Abstract
Exposure to different air pollutants has been linked to type 2 diabetes mellitus, but the evidence for the association between air pollutants and gestational diabetes mellitus (GDM) has not been systematically evaluated. We systematically retrieved relevant studies from PubMed, Embase, and the Web of Science, and performed stratified analyses and regression analyses. Thirteen studies were analyzed, comprising 1 547 154 individuals from nine retrospective studies, three prospective studies, and one case–control study. Increased exposure to particulate matter ≤2.5 µm in diameter (PM2.5) was not associated with the increased risk of GDM (adjusted OR 1.03, 95% CI 0.99 to 1.06). However, subgroup analysis showed positive correlation of PM2.5 exposure in the second trimester with an increased risk of GDM (combined OR 1.07, 95% CI 1.00 to 1.13). Among pollutants other than PM2.5, significant association between GDM and nitrogen dioxide (NO2) (OR 1.05, 95% CI 1.01 to 1.10), nitrogen oxide (NOx) (OR 1.03, 95% CI 1.01 to 1.05), and sulfur dioxide (SO2) (OR 1.09, 95% CI 1.03 to 1.15) was noted. There was no significant association between exposure to black carbon or ozone or carbon monoxide or particulate matter ≤10 µm in diameter and GDM. Thus, systematic review of existing evidence demonstrated association of exposure to NO2, NOx, and SO2, and the second trimester exposure of PM2.5 with the increased risk of GDM. Caution may be exercised while deriving conclusions from existing evidence base because of the limited number and the observational nature of studies.
Keywords: air pollution, GDM, accumulated evidence
Introduction
Diabetes mellitus (DM) is a major cause of concern because of its increasing prevalence that has led to a consequential increase in the microvascular as well as macrovascular complications.1 Gestational diabetes mellitus (GDM) is a special type of DM characterized by any degree of glucose intolerance with onset, or first recognition during the pregnancy.2 It complicates 2%–6% of pregnancies worldwide, and as many as 10%–20% of high-risk pregnancy (body mass index (BMI) >30 kg/m2; previous macrosomic baby weighing ≥4.5 kg; personal history of gestational diabetes; family history of gestational diabetes; family history of diabetes) populations.3 GDM increases the affected woman’s risk of pre-eclampsia, asymptomatic bacteriuria, pyelonephritis, and cesarean delivery.4 Biological factors, such as older age, obesity, and family history, are known to increase the individual’s risk of GDM. However, the exact role and effects of environmental agents in GDM remain unknown.
Air pollution is one of the environmental health risks for GDM.5 Many studies have shown that air pollution exposure is related to impaired glucose homeostasis in susceptible populations.6–8 Association between air pollution and risk of type 2 diabetes mellitus has been reviewed.9 The underlying mechanisms could include endothelial dysfunction, dysregulation of the visceral adipose tissue through inflammation, hepatic insulin resistance, and alterations in autonomic tone that may increase peripheral insulin resistance.10 Type 2 diabetes and GDM share common risk factors, and both are characterized by insulin resistance and impaired insulin secretion.11
The relationship between air pollutants and GDM has not been studied systematically though a number of related studies have been published.12–24 To the best of our knowledge, thus far, there is no available accumulated evidence on their relationship. We therefore systematically identified, and reviewed the epidemiological evidence on the association between air pollutants and GDM.
Materials and methods
Study inclusion
The PubMed and Embase databases and Web of Science were searched for relevant studies published until August 2019. Terms used in the search included ‘air pollution’, ‘air pollutant’, ‘particulate matter’, ‘PM2.5’, ‘PM10’, ‘nitrogen dioxide’, ‘O3’, ‘NO2’, ‘NOx’, ‘SO2’, ‘ozone’, ‘soot’, ‘smog’, ‘gestational diabetes’, ‘gestational diabetes mellitus’, ‘GDM’, ‘pregnancy diabetes mellitus’, ‘pregnancy diabetes’, and ‘pregnancy glucose tolerance’ in combination. The search strategy was further supplemented by inspecting the references of the included articles. Two reviewers (XT and YiH) completed the screening independently, and any discrepancies were resolved by discussion. This report was conducted according to the Meta-analysis Of Observational Studies in Epidemiology25 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses26 guidelines. Because of reanalysis of published data, ethical approval was not needed for this study.
