Summary
The emergence of non-communicable diseases (NCDs) follows multiple aetiological pathways requiring recognition for effective control and prevention. Infections are proving to be conventional, emerging and re-emerging aetiological factors for many NCDs. This review explores the possible mechanisms by which infections induce NCDs citing examples of studies in Africa and elsewhere where NCDs and infections are proposed or confirmed to be causally linked and also discusses the implications and challenges of these observations for science and medicine. The need to re-evaluate and expand early community and individual preventive and control strategies that will lead to reduction and even elimination of NCDs especially in Africa and other developing countries where infections are prevalent is highlighted.
Keywords: Infections, Non-communicable diseases, Chronic disease, Cancer, Developing countries
Introduction
Non-communicable diseases (NCDs) are the commonest cause of death and disability worldwide, accounting for almost 60% of all deaths with incidence rates assuming epidemic proportions in many countries of the world [1]. Eighty percent of deaths from NCDs occur in low and middle income countries of the developing world [1] and if nothing is done to halt this trend it is projected that by 2015 deaths from NCDs may increase by 15–27% in these countries [2]. The aetiology of most NCDs has been linked to multiple risk factors including host genetics and immune response, lifestyle and environmental risk factors [3]. Risk factors are defined as any attribute, characteristic or exposure of an individual, which increase the likelihood of developing a disease or injury [4]. Physical inactivity, alcohol excess, tobacco ingestion, excessive salt ingestion, gender, age, obesity, high cholesterol and unhealthy diet and many other factors are established conventional risk factors for development of many NCDs (Table 1 ) and they remain targets for NCD preventive and control strategies [3], [4]. Over the last two decades however, there has been an emergence of novel aetiological factors (e.g. Helicobacter Pylori and peptic ulcer disease (PUD) [5]), novel risk factors (e.g. low birth weight and Type II Diabetes mellitus [6]) and novel markers (e.g. raised Homocysteine and cardiovascular diseases [7]) for many NCDs. NCDs causation can now be conceptualized as a continuum from womb to disability or death. A successful and durable NCDs preventive and control strategy therefore requires a holistic approach where all possible primary and secondary risk factors are targeted.
Table 1.
Conventional risk factors implicated in the emergence of some common NCDs.
| Hypertension | Diabetes mellitus | Stroke | Cancer | Coronary artery disease | Mental illness | Heart disease | Asthma/COPD | Sickle cell disease | Blindness | Oral health | Osteoporosis | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical inactivity | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | ✓ |
| Alcohol excess | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | ✓ | ✓ | ✓ |
| Drug abuse/use | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ |
| Tobacco use/smoking | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ |
| Salt excess | ✓ | × | ✓ | × | ✓ | × | ✓ | × | × | × | × | × |
| Unhealthy diets | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ |
| Obesity | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | ✓ |
| Abnormal lipids | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | × | × |
| Psychological stress | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ |
| Low socio-economic status | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ |
| Unsafe sex | × | × | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | × | ✓ | × |
| Age | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | ✓ | ✓ |
| Family history/heredity | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Gender | ✓ | × | × | ✓ | ✓ | ✓ | ✓ | × | × | × | × | ✓ |
✓ = increase risk of disease, × = do not increase risk of disease, COPD = chronic obstructive pulmonary disease.
Infectious diseases are the commonest cause of death in Africa and rank third to cardiovascular diseases and cancers respectively, as a cause of death worldwide [8]. As a result of improved laboratory diagnostic techniques and advances in science, technology, medicine and public health, many NCDs including cardiovascular diseases, cancers and endocrine diseases have now been associated with an infectious risk factor. Infections therefore represent novel and emerging risks factors for NCDs with the potential for preventative interventions.
An infectious (communicable) disease is defined as an illness caused by a specific infectious agent or its toxic products that results from transmission of that agent or its products from an infected person, animal or reservoir to a susceptible host [9]. This agent can be transmitted either directly or indirectly through an intermediate plant or animal host, vector or inanimate environment [9]. NCDs on the other hand are defined as a disease or condition that has no known causative agents that are transmitted from one affected individual to another [10]. However, with the increasing number of NCDs being associated with an infectious risk factor, the distinction between an infectious disease and NCDs is blurring and it is important to bring to the fore their linkages and interactions.
This review explores the role of infections in the emergence of NCDs including possible pathogenetic mechanisms citing examples of infections where research in Africa and elsewhere has suggested or confirmed a causal link to NCDs. The implications and challenges of the knowledge obtained in preventing and interrupting full blown emergence of the relevant NCDs in the developing world become obvious.
Determinants of NCD outcome following infection
The disease outcome following an infection is determined by a dynamic interaction between the infectious agent, the host and the environment. We consider each of these factors in turn.
Host
Susceptibility to infection, disease development, disease progression and disease severity are all determined by interplay of several host factors including age, sex, genetics, immune response and nutritional status. Acute rheumatic fever following β hemolytic streptococcus infection [11] is, for instance, a disease of childhood, whereas Alzheimer's disease that has been causally linked to Chlamydia infection is a disease of the elderly [12]. Gender and sex hormones also determine disease manifestations since androgens have been shown to promote liver carcinogenesis [13] and this may to a degree explain why Hepatitis B virus (HBV)-related liver cancer has been reported to be five times commoner in males than in females [14]. The effect of estrogens in stimulating antibody (including autoantibody) production and the effect of testosterone in depressing antibody production also partly explains the higher incidence of autoimmune diseases in females than males [15].
HLA type and immune genetic defects also determine disease outcome following an infection [16]. Despite the known role of infections as a trigger for autoimmune diseases there are discordant infections and autoimmune incidence rates between countries and continents. These differences have been attributable to differences in HLA [16]. HLA B27 is common amongst Caucasians and hence cases of Reiter's arthritis are reported more frequently amongst Caucasians in the western world than amongst Africans [17].
HLA type may however protect against disease development following infection. HLA DR 1302 has been shown from studies in Gambia and Germany to protect against progression of HBV-related chronic diseases by improving clearance of HBV [16]. Genetic polymorphism and mutations of interleukin 10 (IL-10), transforming growth factor (TGF β), tumor necrosis factor (TNF) and other cytokine genes involved in immune protection and immune regulation are all known to promote development of many infection-related NCDs including asthma and allergy [17].
Infectious agent
The type of infection, the infecting dose, the strain involved and the virulence of the infecting agent are all important determinants of the disease outcome. The ability of Helicobacter pylori to induce peptic ulcer disease is determined by the virulence of the infecting strain [5]. Consequently, virulent strains produce products such as the cytotoxin associated gene-pathogenicity island (cag-PAI) products, vacoulating cytotoxin (VacA) and urease which act together with a dysregulated host immune response to promote gastric inflammation and cause PUD [5]. Similarly, of the about 30 genotypes of human papilloma virus (HPV) that cause genital infection strains with genotypes 16 and 18 are known to induce cervical cancer attributable to their potent oncogenic properties [18]. Other strain-specific disease outcomes can be seen in group A β hemolytic streptococcus-related acute glomerulonephritis where M strains types 1, 2, 4, 12, 18, 25, 49, 55, 57 and 60 are more likely to cause acute glomerulonephritis [19] and malaria where Plasmodium malariae is more likely than other species to cause immune complex mediated malaria nephropathy [20], [21]. The mechanisms that underlie how specific strains of an infection cause NCD is related to their ability to release cytotoxic products and also to cause an exaggerated and dysregulated immune response that leads to tissue damage.
Environment
In addition to environmental risk factors, infections may increase the cumulative risk of developing a NCD by serving as triggers, co-factors or themselves aetiological drivers for NCD development. Infections as co-factors with environmental factors in NCD emergence is exemplified in chronic obstructive pulmonary disease (COPD) where the lung damaging effects of smoking are potentiated by concomitant respiratory tract viral infection [22].
The environment may also influence the immune development and host immune response and may consequently protect or predispose an individual to developing a NCD. This analogy is typified in the hygiene hypothesis proposed by Strachan in 1989 [23] which states that an excessively hygienic environment in early childhood may predispose some towards asthma, allergy, atopy and autoimmune diseases. Early microbial exposure is essential for normal immune development [24]. Under excessively hygienic circumstances, early childhood infections are rare and the TH (T helper) 2 cytokines arm of the T helper lymphocytes is preferentially stimulated without modulation from the TH1 cytokine arm. Hence, excessive activation of TH2 cytokine arm predisposes hygienic children to asthma and allergy. In Africa, the low incidence of autoimmune and allergic diseases have been attributed to chronic malarial parasitaemia and recurrent helminthes infestation both of which induce immunosuppressive and anti-inflammatory responses that prevent allergy and autoimmune diseases [17], [24]. In a pioneering experiment by Greenwood and Voller, infection of New Zealand Black (NZB) and Fi hybrid mice with rodent malaria parasite Plasmodium berghei yoeli suppressed the spontaneous autoimmune disease of mice of these two strains [25]. Uncritical acceptance of this hypothesis hygiene may however understate the importance of hygiene in prevention of infectious diseases. While discouraging excessive hygienic practices that eliminate the beneficial effects of surrounding microbial flora in a healthy primary immune response, effective hygienic practices that prevent clinical infection and promote healthy living should always be emphasized and promoted.
