Abstract
BACKGROUND AND AIMS:
Eleven million unauthorized immigrants reside in the United States and may account for 3% of deceased organ donors. Recently introduced federal and state legislation propose to address access to organ transplantation among unauthorized immigrants. The national landscape of liver transplantation (LT) for unauthorized immigrants is unknown.
APPROACH AND RESULTS:
We included all US LT recipients between March 2012 and December 2018 who were linked to Pew Center of Research data to estimate the population of unauthorized immigrants in each US state and by country of origin, based on US Census data. We categorized patients as unauthorized immigrants versus US citizens/residents. The main outcome measures were (1) the proportion of LTs performed for unauthorized immigrants compared with the proportion of unauthorized immigrants among total population in each US state and (2) graft failure and death post-LT. Of 43,192 LT recipients, 43,026 (99.6%) were US citizens/residents and 166 (0.4%) were unauthorized immigrants. Among unauthorized immigrants, most LTs were performed in California (47%) and New York (18%). The absolute difference in proportion of LTs performed for unauthorized immigrants compared with the proportion of unauthorized immigrants among the total population differed among states, ranging from +20% in California to −12% in Texas. The most common countries of birth among LT recipients who were unauthorized immigrants were Mexico (52%), Guatemala (7%), China (6%), El Salvador (5%), and India (5%). In competing risk analysis, unauthorized immigration status (vs. US citizens/residents) was associated with a similar risk of graft failure (subdistribution hazard ratio [sHR] 0.74; 95% confidence interval [CI], 0.40–1.34; P = 0.38) and death (sHR 0.68; 95% CI, 0.36–1.29; P = 0.23).
CONCLUSIONS:
LT for unauthorized immigrants is rare, and disparities in access to LT by state are present. Patient and graft survival among unauthorized immigrants is comparable with citizens/residents.
There are an estimated 11 million unauthorized immigrants residing in the United States.(1,2) In Europe, the population of unauthorized immigrants (also termed illegal migrants in Europe) peaked at approximately 2.2 million in 2015.(3) The rights of unauthorized immigrants to health care differ across countries and can be a divisive political issue. In the field of liver transplantation (LT) in the United States, there is currently no specific guidance set by the United Network for Organ Sharing (UNOS) regarding access to LT for unauthorized immigrants, and LT centers are allowed to set their own policies. Studies focused on LT or any medical condition for unauthorized immigrants are sparse, which is related in part to difficulties identifying such patients in medical registries.
Unauthorized immigrants, also termed illegal aliens in US federal statutes, are defined by the Department of Homeland Security as “all foreign-born non-citizens who are not legal residents.”(1) Legal residents include US citizens, permanent US residents (also termed resident aliens), and those with immigrant visas.(1) In March 2012, UNOS initiated a new requirement that transplant centers record citizenship and residency status of patients undergoing organ transplantation, primarily to better understand transplant tourism. This refinement in UNOS coding, in addition to coding for states of residence, allows differentiation of citizens, lawful residents, and travelers, providing the opportunity to examine trends and outcomes of patients who have undergone LT, including unauthorized immigrants.
Recently, there has been federal and state legislation introduced that proposes to specifically intervene on access to organ transplantation for unauthorized immigrants.(4,5) This may in part have been prompted by a recent study(6) suggesting that non-US citizens/non-US residents (vs. US residents) who received LT have poor post-LT survival and higher probability of being lost to follow-up. However, this study and others(6,7) focused on LT for non-US citizens/non-US residents and included patients traveling to the United States specifically for LT (i.e., transplant tourism). To inform policy regarding LT for unauthorized immigrants who are not transplant tourists, the purpose of this study was to assess the national landscape of LT for unauthorized immigrants and to examine patient and graft survival post-LT by residency status.
Materials and Methods
Prospectively collected UNOS registry data from patients who underwent LT between March 2012 and December 2018 were examined, reflecting the institution of mandated recording of citizenship and residency status in UNOS and maximum available follow-up at analysis. We specifically excluded international transplant tourists (i.e., traveling non-US citizens/non-US residents who traveled to the United States for LT) from this study. We also used estimates from the Pew Center of Research, which are calculated from US Census Bureau data, to estimate the total population of US unauthorized immigrants in each US state and by country of origin, using data from 2016.(2) Between 2012 and 2016, the US population of unauthorized immigrants has remained stable and has varied by less than 5%.(2)
STUDY POPULATION
Adult LT recipients were included, comparing US residents versus presumed unauthorized immigrants. Any patient with age <18, human immunodeficiency virus, or prior LT was excluded. Residents included US citizens, resident aliens, and non-US citizens/US residents. Presumed unauthorized immigrants included nonresident aliens and non-US citizens/non-US residents who traveled to the United States for reasons other than LT (Table 1). To exclude traveling non-US citizens/non-US residents (i.e., transplant tourism), we excluded non-US citizens/non-US residents who traveled to the United States for LT and non-US citizens/non-US residents or nonresident aliens with states of residency listed as a foreign country or unknown. We also excluded patients with unknown and missing citizenship status. Unauthorized immigrants were defined as non-US citizens, non-US residents, and nontravelers who reported a US state as their primary residence (Supporting Fig. S1). In this study, these presumed unauthorized immigrants are the study population of primary interest.
TABLE 1.
Categorization of Residents Versus Non-US Citizens/Non-US Residents
| Study Categories | UNOS Categories |
|---|---|
| Residents |
|
| Presumed unauthorized immigrants* |
|
In subsampling validation, which involved careful chart review of 41 presumed unauthorized immigrants identified at 2 centers in this study, using the corresponding UNOS categories, this algorithm had a 93% positive predictive value for identifying unauthorized immigration status at time of LT (i.e., 38 of 41 were unauthorized immigrants from foreign countries living in the United States).