Inclusion and exclusion criteria
Studies were considered for inclusion based on the following criteria: (1) the study was an original article published in English; (2) it defined air pollution and GDM status clearly; (3) it measured the outdoor air pollution (ambient, including traffic related); (4) it used physical diagnosis of GDM, if diabetes is diagnosed in the first trimester or early second trimester with the standard diagnostic criteria of a hemoglobin A1c of 6.5% or higher, a fasting plasma glucose of 126 mg/dL or higher, or a 2-hour glucose of 200 mg/dL or higher on a 75 g oral glucose tolerance test, it was considered gestational diabetes27; and (5) it provided quantitative measures of association between air pollutants and GDM, and their 95% CIs. Exclusion criteria were as follows: (1) the publication was a review, case report, animal study or letter to the editor, (2) the articles did not clearly define the clinical outcomes, (3) the authors could not provide valid solicited data, and (4) the studies only examined whether the diabetes status would modify the association between air pollution and health outcomes.
For the meta-analysis, only cohort studies about particulate matter ≤2.5 μm in diameter (PM2.5), ozone (O3), sulfur dioxide (SO2), black carbon (BC), nitrogen dioxide (NO2), nitrogen oxide (NOx), particulate matter ≤10 μm in diameter (PM10), and carbon monoxide (CO) were included. We included all studies that quantified these air pollutants as ‘per … μg/m3’ or ‘ppb’ or ‘ppm’.
Data extraction and quality assessment
Two investigators (XT and YiH) independently extracted data from the enrolled studies, using a standard form that included publication year, country of origin, testing method, number of cases, control type, and cut-off value. Two investigators independently assessed the risk of bias for the enrolled studies (XT and FL) using the Newcastle-Ottawa Quality Assessment Scale (NOS) criteria.28 Three factors were considered while scoring the quality of included studies: (1) selection, including representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, and the demonstration that at the initiation of the study the outcome of interest was not present; (2) comparability, assessed on the basis of study design and analysis, and whether any confounding variables were adjusted for; and (3) outcome, based on the follow-up period and adequacy of cohorts, and ascertained by independent blind assessment, record linkage, or self-report. We rated the quality of the studies by awarding stars in each domain following the guidelines of NOS. If there was a disagreement, the investigators discussed the research with the other authors to arrive at a consensus.
Statistical analysis
Heterogeneity and variance between the enrolled studies was evaluated using I2 metric, and Tau2 respectively. Random effects models were performed to synthesize the association between different air pollutants and GDM in case of I2>50%. Random effects models give more weight to smaller studies and have typically wider CIs because the total effect is the average value of the real effect of each study that focuses on the studies with large samples, and pays attention to all included studies in order to balance the effect of each study. Fixed effects models were chosen in case of I2≤50%. ORs as the measure of association were pooled across all studies. If studies reported both unadjusted and covariate-adjusted ORs, we included the latter. When risk ratios and incidence ORs were reported, we directly considered them as ORs. For studies providing different methods of air pollution exposure assessments, we chose the results using spatiotemporal models. We used estimates of association and their SEs reported as ‘per 5 µg/m3’ of exposure in PM2.5, ‘per 10 µg/m3’ of exposure in PM10, ‘per 0.5 µg/m3’ in BC, ‘per 5 ppb’ in O3 and SO2, ‘per 10 ppb’ in NO2 and NOx, and ‘per 0.1 ppm’ in CO. We converted other reported quantities or units where necessary. Potential publication bias was evaluated by Egger’s asymmetry test.29 P values were two tailed, and p<0.05 was considered statistically significant. Sensitivity analyses were conducted when including at least five data points. The statistical analyses were performed with STATA V.12.0 (StataCorp, College Station, TX, USA).
Results
Study selection and study characteristics
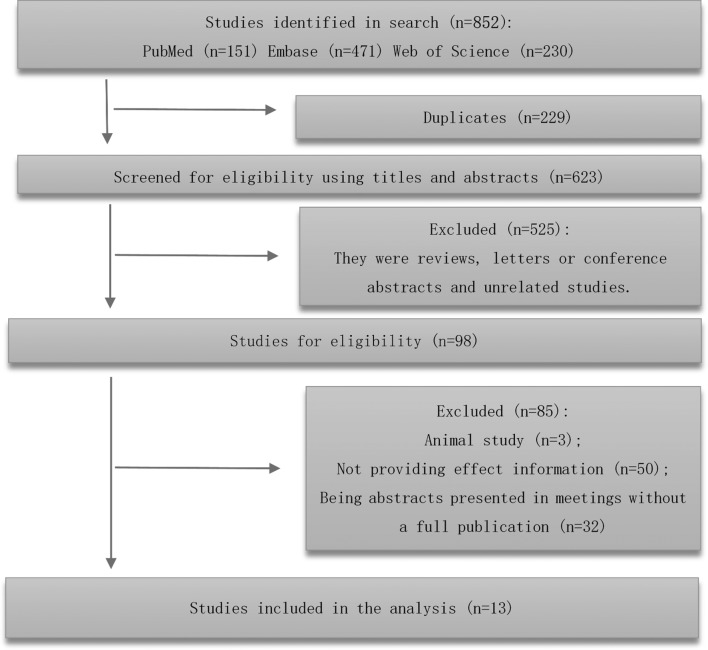
As per our search strategy, we identified 852 potentially relevant records, of which 229 were duplicate, and thus excluded. The remaining 623 manuscripts were subject to title and abstract screening. Further, 525 publications were removed as they were reviews, letters or conference abstracts or unrelated studies. Therefore, 98 articles were eligible for full-text review and data assessment (figure 1). Finally, 85 articles were excluded for other reasons (animal studies (n=3), unable to extract information (n=50), and lack of full publication (n=32)). The remaining 13 studies were enrolled in the meta-analysis12–24 out of which three were prospective cohort studies,13 19 22 nine were retrospective cohort studies12 14–18 20 23 24 and one was a case–control study.21 Seven studies were on PM2.5,12–15 20 23 24 four studies were on O3,15 18 20 24 three studies were on PM10,18 20 24 while two studies on each of the following pollutants were included: SO218 20; NOx18 20; CO; BC12 13; and NO2.23 24Tables 1 and 2 provide an overview of the 13 enrolled studies. Online supplementary table S1 summarizes the data reported in these studies as synthesized in meta-analyses.
