Abstract
Background
Clinical and basic investigations have indicated a significant association between circulating growth differentiation factor 15 (GDF15) and cardiovascular disease; however, the relationship between GDF15 and lower extremity atherosclerotic disease (LEAD) has been less studied. The present study aimed to explore the association between GDF15 and LEAD in Chinese patients with type 2 diabetes mellitus (T2DM). Considering that obesity is an important factor associated with circulating GDF15 levels, whether the relationship between serum GDF15 levels and LEAD is affected by body mass index (BMI) was also analysed.
Methods
A total of 376 hospitalized T2DM patients were enrolled (161 with LEAD and 215 without LEAD). A sandwich enzyme-linked immunosorbent assay was used to detect the serum GDF15 levels. The femoral intima-media thickness (F-IMT) and LEAD were assessed by ultrasonography.
Results
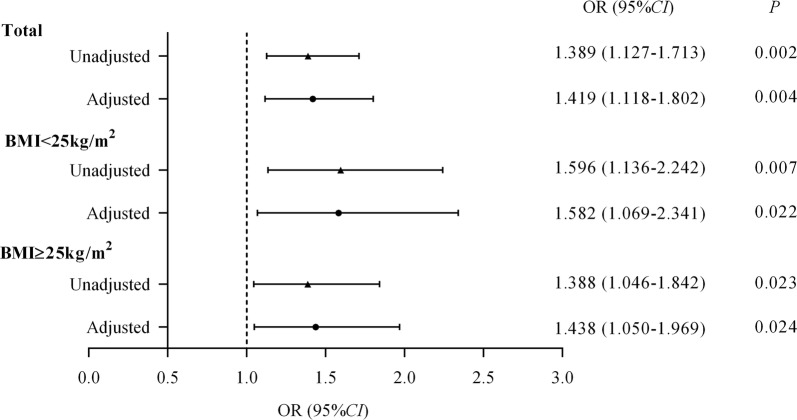
Patients with LEAD had significantly higher serum GDF15 levels than those without LEAD, regardless of whether their BMI was < 25 kg/m2 or ≥ 25 kg/m2 (both P < 0.05). Serum GDF15 levels were independently positively related to the F-IMT (standardized β = 0.162, P = 0.002). After adjusting for confounding factors, per 1-standard deviation (SD) increase in the serum GDF15 levels was significantly related to an approximately 1.4-fold increased risk of LEAD in the total population (P < 0.05). Regardless of whether the BMI was < 25 kg/m2 or ≥ 25 kg/m2, this association remained significant, with approximately 1.6- and 1.4-fold increased risks of LEAD, respectively (both P < 0.05).
Conclusions
High serum GDF15 levels were significantly correlated with an increased risk of LEAD in T2DM patients, and this relationship was independent of BMI.
Keywords: Type 2 diabetes mellitus, Growth differentiation factor 15, Lower extremity atherosclerotic disease, Femoral intima-media thickness, Body mass index
Background
Growth differentiation factor 15 (GDF15), also known as macrophage inhibitory factor-1, is a member of the transforming growth factor-β (TGF-β) cytokine superfamily [1]. Studies have found that GDF15 is a stress-responsive cytokine that is only highly expressed in the placenta [2] and prostate [3] and rarely expressed in myocardial tissues under normal physiological conditions. However, the expression and secretion of GDF15 can be strongly induced in the case of cardiovascular injury, such as pressure overload, myocardial infarction, heart failure, and atherosclerosis [4]. In recent years, a series of clinical studies [5–10] have reported that high circulating GDF15 levels are an independent predictive factor for several cardiovascular diseases in patients with atherosclerosis and acute coronary syndrome, and that investigating the levels of GDF15 could improve risk prediction beyond traditional risk factors and biochemical indicators.
Lower extremity atherosclerotic disease (LEAD) is one of the major vascular complications of diabetes and is associated with a substantial increase in the risk of non-fatal (such as gangrene, amputation, etc.) and fatal cardio- and cerebrovascular events [11, 12]. Furthermore, diabetes was observed to be independently associated with an increased risk of LEAD, depending on the severity of cardiovascular diseases [13]. Nevertheless, most previous related studies have focused on circulating GDF15 levels and myocardial or coronary artery diseases in patients with diabetes [14–16], and the relationship between GDF15 and LEAD has been less explored.
Therefore, in the present study, we hypothesized that serum GDF15 levels were correlated with LEAD as measured by ultrasonography in Chinese patients with type 2 diabetes mellitus (T2DM). Considering that obesity is an important factor associated with circulating GDF15 levels [17–19], we also analysed whether the relationship between serum GDF15 levels and LEAD was affected by body mass index (BMI).