Mechanisms of infectious aetiology of NCD
Inflammation
The ability of an infectious agent and host to induce and sustain chronic inflammation is the focal mechanism involved in the infectious aetiology of most NCD and most NCD are characterized pathologically by evidence of chronic inflammation. Chronic inflammation is a feature of NCDs including atherosclerosis [26], peptic ulcer disease [5], and asthma [27]—all possibly having an infectious trigger. The role of microorganism in initiating this injury and the subsequent development of a NCD is determined largely by dynamic interactions between the host, environment and the infectious agent [28], [29], [30], [31].
The persistence of infectious agents within the cells and tissues of the host is the key driving force for chronic inflammation leading to NCDs. For this reason, most infection-related NCD are more likely to follow chronic persistent viral infections and other intracellular bacteria, parasitic, fungal and Prions infections than acute extracellular infections (e.g. Staphylococcus spp.). Some acute infections may however result in NCD via the “hit and run” hypothesis [32]. This hypothesis suggest that an infection ‘HITS’ by triggering an NCD and ‘RUNS’ (becomes no longer present) when the disease develops. Typical examples of NCD where the “hit and run” hypothesis is thought to play a role include Reiter's arthritis and other reactive arthritides that follow a past gastrointestinal infection (e.g. Campylobacter, Shigella) and genital infections (e.g. Chlamydia urethritis) [28], and also multiple sclerosis that has been postulated to be triggered by childhood corona virus infections in predisposed individuals [32], [33].
Acute infections may also cause NCDs by initiating a vicious chronic inflammatory cycle [34]. In the development of COPD for instance, although the evidence for a primary infectious aetiology is inconclusive, recurrent bacteria infections such as Streptococcus pneumonia is thought to initiate the disease by causing lung damage [34]. Lung damage in turn predisposes to further bacteria infection setting up a vicious cycle that eventually lead to chronic lung damage characteristic of COPD [34].
Infectious agents may also cause an NCD by acting as Superantigens [35]. Superantigens are components or products of infectious agents that unspecifically activate T cells and result in an exaggerated immune response characterized by massive release of cytokines and chemokines [35]. NCD where infectious superantigens have been implicated include Kawasaki disease, eczema and rheumatoid arthritis [35].
Hypersensitivity and autoimmunity
The immune response to an infection may be exaggerated (hypersensitivity) and occasionally immune cells may directly attack host tissue (autoimmunity). These operative immune mechanisms have been classified from type I to type V [36], [37]. Hypersensitivity and autoimmunity-induced inflammation are important mechanisms by which infections induce NCD. In the development of specific NCD, a combination of two or more types of hypersensitivity reactions may be involved [36], [38].
Autoimmunity and autoimmune diseases may be triggered by infectious agents in genetically predisposed individuals [20], [38], [39]. The mechanisms involved include molecular mimicry, exposure of hidden/sequestered antigens, neoantigen formation and immune dysregulation [38], [39]. Molecular mimicry (a process in which infectious agents share a similar antigenic characteristics with components of host tissue) is perhaps the most important mechanism by which most infections trigger autoimmune diseases. In the pathogenesis of acute rheumatic fever, heart and joint symptoms develop 1–2 weeks after group A β hemolytic streptococcus because the M proteins of β hemolytic streptococcus share similar antigenic characteristics with myosin, laminin, and other matrix proteins found in the heart and joints and hence auto-antibodies are directed against these and other tissues in predisposed individuals [31]. Molecular mimicry is also known to play a role in the pathogenesis of several other autoimmune diseases such as type 1 DM, rheumatoid arthritis and Graves's disease [39].
Infections may alter immunological tolerance to self- and foreign antigens or may cause exposure of novel cryptic or sequestered antigens located within cells and tissues. This novel host-infectious antigen is recognized as foreign and subjected to immune destruction resulting in an autoimmune disease. In the pathogenesis of rheumatoid arthritis, infections such as Mycoplasma and Parvovirus may expose novel antigens within the joints, the glomerulus and other sites and may also alter self-antigens when infectious antigens become planted on host tissues [38], [39], [40]. Pancreatic B cell cryptic antigen exposure by viruses (Coxsackie B) has also been suggested as additional mechanism for an infectious aetiopathogenesis of type 1 DM [38].
Cellular transformation
Twenty percent of cancers worldwide are caused by infectious agents and infections rank second only to smoking as the commonest cause of cancers worldwide [41]. Carcinogenesis is a multi-step process and infections may serve as triggers in one or more these steps [42]. In the two hit hypothesis of carcinogenesis, at least two genetic mutations are required for cancers to develop. An inherited germ-line mutation of the tumor suppressor gene can only result in cancer if there is a mutation of the second allele of the tumor suppressor gene [42]. Infections amongst other factors have been implicated in inducing these and other genetic alterations that result in cancers. The mechanism of infectious carcinogenesis may include the following:
-
1.
Oncogene activation. Oncogenes are genes that promote cellular growth. Infectious may activate normal cellular oncogenes or may themselves express oncogenes that accelerate cell growth and result in malignancy. In the development of HBV-related primary liver cell carcinoma (PLCC), the X-protein of the virus has been postulated to directly transactivate viral genes and cellular oncogenes that promote HBV replication and also encourage tumorigenesis [43], [44]. In HPV-related cervical cancers the E5 gene of the virus is an oncogene that activates growth factors promoting carcinogenesis [18], [45]. In the aetiopathogenesis of adult T cell leukaemia, Human T lymphotrophic virus 1 (HTLV-1) Tax protein is an oncogene protein which activates the transcriptional factor nuclear factor β (NF-β) that promotes T cell transformation to cancers [46]. In the same vein, Epstein Barr virus (EBV) is known to induce chromosomal translocations (involving chromosomes 8; 14, or 2; 8, or 8; 22) that cause deregulation of the c-myc cellular oncogene expression and subsequent development of Burkitt's lymphoma [47]. Furthermore, the latent membrane protein 1(LMP1) and Epstein Barr nuclear antigen 2 (EBNA2) are oncogene products of EBV implicated in the tumorigenesis of Hodgkin's lymphoma and other EBV-related non-Hodgkin's lymphomas [47]. These and several other EBV oncogene products have also been linked to the aetiopathogenesis of a number of cancers including nasopharyngeal cancers [47].
-
2.
Loss of tumor suppressor ability. The p53 gene and the Retinoblastoma (pRb) gene code for anti-proliferative signals that suppress cancer development by inhibiting cell division, inducing programmed cell death (also known as apoptosis) and providing the opportunity for DNA repair during a cell cycle [42]. These tumor suppressor genes may become inactivated following an infection. The E6 and E7 gene products of HPV for instance, directly promote abnormal cellular growth that result in cervical cancers by degrading the p53 protein and inactivating the pRb protein, respectively [10], [45]. Aflatoxins produced from the fungus Aspergillus flavus have also been shown to cause a mutation in codon 249 of the p53 gene and is thought to act synergistically with HBV infection in promoting development of PLCC [48], [49]. In Zaria, northern Nigeria, aflatoxin B1, B2, G1, G2 have been found in liver cancer tissue as well as sera of patients with PLCC [50], [51].
-
3.
Chronic inflammation. Chronic inflammation with repeated cycles of cell death and regeneration, release of oxygen free radicals and reactive nitrogen radicals lead to DNA damage and mutations. With every subsequent mutation the risk of carcinogenesis is increased. Chronic inflammation contributes to carcinogenesis in HCV/HBV-related PLCC [39], [40] and Schistosoma haematobium-related bladder cancers [52] since infection with these agents is characterized by repeated cycles of cell necrosis and regeneration.
Viruses can also promote abnormal cellular proliferation by encoding inflammatory and cell growth factors. Human herpes virus 8 (HHV8) encodes a viral interleukin 6 (v-IL-6) and viral G-protein coupled receptor (v-GPCR) both possess pro-inflammatory, pro-growth factors and pro-angiogenic properties [53].
-
4.
Epithelial metaplasia. Infections like other carcinogens can directly cause cancers by provoking metaplasia of epithelial surfaces. This is exemplified in Helicobacter pylori-related gastric cancers where chronic atrophic gastritis results in intestinal metaplasia of the gastric mucosa with a consequent cellular dysplasia and cancer development [5]. Chronic Schistosoma haematobium infection also promotes development of squamous carcinoma of the bladder by inducing squamous metaplasia of the transitional epithelium of the bladder [52].
-
5.