Figure 1.
Literature search and selection process.
Table 1.
Characteristics of the studies on the relationship between air pollutant and gestational diabetes mellitus
| Source | Location | Years of study | Study design and duration of follow-up | Population (n) and age (years) of participants | NOS |
| Choe et al12 | Rhode Island, USA | 2002–2012 (excluded July 2004 to December 2005) | Retrospective cohort study | n=61 640 mother–infant pairs, singleton births to mothers aged 18 years or older and residing in Rhode Island during the study period | 7 |
| Fleisch et al13 | Boston, Massachusetts, USA | 1999–2002 | Prospective cohort study | n=2093 second-trimester pregnant women without known diabetes | 7 |
| Fleisch et al14 | Boston, Massachusetts, USA | 1 January 2003 to 31 December 2008 | Retrospective cohort study | n=159 373 primiparous women during the study period without pre-existing diabetes | 7 |
| Hu et al15 | Florida, USA | 1 January 2004 to 31 December 2005 |
Retrospective cohort study | n=410 267 women who gave birth in Florida during the study period and without non-singleton deliveries, previous preterm births, or pre-pregnancy diabetes mellitus | 8 |
| Lu et al16 | Chiayi City, Taiwan | 2006–2014 | Retrospective cohort study | n=3589 non-diabetic pregnant women during the study period | 7 |
| Malmqvist et al17 | Scania, Sweden | 1999–2005 | Retrospective cohort study | n=81 110 women who had singleton deliveries during the study period | 8 |
| Pan et al18 | Taiwan | 2004–2005 | Retrospective cohort study | n=19 606 women were included after the exclusion criteria were applied | 8 |
| Pedersen et al19 | Danish National Birth Cohort | 1997–2002 | Prospective cohort study | n=72 745 singleton pregnancies without hypertension, pre-existing chronic hypertension, and diabetes before pregnancy | 7 |
| Robledo et al20 | USA | 2002–2008 | Retrospective cohort study | n=219 952 singleton deliveries to mothers without pregestational diabetes | 8 |
| Shen et al21 | Taiwan | 2006–2013 | Case–control study | n=6717 mothers as the cases of newly diagnosed GDM n=6717 control mothers were selected |
8 |
| van den Hooven et al22 |
Rotterdam, Netherlands | 2002–2006 | Prospective cohort study | n=7399 pregnant women who had a delivery date in the study period, 21–38 years | 8 |
| Choe et al23 | New York City | 2008–2010 | Retrospective cohort study | n=256 372 deliveries without non-singleton births, reporting smoking during pregnancy and mothers with pre-existing diabetes | 8 |
| Jo et al24 | Kaiser Permanente Southern California (KPSC) hospitals | 1 January 1999 to 31 December 2009 | Retrospective cohort study | n=239 574 pregnancies without pre-existing diabetes | 8 |
GDM, gestational diabetes mellitus; NOS, Newcastle-Ottawa Quality Assessment Scale criteria.
Table 2.