Materials and methods
Study population
A total of 376 patients (259 men, 117 women) with T2DM who were hospitalized in the Department of Endocrinology and Metabolism of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital were retrospectively included in this study during March 2015 and October 2019. The diagnosis of diabetes was based on the 2010 American Diabetes Association standards [20]. The inclusion criteria were patients with age from 20 to 80 years, 18.5 ≤ BMI < 30 kg/m2, and C-reactive protein levels < 10 mg/L. The exclusion criteria were patients who had severe cardiovascular diseases (n = 19), malignant tumours (n = 23), renal dysfunction (serum creatinine ≥ 115 µmol/L or glomerular filtration rate [GFR] < 60 mL/min/1.73 m2) (n = 49), and hepatic dysfunction (acute viral hepatitis, alanine aminotransferase, or aspartate aminotransferase > 1.5-fold the upper limit of normal) (n = 13). We collected the following clinical information from all the participants: diabetes duration, smoking status, alcohol consumption, and medication use. The study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, and all participants provided written informed consent prior to enrolment.
Anthropometric and biochemical assessments
BMI was calculated as weight/height2 (kg/m2). Systolic and diastolic blood pressure (SBP and DBP, respectively) were measured with a mercury sphygmomanometer after the subjects had rested for at least 10 min. Fasting venous blood samples were collected from subjects who had fasted overnight for 10 h, and 2-h venous blood samples were collected approximately 2 h after they ate breakfast. The levels of fasting plasma glucose (FPG), 2-h postprandial plasma glucose (2hPG), glycated haemoglobin A1c (HbA1c), fasting C-peptide (FCP), 2-h C-peptide (2hCP), serum lipid profiles [including total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-c), and low-density lipoprotein cholesterol (LDL-c)], haemoglobin (Hg) and C-reactive protein (CRP) were assessed with standard laboratory methods, as described previously [21]. The methods used to determine the GFR and homeostasis model assessment 2 of insulin resistance (HOMA2-IR) were also consistent with those used in a previous study [21].
Serum GDF15 levels were measured by a sandwich enzyme-linked immunosorbent assay (R & D Systems, Inc. Minneapolis, USA), with intra- and inter-assay coefficients of variation (CV) of 0.46–4.08% and 5.77–9.24%, respectively.
Ultrasonography measurements and diagnosis of LEAD
Colour Doppler ultrasound examinations of the lower limb arteries were conducted using an Acuson Sequoia 512 scanner (Siemens Medical Solutions, Mountain View, CA, USA) equipped with a linear array transducer with frequencies of 5–13 MHz. The atherosclerotic plaque measurement range included the femoral artery, deep femoral artery, popliteal artery, superficial femoral artery, anterior tibial artery, posterior tibial artery and peroneal artery in each lower limb. According to the Mannheim Consensus [22], intima-media thickness (IMT) was assessed as the distance between the leading edge of the lumen-intima interface and the leading edge of the media-adventitia interface. An atherosclerotic plaque was defined as a focal structure encroaching into the arterial lumen at least 0.5 mm, 50% of the surrounding IMT value, or an IMT thickness ≥ 1.5 mm [22]. The mean value of the IMTs of the bilateral femoral arteries was defined as the femoral intima-media thickness (F-IMT). And the presence of atherosclerotic plaques in any of the lower limb artery segments listed above was defined as LEAD [23].
Statistical analysis
SPSS version 22.0 was used for the statistical analysis. Data distributions were tested for normality. Variables with a normal distribution and F-IMT data are presented as the mean ± standard deviation (SD), while skewed data and categorical variables are expressed as the median (interquartile range: 25 to 75%) and percentages (%), respectively. An unpaired Student’s t test and Wilcoxon rank sum test were used to compare differences in normally distributed and skewed data, respectively. The Chi-square test was used for intergroup comparisons of categorical variables. Subgroup analysis was performed in populations with a BMI < 25 kg/m2 and a BMI ≥ 25 kg/m2, based on the 1998 World Health Organization criteria [24]. Multiple stepwise regression analysis was conducted to explore the factors influencing serum GDF15 levels. The values of serum GDF15 were standardized, and the relationship between the per 1-SD change in serum GDF15 levels and LEAD was analysed by logistic regression analysis. The level of statistical significance was set at a two-tailed P value less than 0.05.
Results
Clinical characteristics of the study participants
A total of 376 T2DM patients with a median age of 48 (38–58) years, including 259 men and 117 women, were included in this study. The study population was divided into four subgroups based on BMI 25 kg/m2 and the presence of LEAD. The clinical characteristics of the subjects are summarized in Table 1. Whether patients had a BMI < 25 kg/m2 or ≥ 25 kg/m2, subjects with LEAD exhibited older age, higher levels of F-IMT, longer diabetes duration, and a higher usage of lipid-lowering therapy but a lower GFR than those without LEAD (all P < 0.05, Table 1).
Table 1.
