Abstract
Considering the pivotal roles played by dendritic cells (DCs) in both innate and adaptive immune responses, advances in the field of porcine immunology DC biology have recently progressed rapidly. As with the more extensively studied murine and human DCs, porcine DC can be generated from bone marrow haematopoietic cells or monocytes, and have been analysed in various immunological and non-immunological tissues. Both conventional DC (cDC) and plasmacytoid DC (pDC) have been characterized. The function of porcine monocyte-derived DC has not only been characterized in terms of antigen presentation and lymphocyte activation, but also their response to various ligands of pattern recognition receptors. These have been characterized in terms of the induction of DC maturation and pro-inflammatory, Th1-like or Th2-like cytokines secretion. Porcine pDC most effectively sense virus infections and are characterized by their capacity to produce large quantities of IFN-α and the pro-inflammatory cytokines TNF-α, IL-6 and IL-12. As such, the DC family as a whole is a powerful ally in the host battle against pathogen attack. Nevertheless, DC in particular tissue environments or under particular stimuli can down-regulate immune response development. This is not only important for preventing over-activation of the immune system and also for ensuring tolerance against self or “friendly” substances including food components, but may also be used as a mechanism of pathogens to evade immune responses.
Keywords: Swine, Antigen presenting cells, Dendritic cells, Natural interferon producing cells
1. Introduction
Dendritic cells (DCs) are a heterogeneous group of potent antigen-presenting cells (APCs) with the unique capacity to prime naive T-cell responses [1]. In order to fulfil their role as sentinels of the immune system, they express several families of specialized pattern recognition receptors (PRRs) for particular pathogen-associated molecular patterns (PAMPs). These include Toll-like receptors (TLRs), nucleotide- binding oligomerization domain (NOD)-like receptors (NLRs), retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs) and C-type lectin receptors (CLRs) all reacting directly with pathogen components [2], [3], [4]. In addition, many other receptors exist such as Fc receptors and activated complement component receptors, reacting with complexes of pathogen antigen with antibody or complement. Another element essential to DC biology is their migratory behaviour in response to chemokine gradients. DCs are the main cellular element controlling T lymphocyte activation and regulation. Furthermore, they are involved in B-cell responses, possibly through the delivery of native antigen to B lymphocytes [5], [6], [7], but certainly through the production of B-cell stimulatory factors important for B-cell proliferation, differentiation and isotype switching [8], [9]. DCs also play a functional role for NK cell activation [10], [11], and are in a two-way communication with neutrophils [12].
Understanding DC biology requires the consideration of the heterogeneity and independence of DC functional plasticity. An important element therein is the functional and phenotypic differentiation of “conventional DC” (cDC) from “plasmacytoid DC” (pDC). The term cDC summarizes all DC subsets with “professional antigen presenting” function, while pDC represent the “professional interferon-α producers” [13]. Indeed, pDC are also referred to as “natural interferon producing cells” (NIPC), a functional entity first described 25 years ago [14]. However, more recent studies have demonstrated that also pDC have important antigen-presenting functions and that the two DC subsets complement each others by having a distinct regulation of MHC class I- and II-dependent antigen presentation [15], [16], [17]. Furthermore, DCs show a high level of heterogeneity, particularly in the specialized roles of various DC subsets dependent on their tissue localization and local immunological environment, which guides their function (Table 1 ).
Table 1.
Comparative phenotype and tissue localisation of porcine DC subsets and related antigen presenting cells
| CD172a | CD1 | CD4 | CD11R1 | CD14 | CD16 | MHCII | CD80/86 | References | |
|---|---|---|---|---|---|---|---|---|---|
| MoDC | + | + | − | − | +/low | + | + | + | [23], [24] |
| GM-CSF BMDC | + | + | − | − | + | + | + | + | [23] |
| Flt3L BMDC | + | + | − | − | +/−a | + | + | + | unpublished |
| blood cDC | low | +/−b | − | − | − | +/−b | high | + | [40] |
| pDC | low/−c | +/−b | + | − | − | +/−b | + | low | [40] |
| thyroid gland DC | + | n.d.d | n.d. | n.d. | n.d. | n.d. | + | n.d. | [78] |
| thymus DC | + | + | n.d. | n.d. | n.d. | n.d. | + | n.d. | [77] |
| skin DC | + | + | n.d. | n.d. | ± | n.d. | + | + | [62] |
| mucosal tissue DC | +/−e | −f | n.d. | +/−e | −f | + | + | + | [46], [47], [61] |
| mucosal lymph DC | +/−g | +/− | n.d. | + | n.d. | +/−g | + | + | [47] |
| monocytes | + | − | − | − | + | + | +/− | low | [40], [44] |
| macrophages | + | +/− | − | − | +/− | + | low | low | [118], [119] |
| fibrocytes | + | + | n.d. | n.d. | + | + | + | + | [25] |
Two subsets.
Variable, two subsets with some animals (see also Fig. 1).
Can be negative in mucosal tissue [55].
Not determined.
Four subsets based on CD172a/CD11RI expression and dependent on localization in LP, PP and MLN [47].
Negative on LP DC [46].
Two subsets: CD172a+CD1+CD16+ and CD172a−CD1−CD16−.
One general functional consideration of all DC subsets is their critical roles as immunological sentinels. Being strategically located at sites of pathogen entry, such as mucosal surfaces and dermal layers, DC can rapidly interact with pathogen PAMPs resulting in cell activation, pathogen uptake and degradative processing of the pathogen (antigen). A critical element therein is the concomitant uptake of antigen with PAMP recognition. The latter represents the “danger” signalling which the DC requires to be activated. In the absence of the “danger” signal, the DCs tend to function more as tolerogenic DC, inducing lymphocyte anergy. Such processes are involved in responses to self-antigens and tolerance of food antigens.
Following interaction with a pathogen (and its PAMPs), cDC endocytic activity—particularly macropinocytosis—is enhanced during the first 2 h after stimulation, followed by down-regulation as the DC mature. The latter relates to a prolonged capacity for efficient presentation of the endocytosed and processed antigen [18]. With completion of the DC maturation process, important biological changes occur to the DC. Chemokine receptor expression is modified, enabling migration to the inductive sites of the adaptive immune system. For example, the CCR1 and CCR5 receptors for inflammatory chemokines such as CCL3 and CCL5 are down-regulated, while the CCR7 receptor for CCL19 and CCL21 is up-regulated [8]. The latter provides DC with the signal for entry into the inductive sites of the adaptive immune system such as the lymph node. DC activation also results in an increase of cell surface MHC and co-stimulatory molecule expression—such as CD80 and CD86—as well as the production of immunoregulatory and/or inflammatory cytokines. MHC class II antigenic peptide complexes are stabilized on the cell surface to ensure efficient stimulation of T-cell responses. Overall, the induced functional changes are usually associated with increased T-lymphocyte stimulatory capacity, although this depends on the stimulus received [19].
Clearly, the interaction of microbial pathogens with DC can provide insight into the pathogenesis of and defence against infectious diseases. Moreover, the central role of DC in immune defence development makes them a prime target for vaccines and immunotherapies. Recent advances in porcine immunology have allowed the characterization of the porcine DC system in this direction (as witnessed by the identified cell types shown in Table 1). This has also been possible through the availability of antibodies against cell surface markers classified in three international swine CD workshops [20], [21], [22] and studies using crossreactive antibodies—summarized in Table 2 . By such means, rapid advancement in the current knowledge on porcine APC and the diversity of porcine DC function has been forthcoming. The subsequent sections of this review will present these advancements.
Table 2.
Reagents used for labelling of surface molecules on porcine APC
| CD name | Functional name | Detection | References |
|---|---|---|---|
| CD1 | mAb 76-7-4 | [23], [24], [77], [119] | |
| CD4 | mAbs 74-12-4, PT90A | [40] | |
| CD2 | MAb MSA-2 | [77] | |
| CD11R1 | CR3 | mAb MIL4, TMG.6-5 | [47] |
| CD11R2 | CD11c (human) | anti-human mAb S-Hcl3 | [40] |
| CD14 | LPS R | mAbs CAM36A, MIL2 | [23], [24] |
| CD16 | FcγRIII | mAb G7 | [40], [46] |
| CD32 | FcγRII | mAb AT-10 (anti-human) | [57] |
| CD40 | anti-human mAb G28-5 | [34] | |
| CD80/86 | B7-1/B7-2 | rh CTLA-4-Ig (anti-human) | [23] |
| CD86 | B7-2 | anti-human mAb HA5.2B7 | unpublishedb |
| CD116 | GM-CSF R* | rp GM-CSF-his-tagged | [40] |
| CD123 | IL3 R | rp IL-3-his-tagged | [40] |
| CD163 | Scavenger R | mAb 2A10 | [45] |
| CD172a | SIRP-α | various | [32] |
| CD184 | CXCR4 | anti-human, clone 44708 | [120] |
| CD191 | CCR1 | anti-human, clone 145 | [34], [120] |
| CD206 | mannose R | anti-human, clone 3.29B1.10 | unpublishedb |
| CD208 | DC lamp | anti-human clone 104.G4 | [49] |
| MHC class II | various clones | [24], [46], [47], [60], [77] |
aDetected using anti-His-Tag mAb (Roche, Basel, Switzerland).
bSummerfield et al.
2. Porcine DC subsets
2.1. Porcine DC generated in vitro
2.1.1. Monocyte-derived DC (MoDC)
Similar to other species, porcine DC can be generated by stimulating blood monocytes with interleukin-4 (IL-4) and granulocyte macrophage-colony-stimulating factor (GM-CSF). After 3–7 days of culture, non-adherent or loosely adherent cells with dendritic morphology can be harvested [23], [24]. Generation of monocyte-derived DC (MoDC) in vitro can also employ a GM-CSF/IFN-α combination. This can prove more potent than the GM-CSF/IL4 method when seeking DC for restimulating virus-specific cytotoxic T-cells [25]. Addition of IFN-α to the GM-CSF/IL-4 cocktail also influences the DC, resulting in an enhanced T-cell stimulatory capacity in mixed leukocyte cultures [26]. In fact, cytokine modulation is important for manipulating the type of DC generated. TGF-β permits the generation of cells with Langerhans cell characteristics [24], while PAMPs modulate mRNA expression levels for particular TLRs [27]. Bautista et al. [28] have also demonstrated that IL-4 can be replaced by IL-13 for the generation of MoDC. Phenotypically, porcine MoDC are characterized as CD1+CD14+CD16+CD80/86+CD172a+ and MHC class II+ [23], [24], [28], [29], [30] (Table 1). From a comparative immunological point of view, it was unexpected to find CD14, because human CD14 is considered to be a typical monocyte/macrophage rather than a DC marker [8]. Nevertheless, MoDC from other species such as cat, cattle and dog have also been shown to express CD14 [31]. Of the other markers, the CD172a was expected due to its classification as the porcine swine workshop cluster 3 (SWC3) antigen expressed on cells of the myelomonocytic lineage [32]. It is expressed on many monocytic and granulocytic cells quite early during their differentiation [33]. Functionally, this marker represents the signal regulatory protein alpha (SIRP-α). Altogether, the co-expression of CD172a and CD1 along with relatively high levels of both CD80/86 and MHC class II represent phenotypic characteristics of porcine MoDC but no marker clearly differentiating them from monocyte-derived macrophages has been identified.