Release of carcinogens. Infections may also cause release of carcinogens thereby promoting carcinogenesis. In chronic schistosomiasis and liver fluke (e.g. Chlonorchis sinesis) infestation, chronic inflammation may result in release of endogenous nitrosamines and exposure to high concentrations of this carcinogen may lead to neoplastic transformation [52]. Adult schistosome and miracidia may also directly liberate carcinogenic amines in the urine and by causing urinary stasis also concentrate urinary endogenous carcinogens. Absorption of these carcinogens may damage the bladder epithelium and promote carcinogenesis [52].
-
6.
Immunosuppression with loss of immunosurveillance. Infections such as HIV that cause predominant cellular immunosuppression are characteristically associated with increased risk of cancers. HIV infection results in both numerical and functional defects in both CD4 and CD8 T cells, cause dysfunctional natural killer (NK) cell, interferon gamma (INF-γ) and IL-2 activities and generally provoke an unfavourable TH2 biased cytokine dysregulation [54]. The TH1 cytokines (INF-γ, IL-2), natural killer cells (NK cells) and both CD4 and CD8 T lymphocytes are important elements involved in tumor immunity and tumor surveillance [55]. These defects therefore predispose HIV patients to cancers including Non-Hodgkin's lymphoma, cervical cancers, Kaposi's sarcoma and other cancers [56]. Malaria induced immunosuppression and polyclonal B cell activation is also thought to encourage EBV transactivation and transformation of B cells characteristic of Burkiitt's lymphoma [57]. The roles of HIV or chronic malaria in triggering lymphomas when associated with EBV infection have also been linked to their ability to stimulate a TH2 B cell growth promoting cytokine profile and suppression of the TH1 tumor protective cytokines [58].
Role of infections in emergence of specific non-communicable diseases
Infections have been implicated in the emergence of several non-communicable diseases but establishing a causal link has been challenging in most studies. Table 2 gives examples of infections with a known or probably aetiological role in the eventual emergence of NCDs. The following discussion highlights some NCDs where infections are primary aetiological factors or associated risk factors.
Table 2.
List of non-communicable diseases (NCDs) and their known or probable infectious risk factors.
| Disease | Infection |
|---|---|
| Cardiovascular | |
| Atherosclerosis and ischemic heart disease | Chlamydiab, CMVb, Herpes Virusb, Dental infectionsb |
| Hypertension | Chlamydiab |
| Peripartum cardiac failure | Coxsackie B virusb, Toxoplasmosisb, Chlamydiab |
| Endomyocardial fibrosis | Loa loab, Toxoplasmosisb, Trichinellab, Ascarisb, Hookwormb, Schistosomab |
| Rheumatic fever/rheumatic heart disease | Group A β hemolytic Streptococcus |
| Dilated cardiomyopathy | Virusesa, Toxoplasmosisa, Chaga'sa, HIVa, Lyme diseasea, etc. |
| Neurology/pyschiatry | |
| Stroke | Chlamydiab |
| Tropical spastic paraparesis | Human T lymphotrophic virus type 1a (HTLV1) |
| Dementia | HIVa |
| Alzheimer's disease | Herpes virusb, Chlamydiab |
| Multiple sclerosis | EBVb, Corona virus |
| Creutzfeldt-Jakob, Kuru, Familial insomnia | Prionsa |
| Subacute sclerosing panencephalitis (SSPE) | Measles virusa |
| Gullian Barre Syndrome | Campylobacter Jejunia |
| Schizophrenia | Intrauterine influenzab |
| Motor neuron disease (MND) | Virusesb |
| Chronic fatigue | HTLV1b, EBVb |
| Tics, Obsessive compulsive disorder | Group A Streptococcus Agalactiaeb |
| Autoimmune/endocrine | |
| Type 1 DM | Enterovirusesb—Coxsackie, Mumps, etc. |
| Graves Disease | Yersinia enterolyticab |
| Sjogren's disease | Helicobacter pylorib |
| Rheumatoid arthritis/SLE | Epstein Barr Virus, Parvovirus, Mycobacterium species, Human endogenous retroviruse |
| Polyarteritis nodosa | Hepatitis B Virusa |
| Mixed cryoglobulinaemia | Hepatitis C Virusa |
| Obesity | Adenovirus 36b |
| Reiter's arthritis | Chlamydiaa, Salmonellaa, Shigellaa, Campylobacter Jejunia, Yersiniaa |
| Gastrointestinal diseases | |
| Peptic ulcer, Gastritis | Helicobacter pyloria |
| Chronic hepatitis, Liver cirrhosis | Hepatitis B Virusa, Hepatitis C Virusa |
| Primary biliary cirrhosis | Helicobacter pylorib |
| Crohn's disease | Mycobacterium paratuberculosisb |
| Whipple's disease | Tropheryma whippleia |
| Malnutrition | Several infectionsa |
| Renal | |
| Nephrotic syndrome/chronic glomerulonephritis | Malariaa, Hepatitis B Virusa, Hepatitis C Virusa, Salmonellaa, Schistosomiasisa, Syphilisa, Leprosya, Tuberculosisa, etc. |
| Acute glomerulonephritis | Post β hemolytic streptococcusa |
| Respiratory | |
| Asthma | Chlamydiac, Mycoplasmab, Aspergillusa, Dermatophagiodesa, Parasitesb |
| Chronis obstructive pulmonary Disease | Chlamydiab, Mycoplasmab, Haemophilusb, Streptoccocusb |
| Sarcoidosis | Mycobacterium speciesb |
| Cancers | |
| Primary liver cell carcinoma | Hepatitis B Virusa, Hepatitis C Virusa, Aflatoxin B1 from Aspergillus flavusa |
| Burkitt's lymphoma | Malaria and Epstein Barr Virusa |
| Malt lymphoma, gastric lymphoma | Helicobacter pyloria |
| Bladder cancer | Schistosoma haematobiuma |
| Cervical cancer, anal, laryngeal, penile, vulva cancers | Human Papilloma Virusa |
| Adult T cell leukemia | Human T lymphotrophic virus 1a |
| Kaposi's sarcoma | Human herpes virus 8a |
| Hodgkin's lymphoma, nasopharyngeal cancer, B cell lymphoma in HIV | Epstein barr virusa |
| Bile duct cancer | Opisthorchis viverrrinia, Chlonorchis sinensisa |
| Others | |
| Blindness | Trachomaa, Onchocerciasisa, Measlesa, etc. |
| Eclampsia | Infectionb[118]? type |
| Dental caries | Several bacteria infectionsa |
| Hemolytic uremic syndrome | Escherichia Coli 0157a |
| Anemia, arthritis | Parvovirus B19a |
| Bacillary angiomatosis | Bartonella henselaea |
| Chronic lyme arthritis | Borrelia Burgdoferia |
| Acne | Propionbacterium acnea |
Known infectious risk factor.
Probable infectious risk factor.
Prenatal infections and non-communicable disease
NCD causation can be described as a continuum from womb to tomb as an insult before and after birth may subsequently promote the development of NCDs. Evidence for this notion is typified in the Baker's hypothesis which suggest that fetal malnutrition and stress permanently affect development and function of certain organs of the body and predispose to the development conditions such as insulin resistance, non-insulin dependent diabetes mellitus (NIDDM), hypertension, stroke and coronary heart disease in adult life [7], [59].
Infections such as malaria, urinary tract infections (UTI) and Toxoplasmosis, Rubella, Cytomegalovirus and Herpes virus infections are all known causes of fetal malnutrition and intrauterine growth retardation [60], [61] especially in developing countries where these infections are prevalent. In Africa, malaria in pregnancy is a leading cause of fetal malnutrition and IUGR [60]. By directly causing fetal malnutrition, infections can indirectly serve as risk factors in the eventual development of NCD like Type 2 DM, hypertension, obesity and ischemic heart disease in genetically predisposed individuals. Low birth weight children are also at an increased risk of developing physical, cognitive and psychological problems all of which adversely influence their quality of life [62].
Prenatal infections with Rubella, Influenza and Toxoplasmosis have also been hypothesized to have an aetiological role in the development of adult schizophrenia via cytokine-induced alteration of fetal neurodevelopment [63].
Infections and cardiovascular diseases
In the pathway for the eventual emergence of cardiovascular diseases such as hypertension, stroke, ischaemic heart disease and cardiomyopathy, the role of conventional risk factors such as unhealthy diet, alcohol ingestion, smoking, obesity and dyslipidaemia (Table 1) have for long been established. Many studies are now suggesting that infections are also contributory risk factors in the emergence of all these cardiovascular diseases [64], [65], [66], [67], [68], [69], [70]. Although, the role of infections as risk factors for hypertension, stroke and ischaemic heart disease remains inconclusive, there are stronger evidences in support of infections as primary drivers for some cardiomyopathies.