SUBSAMPLING VALIDATION
To validate the presumption that our classification of presumed unauthorized immigrants in UNOS reflected unauthorized immigration status, we performed a thorough patient-level chart review of all presumed unauthorized immigrants identified through UNOS who underwent LT at the two centers participating in this study, which accounted for 41 of 166 (24%) of the presumed unauthorized immigrants (10 at University of California San Francisco; 31 at University of Southern California). We subsequently calculated the positive predictive value of immigration status from the UNOS-based algorithm versus manual chart review.
RECIPIENT AND DONOR CHARACTERISTICS
Baseline and clinical characteristics were captured at time of LT. Donor characteristics were those used to calculate the donor risk index.(8) The indication for transplant was categorized as hepatitis C, hepatitis B, alcohol-associated liver disease, nonalcoholic fatty liver disease/cryptogenic, autoimmune (includes autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis), and other (e.g., acute liver failure, drug-induced liver injury, Wilson’s, amyloidosis, glycogen storage diseases), based on primary listing diagnosis. The diagnosis of hepatocellular carcinoma (HCC) was based on any primary or secondary diagnosis of HCC at listing or LT.
POST-TRANSPLANT PATIENT AND GRAFT SURVIVAL
For patient and graft survival analysis, to reflect available survival follow-up (at least 1 year post-LT) in UNOS, patients who underwent LT after December 2017 were excluded (7,215 residents and 48 presumed unauthorized immigrants). Patient mortality was defined as death from any cause. Graft failure was defined as retransplantation or death. We performed a sensitivity analysis that excluded patients with Model for End-Stage Liver Disease (MELD) exception points (4,747 residents and 20 presumed unauthorized immigrants) or living donor LT (1,254 residents and 3 presumed unauthorized immigrants).
STATISTICAL ANALYSIS
Categorical variables were compared using the chi-square test. Continuous variables were first assessed for normality, and then comparisons were made using the two-sample t test and Wilcoxon rank-sum test where appropriate.
In each state, we calculated the proportion of LTs for presumed unauthorized immigrants among total LTs for presumed unauthorized immigrants from UNOS data. We also calculated the proportion of LTs for presumed unauthorized immigrants and the proportion of total unauthorized immigrants in each state using data provided by the Pew Center of Research based on US Census Bureau data. We assessed the country of birth for LT recipients who were presumed unauthorized immigrants with a listed foreign country of birth and calculated the proportion for each of the countries.
Being lost to follow-up, post-LT graft, and patient survival were estimated by residency status using Kaplan-Meier plots. The association between residency status and survival was then assessed using separate competing risk models. For models evaluating being lost to follow-up, patient death was a competing risk, and in models evaluating graft and patient survival, being lost to follow-up was a competing risk. Subdistribution hazard ratios (sHR) and 95% confidence intervals (CI) with robust standard errors to account for center clustering were used. Follow-up time for graft survival was defined as the interval of time between the date of transplant and the date of retransplantation, death, or last follow-up. Follow-up time for patient survival was defined as the interval of time between the date of transplant and the date of death or last follow-up. Given the study period, analyses were performed with exit times of 3 years of follow-up.
Factors with univariate P < 0.1 were included in initial multivariable models, with final models selected using backward elimination (P for removal >0.05). All variables included had less than 5% missing data. Variables used in each model are presented in Tables 3 and 4 and Supporting Tables S1–S5. All statistical analyses were performed using Stata/IC version 13.1 (StataCorp, College Station, TX). P values <0.05 were considered statistically significant.
TABLE 3.
Univariable and Multivariable Competing Risk Analysis for Graft Failure After LT
| Univariable* | Multivariable* | |||
|---|---|---|---|---|
| Characteristic | Hazard Ratio (95% CI) | P | Hazard Ratio (95% CI) | P |
| Presumed Unauthorized Immigrants (vs. Resident) | 0.74 (0.40–1.39) | 0.36 | 0.74 (0.40–1.34) | 0.32 |
| Sex (Male) | 1.03 (0.97–1.10) | 0.31 | — | — |
| Age (per Year) | 1.01 (1.00–1.01) | <0.001 | 1.01 (1.00–1.01) | <0.001 |
| Caucasian | 0.97 (0.90–1.04) | 0.38 | — | — |
| College Education | 0.95 (0.90–1.01) | 0.12 | — | — |
| Private Insurance | 0.87 (0.81–0.93) | <0.001 | 0.90 (0.84–0.96) | 0.002 |
| Portal Vein Thrombosis at LT | 1.34 (1.24–1.44) | <0.001 | 1.32 (1.23–1.42) | <0.001 |
| MELD at LT | 1.01 (1.00–1.01) | <0.001 | 1.01 (1.00–1.01) | 0.001 |
| Mechanical Ventilation at LT | 1.90 (1.68–2.15) | <0.001 | 1.92 (1.67–2.21) | <0.001 |
| Wait Time of Region† | — | — | ||
| Low | Ref | Ref | ||
| Medium | 1.10 (0.99–1.22) | 0.08 | ||
| High | 1.02 (0.92–1.14) | 0.65 | ||
| Simultaneous Liver Kidney Recipient | 0.99 (0.89–1.11) | 0.93 | — | — |
| Donor Risk Index | 1.50 (1.37–1.65) | <0.001 | 1.54 (1.41–1.69) | <0.001 |
Adjusted for center clustering.
UNOS regions were divided into low (3, 6, 10, 11), medium (2, 4, 7, 8), and high wait time (1, 5, 9) regions by waitlist time.
TABLE 4.