Porcine MoDC generated with GM-CSF and IL-4 relate to human MoDC in that they are in an immature state, and represent a convenient cell culture model to study the DC maturation process. Akin to their human counterparts, porcine MoDC up-regulate CD80/86, MHC classes I and II, and T-cell stimulatory activity upon maturation, while inflammatory chemokine receptors such as CCR1 and macropinocytic activity are down-regulated [23], [24], [27], [34], [35], [36].
2.1.2. Bone marrow-derived DC (BMDC)
Porcine DC, which phenotypically and functionally resemble MoDC, can also be generated from bone marrow haematopoietic cells (BMHC), stimulated with GM-CSF plus TNF-α, or GM-CSF alone, for 7–10 days—BMDC [23]. Addition of stem cell factor to the GM-CSF/TNF-α cocktail increases the yield of DC obtained [37]. In contrast to GM-CSF, Flt3 ligand (Flt3L) stimulation induces the differentiation of both cDC and pDC, similar to the situation with human and mouse BMHC [13] (Guzylack-Piriou and Summerfield, unpublished data). Furthermore, Flt3L-induced BMHC-derived cDC phenotypically and functionally differ from GM-CSF-derived DC either generated with monocytes or BMHC. Flt3L induces the differentiation of CD14− cDC which are more sensitive to stimulation by TLR2/TLR6, TR3, TLR4, TLR5 and TLR7 ligands in terms of cytokine responses and maturation [38] (Guzylack-Piriou and Summerfield, unpublished data). This may relate to the central role of Flt3L in the generation of DC from a clonogenic BMHC DC precursor [39].
2.2. Blood DC
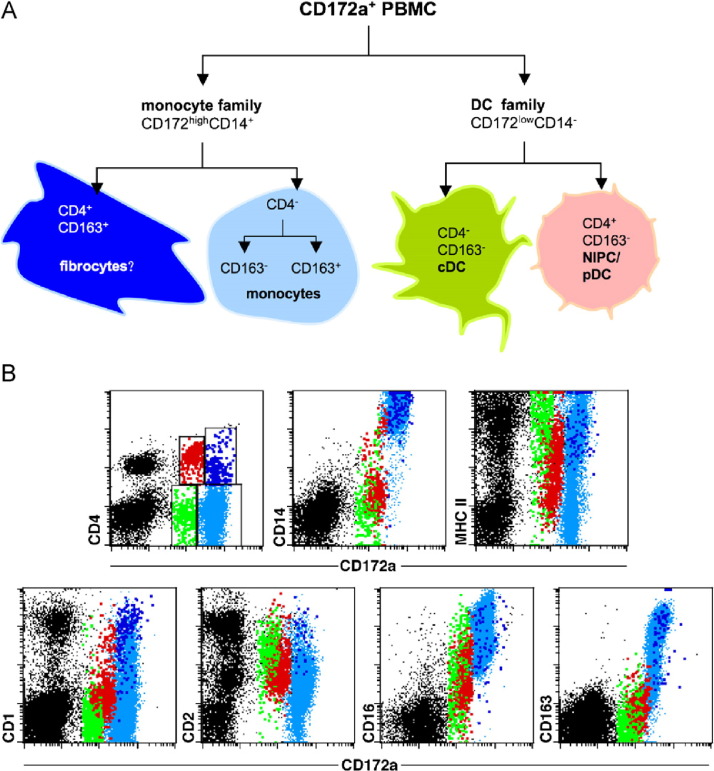
Porcine blood is similar to human blood in representing an important source of APC. Several populations have been identified, including monocytes, DC precursors and fibrocytes. All of these express CD172a, and in a model of antigen presentation of inactivated foot-and-mouth disease virus (FMDV) to T lymphocytes the activation was dependent on the presence of CD172a+ cells [40], [41]. Similar results were also obtained with classical swine fever virus (CSFV) and protein antigens derived from this virus [25], [42], as well as with tetanus toxoid [43]. Separating the CD172a+ PBMC into a major population of CD14+ monocytes and a minor population of CD14− cells showed that the latter contained the CD4− blood cDC along with the CD4+ pDC (Table 1; [40]). It is notable that although the blood cDC and pDC differ phenotypically (CD4 expression), they are similar in their lack of CD14 expression, which distinguishes them from in vitro generated MoDC. However, this simple discrimination is not absolute. The composition of blood APC is more complex, as summarized in Fig. 1 . Accordingly, it is necessary to appreciate each of the blood APC in turn, to obtain a better understanding of their roles and function in immune defences.
Fig. 1.
Phenotype of porcine blood DC. (A) Porcine CD172a+ blood APC can be differentiated into CD14+ monocytic cells and CD14− DC. Two major subpopulations of CD4− monocytic cells can be defined based on CD163 expression (depicted light blue; see also Dominguez et al., this issue). Furthermore, a small CD4+CD14+CD163+ subset with unknown function can be identified (dark blue). Porcine blood DC express relatively low levels of CD172a and lack CD14 and CD163. While cDC are CD4− (green), pDC express high levels of CD4 (red). (B) Expression of CD14, MHC class II, CD1, CD2, CD16 and CD163 on CD172ahighCD4− monocytes (light blue dots), CD172ahighCD4+ monocytic cells (dark blue dots), CD172alowCD4− cDC (green dots) and CD172alowCD4+ pDC (red dots). A representative animal is shown. Comparison of five different SPF pigs of the similar age (6–12 month old) revealed high variability in the expression levels of MHC class II, CD1, CD2 and CD16 on the DC subpopulations.
2.2.1. Conventional blood DC
Porcine blood carries a subpopulation of PBMC, which are CD172a+CD4−CD14−, with characteristics of cDC-high levels of MHC class II and CD80/86 (Fig. 1 and Table 1), nonadherence and potent T-cell stimulatory capacity [40]. After in vitro culture, these cells strongly up-regulate MHC and co-stimulatory molecules, and their dendritic morphology becomes clear. Based on these characteristics, we have proposed that this population contains the precursors of blood cDC. These cells have variable expression of CD1 and CD16 and can be differentiated from monocytes by lower levels of CD172a (Fig. 1 and [40]). Although the majority of porcine blood monocytes are CD1−CD4−CD14+CD16+ CD172a+ (Table 1 and Fig. 1), a detailed analysis of the monocytic population has identified at least four subsets based on CD14 and CD163 [44]. It is currently not clear how the blood cDC population phenotypically defined as CD172a+CD4−CD14− cell relates the CD14−CD163+ monocytic cell. CD163 is proposed as a macrophage marker, which is up-regulated during the differentiation of monocytes to macrophages [45] but down-regulated if monocytes are induced to differentiate into DC by GM-CSF/IL-4 [30]. This would argue for two distinct subsets of cells, a point which is not surprising considering the diversity of the DC family, but still requires further clarification (see also Dominguez et al., this volume).
Based on the frequent expression of the CD11R1 marker on DC in the mucosa [46], [47], this marker has also been proposed for identification of cDC in the blood and other organs as a CD172a+CD11R1+ population [48], [49]. However, this definition may not be sufficient as no functional studies have been described, and it does not consider that a subset of monocytes also express CD11R1 [50].
2.2.2. Natural interferon producing cells/plasmacytoid DC (pDC)
Although several cell types can produce type I IFN upon viral infection, pDC are particularly adept at secreting very high levels of type I IFNs [13]. Representing less of 0.5% of the PBMC [40], porcine pDC were identified through their IFN-α responses to transmissible gastroenteritis virus (TGEV) [51]. Charley and Lavenant [51] originally described them as being non-adherent, non-T, non-B, CD4+, MHC-class-II positive cells. Subsequently, they went on to describe their ontogeny [52], [53] and migration into lymphoid tissue after viral challenge in vivo [54], [55]. Recently, using the ovine and porcine models, it has been demonstrated that pDC also migrate in the afferent lymph of cannulated animals [56].
Phenotypically, porcine pDC can be clearly identified as CD172alowCD4highCD14−CD163− within the peripheral blood population (Table 1). They express no or low levels of the T-cell markers CD3, CD5 and CD6, as well as no CD21 [40], but can carry low levels of CD1 and moderate levels of CD2 (Fig. 1). Related to their interaction with immune complexes porcine pDC express Fc receptors including CD16 (Fig. 1, [40]) and CD32 [57]. In contrast to porcine pDC, ovine pDC do not express CD4 and CD172a but are characterized by high expression of CD45RB [56].
Porcine pDC appear to be the major DC population producing high quantities of IFN-α and TNF-( in response to CpG motifs [58]. This clearly relates to the human DC system, placing the porcine DC system in line with that of humans and therefore distinct from the murine model [59]. Certainly related to their human and mouse counterparts is their ability to respond to many viruses by the production of large quantities of IFN-α (see below).
2.3. Mucosal DC
2.3.1. cDC
With the major site for pathogen entry being through the mucosa of the respiratory and digestive tract, it is not surprising that most lymphocytes are in the mucosalassociated lymphoid tissues (MALT). Consequently, it is essential to regulate the mucosal immune responses against harmless microorganisms and food antigens in contact with the mucosae. This is a major role played by mucosal DC and is reflected by their anatomical localization in the mucosal tissues. They can mediate tolerance to self-antigens and harmless entities, while acting as sentinels sensing the danger posed by invading pathogens and deleterious entities. The first report on porcine mucosal DC described a putative DC in Peyer's patches (PP) as MHCII+ cell lacking T- and B-cell markers [60]. In the lamina propria (LP) of the small intestine the presence of an MHCII+CD172a+CD11R1+ CD16+ DC subset was demonstrated [46]. Bimczok and colleagues [47] further characterized DC in other immunological sites of the gut and proposed four phenotypically distinct subsets of DC based on the expression of CD11R1 and CD172a. LP DC are mainly CD172a+ CD11R1+, PP DC are mainly CD172a+CD11R1− in subepithelial domes and CD172a−CD11R1− in interfollicular regions, and mesenteric lymph node (MLN) DC are mostly CD172a− CD11R1+. Interestingly, only the CD11R1+ DC subsets were present in lymph, suggesting that DC migration to MLN originates largely from the LP. With respect to antigen sampling a rare population of LP DC extending cytoplasmic processes between enterocytes have been described [61]. In the PP, it appears that antigen transfer from M cells to DC is an important process, as many DC in the subepithelial dome have been demonstrated to be adjacent to M cells [61].
In contrast to the lack of CD172a on many DC in the inductive interfollicular areas of the MLN and PP, CD172a is expressed on porcine DC is at peripheral sites of pathogen entry and antigen contact such as the skin, LP and PP subepithelial dome [46], [47], [62]. This would indicate a possible down-regulation of this molecule during the maturation and migration process, and would be supported by the observed expression of CD172a on MoDC, BMDC generated using either GM-CSF or Flt3L, as well as circulating blood DC [23], [37], [38]. Nevertheless, with in vitro maturation studies using MoDC, BMDC as well as blood DC [23], [57], [58], [63], [64] no loss of CD172a was observed indicating that additional factors would be required for this process. An alternative explanation would be that CD172a− DC represent lymph node tissue resident DC which are phenotypically distinct from in vitro generated DC.