Air pollutant exposure and outcome definitions of studies included
| Source | Outcome | Definition of outcome | Exposure | Definition of exposure | Exposure estimates |
| Choe et al12 | GDM | Birth certificate data and ICD-9648.8x were listed, and absent otherwise. | PM2.5, black carbon | PM2.5 and black carbon from spatiotemporal models. | Mean±SD First trimester PM2.5: 9.7±1.9 µg/m3; second trimester PM2.5: 9.6±1.9 µg/m3 Third trimester PM2.5: 9.5±2.1 µg/m3; first trimester black carbon: 0.5±0.1 µg/m3; second trimester black carbon: 0.5±0.1 µg/m3; third trimester black carbon: 0.5±0.1 µg/m3 |
| Fleisch et al13 | GDM | Failed GCT(1) with ≥2 high values on the OGTT(2). | PM2.5, black carbon, traffic exposure | PM2.5 and black carbon from central sites within 40 km of residence. PM2.5 and black carbon from spatiotemporal models. Neighborhood traffic density [(vehicles/day) × km] within 100 m. |
Mean±SD From central sites: PM2.5: 10.9±1.4 µg/m3; black carbon: 0.9±0.1 µg/m3 From spatiotemporal models: PM2.5: 11.9±1.4 µg/m3; black carbon: 0.7±0.2 µg/m3 Traffic density: 1621±2234 (vehicles/day × km) |
| Fleisch et al14 | GDM | Failed GCT with ≥2 high values on the OGTT. | PM2.5, traffic exposure | PM2.5 from spatiotemporal models. Neighborhood traffic density [(vehicles/day) × km] within 100 m. |
Mean±SD First trimester PM2.5: 10.4±1.7 µg/m3; second trimester PM2.5: 10.4±1.7 µg/m3 Traffic density: 1317±2025 (vehicles/day × km) |
| Hu et al15 | GDM | According to the American Diabetes Association 2003, failed GCT with ≥2 high values on the OGTT. | PM2.5, O3 | Air pollution exposure data were obtained from the US EPA and CDC’s National Environmental Public Health Tracking Network (2003–2005) (US EPA 2014) | Mean±SD Trimester 1 PM2.5: 9.73±2.07 µg/m3; O3: 37.20±6.04 ppb Trimester 2 PM2.5: 9.88±2.06 µg/m3; O3: 37.54±6.10 ppb Full pregnancy PM2.5: 9.93±1.67 µg/m3; O3: 37.40±4.10 ppb |
| Lu et al16 | GDM | A woman with a positive GCT and two or more abnormal 100 g OGTT values. | PM2.5, SO2, NOx, CO, O3 | The exposure assessment of this study based on data from a single fixed-site monitoring station (Chiayi station). | Mean±SD 3 months pre-pregnancy PM2.5: 44.38±12.09 µg/m3 First trimester PM2.5: 43.52±12.87 µg/m3; second trimester PM2.5: 41.20±13.43 µg/m3 |
| Malmqvist et al17 | GDM | GDM as defined in the Swedish Medical Birth Registry. | NOx, traffic exposure | Monthly and trimester means of NOx assigned by dispersion modeling at a spatial resolution of 500×500 m throughout the pregnancy. Traffic density within a 200 m radius. |
Quartiles of NOx exposure (μg/m3): Q1: 2.5–8.9; Q2: 9.0–14.1; Q3: 14.2–22.6; Q4: >22.7 Categories of traffic density within 200 m (vehicles/min): 1: no road; 2: <2; 3: 2–5; 4: 5–10; 5: >10 |
| Pan et al18 | GDM | According to the American Diabetes Association criteria, had two of the abnormal values on the OGTT. | PM10, CO, NOx, SO2, O3 | Collected from 77 fixed-site air monitoring stations in Taiwan during 2004–2006. | Mean±SD PM10 (μg/m3): first trimester: 61.4±18.3; second trimester: 61.2±17.2; third trimester: 62.2±19.5 CO (ppm): first trimester: 0.6±0.1; second trimester: 0.6±0.1; third trimester: 0.6±0.2 NO (ppb): first trimester: 6.5±3.3; second trimester: 6.9±3.1; third trimester: 6.9±3.2 NO2 (ppb): First trimester: 20.2±5.3; second trimester: 19.8±5.5; third trimester: 19.1±5.9 NOx (ppb): first trimester: 26.6±7.8; second trimester: 26.5±7.8; third trimester: 25.7±8.2 SO2 (ppb): first trimester: 4.5±1.8; second trimester: 4.8±1.7; third trimester: 4.9±1.7 O3 (ppb): first trimester: 25.8±3.8; second trimester: 25.6±3.2; third trimester: 25.5±3.7 |
