysed by recognised, sound epidemiological methods and subjected to peer-review in appropriate journals remains a vital means for reliable communication within the medical/scientific community.
Current indications are that MERS-CoV has limited epidemic potential [85], [86]. However, human-to-human transmission occur usually in healthcare -associated outbreaks such as those included in the current review, and other outbreaks from other countries in the Middle East, and the Republic of Korea [11], [12], [13], [14], [22], [23], [24], [25], [26], [27]. The healthcare associated outbreaks were linked to poor compliance with infection prevention and control procedures [53], [64], [87], [88], [89], [90], [91]. Effectiveness of consistent promotion and application of basic and advanced infection control procedures in reduction of cases has been demonstrated in hospital-associated MERS-CoV outbreaks in Saudi Arabia and Korea [53], [85], [91]. However, MERS-CoV has a high morbidity and case-fatality rate, particularly among ICU and/or critically ill patients, those with comorbid illness, older patients and those with a high viral load [11], [12], [15], [92], [93], [94]. The potential for viral mutations, for example in the viral spike (S) protein, which mediates viral entry into host cells, or in viral proteases such as Mpro, could increase viral affinity for human host cells and expand host cell range [50], [94], [95], [96]. Thus, surveillance, contact tracing and research into possible animal hosts and transmission pathways to humans need to be prioritized [37]. This is vital to fill in gaps in knowledge and understanding of MERS-CoV. Such gaps include exposure to infected dromedary camels, direction of transmission between humans and camels, the role of a third link in the chain of cross-species transmission, such as bats, and the reasons behind limited human-to-human transmission [97]. There is no specific therapy for MERS-CoV, despite promising results in animal studies for few antiviral synthetic peptides and candidate vaccines. GLS-5300, a DNA-plasmid vaccine encoding MERS-CoV S protein (Inovio, GeneOne Life Science Inc. and the Walter Reed Army Institute of Research) is the first potential MERS-CoV vaccine to enter human testing [98], however it is intended for prophylactic use, rather than in outbreak situations. In terms of diagnosis, MERS-CoV was confirmed by PCR. This is expected, as real-time PCR is the major method for detection of MERS-CoV [99]. Antibody-based methods are not widely used as yet, although there is some interest in developing and implementing such methods in routine testing, especially to test for possible previous infection or if symptoms arose more than fourteen days previously as recommended by the Centers for Disease Control and Prevention (CDC) [99], [100].
In conclusion, most epidemiology articles on MERS-CoV had no preferential publication advantage over other articles. Collaboration of the research community and the scientific publishing industry is needed to facilitate timely publication of emerging infectious diseases.
Funding
No funding sources.
Competing interest
None declared.
Ethical approval
Not required.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jiph.2017.05.005.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D., Gittleman J.L. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morens D.M., Folkers G.K., Fauci A.S. The challenge of emerging and re-emerging infectious diseases. Nature. 2004;430:242–249. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connolly MA, A field manual—Communicable disease control in emergencies. Geneva: World Health Organization. Available from http://www.who.int/diseasecontrol_emergencies/publications/9241546166/en/; [accessed 03 April 2017].
- 4.WHO. MERS-CoV summary and literature update — as of 20 June 2013. http://www.who.int/csr/disease/coronavirus_infections/update_20130620/en/.
- 5.Xing W., Hejblum G., Leung G.M., Valleron A.-J. Anatomy of the epidemiological literature on the 2003 SARS outbreaks in Hong Kong and Toronto: a time-stratified review. PLoS Med. 2010;7:e1000272. doi: 10.1371/journal.pmed.1000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Tawfiq J.A., Memish Z.A. Drivers of MERS-CoV transmission: what do we know? Expert Rev Respir Med. 2016;10:331–338. doi: 10.1586/17476348.2016.1150784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Memish Z., Al-Tawfiq J., Memish Z. Middle East respiratory syndrome coronavirus: epidemiology and disease control measures. Infect Drug Resist. 2014;3:281–287. doi: 10.2147/IDR.S51283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D.M.E., Fouchier R.A.M. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 9.Hijawi B., Abdallat M., Sayaydeh A., Alqasrawi S., Haddadin A., Jaarour N. Novel coronavirus infections in Jordan, April 2012: epidemiological findings from a retrospective investigation/Infections par le nouveau coronavirus en Jordanie, avril 2012: résultats épidémiologiques d'une étude rétrospective. East Mediterr Health J. 2013;19:S12. [PubMed] [Google Scholar]
- 10.WHO. Middle East respiratory syndrome coronavirus (MERS-CoV) n.d. http://www.who.int/emergencies/mers-cov/en/.