In humans, rat, cattle and sheep, the expression of CD172a differentiates functionally distinct DC subsets. While CD172a+ DC are more stimulatory for T cells, it is possible that the CD172a− subsets is specialized in the phagocytosis of apoptotic cells [65], [66], [67], [68], [69]. Future studies are required to clarify such functional differences in the pig.
DCs from the porcine upper respiratory tract have also been described. In the tracheal mucosa many DC are located above the basal membrane and inside the epithelial layer where they form a dense network with many cytoplasmic processes probably related to their important role as immunological sentinels in this organ [61]. The majority of these cells co-express CD16 and MHC class II but not CD11R1. Jamin et al. [49] recently described putative DC in the tonsils by co-expression of CD11R1 and CD208 (DC lamp) or co-expression of CD11R1 and CD172a. Nevertheless, from this study it is unclear whether a CD172a− DC would exist in this organ. It is also not yet clear how CD172a is expressed in DC of non-mucosal lymphoid tissue.
Several functional properties have been assigned to mucosal DC originating from the gut including the capacity to imprint the mucosal homing receptors a4b7 integrin and CCR9 on T and B lymphocytes, the secretion of cytokines of the mucosal microenvironment such as IL-10 and TGF-β, the promotion of T regulatory and Th2 rather than Th1 responses, and the induction of IgA secretion [70], [71], [72], [73], [74]. Considering that the capacity of gut DC to produce retinoic acid (RA) is a requirement for many of these functions and that gut DC are likely to be themselves under the influence of RA derived from gut epithelial cells, we have tested whether porcine MoDC can acquire the function of gut mucosal DC. After treatment of porcine MoDC with RA the DC acquired the capacity to promote a4b7 integrin and CCR9 on T lymphocytes, to secrete TGF-β and to promote IgA responses [75]. We have extended these studies and also demonstrated that RA induces the expression of retinaldehydrogenase, a rate-limiting enzyme in the synthesis of RA. The drug-mediated inhibition of this enzyme in RA-treated DC abrogated their capacity to promote mucosal homing receptors expression on lymphocytes (Saurer and Summerfield, unpublished data). This underlines the important role of tissue-specific factors in governing DC function.
2.3.2. pDC
NIPC/pDC have been identified as IFN-α-positive cells by immunohistochemistry in the intestinal epithelial layer, the LP, near the PP and in the MLN early after infection with transmissible gastroenteritis virus (TGEV) [55]. Since this was associated with high levels of serum IFN-α and only few IFN-α producing cells were identified in other organs it appears that during an enteropathic virus infection IFN-α would almost exclusively originate from gut pDC triggered locally. The rapid IFN-α response of pDC as early as 6 h after infection would imply that pDC are present in mucosal tissue fulfilling their role as sentinels. This relates to the recently identified CCR9 expression and migration of mouse pDC to the small intestine under steady-state conditions [76] and also to the presence of pDC identified as CD172a+CD4+ cells in tonsils and MLN of healthy pigs [49].
2.3.3. DC in other organs
Bautista et al. have isolated DC migrating from porcine skin explants. Phentotypically these cells resemble MoDC in terms of CD172a co-expression with CD1 and the high levels of MHC class II and CD80/86 (Table 1). Moreover, isolated skin-derived DC show variable expression of CD11R2, CD14 and CD16 [62].
Immunohistochemical analysis of porcine thymic tissue has shown DC to be large cells located in the medullary and the cortico-medullary regions, as evidenced by the presence of surrounding Hassall's corpuscles. Porcine thymic DC have also been partially purified and characterized [77]. They too relate to MoDC and skin DC in their CD1, CD172a and MHC class II expressions, but additionally express CD2 (Table 1), which can also be found on blood DC (Fig. 1).
Croizet and colleagues [78] demonstrated the value of the porcine model for characterizing DC from non-lymphoid organs, such as the thyroid DC.
2.3.4. Fibrocytes
Besides the more “classical” APC, a relatively recent addition has been described. Fibrocytes are a blood-derived cell population with fibroblastoid morphology, which is distinct from DC. Fibrocytes have been described for mice, humans and pigs [25], [79], [80], and represent 0.5–1% of nucleated cells in peripheral blood. They express CD13 and CD34, which would suggest a haematopoietic origin, possibly myeloid. The presence of CD14, CD16 and CD172a on porcine fibrocytes [25], and the differentiation of human fibrocytes in vitro from a blood-derived CD14+ population [81] support this hypothesis. Porcine fibrocytes originate from a CD163+ PBMC subpopulation [82]. Fibrocytes are important during wound healing, rapidly entering sites of injury together with inflammatory leukocytes [80]. They are also an important source of cytokines and chemokines important for T lymphocyte and DC development. These include IL-6, IL-10, macrophage-colony-stimulating factor, macrophage inflammatory protein-1a, MIP-1b and monocyte chemoattractant protein-1 [83].
It has been suggested that fibrocytes may play an early role in the induction of antigen-specific immunity [83], [84], in particular the activation of T helper lymphocytes [80]. Porcine fibrocytes were also shown to be potent APC, relating to their expression of MHC class II, CD1 and CD80/CD86, as well as their endocytic activity [25]. These cells activate CD4+ T cells, but also efficiently stimulate virus-specific CD8+ CTL. In fact, fibrocytes are effective at low ratios with T lymphocytes, ratios at which MoDC are less efficient [25]. Porcine fibrocytes also respond to TLR ligands by producing large quantities of IL-6 [82]. These TLR ligands include LPS (TLR4-ligand), lipopeptide (diacylated form recognized by TLR1/TLR2 heterodimers; triacylated form recognized by TLR2/TLR6 heterodimers), and TLR7 ligands [82].
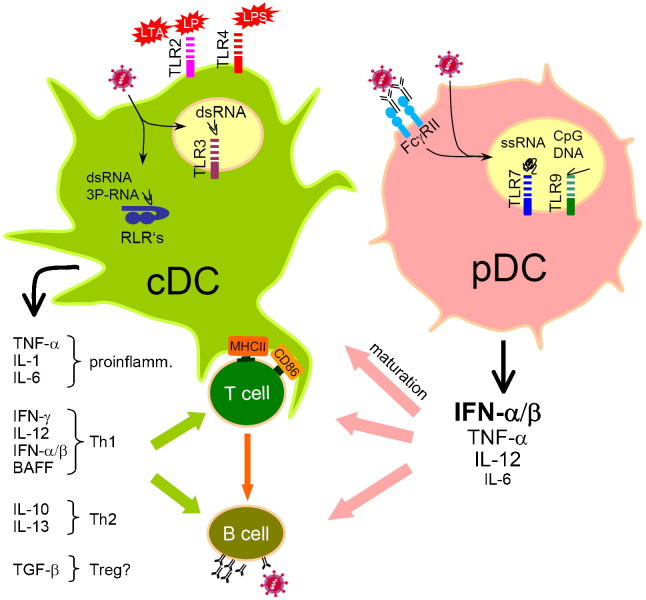
3. Porcine DC recognition of “danger”
The importance of DC within the innate immune system is due to their recognition of PAMPs through their PRRs. TLR play a central role in this concept of innate immune recognition. This results in a robust cytokine and chemokine response, along with DC activation and maturation, all essential for adaptive immune response development (Fig. 2 ). A simplified concept is that antigen presentation in the absence of DC activation leads to tolerance or shortlived immune responses without immunological memory development [85]. The current evidence shows that concomitant recognition of the antigen and a “danger” signal is essential for the DC to promote adaptive immune defence development [86]. With self and food antigens, the absence of the “danger” signal ensure that the DC involved are tolerogenic.
Fig. 2.
Functional specialization of porcine cDC and pDC at the interface innate-adaptive immunity. The current knowledge on PAMP responsiveness and cytokine profile is schematically represented. Porcine pDC produce not only particularly large quantities of type I IFN but also TNF-α, IL-12 and IL-6 after stimulation with certain viruses, TLR7 and TLR 9 ligands. These cytokines promote cDC maturation. The latter are involved in antigen presentation and regulate lymphocyte responses. This is partially controlled by the cytokines profile, which depends on stimulation by TLR ligands, RLR ligands, viruses and bacteria as well as other factor such as the tissue environment. The cytokine profiles can be classified as proinflammatory, Th1- and Th2-like. The influence of porcine DC on differentiation of T regulatory cells (Treg) has not yet been described.
For efficacious immune defence development, the cell subset-specific recognition of PAMPs plays a critical role, resulting in the DC-derived cytokines necessary for both the innate response and the strength and quality of the adaptive response. In addition to phenotypic differences, it is also in this area of PAMP recognition that species-dependent differences are observed. Consequently, it is important to understand how porcine APC recognition of PAMP compared with human APC, and to determine the distribution of TLR within the porcine DC system. In Fig. 2, a schematic overview of the functional specialization and cytokine production of porcine cDC and pDC is represented. The current knowledge on the cytokine responses of MoDC is also included in the overview provided by Table 3 .
Table 3.
Response of MoDC to stimulation by TLR ligands and cytokines
| MHCII | CD80/86 | endo- cytosis | T-cell activation | Cytokine secretion | References | |
|---|---|---|---|---|---|---|
| TLR/RLR ligands | ||||||
| LPS | ↑ | ↑ | ↓ | ↑ | TNF-α IL-6, IL-10a, IL-12a, IL-13a, IFN-γa | [23], [27], [35], [87] |
| Pam-3-Cys | ↑ | ↑ | ↓ | n.d.b | IL-6 | [35], [75] |
| LTA | ↑ | ↑ | n.d. | n.d. | IL-10a, IL-12a, IL-13a, IFN-γa | [27] |
| Peptidogycan | ↑ | ↑ | n.d. | n.d. | IL-12a | [27] |
| CpG | ↑ | ↑ | n.d. | n.d. | IL-12p35a, IFN-γa | [27] |
| PolyIC | ↑ | ↑ | ↓ | ↑ | INF-αβIL-6, IL-12a, IFN-γa | [36], [75], [87] |
| PolyIC tfc | ↑ | ↑ | n.d. | n.d. | INF-αβ | [36] |
| mRNA tf | ↑ | ↑↑ | n.d. | ↑ | INF-αβ | [36] |
| pDNA tf | ↑ | n.d. | n.d. | n.d. | IL-12 | [26] |
| Other microbial components | ||||||
| CTd | ↓ | ↑ | ↓ | ↓↓ | TNF-α↓, IL-10 | [34] |
| LTe | ↓ | ↑ | = | n.d. | n.d. | [75] |
| Actinobacillus | n.d. | n.d. | n.d. | n.d. | IL-6, IL-10, IL-12 | [26] |
| Fusarium toxin | = | ↓ | ↓ | = | IL-10↓ | [121] |
| Cytokines, cytokine/TLR ligand cocktails | ||||||
| TNF-α | = | ↑ | n.d. | ↑↑ | n.d. | [64] |
| TNF-α/LPS | ↑↑ | ↑↑ | ↓ | ↑ | [34] | |
| IFN-α/pIC | ↑↑ | ↑↑ | ↓ | n.d. | n.d. | [64] |
| IFN-α/TNF-α | ↑↑ | ↑↑ | ↓ | ↑ | n.d. | [64] |
| IFN-α/TNF-α/TLR ligand | ↑↑↑ | ↑↑↑ | ↓ | n.d. | n.d. | [35], [64] |
mRNA levels analysed.