Characteristics of the study participants
| Variable | BMI < 25 kg/m2 | BMI ≥ 25 kg/m2 | ||
|---|---|---|---|---|
| With LEAD (n = 89) |
Without LEAD (n = 95) |
With LEAD (n = 72) |
Without LEAD (n = 120) |
|
| n (men/women) | 58/31 | 59/36 | 55/17 | 87/33 |
| Age (years) | 59 (53–65)** | 42 (35–51) | 58 (50–63)** | 40 (33–46) |
| BMI (kg/m2) | 23.51 (22.50–24.22)** | 22.60 (21.23–23.88) | 26.88 (25.74–28.25) | 27.34 (26.21–28.27) |
| SBP (mmHg) | 120 (115–131) | 120 (112–130) | 128 (120–140) | 126 (120–138) |
| DBP (mmHg) | 77 (70–82) | 80 (70–85) | 80 (76–90) | 80 (76–90) |
| TC (mmol/L) | 4.87 ± 1.28 | 4.73 ± 1.04 | 4.80 ± 1.18 | 4.95 ± 1.11 |
| TG (mmol/L) | 1.28 (0.97–1.98) | 1.21 (0.78–1.97) | 1.90 (1.23–2.64) | 2.00 (1.38–2.74) |
| HDL-c (mmol/L) | 1.12 (0.87–1.33) | 1.08 (0.94–1.30) | 0.93 (0.84–1.10) | 0.96 (0.81–1.11) |
| LDL-c (mmol/L) | 2.99 ± 1.14 | 2.92 ± 0.81 | 3.00 ± 0.95 | 3.03 ± 0.94 |
| CRP (mg/L) | 0.84 (0.45–1.74) | 0.65 (0.30–1.42) | 1.07 (0.50–1.88) | 1.25 (0.69–2.21) |
| FPG (mmol/L) | 7.69 (6.62–10.22) | 7.50 (6.19–8.95) | 9.11 (6.94–10.64) | 7.95 (6.89–10.03) |
| 2hPG (mmol/L) | 12.74 (10.38–15.14) | 12.38 (9.21–15.23) | 13.67 (9.72–16.81) | 13.31 (10.85–15.91) |
| HbA1c (%) | 10.0 (8.1–11.2) | 9.3 (7.2–10.8) | 9.8 (8.2–10.8) | 9.5 (7.7–11.3) |
| FCP (ng/mL) | 1.35 (1.03–1.94) | 1.50 (0.82–2.04) | 1.78 (1.31–2.26) | 1.84 (1.29–2.64) |
| 2hCP (ng/mL) | 2.64 (1.74–3.78) | 2.90 (1.70–4.57) | 3.33 (2.39–4.48) | 3.83 (2.32–6.50) |
| HOMA2-IR | 1.18 (0.83–1.66) | 1.29 (0.70–1.75) | 1.53 (1.17–2.10) | 1.60 (1.15–2.24) |
| Hg (g/L) | 142 (132–150)* | 145 (137–154) | 148 (135–154) | 148 (139–155) |
| GFR (mL/min/1.73 m2) | 94.80 (83.00–110.70)** | 104.50 (92.70–121.56) | 93.79 (79.95–108.58)** | 107.66 (89.18–124.33) |
| Diabetes duration (years) | 10.00 (6.00–14.00)** | 6.00 (2.00–10.00) | 10.50 (5.00–14.00)** | 4.00 (0.33–9.00) |
| F-IMT (mm) | 0.85 ± 0.00** | 0.60 ± 0.03 | 0.85 ± 0.01** | 0.60 ± 0.03 |
| Current smoking, n (%) | 35 (39.33) | 25 (26.32) | 24 (33.33) | 41 (34.17) |
| Current alcohol consumption, n (%) | 14 (15.73) | 20 (21.05) | 14 (19.44) | 30 (25.00) |
| Anti-hypertensive therapy, n (%) | 39 (43.82)** | 18 (18.95) | 31 (43.06) | 39 (32.50) |
| Lipid-lowering therapy, n (%) | 71 (79.78)** | 46 (48.42) | 59 (81.94)** | 73 (60.83) |
Data are expressed as mean ± standard deviation, median (interquartile range: 25 to 75%), or n (%)
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, TC total cholesterol, TG triglyceride, HDL-c high-density lipoprotein cholesterol, LDL-c low-density lipoprotein cholesterol, CRP C-reactive protein, FPG fasting plasma glucose, 2hPG 2-h plasma glucose, HbA1c glycated haemoglobin A1c, FCP fasting C-peptide, 2hCP 2-h C-peptide, HOMA2-IR homeostasis model assessment 2 of insulin resistance, Hg haemoglobin, GFR glomerular filtration rate, F-IMT femoral intima-media thickness
* P < 0.05 versus without LEAD
** P < 0.01 versus without LEAD
The median (25th, 75th percentile) serum GDF15 levels among the entire study population was 796.78 (546.46–1224.60) pg/mL. No significant difference was found between men and women [792.11 (566.44–1254.75) pg/mL versus 814.98 (524.73–1196.70) pg/mL, P = 0.532]. Those with LEAD had significantly higher levels of GDF15 than those without LEAD [910.29 (604.11–1379.41) pg/mL versus 718.43 (528.75–1108.79) pg/mL, P = 0.002].