- 11.Assiri A., McGeer A., Perl T.M., Price C.S., Rabeeah A.l., Cummings D.A.T. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oboho I.K., Tomczyk S.M., Al-Asmari A.M., Banjar A.A., Al-Mugti H., Aloraini M.S. 2014 MERS-CoV outbreak in Jeddah—a link to health care facilities. N Engl J Med. 2015;372:846–854. doi: 10.1056/NEJMoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drosten C., Muth D., Corman V.M., Hussain R., Al Masri M., HajOmar W. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, Kingdom of Saudi Arabia. Clin Infect Dis. 2014;2015(60):369–377. doi: 10.1093/cid/ciu812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fagbo S.F., Skakni L., Chu D.K.W., Garbati M.A., Joseph M., Peiris M. Molecular epidemiology of hospital outbreak of Middle East Respiratory Syndrome, Riyadh, Saudi Arabia. Emerg Infect Dis. 2014;2015(21):1981–1988. doi: 10.3201/eid2111.150944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Almekhlafi G.A., Albarrak M.M., Mandourah Y., Hassan S., Alwan A., Abudayah A. Presentation and outcome of Middle East respiratory syndrome in Saudi intensive care unit patients. Crit Care. 2016;20(123) doi: 10.1186/s13054-016-1303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balkhy H.H., Alenazi T.H., Alshamrani M.M., Baffoe-Bonnie H., Al-Abdely H.M., El-Saed A. Notes from the field: nosocomial outbreak of Middle East respiratory syndrome in a large tertiary care hospital-Riyadh, Saudi Arabia, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:163–164. doi: 10.15585/mmwr.mm6506a5. [DOI] [PubMed] [Google Scholar]
- 17.Thorner A.R., Cao B., Jiang T., Warner A.J., Bonis P.A. Correlation between UpToDate searches and reported cases of Middle East respiratory syndrome during outbreaks in Saudi Arabia. Open Forum Infect Dis. 2016:ofw043. doi: 10.1093/ofid/ofw043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hossain N., Househ M. Using HealthMap to analyse Middle East Respiratory Syndrome (MERS) data. Stud Health Technol Inform. 2016;226:213–216. [PubMed] [Google Scholar]
- 19.Ajlan A.M., Ahyad R.A., Jamjoom L.G., Alharthy A., Madani T.A. Middle East respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings. Am J Roentgenol. 2014;203:1–6. doi: 10.2214/AJR.14.13021. [DOI] [PubMed] [Google Scholar]
- 20.Al Ghamdi M., Alghamdi K.M., Ghandoora Y., Alzahrani A., Salah F., Alsulami A. Treatment outcomes for patients with Middle Eastern Respiratory Syndrome Coronavirus (MERS CoV) infection at a coronavirus referral center in the Kingdom of Saudi Arabia. BMC Infect Dis. 2016;16:174. doi: 10.1186/s12879-016-1492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alagaili A.N., Briese T., Mishra N., Kapoor V., Sameroff S.C., de Wit E. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. mBio. 2014;5 doi: 10.1128/mBio.00884-14. e00884-14-e00884-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alghamdi I.G., Hussain I.I., Almalki S.S., Alghamdi M.S., Alghamdi M.M., El-Sheemy M.A. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417–423. doi: 10.2147/IJGM.S67061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Hameed F., Wahla A.S., Siddiqui S., Ghabashi A., Al-Shomrani M., Al-Thaqafi A. Characteristics and outcomes of Middle East respiratory syndrome coronavirus patients admitted to an intensive care unit in Jeddah, Saudi Arabia. J Intensive Care Med. 2016;31:344–348. doi: 10.1177/0885066615579858. [DOI] [PubMed] [Google Scholar]