Not determined.
Transfection.
Cholera toxin.
Heat-labile enterotoxin (E. Coli).
3.1. Response of cDC to TLR ligands
3.1.1. Maturation and phenotypic modulation
One of the important responses induced by TLR ligation on DC is the induction of maturation. As a simple read-out of this process increased levels of surface molecules involved in antigen presentation such as MHC class II, CD40 and CD80/86 are often used. Nevertheless, the interpretations of such results alone do not permit definitive conclusions on the maturation status of a DC in terms of T-cell stimulatory activities [19].
Porcine MoDC as a model of cDC relate to those from other species in their response to TLR ligands by upregulation of MHC and CD80/86 (Table 3). These include TLR2 ligands Pam3Cys lipopeptide, pseudomonas OprI lipoprotein, lipoteichoic acid (LTA) and peptidoglycan [27], [35], TLR3 ligands such as synthetic double-stranded (ds) RNA polyinosinic– polycytidylic acid (polyIC) [27], [28], [36], [87], TLR4 ligand lipopolysaccharide (LPS) [23], [24], [27] and the TLR7 ligands R837 and polyuridylic acid [38]. Similar to human DC, both porcine MoDC and blood cDC have been reported to be unreceptive to the TLR9 ligand CpG-ODN, when analysed for MHC class II and CD80/86 expression [58]. Nevertheless, MoDC express TLR9 mRNA [27], [38], and CpG-ODN can induce the mRNA of TLR4, TLR9, IFN-g and IL12 p35, as well as increased levels MHC class II as well as CD80/86 [27]. Such discrepancies between the studies may have been caused by sequence differences in the ODN employed or may reflect differences in the responsive status of the cells employed. For example, the relatively modest increase of CD80/86 and MHC class II expression on MoDC after TLR stimulation is synergistically enhanced in the presence of IFN-α [64]. In this study it was also shown that a full phenotypic maturation only occurred during antigen presentation to T lymphocytes. We have also observed that in contrast to MoDC, Flt3-ligand derived BMDC are clearly more responsiveness to a range of TLR ligands including TLR2, 3, 4, 7 and 9 (Guzylack-Piriou and Summerfield, unpublished data).
3.1.2. Cytokine responses to TLR ligands
TLR ligation can induce cytokine mRNA species for IL-10, IL-12p35, IL-13 and IFN-g in DC, although this depends on the TLR ligand employed [27]. While polyIC, LPS, LTA, and CpG induced the Th1 promoting cytokines IL12 and IFN-g, the Th2-like cytokines IL-10 and IL-13 were induced only by LPS and LTA (Table 3). Raymond et al. [27] also demonstrated that similar to human and mouse DC, the cytokine response of porcine DC can be modulated by cytokines. For example, IL-12p35 mRNA can be enhanced with TNF-α, IL-12 and IFN-γ and reduced with IL-10 treatment of DC. Along the same line, the Th1/Th2 cytokine profile will depend on the type of antigen encountered [88]. At the protein level MoDC have been reported to produce TNF-α and IL-6 after stimulation with poly(IC), LPS, OprI and Pam3Cys (both TLR2 ligands), while production of IL-10 and IL-12 has been difficult to detect by ELISA [34], [35], [75], [87]. Related to the stimulation by these specific TLR ligands is the cytokine response of MoDC to heat-inactivated Actinobacillus pleuropneumoniae in terms of IL-6, IL-10 and IL-12 secretion [26]. MoDC also produce type I IFN after stimulation with poly(IC) and mRNA transfection [28], [36], [87]. The latter is dependent on the secondary structure of the mRNA molecule forming dsRNA structures [36].
It is important to note that MoDC maturation and cytokine production is highly variable and subject to immunomodulation. Another example for this is the observation that RA has a potent synergistic effect on IL-6 secretion induced by TLR ligands [75]. This relates to the fact that the DC family has a high diversity to deal with the varying environments and signals it receives in vivo from the local tissue environment and from pathogens. With in vitro analyses, it is only possible to reproduce a small fraction of this diverse scene. Therefore, what we are observing in vitro is true for the conditions being created, but can not be taken as a general rule for all DC subsets under all conditions in vivo.
3.2. Response of pDC to TLR ligands
As with cDC, the pDC can also upregulate MHC class II and co-stimulatory molecules after in vitro culture [40] and when stimulated with TLR ligands [58]. However, the notable trait of pDC is their ability to produce INF-α Similar to the human and mouse immune system, porcine pDC are the most potent producers of INF-α after stimulation with certain PAMPs. These PAMPs are the CpG type A motifs [58] and TLR7/8 ligands such as R837 [89]. Such characteristics show a particularly close relationship to the human DC system [13]; pDC respond to TLR7 and 9 ligands, whereas cDC such as MoDC tend to recognize more TLR2-4 ligands. In contrast, murine DC and macrophages also respond well to TLR9 ligands, although it is again the pDC which produce large quantities of IFN-( [13]. Dependent on the stimulus, porcine pDC also produce large quantities of TNF-α, IL-6 and as mentioned above IL-12 [58], [89]. It is this IL-12 induction, which distinguishes porcine pDC from their human counterparts [13].
3.3. Antiviral responses of DC
The DC family is particularly effective at sensing viruses through cytosolic and endosomal PRR, which detect viral nucleic acid. Important cytosolic receptors include the dsRNA-dependent protein kinase R (PKR) and the RLR's RIG-I and MDA-5 [90]. Generally, such receptors recognize viral replication occurring in situ—being cytosolic, these PRR will detect the intermediates, which are also usually cytosolic. While RIG-I can sense 5′-triphosphorylated singlestranded RNA, MDA-5 appears to be more specific for dsRNA, but the fine specifity within the helicase system is not entirely clear [91]. Although these receptors are ubiquitously expressed, their important role in the interaction of cDC with viruses has been demonstrated [92]. This is different with the endosomal PRR, all members of the TLR family including TLR3, 7, 8 and 9, which are expressed only on cells playing a specialized role in innate immune responses such as DC. TLR3 represents a receptor for dsRNA, TLR7 and 8 for single-stranded RNA and TLR9 for CpG-motif containing DNA. TLR3 will not only sense viruses with dsRNA genomes but also endocytosed dsRNA replicative intermediates produced during the replicative cycle of singlestranded RNA viruses, released from dying cells in the vicinity.
As summarized in Table 4 , the studies with porcine cDC and pDC demonstrate that similar to human and mouse, pDC produce high levels of IFN type I to most viruses studied including classical swine fever virus, FMDV, influenza virus, lentiviral vectors (LV), pseudorabies virus (PRV) and TGEV, while such responses are absent or weak with cDC. The only exceptions described to date are the porcine circovirus 2, which can suppress IFN response in pDC [93], and Sendai virus which is a potent inducer of IFN type I in cDC [26].
Table 4.
DC interaction with viruses and IFN-α/β induction
| cDC |
pDC |
References | ||||
|---|---|---|---|---|---|---|
| Infection | Maturation | INF-α/β | Infection | INF-α/β | ||
| CSFV | ++ | +/- | supression | + | +++ | [57], [87], [97] |
| FMDV | (+)a | −/+b | + | + | ++/−c | [63], [109], [112],[110] |
| Influenza V | + | + | − | + | +++ | unpublished |
| LV vectord | + | + | − | + | +++ | [38] |
| PCV2 | (+)e | − | − | n.d.f | supression | [89], [93], [122] |
| PRRSV | + | ↓ | supression | n.d. | n.d. | [101], [102], [103], [104], [115] |
| PRV | n.d.b | n.d. | n.d. | n.d. | +++ | [89] |
| SV | n.d. | n.d. | + | n.d. | n.d. | [26] |
| TGEV | − | − | − | − | +++ | [40], [51], [63] |
Infection with transient or abortive replication.
Unpublished results (Guzylack-Piriou and Summerfield).
Stimulation strain-dependent or FMDV complexed with immune immunoglobulins.
HIV-derived VSV-G protein pseudotyped vector.
PCV2: persisting infection.
Not determined.
An important basis for the responsiveness of pDC to viruses is the expression of endosomal TLR7 and TLR9, which can be triggered by DNA and RNA viruses respectively independently of viral replication [94]. In addition, the constitutive expression of IRF7, the master regulator of type I IFN, represents a unique feature of pDC [13], [95].
A good example showing the importance of pDC recognition of viruses is the response seen with CSFV. This monocytotropic, haemorrhagic RNA virus replicates efficiently in cDC without apparently inducing their activation or maturation [87]. The lack of DC activation is not due to the absence of a trigger, because the virus generates a dsRNA intermediate in infected MoDC theoretically capable of stimulating RLRs. CSFV actively prevents the cDC response to dsRNA through its non-structural Npro protein targeting the IRF-3 pathway [96], on which cDC depend for induction of IFN [97]. In contrast, in pDC CSFV will induce IFN-( production [57]. As mentioned above, these cells do not rely on IRF-3 due to their high levels of constitutive IRF-7 [13]. The production of large quantities of IFN-( in the serum of CSFV-infected pigs [98], [99] presumably originating from pDC [99] indicates the importance of pDC for systemic IFN-( responses, particularly when cDC activities are impaired by the pathogen. In fact, a number of RNA viruses encode proteins interfering with cellular antiviral machinery and therefore prevent activation of cDC [100].
Also with porcine reproductive and respiratory syndrome virus (PRRSV), a productive infection of cDC has been observed [101], [102], [103], [104]. This apparently does not result in the secretion of type I IFN, although IFN mRNA is induced, indicating a block of the IFN system at the translational level [104]. Whether PRRSV can activate pDC has not yet been described.
In addition to the TLR-recognition of viral PAMPs, pDC possess other receptors to sense viruses. This has been demonstrated for TGEV, an RNA-genome coronavirus, which can activate pDC using a surface receptor interacting with the viral M glycoprotein [105]. Use of inactivated virus and subunit structures has demonstrated that this activation is independent of viral nucleic acid [106], excluding a role for TLR3 and TLR7. Moreover, mutation of the glycosylation site in the M protein yields a virus incapable of inducing pDC, but still capable of replication [107]. Also studies in our own laboratory support the conclusion of triggering through a cell surface receptor-inhibitors of endosomal acidification such as chloroquine and bafilomycin prevent CpG-induction, but not TGEV-induction of IFNa production by pDC [63]. Similar observations have been made with other viral proteins such as HIV-derived gp120 and human pDC [108].