Comparison of serum GDF15 levels between patients with a BMI < 25 kg/m2 and those with a BMI ≥ 25 kg/m2
Compared with patients with a BMI < 25 kg/m2, patients with a BMI ≥ 25 kg/m2 exhibited much higher serum GDF15 levels [863.87 (587.51–1363.77) pg/mL versus 691.78 (521.30–1093.18) pg/mL, P = 0.001]. Regardless of LEAD status, subjects with a BMI ≥ 25 kg/m2 had significantly higher levels of GDF15 than subjects with a BMI < 25 kg/m2 (both P < 0.05, Fig. 1). Additionally, the serum GDF15 levels were observed to be significantly higher in patients with LEAD than in those without LEAD, regardless of whether their BMI was < 25 kg/m2 or ≥ 25 kg/m2 (both P < 0.05, Fig. 1).
Fig. 1.

Comparison of serum GDF15 levels. Data are shown as the median with 2.5th and 97.5th percentiles
Correlations of serum GDF15 levels with F-IMT and other metabolic parameters
Spearman’s correlation analysis showed that the serum GDF15 levels were positively associated with F-IMT (r = 0.164, P = 0.001). In addition, the serum GDF15 levels were also positively correlated with age (r = 0.205, P < 0.001), BMI (r = 0.179, P < 0.001), FCP (r = 0.110, P = 0.033), HOMA2-IR (r = 0.103, P = 0.046), TG (r = 0.130, P = 0.012), and diabetes duration (r = 0.257, P < 0.001), but negatively correlated with TC (r = − 0.214, P < 0.001), LDL-c (r = − 0.206, P < 0.001), and HDL-c (r = − 0.142, P = 0.006).
Multivariate stepwise regression analysis defined the serum GDF15 levels as the dependent variable, and gender, BMI, SBP, DBP, HbA1c, HOMA2-IR, Hg, TC, TG, HDL-c, LDL-c, CRP, GFR, F-IMT, current smoking status, and current alcohol consumption status were designated as the independent variables. The results showed that F-IMT (standardized β = 0.162, P = 0.002) and BMI (standardized β = 0.193, P < 0.001) were independently and positively associated with serum GDF15 levels. In addition, LDL-c (standardized β = − 0.263, P < 0.001) was negatively associated with the serum GDF15 levels (Table 2).
Table 2.
Multivariate regression analyse of factors associated with serum GDF15 levels
| Variable | Standardized β | t | P |
|---|---|---|---|
| LDL-c | − 0.263 | − 5.187 | < 0.001 |
| BMI | 0.193 | 3.804 | < 0.001 |
| F-IMT | 0.162 | 3.196 | 0.002 |
Independent variables originally included: gender, BMI, SBP, DBP, HbA1c, HOMA2-IR, Hg, TC, TG, HDL-c, LDL-c, CRP, GFR, F-IMT, current smoking, current alcohol consumption
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HbA1c glycated hemoglobin A1c, HOMA2-IR homeostasis model assessment 2 of insulin resistance, Hg hemoglobin, TC total cholesterol, TG triglyceride, HDL-c high-density lipoprotein cholesterol, LDL-c low-density lipoprotein cholesterol, CRP C-reactive protein, GFR glomerular filtration rate, F-IMT femoral intima-media thickness, GDF15 serum growth differentiation factor 15
Relationships between serum levels of GDF15 (per 1-SD increase) and LEAD
Defining LEAD as the dependent variable, the present study constructed three logistic regression models to further determine the relationship between serum GDF15 levels and LEAD in the total population, patients with a BMI < 25 kg/m2, and patients with a BMI ≥ 25 kg/m2. It was observed that per 1-SD increase in serum GDF15 levels was associated with an increased risk of LEAD in all three groups, with OR values of 1.389 (95% CI 1.127–1.713, P = 0.002), 1.596 (95% CI 1.136–2.242, P = 0.007), and 1.388 (95% CI 1.046–1.842, P = 0.023) in the total population, patients with a BMI < 25 kg/m2, and patients with a BMI ≥ 25 kg/m2, respectively. After multivariable adjustment (including gender, SBP, DBP, HbA1c, CRP, TC, TG, HDL-c, LDL-c, HOMA2-IR, GFR, current smoking status, current alcohol consumption status, anti-hypertensive therapy, and lipid-lowering therapy), per 1-SD increase in serum GDF15 levels remained significantly related to LEAD, with 1.419 (1.118–1.802)-fold increased odds in the total population, and 1.582 (1.069–2.341)- and 1.438 (1.050–1.969)-fold increased odds in patients with a BMI < 25 kg/m2 and patients with a BMI ≥ 25 kg/m2, respectively (all P < 0.05, Fig. 2).
Fig. 2.
Relationships between serum levels of GDF15 (per 1-SD increase) and LEAD in the total population, patients with a BMI < 25 kg/m2, and patients with a BMI ≥ 25 kg/m2. Independent variables in the adjusted models included: gender, SBP, DBP, HbA1c, CRP, TC, TG, HDL-c, LDL-c, HOMA2-IR, GFR, GDF15, current smoking status, current alcohol consumption status, anti-hypertensive therapy, and lipid-lowering therapy
In addition, the logistic regression models also showed that in all three groups, the GFR was independently negatively and lipid-lowering therapy was independently positively associated with LEAD (all P < 0.05).