| Pedersen et al19 | GDM | Self-reported, physician-diagnosed GDM. | NO2, noise from road traffic (Lden) exposure | NO2 was using the advanced AirGIS dispersion model. Road traffic noise was using SoundPLAN based on the Nordic prediction method. | First trimester:NO2 (μg/m3): 11.5 (5.8, 27.4); road traffic noise (dB): 57.5 (49.3, 69.8); railway noise (dB): 51.3 (31.1, 68.6) |
| Robledo et al20 | GDM | GDM was recorded in the medical record or discharge records (code 648.8) using the International Classification of Diseases, Ninth Revision. | PM10, PM2.5, SO2, O3, CO, NOx | Using a modified Community Multiscale Air Quality (CMAQ) model version 4.7.1. | IQR Preconception PM2.5 (μg/m3): 5.54; PM10 (μg/m3): 6.3; SO2 (ppb): 3.30; NOx (ppb): 28.55; O3 (ppb): 12.33; CO (ppm): 0.26 First trimester PM2.5(μg/m3): 5.28; PM10 (μg/m3): 6.32; SO2 (ppb): 3.31; NOx (ppb): 30.21; O3 (ppb): 12.36; CO(ppm): 0.26 |
| Shen et al21 | GDM | International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code: 648.0 or 648.8. | PM10, PM2.5, SO2, O3, CO, NO2 | Collected from 76 fixed-site air quality monitoring stations supervised by the Taiwan Environmental Protection Agency during 2005–2013. | |
| van den Hooven et al 22 |
GDM | GDM diagnosed according to the Dutch midwifery and obstetric guidelines. | Traffic exposure | Distance-weighted traffic density (DWTD) within a 150 m radius around residence (vehicles/24 hours × m); proximity to a major road (>10 000 vehicles/day). | Median (P25–P75) DWTD (vehicles/24 hours × m): 5.5×105 (1.6×105−1.2×106) Proximity to a major road (m): 140 (74–225) |
| Choe et al23 | GDM | ICD-9-CM code: 648.8. | PM2.5, NO2 | Air pollution samples were collected at 150 monitoring sites in each of the four seasons for one 2-week session and in every 2 weeks at five reference locations to track city-wide temporal variation. | Mean±SD Trimester 1 PM2.5: 12.0±2.5 µg/m3; NO2: 27.9±6.3 ppb Trimester 2 PM2.5: 11.9±2.4 µg/m3; O3: 27.9±6.3 ppb |
| Jo et al24 | GDM | Based on laboratory values confirming a plasma glucose level of 200 mg/dL or higher on the glucose challenge test or at least two plasma glucose values meeting or exceeding the following values on the 100 or 75 g oral glucose tolerance test. | PM2.5, PM10, NO2, O3 | Distance-weighted monthly average from four closest monitoring stations within 50 km, except for geocoded locations within 0.25 km of a monitor. | Mean±SD PM2.5: 18.2±5.5 µg/m3; PM10: 38.4±10.9 µg/m3; NO2: 25.8±8.2 ppb; O3: 41.3±7.6 ppb |
(1) Glucose change test: serum glucose 1 hour after a non-fasting 50 g oral glucose load. (2) Oral glucose tolerance test: serum glucose 3 hours after a fasting 100 g glucose load.
CDC, Centers for Disease Control and Prevention; CO, carbon monoxide; EPA, Environmental Protection Agency; GCT, glucose change test; GDM, gestational diabetes mellitus; NO, nitric oxide; NO2, nitrogen dioxide; NOx, nitrogen oxide; O3, ozone; OGTT, oral glucose tolerance test; PM10, particulate matter ≤10 μm in diameter; PM2.5, particulate matter ≤2.5 μm in diameter; SO2, sulfur dioxide.
bmjdrc-2019-000937supp001.pdf (334.2KB, pdf)
Quality assessment
Quality assessment using the NOS evaluation tool resulted in high ratings for all the 13 studies (score 7 or 8) (online supplementary table S2).
Meta-analysis results
There were 13 sets of data on PM2.5 (Q=106.07, I2=88.7%, p=0.000), 8 sets of data on O3 (Q=344.11, I2=98.0%, p<0.001), 6 sets of data on PM10 (Q=8.91, I2=43.9%, p=0.113), 4 sets of data on each of the following: NO2 (Q=17.50, I2=82.9%, p=0.001), SO2 (Q=4.26, I2=29.6%, p=0.234), CO (Q=7.08, I2=57.7%, p=0.069), NOx (Q=7.12, I2=57.9%, p=0.068), and 3 sets of data on BC (Q=0.34, I2=0.0%, p=0.562). As per the heterogeneity, the random effects model was selected for analysis of PM2.5, O3, NO2, CO, and NOx, while the fixed effects model was chosen for SO2, PM10, and BC.