Univariable and Multivariable Competing Risk Analysis for Patient Death After LT
| Univariable* | Multivariable* | |||
|---|---|---|---|---|
| Characteristic | Hazard Ratio (95% CI) | P | Hazard Ratio (95% CI) | P |
| Presumed Unauthorized Immigrants (vs. Resident) | 0.76 (0.38–1.51) | 0.43 | 0.68 (0.36–1.29) | 0.23 |
| Sex (Male) | 1.04 (0.98–1.11) | 0.17 | — | — |
| Age (per Year) | 1.02 (1.01–1.02) | <0.001 | 1.02 (1.02–1.02) | <0.001 |
| Caucasian | 0.98 (0.92–1.06) | 0.66 | — | — |
| College Education | 0.91 (0.85–0.96) | 0.002 | 0.93 (0.88–0.99) | 0.02 |
| Private Insurance | 0.80 (0.75–0.86) | <0.001 | 0.87 (0.80–0.94) | 0.001 |
| Portal Vein Thrombosis at LT | 1.33 (1.24–1.44) | <0.001 | 1.27 (1.18–1.37) | <0.001 |
| MELD at LT | 1.01 (1.01–1.01) | <0.001 | 1.01 (1.01–1.01) | <0.001 |
| Mechanical Ventilation at LT | 2.03 (1.77–2.33) | <0.001 | 1.96 (1.65–2.32) | <0.001 |
| Wait Time of Region† | — | — | ||
| Low | Ref | Ref | ||
| Medium | 1.11 (0.99–1.25) | 0.07 | ||
| High | 1.01 (0.90–1.14) | 0.83 | ||
| Simultaneous Liver Kidney Recipient | 1.09 (0.97–1.22) | 0.14 | — | — |
| Donor Risk Index | 1.35 (1.22–1.49) | <0.001 | 1.37 (1.24–1.51) | <0.001 |
Adjusted for center clustering.
UNOS regions were divided into low (3, 6, 10, 11), medium (2, 4, 7, 8), and high wait time (1, 5, 9) regions by waitlist time.
Results
Of 43,192 LT recipients, 43,026 (99.6%) were residents and 166 (0.4%) were presumed unauthorized immigrants (Supporting Fig. S1). In our subsampling validation, which involved careful chart review of the 41 of 166 (24%) presumed unauthorized immigrants at 2 centers in this study, we found that the UNOS algorithm used to identify presumed unauthorized immigrants had a 93% positive predictive value for identifying unauthorized immigration status at time of LT (i.e., 38 of 41 were undocumented immigrants from foreign countries living in the United States). Three of 41 presumed unauthorized immigrants (7.3%) were not in fact unauthorized immigrants: one was a graduate student from India, and two (from United Arab Emirates and Korea, respectively) were traveling in the United States. There were 297 non-US citizens/non-US resident travelers (i.e., transplant tourists) who were excluded from this study (Supporting Fig. S1).
Among the entire study cohort, presumed unauthorized immigrants (vs. residents) were younger (49 vs. 58; P < 0.001), more frequently Hispanic (59% vs. 14%; P < 0.001) or Asian (16% vs. 4%; P < 0.001), with high school or below as highest level of education (62% vs. 45%; P < 0.001), and with Medicaid as payer for LT (51% vs. 14%; P < 0.001). They had higher MELD scores (29 vs. 21; P < 0.001) and more often required renal replacement therapy at LT (31% vs. 15%; P < 0.001). The proportion of living donor LT was similar between presumed unauthorized immigrants versus residents (3.0% vs. 4.0%; P = 0.51). The primary listing indication for LT among presumed unauthorized immigrants (vs. residents) was more frequently hepatitis B (10% vs. 2%; P < 0.001) and less frequently hepatitis C (13% vs. 23%; P = 0.004). Presumed unauthorized immigrants (vs. residents) were less likely to have HCC (25% vs. 34%; P = 0.02). Baseline characteristics are summarized in Table 2.
TABLE 2.
Recipient Characteristics at Time of LT
| Recipient Characteristic | Resident (n = 43,026) | Presumed Unauthorized Immigrants (n = 166) | P |
|---|---|---|---|
| Age (years) | 58 (51–63) | 49 (39–58) | <0.001 |
| Male | 28,336 (66) | 100 (60) | 0.13 |
| Medicaid as Payer of LT | 6,035 (14) | 85 (51) | <0.001 |
| Private Insurance as Payer of LT | 22,543 (52) | 53 (32) | <0.001 |
| Race/Ethnicity | |||
| Caucasian | 30,678 (71) | 29 (18) | <0.001 |
| Black | 3,889 (9) | 10 (6) | |
| Hispanic | 6,026 (14) | 98 (59) | |
| Asian | 1,789 (4) | 26 (16) | |
| Other | 644 (2) | 3 (2) | |
| Highest Education Level | |||
| High School or Below | 19,694 (46) | 102 (61) | <0.001 |
| College or Above | 21,576 (50) | 54 (32) | |
| Unknown | 1,756 (4) | 10 (6) | |
| Body Mass Index | 28.5 (25.0–32.7) | 26.7 (23.7–30.2) | 0.001 |
| Diabetes* | 12,138 (28) | 33 (20) | 0.05 |
| Renal Replacement Therapy | 6,621 (15) | 51 (31) | <0.001 |
| Portal Vein Thrombosis at LT† | 5,798 (14) | 22 (13) | 0.93 |
| MELD Score at LT | 21 (14–31) | 29 (20–37) | <0.001 |
| Simultaneous Liver Kidney Recipient | 3,710 (9) | 22 (13) | 0.03 |
| Living Donor | 1,723 (4) | 5 (3) | 0.51 |
| Days on Waitlist | 108 (20–307) | 56 (7–270) | <0.001 |
| indication‡ for LT | Resident (n = 43,026) | Presumed Unauthorized immigrants (n = 166) | P |
| Alcohol | 10,568 (25) | 38 (23) | 0.62 |
| Hepatitis C | 9,764 (23) | 22 (13) | 0.004 |
| Hepatitis B | 977 (2.3) | 16 (10) | <0.001 |
| Nonalcoholic Fatty Liver Disease or Cryptogenic | 8,083 (19) | 26 (16) | 0.30 |
| Autoimmune§ | 4,167 (9.7) | 18 (11) | 0.61 |
| Other | 3,103 (7.2) | 20 (12) | 0.02 |
| Hepatocellular Carcinoma | 14,703 (34) | 42 (25) | 0.2 |
Note: Data are presented as n (%) or median (IQR).
