Abstract
Clots in the fetal circulation of the placenta may occlude or narrow the lumens of fetal vessels sufficiently to diminish the placental oxygen and nutritional exchange, causing significant reduction in placental function. When extensive, growth restriction, neonatal encephalopathy, and stillbirth may occur. Propagation of clots in other organs, such as brain, kidney, and liver, may affect the function of these organs, resulting in infarcts and neonatal stroke. This article presents an account of the placental pathology and clinical sequelae of this condition, called fetal thrombotic vasculopathy.
Keywords: Fetal thrombotic vasculopathy, Clots, Placental oxygen, Fetal circulation
Overview
Fetal thrombotic vasculopathy (FTV) is a vascular thrombotic condition causing obstruction of arteries and veins in the fetal circulation of the placenta, resulting in ischemic changes in the villi peripheral to the obstruction. When sufficiently extensive, FTV may cause a reduction in functional placental reserve or in other cases may be associated with additional thrombotic or thromboembolic events in the somatic vessels of the fetus itself. When extensive, the former condition can lead to fetal growth restriction or stillbirth, whereas the latter may result in infarcts of various fetal structures, such as the brain, kidney, or, rarely, an extremity, such as an arm or leg. As with intravascular clotting in general, causal factors of FTV include a combination of the triad of stasis (by compression of cord or aberrant vessels); a thrombophilic state, both genetic (eg, protein S or factor V Leiden) and acquired (anticardiolipin antibody and so forth); and vascular injury (inflammatory and localized compression). The most serious outcomes include growth restriction, neurologic injury, and perinatal death.
Key Features FTV: Potential Morphologic or Clinical Associations and Sequelae.
Obstructive cord lesion or cord accident (common)
Admit to neonatal ICU; normal at discharge (common)
Neonatal encephalopathy (%)
Cerebral palsy (rare); includes cerebral infarct, porencephalic cyst, hypoxic-ischemic encephalopathy
Stillbirth (uncommon)
Intrauterine growth restriction (uncommon)
Oligohydramnios
Maternal diabetes mellitus (common)
Maternal autoimmune disease (lupus, anticardiolipin antibodies, and so forth) (uncommon)
Severe acute respiratory syndrome (rare)
Cytomegalovirus, Toxoplasma gondii (rare)
Transverse limb reduction (rare)
Maternal thrombophilic state (occurs equally in nonthrombophilic mothers)
Prevalence
In an unselected series of 1153 deliveries, FTV was identified histologically in 11 placentas (1%), including 1 case of maternal gestational diabetes and 2 newborns small for gestational age; the remaining 9 mothers and newborns were clinically normal.1 In a selected series of 2910 placentas submitted for clinical indications from a total of 19674 deliveries, 183 placentas (6%) had histologic FTV.2
Clinical features
Before delivery, FTV is clinically silent, with no predelivery warning of its presence. As discussed previously, FTV occurs more frequently in placentas selected for clinical study than in unselected pregnancies, but the factors involved in selection of placentas for pathologic study are diverse and nonspecific: maternal hypertension and diabetes mellitus, fetal growth restriction, abnormal fetal heart rate during labor, and so forth. Ultrasound and other imaging techniques do not detect FTV. When there seems to be some sort of fetal distress during labor, there is no way to suggest that the actual cause of these symptoms is FTV until the placenta is examined. In most cases, when FTV is identified on placental examination, the newborn usually appears well, there are no subsequent clinical abnormalities in the nursery, and the newborn goes home on schedule. Especially in more extensive or severe cases, FTV is associated significantly with neonatal encephalopathy,3 cerebral palsy,4 intrauterine growth restriction,5 stillbirth, oligohydramnios, and fetal cardiac anomalies.6 Cerebral infarcts may be the most common specific cerebral lesion associated with placental FTV.7
Other fetal structural anomalies attributed to vascular disruption (including thrombi) include porencephaly, cerebral infarcts, bowel atresias, gastroschisis, unilateral renal absence, cleft lip or palate, and transverse limb or digit reduction.8
Risk factors
The most significant predisposing abnormalities are problems resulting in vascular stasis. These include cord prolapse, hypercoiling, and velamentous insertion.9, 10 Large vessel thrombi have a similar effect. FTV is a major finding in cases of stillbirth, even after the vascular features secondary to stillbirth itself are excluded.6 In a study of 130 stillbirths in Australia, proved perinatal cytomegalic inclusion infection occurred in 20 cases; FTV was found disproportionately in more (60%) of the cytomegalovirus cases compared with a smaller number (28%) of the noninfected cases. FTV may occur more frequently in association with maternal diabetes mellitus.1 Extensive FTV was discovered in the placentas of 2 women convalescent in the third trimester with severe acute respiratory syndrome during an outbreak in Hong Kong11; the 2 newborns were growth restricted.
The possibility of a correlation between placental FTV and parental or fetal thrombophilias has been suggested by anecdotal observations and some earlier studies.12, 13, 14, 15 Later observations, controlled by comparing FTV cases with non-FTV cases, found similar proportions of maternal thrombophilias in the FTV and non-FTV cases.16, 17, 18 FTV and thrombophilias occur together, but a thrombophilia alone does not seem to increase the prevalence of FTV.
Box 1 summarizes risk factors for FTV.
Box 1. Risk factors for fetal thrombotic vasculopathy.
Stasis: cord compression and cord hypercoiling
Maternal diabetes mellitus
Neonatal encephalopathy
Growth restriction
Stillbirth
Gross features
Thrombi in the larger vessels of the chorionic plate are often visible on gross examination (Fig. 1 ). Distension of the chorionic plate vessels (Fig. 2 ) should prompt a search for thrombosed fetal vessels and for devascularized villi by selecting multiple tissue blocks for histologic confirmation. Regions to select for this purpose include pale triangular regions with a base at the maternal surface (Fig. 3 ). Areas of villous parenchyma peripheral to an occluded vein are often darker red and congested. Older lesions may become firm and depigmented, eventually with a gray-white color. Even large lesions can often be indistinct and difficult to recognize. Formalin fixation may accentuate the appearance of lesions that were not apparent on sectioning of the fresh placenta.
