Abstract
Background
The population of older prisoners (age ≥50), a group with high suicide rates, is growing. We sought to explore the associations among functional disability, depression, and suicidal ideation (SI) among older prisoners, focusing on the mediating role of depression.
Methods
Study participants were 220 sentenced male inmates age ≥50 who were incarcerated in 8 prisons. Face-to-face interviews were conducted following consent. Functional disability was assessed objectively, using the Short Physical Performance Battery (SPPB), and via self-report by asking participants their level of difficulty climbing stairs and completing activities necessary for daily living in prison (PADLS) such as standing in line for medications. The PHQ-9 and the Geriatric Suicide Ideation Scale assessed depressive symptoms and SI, respectively. Data were analyzed using linear regression models and causal mediation models.
Results
Participants were racially diverse and ranged from age 50 to 79 years. Whereas each functional disability measure was significantly associated with depressive symptoms, difficulty climbing stairs and PADL disability, but not SPPB score, were independently associated with SI. Depressive symptoms mediated the relationship between functional disability, assessed both objectively and via self-report, and SI.
Limitations
Cross-sectional study design; possible under-sampling of participants with depressive symptoms and SI.
Conclusions
Our findings have implications for suicide prevention in older prisoners. As this population continues to grow, prevention efforts should target those with depression, including but not limited to those with functional disability. Furthermore, assessing functional disability may offer a means of identifying those who should be screened for depression and suicidal ideation.
Keywords: aging, depression, depressive symptoms, suicidal ideation, prisoners
Consistent with the trend seen in community-dwelling individuals age ≥50 (CDC 2019), suicide rates among prisoners are also highest in the second half of life (Noonan 2016). The Bureau of Justice Statistics indicates a suicide rate of more than 19 per 100,000/year among U.S. state prisoners in this age group (Noonan 2016).1 Reducing the number of suicide deaths in the U.S. by targeting high-risk groups, such as prisoners, is an important national goal (Colpe and Pringle 2014; Prevention 2014). Yet, despite rapid growth in the older prison population over the past two decades (Carson 2018; Gilliard and Beck 1998; Luallen and Cutler 2015) and the observation that suicide rates are highest among middle-aged and older persons in general, our knowledge regarding which older prisoners are more likely to die by suicide is limited. This lack of knowledge is compounded by numerous challenges of conducting research in correctional facilities, which can deter investigators from working in this setting (Cislo and Trestman 2013).
Although suicide is a rare outcome, depression and suicidal ideation (SI) are both common and strongly associated with suicide and suicide attempt among those living in prison (Fazel et al. 2008) and among older persons living in the community (Conwell et al. 2002; Conwell et al. 1996). Depression and SI are also prevalent among older prisoners (Barry et al. 2016). Consequently, depression and SI represent targets for intervention, and identifying factors associated with depression and SI can inform best practices for early risk detection and suicide prevention in older prisoners.
Functional disability, such as impaired mobility or impaired ability to conduct instrumental activities of daily living (IADLs), has been shown to be associated with depression and SI among community-dwelling elders even after controlling for physical health problems (He et al. 2019; Lampinen and Heikkinen 2003; Lutz and Fiske 2018; Mellqvist Fassberg et al. 2014; Picazzo-Palencia 2016; Veronese et al. 2017a). In accordance with stress process theory (Pearlin et al. 1981), experiencing functional disability may impede one’s ability to fulfill the expected societal role of living independently, ultimately leading to depression and SI (Russell et al. 2009). Individuals “aging in place” in prison, however, are expected to perform day-to-day activities that are highly unique to this setting. Deemed prison activities of daily living, or PADLs, these are activities such as walking to the chow hall for meals, standing in line for medications, and climbing on/off the top bunk (Williams et al. 2006). Emerging evidence indicates that PADL disability is associated with both depression and suicidal ideation severity in older prisoners, with an especially strong association between PADL disability and depression in males (Barry et al. 2017). Thus, difficulty performing these activities, and therefore being unable to fulfill one’s expected “role” as a prisoner, may explain these relationships.
Because functional disability is an identifiable and modifiable factor that is considerably upstream from suicide, it may be an optimal target for suicide prevention among older prisoners. With the exception of the aforementioned study, however, the relationship between functional disability and suicidal ideation in older prisoners has not been evaluated. We sought to determine the relationship between functional disability, depression, and suicidal ideation in a sample of older prisoners (age ≥50 years) from 8 prisons. To achieve this goal, we operationalized functional disability using both self-reported and performance-based assessments, as they may capture different aspects of functioning (Bean et al. 2011). Self-reported assessments of function tend to reflect individuals’ perspectives regarding their ability to perform an activity in a particular environment. Performance-based measures, on the other hand, provide a standardized, objective indicator of function (Gill 2010). Using the stress process framework, we hypothesized that functional disability would be associated with depression and SI in older prisoners even after controlling for demographic, incarceration-related, and clinical factors. Given the strong relationship between depression and subsequent suicidal ideation (Ribeiro et al. 2018), we also hypothesized that depression would act as a mediator such that functional disability would be associated with higher depressive symptoms, which would subsequently be related to higher suicidal ideation severity.
Methods
Procedure
All subjects were enrolled in the “Aging Inmates’ Suicidal Ideation and Depression Study (Aging INSIDE)” at the University of Connecticut Health Center (UConn Health). The study was approved by the UConn Health Institutional Review Board and by the Research Advisory Committee of the Connecticut Department of Correction (CTDOC). Eligible participants were sentenced male inmates age >50, incarcerated in one of eight CTDOC prisons, English-speaking, and they provided voluntary consent to participate. In addition, eligible participants had an expected release date or parole date that was at least 36 months from the date that the recruitment letter was sent. Because incarcerated individuals are often released or paroled prior to their maximum end-of-sentence date, this latter criteria was included to account for a potential lag between receipt of the recruitment letter and the participant interview.
