Abstract
Background:
Recurrence of adhesive small bowel obstruction (ASBO) can lead to multiple admissions. There is limited knowledge of the role of operative and non-operative treatment in the long-term recurrence risk for ASBO. We sought to determine the effect of operative and non-operative management on future ASBO recurrences.
Methods:
This is a retrospective study of administrative discharge data from the Tennessee Hospital Association. Adult discharges from 2007 to 2009 with ASBO and all subsequent readmissions within any hospital in the state were included; patients with prior ASBO from 2003 to 2007 and out-of-state residents were excluded. ASBO recurrence was compared between operative and non-operative approaches using the Andersen-Gill approach for modeling recurrent time-to-event data. Secondary outcomes included mortality, complications, and time-to-recurrence.
Results:
6,191 records were analyzed, 30.0% were initially treated operatively. Patients initially managed surgically had lower overall recurrence (19.0% vs. 25.6%, p<0.005). The hazard for recurrence was lower if the most recent ASBO management was operative (HR 0.27, 95% CI, 0.23–0.31). The risk of ASBO recurrence increased with more cumulative operative or non-operative ASBO admissions relative to patients with fewer prior admissions (operative: HR 2.30, 95% CI, 2.04–2.60; non-operative: HR 1.18, 95% CI, 1.16–1.20). In-hospital mortality (3.7% vs. 2.6%, p=0.025) and time-to-recurrence (729 vs. 550 days, p=0.009) were greater in the operative group.
Conclusion:
Operative management for the most recent ASBO is associated with fewer recurrences. Subsequent cumulative recurrences of ASBO predispose to recurrence regardless of operative or non-operative management. When considering ASBO management ASBO, subsequent recurrences should be considered.
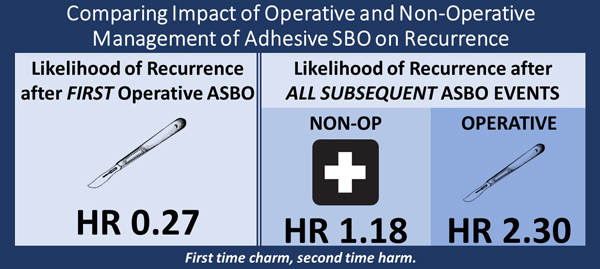
Graphical Abstract
Precis
Patients admitted with adhesive small bowel obstruction are less likely to develop recurrence if they undergo an operation for the first obstruction. Subsequent operative and nonoperative recurrences have greater risk of recurrence. In-hospital mortality and complications are higher after operative management.
Introduction
Adhesive small bowel obstruction (ASBO) is the most common cause of intestinal obstruction. With nearly 1 in 20 patients experiencing this pathophysiology following abdominal or pelvic surgery, ASBO represents a significant burden on the healthcare system.(1) After successful management, whether operative or non-operative, there is a risk of patients developing recurrent obstruction. One of the challenges of counseling patients with ASBO has been providing expectations for the disease’s course, especially with long-term outcomes following different treatment strategies.
Historically, management of ASBO went by the mantra “Never let the sun rise or set on a small bowel obstruction.” While treatment is individualized based on patient presentation and physiology, non-operative management has become accepted as the de facto management for ASBO.(2) The combination of enteral decompression, nil per os (NPO) status, and “bowel rest” composed non-operative management until the mid-2000s when greater success was reported with the incorporation of a small bowel follow-through, serial abdominal x-rays to follow the progress of water-soluble contrasted material.(3, 4) A more recent prospective study identified significant reduction in need for surgery with the incorporation of water-soluble contrast into non-operative treatment compared to those who did not receive contrast.(5) Previous studies have estimated 75% of patients are successfully managed non-operatively during a primary admission for SBO.(6) While both operative and non-operative treatments can be effective in resolving ASBO, the paradox of both treatments is that they can predispose to future adhesive disease.