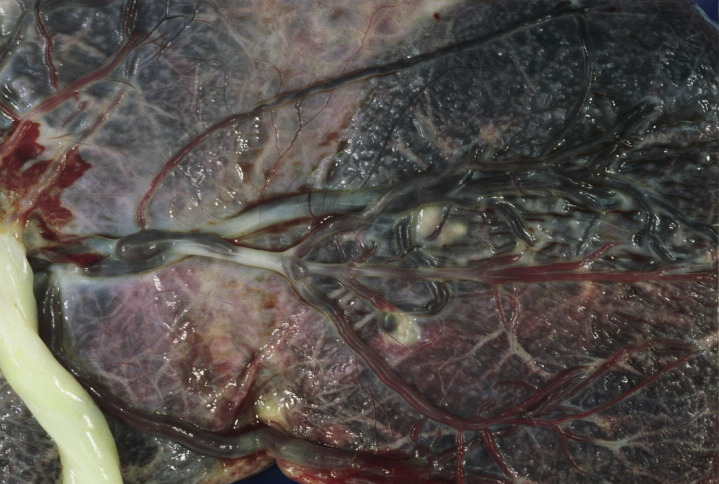
Fig. 1.
A recent thrombus caused expansion of a large fetal artery in the chorionic plate, near the cord insertion, at the left margin.
Fig. 2.
Note the distended vessels in the chorionic plate, as seen in cross-sections of the placenta. Extensive FTV was present in all 12 microscopic sections from widely distributed areas, resulting in dilatation and congestion of vessels proximal to zones of obstruction.
(From Kraus FT, Redline RW, Gersell DJ, et al. Placental Pathology. Washington, DC: American registry of Pathology; 2004:144; with permission.)
Fig. 3.
Multiple areas of FTV form pale triangular areas with base at the maternal surface. This newborn had severe neonatal encephalopathy. Avascular villi from this placenta are shown in Fig. 10.
FTV is commonly associated with functionally significant or potentially obstructive lesions of the umbilical cord, including velamentous insertion, hypercoiling, abnormally long cord, and effects of compression and stasis, such as fetal vascular ectasia and major fetal vessel thrombosis.9, 19
Box 2 summarizes the gross morphology of FTV.
Box 2. Gross morphology of fetal thrombotic vasculopathy.
Large vessels: red or light brown occlusive or nonocclusive thrombi; distended vessel lumens suggesting stasis and increased pressure
Placental cross sections: wedge-shaped areas, pale red-pink if recent; pale tan, if older (chronic)
Microscopic features
The microscopic patterns of the vascular lesions grouped under the general term, fetal thrombotic vasculopathy, vary, especially as the lesions evolve over time. The appearance of the lesions in the larger vessels of the chorionic plate and stem vessels differs from that of the lesions in the capillaries of the terminal villi.
Thrombi in larger vessels have an evolving sequence similar to the histologic changes in thrombosed veins and arteries in adults. Acutely, the vessel wall is distended; the clot becomes adherent as the endothelial cells lyse and disappear and often develops a layered appearance with strata of red cells alternating with leukocytes and fibrin (Fig. 4 ). The breakdown of the endothelial interface allows red blood cells to extravasate and become distributed in variable numbers into the vessel wall (Fig. 5 ).
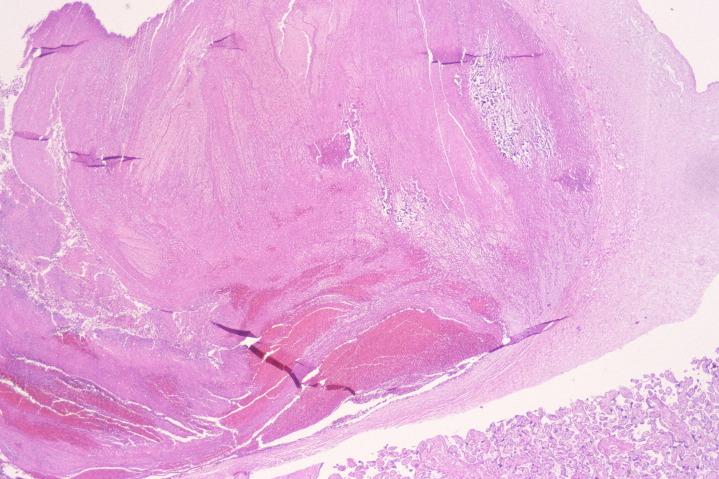
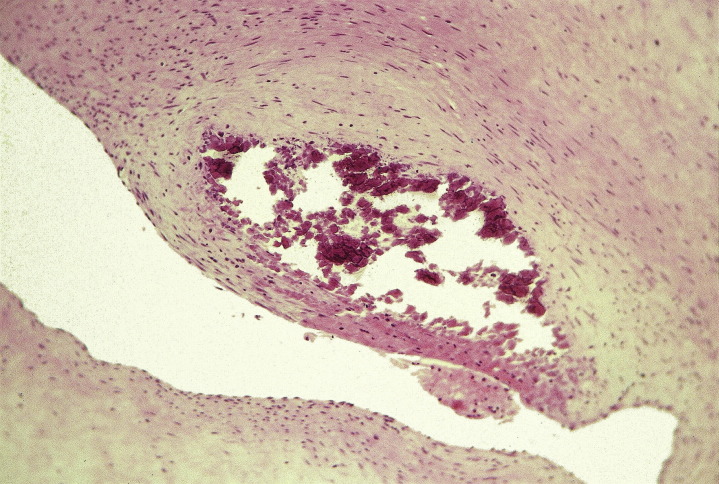
Fig. 4.
Layered blood elements formed progressively over a period of several days in this thrombus occluding a large chorionic plate vessel. Note more recent stratification of red blood cells alternating with layers of fibrin and leukocytes at bottom left. There is an older pale blue granular zone of calcification near the right margin (hematoxylin-eosin, original magnification ×15).