- 24.Al-Mohrej O.A., Al-Shirian S.D., Al-Otaibi S.K., Tamim H.M., Masuadi E.M., Fakhoury H.M. Is the Saudi public aware of Middle East respiratory syndrome? J Infect Public Health. 2016;9:259–266. doi: 10.1016/j.jiph.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almutairi K.M., Al Helih E.M., Moussa M., Boshaiqah A.E., Saleh Alajilan A., Vinluan J.M. Awareness, attitudes, and practices related to coreonavirus pandemic among public in Saudi Arabia. Fam Community Health. 2015;38:332–340. doi: 10.1097/FCH.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 26.Alraddadi B., Bawareth N., Omar H., Alsalmi H., Alshukairi A., Qushmaq I. Patient characteristics infected with Middle East respiratory syndrome coronavirus infection in a tertiary hospital. Ann Thorac Med. 2016;11:128–131. doi: 10.4103/1817-1737.180027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alraddadi B.M., Watson J.T., Almarashi A., Abedi G.R., Turkistani A., Sadran M. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22:49–55. doi: 10.3201/eid2201.151340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alsahafi A.J., Cheng A.C. The epidemiology of Middle East respiratory syndrome coronavirus in the Kingdom of Saudi Arabia, 2012–2015. Int J Infect Dis. 2016;45:1–4. doi: 10.1016/j.ijid.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alshukairi A.N., Khalid I., Ahmed W.A., Dada A.M., Bayumi D.T., Malic L.S. Antibody response and disease severity in healthcare worker MERS survivors. Emerg Infect Dis. 2016;2:2. doi: 10.3201/eid2206.160010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Tawfiq J.A., Hinedi K., Ghandour J., Khairalla H., Musleh S., Ujayli A. Middle East Respiratory Syndrome-Coronavirus (MERS-CoV): a case-controlstudy of hospitalized patients. Clin Infect Dis. 2014;59:160–165. doi: 10.1093/cid/ciu226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Tawfiq J.A., Momattin H., Dib J., Memish Z.A. Ribavirin and interferon therapy in patients infected with the Middle East respiratory syndrome coronavirus: an observational study. Int J Infect Dis. 2014;20:42–46. doi: 10.1016/j.ijid.2013.12.003. PubMed – NCBI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arabi Y.M., Arifi A.A., Balkhy H.H., Najm H., Aldawood A.S., Ghabashi A. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160:389–397. doi: 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- 33.Arabi Y.M., Harthi A., Hussein J., Bouchama A., Johani S., Hajeer A.H. Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV) Infection. 2015;43:495–501. doi: 10.1007/s15010-015-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Assiri A., Abedi G.R., Al Masri M., Bin Saeed A., Gerber S.I., Watson J.T. Middle East respiratory syndrome coronavirus infection during pregnancy: a report of 5 cases from Saudi Arabia. Clin Infect Dis. 2016;63:951–953. doi: 10.1093/cid/ciw412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Assiri A., Al-Tawfiq J.A., Al-Rabeeah A.A., Al-Rabiah F.A., Al-Hajjar S., Al-Barrak A. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Atabani S.F., Wilson S., Overton-Lewis C., Workman J., Kidd I.M., Petersen E. Active screening and surveillance in the United Kingdom for Middle East respiratory syndrome coronavirus in returning travellers and pilgrims from the Middle East: a prospective descriptive study for the period 2013–2015. Int J Infect Dis. 2016;47:10–14. doi: 10.1016/j.ijid.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Breban R., Riou J., Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382:694–699. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Briese T., Mishra N., Jain K., Zalmout I.S., Jabado O.J., Karesh W.B. Middle east respiratory syndrome coronavirus quasispecies that include homologues of human isolates revealed through whole- genome analysis and virus cultured from dromedary camels in Saudi Arabia. mBio. 2014;5 doi: 10.1128/mBio.01146-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butt T.S., Koutlakis-Barron I., AlJumaah S., AlThawadi S., AlMofada S. Infection control and prevention practices implemented to reduce transmission risk of Middle East respiratory syndrome-coronavirus in a tertiary care institution in Saudi Arabia. Am J Infect Control. 2016;44:605–611. doi: 10.1016/j.ajic.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cauchemez S., Fraser C., Van Kerkhove M.D., Donnelly C.A., Riley S., Rambaut A. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cauchemez S., Van Kerkhove M.D., Riley S., Donnelly C.A., Fraser C., Ferguson N.M. Transmission scenarios for middle east respiratory syndrome coronavirus (MERS-CoV) and how to tell them apart. Eurosurveillance. 2013:18. [PMC free article] [PubMed] [Google Scholar]