Many studies have considered operative and non-operative management outcomes.(7–13) Foster found that patients were more likely to have longer time to recurrence after operative treatment, and similarly patients managed surgically had fewer recurrences of SBO during follow-up.(6) Much of the data identifying the recurrence patterns of SBO predate the studies demonstrating the benefit of adding the oral contrast for diagnostic and therapeutic benefit water-soluble contrast.(4) Behman and colleagues recently presented data demonstrating benefit of surgical management for ASBO in reducing the risk of first recurrence.(14) However, surgical management has higher risk of perioperative complications, some of which are specific for the operative approach (intraoperative bowel injury and postoperative wound infection).(15) We sought to develop a more complete clinical picture of the management of ASBO, evaluating recurrence as well as morbidity and mortality in a cohort with long-term longitudinal follow-up. We hypothesized that patients managed operatively will have fewer recurrences than those who are managed non-operatively. This hypothesis was based upon the default among many surgeons to treat non-operatively due to the inherent risks and complications that come with an operation, although, non-operative management has a shorter time to recurrence which we believe may translate into greater likelihood of more recurrences.
Methods
Data Source
The study design was a retrospective cohort study to evaluate the natural history of recurrence of ASBO. The data source for this longitudinal study was the Tennessee Hospital Association (THA) Health Information Network, a non-profit organization made up of most hospitals throughout Tennessee (except federal healthcare facilities). The distinctive feature of this data set was the ability to link patient records across hospitals throughout the state which allowed patient follow-up to not be limited by a single-institution’s records.
Population
Patients admitted for ASBO between January 1, 2007 and December 31, 2009 were included in the cohort. (Figure 1) International Classification of Diseases, Ninth Edition (ICD-9) codes from the primary discharge diagnosis were used to identify the patients admitted with small bowel obstruction due to adhesive disease (560.81, 560.89, and 560.9). Primary diagnosis codes of small bowel obstruction secondary to hernia or malignancy were excluded as management of obstruction secondary to these causes may differ from those secondary to adhesive disease. Patients less than 18 years old were excluded from the cohort. Patients were also excluded if their primary residence zip code was not within the state of Tennessee as we believed that non-residents would be more likely to seek care for recurrent disease in their home state.
Figure 1.
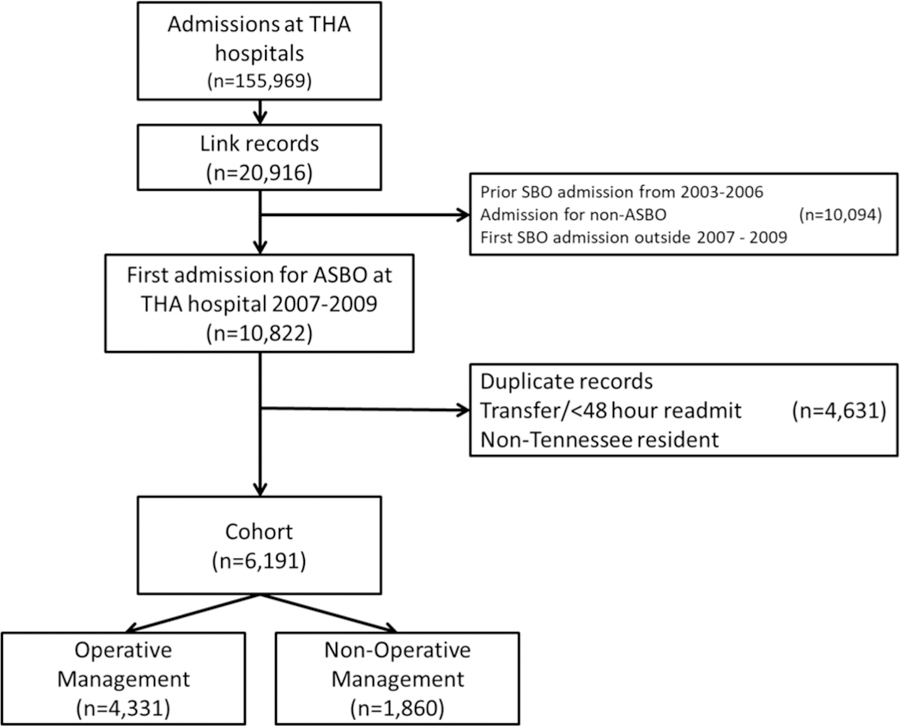
Schematic for cohort selection. THA, Tennessee Hospital Association; ASBO, adhesive small bowel obstruction; SBO, small bowel obstruction.