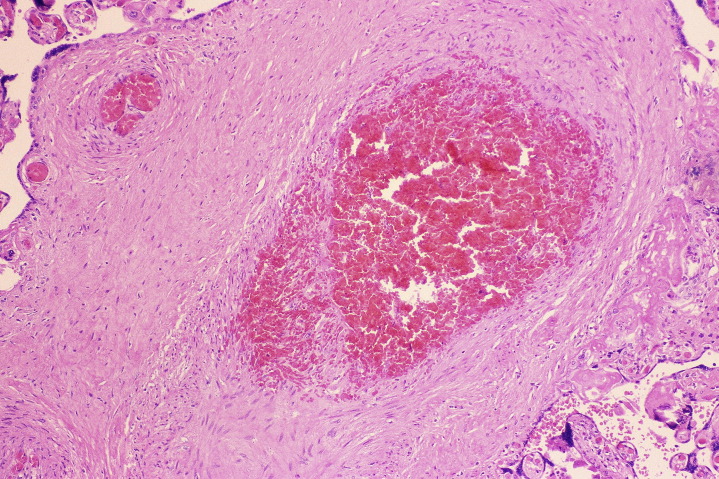
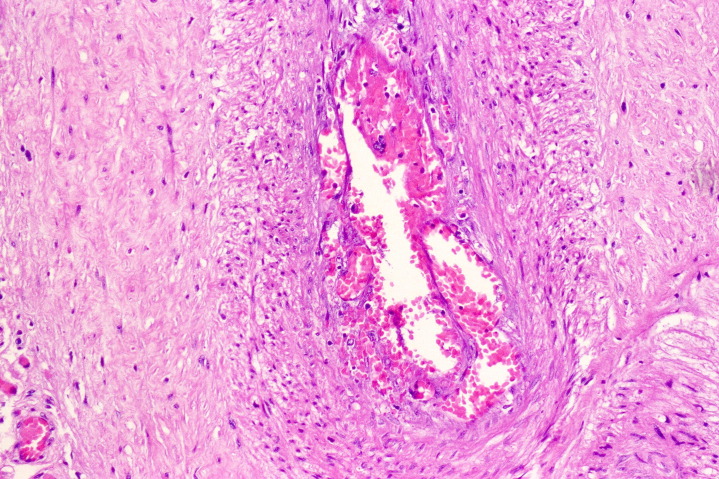
Fig. 5.
Chorionic plate artery (right) occluded by thrombus several days old, with prominent infiltration by fibroblasts. Note the extravasation of red blood cells at the endothelial margin. There are clumps of fibrin within the clot (hematoxylin-eosin, original magnification ×200).
A variant early lesion is a focal accumulation of fibrin, with or without edema, beneath the vascular endothelium of stem vessels, called fibrinous vasculosis.20 In some cases, stem vessels become narrowed by expanded subendothelial organizing masses of connective tissue matrix, lesions called intimal fibrin cushions (Fig. 6 ).21 Focal calcification in these lesions is generally accepted as evidence of increasing chronicity.
Fig. 6.
This chronic intimal fibrin cushion forms an expanded mass within the wall of a large chorionic plate artery, bulging into the lumen. A more recent lesion would contain intramural fibrin or fibrinoid. An adherent mural thrombus may sometimes be present. Focal calcification, as in this image, is common (hematoxylin-eosin, original magnification ×300).
Progressively, as thrombi age and become chronic, spindle cells resembling fibroblasts appear within the thrombus, forming a pattern called septation, in which the fragmenting red cells are divided into multilocular spaces (Fig. 7 ). Eventually the vessel lumen becomes obliterated, so that only an indistinct outline remains; red blood cells, distorted and fragmented, may persist even in the lumen and in the degnerated vascular wall (Fig. 8 ). Calcification may occur focally in the vessel wall as well as in the clot itself (see Figs. 4 and 6). Histologic distinction between arteries and veins after these chronic alterations becomes difficult or impossible.
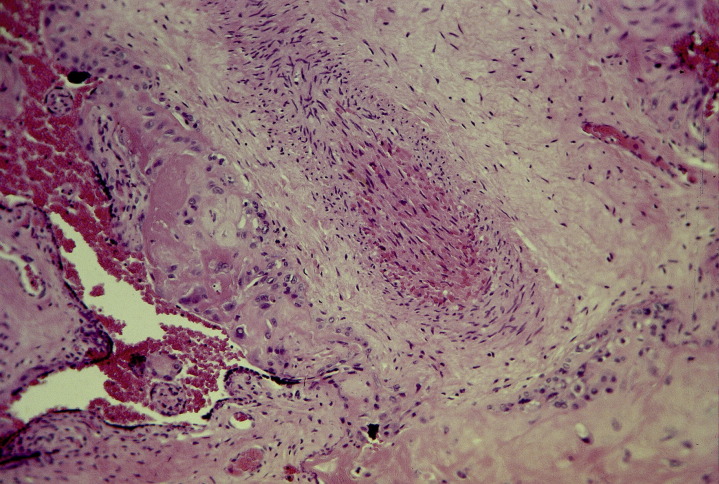
Fig. 7.
Septation in a stem artery is characterized by strands of spindle-shaped fibroblastic cells that dissect into the lumen, separating clusters of red cells into small loculated spaces (hematoxylin-eosin, original magnification ×200). This is from the same placenta as shown in Figs. 4, 5, and 11. This process begins multifocally in areas of stasis in approximately 2 days and becomes extensive after 2 or more weeks.
(From Genest DR. Estimating the time of death in stillborn fetuses: II. Histologic evaluation of the placenta; a study of 71 stillborns. Obstet Gynecol 1992;80:585–92; with permission.)
Fig. 8.
This is an older occluded stem vessel, with completely obliterated lumen. Scattered degenerating red blood cells persist in the organized central area (hematoxylin-eosin, original magnification ×100).
Hemorrhagic endovasculopathy (HEV) is a vasodisruptive process affecting fetal vessels, from the larger stem vessels down to fetal capillaries. At early stages, the integrity of the vessel wall is lost and fragmented endothelial nuclei persist, intermixed with masses of erythrocytes that spill out into the villous stroma and dissect into the walls of larger vessels. The stem vessel wall in HEV appears consistently disrupted with extravasation of red cells. The affected villi in HEV may appear filled, even expanded, by stromal hemorrhage. In time, the stem vessels of both FTV and HEV may show septation and the villi eventually become avascular and hyalinized.
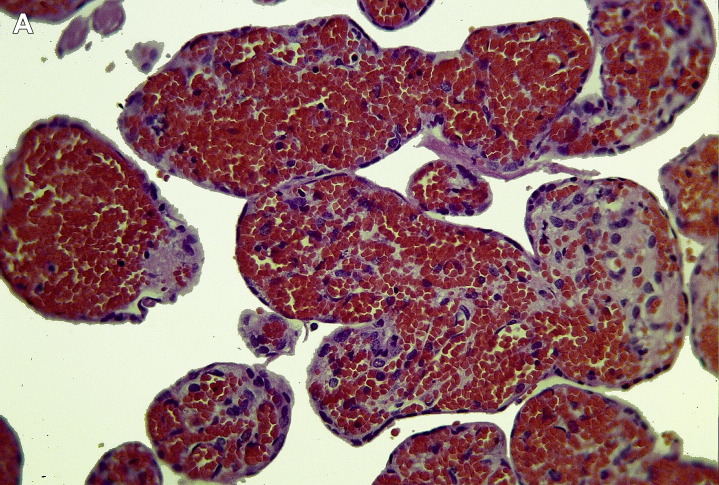
I have been able to show that villi in the distribution of a large placental vein showed the hemorrhagic pattern of HEV (Fig. 9 A),2 suggesting that this may be a variant of FTV in which the main occlusive vessel is sometimes a large placental vein. The clinical and pathologic features of typical FTV and HEV have many similarities. The villi and villous capillaries in the regions of placenta served by the occluded veins or arteries no longer function. In recent lesions (2–5 days), the capillary endothelial cells are at first fragmented (see Fig. 9B); then the red cells, also fragmented, are extravasated, sometimes extensively into the villous stroma (see Fig. 9A). Ultimately, both capillaries and red cells disappear (Fig. 10 ). In chronic villous lesions (4–5 weeks), only an acellular hyalinzed core remains, surrounded by the villous trophoblast, which remains viable (Fig. 11 ). The trophoblast layer survives because it is kept alive by the continued circulation of maternal blood in the intervillous space. Iron is deposited in the basement membrane beneath the trophoblast (Fig. 12 ) and in small clumps in the villous stroma as the red cells disappear.