Discussion
The present study was the first to explore the relationship between serum GDF15 levels and LEAD in Chinese patients with T2DM. The results showed that patients with LEAD exhibited much higher serum GDF15 levels than those without LEAD, regardless of whether they had a BMI < 25 kg/m2 or ≥ 25 kg/m2. The F-IMT was identified as an independent factor positively associated with serum GDF15 levels. High serum GDF15 levels were significantly correlated with an increased risk of LEAD, and this relationship was independent of BMI.
LEAD is the manifestation of peripheral atherosclerotic disease and is characterized as the stenosis and occlusion of lower limb arteries [25]. Due to the similar pathophysiological mechanisms (such as oxidative stress and endothelial dysfunction) between LEAD and atherosclerosis in other vasculature, LEAD is closely related to the occurrence of cardiovascular disease [11, 12, 26]. In addition, diabetes-associated LEAD is often concomitant with neuropathy [27]. The decrease in the sense of pain and temperature caused by diabetic neuropathy may conceal the symptoms of LEAD (e.g., resting pain), leading to a delayed diagnosis of LEAD and more serious outcomes such as amputations [28, 29]. Considering the heavy public health and economic burden and the worse prognosis caused by diabetes-related amputations [30], early detection or exploration of an effective biomarker for LEAD is needed.
The results from previous studies have shown that increased circulating GDF15 levels were closely associated with the development and progression of various cardiovascular diseases (including myocardial ischaemia/reperfusion, heart failure, atherosclerosis, and acute coronary syndrome), and were shown to be a strong and independent predictor of mortality and disease progression in patients with atherosclerosis and coronary artery disease [5–10, 31–36]. In diabetic patients, higher levels of lipids and chronic inflammation may directly damage the cardiovascular system [37]. As expected, circulating GDF15 levels have also been shown to help identify and predict cardiovascular disease risk in patients with diabetes [16, 38, 39]. In a study with newly diagnosed T2DM patients, Shin et al. [16] used the Framingham risk score and the New Pooled Cohort Equation score to estimate the 10-year risk of atherosclerotic cardiovascular disease. After adjusting for traditional risk factors, GDF15 was significantly positively correlated with both the Framingham risk score and the New Pooled Cohort Equation score, indicating that the levels of GDF15 may be a useful predictive biomarker of cardiovascular risk in newly diagnosed T2DM patients. Another study conducted by Dominguez-Rodriguez et al. demonstrated that elevated GDF15 levels could be valuable as a unique independent predictor of diabetic cardiomyopathy. Additionally, the results from receiver operating characteristic curves indicated that GDF15 represents a useful and novel tool to screen for diabetic cardiomyopathy in patients with T2DM [39].
However, the correlation between GDF15 and diabetic cardiovascular complications has mostly been investigated with regard to myocardial or coronary artery diseases, and few data have been reported about GDF15 and LEAD. To the best of our knowledge, this is the first study to investigate an association between serum GDF15 levels and LEAD in T2DM patients. Given that obesity contributes substantially to cardiovascular and other health risks [40], and is one of the most important factors associated with circulating GDF15 levels [17–19], the present study used a BMI cut-off of 25 kg/m2 to assess normal weight or overweight/obesity and analysed the influence of BMI on the relationship between serum GDF15 levels and LEAD. Our results showed that serum GDF15 levels were positively correlated with LEAD, regardless of whether the BMI was < 25 kg/m2 or ≥ 25 kg/m2. After adjusting for confounding factors, per 1-SD increase in the serum GDF15 levels was observed to be significantly related to an approximately 1.4-fold increased risk of LEAD in the total population. Moreover, regardless of whether BMI was < 25 kg/m2 or ≥ 25 kg/m2, this association remained significant, with approximately 1.6- and 1.4-fold increased risks of LEAD, respectively. These results indicated that the association between serum GDF15 levels and LEAD is independent of BMI in T2DM patients.
The mechanism underlying the relationship between serum GDF15 levels and LEAD remains to be determined. On the one hand, elevated GDF15 has been shown to promote inflammation and angiogenesis, implying that GDF15 may play an important role in the pathogenesis of atherosclerosis [41, 42]. However, meanwhile, a reduction in early atherosclerotic lesion size was observed after 4 weeks on a Western-type diet in GDF15-deficient mice; however, no striking differences in lesion size were noticed at the 12-week time point [42]. Similar results were reported in an ApoE(−/−) mouse model of atherosclerosis [43], indicating that GDF15 may play an anti-inflammatory role in the process of atherosclerosis. The expression of GDF15 can be upregulated by multiple proinflammatory stimuli in macrophages, including tumour necrosis factor-α, interleukin (IL)-1b, and IL-2; however, GDF15, in turn, can inhibit the activation of macrophages [1]. Thus, GDF15 functions as a pro- and anti-inflammatory factor in the development and progression of atherosclerosis, and its activity may depend on the pathophysiological environment and progression stage [4].
The present study was limited by the retrospective nature and relatively small sample size, and the cause–effect relationship between the serum GDF15 levels and LEAD and the predictive value of the serum GDF15 levels for LEAD need to be confirmed in further larger prospective studies including nondiabetic populations. Additionally, the present study design did not detect the ankle-brachial index and symptoms of intermittent claudication or ischaemic resting pains, and age was not matched in patients with and without LEAD; these factors need to be addressed in future studies to further explore the association between GDF15 and LEAD. Lastly, the body composition is quite different in Asia/China than in the United States/Europe, so these results may not be applicable to non-Asian populations.