Although porcine pDC like human pDC are highly efficient producers of IFNa and effective at sensing virus infections, not all viruses will activate pDC so efficiently. Nonenveloped viruses such as FMDV-an RNA virus of the Picornaviridae related to poliovirus and rhinoviruses—are less efficient to activate pDC. It should be noted that these viruses either fail to replicate in DC, or produce only an abortive infection [109], [110], [111]. Nevertheless, pDC can be efficiently activated by FMDV under particular conditions. In the presence of opsonizing factors such as virus-specific immunoglobulin (Ig), which mediate FcgRII-enhanced uptake of virions, pDC activation was observed-an event dependent on the presence of intact and active viral RNA [63]. Such an activity would provide important antiviral innate defences at a time early post-vaccination when the adaptive response had begun producing specific antibody, but is inadequate to protect the host from disease or virus replication. This function of pDC would have an additional advantageassisting cDC in promoting the development of an efficacious adaptive immune defence for protecting the host. FMDV can also infect cDC including skin DC and MoDC [109], [112], which results in low levels if IFN-β secretion.
4. Porcine DC and lymphocyte activation
Just as in vitro analyses cover only a proportion of likely events in vivo, focusing on phenotypic modulation of DC and cytokine profiles will reveal only part of the story. During immune defence development, these modulations of the DC serve a purpose beyond the direct attack on the pathogen by the DC. That additional purpose is promoting the functional interaction with the adaptive immune system.
4.1. Interaction of DC with T lymphocytes
The interaction between T lymphocytes and DC is a bilateral process. On one side there is the central role of DC in presenting antigen and stimulating T cells. This has been shown in several models including mixed leukocyte reactions [24], [26], superantigen presentation [23] as well as antigen specific T-cell restimulation [25], [75], [87], [113], [114] (see also Table 3). On the other side, T lymphocytes provide important signals to DC. With porcine MoDC cultures we have observed that after the co-culture of cytokine-matured DC with T cells in the presence of antigens, a further upregulation of MHC class II expression was obtained reaching levels clearly above those obtained with any stimuli in the absence of Tcells [64]. Interestingly, TNF-α pre-treatment of the DC was as efficient as TNF-α/IFN-α cocktails to sensitize the DC for this process. These in vitro observations indicate that MoDC maturation is a regulated multistep process. From a practical point of view this means that although TNF-α alone is not sufficient to induce MoDC maturation, the T-cell responses induced by TNF-α-treated DC can compensate to provide stimuli reaching those obtained with more potent maturation cocktails such as TNF-α/IFN-α or TLR ligands [64]. Moreover, the T-lymphocyte activity provides an additional advantage in that cocktails such as TNF-α/IFN-α, as well as those combined with TLR can have the drawback of “exhausting” the DC.
Similar to other species, it has been demonstrated that DC can modulate the type of T-cell response induced. For example, the Th1/Th2 profile will be influenced by the type of antigen presented as well as by the cytokine environment [88]. Another example of such modulation is the observation that cholera toxin-treated DC have the capacity to suppress T-cell proliferation [34]. This was associated with decreased MHC class II expression and increased IL-10 secretion of the DC and was reversible by addition of TNF-α suggesting an immunoregulatory process. PRRSV has also been described by several authors to modulate DC and monocytes towards reduced T-cell stimulatory capacity after in vitro infection [102], [103]. Also here reduced expression of MHC and co-stimulatory molecules together with increased IL-10 levels have been described [101], [102], [103], [115]. Such studies are valuable to understand viral pathogenesis but care must be taken to avoid any contamination of the cultures with mycoplasma as MoDC cultures apparently efficiently support mycoplasma growth, which can result in a potent antiproliferative activity [116].
DC not only determine the type of T-cell response but also their homing characteristics. As described in section “Mucosal DC”, MoDC treated with RA promote α4β7 and CCR9 expression, representing essential gut homing receptors [75].
4.2. Interaction of DC with B lymphocytes
Classically, B lymphocytes equipped with their surface Ig receptor will recognize native unprocessed antigen and would only require T-cell help for clonal expansion and differentiation into antibody producing cells. In this sense, B cells should show only an indirect requirement for APC such as cDC. Nevertheless, APC produce a number of cytokines, which have a direct stimulatory effect on B cells. These are classical cytokines such as IL-6, IL-10 and IFN-(/β, but also more recently identified cytokines such as the B-cell activating factor (BAFF) and a proliferation-inducing ligand (APRIL)-members of the tumour necrosis factor superfamily [9]. In addition, several studies also demonstrated the “delivery” of native unprocessed antigen by DC to B cells [5], [6], [7]. Our own studies with porcine DC in an in vitro model of FMDV-specific Ig synthesis demonstrated an important direct role of APC's during antigen-specific restimulation of immune B lymphocytes. Purified B cells produced virusspecific Ig only in the presence of Tcells and APC. Monocytes and MoDC but not pDC supported B-cell differentiation into antibody-secreting cells. While IL-2 could replace T-cells, addition of BAFF could compensate for a lack of APC. In fact, blocking of BAFF receptor abrogated the APC-derived help for B-cell responses [41]. In addition, DC also influence isotype switching. As mentioned above, RA-treated MoDC promote virus-specific IgA secretion in vitro [75].
Not surprisingly, similar to the interaction with T lymphocytes, the interplay of DC with B lymphocytes is also bilateral. An important role is certainly played by the “ménage à trois” of FcR expressed on DC, antibody and antigen. This permits an amplification of antigen uptake and presentation, and can also mediate efficient cross-presentation of antigen for stimulation of MHC class I-restricted T-cell responses. Furthermore, the FcR-system sensitizes DC for inflammatory and antiviral cytokine responses. One example is the response of pDC to FMDV mentioned above (Table 4). These pDC only respond by producing IFN-( to FMDV when the virus is complexed with antibodies [63]. Another example is with CSFV, where pDC sensitized with cytophilic antibodies show enhanced IFN-( production in response to lower virus quantities than when no cytophilic antibodies are present [57]. In both cases FcgRII is involved.
4.3. The advantages of the porcine model
Recent advances in the characterization of the porcine immune system, particularly in porcine DC biology, have permitted the use of the porcine model for many immunological studies. Although the library of reagents for such studies is still restricted compared to that for mouse and human studies, knowledge of porcine immunology is well advanced. With the unveiling of the sequence for the porcine genome, there will be clear advantages for using the pig. In particular, the MoDC model has a number of advantages and applicability. Large numbers of DC can be generated without killing the animal. For example, a typical figure of 30–70 million DC can be generated using monocytes isolated from 400 ml of blood. The facility to repeat blood sampling with the pig enables the use of these DC in antigen presentation assays, to monitor autologous T-cell responses in immunization experiments with outbred animals [113]. Moreover, with the MoDC being in an immature state, another advantage is the possibility to study DC maturation in response to cytokines, TLR ligands and infections.
Considering that DC are a rare cell type within the leukocyte populations, the large size of the pig, its lymphoid organs and the availability of larger volumes of blood together with repeated samplings offer an advantage allowing considerable immunological progress. In addition to this facility of recovering large volumes of blood regularly from the same animal, cannulation procedures for porcine lymph vessels at both peripheral and mucosal sites are now available. This approach allows us the much sought ability of studying DC migrating from peripheral sites over periods of several days [47], [56], a procedure not possible with humans and certainly cumbersome with mice considering their size and the quantities of material obtained. Moreover, the pig is more closely related to the human—both genetically and physiologically—when compared to mice. This is reflected by immunological similarities such as the PRR and their cellular distributions [58], [59]. Finally, the advantages which porcine immunology has to offer have gained a further boost with the advent of novel technologies such as RNA interference (RNAi) [38], which can be combined with the generation of transgenic pigs [117].
Acknowledgements
This work was supported by the Swiss State Secretariat for Education and Research Grants 97.0423, 99.0588, 00.0635, 00.0636, 02.0093 and 03.0519 which are linked to EU Projects PL97-3732, QLK2-CT-1999-00445, QLRT-2000- 01374, QLK2-CT-2001-01346, QLRT-2001-00825 and SSPECT- 2003-503603-IMPROCON, respectively. The Schweizerischer Nationalfonds also supported part of this work (Grant 3100-68237 and 310000-116800/1). We are grateful for the precious contributions of all present and former members of our laboratory.