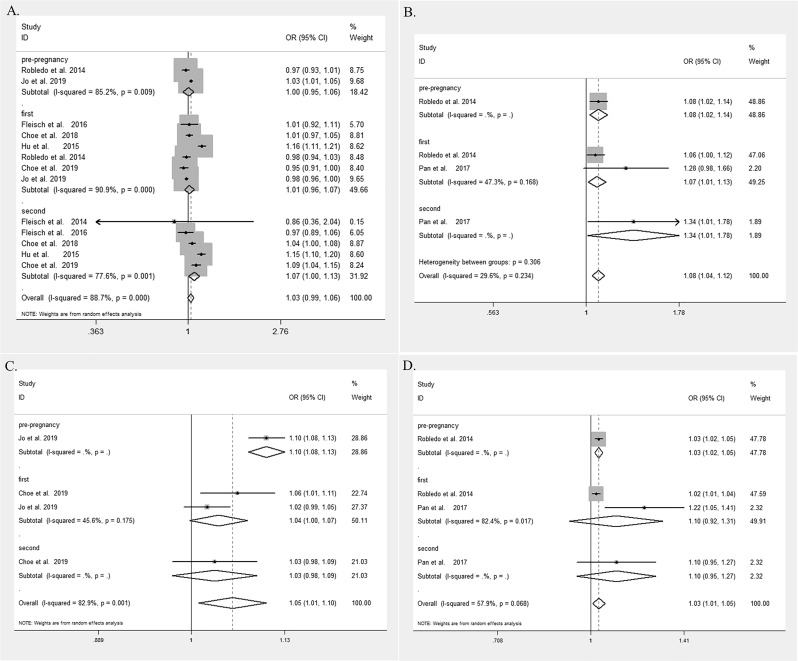
The statistically significant pooled effect value was absent in the relationship between PM2.5 and GDM (Z test, Z=1.55, p=0.122, the combined OR 1.06, 95% CI 0.99 to 1.03). We further performed the subgroup analysis for PM2.5 exposure in the different periods, including the pre-pregnancy, the first trimester and the second trimester. Subgroup analysis revealed that the above non-significant association persisted in both the pre-pregnancy and the first trimester (the overall OR of 1.00 (95% CI 0.95 to 1.06) and 1.01 (95% CI 0.96 to 1.07), respectively). However, in the second trimester, exposure to PM2.5 was associated with the increased risk of GDM (Z=2.11, p=0.035, the overall OR=1.07, 95% CI 1.00 to 1.13) (figure 2A).
Figure 2.
Forest plot and pooled estimates of the association between exposure to A) particulate matter ≤2.5 μm in diameter (PM2.5), B) sulfur dioxide (SO2), C) nitrogen dioxide (NO2) and D) nitrogen oxide (NOx) with risk of gestational diabetes mellitus (GDM). Pre-pregnancy, the exposure to PM2.5 was measured before pregnancy; first, the exposure to PM2.5 was measured during the first trimester; second, the exposure to PM2.5 was measured during the second trimester. GDM, gestational diabetes mellitus; NO2, nitrogen dioxide; NOx, nitrogen oxides; OR, odds ratio; PM2.5, particulate matter ≤ 2.5 μm in diameter; SO2, sulfurdioxide.
The significant relationship of exposure to SO2 with increased risk of GDM was noted (Z=3.83, p<0.001, the overall OR=1.08, 95% CI 1.04 to 1.12). In the subgroup analysis, the positive association was consistently observed in the pre-pregnancy, the first trimester, and the second trimester (the overall OR of 1.08 (95% CI 1.02 to 1.14), 1.07 (95% CI 1.01 to 1.13), and 1.34 (95% CI 1.01 to 1.78), respectively) (figure 2B).
There was a statistically significant correlation between exposure to NO2 and the increased risk of GDM (Z=2.40, p=0.016, the overall OR=1.05, 95% CI 1.01 to 1.10). In the subgroup analysis, the same correlation was persistent in the pre-pregnancy and the first trimester subgroups (pooled OR=1.10 (95% CI 1.08 to 1.13) and 1.04 (95% CI 1.00 to 1.07), respectively) (figure 2C).
Exposure to NOx was also related to an increased risk of GDM (Z=2.62, p=0.009, the overall OR=1.03, 95% CI 1.01 to 1.06). In the pre-pregnancy subgroup, a positive association was noted between the exposure to NOx and GDM (Z=3.96, p=0.000, the overall OR=1.03, 95% CI 1.02 to 1.05). However, in the first trimester, and the second trimester subgroups, the association was missing (first trimester, Z=1.06, p=0.287, the overall OR=1.10, 95% CI 0.92 to 1.31 and second trimester, Z=1.28, p=0.202, the overall OR=1.10, 95% CI 0.95 to 1.27) (figure 2D).
The non-significant relationship between BC and GDM was obtained (Z=1.13, p=0.257, the overall OR=1.02, 95% CI 0.99 to 1.05) (online supplementary figure S1A). Similar results were observed in CO, O3, and PM10 (Z=0.88, p=0.380, the overall OR=1.01, 95% CI 0.99 to 1.03; Z=0.69, p=0.489, the overall OR=1.01, 95% CI 0.98 to 1.04; Z=0.53, p=0.595, the overall OR=1.00, 95% CI 0.99 to 1.01, respectively) (online supplementary figure S1B,C).