Conclusions
In conclusion, among Chinese patients with T2DM, serum GDF15 levels were significantly elevated in those with LEAD. High serum GDF15 levels were significantly correlated with an increased risk of LEAD, and this relationship was independent of BMI. This suggests that GDF15 may be a potential biomarker to identify individuals with a higher risk of LEAD in clinical practice.
Acknowledgements
We are very grateful to all the staff for helping with the present study. We are grateful to all participants for their dedication to data collection and laboratory measurements.
Abbreviations
- BMI
Body mass index
- CRP
C-reactive protein
- DBP
Diastolic blood pressure
- FCP
Fasting C-peptide
- F-IMT
Femoral intima-media thickness
- FPG
Fasting plasma glucose
- GDF15
Growth differentiation factor 15
- GFR
Glomerular filtration rate
- HbA1c
Glycated haemoglobin A1c
- HDL-c
High-density lipoprotein cholesterol
- Hg
Haemoglobin
- HOMA2-IR
Homeostasis model assessment 2 of insulin resistance
- IMT
Intima-media thickness
- LDL-c
Low-density lipoprotein cholesterol
- LEAD
Lower extremity atherosclerotic disease
- SBP
Systolic blood pressure
- SD
Standard deviation
- T2DM
Type 2 diabetes mellitus
- TC
Total cholesterol
- TG
Triglyceride
- 2hCP
2-h C-peptide
- 2hPG
2-h plasma glucose
Authors’ contributions
XM and JZ designed the study. XH, JS, WL, and WZ collected the data. XH and JS performed the statistical analysis and wrote the paper. YW performed the serum GDF15 measurements. XM, JZ, and YB revised the paper and contributed to the discussion. XH and JS contributed equally to this paper and were the guarantors. All authors read and approved the final manuscript.
Funding
This work was funded by the Shanghai Municipal Education Commission—Gaofeng Clinical Medicine Grant Support (20161430) and Shanghai Municipal Key Clinical Specialty.
Availability of data and materials
The datasets used and analysed during the current study are not publicly available due to the individual privacy of the patients included in this study, but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. All participants provided written informed consent prior to enrolment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xingxing He and Jiaorong Su contributed equally to this work
Contributor Information
Xingxing He, Email: dbxx20130201@163.com.
Jiaorong Su, Email: sujr1217@163.com.
Xiaojing Ma, Email: maxiaojing@sjtu.edu.cn.
Wei Lu, Email: luwei2634@126.com.
Wei Zhu, Email: zhuwei_ly@163.com.
Yufei Wang, Email: wang1fei@126.com.
Yuqian Bao, Email: yqbao@sjtu.edu.cn.
Jian Zhou, Email: zhoujian@sjtu.edu.cn.
References
- 1.Bootcov MR, Bauskin AR, Valenzuela SM, Moore AG, Bansal M, He XY, et al. MIC-1, a novel macrophage inhibitory cytokine, is a divergent member of the TGF-beta superfamily. Proc Natl Acad Sci USA. 1997;94:11514–11519. doi: 10.1073/pnas.94.21.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawton LN, Bonaldo MF, Jelenc PC, Qiu L, Baumes SA, Marcelino RA, et al. Identification of a novel member of the TGF-beta superfamily highly expressed in human placenta. Gene. 1997;203:17–26. doi: 10.1016/S0378-1119(97)00485-X. [DOI] [PubMed] [Google Scholar]
- 3.Paralkar VM, Vail AL, Grasser WA, Brown TA, Xu H, Vukicevic S, et al. Cloning and characterization of a novel member of the transforming growth factor-beta/bone morphogenetic protein family. J Biol Chem. 1998;273:13760–13767. doi: 10.1074/jbc.273.22.13760. [DOI] [PubMed] [Google Scholar]
- 4.Wang J, Wei L, Yang X, Zhong J. Roles of growth differentiation factor 15 in atherosclerosis and coronary artery disease. J Am Heart Assoc. 2019;8:e012826. doi: 10.1161/JAHA.119.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skau E, Henriksen E, Wagner P, Hedberg P, Siegbahn A, Leppert J. GDF-15 and TRAIL-R2 are powerful predictors of long-term mortality in patients with acute myocardial infarction. Eur J Prev Cardiol. 2017;24:1576–1583. doi: 10.1177/2047487317725017. [DOI] [PubMed] [Google Scholar]
- 6.Hagström E, Held C, Stewart RA, Aylward PE, Budaj A, Cannon CP, et al. Growth differentiation factor 15 predicts all-cause morbidity and mortality in stable coronary heart disease. Clin Chem. 2017;63:325–333. doi: 10.1373/clinchem.2016.260570. [DOI] [PubMed] [Google Scholar]
- 7.Ho JE, Lyass A, Courchesne P, Chen G, Liu C, Yin X, et al. Protein biomarkers of cardiovascular disease and mortality in the community. J Am Heart Assoc. 2018;7:e008108. doi: 10.1161/JAHA.117.008108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Zhen C, Wang R, Wang G. Growth-differentiation factor-15 predicts adverse cardiac events in patients with acute coronary syndrome: a meta-analysis. Am J Emerg Med. 2019;37:1346–1352. doi: 10.1016/j.ajem.2019.04.035. [DOI] [PubMed] [Google Scholar]