The CTDOC provided quarterly lists of eligible prisoners to the designated study personnel. Between November 2017 and January 2019, recruitment letters were sent in batches (by facility) to 1,019 eligible prisoners across 8 correctional facilities. Prisoners interested in participating were asked to write their name, Inmate Number, housing unit, and date on page 2 of the letter and to place the completed form in the Medical Requisition Box or deputy warden mailbox, depending on the facility. After retrieving the forms from the 288 (28.3%) inmates who returned the letters indicating their interested in participating, the research assistants (RAs) submitted visitation requests to the respective prison to schedule the eligibility screenings. The two RAs had their master’s degrees, were trained in the responsible conduct of research and how to administer the study measures, and received required safety training through the CTDOC. Meetings between potential participants and an RA were conducted privately in designated areas within each correctional facility (e.g., room in the medical wing; open classroom in the school). The RA reviewed the study purpose and specified that there were neither incentives for participating nor negative consequences for refusing. Prisoners were also asked to describe the study purpose and procedures, in their own words, to ensure their understanding of the study. In addition, in accordance with the study protocol, prisoners were also told during the informed consent process that all of their responses would remain confidential unless they disclosed information requiring clinician referral. Potential participants were informed that “Based on your answers to some of the questions that will be asked during the interview, the researcher may feel that you are at immediate risk of harming yourself. If the researcher thinks that you may harm yourself, the mental health staff will be notified.” A total of 228 (79.2%) of the older prisoners provided written consent. Of the 60 prisoners who submitted a form but did not participate, 40 refused, 10 were not eligible, 1 ended the recruitment interview, 1 was in administrative segregation, and 8 were still deciding if they wanted to participate. Face-to-face interviews occurred immediately thereafter, and data including demographics, age at first incarceration, and current housing were collected. Reviews of medical charts and CTDOC data were completed within approximately 2 weeks of the interviews.
Measures
Depressive symptoms
The 9-item Patient Health Questionnaire (PHQ-9) assessed depressive symptom severity (Kroenke et al. 2001). Participants were asked how often in the past 2 weeks they were bothered by problems including “feeling down, depressed, or hopeless,” and “feeling tired or having little energy.” Symptom frequency is rated from 0 to 3 (“from not at all” to “nearly every day”) with scores ranging from 0 to 27 and higher scores indicate higher severity. In addition, participants underwent a diagnostic assessment of current Major Depressive Episode (MDE) using Module D of the Structured Clinical Interview for DSM-V (SCID) (First 2015). Participants meeting the diagnostic criteria were coded as experiencing a current MDE.
Suicidal Ideation Severity and Past Suicide Attempt
The Geriatric Suicide Ideation Scale (GSIS) assessed SI severity (Heisel and Flett 2006; Heisel and Flett 2015). Study participants indicated their level of agreement with 31 statements using a 5-point Likert scale, from (1) Strongly disagree to (5) Strongly agree. Total scores range from 31 to 165 (Cronbach’s alpha = 0.93) with higher scores indicating higher severity. Responding Agree or Strongly agree to the statement “I have tried ending my life in the past,” which is part of the GSIS but not included in instrument scoring, indicated lifetime suicide attempt.
Functional disability
Self-reported functional disability was assessed using a modified version of the Williams Prison Activities of Daily Living (PADL) Disability Index (Williams et al. 2006). Participants rated their level of difficulty performing five activities specific to living in prison: climbing on/off the top bunk, walking while wearing handcuffs or shackles, standing in line for medications, walking to chow, and cleaning my cell/living space. Those reporting one or more PADL as “very difficult” or “cannot do” were considered as having PADL disability. In addition, study participants were asked about their ability to climb stairs. Participants responding that it is “very difficult” or that they “cannot climb stairs without help” were considered as having reported functional disability.
Functional disability was assessed objectively using the Short Physical Performance Battery (SPPB). The SPPB is a validated instrument that includes the following three timed (in seconds) tasks: a 4-meter walk at one’s usual pace, 5 chair rises (sit-to-stand) without using one’s arms, and maintaining standing balance while feet are side-by-side and in semi-tandem and full-tandem positions (Guralnik et al. 1995; Guralnik et al. 1994). The test, which is designed for a lay interviewer to administer, takes about 10–15 minutes to complete. Each of the three tasks is then scored from 0 to 4, with 0 indicating inability to complete the task and 4 indicating maximum performance. The values are summed to create a total score ranging from 0 to 12 with higher scores representing better performance. Study participants who were confined to a wheelchair (n=8) were unable to complete the SPPB and thus were coded as missing this variable. In addition to the SPPB, we also considered individual objective performance measures as independent variables. Timed gait, time to complete five chairs stands, and time to hold a single leg stance were operationalized as continuous variables.
Other potential covariates
Current age, age at incarceration, and years in prison for the current offense were considered as continuous variables and race was categorized as non-Hispanic white (referent), Black, and Hispanic/Other. Education was dichotomized as completing versus not completing high school or the equivalent. Current housing was dichotomized as single cell no roommate versus other (i.e., single cell with a roommate, dormitory). Type of offense was categorized as violent or non-violent according to the CTDOC Classification Manual. (CTDOC 2012). The CAGE, a 4-question screening test for alcohol dependence (Bush et al. 1987), was administered to participants endorsing lifetime alcohol use. The CAGE acronym refers to the four screening questions which ask if you have you ever felt that you should “cut down” on drinking, if others have “annoyed” you by criticizing your drinking, if you have ever felt “guilty” about drinking, and if you have ever had an “eye-opener” drink, that is, a drink first thing in the morning? Two positive responses indicate possible alcohol dependence. Lifetime illicit drug use (i.e., drugs/medications not prescribed by a physician) was assessed using the Question 1 from the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) version 3.0. (Group 2002). Participants who endorsed ever using an illicit drug were also asked if they were using the drug at the time of incarceration for the current offense. As determined via medical chart review, number of common chronic medical conditions (e.g., hypertension, diabetes, HIV/AIDS, Hepatitis C) was considered as a continuous variable and currently receiving mental health treatment, including medication or counseling, was considered as a dichotomous variable.