For diabetes status, 75 (0.2%) missing values among residents, 0 (0%) missing values among presumed unauthorized immigrants.
For portal vein thrombosis at LT, 237 (0.6%) missing values among residents, 0 (0%) missing values among presumed unauthorized immigrants.
The indication for transplant was categorized as hepatitis C, hepatitis B, alcohol-associated liver disease, nonalcoholic fatty liver disease, cryptogenic, autoimmune (includes autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis), and other (e.g., acute liver failure, drug-induced liver injury, Wilson’s, amyloidosis, glycogen storage diseases) based on primary listing diagnosis. The diagnosis of HCC was based on any primary or secondary diagnosis of HCC at listing or LT.
Includes autoimmune hepatitis, primary sclerosing cholangitis, and primary biliary cholangitis.
We performed sensitivity analyses by restricting the cohort to type of medical insurance as primary payment for LT. Among patients with private insurance, presumed unauthorized immigrants versus resident LT recipients had higher MELD (29 vs. 22; P < 0.001) and need for renal replacement therapy at LT (28% vs. 14%; P = 0.003). Among patients with Medicaid insurance, presumed unauthorized immigrants (vs. resident) LT recipients had higher MELD (31 vs. 25; P = 0.003) and need for renal replacement therapy at LT (31% vs. 19%; P = 0.006). Full baseline characteristics among patients with private insurance and Medicaid insurance are summarized in Supporting Tables S6 and S7, respectively.
Among 166 presumed unauthorized immigrants, most LTs were performed in California (n = 78; 47%) and New York (n = 30; 18%). Similar to the full study population, presumed unauthorized immigrants (vs. residents) in California and New York (n = 6,668) had higher MELD (33 vs. 23; P < 0.001) and need for renal replacement therapy at LT (41% vs. 27%; P = 0.001). Baseline characteristics of patients who received LT in California and New York are summarized in Supporting Table S8. Among the general US population, California accounted for 27% of the total US unauthorized immigrant population and 7% for New York. The proportion of LTs performed for unauthorized immigrants compared with the total population of unauthorized immigrants differed among states, with the highest differences in proportions in California (+20%) and New York (+11%) and lowest in Texas (−12%) and Florida (−3%), as shown in Fig. 1 and Supporting Table S9. Among 115 presumed unauthorized immigrants with listed countries of birth, the five most common countries were Mexico (n = 52; 45%), Guatemala (n = 7; 6%), China (n = 6; 5%), El Salvador (n = 5; 4%), and India (n = 5; 4%). According to the most recent data from the Pew Center of Research, we estimated Mexico, Guatemala, China, El Salvador, and India to account for 51%, 5%, 3%, 7%, and 4% of the unauthorized immigrant population in the United States, respectively (Fig. 2).
FIG. 1.
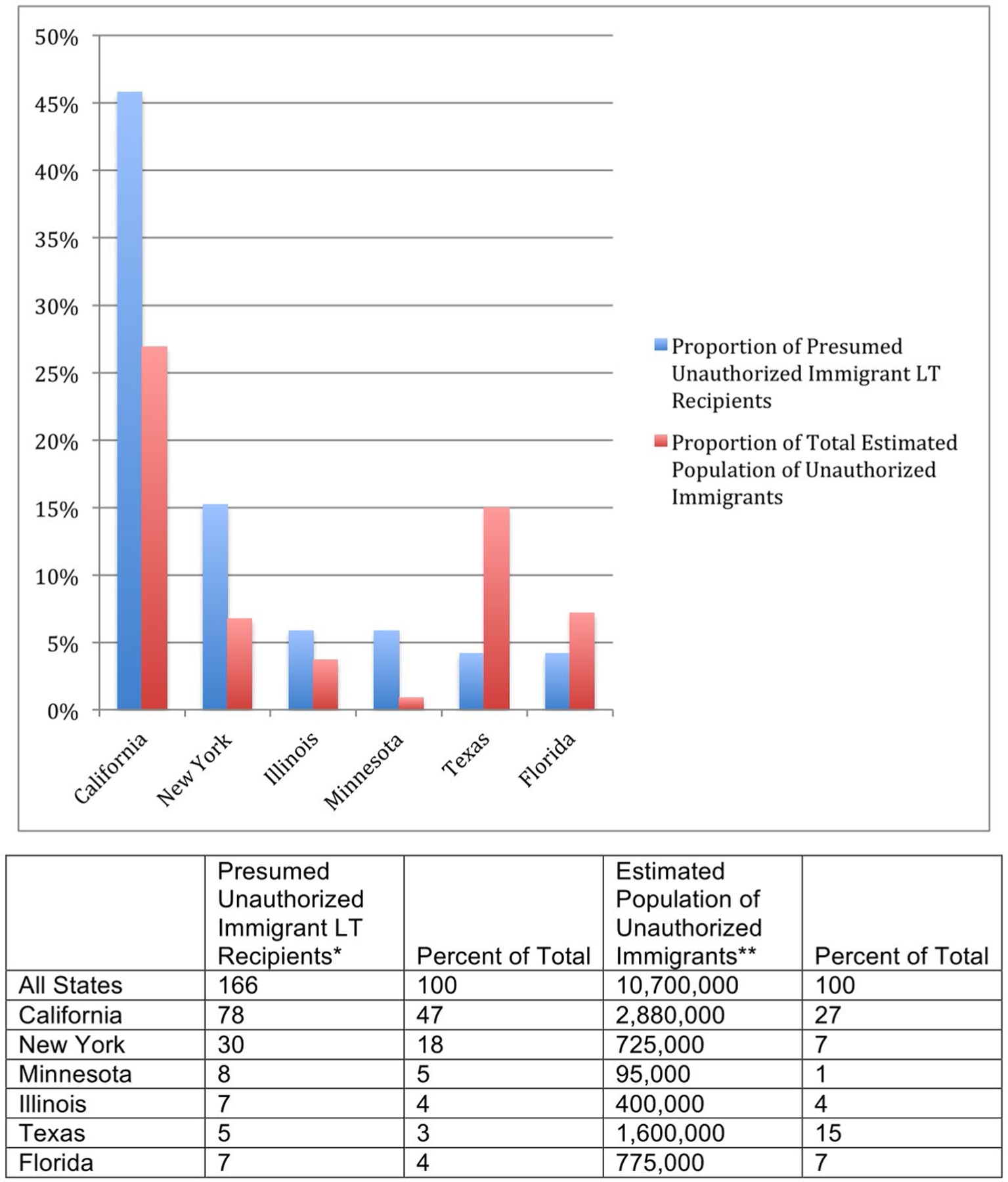
Proportion of presumed unauthorized immigrants among the LT and general population by state. Results from six states with highest absolute number of LT recipients for unauthorized immigrants between March 2012 and December 2018. Among presumed unauthorized immigrants who received LT, most LTs were performed in California (n = 78; 47%) and New York (n = 30; 18%). Among the general US population in 2016, California accounted for 27% of the total US unauthorized immigrant population and 7% for New York. The proportion of LTs performed for unauthorized immigrants compared with the total population of unauthorized immigrants differed among states, with the highest differences in proportions in California (+20%) and New York (+11%) and lowest in Texas (−12%) and Florida (−3%). *Between March 2012 and December 2018. **According to Pew Research Center Estimates from US Census Bureau data in 2016.
FIG. 2.
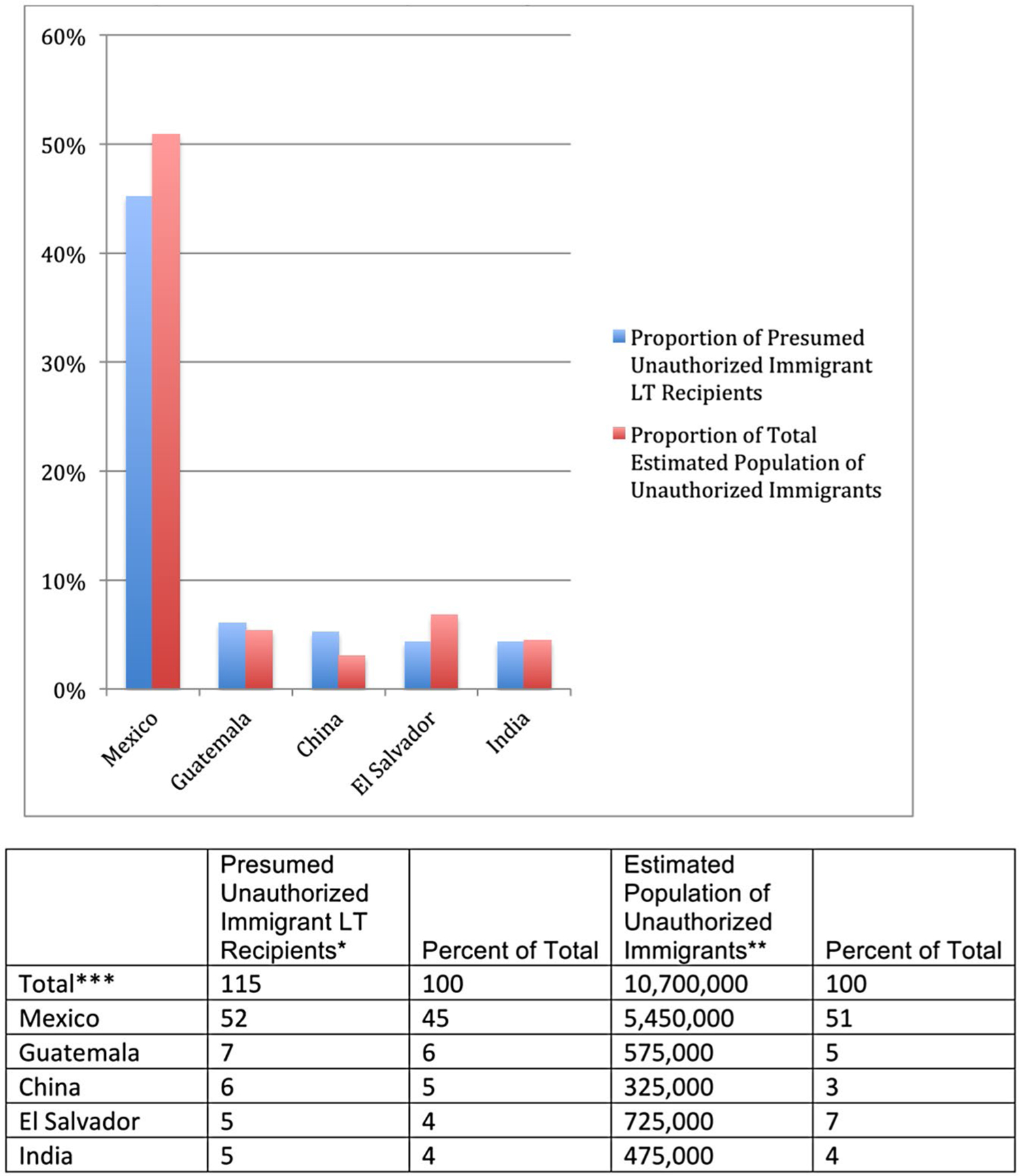
Countries of birth of presumed unauthorized immigrants among the LT and general population by state. Among 115 presumed unauthorized immigrants who received LT between March 2012 and December 2018 with listed countries of birth, the 5 most common countries were Mexico (n = 52; 46%), Guatemala (n = 7; 6%), China (n = 6; 5%), El Salvador (n = 5; 4%), and India (n = 5; 4%). According to the most recent data from the Pew Center of Research, we estimated Mexico, Guatemala, China, El Salvador, and India to account for 51%, 5%, 3%, 7%, and 4% of the unauthorized immigrant population in the United States, respectively. *Between March 2012 and December 2018. **According to Pew Research Center Estimates from US Census Bureau data in 2016. ***Only 115 of 166 had available data for country of birth.