Sensitivity analysis
Sensitivity analyses of PM2.5, PM10, and O3 were performed through single elimination of studies. The sensitivity analyses between the exposures to PM2.5, PM10, and O3 and the risk of GDM indicated no significant change in results.
Publication bias
According to the Cochrane Handbook version 5.1.0,30 as a rule of thumb, tests for funnel plot asymmetry should be used only when there are not too few research included in the meta-analysis, because when there are fewer studies, the power of the tests is too low to distinguish chance from real asymmetry. Therefore, we restricted this analysis to PM2.5, O3, and PM10, no significant bias exists among the studies by Egger’s test. The funnel figure of these studies showed a symmetrical inverted distribution that was consistent with the results of Egger’s test (online supplementary figure S2).
Discussion
In this study, we carried out the accumulated evidence to explore the relationship between air pollutants and GDM from observational studies. Results indicated that exposure to PM2.5 in the second trimester, and exposures to SO2, NO2 and NOx were significantly associated with the increased risk of GDM.
In the current analysis, the relationship of PM2.5 and risk of GDM was observed only in the second trimester, but not in the pre-pregnancy or the first trimester. This is consistent with the results of a prior study that suggested PM2.5 may affect glucose homeostasis only during the second trimester of pregnancy.23 Additionally, Fleisch et al13 found that women with the highest quartile exposure (12.8–15.9 µg/m3) to PM2.5 during the second trimester had a 2.63 (95% CI 1.15 to 6.01) times higher risk of having impaired glucose tolerance (IGT) than the women who had first quartile exposure. In another study, Fleisch et al14 noted that women younger than 20 years had 1.36 higher odds of GDM (95% CI 1.08 to 1.70) for each interquartile increment in PM2.5 exposure than the older women, at the second trimester. O3 was the other air pollutant that showed significant association with GDM in our analysis, consistent with Robledo et al,20 who found significant associations of GDM with interquartile increment in the preconception (5.37 ppb) and the first trimester (3.31 ppb) periods, with ORs of 1.05 (95% CI 1.01 to 1.09) and 1.04 (95% CI 1.01 to 1.08). A previous study noted increased risks of GDM in relation to nitric oxide exposures,18 while our study documented a significant association between NO2 and NOx exposure with the risk of GDM.
The possible mechanisms underlying the associations between air pollutants and GDM are still unclear. Several different aspects were raised by many researchers based on their opinions, including inflammation (adipose tissue inflammation,31 peripheral inflammation,32 systemic inflammation which is indicated by elevated serum C-reactive protein33 and cytokines34), oxidative damage,35 direct endothelial dysfunction,36 and dyslipidemia.37
PM2.5 was considered to initiate toxic effects and stimulate the production of free radicals or reactive oxygen.38 Levels of oxidative stress biomarkers, glutathione peroxidase and malonic dialdehyde, for instance, vary after PM2.5 exposure.39 40 Moreover, PM2.5 exposure during pregnancy can downregulate the expression of glucose transporter 2 in pancreatic β-cells and thereby yield glucose intolerance in GDM rats.41 Similarly, possible mechanisms linking insulin resistance with exposure to PM2.5 have been demonstrated by several human studies and are recognized as one of the important underlying metabolic conditions contributing to the development of GDM.42 The observation that O3-induced insulin resistance was associated with neuronal activation and sympathetic stimulation has been found by Bass et al.43 The other opinion shows that O3 may damage the β-cells of the pancreas, according to which O3 is known to alter T-cell-dependent immune response,44 leading to the reduced insulin secretion.45 For the SO2, studies also showed similar mechanisms, such as inflammation46 and dysfunction of pancreatic β-cells.47 It has been argued that NO2 and NOx can lead similar inflammation responses to those of particulate matter and O3.48
The strengths of our study included the adjustment for multiple confounders including geographic, sex, BMI, smoking, alcohol consumption, socioeconomic status, and age variables that affected the individual studies, but were reduced by our study design. Further, our meta-analysis is the most recent that comprehensively, critically, and quantitatively assesses the association between air pollutants and gestational diabetes.
Our study had the following limitations. (1) All included studies were observational studies, thus, the causal effect between air pollutants and GDM could not be described. (2) The high heterogeneity identified for some of the pollutants may be due to differences in race, blood glucose measurement, and pollutant concentrations in different regions. (3) This article analyzed respectively the relationship between eight different air pollutants (PM2.5, O3, SO2, NO2, NOx, CO, PM10, and BC) with GDM. Besides these eight kinds of air pollutants, there are also some other pollutants that may influence the risk of GDM.18 (4) In our daily life, different kinds of air pollutants are mixed and it is impossible to distinguish them from each other. The influence of the mixed air pollutants could not be analyzed because of the diversity of methods that researchers chose in individual studies. (5) Most studies were performed during the first and second trimesters, however, only few studies were performed before the conception. It was thus difficult to perform analyses during the preconception stage. (6) In addition to concentration of outdoor air pollutants, the distance from the main traffic road and noise, active and passive smoking are also potential risk factors for GDM. However, because of the scope of our study and the differences in measuring ways and indicators, we were unable to study these variables.