Recurrence of ASBO was determined by evaluating all included patients’ subsequent admissions. ICD-9 and −10 codes for the primary admitting diagnosis were used to identify an ASBO admission. (eDocument 1) If a recurrence occurred within 48 hours of a previous discharge, then the details of the two encounters were combined as one admission.
We excluded patients with an ASBO from January 1, 2003 to December 31, 2006 in order to capture patients experiencing their first ASBO. Previous literature has suggested that patients who do recur after an episode of SABO have a mean time to recurrence of less than two years for both operative and non-operative approaches.(6, 16, 17) We sought patients with their first ASBO admission as we anticipated the management and time to recurrence would differ between patients with history of different number of admissions.
Exposures
During the index and recurrent ASBO, patients could be exposed to non-operative management or operative management. Operative management was ascertained using ICD-9 and −10 procedure codes. (eDocument 1) Operative management for ASBO included exploratory laparotomy, exploratory laparoscopy, small bowel resection, and lysis of adhesions. The presence of a procedure was used to define operative management. The absence of a procedure was used to define non-operative management. When two admissions within 48 hours were combined into a single episode of care, the combined episode was categorized as operative if either admission included a procedure.
Covariates
Several covariates which may impact the likelihood of ASBO recurrence as well as operative or non-operative management were considered including age, gender, race, ethnicity, insurance status, and the Charlson comorbidity index. The Charlson comorbidity index was calculated using the secondary diagnosis codes with indicators that they were “Present on Admission” to reflect the patient’s outpatient condition upon presentation. Covariates were time-varying and reflected the patient’s status at each admission.
Outcomes
The primary outcome of recurrent ASBO was determined using the ICD-9/10 criteria used to identify the cohort. ASBO recurrence must be with the short-term complications during the hospital admission for ASBO. Thus, secondary outcomes were in-hospital mortality and hospital morbidity (myocardial infarction, pulmonary embolism, deep vein thrombosis (DVT), pneumonia, acute kidney injury (AKI), cerebrovascular accident (CVA), wound infection, and deep space infection). Time to recurrence was also between operative and non-operative management as a balancing measure.
Analysis
Descriptive statistics were used to characterize the cohort of patients at the time of their first ASBO. Student’s t-test (continuous) and Chi-squared tests (categorical) were used to compare features between those initially managed operatively and those initially managed non-operatively. Then, we constructed time-to-recurrent-event models to evaluate the association between the management approach for each episode of ASBO and any subsequent recurrence. We used the Andersen-Gill model to take into account correlation between the time to recurrent ASBO and the time dependent covariates of each recurring ASBO.(18) A variable for the cumulative number of admissions, either operative or non-operative, was included in the model as we expect surgeons’ management decisions to be influenced by prior recurrence. Subjects were censored if they experience an in-hospital death or the conclusion of the follow-up period was achieved (December 31, 2016). The hazard ratio for the recurrence based on the immediate prior admission’s management approach (operative or non-operative) is reported. Hazard ratios for the likelihood of developing recurrent ASBO if there were more than one prior operative or non-operative recurrence are also given.
Multivariable logistic regression was used to model the probability of complications during each admission, and Cox proportional hazard model was used to compare the in-hospital mortality of operative and non-operatively managed study subjects. For those experiencing a recurrence, time to first recurrence was compared using the Wilcoxon rank-sum test.
Results
Descriptive Statistics
There were 20,916 unique patients with 155,969 admissions from 1/1/2003 to 12/31/2016. There were 12,485 patients with an ASBO between 2007 and 2009. 1,663 patients were excluded because they had a prior ASBO from 2003 to 2006. An additional 4,302 patients were excluded if the patient’s residence was not in Tennessee. After exclusions, 6,191 patients were included for analysis.
