Case presentation
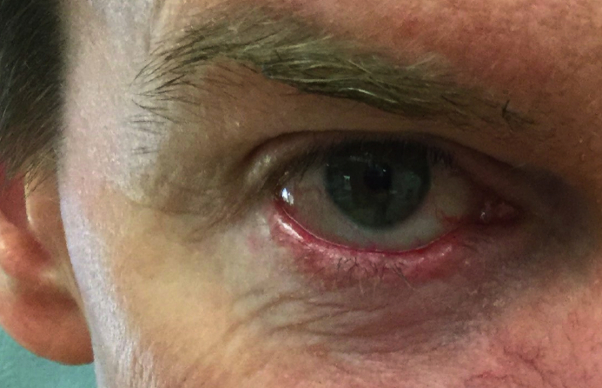
A 49-year-old man with a history of oculocutaneous rosacea and numerous nonmelanoma skin cancers presented for treatment of a biopsy-proven nodular basal cell carcinoma (BCC) of the medial right side of the lower eyelid margin, measuring 0.5 × 0.8 cm (Fig 1). There was no visible medial canthus involvement, but madarosis of the lower lid was present. Mohs micrographic surgery was performed. On microscopic examination of the first stage, a palisaded basaloid proliferation consistent with BCC was noted within the lacrimal canaliculus (Fig 2, A and B) on multiple sections. Sectioning through the block revealed no adjacent or contiguous BCC. Intraoperative consultation with a dermatopathologist confirmed intraductal BCC. A subsequent stage revealed no persisting tumor in the margins.
Fig 1.
BCC of the medial right side of the lower eyelid margin.
Fig 2.
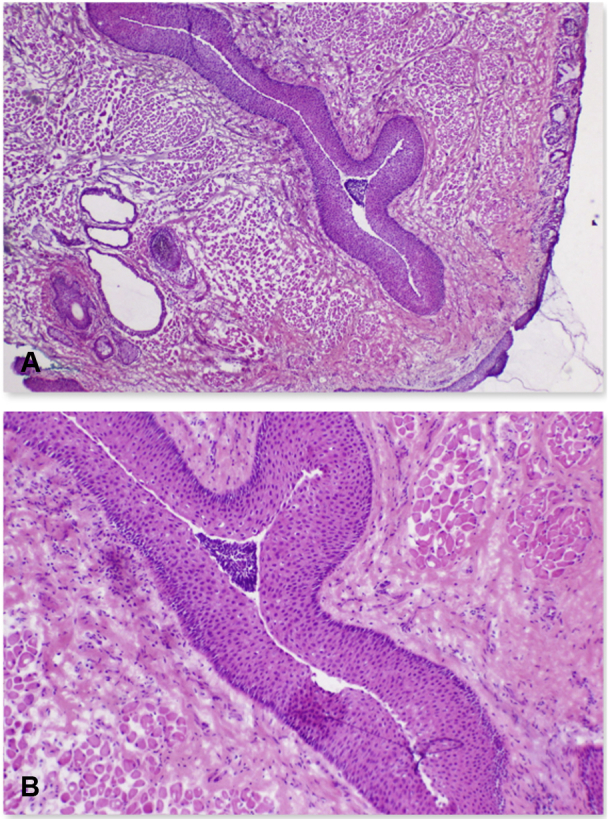
BCC within the lacrimal canaliculus. (A and B, Hematoxylin-eosin stain; original magnifications: A, ×4; B, ×10.)
Discussion
BCC is the most common periorbital epithelial malignancy, with a majority of these involving the medial canthus or lower eyelid.1 There are a number of reported cases of BCC invasion of the lacrimal caruncle, lacrimal gland, or nasolacrimal duct. There are also several reported cases of primary BCC arising in the lacrimal system. However, BCC invasion of the lacrimal canaliculus or lacrimal sac is rare, with only 6 previously reported cases1, 2, 3, 4, 5 (Table I).
Table I.