References
- 1.Iwasaki A., Kelsall B.L. Localization of distinct Peyer's patch dendritic cell subsets and their recruitment by chemokines macrophage inflammatory protein (MIP)-3alpha, MIP-3beta, and secondary lymphoid organ chemokine. J Exp Med. 2000;191:1381–1394. doi: 10.1084/jem.191.8.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson M.J., Sancho D., Slack E.C., LeibundGut-Landmann S., Reis e Sousa C. Myeloid C-type lectins in innate immunity. Nat Immunol. 2006;7:1258–1265. doi: 10.1038/ni1417. [DOI] [PubMed] [Google Scholar]
- 3.Trinchieri G., Sher A. Cooperation of Toll-like receptor signals in innate immune defence. Nat Rev Immunol. 2007;7:179–190. doi: 10.1038/nri2038. [DOI] [PubMed] [Google Scholar]
- 4.Lee M.S., Kim Y.J. Signaling pathways downstream of patternrecognition receptors and their cross talk. Annu Rev Biochem. 2007;76:447–480. doi: 10.1146/annurev.biochem.76.060605.122847. [DOI] [PubMed] [Google Scholar]
- 5.Wykes M., Pombo A., Jenkins C., MacPherson G.G. Dendritic cells interact directly with naive B lymphocytes to transfer antigen and initiate class switching in a primary T-dependent response. J Immunol. 1998;161:1313–1319. [PubMed] [Google Scholar]
- 6.Dubois B., Caux C. Critical role of ITIM-bearing FcgammaR on DCs in the capture and presentation of native antigen to B cells. Immunity. 2005;23:463–464. doi: 10.1016/j.immuni.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Bergtold A., Desai D.D., Gavhane A., Clynes R. Cell surface recycling of internalized antigen permits dendritic cell priming of B cells. Immunity. 2005;23:503–514. doi: 10.1016/j.immuni.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Banchereau J., Briere F., Caux C., Davoust J., Lebecque S., Liu Y.J. Immunobiology of dendritic cells. Annu Rev Immunol. 2000;18:767–811. doi: 10.1146/annurev.immunol.18.1.767. [DOI] [PubMed] [Google Scholar]
- 9.MacLennan I., Vinuesa C. Dendritic cells, BAFF, and APRIL: innate players in adaptive antibody responses. Immunity. 2002;17:235–238. doi: 10.1016/s1074-7613(02)00398-9. [DOI] [PubMed] [Google Scholar]
- 10.Della C.M., Sivori S., Castriconi R., Marcenaro E., Moretta A. Pathogen-induced private conversations between natural killer and dendritic cells. Trends Microbiol. 2005;13:128–136. doi: 10.1016/j.tim.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 11.gli-Esposti M.A., Smyth M.J. Close encounters of different kinds: dendritic cells and NK cells take centre stage. Nat Rev Immunol. 2005;5:112–124. doi: 10.1038/nri1549. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig I.S., Geijtenbeek T.B., van Kooyk Y. Two way communication between neutrophils and dendritic cells. Curr Opin Pharmacol. 2006;6:408–413. doi: 10.1016/j.coph.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y.J. IPC: professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors. Annu Rev Immunol. 2005;23:275–306. doi: 10.1146/annurev.immunol.23.021704.115633. [DOI] [PubMed] [Google Scholar]
- 14.Fitzgerald-Bocarsly P. Human natural interferon-alpha producing cells. Pharmacol Ther. 1993;60:39–62. doi: 10.1016/0163-7258(93)90021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Pucchio T., Chatterjee B., Smed-Sorensen A., Clayton S., Palazzo A., Montes M. Direct proteasome-independent cross-presentation of viral antigen by plasmacytoid dendritic cells on major histocompatibility complex class I. Nat Immunol. 2008;9:551–557. doi: 10.1038/ni.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Young L.J., Wilson N.S., Schnorrer P., Mount A., Lundie R.J., La Gruta N.L. Dendritic cell preactivation impairs MHC class II presentation of vaccines and endogenous viral antigens. Proc Natl Acad Sci USA. 2007;104:17753–17758. doi: 10.1073/pnas.0708622104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villadangos J.A., Schnorrer P. Intrinsic and cooperative antigenpresenting functions of dendritic-cell subsets in vivo. Nat Rev Immunol. 2007;7:543–555. doi: 10.1038/nri2103. [DOI] [PubMed] [Google Scholar]
- 18.West M.A., Wallin R.P., Matthews S.P., Svensson H.G., Zaru R., Ljunggren H.G. Enhanced dendritic cell antigen capture via Toll-like receptor-induced actin remodeling. Science. 2004;305:1153–1157. doi: 10.1126/science.1099153. [DOI] [PubMed] [Google Scholar]
- 19.Reis e Sousa C. Dendritic cells in a mature age. Nat Rev Immunol. 2006;6:476–483. doi: 10.1038/nri1845. [DOI] [PubMed] [Google Scholar]
- 20.Lunney J.K. Characterization of swine leukocyte differentiation antigens. Immunol Today. 1993;14:147–148. doi: 10.1016/0167-5699(93)90227-C. [DOI] [PubMed] [Google Scholar]
- 21.Saalmuller A. Characterization of swine leukocyte differentiation antigens. Immunol Today. 1996;17:352–354. doi: 10.1016/S0167-5699(96)90273-X. [DOI] [PubMed] [Google Scholar]
- 22.Haverson K., Saalmuller A., Chen Z., Huang C.A., Simon A., Seebach J. Summary of the first round analyses of the Third International Workshop on Swine Leukocyte Differentiation Antigens. Vet Immunol Immunopathol. 2001;80:25–34. doi: 10.1016/s0165-2427(01)00291-4. [DOI] [PubMed] [Google Scholar]
- 23.Carrasco C.P., Rigden R.C., Schaffner R., Gerber H., Neuhaus V., Inumaru S. Porcine dendritic cells generated in vitro: morphological, phenotypic and functional properties. Immunology. 2001;104:175–184. doi: 10.1046/j.0019-2805.2001.01299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paillot R., Laval F., Audonnet J.C., Andreoni C., Juillard V. Functional and phenotypic characterization of distinct porcine dendritic cells derived from peripheral blood monocytes. Immunology. 2001;102:396–404. doi: 10.1046/j.1365-2567.2001.01200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balmelli C., Ruggli N., McCullough K., Summerfield A. Fibrocytes are potent stimulators of anti-virus cytotoxic T cells. J Leukoc Biol. 2005;77:923–933. doi: 10.1189/jlb.1204701. [DOI] [PubMed] [Google Scholar]
- 26.Johansson E., Domeika K., Berg M., Alm G.V., Fossum C. Characterisation of porcine monocyte-derived dendritic cells according to their cytokine profile. Vet Immunol Immunopathol. 2003;91:183–197. doi: 10.1016/s0165-2427(02)00310-0. [DOI] [PubMed] [Google Scholar]
- 27.Raymond C.R., Wilkie B.N. Toll-like receptor, MHC II, B7 and cytokine expression by porcine monocytes and monocytederived dendritic cells in response to microbial pathogenassociated molecular patterns. Vet Immunol Immunopathol. 2005;107:235–247. doi: 10.1016/j.vetimm.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 28.Bautista E.M., Nfon C., Ferman G.S., Golde W.T. IL-13 replaces IL-4 in development of monocyte derived dendritic cells (MoDC) of swine. Vet Immunol Immunopathol. 2007;115:56–67. doi: 10.1016/j.vetimm.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Foss D.L., Bennaars A.M., Pennell C.A., Moody M.D., Murtaugh M.P. Differentiation of porcine dendritic cells by granulocytemacrophage colony-stimulating factor expressed in Pichia pastoris. Vet Immunol Immunopathol. 2003;91:205–215. doi: 10.1016/s0165-2427(03)00002-3. [DOI] [PubMed] [Google Scholar]
- 30.Chamorro S., Revilla C., Gomez N., Alvarez B., Alonso F., Ezquerra A. In vitro differentiation of porcine blood CD163− and CD163+ monocytes into functional dendritic cells. Immunobiology. 2004;209:57–65. doi: 10.1016/j.imbio.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Miranda de Carvalho C., Bonnefont-Rebeix C., Rigal D., Chabanne L. Dendritic cells in different animal species: an overview. Pathol Biol (Paris) 2006;54:85–93. doi: 10.1016/j.patbio.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Alvarez B., Sanchez C., Bullido R., Marina A., Lunney J., Alonso F. A porcine cell surface receptor identified by monoclonal antibodies to SWC3 is a member of the signal regulatory protein family and associates with protein-tyrosine phosphatase SHP-1. Tissue Antigens. 2000;55:342–351. doi: 10.1034/j.1399-0039.2000.550408.x. [DOI] [PubMed] [Google Scholar]
- 33.Summerfield A., McCullough K.C. Porcine bone marrow myeloid cells: phenotype and adhesion molecule expression. J Leukoc Biol. 1997;62:176–185. doi: 10.1002/jlb.62.2.176. [DOI] [PubMed] [Google Scholar]
- 34.Bimczok D., Rau H., Wundrack N., Naumann M., Rothkotter H.J., McCullough K. Cholera toxin promotes the generation of semi-mature porcine monocyte-derived dendritic cells that are unable to stimulate T cells. Vet Res. 2007;38:597–612. doi: 10.1051/vetres:2007020. [DOI] [PubMed] [Google Scholar]
- 35.Rau H., Revets H., Cornelis P., Titzmann A., Ruggli N., McCullough K.C. Efficacy and functionality of lipoprotein OprI from Pseudomonas aeruginosa as adjuvant for a subunit vaccine against classical swine fever. Vaccine. 2006;24:4757–4768. doi: 10.1016/j.vaccine.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 36.Ceppi M., Ruggli N., Tache V., Gerber H., McCullough K.C., Summerfield A. Double-stranded secondary structures on mRNA induce type I interferon (IFN alpha/beta) production and maturation of mRNA-transfected monocyte-derived dendritic cells. J Gene Med. 2005;7:452–465. doi: 10.1002/jgm.685. [DOI] [PubMed] [Google Scholar]
- 37.Summerfield A., Horn M.P., Lozano G., Carrasco C.P., Atze K., McCullough K. C-kit positive porcine bone marrow progenitor cells identified and enriched using recombinant stem cell factor. J Immunol Methods. 2003;280:113–123. doi: 10.1016/s0022-1759(03)00273-4. [DOI] [PubMed] [Google Scholar]
- 38.Alves M.P., Neuhaus V., Guzylack-Piriou L., Ruggli N., McCullough K.C., Summerfield A. Toll-like receptor 7 and MyD88 knockdown by lentivirus-mediated RNA interference to porcine dendritic cell subsets. Gene Ther. 2007;14:836–844. doi: 10.1038/sj.gt.3302930. [DOI] [PubMed] [Google Scholar]
- 39.Onai N., Obata-Onai A., Schmid M.A., Ohteki T., Jarrossay D., Manz M.G. Identification of clonogenic common Flt3+M-CSFR+ plasmacytoid and conventional dendritic cell progenitors in mouse bone marrow. Nat Immunol. 2007;8:1207–1216. doi: 10.1038/ni1518. [DOI] [PubMed] [Google Scholar]
- 40.Summerfield A., Guzylack-Piriou L., Schaub A., Carrasco C.P., Tache V., Charley B. Porcine peripheral blood dendritic cells and natural interferon-producing cells. Immunology. 2003;110:440–449. doi: 10.1111/j.1365-2567.2003.01755.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bergamin F., Vincent I.E., Summerfield A., McCullough K.C. Essential role of antigen-presenting cell-derived BAFF for antibody responses. Eur J Immunol. 2007;37:3122–3130. doi: 10.1002/eji.200636791. [DOI] [PubMed] [Google Scholar]
- 42.Rau H., Revets H., Balmelli C., McCullough K.C., Summerfield A. Immunological properties of recombinant classical swine fever virus NS3 protein in vitro and in vivo. Vet Res. 2006;37:155–168. doi: 10.1051/vetres:2005049. [DOI] [PubMed] [Google Scholar]