At the initial admission 4,331 (70.0%) patients were treated non-operatively while 1,860 (30.0%) patients underwent operative management. (Table 1) The median follow-up times were similar for the operative and non-operative groups (3587 days (9.82 years) vs. 3607 days (9.88 years).
Table 1.
Demographic Characteristics of Patient Cohort
| Variable | Nonoperative, n = 4331 | Operative, n = 1860 | p Value |
|---|---|---|---|
| Age, y, mean (SD) | 63 (17) | 62 (16) | 0.03 |
| Sex, n (%) | <0.005 | ||
| Men | 1905 (44.0) | 703 (37.8) | |
| Women | 2426 (56.0) | (1157 (62.2) | |
| Race, n (%) | 0.001 | ||
| White | 3396 (78.4) | 1353 (72.7) | |
| Black | 603 (13.9) | 361 (19.4) | |
| Asian | 16 (0.4) | 5 (0.3) | |
| Native American | 2 (0.1) | 2 (0.1) | |
| Other/unknown | 314 (7.3) | 139 (7.5) | |
| Ethnicity, n (%) | <0.005 | ||
| Not Hispanic | 3182 (73.5) | 1457 (78.3) | |
| Hispanic | 145 (3.3) | 48 (2.6) | |
| Other/unknown | 1004 (23.4) | 355 (19.1) | |
| Insurance status, n (%) | 0.01 | ||
| Private insurance | 1410 (32.6) | 662 (35.6) | |
| Medicare/Medicaid | 2632 (60.7) | 1049 (56.4) | |
| Self-Pay | 253 (5.8) | 129 (6.9) | |
| Unknown | 36 (0.8) | 20 (1.1) | |
| Charlson Comorbidity Index, median (SD) | 1.26 (1.98) | 1.11 (1.85) | 0.028 |
| Hospital location, n (%) | <0.005 | ||
| Rural | 870 (20.6) | 277 (15.6) | |
| Urban/suburban | 3363 (79.4) | 1508 (84.5) |
Recurrences
Among all 6,191 patients, 4,717 (76.2%) patients did not experience a recurrence. Among the patients managed non-operatively during initial admission, 25.6% developed at least one recurrence compared with 19.0% of patients initially managed operatively (p < 0.005). (Figure 2) The majority of patients recurring experienced only one recurrence, and more patients managed operatively had just one recurrence (non-operative 644/1112, 57.9%; operative 241/354, 68.1%; p < 0.005). At each subsequent recurrence, patients initially managed non-operatively tended to have a higher proportion of subsequent recurrences, and both groups had higher recurrence rates for each subsequent recurrence. (Figure 3)
Figure 2.
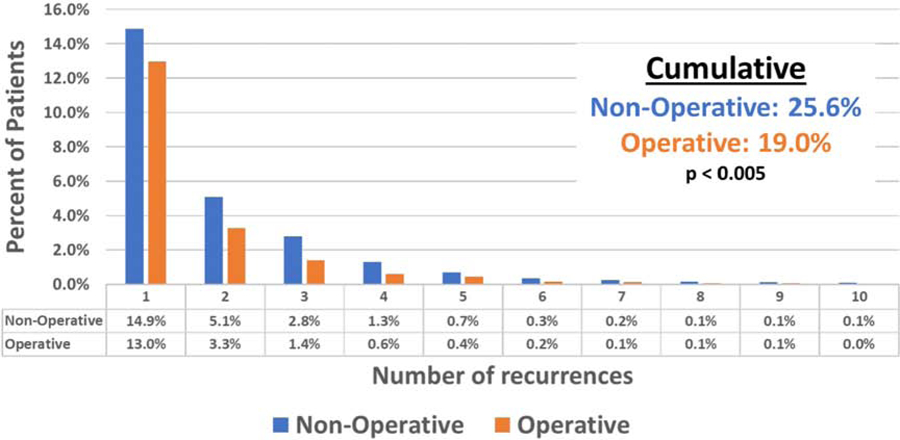
Distribution of the number of adhesive small bowel obstruction recurrences by number of recurrences.