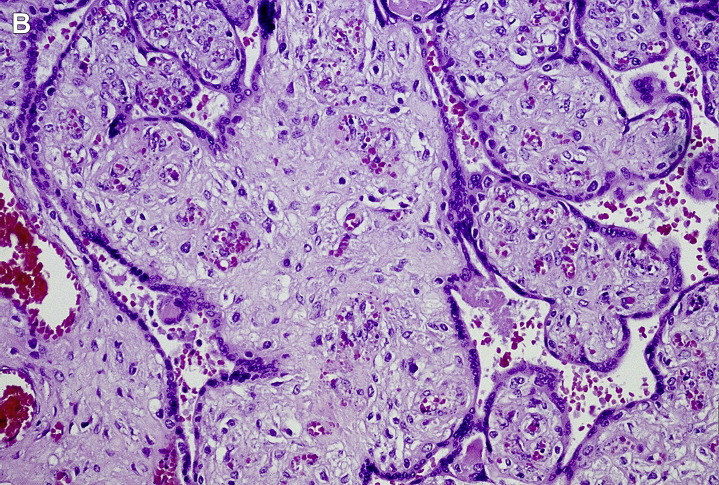
Fig. 9.
(A) Acute villous lesion. This instance of more extensive acute intravillous hemorrhage was traced to an occlusive thrombus in a large vein just before joining the umbilical vein. (B) Acute villous lesion. Fetal villous capillary lesions of recent (2–4 days) duration show disappearance of most endothelial cells, extravasation, and fragmentation of red blood cells, in a region of stasis downstream from a recent stem vessel thrombus (hematoxylin-eosin, original magnification ×300).
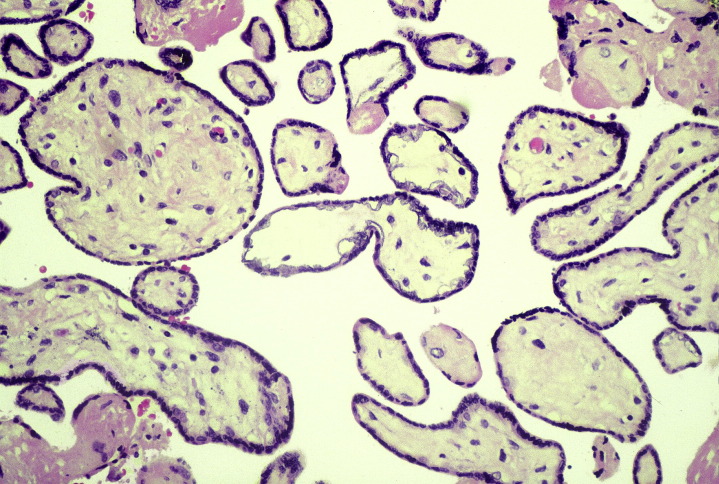
Fig. 10.
Old, chronic avascular hyalinized villi show mineralization in the basal lamina beneath the trophoblastic layer, visible in this hematoxylin-eosin–stained section. Such hyalinized villous lesions were extensive in multiple sections of this placenta (hematoxylin-eosin, original magnification ×200). This is the same same placenta as shown grossly in Fig. 3.
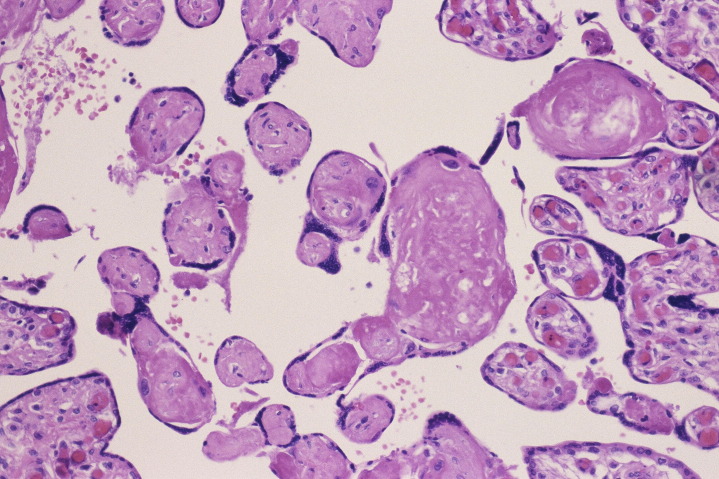
Fig. 11.
These villi, from the same placenta as shown in Figs. 4, 5, and 7, show chronic villous changes of FTV at the margin of a much larger lesion. The villi clustered at left are avascular and hyalinzed, in contrast to some adjacent normally perfused villi at right. The fetus associated with this placenta experienced intrauterine death just 36 hours before delivery. There were both old and recent thrombi in the fetal vessels, and multiple clusters of hyalinized avascular villi were present in this placenta. The intravascular clotting injury in this placenta began many days, possibly even weeks, before the fetal death. No symptoms were detected during the course of this carefully monitored pregnancy (hematoxylin-eosin, original magnification ×200).
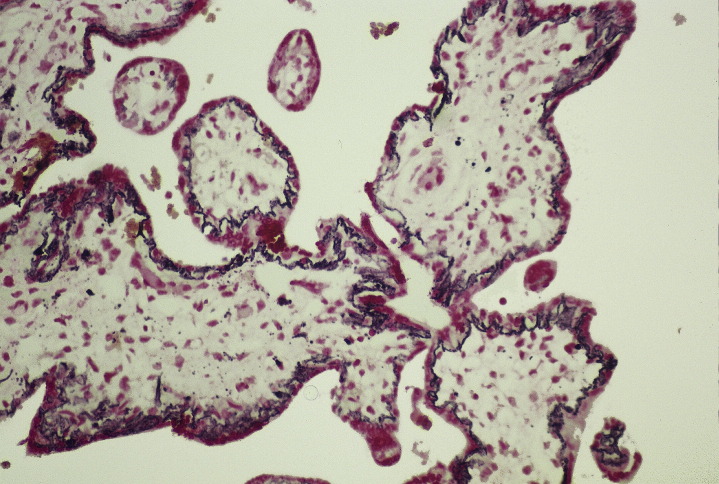
Fig. 12.