Statistical analysis
Descriptive statistics were calculated for participants’ characteristics. We then evaluated the bivariate associations between participants’ characteristics (including the objective and self-reported functional disability measures) and the dependent variables, depressive symptoms and SI severity. Either t-tests or ANOVA tests were used when participants’ characteristics were categorical and either Pearson correlation coefficients or Kruskal–Wallis H tests were used when the characteristics were continuous or count variables, respectively. Regression-based models testing the effect of functional disability on the dependent variables were run, adjusting for age, race, and education. These models also included variables that were significantly (p<0.05) associated with the outcomes in bivariate analyses and/or were theoretically presumed to confound the relationships between the predictors and the dependent variables (e.g., time in prison for the current offense, lifetime suicide attempt; current mental health treatment). Correctional facility was not included as a potential covariate because intra-class correlations for the primary independent variables (objective and self-reported functional disability) and outcomes (depressive symptoms and suicidal ideation severity) did not show significant within-facility homogeneity.
To investigate the precise causal relationship between functional disability (objective and self-reported) and suicidal ideation we used Mplus 8.2 (Muthén and Asparouhov 2015) to estimate causal mediation models (Pearl 2001) that presumed depressive symptoms as a mediating process. These structural equation models rely on maximum likelihood estimation, yet are mere extensions of linear regressions that allow for the same variable to be both a cause and an effect (i.e. mediators) (Muthén et al. 2016). We examined the direct, indirect, and total effects. In the “classical” Baron-Kenny mediation modeling approach (Baron and Kenny 1986), the direct effect explains the pathway from functional disability to suicidal ideation while controlling for depressive symptoms. The indirect effect describes the pathway from functional disability to suicidal ideation through depressive symptoms. The total effect is the sum of the direct and indirect effects of functional disability on suicidal ideation. We specified the causal models to include lifetime suicide attempt and currently receiving mental health treatment to act as confounders of the relationship between depression and suicidal ideation. Furthermore, we retained the predictor-mediator interaction in the mediation model as failure to include the interaction term can bias effect estimates even when it is non-significant (VanderWeele 2015). We report model fit using the chi-square statistic, comparative fit index (CFI) and root mean square error of approximation (RMSEA). Finally, we repeated the mediation models by substituting SPPB score with each of the individual objective performance measures and by substituting current Major Depressive Episode (MDE) for depressive symptoms as assessed by the PHQ-9.
Results
Table 1 presents the characteristics of the study sample. The 220 study participants had an average age of 56.1(SD=6.1) years (range 50 to 79 years) with 24% age ≥60 years. They were racially diverse, and the majority were incarcerated for a violent offense (89.6%), were repeat offenders (70.0%), and were using illicit drugs at the time of incarceration (56.4%). Average age at first incarceration was approximately 28 years, with a range of ages 7 to 76 years. Approximately 28% of the study participants reported a lifetime suicide attempt and a total of 58 (26.5%) of the participants were receiving current mental health treatment. A total of 48% of the participants were considered as having PADL disability and nearly 30% reported experiencing difficulty climbing stairs. Based on the performance-based assessment, average SPPB score was 10.8(SD=1.8). There were moderate correlations between SPPB score and the self-reported measures of PADL disability (rho = −0.26) and difficulty climbing stairs (rho = −0.39)
Table 1.
Characteristics of the study sample.
| Characteristic | N=220 |
|---|---|
| Demographics | |
| Age, mean (SD) | 56.1 (6.1) |
| Race, n(%) | |
| White | 82 (37.2) |
| Black | 94 (42.7) |
| Hispanic/Other* | 42 (19.1) |
| Did not graduate high school, n (%) | 48 (21.8) |
| Incarceration-related factors | |
| Age at first incarceration, mean (SD) | 27.8 (14.6) |
| Violent offense, n (%) | 197 (89.6) |
| Repeat offender, n (%) | 154 (70.0) |
| Years in prison for current offense, mean (SD) † | 13.3 (9.5) |
| Single cell, no roommate, n (%) | 36 (16.4) |
| Clinical and behavioral factors | |
| Number of chronic conditions, mean (SD)§ | 2.1 (1.1) |
| Lifetime history of alcohol abuse, n (%) | 94 (42.7) |
| Illicit drug use at time of incarceration, n (%) | 124 (56.4) |
| Lifetime suicide attempt, n (%) | 62 (28.2) |
| Treatment | |
| Current mental health treatment, n (%)∥ | 58 (26.5) |
| Objective functional disability measures | |
| SPPB score, mean (SD) | 10.8 (1.8) |
| Gait speed in seconds, mean (SD) | 3.6 (1.0) |
| Chair stands time in seconds, mean (SD) | 10.4 (3.5) |
| Single leg stand time in seconds, mean (SD) | 19.9 (11.6) |
| Self-reported functional disability measures | |
| PADL disability, n (%) | 106 (48.2) |
| Difficulty climbing stairs, n (%) | 65 (29.6) |
There were 3 study participants who were missing data regarding race. There were 9 participants coded as Other, with Native American/American Indian (n=6), Native Hawaiian/Pacific Islander (n=1), and Mixed race (n=2).
Range 0.42 years to 37.0 years.
Range 0.02 years to 66.6 years.
Chronic conditions, assessed via medical chart review, included hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, cancer, HIV, and Hepatitis C.
Current mental health treatment includes both medication and/or counseling and could not be determined for 1 participant.