GRAFT AND PATIENT SURVIVAL
The 35,929 LT recipients (118 presumed unauthorized immigrants, 35,811 residents) included in our survival analysis excluded LT recipients who underwent LT after December 2017. Seven of 118 (5.9%) presumed unauthorized immigrants versus 312 of 35,811 (0.9%) residents were lost to follow-up after 1.85 years (interquartile range [IQR] 1.05–2.00) versus 2.05 years (IQR 1.05–3.08) post-LT, respectively. In multivariable competing risk analysis to account for death events, presumed unauthorized immigrants (vs. residents) were more likely to be lost to follow-up (sHR 9.4; 95% CI 3.8–22.8; P < 0.001). Full multivariable model shown in Supporting Table S1. Unadjusted cumulative 1-year and 3-year survival were 95% (95% CI, 89%−98%) and 88% (95% CI, 79%−93%) among presumed unauthorized immigrants versus 92% (95% CI, 92%−92%) and 85% (95% CI, 85%−86%) among residents, respectively. In multivariable competing risk analysis, presumed unauthorized immigrant status (vs. resident) was not associated with risk of graft failure (sHR 0.74; 95% CI, 0.40–1.34; P = 0.32; Fig. 3A) or patient death (sHR 0.68; 95% CI, 0.36–1.29; P = 0.23; Fig. 3B). Full multivariable models are shown in Tables 3 and 4. A total of 2/118 (1.7%) presumed unauthorized immigrants versus 941/35,811 (2.6%) residents underwent retransplantation (P = 0.53). In a sensitivity analysis excluding LT recipients with MELD exception points, for living donor LT, as a multivariable competing risk analysis, presumed unauthorized immigrant status (vs. resident) was not associated with higher risk of graft failure or patient death (Supporting Tables S2 and S3). In a sensitivity analysis assuming that all patients lost to follow-up died as a Cox regression analysis, presumed unauthorized immigrant status (vs. resident) was not associated with higher risk of graft failure or patient death (Supporting Tables S4 and S5).
FIG. 3.
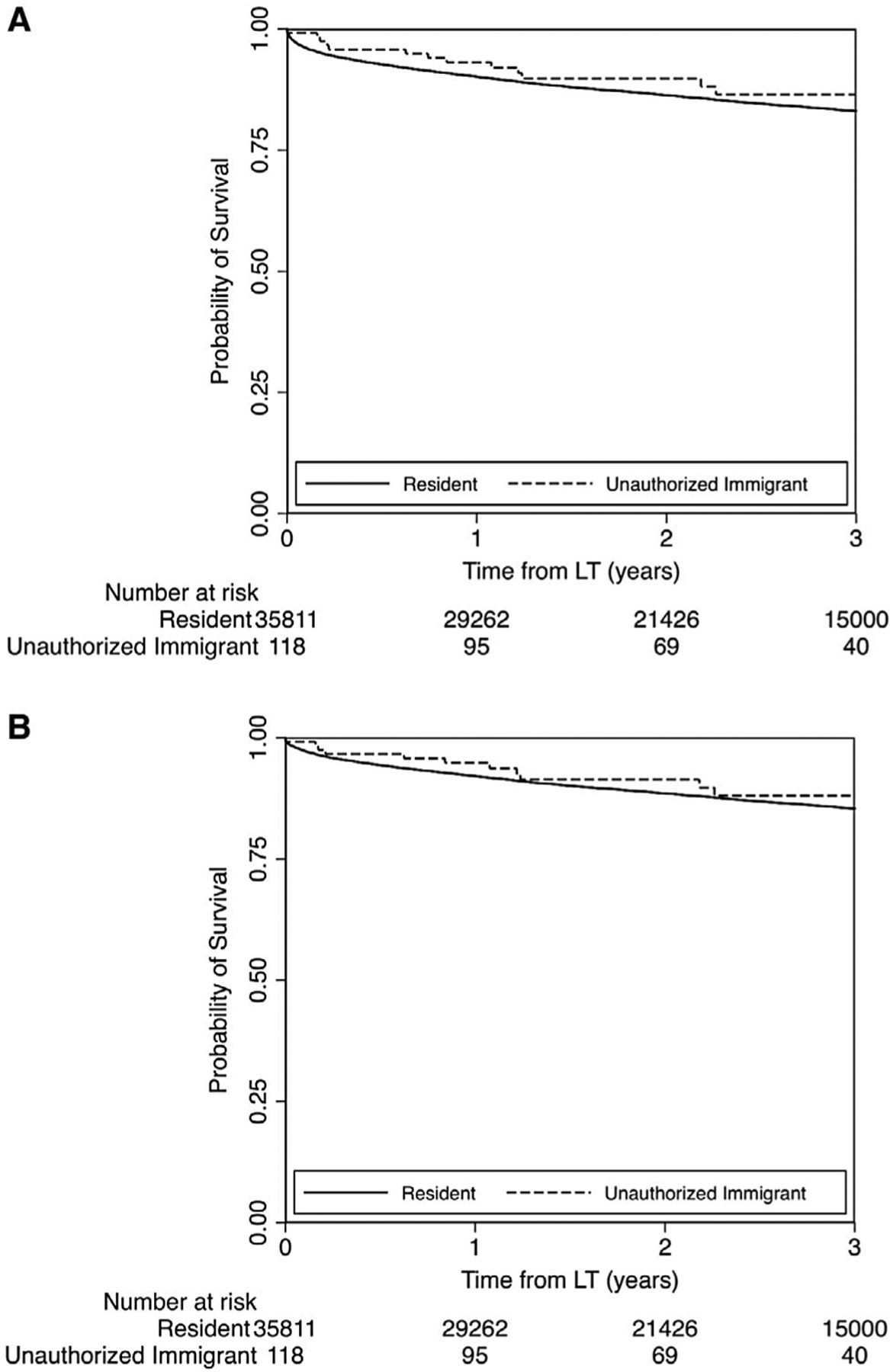
(A) Probability of graft survival among presumed unauthorized immigrants versus residents. Cumulative unadjusted probabilities of post-LT graft survival at 1 year and 3 years were 93% (95% CI, 87%−96%) and 86% (95% CI, 77%−92%) among presumed unauthorized immigrants versus 90% (95% CI, 90%−90%) and 83% (95% CI, 83%−83%) among residents (P = 0.36). (B) Probability of patient survival among presumed unauthorized immigrants versus residents. Cumulative unadjusted probabilities of post-LT patient survival at 1 year and 3 years were 95% (95% CI, 89%−98%) and 88% (95% CI, 79%−93%) among presumed unauthorized immigrants versus 92% (95% CI, 92%−92%) and 85% (95% CI, 85%−86%) among residents (P = 0.43).