Figure 3.
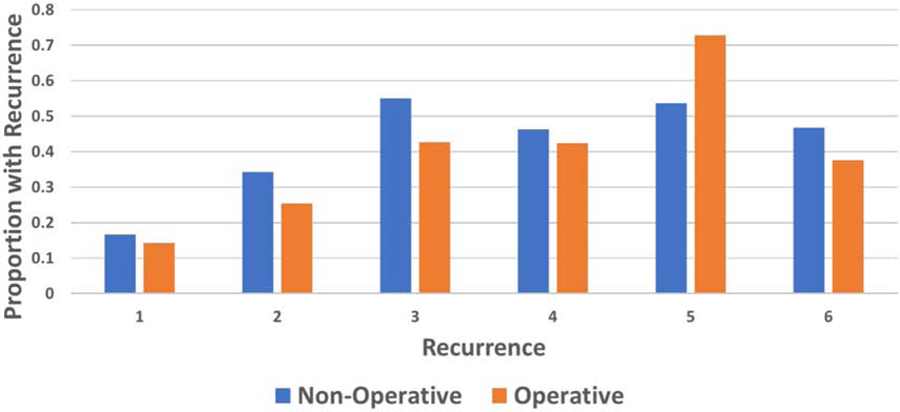
Proportion of patients developing recurrence after each recurrence, stratified by initial adhesive small bowel obstruction management.
Primary outcome
Adjusting for covariates, patients who underwent operative management were less likely to develop recurrence of ASBO in the follow-up period (hazard ratio (HR) 0.27; 95% CI 0.23 to 0.31). For those patients with multiple recurrence, each additional non-operative recurrence increased the risk of recurrence (HR 1.18; 95% CI 1.16 to 1.20), as did each additional operative recurrence (HR 2.30, 95% CI 2.04 to 2.60). Men were less likely to develop recurrence (HR 0.88; 95% CI 0.81 to 2.60).
Secondary outcomes
More patients died during the initial admission if they were managed surgically (3.7% vs. 2.6%, p=0.025). (Table 2) After adjusting for covariates, the hazard of operative ASBO patients dying were 3.89 times the hazard of non-operative patients dying (HR 3.89; 95% CI 2.14 to 7.06). Operative patients were more likely to have an in-hospital myocardial infarction (OR 2.46; 95% CI 1.63 to 3.69), pulmonary embolism (OR 3.26; 95% CI 1.48 to 7.21), pneumonia (OR 3.36; 95% CI 2.69 to 4.19), AKI (OR 2.12; 95% CI 1.74 to 2.57), deep space infection (OR 10.47; 95% CI 6.11 to 17.92), and wound infection (OR 14.4, 95% CI 6.31 to 32.84). No differences were observed between operatively and non-operatively managed ASBO patients for DVT and CVA.
Table 2.
Odds Ratio After Multivariable Logistic Regression for Complications After Operative Management Compared to Nonoperative Management
| Variable | Nonoperative, %, n = 6681 | Operative, %, n = 2379 | Odds ratio | 95% CI |
|---|---|---|---|---|
| Myocardial infarction | 0.75 | 1.14 | 2.46 | (1.63, 3.69) |
| Pulmonary embolism | 0.18 | 0.59 | 3.26 | (1.48, 7.21) |
| Pneumonia | 2.68 | 7.69 | 3.36 | (2.69, 4.19) |
| Acute kidney injury | 4.51 | 8.53 | 2.12 | (1.74, 2.57) |
| Cerebrovascular accident | 0.31 | 0.67 | 1.75 | (0.98, 3.15) |
| Deep space infection | 0.14 | 1.79 | 10.47 | (6.11, 17.92) |
| Wound infection | 0.10 | 1.47 | 14.4 | (6.31, 32.84) |
| Death | 2.61 | 3.53 | 3.89 | (2.14, 7.06) |
The median time to first recurrence was longer for those who underwent operative management compared to those managed non-operatively (729 vs. 550 days, p=0.009).