Avascular hyalinized villi after Prussian blue stain for iron show dark blue linear deposits in the basement membranes beneath the trophoblast layer (Prussian blue, original magnification ×200).
Box 3 summarizes the microscopic morphology of FTV.
Box 3. Microscopic morphology of fetal thrombotic vasculopathy.
Stem vessels, chorionic plate vessels
Recent thrombi are adherent to the vessel wall, the endothelium is gone, and there is focal or extensive red cell extravasation.
Older, chronic thrombi have a fibroblastic infiltrate into the thrombus, with marked red blood cell extravasation and fragmentation; areas of fibrovascular sclerosis and endothelial cushions are often calcified.
Distal chorionic villi
In recent lesions, variably sized clusters of villi have stromal-endothelial karyorrhexis and red blood cell extravasation. The intervillous space is normal and the syncytiotrophoblastic epithelium survives.
In chronic lesions, the clusters of villi are now avascular with hyalinized stroma, but the trophoblastic cover still persists. The basal lamina beneath the trophoblast becomes mineralized (iron stain positive).
Differential diagnosis
Intrauterine Fetal Death
The histologic changes in vascular morphology after intrauterine fetal death, like the vascular changes in FTV, result from cessation of blood flow through the fetal vessels, except that the changes are diffuse throughout the entire placenta. The vascular changes are all approximately the same age, however, which depends on the length of time between fetal death and delivery. In contrast, the clusters of avascular villi of FTV form well-circumscribed clusters, surrounded by normally perfused villi. The endothelial cells fragment and the blood in larger stem vessels after fetal death is soon invaded by spindle-shaped fibroblasts, but the layered strata of leukocytes, fibrin, and red cells characteristic of thrombi in flowing blood does not occur. Red cells extravasate into the adjacent stroma. It takes approximately 2 days for the early changes of FTV to appear in villi,22 so older, avascular hyalinzed villi or other well-established FTV changes identified within a 48-hour interval between fetal death and delivery (see Fig. 12) are truly pathologic FTV lesions, even though the stillborn (see Fig. 12 description) died 36 hours before delivery.23
Chronic Villitis with Obliterative Fetal Vasculopathy
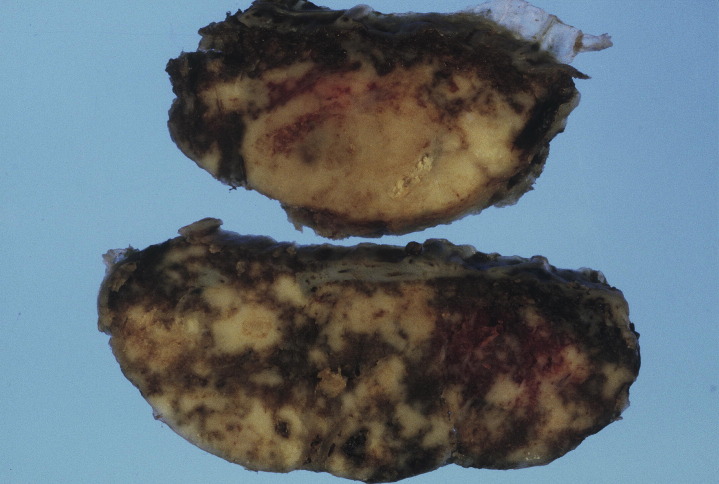
The larger affected areas are grossly indurated, with a gray-tan color and irregular blotchy outlines (Fig. 13 ). Stem villi involved by foci of chronic villitis may be infiltrated by the inflammatory process, and blood vessels may become thrombosed due to local endothelial injury (Fig. 14 ). The thrombi are generally limited to inflamed stem villi, but downstream avascular villi are not necessarily always involved in the inflammatory process. The inflamed villous stroma is infiltrated by predominately CD8-positive maternal T-lymphocytes and macrophages (predominately activated Hofbauer-type fetal macrophages).24 Groups of villli may become agglutinated by fibrin on the villous surfaces. Clusters of downstream terminal villi are avascular and hyalinized, as seen with FTV. Unlike with FTV, there is no evidence of cord occlusion.
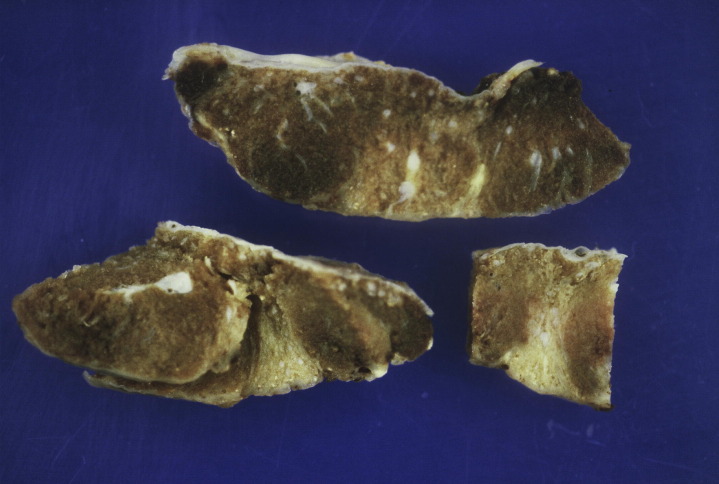
Fig. 13.
These are cross-sections of a placenta with extensive localized areas of chronic villitis. The affected areas are firm, pale, and generally well circumscribed, with functional placental villi in-between.