- 43.Piersma S.J., Leenaars M.P., Guzylack-Piriou L., Summerfield A., Hendriksen C.F., McCullough K.C. An in vitro immune response model to determine tetanus toxoid antigen (vaccine) specific immunogenicity: Selection of sensitive assay criteria. Vaccine. 2006 doi: 10.1016/j.vaccine.2006.01.061. [DOI] [PubMed] [Google Scholar]
- 44.Chamorro S., Revilla C., Alvarez B., Alonso F., Ezquerra A., Dominguez J. Phenotypic and functional heterogeneity of porcine blood monocytes and its relation with maturation. Immunology. 2005;114:63–71. doi: 10.1111/j.1365-2567.2004.01994.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sanchez C., Domenech N., Vazquez J., Alonso F., Ezquerra A., Dominguez J. The porcine 2A10 antigen is homologous to human CD163 and related to macrophage differentiation. J Immunol. 1999;162:5230–5237. [PubMed] [Google Scholar]
- 46.Haverson K., Singha S., Stokes C.R., Bailey M. Professional and non-professional antigen-presenting cells in the porcine small intestine. Immunology. 2000;101:492–500. doi: 10.1046/j.1365-2567.2000.00128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bimczok D., Sowa E.N., Faber-Zuschratter H., Pabst R., Rothkotter H.J. Site-specific expression of CD11b and SIRPalpha (CD172a) on dendritic cells: implications for their migration patterns in the gut immune system. Eur J Immunol. 2005;35:1418–1427. doi: 10.1002/eji.200425726. [DOI] [PubMed] [Google Scholar]
- 48.Zhang W., Wen K., Azevedo M.S., Gonzalez A., Saif L.J., Li G. Lactic acid bacterial colonization and human rotavirus infection influence distribution and frequencies of monocytes/ macrophages and dendritic cells in neonatal gnotobiotic pigs. Vet Immunol Immunopathol. 2008;121:222–231. doi: 10.1016/j.vetimm.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jamin A., Gorin S., Le Potier M.F., Kuntz-Simon G. Characterization of conventional and plasmacytoid dendritic cells in swine secondary lymphoid organs and blood. Vet Immunol Immunopathol. 2006;114:224–237. doi: 10.1016/j.vetimm.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 50.Dominguez J., Alvarez B., Alonso F., Thacker E., Haverson K., McCullough K. Workshop studies on monoclonal antibodies in the myeloid panel with CD11 specificity. Vet Immunol Immunopathol. 2001;80:111–119. doi: 10.1016/s0165-2427(01)00286-0. [DOI] [PubMed] [Google Scholar]
- 51.Charley B., Lavenant L. Characterization of blood mononuclear cells producing IFN alpha following induction by coronavirus-infected cells (porcine transmissible gastroenteritis virus) Res Immunol. 1990;141:141–151. doi: 10.1016/0923-2494(90)90133-J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Splichal I., Bonneau M., Charley B. Ontogeny of interferon alpha secreting cells in the porcine fetal hematopoietic organs. Immunol Lett. 1994;43:203–208. doi: 10.1016/0165-2478(94)90224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Splichal I., Rehakova Z., Sinkora M., Sinkora J., Trebichavsky I., Laude H. In vivo study of interferon-alpha-secreting cells in pig foetal lymphohaematopoietic organs following in utero TGEV coronavirus injection. Res Immunol. 1997;148:247–256. doi: 10.1016/S0923-2494(97)80866-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Riffault S., Carrat C., Besnardeau L., La Bonnardiere C., Charley B. In vivo induction of interferon-alpha in pig by noninfectious coronavirus: tissue localization and in situ phenotypic characterization of interferon-alpha-producing cells. J Gen Virol. 1997;78(Part 10):2483–2487. doi: 10.1099/0022-1317-78-10-2483. [DOI] [PubMed] [Google Scholar]
- 55.Riffault S., Carrat C., van Reeth K., Pensaert M., Charley B. Interferon-alpha-producing cells are localized in gut-associated lymphoid tissues in transmissible gastroenteritis virus (TGEV) infected piglets. Vet Res. 2001;32:71–79. doi: 10.1051/vetres:2001111. [DOI] [PubMed] [Google Scholar]
- 56.Pascale F., Contreras V., Bonneau M., Epardaud M., Niborsky V., Riffault S. Plasmacytoid dendritic cells migrate in afferent skin lymph. J Immunol. 2008;180:5963–5972. doi: 10.4049/jimmunol.180.9.5963. [DOI] [PubMed] [Google Scholar]
- 57.Balmelli C., Vincent I.E., Rau H., Guzylack-Piriou L., McCullough K., Summerfield A. FcgammaRII-dependent sensitisation of natural interferon-producing cells for viral infection and interferon-alpha responses. Eur J Immunol. 2005;35:2406–2415. doi: 10.1002/eji.200525998. [DOI] [PubMed] [Google Scholar]
- 58.Guzylack-Piriou L., Balmelli C., McCullough K.C., Summerfield A. Type-A CpG oligonucleotides activate exclusively porcine natural interferon-producing cells to secrete interferonalpha, tumour necrosis factor-alpha and interleukin-12. Immunology. 2004;112:28–37. doi: 10.1111/j.1365-2567.2004.01856.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hochrein H., Wagner H. Of men, mice and pigs: looking at their plasmacytoid dendritic cells [corrected] Immunology. 2004;112:26–27. doi: 10.1111/j.1365-2567.2004.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Makala L.H., Haverson K., Stokes C.R., Bailey M., Bland P.W. Isolation and characterisation of pig Peyer's patch dendritic cells. Vet Immunol Immunopathol. 1998;61:67–81. doi: 10.1016/s0165-2427(97)00125-6. [DOI] [PubMed] [Google Scholar]
- 61.Bimczok D., Post A., Tschernig T., Rothkotter H.J. Phenotype and distribution of dendritic cells in the porcine small intestinal and tracheal mucosa and their spatial relationship to epithelial cells. Cell Tissue Res. 2006;325:461–468. doi: 10.1007/s00441-006-0195-3. [DOI] [PubMed] [Google Scholar]
- 62.Bautista E.M., Gregg D., Golde W.T. Characterization and functional analysis of skin-derived dendritic cells from swine without a requirement for in vitro propagation. Vet Immunol Immunopathol. 2002;88:131–148. doi: 10.1016/s0165-2427(02)00152-6. [DOI] [PubMed] [Google Scholar]
- 63.Guzylack-Piriou L., Bergamin F., Gerber M., McCullough K.C., Summerfield A. Plasmacytoid dendritic cell activation by foot-and-mouth disease virus requires immune complexes. Eur J Immunol. 2006;36:1674–1683. doi: 10.1002/eji.200635866. [DOI] [PubMed] [Google Scholar]
- 64.Guzylack-Piriou L., Piersma S., McCullough K., Summerfield A. Role of natural interferon-producing cells and T lymphocytes in porcine monocyte-derived dendritic cell maturation. Immunology. 2006;118:78–87. doi: 10.1111/j.1365-2567.2006.02343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Huang F.P., Platt N., Wykes M., Major J.R., Powell T.J., Jenkins C.D. A discrete subpopulation of dendritic cells transports apoptotic intestinal epithelial cells to T cell areas of mesenteric lymph nodes. J Exp Med. 2000;191:435–444. doi: 10.1084/jem.191.3.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu L., Zhang M., Jenkins C., MacPherson G.G. Dendritic cell heterogeneity in vivo: two functionally different dendritic cell populations in rat intestinal lymph can be distinguished by CD4 expression. J Immunol. 1998;161:1146–1155. [PubMed] [Google Scholar]
- 67.Howard C.J., Sopp P., Brownlie J., Kwong L.S., Parsons K.R., Taylor G. Identification of two distinct populations of dendritic cells in afferent lymph that vary in their ability to stimulate Tcells. J Immunol. 1997;159:5372–5382. [PubMed] [Google Scholar]
- 68.Epardaud M., Bonneau M., Payot F., Cordier C., Megret J., Howard C. Enrichment for a CD26hi SIRP—subset in lymph dendritic cells from the upper aero-digestive tract. J Leukoc Biol. 2004;76:553–561. doi: 10.1189/jlb.0404223. [DOI] [PubMed] [Google Scholar]
- 69.Latour S., Tanaka H., Demeure C., Mateo V., Rubio M., Brown E.J. Bidirectional negative regulation of human T and dendritic cells by CD47 and its cognate receptor signalregulator protein-alpha: down-regulation of IL-12 responsiveness and inhibition of dendritic cell activation. J Immunol. 2001;167:2547–2554. doi: 10.4049/jimmunol.167.5.2547. [DOI] [PubMed] [Google Scholar]
- 70.Iwasaki A. Mucosal dendritic cells. Annu Rev Immunol. 2007;25:381–418. doi: 10.1146/annurev.immunol.25.022106.141634. [DOI] [PubMed] [Google Scholar]
- 71.McGhee J.R., Kunisawa J., Kiyono H. Gut lymphocyte migration: we are halfway ‘home’. Trends Immunol. 2007;28:150–153. doi: 10.1016/j.it.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 72.Mora J.R., Iwata M., Eksteen B., Song S.Y., Junt T., Senman B. Generation of gut-homing IgA-secreting B cells by intestinal dendritic cells. Science. 2006;314:1157–1160. doi: 10.1126/science.1132742. [DOI] [PubMed] [Google Scholar]
- 73.Sun C.M., Hall J.A., Blank R.B., Bouladoux N., Oukka M., Mora J.R. Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 Treg cells via retinoic acid. J Exp Med. 2007;204:1775–1785. doi: 10.1084/jem.20070602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mucida D., Park Y., Kim G., Turovskaya O., Scott I., Kronenberg M. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317:256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- 75.Saurer L., McCullough K.C., Summerfield A. In vitro induction of mucosa-type dendritic cells by all-trans retinoic acid. J Immunol. 2007;179:3504–3514. doi: 10.4049/jimmunol.179.6.3504. [DOI] [PubMed] [Google Scholar]
- 76.Wendland M., Czeloth N., Mach N., Malissen B., Kremmer E., Pabst O. CCR9 is a homing receptor for plasmacytoid dendritic cells to the small intestine. Proc Natl Acad Sci USA. 2007;104:6347–6352. doi: 10.1073/pnas.0609180104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Salmon H., Johnson I., Germana S., Haller G.W., Sachs D.H., Leguern C. Dendritic cells enriched from swine thymus coexpress CD1, CD2 and major histocompatibility complex class II and actively stimulate alloreactive T lymphocytes. Scand J Immunol. 2000;52:164–172. doi: 10.1046/j.1365-3083.2000.00768.x. [DOI] [PubMed] [Google Scholar]
- 78.Croizet K., Rabilloud R., Kostrouch Z., Nicolas J.F., Rousset B. Culture of dendritic cells from a nonlymphoid organ, the thyroid gland: evidence for TNFalpha-dependent phenotypic changes of thyroid-derived dendritic cells. Lab Invest. 2000;80:1215–1225. doi: 10.1038/labinvest.3780129. [DOI] [PubMed] [Google Scholar]
- 79.Bucala R., Spiegel L.A., Chesney J., Hogan M., Cerami A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol Med. 1994;1:71–81. [PMC free article] [PubMed] [Google Scholar]
- 80.Chesney J., Bacher M., Bender A., Bucala R. The peripheral blood fibrocyte is a potent antigen-presenting cell capable of priming naive T cells in situ. Proc Natl Acad Sci USA. 1997;94:6307–6312. doi: 10.1073/pnas.94.12.6307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Abe R., Donnelly S.C., Peng T., Bucala R., Metz C.N. Peripheral blood fibrocytes: differentiation pathway and migration to wound sites. J Immunol. 2001;166:7556–7562. doi: 10.4049/jimmunol.166.12.7556. [DOI] [PubMed] [Google Scholar]