- 42.Chowell G., Abdirizak F., Lee S., Lee J., Jung E., Nishiura H. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chowell G., Blumberg S., Simonsen L., Miller M.A., Viboud C. Synthesizing data and models for the spread of MERS-CoV, 2013: key role of index cases and hospital transmission. Epidemics. 2014;9:40–51. doi: 10.1016/j.epidem.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corman V.M., Albarrak A.M., Omrani A.S., Albarrak M.M., Farah M.E., Almasri M. Viral shedding and antibody response in 37 patients with middle east respiratory syndrome coronavirus infection. Clin Infect Dis. 2015 doi: 10.1093/cid/civ951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corman V.M., Ithete N.L., Richards L.R., Schoeman M.C., Preiser W., Drosten C. Rooting the phylogenetic tree of MERS-coronavirus by characterization of a conspecific virus from an African bat. J Virol. 2014;88:11297–11303. doi: 10.1128/JVI.01498-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cotten M., Watson S.J., Kellam P., Al-Rabeeah A.A., Makhdoom H.Q., Assiri A. Transmission and evolution of the Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive genomic study. Lancet. 2013;382:1993–2002. doi: 10.1016/S0140-6736(13)61887-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cotten M., Watson S.J., Zumla A.I. Spread circulation, and evolution of the Middle East respiratory syndrome coronavirus. mBio. 2014;5 doi: 10.1128/mbio.01062-13. pii: e01062-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Das K.M., Lee E.Y., Enani M.A., AlJawder S.E., Singh R., Bashir S. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR Am J Roentgenol. 2015;204:736–742. doi: 10.2214/ajr.14.13671. [DOI] [PubMed] [Google Scholar]
- 49.Feikin D.R., Alraddadi B., Qutub M., Shabouni O., Curns A., Oboho I.K. Association of higher MERS-CoV virus load with severe disease and death, Saudi Arabia, 2014. Emerg Infect Dis. 2015;21:2029–2035. doi: 10.3201/eid2111.150764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Forni D., Filippi G., Cagliani R., De Gioia L., Pozzoli U., Al-Daghri N. The heptad repeat region is a major selection target in MERS-CoV and related coronaviruses. Sci Rep. 2015;5:14480. doi: 10.1038/srep14480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Furuse Y., Okamoto M., Oshitani H. Conservation of nucleotide sequences for molecular diagnosis of Middle East respiratory syndrome (MERS) coronavirus. Int J Infect Dis. 2015;40:25–27. doi: 10.1016/j.ijid.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gierer S., Hofmann-Winkler H., Albuali W.H., Bertram S., Al-Rubaish A.M., Yousef A.A. Lack of MERS coronavirus neutralizing antibodies in humans, eastern province, Saudi Arabia. Emerg Infect Dis. 2013;19:2034–2036. doi: 10.3201/eid1912.130701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hastings D.L., Tokars J.I., Abdel Aziz I.Z.A.M., Alkhaldi K.Z., Bensadek A.T., Alraddadi B.M. Outbreak of middle east respiratory syndrome at tertiary care hospital, Jeddah, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22:794–801. doi: 10.3201/eid2205.151797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hemida M.G., Perera R.A., Wang P., Alhammadi M.A., Siu L.Y., Li M. Middle East respiratory syndrome (MERS) coronavirus seroprevalence in domestic livestock in Saudi Arabia, 2010 to 2013. Eurosurveillance. 2013;18 doi: 10.2807/1560-7917.ES2013.18.50.20659. [DOI] [PubMed] [Google Scholar]