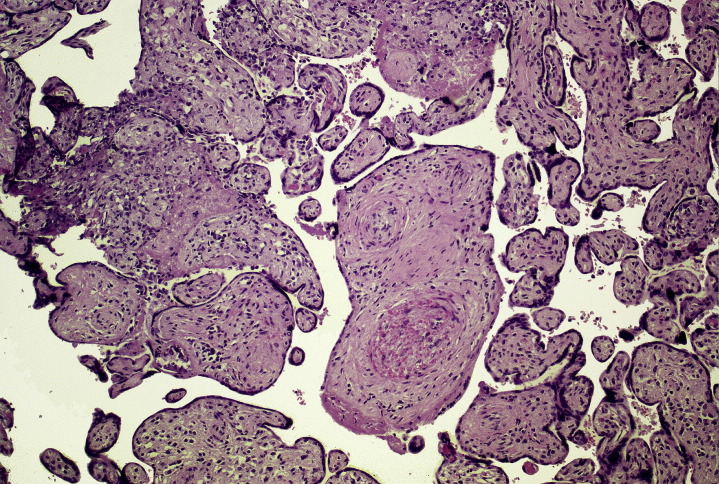
Fig. 14.
Chronic villitis causing agglutination of villi at left. The occlusive stem vessel thrombus just below center resulted in downstream ischemia of clusters of avascular villi at right (hematoxylin-eosin, original magnification ×100).
Mesenchymal Dysplasia
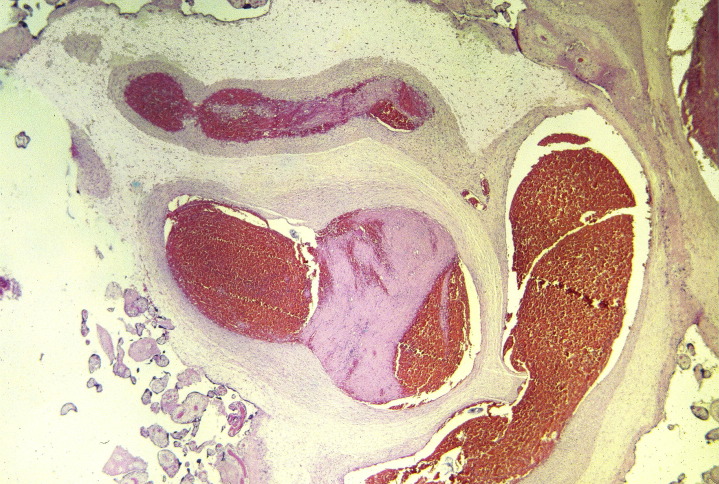
The placenta is usually enlarged; chorionic plate vessels are conspicuously, even aneurysmally, dilated, tortuous, and often contain large mural thrombi (Fig. 15 ). Many large, vesicular, swollen, edematous villi have an appearance suggestive of molar villi (Fig. 16 ). Placental ultrasound images are often interpreted as partial or complete hydatidiform mole. There is an increased amount of edematous mesenchymal villous stroma. Trophoblastic hyperplasia, a feature of partial or complete moles, is not present.25 The fetus, typically female, may appear normal, but is often growth restricted, and some fetuses are stillborn, depending on the amount of functioning placenta available to the fetus. There is an association with Beckwith-Wiedemann syndrome in approximately one-third of cases.
Fig. 15.
Mesenchymal dysplasia. Dilated, aneurysmal stem vessels are partially occluded by thrombi and surrounded by excessive amounts of edematous mesenchyme (hematoxylin-eosin, original magnification ×15).
Fig. 16.
Mesenchymal dysplasia. Many enlarged subchorionic villi contain abundant pale gray connective tissue; some have dilated stem vessels. A prominent component of more normal villous parenchyma at left contrasts with the markedly dysmorphic component at the right.
(Courtesy of Deborah J. Gersell, MD, St. John’s Mercy Medical Center, St Louis, MO; with permission.)
Infarct
The intervillous space in FTV remains open and perfused by maternal blood, whereas the intervillous space of an infarct is collapsed as the villi become adherent, separated only by thin strands of fibrin. The syncytiotrophoblast cover of infarcted villi undergoes necrosis and disappears, whereas the trophoblast surface of villi in FTV remains viable. In time, all of the cellular components of an infarct undergo necrosis and nuclear staining disappears throughout.
Table 1 presents a summary of differential diagnoses.
Table 1.
Differential diagnosis of fetal thrombotic vasculopathy
| FTV Versus | Helpful Distinguishing Features |
|---|---|
| Intrauterine fetal death |
|
| Chronic villitis |
|
| Mesenchymal dysplasia |
|
Impact on outcome
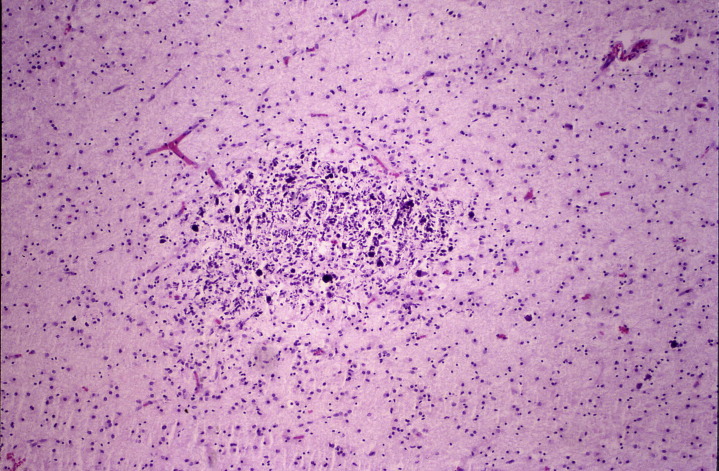
Placentas affected by FTV result in a 9-fold increase in prevalence of stillbirth, a 6-fold increase in cardiac abnormalities, and a 2-fold increase in growth restriction,6 in comparison with normal placentas. The odds ratio for preterm birth is also increased.6 Some newborns with FTV may have clinical or autopsy evidence of thrombotic lesions elsewhere in the fetal circulation. Infarcts in the brain, which may occur before birth (Fig. 17 ), have been demonstrated in perinatal autopsies.2, 26 In a study of 186 neonatal stroke patients in the Canadian Pediatric Ischemic Stroke Registry, only 12 had placental pathologic examinations, but of these 12, 6 had thrombi in cord, chorionic plate vessels, or other features of FTV.27 FTV is also an important cause of hypoxic-ischemic encephalopathy, especially when associated with obstructive umbilical cord problems.28 An autopsy study of stillbirths that correlated neuropathology with placental pathology found that FTV correlated with neuronal injury (nuclear karyorrhexis) in the brain.29
Fig. 17.
This cerebral infarct has chronic histologic features, associated with thrombi in the fetal circulation in the placenta, possibly the result of embolism to the middle cerebral artery. The central necrosis, focal calcification, and marked astrocytic proliferation indicate at least several days' duration. The newborn had bradycardia during labor and severe neonatal encephalopathy but lived only 2.5 hours after birth; the placenta showed extensive chronic FTV with many clusters of avascular hyalinized villi. Both the FTV and the cerebral infarct occurred prenatally, long before the delivery (hematoxylin-eosin, original magnification ×100).