SPPB = Short Physical Performance Battery
PADL = Prison Activities of Daily Living
Mean PHQ-9 score was 6.0(SD=5.7) and there were 25(11.4%) participants who met criteria for a current major depressive episode (MDE). The mean GSIS score was 60.3(SD=18.8), range 33 to 139. Average GSIS score for the 25 participants experiencing a current MDE was 79.8(SD=25.3). Average depressive symptoms scores and average GSIS scores were significantly (at the p<0.05 level) higher among participants who did not complete high school, had a lifetime suicide attempt, and were receiving current mental health-related treatment, and were significantly lower among Blacks as compared with non-Hispanic whites and Hispanics.
Table 2 provides the results from the linear regression models. The self-reported measures of functional disability, difficulty climbing stairs and PADL disability, were each positively associated with the two outcomes (p < 0.001) both before and after adjustment. The findings were consistent when depressive symptoms, assessed using the PHQ-9, was substituted with current major depressive episode (MDE). In unadjusted analyses, SPPB score was associated with both depressive symptoms (p<0.01) and suicidal ideation (p < 0.01). Yet, after adjustment, the association between SPPB score and suicidal ideation no longer reached statistical significance. In addition, neither SPPB score nor any of its individual components was associated with MDE.
Table 2.
Unadjusted and adjusted results from the linear regression models.
| Depressive Symptoms | Suicidal Ideation | |||||||
|---|---|---|---|---|---|---|---|---|
| Functional Disability | Unadjusted | Adjusted* | Unadjusted | Adjusted* | ||||
| Self-reported measures | Beta estimate (SD) | t-statistic, p-value | Beta estimate (SD) | t-statistic, p-value | Beta estimate (SD) | t-statistic, p-value | Beta estimate (SD) | t-statistic, p-value |
| PADL disability | 3.83 (0.73) | 5.25, <0.001 | 2.81 (0.68) | 4.15, <0.001 | 9.03 (2.43) | 3.71, <0.001 | 6.45 (2.22) | 2.90, 0.004 |
| Difficulty climbing stairs | 4.74 (0.77) | 6.18, <0.001 | 3.24 (0.75) | 4.33, <0.001 | 11.41 (2.58) | 4.42, <0.001 | 6.27 (2.48) | 2.53, 0.01 |
| Objective measures | ||||||||
| SPPB total | −0.87 (0.21) | 4.15, <0.001 | −0.63 (0.21) | −3.02, <0.01 | −2.20 (0.73) | −3.03, 0.003 | −0.99 (0.71) | −1.39, 0.17 |
| Timed gait | 0.74 (0.39) | 1.88, 0.06 | 0.77 (0.37) | 2.10, 0.04 | 1.76 (1.31) | 1.34, 0.18 | 1.41 (1.22) | 1.16, 0.25 |
| Chair stands time | −0.01 (0.11) | −0.07, 0.95 | 0.03 (0.10) | 0.30, 0.77 | 0.29 (0.37) | 0.77, 0.44 | 0.52 (0.35) | 1.48, 0.14 |
| Single-leg balance time | −0.06 (0.03) | −1.8.2, 0.07 | −0.02 (0.03) | −0.59, 0.56 | 0.02 (0.11) | 0.14, 0.89 | 0.17 (0.11) | 1.52, 0.13 |
SPPB = Short Physical Performance Battery; PADL = Prison Activities of Daily Living
Adjusted for age, race, education, age at first incarceration, time spent in prison for the current offense, residing in a single cell with no roommate, number of chronic conditions, lifetime suicide attempt, and currently receiving mental health treatment.
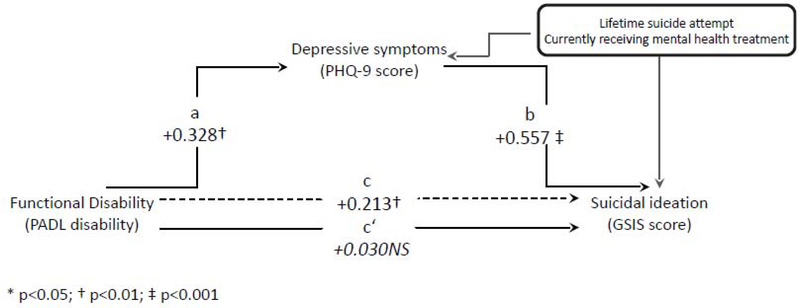
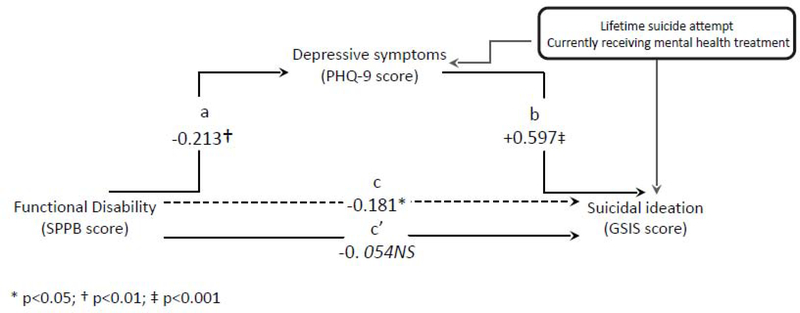
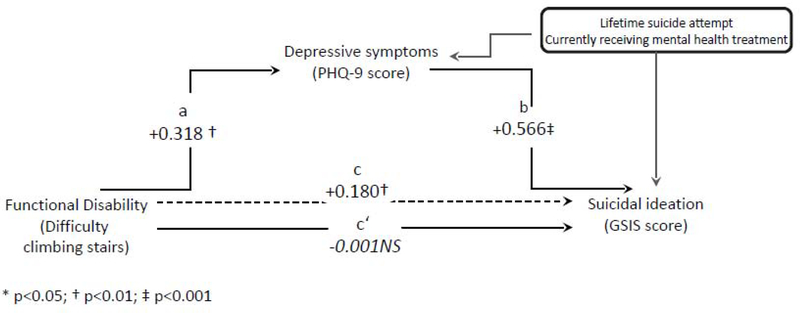
Figures 1a–1c present the standardized beta estimates from the causal mediation models. In each model, the original path (shown as c’) between the functional disability measure and suicidal ideation was non-significant when considering depressive symptoms as a mediator (shown as c). Depressive symptoms accounted for at least 70% of the relation between objective functional disability (as measured by the SPPB) and suicidal ideation (as measured by the GSIS). The amount of variance explained by depressive symptoms increased to 86% for the relation between PADL disability and suicidal ideation, and explained 100% of the relation between self-reported difficulty climbing stairs and SI. The interactions between depressive symptoms and the three functional disability variables, respectively, were non-significant. Additionally, each of the three models had reasonably good fit, as indicated by the χ2 and RMSEA values. The final standardized effect estimates indicate that the total effect of PADL on GSIS (total effect = 0.213; p<0.01) was stronger than the standardized effect estimates of difficulty climbing stairs (total effect = 0.180; p<0.01) and SPPB score (total effect = −0.181; p<0.05) on GSIS, respectively. We also found that depressive symptoms was a mediator of the relationship between timed gait and SI (total effect= −0.156; p<0.05). However, when substituting major depressive episode (MDE) for PHQ-9 score in the causal mediation models, depression was no longer a mediator of the relationship between functional disability and suicidal ideation.