Peripartum cardiac failure (PPCF), a cardiomyopathy causing cardiac failure during pregnancy or 6 months after delivery, is a disease of largely unknown aetiology seen predominantly in black multiparous women of poor socio-economic status [69], [71]. In Zaria, northern Nigeria it has been shown to follow ingestion of high sodium containing potash which induces heart failure in women unable to handle excessive salt [72]. Malnutrition, alcoholism, hypertension and infection-induced myocarditis are other suggested risk factors for PPCF [69], [71]. In Niger, Sub-Saharan Africa, Cenac et al. suggested a possible aetiological role of Chamydiae pneumoniae in PPCF when they demonstrated a significant higher IgG seropositivity in patients with PPCF when compared to controls [70]. PPCF has also been aetiologically linked to viral myocarditis [71]. Myocardial biopsies of patients with PPCF have revealed features consistent with viral myocarditis and Coxsackie B virus is thought to be the most common cause of myocarditis in affected patients [71].
In addition to the numerous non-infectious causes of dilated cardiomyopathy including nutritional deficiencies (e.g. thiamine), toxins (e.g. alcohol), drugs (e.g. adriamycin) and metabolic disorders (e.g. thyrotoxicosis), infections such as HIV, Chagas's disease, Lyme disease are also gradually emerging as prominent causes of dilated cardiomyopathy, especially in the developing world [73]. Idiopathic dilated cardiomyopathy has also been ascribed to Coxsackie B virus and Toxoplasma gondii from serological studies in Africa [64]. Endomyocardial fibrosis (EMF) akin to Loeffler's eosinophilic endocarditis in western world is another cardiomyopathy prevalent in developing countries. Jaiyesimi [74] and Andy et al. [75], [76] in Nigeria have described EMF as a burnt out phase of helminth-induced hypereosinophilia. Microfiliaria, Trichinella Spirallis, Ascaris Hookworm, Schistosomiasis, Giardia Lamblia and Fascioliasis have been reported to be possible triggers for eosinophilia. Eosinophils induce EMF probably through the release of eosinophil basic proteins which are highly toxic to the endothelia and muscles of the heart, blood vessels and other organs [75], [76].
Infections, peptic ulcer and tropical splenomegaly syndrome
Following groundbreaking studies by Marshall and Warren [77], peptic ulcer disease previously attributed to stress, diet, smoking and other environmental factors have now been primarily aetilogically linked due to Helicobacter pylori infection. Helicobacter pylori is also a major aetiological factor in gastritis, gastric cancers and mucosa associated lymphomas. Immune-mediated mechanisms underlie Helicobacter pylori mediated extra-gastric manifestations including such as ischemic heart disease and autoimmune diseases like Sjogren's syndrome [78].
Malaria, an endemic disease in most developing countries, has been implicated in the aetiopathogenesis of hyperimmune malaria splenomegaly syndrome, previously called Tropical Splenomegaly syndrome [79], [80]. This syndrome is characterised by chronic malaria parasitaemia, T-suppressor cell defect, high IgM antibodies, formation of high molecular weight immune complexes and hepatosplenomegaly [79], [80]. It occurs in adults with good immunity against malaria and responds to prolonged antimalarial (proguanil) with regression of splenomegaly [79].
Infections, malnutrition and obesity
Chronic malabsorption in the Tropics is driven primarily by infections of the gastrointestinal mucosa [81]. Protozoan and helminth infections such as Giardia intestinalis, Isospora belli, Cryptosporidium parvum, Strongyloides stercoralis and Capillaria Philippinensis result in weight loss and growth stunting by causing chronic diarrhea and by promoting mucosal abnormalities that result in nutrient malabsorption [81]. Tropical sprue, another cause of malabsorption of unknown aetiology has been linked to mucosal damage induced by bacteria toxins of Klebsiella, Enterobacter and Escherichia coli [81]. Uncommon outside the Tropics, Whipple's disease (previously an unknown cause of weight loss, arthritis and diarrhea) is now established to be due to an infectious agent named Tropheryma whipplei [82].
According to WHO, malnutrition contributes to 50% of under 5 mortality in sub-Saharan with poor nutrition contributing to about 50% of all deaths due to infections [83]. Malaria, diarrheal disease, tuberculosis, respiratory tract infections, measles and several other infectious diseases prevalent in Africa are known to directly or indirectly induce changes that result in malnutrition [83]. Pro-inflammatory cytokines such as IL-1, IL-6, IL-8 and TNF that may be released during any of these infections have been shown to directly induce malnutrition by initiating cellular hypermetabolism, increasing muscle protein catabolism, impairing cellular uptake of fatty acids from plasma triglcerides and promoting sizable lost of many minerals and vitamins [84].
Paradoxically, in the concept named “Infectobesity” infections have been suggested as risk factors contributing to the development of obesity [85]. Dhurandhar et al. [85] observed that human adenovirus type 36 (Ad-36) experimentally induced obesity and paradoxically low levels of serum cholesterol and triglycerides in mice. A role of adenovirus in human obesity was suggested by a study in India where significantly higher prevalence rate of Ad-36 antibodies was reported in the obese humans when compared to non-obese (30% vs. 5%) [85]. Adenoviruses are thought to induce obesity by causing long-term hyperplasia and hyperproliferation of adipocytes [85]. It should be noted however that while the viral-associated obesity in animals has met Koch's criteria for causation, in human, infections are risk factors for obesity requiring concrete causal establishment.
Infections, neuropsychiatric diseases and physical disabiliites
The discovery of prions by Prusiner B in the early 1980s completely revolutionalised the concept of an infectious agent [86]. Prions are small proteinaceous particles that unlike other infectious agents lack DNA or RNA [87]. They are the only known transmissible agents that may manifest as infectious, genetic or sporadic diseases. By causing neuronal dysfunction leading to vacoulation and death of neural cells, proins induce neurodegenerative human diseases and they are now established causes of diseases such as Kuru and Creutzfeldt-Jakob disease [87]. Alzheimer's disease is another neurodegenerative condition where infections such as Chlamydia pnuemonia are thought to play an aetiological role [88] but the evidence remains inconclusive.
In tropical Africa as in most developing countries of the world many non-communicable neurological diseases may follow infections. HIV is a known cause of dementia and has been implicated in several immune-mediated neuropsychiatric manifestations including peripheral neuropathy, transverse myelitis and encephalitis [89]. Human T lymphotrophic virus type 1 (HTLV-I) is an established cause of tropical spastic paraparesis [90], [91]. Self-limiting neuropsychiatric manifestations such as peripheral neuropathy, psychosis, schizophrenia-like states, cerebellar ataxia, parkinsonism and stroke-like states may occasionally be manifestation of severe malaria and typhoid fever [92], [93], [94]. These manifestations are due to direct effects of toxic microbial products on cells of the central nervous system as well as due to effect of high levels of cytokine particularly TNFα.
Physical disabilities have multiple risk factors but it is important to also highlight how some infections are worsening the burden of physical disabilities in the developing world by serving as primary drivers of for instance, limb paralysis and blindness. Poliomyelitis is still endemic in four countries of the world and according to the WHO one in 200 infections leads to paralysis of the lower limbs [95]. Nigeria has one the highest incidence of poliomyelitis cases with high rates of acute flaccid paralysis resulting in long-term disability of affected children [96]. Leprosy is still common in India, Nigeria and South America and it is a major cause of limb deformity, cosmetic disfigurement and permanent disabilities [97].
In view of all the forgoing, it is important for health practitioners in the developing world to also consider an associated infectious risk factor in the evaluation, management and prevention of neuropsychiatric diseases and physical disabilities.
Infections, chronic kidney disease and tropical nephropathy
Hypertension, diabetes mellitus and glomerulonephritis are some of the commonest causes of chronic kidney disease worldwide. While infections have no established role in hypertensive and diabetic-related nephropathy, they are often the major aetiological drivers for glomerulonephritis particularly in developing countries where infections are highly prevalent [99], [100]. Infections can also result in kidney diseases by directly or indirectly damaging the renal parenchyma and interstitium [100]. In the entity named Tropical nephropathy, many infections have been shown to cause renal disease by invasion of the kidney/urinary tract (e.g. schistosomiasis, tuberculosis, leprosy), by direct renal injury (e.g. Salmonella) and by immune-mediated renal damage (e.g. Plasmodium spp., HBV, HCV, Yersinia enterolytica and β hemolytic streptococcus) [99], [100]. Perhaps the earliest and the most remarkable example of how infections can result in renal disease is the Gilles and Hendrichse [101] 1963 account of Nephrosis in Nigerian children attributed to Plasmodium malariae. In a large study amongst adults and children in Uganda, Kibukamusoke et al. [102] in 1967, established a cause and effect relationship between Plasmodium malariae and nephrotic syndrome. This condition now called quartan malarial nephropathy is due to immune complex mediated damage of the kidney [21].