- 55.Khalafalla A.I., Lu X., Al-Mubarak A.I., Dalab A.H., Al-Busadah K.A., Erdman D.D. MERS-CoV in upper respiratory tract and lungs of dromedary camels, Saudi Arabia, 2013–2014. Emerg Infect Dis. 2015;21:1153–1158. doi: 10.3201/eid2107.150070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khalid I., Alraddadi B.M., Dairi Y., Khalid T.J., Kadri M., Alshukairi A.N. Acute management and long-term survival among subjects with severe Middle East respiratory syndrome coronavirus pneumonia and ARDS. Respir Care. 2016;61:340–348. doi: 10.4187/respcare.04325. [DOI] [PubMed] [Google Scholar]
- 57.Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Das K.M., Lee E.Y., Al Jawder S.E., Enani M.A., Singh R., Skakni L. Acute Middle East respiratory syndrome coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. Am J Roentgenol. 2015;205:W267–S274. doi: 10.2214/AJR.15.14445. [DOI] [PubMed] [Google Scholar]
- 59.Khalid M., Khan B., Al Rabiah F., Alismaili R., Saleemi S., Rehan-Khaliq A.M. Middle Eastern Respiratory Syndrome Corona Virus (MERS CoV): case reports from a tertiary care hospital in Saudi Arabia. Ann Saudi Med. 2014;34:396–400. doi: 10.5144/0256-4947.2014.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kharma M.Y., Alalwani M.S., Amer M.F., Tarakji B., Aws G. Assessment of the awareness level of dental students toward Middle East respiratory syndrome-coronavirus. J Int Soc Prev Commu Dent. 2015;5:163–169. doi: 10.4103/2231-0762.159951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lessler J., Rodriguez-Barraquer I., Cummings D.A., Garske T., Van Kerkhove M., Mills H. Estimating potential incidence of MERS-CoV associated with Hajj Pilgrims to Saudi Arabia. PLoS Curr. 2014:1–18. doi: 10.1371/currents.outbreaks.c5c9c9abd636164a9b6fd4dbda974369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lessler J., Salje H., Van Kerkhove M.D., Ferguson N.M., Cauchemez S., Rodriquez-Barraquer I. Estimating the severity and subclinical burden of Middle East respiratory syndrome coronavirus infection in the Kingdom of Saudi Arabia. Am J Epidemiol. 2016;183:657–663. doi: 10.1093/aje/kwv452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Luke T., Wu H., Zhao J., Channappanavar R., Coleman C.M., Jiao J.-A. Human polyclonal immunoglobulin G from transchromosomic bovines inhibits MERS-CoV in vivo. Sci Transl Med. 2016;8:326ra21. doi: 10.1126/scitranslmed.aaf1061. [DOI] [PubMed] [Google Scholar]
- 64.Madani T.A., Althaqafi A.O., Alraddadi B.M. Infection prevention and control guidelines for patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection. Saudi Med J. 2014;35:897–913. doi: 10.4049/jimmunol.1303196. [DOI] [PubMed] [Google Scholar]
- 65.Majumder M.S., Rivers C., Lofgren E., Fisman D. Estimation of MERS-coronavirus reproductive number and case fatality rate for the spring Saudi Arabia outbreak: insights from publicly available data. PLOS Curr Outbreaks. 2014:1–18. doi: 10.1371/currents.outbreaks.98d2f8f3382d84f390736cd5f5fe133c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Memish Z.A., Al-Tawfiq J.A., Assiri A., AlRabiah F.A., Al Hajjar S., Albarrak A. Middle East respiratory syndrome coronavirus disease in children. Pediatr Infect Dis J. 2014;33:904–906. doi: 10.1097/INF.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 67.Memish Z.A., Al-Tawfiq J.A., Makhdoom H.Q., Al-Rabeeah A.A., Assiri A., Alhakeem R.F. Screening for Middle East respiratory syndrome coronavirus infection in hospital patients and their healthcare worker and family contacts: a prospective descriptive study. Clin Microbiol Infect. 2014;20:469–474. doi: 10.1111/1469-0691.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Memish Z.A., Assiri A.M., Al-Tawfiq J.A. Middle East respiratory syndrome coronavirus (MERS-CoV) viral shedding in the respiratory tract: an observational analysis with infection control implications. Int J Infect Dis. 2014;29:307–308. doi: 10.1016/j.ijid.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Müller M.A., Meyer B., Corman V.M., Al-Masri M., Turkestani A., Ritz D. Presence of Middle East respiratory syndrome coronavirus antibodies in Saudi Arabia: a nationwide, cross-sectional, serological study. Lancet Infect Dis. 2015;15:559–564. doi: 10.1016/S1473-3099(15)70090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Muth D., Corman V.M., Meyer B., Assiri A., Al-Masri M., Farah M. Infectious Middle East respiratory syndrome coronavirus excretion and serotype variability based on live virus isolates from patients in Saudi Arabia. J Clin Microbiol. 