Figure 1a:
Mediation of self-reported functional disability (PADL disability) and suicidal ideation (GSIS score) by depressive symptoms (PHQ-9 score). χ2(31) = 59.532, p = 0.002, CFI = 0.880, RMSEA = 0.066, 95%CI (0.040; 0.091); indirect effect = 0.183. Unstandardized beta estimate(SE) for the PADL by PHQ-9 interaction = 0.270(1.312), p=0.837.
Figure 1c:
Mediation of objective functional disability (SPPB score) and suicidal ideation (GSIS score) by depressive symptoms (PHQ-9 score). Model fit statistics: χ2(16) = 41.538, p < 0.001, CFI = 0.912, RMSEA = 0.054, 95%CI (0.024; 0.081); indirect effect = −0.127. Unstandardized beta estimate(SE) for the SPPB by PHQ-9 interaction = −0.044(0.047), p=0.324.
Notes: *Unstandardized beta weight is significant at p<0.05; †Unstandardized beta weight is significant at p<0.01. ‡Unstandardized beta weight is significant at p<0.001. Co-predictors of GSIS in each model are age, Black race, Hispanic ethnicity, education, time in prison for the current offense, age at first incarceration, residing in a single cell with no roommate, and number of chronic conditions.
Discussion
The population of older prisoners, a group with high suicide rates, is increasing rapidly. Importantly, a growing number of studies highlight the prevalence of suicidal ideation among older prisoners, with the majority of the research occurring outside of the U.S. (Di Lorito et al. 2018; Haesen et al. 2019). Largely missing from the literature, however, is a focus on actionable factors that are specific to this vulnerable population. Building on prior research, we found that self-reported functional disability, operationalized as difficulty conducting activities needed for daily living in prison or difficulty climbing stairs, is independently associated with both depression and suicidal ideation in older prisoners. In addition, we found that by largely acting through depression, increasingly lower (worse) performance-based functional disability scores are associated with higher suicidal ideation severity.
In an earlier preliminary study, that included 167 male and female inmates age ≥50 years from 3 Connecticut prisons, we found that PADL disability was associated with depression and worse suicidal ideation, with a particularly strong effect in males (Barry et al. 2017). In the current study, which focused on male inmates across 8 prisons in CT, we evaluated a broader range of functional disability that not only included PADL disability, but also included mobility disability and objective assessments of function. Consistent with the earlier findings, our results again indicated that self-reported rating of PADL disability was strongly associated with depression and SI, even after controlling for important confounders such as lifetime suicide attempt and whether one currently receives mental health-related treatment in the regression models. Average PHQ-9 scores and GSIS scores were approximately 3 points and 6 points higher, respectively, than those without PADL disability. Moreover, we found similar results when comparing those with and without self-reported difficulty climbing stairs. These differences are clinically meaningful, particularly bearing in mind that the study participants’ average scores on these measures are already considerably higher than those of the same age living in the community (Heisel and Flett 2006; Tomitaka et al. 2018). Consequently, whether operationalized as PADL disability or difficulty climbing stairs, self-reported functional disability was positively associated with these outcomes.
Findings from the regression models further indicated that performance-based functional disability, operationalized as SPPB score and as timed gait, was significantly associated with depressive symptoms; as SPPB score decreased, depressive symptoms score increased. However, unlike self-reported functional disability, performance-based functional disability was not independently associated with SI. Taken together, these findings suggest that the meaningfulness and relevance of functional limitations in older inmates’ daily lives, as indicated through their self-ratings of function, may be more closely related to SI than what is measured objectively. It is possible that we would have seen a direct association between performance-based functional disability and SI had we used an objective measure known to provide a wider range of variability in higher-functioning individuals, such as the 400-meter walk (Sayers et al. 2006). In the present study, while the average SPPB score was 10.8 (SD=1.8) for the sample, even those who reported PADL disability or difficulty climbing stairs had average SPPB scores of 10.4 (SD=2.2) and 9.8 (SD=2.6), respectively. As SPPB score ≤9 has previously been considered an indicator of poor physical performance (Guralnik et al. 1994; Veronese et al. 2017b), the aforementioned mean scores indicate that even those older prisoners who report some functional disability may still have been able to complete the SPPB tasks relatively quickly. Thus, future studies that utilize multiple objective measures of performance are needed to confirm our results.