- 82.Balmelli C., Alves M.P., Steiner E., Zingg D., Peduto N., Ruggli N. Responsiveness of fibrocytes to Toll-like receptor danger signals. Immunobiology. 2007;212:693–699. doi: 10.1016/j.imbio.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 83.Chesney J., Metz C., Stavitsky A.B., Bacher M., Bucala R. Regulated production of type I collagen and inflammatory cytokines by peripheral blood fibrocytes. J Immunol. 1998;160:419–425. [PubMed] [Google Scholar]
- 84.Grab D.J., Lanners H., Martin L.N., Chesney J., Cai C., Adkisson H.D. Interaction of Borrelia burgdorferi with peripheral blood fibrocytes, antigen-presenting cells with the potential for connective tissue targeting. Mol Med. 1999;5:46–54. [PMC free article] [PubMed] [Google Scholar]
- 85.Moser M. Dendritic cells in immunity and tolerance—do they display opposite functions? Immunity. 2003;19:5–8. doi: 10.1016/s1074-7613(03)00182-1. [DOI] [PubMed] [Google Scholar]
- 86.Matzinger P. The danger model: a renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 87.Carrasco C.P., Rigden R.C., Vincent I.E., Balmelli C., Ceppi M., Bauhofer O. Interaction of classical swine fever virus with dendritic cells. J Gen Virol. 2004;85:1633–1641. doi: 10.1099/vir.0.19716-0. [DOI] [PubMed] [Google Scholar]
- 88.Raymond C.R., Sidahmed A.M., Wilkie B.N. Effects of antigen and recombinant porcine cytokines on pig dendritic cell cytokine expression in vitro. Vet Immunol Immunopathol. 2006;111:175–185. doi: 10.1016/j.vetimm.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 89.Vincent I.E., Balmelli C., Meehan B., Allan G., Summerfield A., McCullough K.C. Silencing of natural interferon producing cell activation by porcine circovirus type 2 DNA. Immunology. 2007;120:47–56. doi: 10.1111/j.1365-2567.2006.02476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mogensen T.H., Paludan S.R. Reading the viral signature by Tolllike receptors and other pattern recognition receptors. J Mol Med. 2005;83:180–192. doi: 10.1007/s00109-004-0620-6. [DOI] [PubMed] [Google Scholar]
- 91.Schlee M., Barchet W., Hornung V., Hartmann G. Beyond doublestranded RNA-type I IFN induction by 3pRNA and other viral nucleic acids. Curr Top Microbiol Immunol. 2007;316:207–230. doi: 10.1007/978-3-540-71329-6_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Eisenacher K., Steinberg C., Reindl W., Krug A. The role of viral nucleic acid recognition in dendritic cells for innate and adaptive antiviral immunity. Immunobiology. 2007;212:701–714. doi: 10.1016/j.imbio.2007.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vincent I.E., Carrasco C.P., Guzylack-Piriou L., Herrmann B., McNeilly F., Allan G.M. Subset-dependent modulation of dendritic cell activity by circovirus type 2. Immunology. 2005;115:388–398. doi: 10.1111/j.1365-2567.2005.02165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fitzgerald-Bocarsly P. Natural interferon-alpha producing cells: the plasmacytoid dendritic cells. Biotechniques. 2002;22(Suppl.16–20):24–29. [PubMed] [Google Scholar]
- 95.Honda K., Yanai H., Negishi H., Asagiri M., Sato M., Mizutani T. IRF-7 is the master regulator of type-I interferondependent immune responses. Nature. 2005;434:772–777. doi: 10.1038/nature03464. [DOI] [PubMed] [Google Scholar]
- 96.Bauhofer O., Summerfield A., Sakoda Y., Tratschin J.D., Hofmann M.A., Ruggli N. Classical swine fever virus Npro interacts with interferon regulatory factor 3 and induces its proteasomal degradation. J Virol. 2007;81:3087–3096. doi: 10.1128/JVI.02032-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bauhofer O., Summerfield A., McCullough K.C., Ruggli N. Role of double-stranded RNA and N(pro) of classical swine fever virus in the activation of monocyte-derived dendritic cells. Virology. 2005;343:93–105. doi: 10.1016/j.virol.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 98.Summerfield A., Alves M., Ruggli N., de Bruin M.G., McCullough K.C. High IFN-alpha responses associated with depletion of lymphocytes and natural IFN-producing cells during classical swine fever. J Interferon Cytokine Res. 2006;26:248–255. doi: 10.1089/jir.2006.26.248. [DOI] [PubMed] [Google Scholar]
- 99.Jamin A., Gorin S., Cariolet R., Le Potier M.F., Kuntz-Simon G. Classical swine fever virus induces activation of plasmacytoid and conventional dendritic cells in tonsil, blood, and spleen of infected pigs. Vet Res. 2008;39:7. doi: 10.1051/vetres:2007045. [DOI] [PubMed] [Google Scholar]
- 100.Levy D.E., Garcia-Sastre A. The virus battles: IFN induction of the antiviral state and mechanisms of viral evasion. Cytokine Growth Factor Rev. 2001;12:143–156. doi: 10.1016/s1359-6101(00)00027-7. [DOI] [PubMed] [Google Scholar]
- 101.Chang HC, Peng YT, Chang HL, Chaung HC, Chung WB. Phenotypic and functional modulation of bone marrowderived dendritic cells by porcine reproductive and respiratory syndrome virus. Vet Microbiol 2007. [DOI] [PubMed]
- 102.Wang X., Eaton M., Mayer M., Li H., He D., Nelson E. Porcine reproductive and respiratory syndrome virus productively infects monocyte-derived dendritic cells and compromises their antigen-presenting ability. Arch Virol. 2007;152:289–303. doi: 10.1007/s00705-006-0857-1. [DOI] [PubMed] [Google Scholar]
- 103.Charerntantanakul W., Platt R., Roth J.A. Effects of porcine reproductive and respiratory syndrome virus-infected antigen- presenting cells on Tcell activation and antiviral cytokine production. Viral Immunol. 2006;19:646–661. doi: 10.1089/vim.2006.19.646. [DOI] [PubMed] [Google Scholar]
- 104.Loving C.L., Brockmeier S.L., Sacco R.E. Differential type I interferon activation and susceptibility of dendritic cell populations to porcine arterivirus. Immunology. 2007;120:217–229. doi: 10.1111/j.1365-2567.2006.02493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Baudoux P., Carrat C., Besnardeau L., Charley B., Laude H. Coronavirus pseudoparticles formed with recombinant M and E proteins induce alpha interferon synthesis by leukocytes. J Virol. 1998;72:8636–8643. doi: 10.1128/jvi.72.11.8636-8643.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Baudoux P., Besnardeau L., Carrat C., Rottier P., Charley B., Laude H. Interferon alpha inducing property of coronavirus particles and pseudoparticles. Adv Exp Med Biol. 1998;440:377–386. doi: 10.1007/978-1-4615-5331-1_49. [DOI] [PubMed] [Google Scholar]
- 107.Laude H., Gelfi J., Lavenant L., Charley B. Single amino acid changes in the viral glycoprotein M affect induction of alpha interferon by the coronavirus transmissible gastroenteritis virus. J Virol. 1992;66:743–749. doi: 10.1128/jvi.66.2.743-749.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Del Corno M., Gauzzi M.C., Penna G., Belardelli F., Adorini L., Gessani S. Human immunodeficiency virus type 1 gp120 and other activation stimuli are highly effective in triggering alpha interferon and CC chemokine production in circulating plasmacytoid but not myeloid dendritic cells. J Virol. 2005;79:12597–12601. doi: 10.1128/JVI.79.19.12597-12601.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bautista E.M., Ferman G.S., Gregg D., Brum M.C., Grubman M.J., Golde W.T. Constitutive expression of alpha interferon by skin dendritic cells confers resistance to infection by foot-andmouth disease virus. J Virol. 2005;79:4838–4847. doi: 10.1128/JVI.79.8.4838-4847.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Harwood L., Gerber H., Sobrino F., Summerfield A., McCullough K. Dendritic cells internalisation of foot-and-mouth disease virus: influence of heparin sulphate binding on virus uptake and immune response induction. J Virol. 2008;82:6379–6394. doi: 10.1128/JVI.00021-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Summerfield A, Guzylack-Piriou L, Harwood L, McCullough K. Innate immune responses against foot-and-mouth disease virus: current understanding and future directions. Vet Immunol Immunopathol, 2008, in press. [DOI] [PubMed]
- 112.Nfon C.K., Ferman G.S., Toka F.N., Gregg D.A., Golde W.T. Interferon-alpha production by swine dendritic cells is inhibited during acute infection with foot-and-mouth disease virus. Viral Immunol. 2008;21:68–77. doi: 10.1089/vim.2007.0097. [DOI] [PubMed] [Google Scholar]
- 113.Piras F., Bollard S., Laval F., Joisel F., Reynaud G., Charreyre C. Porcine reproductive and respiratory syndrome (PRRS) virus-specific interferon-gamma(+) T-cell responses after PRRS virus infection or vaccination with an inactivated PRRS vaccine. Viral Immunol. 2005;18:381–389. doi: 10.1089/vim.2005.18.381. [DOI] [PubMed] [Google Scholar]
- 114.Ceppi M., de Bruin M.G., Seuberlich T., Balmelli C., Pascolo S., Ruggli N. Identification of classical swine fever virus protein E2 as a target for cytotoxic T cells by using mRNAtransfected antigen-presenting cells. J Gen Virol. 2005;86:2525–2534. doi: 10.1099/vir.0.80907-0. [DOI] [PubMed] [Google Scholar]
- 115.Flores-Mendoza L, Silva-Campa E, Resendiz M, Osorio FA, Hernandez J. Porcine reproductive and respiratory syndrome virus (PRRSV) infects mature porcine dendritic cells and upregulates IL-10 production. Clin Vaccine Immunol 2008. [DOI] [PMC free article] [PubMed]
- 116.Alves M.P., Carrasco C.P., Balmelli C., Ruggli N., McCullough K.C., Summerfield A. Mycoplasma contamination and viral immunomodulatory activity: dendritic cells open Pandora's box. Immunol Lett. 2007;110:101–109. doi: 10.1016/j.imlet.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 117.Hofmann A., Kessler B., Ewerling S., Weppert M., Vogg B., Ludwig H. Efficient transgenesis in farm animals by lentiviral vectors. EMBO Rep. 2003;4:1054–1060. doi: 10.1038/sj.embor.7400007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McCullough K.C., Schaffner R., Natale V., Kim Y.B., Summerfield A. Phenotype of porcine monocytic cells: modulation of surface molecule expression upon monocyte differentiation into macrophages. Vet Immunol Immunopathol. 1997;58:265–275. doi: 10.1016/s0165-2427(97)00045-7. [DOI] [PubMed] [Google Scholar]
- 119.Chun T., Wang K., Zuckermann F.A., Gaskins H.R. Molecular cloning and characterization of a novel CD1 gene from the pig. J Immunol. 1999;162:6562–6571. [PubMed] [Google Scholar]
- 120.Rigden R.C., Carrasco C.P., Barnett P.V., Summerfield A., McCullough K.C. Innate immune responses following emergency vaccination against foot-and-mouth disease virus in pigs. Vaccine. 2003;21:1466–1477. doi: 10.1016/s0264-410x(02)00663-1. [DOI] [PubMed] [Google Scholar]
- 121.Bimczok D., Doll S., Rau H., Goyarts T., Wundrack N., Naumann M. The Fusarium toxin deoxynivalenol disrupts phenotype and function of monocyte-derived dendritic cells in vivo and in vitro. Immunobiology. 2007;212:655–666. doi: 10.1016/j.imbio.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 122.Vincent I.E., Carrasco C.P., Herrmann B., Meehan B.M., Allan G.M., Summerfield A. Dendritic cells harbor infectious porcine circovirus type 2 in the absence of apparent cell modulation or replication of the virus. J Virol. 2003;77:13288–13300. doi: 10.1128/JVI.77.24.13288-13300.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]