2015;53:2951–2955. doi: 10.1128/JCM.01368-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Noorwali A.A., Turkistani A.M., Asiri S.I., Trabulsi F.A., Alwafi O.M., Alzahrani S.H. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah Region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203–209. doi: 10.5144/0256-4947.2015.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Omrani A.S., Saad M.M., Baig K., Bahloul A., Abdul-Matin M., Alaidaroos A.Y. Ribavirin and interferon alfa-2a for severe Middle East respiratory syndrome coronavirus infection: a retrospective cohort study. Lancet Infect Dis. 2014;14:1090–1095. doi: 10.1016/S1473-3099(14)70920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Poletto C., Colizza V., Boëlle P.-Y. Quantifying spatiotemporal heterogeneity of MERS-CoV transmission in the Middle East region: a combined modelling approach. Epidemics. 2016;15:1–9. doi: 10.1016/j.epidem.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Poletto C., Pelat C., Lévy-Bruhl D., Yazdanpanah Y., Boëlle P.Y., Colizza V. Assessment of the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic in the Middle East and risk of international spread using a novel maximum likelihood analysis approach. Eurosurveillance. 2014;1:9. doi: 10.2807/1560-7917.ES2014.19.23.20824. [DOI] [PubMed] [Google Scholar]
- 75.Saad M., Omrani A.S., Baig K., Bahloul A., Elzein F., Matin M.A. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sabir J.S.M., Lam T.T., Mohamed M.M., Li L., Shen Y., Abo-aba S.E.M. Co-circulation of three camel coronavirus species and recombination of MERS-CoVs in Saudi Arabia. Science. 2015;351:1–6. doi: 10.1126/science.aac8606. [DOI] [PubMed] [Google Scholar]
- 77.Shalhoub S., Farahat F., Al-Jiffri A., Simhairi R., Shamma O., Siddiqi N. IFN-α2a or IFN-β1a in combination with ribavirin to treat Middle East respiratory syndrome coronavirus pneumonia: a retrospective study. J Antimicrob Chemother. 2015;70:2129–2132. doi: 10.1093/jac/dkv085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stirling B.V., Harmston J., Alsobayel H. An educational programme for nursing college staff and students during a MERS- coronavirus outbreak in Saudi Arabia. BMC Nurs. 2015;14:20. doi: 10.1186/s12912-015-0065-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Williams H.A., Dunville R.L., Gerber S.I., Erdman D.D., Pesik N., Kuhar D. CDC’s early response to a novel viral disease, Middle East Respiratory Syndrome Coronavirus (MERS-CoV), September 2012-May 2014. Public Health Rep. 2015;130(4):307. doi: 10.1177/003335491513000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hashkes P., Uziel Y., 4th Park City PR The publication rate of abstracts from the 4th Park City Pediatric Rheumatology meeting in peer-reviewed journals: what factors influenced publication? J Rheumatol. 2003;30(3):597–602. [PubMed] [Google Scholar]
- 81.Stern J.M., Simes R.J. Publication bias: evidence of delayed publication in a cohort study of clinical research projects. BMJ. 1997;315(7109):640–645. doi: 10.1136/bmj.315.7109.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Owada K., Eckmanns T., Kamara K.-B.O., Olu O.O. Epidemiological data management during an outbreak of Ebola virus disease: key issues and observations from sierra leone. Front Public Health. 2016;4:163. doi: 10.3389/fpubh.2016.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2014. Data quality monitoring and surveillance system evaluation — a handbook of methods and applications. [Google Scholar]