Acute glomerulonephritis may follow β hemolytic streptococcus infections of skin or throat but it is noteworthy that in some parts of the Tropics, scabies in children may promote glomerulonephritis when they become secondarily infected by β hemolytic streptococcus [103], [104]. Aikhonbare and Abdulrahman have given accounts of acute glomerulonephritis in Nigerian children following secondary bacterial infection of scabies skin lesions [103], [104]. Since scabies facilitates infection with β hemolytic skin infection, it also constitutes a risk factor for glomerulonephritis demanding preventative interventions.
Infections and asthma
Asthma is a disease with multifactorial risk factors (Table 1). Infections are also known to be contributory risk factors in the initiation, symptomatic exacerbation and pathological progression of the disease [105], [106], [107], [108]. House dust mites (e.g. dermatophagoides farinae) and respiratory tract infections due to influenza viruses and Chlamydia pneumonia are some examples of infections which can trigger an asthmatic attack and also promote the progression of the disease [106], [108]. Evidence for the role of house dust mite (dermatophagiodes pteronnysinus) and aspergillus flavus in triggering asthma has been suggested by a study from northern Nigeria where significant levels of IgE antibodies of these agents were found in sera of patient with asthma [107]. Some other workers have also reported significantly higher antibodies to Chlamydia pneumonia and Mycoplasma pneumonia in patients with asthma than normal controls [108]. While these findings do not prove causality, they have formed the basis for ongoing research aimed at elucidating the aetiopathogenetic role of several infections in asthma.
In Africa, asthma like symptoms follows infections with several parasitic infections especially during parasite larval migration through the lungs of infected individuals [106]. Hookworm, schistosomiasis and Strongyloides are typical examples of parasitic infections where asthma-like symptoms are known to occur [106]. Routine exclusion of an associated parasitic infection should therefore be an integral component of the management of patients with asthma-like symptoms in the developing world.
Malaria and red cell genetic defects
Hemoglobinopathies, glucose-6-phosphate dehydrogenase deficiency (G6PD) and thalassemia are examples of red cell genetic defects whose evolutional emergence are thought to have been promoted by malaria [110], [111], [112]. Malaria kills a child in Africa every 30 s and according to the WHO malaria causes 1.5–2 million deaths amongst children annually and 90% of these deaths occur in Africa [109]. In other to survive these attacks of malaria, a protective genetic mutation is thought to have been induced by an evolutionary pressure of malaria on the red cell genes of affected populations conferring recipients with survival and reproductive advantage over others [109], [110], [111], [112]. The evolutionary relationship between malaria and sickle hemoglobin is supported by striking coincidences in their geographical distribution [112]. By impairing malarial growth and development, the sickle cell trait (heterozygotes, AS) gives survival advantage over people with normal hemoglobin (AA) in malaria endemic regions [110]. Unfortunately individuals with homozygous state (SS) genetic red cell defects fail to attain survival advantage as they are more likely to have recurrent and severe attacks of malaria most often leading to death. This process by which the heterozygote of two alleles of a gene has an advantage over either of the homozygous states is called balanced polymorphism.
Similarly, the genetic mutation leading to G6PD deficient red cells is thought to have occurred because of the need to survive malaria parasite infection [112]. G6PD prevents generation of oxygen radicals in red cells and in G6PD deficient individual's accumulation of oxygen radicals within red cells prevents the growth of the malarial parasite [112]. Despite all these protective genetic mutations, the malaria parasite, like most infectious agents, is continually evolving new strategies to survive within the human host. For instance, in order to avoid the deleterious effects of oxygen radicals on parasite survival in G6PD deficiency there are reports of Plasmodium falciparum specie that produce their own G6PD [113].
Nanobacteria and tissue calcification
Newly discovered but still controversial bacteria called Nanobacteria or infectious calcifying particles have been shown to possess mineralization properties in in vitro studies and are suggested to directly cause calcium phosphate deposition and stone formation in tissues that characterize diseases like nephrolithiasis, cholelithiasis, vascular plaques, valvular calcification, prostatic stones and psamomma bodies in ovarian cancer [114], [115]. Nanobacteria were identified as cell-walled and self-propagating infectious particles which differed from other known bacteria in their smaller size requiring electron microscope for identification. If confirmed, Nanobacteria will upturn existing paradigms of bacteria infections and may break new frontiers for understanding and unraveling unknown associations between NCDs and infections.
Human endogenous retroviruses (hervs) and NCDs
Studies of the human genome over the last three decades have revealed the existence of endogenous retroviruses which constitute about 1% of the human genome [116]. HERVs are closely related to exogenous animal and human retroviruses and are referred to as ‘fossil’ viruses because they are thought to have been acquired by cross-species transmission of exogenous retroviruses at some point during evolution and are transmitted vertically through the germ-line with inheritance by successive generations in a Mendelian fashion. They may provide evolutionary advantage to the infected host by protecting against exogenous forms of the virus but may be harmful when defective viruses produced by random mutations recombine with other viruses, serve as superantigens or antigenic mimics in promoting disease development [116]. HERVs have been implicated in the aetiopathogenesis of autoimmune diseases such as SLE, Sjogren's disease and Multiple sclerosis and also in cancers especially Germ cell cancers [116].
Implications for an infectious role in emergence of non-communicable diseases
Design of prevention and control strategies for NCDs
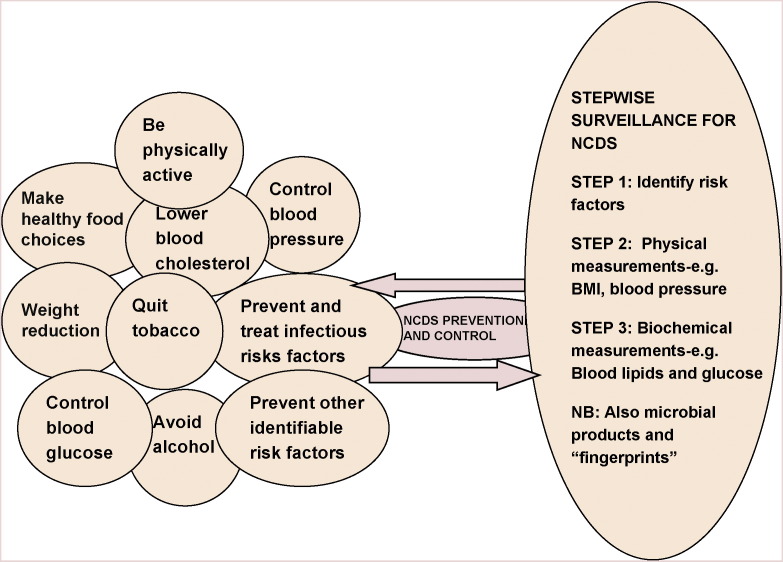
NCDs are diseases with multiplicity of risk factors (Table 1). While focusing and expanding on preventing known risk factors for NCDs there is a need to identify all novel or emerging risk factors for the purpose of an integrated and unparallel NCD control strategy. As evidence gathers for a primary or precipitating role of infections in many NCDs, there is a need to re-design NCD control and preventive strategies to also include infection control while continuing to recognize NCD aetiopathogenesis as spread over a continuum. This review has brought to light the high incidences of various infections in the developing world and the contributory role of infections in programming, initiating, precipitating and promoting the development of NCDs. Consequently, an effective NCDs prevention can only be achieved in developing countries if infection controls is integrated with control of other environmental risk factors (Fig. 1 ). Understanding that infections can contribute to NCD causation from fetal life to adulthood, emphasizes the need to also include prevention of infection in pregnancy (particularly malaria) and prevention of childhood infections (by routine immunization) as integral elements of NCDs control strategy in the developing world.
Figure 1.
Novel integrated approach to NCDs prevention and control in developing countries: identifying and targeting associated infectious risk factors. NB: microbial fingerprints may include microbial DNA, RNA or protein detected by molecular biology techniques.
Prevention and eradication of NCDs by antimicrobial therapy and vaccination
The knowledge of an infectious aetiology of NCDs has offered the potential for preventing and controlling specific NCD through interventions that prevent acquisition of the infection (e.g. vaccination) or eradicates the infection (e.g. antibiotics). Table 3 gives examples of how some NCDs are being prevented by this approach.
Table 3.
Examples of NCDs prevented and managed by strategies targeting known microbial aetiological factors.
| NCD | Antimicobrial/vaccine targets |
|---|---|
| Peptic ulcer disease gastric cancer | Helicobacter pyloria |
| Whipple's disease | Tropheryma whippleia |
| Rheumatic heart disease | β Hemolytic streptococcusa |
| Liver cirrhosis primary liver cell cancer | Hepatitis B virus |
| Cervical carcinoma | Human papilloma virus |
Vaccines yet to be developed.