Discussion
This study highlights the national landscape of LT for unauthorized immigrants in the United States. We found that the proportion of transplants allocated to unauthorized immigrants between 2012 and 2018 was low: 0.4%. Although this study does not investigate possible differences in the need for LT among residents versus unauthorized immigrants, this proportion is 10-fold lower than the proportion of unauthorized immigrants among the total US population, estimated to be 4%.(1) Compared to residents, presumed unauthorized immigrants had characteristics suggesting higher severity of disease at time of LT, as evidenced by higher MELD scores and need for renal replacement therapy, across a number of sensitivity analyses including geography and type of medical insurance, which suggests late access to LT. Although the most common countries of birth among presumed unauthorized immigrants who received LT were similar to that of the general US population of authorized immigrants (i.e., Mexico, El Salvador, Guatemala, China, India), the states in which the LTs were performed were not consistent with the general population distribution of unauthorized immigrants among US states—the proportion of LTs for unauthorized immigrants attributable to centers in California and New York was more than expected, whereas Texas and Florida were less than expected. These findings highlight a disparity in access to LT for unauthorized immigrants across the United States.
Our study differs from studies(6,7) that have examined non-US citizens/non-US residents as a composite group: non-US citizens/non-US residents who traveled to the United States for the purpose of LT (i.e., transplant tourists) and non-US citizens/non-US residents who are unauthorized immigrants. The distinction is critical because unauthorized immigrants pay social security tax and contribute to organ donation, estimated at 3% of the total donated US organs,(9,10) whereas transplant tourists do not. Transplant tourists contribute financially to the medical system during a limited time period surrounding LT, whereas unauthorized immigrants contribute over a lifetime. Importantly, we found that the number of LTs performed for unauthorized immigrants was less than half the LTs performed for US transplant tourists. Indeed, without distinguishing transplant tourists from unauthorized immigrants, the non-US citizens/non-US resident group in LT has been described as predominantly of high socioeconomic class, from Gulf countries (e.g., Saudi Arabia, United Arab Emirates, Kuwait, and so on), and with worse post-LT survival.(6,7) With our exclusion criteria to identify presumed unauthorized immigrants, we found that non-US citizen/non-US resident LT recipients in our study reflect the general US unauthorized immigrant population and are predominantly from Latin America. More importantly, contrary to a study examining non-US citizens/non-US residents that included transplant tourists,(6) our study found that patient survival was similar between non-US citizens/non-US residents and residents when excluding transplant tourists. Although we found a higher likelihood of being lost to follow-up among presumed unauthorized immigrants, this finding should be interpreted with caution, as it was based on only seven events. Given these findings of acceptable survival outcomes among unauthorized immigrants, concern for worse survival should not be used as a reason to deny access to LT.
Our study provides insight to the barriers that may exist for unauthorized immigrants in need of LT. It is mandated by federal law that allocation of organs be based exclusively on “established medical criteria,” which presumably would not allow a tiered allocation system by citizenship. Almost half of presumed unauthorized immigrants had their LT paid for by Medicaid; federal law allows states to apply for waivers to reallocate Medicaid funds for health care costs incurred by uninsured patients, including unauthorized immigrants.(11) State responses to this federal law have been variable: some states, including Texas and Florida, have resisted Medicaid expansion as afforded by the Affordable Care Act,(11) and these were states that we found to have the less than expected proportions of LT for unauthorized immigrants. Conversely, in addition to Medicaid expansion, California recently passed legislation to become the first state to allow unauthorized immigrants to enroll in state health insurance exchange, and we found this state to have a more than expected proportion of LT for unauthorized immigrants.(11) However, there have been media reports of individual plights in obtaining LT because of immigration status, in some instances even with adequate insurance coverage.(12,13) These findings suggest that barriers to LT for unauthorized immigrants are likely multifactorial but are related in part to different state policies regarding financial coverage and center/provider attitudes.
Although this study focuses on LT specifically, we hypothesize that our findings may be present in transplant for other organs. The implications may be considerable, particularly given recent estimates that 6,500 unauthorized immigrants have end-stage renal disease in the United States(14) and the high costs associated with the reimbursement policy for emergency-only hemodialysis. Such future studies would be informative for a concerted approach to address access and policy for organ transplantation among unauthorized immigrants.