We also found that functional disability, regardless of how it was operationalized, had an indirect association with SI by largely working through depressive symptoms. In particular, when considering depressive symptoms as a mediator, the total effect of PADL disability on SI was especially strong. These findings have important implications for suicide prevention in the prison setting. On one level, considering the strong relationship between depression and SI in older prisoners, prevention efforts should target those with depression, including but not limited to those with functional disability. On another level, selectively targeting those with functional disability may be a useful strategy for reducing incident depression ─ a preventive approach that is considerably upstream from suicide.
Screening for depression in older prisoners with PADL disability or difficulty climbing stairs may help to detect those who, even despite treatment, may still have significant depressive symptoms that put them at increased risk for suicide. These findings provide rationale for developing studies to test prison-based interventions directed towards older prisoners with functional disability. For example, the options of geriatric-specific housing and/or housing close to the dining hall (i.e., chow) or medical facilities are potential means of adapting correctional facilities to better accommodate older prisoners with functional disability (Kerbs and Jolley 2009). Such interventions may minimize these difficulties and subsequently alter the trajectory from functional disability to depression and subsequent SI. However, these interventions must be balanced in accordance with Title II of the Americans with Disabilities Act (ADA) (Subpart D: § 35.152; Part 35 Nondiscrimination on the Basis of Disability in State and Local Government Services (as amended by the final rule published on August 11, 2016)). This regulation indicates that regardless of disability status, prisoners must be housed in integrated settings that are appropriate for their classification (a rating that considers factors such as escape profile, severity/violence of the current offense, and length of sentence) and that provide access to all programs for which they are eligible. Considering the high proportion of self-reported functional disability in older prisoners reported in our study and elsewhere (Bronson and Berzofsky 2015; Greene et al. 2018; Leigey and Hodge 2012; Williams et al. 2006), maintaining this balance may become more difficult as the number of older prisoners continues to grow.
Our findings also have implications for when older prisoners transition from prison back to the community. Whereas this transition poses challenges for those of any age, those returning to the community in later life may be especially vulnerable given their high rates of chronic conditions and estrangement from family and friends due to long periods of incarceration. Moreover, recent findings indicate that those transitioning from prison to the community in later life are at high risk for suicide attempt and death by drug overdose or other accidental injury (Barry et al. 2018). Considering the association between functional disability, depression and suicidal ideation found in the present study, those with functional disability may be at especially high risk of suicidal behavior upon release. Future research is needed to evaluate how functional disability during incarceration impacts rates of depression and suicidal behaviors once these older individuals reenter the community.
A considerable strength of the present study was operationalizing functional disability using both self-reported and performance-based measures. Assessing functional disability in different ways, yet finding generally consistent outcomes, demonstrates the strength of functional disability as an important factor in the context of depression and suicidal ideation in older prisoners. To the best of our knowledge, the present study is the first study to conduct performance-based assessments of function in older prisoners. Thus, we have shown that it is feasible to assess objective measures of function in the prison setting. Furthermore, conducting research “on the inside” is particularly onerous. Administrative challenges include obtaining the necessary permissions and safety training to go “inside” and dealing with multiple layers of review regarding human subjects protections. Methodological challenges include working around inmate headcount schedules that occur multiple times per day and dealing with unexpected events such as lockdowns that may last from several hours to several days. Despite these challenges, we were able to successfully recruit and interview 220 older prisoners.
There are, however, several limitations to note. With a 28% response rate, the Aging INSIDE study sample may not be representative of all older, sentenced prisoners in the U.S. Other approaches to recruiting older prisoners, such as mailed surveys, have also resulted in relatively low response rates thus reflecting that recruitment challenges are an inherent part of conducting research with prisoners (Maschi et al. 2014; Skarupski et al. 2015). Furthermore, it is possible that those individuals who were more depressed and/or were experiencing feelings of suicidal ideation may have been less willing to participate, thereby resulting in systematic under-sampling of older prisoners with these conditions. The cross-sectional design of the present study precludes the ability to make causal inferences. However, by using causal mediation models, we found that functional disability works through depression to impact SI, thus suggesting that functional disability and depression likely precede SI. Longitudinal studies are need to clarify the temporal relationship among functional disability, depression, and SI. Finally, we were also not able to include non-English-speaking prisoners.
Our findings indicate that functional disability, and particularly ratings of disability specific to the prison setting, is both directly associated with suicidal ideation and indirectly associated with this outcome through depression. As the population of older prisoners in the U.S. continues to grow, assessing functional disability may offer a means of identifying those who should be screened for depression and suicidal ideation. Ultimately, functional assessments may play an integral role in the design and implementation of interventions to reduce suicide-related morbidity and mortality in this high-risk group.
Figure 1b:
Mediation of self-reported functional disability (difficulty climbing stairs) and suicidal ideation (GSIS score) by depressive symptoms (PHQ-9 score). Model fit statistics: χ2(31) = 50.421, p = 0.015, CFI = 0.884, RMSEA = 0.064, 95%CI (0.038; 0.089); indirect effect = 0.180. Unstandardized beta estimate(SE) for the difficulty climbing stairs by PHQ-9 interaction = 0.031(0.189), p=0.871.
HIGHLIGHTS.
First study to evaluate functional disability in older prisoners using both self-report and performance-based assessments.
Functional disability is directly associated with both depression and suicidal ideation in older prisoners.
Functional disability, particularly ratings of disability specific to the prison setting, is indirectly associated with suicide ideation through depression.
ACKNOWLEDGEMENTS
We thank Deborah Noujaim, MPH and Danielle Zaugg, MSW, LCSW for assistance with recruitment, data collection and data entry.
Funding: This work was supported by the National Institute of Health/National Institute of Mental Health (L.C. Barry) under grant number R01 MH106529.