Published reports of basal cell carcinoma invasion of the lacrimal canaliculus or lacrimal sac
| Authors | Date published | Patient age, years | Patient sex | Location | Recurrence (initial treatment modality) | Treatment |
|---|---|---|---|---|---|---|
| Garrett et al2 | 1993 | 63 | M | Canaliculus | Yes (Mohs) | Mohs (3 stages) |
| Fosko et al1 | 1997 | n1: 30 n2: 62 |
n1: F n2: M |
n1: canaliculus n2: canaliculus |
n1: yes (laser) n2: yes (n/a) |
n1: Mohs (3 stages) n2: Mohs (2 stages) |
| Hatano et al3 | 1999 | 66 | F | Canaliculus | No | Wide local excision |
| Altan-Yaycioglu et al5 | 2007 | 58 | F | Lacrimal sac | No | Dacryocystorhinostomy |
| Katircioglu et al4 | 2007 | 53 | F | Lacrimal sac | No | Excision |
F, Female sex; M, male sex; n/a, not applicable.
BCCs near the medial canthus may invade the lacrimal apparatus through direct spread along the mucosa,1,2 which likely occurred in our patient. BCC was noted within the lacrimal canaliculus, with no invasive component surrounding the lacrimal canaliculus (Fig 1). Fosko et al1 similarly reported 2 cases of BCC involving the lacrimal system while suggesting tumor spread was via direct mucosal extension. The tarsal plate and medial canthal tendon are thought to provide a structural resistance, resulting in “shelving and skating” of the tumor along the path of least resistance.1,3 This mechanism of invasion could explain why periocular BCCs can involve the nasal cavity without destruction of nasal cartilage or bone, resulting in subtle clinical features yet extensive tissue spread.3
An understanding of the lacrimal system anatomy is helpful when surgery is performed in the area. Tears drain from the lacrimal gland (located superolaterally above the eye) into the lacrimal lake at the medial canthus. They are then suctioned through the lacrimal puncta (located medially on upper and lower eyelid margins) into the lacrimal canaliculi via contraction of the lid retractors. The lacrimal canaliculi then join the dilatated portion of the nasolacrimal duct, called the lacrimal sac. The nasolacrimal duct further drains into the inferior nasal meatus in the nasal cavity.
Lacrimal tumors may present as epiphora, induration, recurrent swelling, or dacryocystitis, all of which are the result of lacrimal system obstruction.1, 2, 3 Madarosis, as was observed in our patient, can indicate invasion along the tarsal plate,1 which can result in shelving and skating of the tumor along mucosal surfaces and ultimately in the lacrimal system, as mentioned previously.
Appropriate primary treatment for medial canthus BCCs is paramount because recurrence in this area is particularly high, predominantly because of inadequate excision and underestimation of the extent of invasion.3 Mohs micrographic surgery is regarded to be the most efficacious means of treating periocular BCC owing to its high cure rate in this area.1, 2, 3 Although rare, lacrimal system involvement should be considered when BCCs involving the medial canthus and medial eyelid margin are treated, and surgeons performing Mohs micrographic surgery should closely examine the lacrimal system histologically even when there is no obvious tumor surrounding it. In any case of lacrimal involvement, close long-term follow-up is recommended to monitor for recurrence.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Fosko S., Gibney M., Holds J. Basal cell carcinoma involving the lacrimal canaliculus. A documented mechanism of tumor spread. Dermatol Surg. 1997;23(3):203–206. doi: 10.1111/j.1524-4725.1997.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 2.Garrett A., Dufresne R., Ratz J.L., Berlin A.J. Basal cell carcinoma originating in the lacrimal canaliculus. Opthalmic Surg. 1993;24(3):197–199. [PubMed] [Google Scholar]
- 3.Hatano Y., Terashi H., Kurata S. Invasion of the lacrimal system by basal cell carcinoma. Dermatol Surg. 1999;25(10):823–826. doi: 10.1046/j.1524-4725.1999.99013.x. [DOI] [PubMed] [Google Scholar]
- 4.Katircioglu Y.A., Yildez E.H., Kocaoglu F.A. Basal cell carcinoma in lacrimal sac. Orbit. 2007;26(4):303–307. doi: 10.1080/01676830600987441. [DOI] [PubMed] [Google Scholar]
- 5.Altan-Yaycioglu R., Bolat F., Akova Y.A. Basosquamous carcinoma of the lacrimal sac: a case report. Orbit. 2007;26(4):267–269. doi: 10.1080/01676830600987565. [DOI] [PubMed] [Google Scholar]