Successful vaccination and immunization programmes have enormous potential of protecting a large population of people from both infectious diseases and NCDs. Unfortunately, there are still barriers to achieving optimal and sustainable vaccination programmes in many developing countries due to multiple factors [117]. Lack of political wills by local governments, stakeholder apathy and corruption are some examples of factors leading to failure of vaccination programmes in many areas. Inadequate coverage is usually attributed to insufficient supply or absence of vaccines, difficult to reach terrains within communities and rejection of vaccines due to religious/cultural beliefs and illiteracy. There are also problems of high cost of local production of vaccines, lack of knowledge of local antigenic serotypes for many infections and scarcity of the required expertise and technology needed for vaccine development in developing countries. Policy makers in this part of the world must therefore be prepared to re-organize and strengthen their vaccination programmes and also tackle problems confronting provision of effective vaccination. Health practitioners must be proactive in initiating research that identifies prevailing local serotypes of an infection. Non-governmental organizations and countries of the developed world have also a role in providing support and the needed technology for local vaccine development.
Future directions
As old and novel infectious diseases continue to emerge and re-emerge, we are faced with the challenge of not only preventing and managing these diseases but also determine if they may participate in the fusion of risk factors that leads to emergence of novel or even old NCDs. To successfully identify whether any infection is a risk factor or primary aetiological factor for a NCD, there is a need for collaborative efforts between public health physicians, clinicians, pathologist and molecular biologist. This collaboration should be aimed at identifying NCD epidemiological trends, clinical manifestations and disease pathologies in relation to exposure to specific infections. Since not all infections are cultivatable, the role of the molecular biologist is to detect using molecular biotechnology, microbial “finger prints” (such as microbial DNA, RNA or protein) which when detected may further strengthen the evidence suggesting a link between an infection and a NCD. A surveillance network made of all these stakeholders is therefore very necessary and most be strengthened in developing countries.
It should be emphasized that there is a need for all developing countries to make conscious efforts at implementing the WHO stepwise NCD surveillance approach [4] while recognizing the need to also include infectious risk factors in NCDs where infections have strong causal links. Perhaps, one of the greatest challenges in this regard, is the absence of adequate expertise and technology needed for detection of microbial fingerprints by molecular biotechnology. Governmental and NGO within developing countries most therefore take the responsibility of funding the research, training and technology required for molecular diagnosis.
Conclusion
The developing world is presently experiencing two raging epidemics of infectious diseases and NCDS. With the increasing recognition of the role of infections in promoting the emergence of many NCDs, there is a need to integrate infection control efforts with control of other known environmental risk factors for NCDs. This novel NCD preventive approach offers great potential for mitigating the dual infectious diseases and NCDs epidemics in the developing world.
Conflict of interest
Funding: No funding sources.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Facts on chronic disease: WHO Publication 2005. Retrieved August 2008. Available at www.who.int.
- 2.Chronic diseases, facing the facts. WHO publication 2008. http://www.who.int/clip/chronic-disease-report/en/.
- 3.Non-communicable diseases. Publication of Disease Control Priorities Project 2006. The World Bank. Available at www.worldbank.org.
- 4.Surveillance of non-communicable diseases risk factors. WHO publication retrieved January 2008. www.who.int/mediacentre/factsheets/fs273/en/.
- 5.Suerbaum S., Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347(October 10 (15)):1175–1186. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 6.Barker D.J. The development origin of adult disease. Am Coll Nutr. 2004;23(6):588–595. doi: 10.1080/07315724.2004.10719428. [DOI] [PubMed] [Google Scholar]
- 7.Scott J. Homocysteine and cardiovascular disease. Q J Med. 1996;89:561–563. doi: 10.1093/qjmed/89.8.561. [DOI] [PubMed] [Google Scholar]
- 8.Top 10 causes of Death. WHO Fact Sheet. March 2007. http://www.who.int/medicentre/factsheets/ts310.pdf.
- 9.Barreto M.L., Teixeira M.G., Carmo H.E. Infectious disease epidemiology. J Epidemiol Comm Health. 2006;60:192–195. doi: 10.1136/jech.2003.011593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daar A.S., Singer P.A., Persad D.L., Pramming S.K., Matthews D.R., Beaglehole R. Grand challenges in chronic non-communicable diseases. Nature. 2007;November (450):494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 11.Meador RJ. Acute rheumatic fever. E-medicine article updated October 22, 2007. Available at www.e-medicine.com.
- 12.Bahn B.J., Appelt D.M. Role of infection in Alzheimer's disease. J Am Osteopath Assoc. 2001;101(December (12 Suppl.)):1–6. [PubMed] [Google Scholar]
- 13.Dienstag J.L., Isselbacher K.J. Tumours of the liver and biliary tract. In: Braunwald F., editor. 15th ed. vol. 91, no. 1. McGraw Hill (Pub.); 2001. (Harrison's principles of internal medicine). p. 588–589. [Google Scholar]
- 14.Fakunle Y.M., Ajdukiewic A.B., Greenwood B., Edington G.M. Primary liver cell carcinoma (PLCC) in the northern Guinea savannah of Nigeria. Trans Roy Soc Trop Med Hyg. 1977;71(4) doi: 10.1016/0035-9203(77)90114-6. [DOI] [PubMed] [Google Scholar]
- 15.Bouman A., Heineman M.J., Faas M.M. Sex hormones and the immune response in humans. Hum Rep Update. 2005;11(4):411–423. doi: 10.1093/humupd/dmi008. [DOI] [PubMed] [Google Scholar]
- 16.Adrain Hill. The immunogentics of human infectious diseases. Annu Rev Immunol. 1998;16:593–617. doi: 10.1146/annurev.immunol.16.1.593. [DOI] [PubMed] [Google Scholar]
- 17.Bach Jean Francois The effect of infectious in susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347(September (12)):911–920. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 18.Richard R. Human papillomaviruses (HPV) In: Braunwald F., editor. 15th ed. vol. 1, no. 188. McGraw Hill (Pub.); 2001. (Harrison's principles of internal medicine). p. 1118–1120. [Google Scholar]
- 19.Brady H., O’meara Y., Brenner B. The major glomerulopathies. In: Braunwald F., editor. 15th ed. vol. 1, no. 274. McGraw Hill (Pub.); 2001. (Harrison's principle of internal medicine). p. 158. [Google Scholar]
- 20.Mohammed I. The role of immune complexes in human malaria and some of its complications. J Infect. 1982;4:97–104. doi: 10.1016/s0163-4453(82)93625-8. [DOI] [PubMed] [Google Scholar]
- 21.Barsoum R. Malarial Nephropathies. Nephrol Dial Transplant. 1998;13:1588–1597. doi: 10.1093/ndt/13.6.1588. [DOI] [PubMed] [Google Scholar]
- 22.John Gever: Smoking conspires with viruses to advance COPD. MedpageToday, July 24, 2008. www.medpagetoday.com/pulmonary/smokingCOPD/ts/10249.
- 23.Strachan D.P. Hay fever, hygiene and household size. Br Med J. 1989;299:1259–1260. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith RS, Bloomfield S. The hygiene hypothesis and implications for home hygiene. Report of the international scientific forum on Home Hygiene, 2004.
- 25.Greenwood B.M., Voller A. Suppression of autoimmune disease in New Zealand Mice associated with infection with Malaria I & II. Clin. Exp. Immunol. 1970;8 793 and 805. [PMC free article] [PubMed] [Google Scholar]
- 26.Epstein F. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 27.Eder W., Ege M., Von-Mutius E. The asthma epidemic. N Engl J Med. 2006;355(November (21)):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 28.Microbial Triggers of Chronic illness. Publication of American Academy of Microbiology 2005. www.asm.org.
- 29.Strange Bed fellows; Infection and Chronic disease. Conference report. Canadian Public Health Association 2001. www.cpha.com.
- 30.Connor S.M., Taylor C.E., Hughes S. Emerging infectious determinants of chronic diseases. Emerg Infect Dis. 2006;12(July (7)):1051–1057. doi: 10.3201/eid1207.060037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pincus Seth. vol. 71, no. 1. ASM Press; 2006. (Potential role of infectious in chronic inflammatory diseases). p. 529–535. [Google Scholar]
- 32.Scarisbrick A., Rodriguez M. Hit-Hit and Hit run. Viruses in the playing field of multiple sclerosis. Curr Neuro Neurosci Rep. 2003;3(June (3)):265–271. doi: 10.1007/s11910-003-0087-9. [DOI] [PubMed] [Google Scholar]
- 33.Noseworthy J., Lucchiretti C., Rodriguez M., Weinsheinker B. Multiple Sclerosis. N Engl J Med. 2000;(September 28):938–952. doi: 10.1056/NEJM200009283431307. [DOI] [PubMed] [Google Scholar]
- 34.Sanjay Sethi Bacterial Infections and the pathogenesis of COPD. Chest. 2000;117:2865–2913. doi: 10.1378/chest.117.5_suppl_1.286s. [DOI] [PubMed] [Google Scholar]
- 35.Hemalatha V., Srikanth P., Mallika M. Superantigens—concepts, clinical disease and therapy. Int J Med Microbiol. 2004;22(4):204–211. [PubMed] [Google Scholar]
- 36.Platts-Mill T., Male D., Hay F., Britton W., Westwood O. Hypersensitivity reactions. In: Ivam R., Brostoff J., Male D., editors. Immunology. 6th ed. Mosby (Pub.); 2001. p. 323–382. [Google Scholar]
- 37.Lori A., Inman R.D. Molecular mimicry and autoimmunity. N Engl J Med. 1999;(December):2068–2074. doi: 10.1056/NEJM199912303412707. [DOI] [PubMed] [Google Scholar]
- 38.Ivam R., Brostoff J., Male D., editors. Immunology. 6th ed. Mosby (Pub.); 2001. Autoimmunity and autoimmune disease. p. 401–415. [Google Scholar]
- 39.Hypersensitivity. In Wikipedia Free encyclopedia updated 31 July 2008. Available at www.wikipedia.com.