- 84.Hayden F.G., Farrar J., Peiris J.S.M. Towards improving clinical management of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2014;14(7):544–546. doi: 10.1016/S1473-3099(14)70793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Omrani A.S.S., Shalhoub S. Middle East respiratory syndrome coronavirus (MERS-CoV): what lessons can we learn? J Hosp Infect. 2015;91:188–196. doi: 10.1016/j.jhin.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Memish Z.A., Zumla A., Al-Tawfiq J.A. How great is the risk of Middle East respiratory syndrome coronavirus to the global population? Expert Rev Anti Infect Ther. 2013;11:979–981. doi: 10.1586/14787210.2013.836965. [DOI] [PubMed] [Google Scholar]
- 87.Balkhy H.H., Perl T.M., Arabi Y.M. Preventing healthcare-associated transmission of the Middle East Respiratory Syndrome (MERS): our Achilles heel. J Infect Public Health. 2016;9:208–212. doi: 10.1016/j.jiph.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hunter J.C., Nguyen D., Aden B., Al Bandar Z., Al Dhaheri W., Abu Elkheir K. Transmission of Middle East respiratory syndrome coronavirus infections in healthcare settings, Abu Dhabi. Emerg Infect Dis. 2016;22:647–656. doi: 10.3201/eid2204.151615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kim Y., Lee S., Chu C., Choe S., Hong S., Shin Y. The characteristics of middle eastern respiratory syndrome coronavirus transmission dynamics in South Korea. Osong Public Heal Res Perspect. 2016;7:49–55. doi: 10.1016/j.phrp.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Al-Tawfiq J.A., Perl T.M. Middle East respiratory syndrome coronavirus in healthcare settings. Curr Opin Infect Dis. 2015;28:392–396. doi: 10.1097/QCO.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 91.Kim J.Y., Song J.Y., Yoon Y.K., Choi S.-H., Song Y.G., Kim S.-R. Middle East respiratory syndrome infection control and prevention guideline for healthcare facilities. Infect Chemother. 2015;47:278–302. doi: 10.3947/ic.2015.47.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Al-Dorzi H.M., Alsolamy S., Arabi Y.M. Critically ill patients with Middle East respiratory syndrome coronavirus infection. Crit Care. 2016;20:65. doi: 10.1186/s13054-016-1234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Memish Z., Zumla A.I., Al-Hakeem R.F., Al-Rabeeah A.A., Stephens G.M. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;368:2487–2494. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 94.Durai P., Batool M., Shah M., Choi S. Middle East respiratory syndrome coronavirus: transmission, virology and therapeutic targeting to aid in outbreak control. Exp Mol Med. 2015;47:e181. doi: 10.1038/emm.2015.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ho B.-L., Cheng S.-C., Shi L., Wang T.-Y., Ho K.-I., Chou C.-Y. Critical assessment of the important residues involved in the dimerization and catalysis of MERS coronavirus main protease. PLoS One. 2015;10:e0144865. doi: 10.1371/journal.pone.0144865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yang Y., Liu C., Du L., Jiang S., Shi Z., Baric R.S. Two mutations were critical for bat-to-human transmission of middle east respiratory syndrome coronavirus. J Virol. 2015;89:9119–9123. doi: 10.1128/JVI.01279-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Banik G.R.R., Khandaker G., Rashid H. Middle East Respiratory Syndrome Coronavirus MERS-CoV: current knowledge gaps. Paediatr Respir Rev. 2015;16:197–202. doi: 10.1016/j.prrv.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Inovio. MERS GLS-5300 SynCon® immunotherapy targeting Middle East Respiratory Syndrome 2016. http://www.inovio.com/products/infectious-disease-vaccines/mers/; [accessed 31 December 2016].
- 99.Al Johani S., Hajeer A.H. MERS-CoV diagnosis: an update. J Infect Pub Health. 2016;9(3):216–219. doi: 10.1016/j.jiph.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Centers for Disease Control and Prevention. Interim Guidance for Healthcare Professionals. https://www.cdc.gov/coronavirus/mers/interim-guidance.html; 2016, [accessed 04 April 2017].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.