Our study had limitations. First, classification of presumed unauthorized immigrants was based on self-report and data entered by LT coordinators and is at risk for misclassification. We relied on identifiers that were instated to identify transplant tourists, not unauthorized immigrants, and our presumed unauthorized immigrant group may include foreign persons on extended visas who have obtained a US residence as a primary address or exclude unauthorized immigrants who have not responded truthfully. However, our subsampling validation shows that our algorithm likely identifies unauthorized immigrants with high positive predictive value, although we note that this subsampling validation used two large transplant centers in California, a state that may have more liberal medical coverage policies toward unauthorized immigrants. Moreover, the demographics of our presumed unauthorized immigrant group by race/ethnicity, country of origin, and socioeconomic class are strikingly similar to the demographics of the total US population of unauthorized immigrants. Furthermore, some uncertainty in our estimates caused by misclassification is unlikely to dramatically alter our main conclusions that unauthorized immigrants are underrepresented among the LT population and likely face state-specific barriers in access to LT given the magnitude of the differences and plausibility. Second, this study relies on registry data, and reporting of citizenship and residency are a relatively new mandate; less missing data and more granular details and longer term follow-up would be helpful to understand barriers to LT and post-LT outcomes, including changes to insurance status, social/family support, health care literacy, and adherence to medical care. However, given the rarity of LT in this population, this topic will likely best be studied through national registry data. Finally, we did not examine waitlist selection, denials, or waitlist outcomes other than receipt of LT, which would be an important area for future investigation.
In conclusion, we found that LT for presumed unauthorized immigrants is very rare, and access to LT appears to be variable across the United States. A minority of unauthorized immigrants is lost to follow-up, and overall patient and graft survival are comparable with residents/citizens. This evidence regarding outcomes in this understudied group should help guide state and national policies regarding LT for unauthorized immigrants.
Supplementary Material
Acknowledgment:
Thanks to Neil Mehta, Caitlin Hohe, Vandana Prakash, and Jeffrey Kahn for their help with this endeavor.
Supported by the Clinical & Translational Core of the UCSF Liver Center (P30 DK026743) and training grant support for B.P.L. (T32 DK060414).
Abbreviations:
- CI
confidence interval
- HCC
hepatocellular carcinoma
- IQR
interquartile range
- LT
liver transplantation
- MELD
Model for End-Stage Liver Disease
- sHR
subdistribution hazard ratio
- UNOS
United Network for Organ Sharing
Footnotes
Supporting Information
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep.30926/suppinfo.
Potential conflict of interest: Dr. Terrault advises Intercept and received grants from Gilead.
REFERENCES
- 1).Department of Homeland Security. Population estimates: illegal alien population residing in the United States: January 2015. https://www.dhs.gov/sites/default/files/publications/18_1214_PLCY_pops-est-report.pdf. December 2018. Accessed January 2019.
- 2).Pew Research Center. U.S. unauthorized immigrant population estimates by state, 2016. http://www.pewhispanic.org/interactives/u-s-unauthorized-immigrants-by-state/ Published February 5, 2019
- 3).European Commission. Annexes to the communication from the commission to the European Parliament, the Eurpoean Council and the Council: progress report on the Implementation of the European Agenda on Migration. https://ec.europa.eu/home-affairs/sites/homeaffairs/files/what-we-do/policies/european-agendamigration/20180516_annexes_progress-report-european-agendamigration_en.pdf. Published May 16, 2018
- 4).To Amend the Public Health Service Act to Establish a Preference, in the Allocation of Donated Organs, for Individuals who Are Lawfully Present in the United States, and for Other Purposes. HR 5518, 115th Cong (2018). https://www.congress.gov/bill/115th-congress/house-bill/5518/text.
- 5).Organ and Tissue Transplantation: Uninsured or Undocumented Individuals. AB 2846 (Ca 2018) https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201720180AB2846.
- 6).Ferrante ND, Goldberg DS. Transplantation in foreign nationals: lower rates of waitlist mortality and higher rates of lost to follow-up posttransplant. Am J Transpl 2018;18:2663–2669. [DOI] [PubMed] [Google Scholar]
- 7).Delmonico FL, Gunderson S, Iyer KR, Danovitch GM, Pruett TL, Reyes JD, et al. Deceased donor organ transplantation and nonresidents. Transplantation 2018;102:1124–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 2006;6:783–790. [DOI] [PubMed] [Google Scholar]
- 9).Hartsock JA, Ivy SS, Helft PR. Liver allocation to non-U.S. citizen non-U.S. residents: an ethical framework for a last-in-line approach. Am J Transpl 2016;16:1681–1687. [DOI] [PubMed] [Google Scholar]
- 10).Glazier AK, Danovitch GM, Delmonico FL. Organ transplantation for nonresidents of the United States: a policy for transparency. Am J Transpl 2014;14:1740–1743. [DOI] [PubMed] [Google Scholar]
- 11).Kelley AT, Tipirnenini R. Care for undocumented immigrants — rethinking state flexibility in Medicaid waivers. N Engl J Med 2018;378:1661–1663. [DOI] [PubMed] [Google Scholar]
- 12).Rosenberg E A hospital refused a new liver to a woman because she was undocumented. Then it found its heart. Washington Post. February 7, 2018. https://www.washingtonpost.com/news/to-your-health/wp/2018/02/07/a-hospital-refused-a-new-kidney-to-a-woman-because-she-was-undocumented-then-it-found-its-heart/ [Google Scholar]
- 13).Danna J Undocumented immigrants fight for lifesaving liver transplants. Chicago Tribune. June 11, 2012. https://www.chicagotribune.com/news/ct-xpm-2012-06-11-ct-met-immigrant-hunger-strike-20120612-story.html [Google Scholar]
- 14).Cervantes L, Grafals M, Rodriguez RA. The United States needs a national policy on dialysis for undocumented immigrants with ESRD. Am J Kidney Dis 2018;71:157–159. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