Instances of gangrene of an arm or leg associated with FTV are rare,30 but dramatic, when they occur.31 Some cases of bowel atresia have also occurred in this context, as a feature of vascular disruption (Fig. 18 ).8 Placental vein thrombi appeared to have had some significance in the development of a case of twin reversed arterial perfusion sequence reported by Steffensen and colleagues.32 In a similar context, sudden, rapid onset of twin-twin transfusion syndrome occurred as the result of a thrombus forming in one of the balancing AV anastomoses in a monochorionic twin placenta.33
Fig. 18.
Esophageal atresia associated with extensive placental FTV. Very recent fetal death in utero occurred at 32 weeks. The largest fetal vessels at the chorionic plate appeared dilated and congested. The cord had a single umbilical artery and was tightly wrapped multiple times about the left leg of the fetus, resulting in compression marks on the leg. There were several large stem vessel thrombi; both old hyalinized villi and more recent hemorrhagic villi with extravasated red blood cells were present. Instances of atresia in the digestive tract have been attributed to vascular disruptions, most likely caused by thrombi. Unfortunately, attempts to relate bowel atresia to placental pathology are not commonly made.
Both fetal somatic thrombi and placental thrombi (FTV) give no specific sign or symptom of their presence until fetal death occurs or growth restriction becomes apparent. There may be reduction of amniotic fluid, but this is nonspecific, and growth restriction has many causes. FTV was one of the main placental lesions (27% of cases of severe intrauterine growth restriction) causing reduced or reversed end diastolic blood flow, as demonstrated by umbilical cord blood flow Doppler velocimetry.5
FTV may increase progressively as the process of intravascular thrombosis extends within the placenta. Thus, FTV tends to reduce placental function progressively without causing perceptible injury until the cumulative effects of reduced placental reserve and the stress of labor onset combine to cause heart rate abnormalities, such as bradycardia, fetal distress, and even late perinatal stillbirth. It should be emphasized that FTV, as well as other pathologic processes that affect the placenta, commonly begin long before delivery, but produce no symptoms, and, finally, as injury progresses, may produce nonspecific stress related alterations, such as bradycardia, occur at onset of labor. Often it is at this stressful time, hours before delivery, that the reduced placental function finally causes acute injury to the brain, kidneys, and other organs of the fetus, even though it is the older placental pathologic lesions that initiated the chain of events that culminated in the serious injuries that the newborn must face after delivery.
Growth restriction is common when involvement is more extensive. When the placenta is also small for gestational age, the cumulative effects of reduced size and more extensive lesions may enhance the destructive effects of reduced placental function on the organs of the fetus.
Long-term follow-up of newborns with FTV that was not associated with either reduced placental function, in the absence of symptomatic clots in the somatic circulation is not available.
Umbilical cord thrombi
Cord thrombi may be evident grossly as localized areas of fusiform enlargement or discoloration. Old thrombi may calcify. They may be associated with knots, torsion, amniotic bands, varices, infection, compression, or velamentous insertion. The umbilical vein is most commonly affected.
Thrombi in umbilical cord vessels may be partly or completely occlusive. There is a strong association with fetal morbidity, including growth restriction, and two-thirds are stillborn. Heifetz34 found an incidence of 1:1000 perinatal autopsies, increasing to 1:250 in high-risk pregnancies. In an autopsy series of 317 consecutive stillbirths at 15 to 40 weeks gestation, Avigliano and colleagues35 found 32 cases with thrombi in cord vessels, an incidence of 1:10. The larger incidence in this report may be related to an acceptance of fibrin identified only in phosphotungstic acid-hemotoxylin stains of cord as evidence of clots, even if lacking adherence and changes at the clot-endothelial interface in some cases; others in this study did show loss of endothelium and extravasation of red cells at the inner vessel margin. The umbilical vein was most often involved. Cord abnormalities (eg, knots and hypercoiling) were present in 13 cases. Cord thrombi and FTV do occur together, but not invariably, in this series, as well as in my experience.
References
- 1.Pathak S., Lees C.C., Hackett G. Frequency and clinical significance of placental histological lesions in an unselected population at or near term. Virchows Arch. 2011;459:565–572. doi: 10.1007/s00428-011-1157-z. [DOI] [PubMed] [Google Scholar]
- 2.Kraus F.T., Acheen V.I. Fetal thrombotic vasculopathy in the placenta: cerebral thrombi and infarcts, coagulopathies, and cerebral palsy. Hum Pathol. 1999;30:759–769. doi: 10.1016/s0046-8177(99)90136-3. [DOI] [PubMed] [Google Scholar]
- 3.McDonald D.G., Kelehan P., McMenamin J.B. Placental fetal thrombotic vasculopathy is associated with neonatal encephalopathy. Hum Pathol. 2004;35:875–880. doi: 10.1016/j.humpath.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Redline R.W. Severe fetal placental vascular lesions in term infants with neurologic impairment. Am J Obstet Gynecol. 2005;192:452–457. doi: 10.1016/j.ajog.2004.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Dicke J.M., Huettner P., Yan S. Umbilical artery Doppler indices in small for gestational age fetuses. Correlation with adverse outcomes and placental abnormalities. J Ultrasound Med. 2009;28:1603–1610. doi: 10.7863/jum.2009.28.12.1603. [DOI] [PubMed] [Google Scholar]
- 6.Saleemuddin A., Tantbirojn P., Sirois K. Obstetric and perinatal complications in placentas with fetal thrombotic vasculopathy. Pediatr Dev Pathol. 2010;13:459–464. doi: 10.2350/10-01-0774-OA.1. [DOI] [PubMed] [Google Scholar]