- 40.Carty S.M., Snowden N., Silman A.J. Should infection still be considered as the most likely triggering factor for rheumatoid arthritis? Ann Rheum Dis. 2004;63(Suppl. 11):i46–ii49. doi: 10.1136/ard.2004.028241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cancer. WHO Fact Sheet. 2006, Feb. Available at www.who.int.
- 42.Cancer. In Wikipedia free encyclopedia. 2008 January. Available at www.wikipedia.com.
- 43.Kim C., Koke K., Saito L., Miyamura T., Jay G. HBX gene of hepatitis B virus induces liver cancer in transgenic mice. Nature. 1991;351(May 23):317–320. doi: 10.1038/351317a0. [DOI] [PubMed] [Google Scholar]
- 44.Brechot C. Pathogenesis of hepatitis B virus related hepatocellular carcinoma; old and new paradigms. Gastroenterology. 2003;127(5):556–561. doi: 10.1053/j.gastro.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 45.Gravitt P. HPV: the ultimate cancer initiator. HPV Today Monogr. 2003;3(September):1–4. [Google Scholar]
- 46.Yasunagu J., Matsuoka M. Human T-cell leukemia virus, type 1 induces adult T cell leukemia: from clinical aspects to molecular mechanism. Cancer Control. 2007;14(April (2)):133–140. doi: 10.1177/107327480701400206. [DOI] [PubMed] [Google Scholar]
- 47.Cohen J.I. Epstein-Barr virus infection. N Engl J Med. 2000;343(August 17 (7)):481–492. doi: 10.1056/NEJM200008173430707. [DOI] [PubMed] [Google Scholar]
- 48.Ming L., Thorgeirsson S.S., Gail M.H., Lu P., Harris C.C., Wang N. Dominant role of hepatitis B virus and cofactor role of aflatoxin in hepatocarcinogenesis in Qidong, China. Hepatology. 2002;36(November (5)):1046. doi: 10.1053/jhep.2002.36366. [DOI] [PubMed] [Google Scholar]
- 49.Ndububa D.A., Yakicier C.M., Ojo O.S., Adeodu O.O., Rotimi O., Ogunbiyi O. P53 Codon 249 mutation in hepatocellular carcinoma from Nigeria. Afr J Med Med Sci. 2001;30(March–June (1–2)):125–127. [PubMed] [Google Scholar]
- 50.Onyemelukwe G.C., Ogbadu G., Salifu A. Aflatoxins B1, B2, G1, G2 in primary liver cell carcinoma. Toxico Lett. 1982;10(February (2–3)):309–312. doi: 10.1016/0378-4274(82)90093-5. [DOI] [PubMed] [Google Scholar]
- 51.Onyemelukwe G.C., Nirodi C., West C.E. Aflatoxin B in hepatocellular carcinoma. Trop Geogr Med. 1980;32(September (3)):237–240. [PubMed] [Google Scholar]
- 52.Khurana S., Dubey M.L., Malla N. Association of parasitic infections and cancers. Indian J Med Microbiol. 2005;23(2):74–79. doi: 10.4103/0255-0857.16044. [DOI] [PubMed] [Google Scholar]
- 53.Rezaee J.A., Cunningham C., Davison A., Blackbourn D.J. Kaposi's sarcoma associated herpes virus immune modulation: an overview. J Gen Virol. 2006;87:1781–1804. doi: 10.1099/vir.0.81919-0. [DOI] [PubMed] [Google Scholar]
- 54.Lederman M. Immunopathogenesis of HIV; In HIV In-site Knowledge base. January 2006. Available at www.hivinsite.com.
- 55.Beverley P. Tumour immunology. In: Roit Ivan, Brostof H., Male D., editors. Immunology. 6th ed. Mosby (Pub.); 2001. p. 289–300. [Google Scholar]
- 56.Schouten JT. AIDS-Related Cancer; An update; In The Body, Retrieved August 2008, http://www/thebody.com/content/cert,4400.html.
- 57.Whittle H.C., Brown J., Marsh K., Blackman M., Jobe O., Shenton F. The effects of plasmodium Falciparum on immune control of B lymphocytes in Gambian children. Clin Exp Immunol. 1990;80(May (2)):213–218. doi: 10.1111/j.1365-2249.1990.tb05236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lubega J. T-helper 1 versus T-helper 2 lymphocyte immunodysregulation is the central factor in genesis of Burkitt's lymphoma; hypothesis. Infect Agents Cancer. 2007;2(10):2–10. doi: 10.1186/1750-9378-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Forrester T. Historic and early life origins of hypertension in Africans. J Nutr. 2004;134:211–216. doi: 10.1093/jn/134.1.211. [DOI] [PubMed] [Google Scholar]
- 60.Malaria in pregnancy. Roll back malaria, WHO Retrieved August 2008. http://www.int/CMC-upload,10/000/015/369/RBMinfosheet_4.htm.
- 61.Dogra SV. Intrauterine growth retardation. Update. Dec. 28, 2006. e-medicine, available at www.emedicine.com.
- 62.Intrauterine growth retardation in newborn children. WHO publication. http://www/who.int/ceh/indication/ugrnewborn.pdf. Retrieved August 2008.
- 63.Brown A.S. Prenatal Infections as a risk factor for schizophrenia. Schizophrenia Bull. 2006;32(2):200–202. doi: 10.1093/schbul/sbj052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Falase A.O., Sekoni G.A., Adenle A.D. Dilated cardiomyopathy in young Africans; a sequel to infections. Afr J Med Med Sci. 1982;11:1–5. [PubMed] [Google Scholar]
- 65.Falase A.O. Infections dilated cardiomyopathy in Nigeria. Heart Vessels Suppl. 1985;1:40–44. doi: 10.1007/BF02072358. [DOI] [PubMed] [Google Scholar]
- 66.Cook P.J., Lip G.Y. Infectious agents and atherosclerotic vascular disease. Q J Med. 1996;89:727–735. doi: 10.1093/qjmed/89.10.727. [DOI] [PubMed] [Google Scholar]
- 67.Cook P.J., Lip G.Y., Davies P., Beevers D.G., Wise R., Honeybourne D. Chlamydia pneumonia antibodies in severe essential hypertension. Hypertension. 1998;31:589–594. doi: 10.1161/01.hyp.31.2.589. [DOI] [PubMed] [Google Scholar]
- 68.Wimmer M.L., Sandmann-Strupp R., Saikku P., Haberl R.L. Association of Chlamydia Infection with Cardiovascular disease. Stroke. 1996;27(December (12)):2207–2210. doi: 10.1161/01.str.27.12.2207. [DOI] [PubMed] [Google Scholar]
- 69.Falase A.O. Peripartum heart disease. Heart Vessels Suppl. 1985;1:232–235. doi: 10.1007/BF02072400. [DOI] [PubMed] [Google Scholar]
- 70.Cenac C., Djibo A., Sueur J.M., Chaigneau C., Orfila J. Chlamydia infection and Peripartum Cardiomyopathy. Nigerian Med Trops (Mars) 2000;60(2):137–140. [PubMed] [Google Scholar]
- 71.Bhakta P., Biswas B., Barnerjee B. Peripartum Cardiomyopathy. Yonsei Med J. 2007;48(5):731–747. doi: 10.3349/ymj.2007.48.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ford l., Abdullahi A., Anjorin F., Danbauchi S., Isa M., Mauda G. The outcome of peripartum cardiac failure in zaria. Nigeria Q J Med. 1998;91:93–103. doi: 10.1093/qjmed/91.2.93. [DOI] [PubMed] [Google Scholar]
- 73.Wynne J., Braunwald E. The Cardiomyopathies and Myocarditis. In: Braunwald Fauci., editor. 15th ed. vol. 238. McGraw Hill (Pub.); 2001. (Harisson's principles of internal medicine). p. 1359–1365. [Google Scholar]
- 74.Jaiyesimi F. Controversies and advances in Endomyocardial fibrosis—a review. Afr J Med Med Sci. 1982;11:37–46. [PubMed] [Google Scholar]
- 75.Andy J.J. Aetiology of Endomyocardial fibrosis (EMF) West Afr J Med. 2001;20(July–September (3)):199–207. [PubMed] [Google Scholar]
- 76.Andy J.J., Ogunowo P.O., Akpan N.A., Odigwe C.O., Ekanem I.A., Esin R.A. Helminth associated hypereosinophilia and tropical endomyocardial fibrosis (EMF) in Nigeria. Acta Tropica. 1998;69(May (2)):127–140. doi: 10.1016/s0001-706x(97)00125-3. [DOI] [PubMed] [Google Scholar]
- 77.Marshall B.J., Warren J.R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 78.Gasbarrini A., Franceschi F., Armuzzi A., Ojetti V., Candelli M., Torre E. Extradigestive manifestations of Helicobacter pylori gastric infection. Gut. 1999;45:9–12. doi: 10.1136/gut.45.2008.i9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paparello S., Hoffman S. Hyper-reactive malarial splenomegaly I & II. Postgrad Doct Afr. 1993;15(2–3):20–24. 48-51. [Google Scholar]
- 80.Bryceson A., Fakunle Y.M., Fleming A.F., Crane G., Hutt M.S., de Cock K.M. Malaria and splenomegaly. Trans Soc Trop Med Hyg. 1983;77:879–883. doi: 10.1016/0035-9203(83)90319-x. [DOI] [PubMed] [Google Scholar]
- 81.Ramakrishna B.S., Venkataraman S., Mukhopadhy G.A. Tropical malabsorption. Postgrad Med J. 2006;82:779–787. doi: 10.1136/pgmj.2006.048579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fenollar F., Puechal X., Raoult D. Whipple's disease. N Engl J Med. 2007;356:55–66. doi: 10.1056/NEJMra062477. [DOI] [PubMed] [Google Scholar]
- 83.Water related diseases. WHO 2008. Available at www.who.int.