Discussion
In many institutions, non-operative management with enteral decompression and small-bowel follow-through has become a preferred method for management.(19) The discussed advantages of this approach are the possibility of avoiding the operative risks that are inherent with surgical intervention and that perhaps further contribute to the development of adhesive burden, ultimately predisposing to more ASBOs. For patients managed non-operatively, the length of duration of non-operative management before intervention has been debated. Many surgeons favor longer periods to allow patients to resolve the obstruction without surgery because no increased perioperative morbidity or mortality has been observed when comparing early versus delayed operative management.(20) This study suggests that there may be an unaccounted benefit of reduced risk of ASBO recurrence with operative management which might counterbalance the inherent risk of any surgical intervention.
We found patients who undergo surgery for their initial ASBO have a reduced risk of recurrence than those who were managed without operation, which is comparable to results of a cohort study of ASBO patients in Ontario, Canada that showed a hazard ratio for recurrence of 0.62 favoring surgical management.(14) Our analysis has also demonstrated, for the first time, that additional recurrences are more likely with history of a higher number of previous recurrences for both operative and non-operative patients. The pathogenesis of adhesion development is complex,(21) and the variability in development of postoperative adhesions by individual patient suggests that some patients may have an inherent propensity to develop future recurrences than other patients. Efforts should be made to reduce the likelihood of developing a recurrence because more recurrences portend additional future recurrences.
Given that our data show decreased incidence of recurrence in operatively managed patients when compared to non-operatively managed patients and that decreased number of recurrences portends lower hazard of recurrence, a picture emerges that patients presenting with initial ASBO may benefit by reduced incidence of initial recurrence and subsequent recurrence from surgical intervention than from non-operative management.
Also consistent with prior literature, we show a longer time to recurrence among those managed operatively compared to those managed non-operatively suggesting that the physical removal of the obstruction could have greater impact than just enteral decompression and non-operative management.(6) Increasing the amount of time between recurrence of disease may have substantial impact on quality of life and financial well-being in this subset of patients. Our findings have considerable implications not only in deciding the appropriate management strategy, but also in counseling patients about the risks and benefits of the management options.
The complications associated with both operative and non-operative management must be considered when balancing the benefits of reducing future recurrence. The increased risk of in-hospital mortality as well as perioperative morbidity should be understood. We identified 3.7% in-hospital mortality rate in the operative group while another study found that emergency laparotomy for SBO harbored a 30-day mortality rate of 7.2%.(22) Wound infections and intra-abdominal infections are almost exclusive to the operative patient population, and their development may require further interventions while increasing hospital length of stay. Furthermore, an increased risk for cardiac and pulmonary complications is inherent with any surgical intervention and must be factored into the decision-making process. Any discussion of operative management must consider these complications. For example, an older patient with significant cardiac history may benefit from non-operative management with a higher risk of recurrence. While another patient without significant risk factors may benefit from early operative management and reduced risk of recurrence. Although the complications may be inherently related to the act of performing surgery, this may be another consideration when counseling patients.
Although there remains significant variation in surgeon approach to ASBO, the current paradigm shift of the last decade has been towards non-operative management for ASBO, (23) and Matsushima and colleagues have observed the trend toward decreased operative intervention during admissions for ASBO.(19) It has also been identified that the trend toward earlier operation is increasing and that delayed operative invention beyond 72 hours may have increased mortality.(22) The Eastern Association for the Surgery of Trauma and other groups have recommended initial non-operative management for ASBO, and if no resolution of obstruction is noted, to pursue surgery.(24) The duration of the non-operative management period should be informed by patient risk factors and surgical history; surgeons should consider the long-term improvement that operative management may provide with respect to recurrence and, perhaps, move quickly to operation in the absence of other risk factors.