- 7.Takenouchi T., Kasdorf E., Engel M. Changing pattern of perinatal brain injury in term infants in recent years. Pediatr Neurol. 2012;46:106–110. doi: 10.1016/j.pediatrneurol.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Gilbert-Barness E., Van Allen M.I. Vascular disruptions. In: Gilbert-Barness E., editor. Potter's pathology of the fetus and infant. 2nd edition. Mosby; St Louis (MO): 2007. pp. 176–200. [Google Scholar]
- 9.Redline R.W. Clinical and pathological umbilical cord abnormalities in fetal thrombotic vasculopathy. Hum Pathol. 2004;35:1494–1498. doi: 10.1016/j.humpath.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Tantbirojn P., Saleemuddin A., Sirois K. Gross abnormalities of the umbilical cord: related placental histology and clinical significance. Placenta. 2009;30:1083–1088. doi: 10.1016/j.placenta.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Ng W.F., Wong S.F., Lam A. The placentas of patients with severe acute respiratory syndrome: a pathophysiological evaluation. Pathology. 2006;38:210–218. doi: 10.1080/00313020600696280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arias F., Romero R., Joist H. Thrombophilia: a mechanism of disease in women with adverse pregnancy outcome and thrombotic lesions in the placenta. J Matern Fetal Med. 1998;7:277–286. doi: 10.1002/(SICI)1520-6661(199811/12)7:6<277::AID-MFM5>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 13.Khong T.Y., Hague W.M. Biparental contribution to fetal thrombophilia in discordant twin intrauterine growth restriction. Am J Obstet Gynecol. 2001;185:244–245. doi: 10.1067/mob.2001.113320. [DOI] [PubMed] [Google Scholar]
- 14.Redline R.W., Pappin A. Fetal thrombotic vasculopathy: the clinical significance of extensive avascular villi. Hum Pathol. 1995;26:80–85. doi: 10.1016/0046-8177(95)90118-3. [DOI] [PubMed] [Google Scholar]
- 15.Vern T.Z., Alles A.J., Kowal-Vern A. Frequency of Factor V Leiden and Prothrombin G20210A in placentas and their relationship with placental lesions. Hum Pathol. 2000;31:1036–1043. doi: 10.1053/hupa.2000.16281. [DOI] [PubMed] [Google Scholar]
- 16.Ariel I.B., Anteby E., Hamani Y. Placental pathology in fetal thrombophilia. Hum Pathol. 2004;35:729–733. doi: 10.1016/j.humpath.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Leistra-Leistra M.J., Timmer A., van Spronsen F.J. Fetal thrombotic vasculopathy in the placenta: a thrombophilic connection between pregnancy complications and neonatal thrombosis? Placenta. 2004;25(Suppl A):S102–S105. doi: 10.1016/j.placenta.2004.01.010. Trophoblast Research. [DOI] [PubMed] [Google Scholar]
- 18.Mousa H.A., Alfirevic Z. Do placental lesions reflect thrombophilic state in women with adverse pregnancy outcome? Hum Reprod. 2000;15:1830–1833. doi: 10.1093/humrep/15.8.1830. [DOI] [PubMed] [Google Scholar]
- 19.Parast M.M., Crum C.P., Boyd T.K. Placental histological criteria for umbilical flow restriction in unexplained stillbirth. Hum Pathol. 2008;39:948–953. doi: 10.1016/j.humpath.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 20.Scott J.M. Fibrinous vasculosis in the human placenta. Placenta. 1983;4:87–100. doi: 10.1016/s0143-4004(83)80020-4. [DOI] [PubMed] [Google Scholar]
- 21.De Sa D.J. Intimal cushions of foetal placental veins. J Pathol. 1973;110:347–352. [Google Scholar]
- 22.Genest D.R. Estimating the time of death in stillborn fetuses: II. Histologic evaluation of the placenta; a study of 71 stillborns. Obstet Gynecol. 1992;80:585–592. [PubMed] [Google Scholar]
- 23.Redline R.W. Villitis of unknown etiology: noninfectious chronic villitis in the placenta. Hum Pathol. 2007;38:1439–1446. doi: 10.1016/j.humpath.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 24.Parveen Z., Tongson-Ignacio J.E., Fraser C.R. Placental mesenchymal dysplasia. Arch Pathol Lab Med. 2007;131:131–137. doi: 10.5858/2007-131-131-PMD. [DOI] [PubMed] [Google Scholar]
- 25.Kaiser-Rogers K.A., McFadden D.E., Livasy C.A. Androgenetic/biparental mosaicism causes placental mesenchymaql dysplasia. J Med Genet. 2006;43:187–192. doi: 10.1136/jmg.2005.033571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thorarensen O., Ryan S., Hunter J. Factor V Leiden 19 mutations: an unrecognized cause of hemiplegic cerebral palsy, neonatal stroke, and placental thrombosis. Ann Neurol. 1997;42:372–375. doi: 10.1002/ana.410420316. [DOI] [PubMed] [Google Scholar]
- 27.Elbers J., Viero S., MacGregor D. Placental pathology in neonatal stroke. Pediatrics. 2011;127:e722–e729. doi: 10.1542/peds.2010-1490. [DOI] [PubMed] [Google Scholar]
- 28.Wintermark P., Boyd T.K., Gregas M.C. Placental pathology in asphyxiated newborns meeting the criteria for therapeutic hypothermia. Am J Obstet Gynecol. 2010;203(6):579.e1–579.e9. doi: 10.1016/j.ajog.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 29.Chang K.T., Keating S., Costa S. Third trimester stillbirths: corrlative neuropathology and placental pathology. Pediatr Dev Pathol. 2011;14:345–352. doi: 10.2350/10-07-0882-OA.1. [DOI] [PubMed] [Google Scholar]
- 30.Hoyme H.E., Jones K.L., Van Allen M.I. Vascular pathogenesis of transverse limb reduction defects. J Pediatr. 1982;101:839–843. doi: 10.1016/s0022-3476(82)80343-0. [DOI] [PubMed] [Google Scholar]
- 31.Kraus F.T., Redline R.W., Gersell D.J. American Registry of Pathology; Washington, DC: 2004. Placental Pathology. [Google Scholar]
- 32.Steffensen T.S., Gilbert-Barness E., Spellacy W. Placental pathology in trap sequence: clinical and pathogenetic implications. Fetal Pediatr Pathol. 2008;27:13–29. doi: 10.1080/15513810801893389. [DOI] [PubMed] [Google Scholar]
- 33.Nikkels P.G., Van Gemert M.J., Sollie-Szarynska K.M. Rapid onset of severe twin-twin transfusion syndrome caused by placental venous thrombosis. Pediatr Dev Pathol. 2002;5:310–314. doi: 10.1007/s10024-001-0156-5. [DOI] [PubMed] [Google Scholar]
- 34.Heifetz S.A. Thrombosis of the umbilical cord; analysis of 52 cases and literature review. Pediatr Pathol. 1988;8:37–54. doi: 10.3109/15513818809022278. [DOI] [PubMed] [Google Scholar]
- 35.Avagliano L., Marconi A.M., Candiani M. Thrombosis of the umbilical vessels revisited. An observational study of 317 consecutive autopsies at a single institution. Hum Pathol. 2010;41:971–979. doi: 10.1016/j.humpath.2009.07.026. [DOI] [PubMed] [Google Scholar]