- 84.Beisel W.R. Infection induced malnutrition; from cholera to cytokines. Am J Clin Nutr. 1995;62:813–819. doi: 10.1093/ajcn/62.4.813. [DOI] [PubMed] [Google Scholar]
- 85.Dhurandhar N. Infectoberity: obesity of infectious origin. J Nutr. 2001;131:2794–2797. doi: 10.1093/jn/131.10.2794S. [DOI] [PubMed] [Google Scholar]
- 86.Prusiner S.B. Novel Proteinaceous infectious particles cause Scrapie. Science. 1982;216:136–144. doi: 10.1126/science.6801762. [DOI] [PubMed] [Google Scholar]
- 87.Johnson R.T., Gibbs C.J. Creutzfeldt–Jakob disease and related transmissible Spongiform Encephalopathies. N Engl J Med. 1998;339(December 31 (27)):1994–2004. doi: 10.1056/NEJM199812313392707. [DOI] [PubMed] [Google Scholar]
- 88.The Emerging Role of Infection in Alzheimer, Disease IOS Press 2008, May 25. Science Daily. Retrieved August 9, 2008.
- 89.Vitiello B, Vitkovic L. The links between infections and Psychiatric Diseases. Medscape Psychiatry & Mental Health e-Journal, 1997, 2 (2) Retrieved August 2008.
- 90.Gessaini A., Francis H., Sonan T., Giordano C., Akani F., Piquemal M. HTLV-1 and Tropical spastic paraparesis in Africa. Lancet. 1986;2(September 20 (8508)):698. doi: 10.1016/s0140-6736(86)90218-7. [DOI] [PubMed] [Google Scholar]
- 91.Cabre P., Smadja D., Cabie A., Newton C.J. HTLV-1 and HIV infection of the Central Nervous System in tropical areas. J Neurol Neurosurg Psychiatry. 2000;68:550–557. doi: 10.1136/jnnp.68.5.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ali G., Rashid S., Kamli M.A., Shah P.A., Allaqaband G.Q. Spectrum of neuropsychiatric complications in 791 cases of typhoid fever. Trop Med Int health. 1997;2(4):314–318. doi: 10.1111/j.1365-3156.1997.tb00145.x. [DOI] [PubMed] [Google Scholar]
- 93.Danbauchi S.S. Malaria presenting with self limiting cerebellar syndrome. Nigerian J Med. 1995;4(1):18–20. [Google Scholar]
- 94.Garg R.K., Kerak B., Misra S. Neurological manifestation of malaria: an update. Neurol India. 1999;47:85–91. [PubMed] [Google Scholar]
- 95.Poliomyelitis. WHO Fact sheet Update January 2008. Available at www.who.int.
- 96.Wild poliovirus weekly update; publication of Global polio eradication initiative. 2008, Aug 6. http://www.polioeradication.org/casecount.asp.
- 97.Leprosy. WHO fact sheet October 2005. Retrieved August 2008. Available at www.who.int.
- 99.Kibukamusoke J.W. (ed.) Tropical Nephropathy Citforge Pty Ltd, G.P.O. Box 1291, Canberra City, ACT 2601, Australia, 1984.
- 100.Akinkugbe O.O. Tropical nephropathy: an overview. Afr J Med Med Sci. 1992;21(October (1)):3–7. [PubMed] [Google Scholar]
- 101.Gilles H.N., Hendrichse R.G. Nephrosis in Nigerian Children Role of Malaria and effect of antimalarial treatment. Br Med J. 1963;2:27. doi: 10.1136/bmj.2.5348.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kibukamusoke J.W., Hunt M.R., Wilkes N.E. The Nephrotic syndrome in Ugandan and its association with Quartan Malaraie. Q J Med. 1967;36:393. [PubMed] [Google Scholar]
- 103.Aikhonbare H.A., Abdulrahman M.B. Acute glomerulonephritis in Zaria, Nigeria. Nig. J. Pediatrics. 1984;11(2):59–62. [Google Scholar]
- 104.Abdurrahman M.B. The role of infectious agents in the aetiology and pathogenesis of childhood nephritic syndrome in Africa. J Infect. 1984;8(March (2)):100–109. doi: 10.1016/s0163-4453(84)92356-9. [DOI] [PubMed] [Google Scholar]
- 105.Gencay J.B., Ridiger J., Tamm M., Soler M., Perruchoud A., Roth M. Increased frequency of Chlamydia pneumonia antibodies in patients with asthma. Am J Respir Crit Care Med. 2001;163:1097–1100. doi: 10.1164/ajrccm.163.5.2003162. [DOI] [PubMed] [Google Scholar]
- 106.Wjst M., Boakye D. Asthma in Africa. PLOS Med. 2007;4(February (2)):e72. doi: 10.1371/journal.pmed.0040072. 0203–0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Onyemelukwe G.C., Shakib F., Saeed T.K., Salloum Z.A., Lawande R.V., Obineche E. RAST—specific IgE in Nigerian asthmatic patients. Ann Allergy. 1986;56(February (2)):167–170. [PubMed] [Google Scholar]
- 108.Casell G.H. Infectious causes of chronic inflammatory disease and cancer. Emerg Infect Dis. 1998;4(July–September (3)) doi: 10.3201/eid0403.980339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Malaria. WHO fact sheet 2007, May, Retrieved August 2008. Available at www.who.int.
- 110.Nagel R.L., Roth E.F. Malaria and red cell genetic defects. Blood. 1989;74:1213–1221. [PubMed] [Google Scholar]
- 111.Malaria and the sickle cell Hemoglobin Gene 2002. April. Available at www.sickle.bioh.harvard.edu/malariasickle.html.
- 112.Adaptation by Natural selection; Sickle cell Hemoglobin and Malaria. http://www.as.ua.edu/ant/bindos/ant475/sicklecell/sicklecell.pdf. 2004.
- 113.Usanga E.A., Luzzatto L. Adaptation of plasmodium falciparum to glucose-6-phosphate dehydrogenase deficient host red cells by production of parasite encoded enzyme. Nature. 1985;313:793–795. doi: 10.1038/313793a0. [DOI] [PubMed] [Google Scholar]
- 114.Kajander E.O., Ciftcioglu N. Nanobacteria: an alternative mechanism for pathogenic intra- and extra cellular calcification and stone formation. Proc Natl Acad Sci USA. 1998;95(July):874–889. doi: 10.1073/pnas.95.14.8274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Urbano P., Urbano F. Nanobacteria: facts or fancies. PLOS Pathogens. 2007;3(5):e55. doi: 10.1371/journal.ppat.0030055. 0567-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nelson P.N., Carnegie P.R., Martin J., Ejtehadi D., Hooley P., Roden D. Demystified-Human Endogenous Retroviruses. Mol Pathol. 2003;56(February (1)):11–18. doi: 10.1136/mp.56.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.WHO fact sheet. Immunization against diseases of public health importance. March 2005. Available at www.who.int.
- 118.Ekwempu C.C. Infection Theory of Eclampsia Re-evaluated. Int J Gynaecol Obstect. 1980;18(4):300–302. doi: 10.1002/j.1879-3479.1980.tb00500.x. [DOI] [PubMed] [Google Scholar]