Abbreviations
- GSIS
Geriatric Suicide Ideation Scale
- Aging INSIDE
Aging Inmates’ Suicidal Ideation and Depression Study
- CTDOC
Connecticut Department of Correction
- PADL
Prison activities of daily living
- SPPB
Short Physical Performance Battery
- SI
suicidal ideation
Footnotes
CONFLICT OF INTEREST
There are no conflicts of interest to report.
Declarations of interest: None.
Suicide rates are only available for prisoners age 55 years and older.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations J Personality Soc Psychol 51:1173–1182 doi: 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Barry LC, Steffens DC, Covinsky KE, Conwell Y, Li Y, Byers AL (2018) Increased Risk of Suicide Attempts and Unintended Death Among Those Transitioning From Prison to Community in Later Life Am J Geriatr Psychiatry 26:1165–1174 doi: 10.1016/j.jagp.2018.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry LC, Wakefield DB, Trestman RL, Conwell Y (2016) Active and Passive Suicidal Ideation in Older Prisoners. Crisis 37:88–94 doi: 10.1027/0227-5910/a000350 [DOI] [PubMed] [Google Scholar]
- Barry LC, Wakefield DB, Trestman RL, Conwell Y (2017) Disability in prison activities of daily living and likelihood of depression and suicidal ideation in older prisoners Int J Geriatr Psychiatry 32:1141–1149 doi: 10.1002/gps.4578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bean JF, Olveczky DD, Kiely DK, LaRose SI, Jette AM (2011) Performance-based versus patient-reported physical function: what are the underlying predictors? Phys Ther 91:1804–1811 doi: 10.2522/ptj.20100417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronson J, Berzofsky M (2015) Disabilities Among Prison and Jail Inmates, 2011–12; U.S. Department of Justice,Report NCJ 249151; December 2015. [Google Scholar]
- Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD (1987) Screening for alcohol abuse using the CAGE questionnaire Am J Med 82:231–235 [DOI] [PubMed] [Google Scholar]
- Carson EA (2018) Prisoners in 2016. U.S. Department of Justice, Bureau of Justice Statistics; January 2018, NCJ 251149 [Google Scholar]
- CDC (2019) Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS) https://wisqars.cdc.gov:8443/nvdrs/nvdrsController.jsp Accessed on April 23, 2019. [Google Scholar]
- Cislo AM, Trestman R (2013) Challenges and solutions for conducting research in correctional settings: the U.S. experience Int J Law Psychiatr 36:304–310 doi: 10.1016/j.ijlp.2013.04.002 [DOI] [PubMed] [Google Scholar]
- Colpe LJ, Pringle BA (2014) Data for building a national suicide prevention strategy: what we have and what we need Am J Prev Med 47:S130–136 doi: 10.1016/j.amepre.2014.05.024 [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Caine ED (2002) Risk factors for suicide in later life Biol Psychiatry 52:193–204 doi:S0006322302013471 [pii] [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED (1996) Relationships of age and Axis I diagnoses in victims of completed suicide: a psychological autopsy study Am J Psychiatry 153:1001–1008 [DOI] [PubMed] [Google Scholar]
- CTDOC (2012) Connecticut Department of Correction Objective Classification Manual Rev. 4/12; Available at https://portal.ct.gov/-/media/DOC/Pdf/PDFReport/ClassificationManualLibraryCopypdf.pdf. Accessed on August 5, 2019. [Google Scholar]
- Di Lorito C, Vllm B, Dening T (2018) Psychiatric disorders among older prisoners: a systematic review and comparison study against older people in the community Aging Ment Health 22:1–10 doi: 10.1080/13607863.2017.1286453 [DOI] [PubMed] [Google Scholar]
- Fazel S, Cartwright J, Norman-Nott A, Hawton K (2008) Suicide in prisoners: a systematic review of risk factors J Clin Psychiatry 69:1721–1731 doi:ej07r03949 [pii] [PubMed] [Google Scholar]
- First MB (2015) Structured Clinical Interview for the DSM (SCID) The Encyclopedia of Clinical Psychology. 1–6. Wiley-Blackwell; Cautin Robin L. (Eds.). [Google Scholar]
- Gill TM (2010) Assessment of function and disability in longitudinal studies J Am Geriatr Soc 58 Suppl 2:S308–312 doi: 10.1111/j.1532-5415.2010.02914.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliard D, Beck AJ (1998) Prisoners in 1997. U.S. Department of Justice, Bureau of Justice Statistics; August 1998, NCJ 170014 [Google Scholar]
- Greene M, Ahalt C, Stijacic-Cenzer I, Metzger L, Williams B (2018) Older adults in jail: high rates and early onset of geriatric conditions Health Justice 6:3 doi: 10.1186/s40352-018-0062-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group WAW (2002) The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility Addiction 97:1183–1194 [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB (1995) Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England J Med 332:556–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM et al. (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission J Gerontol 49:M85–94 [DOI] [PubMed] [Google Scholar]
- Haesen S, Merkt H, Imber A, Elger B, Wangmo T (2019) Substance use and other mental health disorders among older prisoners Int J Law Psychiatr 62:20–31 doi: 10.1016/j.ijlp.2018.10.004 [DOI] [PubMed] [Google Scholar]
- He M et al. (2019) Association between activities of daily living disability and depression symptoms of middle-aged and older Chinese adults and their spouses: A community based study J Affect Disord 242:135–142 doi: 10.1016/j.jad.2018.08.060 [DOI] [PubMed] [Google Scholar]
- Heisel MJ, Flett GL (2006) The development and initial validation of the geriatric suicide ideation scale Am J Geriatr Psychiatry 14:742–751 14/9/742 [pii] doi: 10.1097/01.JGP.0000218699.27899.f9 [DOI] [PubMed] [Google Scholar]