One of the major strengths of this study is the statewide analysis of recurrence. We anticipated that patients would use multiple hospitals or be transferred for further operative or non-operative management at a higher level of care, thus limiting a true picture of the impact of ASBO on patient lives beyond what can be obtained from any single institutions’ medical record. With this strength comes several limitations to the study, most of which stem from its design as a retrospective cohort study with an administrative database source. This study includes only admission records from the state of Tennessee. Residents who live near the border of states may be able to travel across state lines to receive care at another hospital for their recurrence of ASBO. Furthermore, patient emigration from the state cannot be tracked. The study follow-up period is 10 years, which leaves the potential for emigration from the state. To account for these limitations, we limited the cohort to Tennessee residents to increase the likelihood that patients in the cohort would follow up at a Tennessee hospital compared to a resident from a nearby state who may be more likely to follow-up at a non-Tennessee hospital.
Another limitation is that individual, physiologic, and patient history data are available, a drawback in evaluating a clinical problem. The potential for unmeasured confounding exists Because, for example, patients who present with physiologic instability might force surgeons to treat with an operation more than non-operative management. Additionally, a patient who has had a several abdominal operations in the past is much more likely than someone who has had only one prior abdominal operation. To mitigate this limitation, we excluded patients who had a previous admission for ASBO in the 4 years prior to the study enrollment. We are not able to determine prior operative history beyond this or if there were any other medical events that could contribute to the management decisions. However, our data indicates that the median time to ASBO recurrence is 1.6 years, suggesting that the 4 years prior to 2007 serving as an exclusion period is adequate.
This study also has the potential to initiate further investigations into the value of the care provided by surgeons. It has been difficult modeling long-term value of surgical treatments due to challenges in obtaining and analyzing longitudinal data. The concept of value is multifaceted; however, modeling long-term death, recurrence, and cost together in future studies will be the foundation for ultimately developing a model of value determining the best treatment for patients with SBO and other chronic, surgically-managed diseases.
Conclusion
The initial operative admissions are associated with decreased recurrence risk. However, with each additional operative or non-operative recurrence, the risk of future recurrence is increased for non-operatively and even greater with operative management. ASBO recurrences managed operatively have greater likelihood of in-hospital complications. Weighting the risk-benefit of the recurrence with complications may improve the decision-making process in complex patient populations. Surgeons are often confronted with the decision to operate, and much of the management relies on predictive data for resolution of a single episode of SBO. Our data show long-term consequences must also be considered. Identifying the greater risk of recurrence with non-operative management not only gives providers an additional piece of information when weighing the risks and benefits of ASBO management, but it may predict future hospitalizations based on the prior episodes of bowel obstruction.
Supplementary Material
Acknowledgments
Support: Drs Lindsell, Medvecz and Wang are supported by NIH/National Center for Advancing Translational Sciences Grant (ULI TR00243)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Disclosures outside the scope of this work: Dr Dennis receives honoraria for educational lectures from Prytime Medical.
Presented at the Southern Surgical Association 131st Annual Meeting, Hot Springs, VA, December 2019
REFERENCES
- 1.Barmparas G, Branco BC, Schnüriger B, et al. The Incidence and Risk Factors of Post-Laparotomy Adhesive Small Bowel Obstruction. [Internet]. J. Gastrointest. Surg [Internet] Springer-Verlag; 2010;14:1619–1628. [DOI] [PubMed] [Google Scholar]