- 9.Shang L, Feng M, Zhou X, Tang B. Growth differentiation factor 15: a promising prognostic stratification biomarker in patients with acute coronary syndrome. Int J Cardiol. 2019;297:16. doi: 10.1016/j.ijcard.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Zhang S, Dai D, Wang X, Zhu H, Jin H, Zhao R, et al. Growth differentiation factor-15 predicts the prognoses of patients with acute coronary syndrome: a meta-analysis. BMC Cardiovasc Disord. 2016;16:82. doi: 10.1186/s12872-016-0250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olivier CB, Mulder H, Hiatt WR, Jones WS, Fowkes FGR, Rockhold FW, et al. Incidence, characteristics, and outcomes of myocardial infarction in patients with peripheral artery disease: insights from the EUCLID Trial. JAMA Cardiol. 2019;4:7–15. doi: 10.1001/jamacardio.2018.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pourghaderi P, Yuquimpo KM, Roginski Guetter C, Mansfield L, Park HS. Outcomes following lower extremity amputation in patients with diabetes mellitus and peripheral arterial disease. Ann Vasc Surg. 2020;63:259–268. doi: 10.1016/j.avsg.2019.08.084. [DOI] [PubMed] [Google Scholar]
- 13.Kamil S, Sehested TSG, Carlson N, Houlind K, Lassen JF, Bang CN, et al. Diabetes and risk of peripheral artery disease in patients undergoing first-time coronary angiography between 2000 and 2012—a nationwide study. BMC Cardiovasc Disord. 2019;19:234. doi: 10.1186/s12872-019-1213-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adela R, Banerjee SK. GDF-15 as a target and biomarker for diabetes and cardiovascular diseases: a translational prospective. J Diabetes Res. 2015;2015:490842. doi: 10.1155/2015/490842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Retnakaran R. Novel biomarkers for predicting cardiovascular disease in patients with diabetes. Can J Cardiol. 2018;34:624–631. doi: 10.1016/j.cjca.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Shin MY, Kim JM, Kang YE, Kim MK, Joung KH, Lee JH, et al. Association between growth differentiation factor 15 (GDF15) and cardiovascular risk in patients with newly diagnosed type 2 diabetes mellitus. J Korean Med Sci. 2016;31:1413–1418. doi: 10.3346/jkms.2016.31.9.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vila G, Riedl M, Anderwald C, Resl M, Handisurya A, Clodi M, et al. The relationship between insulin resistance and the cardiovascular biomarker growth differentiation factor-15 in obese patients. Clin Chem. 2011;57:309–316. doi: 10.1373/clinchem.2010.153726. [DOI] [PubMed] [Google Scholar]
- 18.Kempf T, Guba-Quint A, Torgerson J, Magnone MC, Haefliger C, Bobadilla M, et al. Growth differentiation factor 15 predicts future insulin resistance and impaired glucose control in obese nondiabetic individuals: results from the XENDOS trial. Eur J Endocrinol. 2012;167:671–678. doi: 10.1530/EJE-12-0466. [DOI] [PubMed] [Google Scholar]
- 19.Dostálová I, Roubícek T, Bártlová M, Mráz M, Lacinová Z, Haluzíková D, et al. Increased serum concentrations of macrophage inhibitory cytokine-1 in patients with obesity and type 2 diabetes mellitus: the influence of very low calorie diet. Eur J Endocrinol. 2009;161:397–404. doi: 10.1530/EJE-09-0417. [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He X, Hu X, Ma X, Su H, Ying L, Peng J, et al. Elevated serum fibroblast growth factor 23 levels as an indicator of lower extremity atherosclerotic disease in Chinese patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2017;16:77. doi: 10.1186/s12933-017-0559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, et al. Mannheim intima-media thickness consensus. Cerebrovasc Dis. 2004;18:346–349. doi: 10.1159/000081812. [DOI] [PubMed] [Google Scholar]
- 23.Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries Endorsed by: the European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2018;39:763–816. doi: 10.1093/eurheartj/ehx095. [DOI] [PubMed] [Google Scholar]
- 24.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–253. [PubMed]
- 25.Nativel M, Potier L, Alexandre L, Baillet-Blanco L, Ducasse E, Velho G, et al. Lower extremity arterial disease in patients with diabetes: a contemporary narrative review. Cardiovasc Diabetol. 2018;17:138. doi: 10.1186/s12933-018-0781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takahara M, Iida O, Kohsaka S, Soga Y, Fujihara M, Shinke T, et al. Diabetes mellitus and other cardiovascular risk factors in lower-extremity peripheral artery disease versus coronary artery disease: an analysis of 1,121,359 cases from the nationwide databases. Cardiovasc Diabetol. 2019;18:155. doi: 10.1186/s12933-019-0955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep. 2019;19:86. doi: 10.1007/s11892-019-1212-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sen S, Barsun A, Romanowski K, Palmieri T, Greenhalgh D. Neuropathy may be an independent risk factor for amputation after lower-extremity burn in adults with diabetes. Clin Diabetes. 2019;37:352–356. doi: 10.2337/cd18-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang SL, Zhu LY, Han R, Sun LL, Li JX, Dou JT. Pathophysiology of peripheral arterial disease in diabetes mellitus. J Diabetes. 2017;9:133–140. doi: 10.1111/1753-0407.12474. [DOI] [PubMed] [Google Scholar]