- Heisel MJ, Flett GL (2015) Investigating the psychometric properties of the Geriatric Suicide Ideation Scale (GSIS) among community-residing older adults Aging Ment Health:1–14 doi: 10.1080/13607863.2015.1072798 [DOI] [PubMed] [Google Scholar]
- Kerbs JJ, Jolley JM (2009) A commentary on age segregation for older prisoners: philosophical and pragmatic considerations for correctional systems Criminal Justice Rev 34: 119–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure J Gen Intern Med 16:606–613 doi:jgi01114 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampinen P, Heikkinen E (2003) Reduced mobility and physical activity as predictors of depressive symptoms among community-dwelling older adults: an eight-year follow-up study Aging Clin Exp Res 15:205–211 [DOI] [PubMed] [Google Scholar]
- Leigey ME, Hodge JP (2012) Gray Matters: Gender Differences in the Physical and Mental Health of Older Inmates Women & Criminal Justice 22:289–308 [Google Scholar]
- Luallen J, Cutler C (2015) The Growth of Older Inmate Populations: How Population Aging Explains Rising Age at Admission J Gerontol B Psychol Sci Soc Sci 72:888–900 doi: 10.1093/geronb/gbv069 [DOI] [PubMed] [Google Scholar]
- Lutz J, Fiske A (2018) Functional disability and suicidal behavior in middle-aged and older adults: A systematic critical review J Affect Disord 227:260–271 doi: 10.1016/j.jad.2017.10.043 [DOI] [PubMed] [Google Scholar]
- Maschi T, Viola D, Morgen K (2014) Unraveling trauma and stress, coping resources, and mental well-being among older adults in prison: empirical evidence linking theory and practice Gerontologist 54:857–867 doi: 10.1093/geront/gnt069 [DOI] [PubMed] [Google Scholar]
- Mellqvist Fassberg M et al. (2014) Functional disability and death wishes in older Europeans: results from the EURODEP concerted action Soc Psychiatry Psychiatr Epidemiol 49:1475–1482 doi: 10.1007/s00127-014-0840-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T (2015) Causal effects in mediation modeling: An introduction with applications to latent variables Structural Equation Modeling: A Multidisciplinary Journal 22:12–23 [Google Scholar]
- Muthén B, Muthén L, Asparouhov T (2016) Regression and mediation analysis using Mplus Noonan ME (2016) Mortality in Local Jails and State Prisons, 2000–2014 - Statistical Tables. U.S. Department of Justice, Bureau of Justice Statistics; December 2016, NCJ 250150 [Google Scholar]
- Pearl J (2001) Direct and indirect effects In: Proceedings of the seventeenth conference on uncertainty in artificial intelligence Morgan Kaufmann Publishers Inc; https://arxiv.org/ftp/arxiv/papers/1301/1301.2300.pdf, pp 411–420 [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT (1981) The stress process Journal of Health & Social Behavior 22:337–356 [PubMed] [Google Scholar]
- Picazzo-Palencia E (2016) Depression and Mobility Among Older Adults in Mexico: ENSANUT 2012 Hispanic Health Care Int 14:94–98 doi: 10.1177/1540415316650846 [DOI] [PubMed] [Google Scholar]
- Prevention NAAfS (2014) Research Prioritization Task Force A prioritized research agenda for suicide prevention: An action plan to save lives. National Institute of Mental Health and the Research Prioritization Task Force; Rockville, MD [Google Scholar]
- Ribeiro JD, Huang X, Fox KR, Franklin JC (2018) Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies Br J Psychiatry 212:279–286 doi: 10.1192/bjp.2018.27 [DOI] [PubMed] [Google Scholar]
- Russell D, Turner RJ, Joiner TE (2009) Physical disability and suicidal ideation: a community-based study of risk/protective factors for suicidal thoughts Suicide Life Threat Behav 39:440–451 doi: 10.1521/suli.2009.39.4.44010.1521/suli.2009.39.4.440 [pii] [DOI] [PubMed] [Google Scholar]
- Sayers SP, Guralnik JM, Newman AB, Brach JS, Fielding RA (2006) Concordance and discordance between two measures of lower extremity function: 400 meter self-paced walk and SPPB Aging-Clin Exp Res 18:100–106 [DOI] [PubMed] [Google Scholar]
- Skarupski KA, Parisi JM, Thorpe R, Tanner E, Gross D (2015) The association of adverse childhood experiences with mid-life depressive symptoms and quality of life among incarcerated males: exploring multiple mediation Aging Ment Health:1–12 doi: 10.1080/13607863.2015.1033681 [DOI] [PubMed] [Google Scholar]
- Tomitaka S, Kawasaki Y, Ide K, Akutagawa M, Ono Y, Furukawa TA (2018) Stability of the Distribution of Patient Health Questionnaire-9 Scores Against Age in the General Population: Data From the National Health and Nutrition Examination Survey Front Psychiatry 9:390 doi: 10.3389/fpsyt.2018.00390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele T (2015) Explanation in causal inference: methods for mediation and interaction. Oxford University Press; New York, NY [Google Scholar]
- Veronese N et al. (2017a) Frailty and incident depression in community-dwelling older people: results from the ELSA study Int J Geriatr Psychiatry 32:e141–e149 doi: 10.1002/gps.4673 [DOI] [PubMed] [Google Scholar]
- Veronese N et al. (2017b) Poor Physical Performance Predicts Future Onset of Depression in Elderly People: Progetto Veneto Anziani Longitudinal Study Phys Ther 97:659–668 doi: 10.1093/ptj/pzx017 [DOI] [PubMed] [Google Scholar]
- Williams BA, Lindquist K, Sudore RL, Strupp HM, Willmott DJ, Walter LC (2006) Being old and doing time: functional impairment and adverse experiences of geriatric female prisoners J Am Geriatr Soc 54:702–707 10.1111/j.15325415.2006.00662.x [DOI] [PubMed] [Google Scholar]