- 2.Azagury D, Liu RC, Morgan A, Spain DA. Small bowel obstruction: A practical step-by-step evidence-based approach to evaluation, decision making, and management. J. Trauma Acute Care Surg; 2015;79:661–668. [DOI] [PubMed] [Google Scholar]
- 3.Choi H-K, Chu K-W, Law W-L. Therapeutic Value of Gastrografin in Adhesive Small Bowel Obstruction After Unsuccessful Conservative Treatment A Prospective Randomized Trial. Ann. Surg; 2002;236:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burge J, Abbas SM, Roadley G, et al. Randomized controlled trial of gastrografin in adhesive small bowel obstruction. ANZ J. Surg; 2005;75:672–674. [DOI] [PubMed] [Google Scholar]
- 5.Zielinski MD, Haddad NN, Cullinane DC, et al. Multi-institutional, prospective, observational study comparing the Gastrografin challenge versus standard treatment in adhesive small bowel obstruction. J. Trauma Acute Care Surg; 2017;83:47–54. [DOI] [PubMed] [Google Scholar]
- 6.Foster NM, McGory ML, Zingmond DS, Ko CY. Small Bowel Obstruction: A Population-Based Appraisal. J. Am. Coll. Surg; 2006;203:170–176. [DOI] [PubMed] [Google Scholar]
- 7.O’leary MP, Neville AL, Keeley JA, et al. Predictors of ischemic bowel in patients with small bowel obstruction. Am. Surg; 2016;82:992–994. [PubMed] [Google Scholar]
- 8.Rocha FG. Nonoperative Management of Patients With a Diagnosis of High-grade Small Bowel Obstruction by Computed Tomography. Arch. Surg; 2009;144:1000. [DOI] [PubMed] [Google Scholar]
- 9.Meier RPH, de Saussure WO, Orci LA, et al. Clinical Outcome in Acute Small Bowel Obstruction after Surgical or Conservative Management. World J. Surg; 2014;38:3082–3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barkan H, Webster S, Ozeran S. Factors predicting the recurrence of adhesive small-bowel obstruction. Am J Surg; 1995;170:361–5. [DOI] [PubMed] [Google Scholar]
- 11.Landercasper J, Cogbill TH, Merry WH, et al. Long-term Outcome After Hospitalization for Small-Bowel Obstruction. Arch. Surg; 1993;128:765–771. [DOI] [PubMed] [Google Scholar]
- 12.Springer JE, Bailey JG, Davis PJB, Johnson PM. Management and outcomes of small bowel obstruction in older adult patients: a prospective cohort study. Can. J. Surg; 2014;57:379–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fevang BTS, Fevang J, Lie SA, et al. Long-term prognosis after operation for adhesive small bowel obstruction. Ann. Surg; 2004;240:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Behman R, Nathens AB, Mason S, et al. Association of Surgical Intervention for Adhesive Small-Bowel Obstruction With the Risk of Recurrence. JAMA Surg; 2019:1–8. [DOI] [PMC free article] [PubMed]
- 15.Hajibandeh S, Hajibandeh S, Panda N, et al. Operative versus non-operative management of adhesive small bowel obstruction: A systematic review and meta-analysis. Int. J. Surg; 2017;45:58–66. [DOI] [PubMed] [Google Scholar]
- 16.Miller G, Boman J, Shrier I, Gordon P. Natural history of patients with adhesive small bowel obstruction. Br. J. Surg; 2000;87:1240. [DOI] [PubMed] [Google Scholar]
- 17.Tingstedt B, Isaksson J, Andersson R. Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br. J. Surg; 2007;94:743–748. [DOI] [PubMed] [Google Scholar]
- 18.Amorim LDAF, Cai J. Modelling recurrent events: A tutorial for analysis in epidemiology. Int. J. Epidemiol; 2015;44:324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsushima K, Sabour A, Park C, et al. Management of adhesive small bowel obstruction. [Internet].J. Trauma Acute Care Surg; 2019;86:383–391. [DOI] [PubMed] [Google Scholar]
- 20.Bauer J, Keeley B, Krieger B, et al. Adhesive small bowel obstruction: Early operative versus observational management. Am. Surg; 2015;81:614–620. [PubMed] [Google Scholar]
- 21.Arung W, Meurisse M, Detry O. World J. Gastroenterol 2011;17:4545–4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peacock O, Bassett MG, Kuryba A, et al. Thirty-day mortality in patients undergoing laparotomy for small bowel obstruction. Br. J. Surg; 2018;105:1006–1013. [DOI] [PubMed] [Google Scholar]
- 23.Lavallee DC, Flum DR, Thornblade LW, et al. Surgeon attitudes and practice patterns in managing small bowel obstruction: a qualitative analysis. J. Surg. Res 2017;219:347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maung AA, Johnson DC, Piper GL, et al. Evaluation and management of small-bowel obstruction: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg; 2012;73:362–369. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