- 30.Graz H, D’Souza VK, Alderson DEC, Graz M. Diabetes-related amputations create considerable public health burden in the UK. Diabetes Res Clin Pract. 2018;135:158–165. doi: 10.1016/j.diabres.2017.10.030. [DOI] [PubMed] [Google Scholar]
- 31.Hsu LA, Wu S, Juang JJ, Chiang FT, Teng MS, Lin JF, et al. Growth differentiation factor 15 may predict mortality of peripheral and coronary artery diseases and correlate with their risk factors. Mediat Inflamm. 2017;2017:9398401. doi: 10.1155/2017/9398401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Haan JJ, Haitjema S, den Ruijter HM, Pasterkamp G, de Borst GJ, Teraa M, et al. Growth differentiation factor 15 is associated with major amputation and mortality in patients with peripheral artery disease. J Am Heart Assoc. 2017;6(9):e006225. doi: 10.1161/JAHA.117.006225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munk PS, Valborgland T, Butt N, Larsen AI. Response of growth differentiation factor-15 to percutaneous coronary intervention and regular exercise training. Scand Cardiovasc J. 2011;45:27–32. doi: 10.3109/14017431.2010.516368. [DOI] [PubMed] [Google Scholar]
- 34.Farhan S, Freynhofer MK, Brozovic I, Bruno V, Vogel B, Tentzeris I, et al. Determinants of growth differentiation factor 15 in patients with stable and acute coronary artery disease. A prospective observational study. Cardiovasc Diabetol. 2016;15:60. doi: 10.1186/s12933-016-0375-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gohar A, Gonçalves I, Vrijenhoek J, Haitjema S, van Koeverden I, Nilsson J, et al. Circulating GDF-15 levels predict future secondary manifestations of cardiovascular disease explicitly in women but not men with atherosclerosis. Int J Cardiol. 2017;241:430–436. doi: 10.1016/j.ijcard.2017.03.101. [DOI] [PubMed] [Google Scholar]
- 36.Liu H, Lyu Y, Li D, Cui Y, Huang Y, Dai W, et al. Potential relation between soluble growth differentiation factor-15 and testosterone deficiency in male patients with coronary artery disease. Cardiovasc Diabetol. 2019;18:21. doi: 10.1186/s12933-019-0823-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kozakova M, Morizzo C, Goncalves I, Natali A, Nilsson J, Palombo C. Cardiovascular organ damage in type 2 diabetes mellitus: the role of lipids and inflammation. Cardiovasc Diabetol. 2019;18:61. doi: 10.1186/s12933-019-0865-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berezin AE. Diabetes mellitus related biomarker: the predictive role of growth-differentiation factor-15. Diabetes Metab Syndr. 2016;10(1 Suppl 1):S154–S157. doi: 10.1016/j.dsx.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 39.Dominguez-Rodriguez A, Abreu-Gonzalez P, Avanzas P. Usefulness of growth differentiation factor-15 levels to predict diabetic cardiomyopathy in asymptomatic patients with type 2 diabetes mellitus. Am J Cardiol. 2014;114:890–894. doi: 10.1016/j.amjcard.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 40.Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72:1506–1531. doi: 10.1016/j.jacc.2018.08.1037. [DOI] [PubMed] [Google Scholar]
- 41.Bonaterra GA, Zügel S, Thogersen J, Walter SA, Haberkorn U, Strelau J, et al. Growth differentiation factor-15 deficiency inhibits atherosclerosis progression by regulating interleukin-6-dependent inflammatory response to vascular injury. J Am Heart Assoc. 2012;1:e002550. doi: 10.1161/JAHA.112.002550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Jager SC, Bermúdez B, Bot I, Koenen RR, Bot M, Kavelaars A, et al. Growth differentiation factor 15 deficiency protects against atherosclerosis by attenuating CCR2-mediated macrophage chemotaxis. J Exp Med. 2011;208:217–225. doi: 10.1084/jem.20100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnen H, Kuffner T, Brown DA, Wu BJ, Stocker R, Breit SN. Increased expression of the TGF-b superfamily cytokine MIC-1/GDF15 protects ApoE(−/−) mice from the development of atherosclerosis. Cardiovasc Pathol. 2012;21:499–505. doi: 10.1016/j.carpath.2012.02.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study are not publicly available due to the individual privacy of the patients included in this study, but are available from the corresponding author on reasonable request.