Prospects and conclusion
Future studies may focus on the relationship between exposure to different air pollutants before conception and GDM. The relationship between some other outdoor air pollutants, such as sulfur oxide, and GDM needs to be analyzed, and a dose–response manner should be of important consideration while analyzing the association of air pollutants with the risk of GDM. The effect of different combinations of air pollutants also needs to be studied more systematically. In addition, the distance from the main traffic road and noise are also potential risk factors for GDM,49 so as passive smoking during the pregnancy.50 Thus, further exploration for the effect of these factors is needed to help develop more accurate prevention strategies.
To sum up, the available evidence indicated direct association of air pollutants and GDM risk. High-quality and longitudinal studies are needed to improve our understanding of this association.
Acknowledgments
Authors are solely responsible for the design and conduct of this study; all study analyses, the drafting and editing of the manuscript, and its final contents.
Footnotes
XT and J-BZ contributed equally.
Contributors: The authors are solely responsible for the design and conduct of this study; all study analyses, the drafting and editing of the manuscript, and its final contents. XT and J-BZ contributed to the interpretation of data, and drafting the report. XT, FL, and YiH contributed to the data collection, statistical analysis and drafting the report. MAC and YoH made revisions. J-BZ and LQ contributed to study design and review.
Funding: This work was supported by the National Science Foundation Council of China (81870556, 81670738), the Beijing Municipal Administration of Hospital's Youth Programme (QML20170204), and the Excellent Talents in Dongcheng District of Beijing (2018019).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Kar P, Holt RIG. The effect of sulphonylureas on the microvascular and macrovascular complications of diabetes. Cardiovasc Drugs Ther 2008;22:207–13. 10.1007/s10557-008-6090-2 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37 Suppl 1:S81–90. 10.2337/dc14-S081 [DOI] [PubMed] [Google Scholar]
- 3.Galtier F. Definition, epidemiology, risk factors. Diabetes Metab 2010;36:628–51. 10.1016/j.diabet.2010.11.014 [DOI] [PubMed] [Google Scholar]
- 4.Inocêncio G, Braga A, Lima T, et al. Which factors influence the type of delivery and cesarean section rate in women with gestational diabetes? J Reprod Med 2015;60:529–34. [PubMed] [Google Scholar]
- 5.Beelen R, Raaschou-Nielsen O, Stafoggia M, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre escape project. Lancet 2014;383:785–95. 10.1016/S0140-6736(13)62158-3 [DOI] [PubMed] [Google Scholar]
- 6.Chuang K-J, Yan Y-H, Chiu S-Y, et al. Long-Term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med 2011;68:64–8. 10.1136/oem.2009.052704 [DOI] [PubMed] [Google Scholar]
- 7.Tamayo T, Rathmann W, Krämer U, et al. Is particle pollution in outdoor air associated with metabolic control in type 2 diabetes? PLoS One 2014;9:e91639 10.1371/journal.pone.0091639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitsel EA, Quibrera PM, Christ SL, et al. Heart rate variability, ambient particulate matter air pollution, and glucose homeostasis: the environmental epidemiology of arrhythmogenesis in the women's health Initiative. Am J Epidemiol 2009;169:693–703. 10.1093/aje/kwn400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eze IC, Hemkens LG, Bucher HC, et al. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 2015;123:381–9. 10.1289/ehp.1307823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riant M, Meirhaeghe A, Giovannelli J, et al. Associations between long-term exposure to air pollution, glycosylated hemoglobin, fasting blood glucose and diabetes mellitus in northern France. Environ Int 2018;120:121–9. 10.1016/j.envint.2018.07.034 [DOI] [PubMed] [Google Scholar]
- 11.Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes mellitus and its association with type 2 diabetes. Diabet Med 2004;21:103–13. 10.1046/j.1464-5491.2003.00985.x [DOI] [PubMed] [Google Scholar]
- 12.Choe S-A, Kauderer S, Eliot MN, et al. Air pollution, land use, and complications of pregnancy. Sci Total Environ 2018;645:1057–64. 10.1016/j.scitotenv.2018.07.237 [DOI] [PubMed] [Google Scholar]
- 13.Fleisch AF, Gold DR, Rifas-Shiman SL, et al. Air pollution exposure and abnormal glucose tolerance during pregnancy: the project VIVA cohort. Environ Health Perspect 2014;122:378–83. 10.1289/ehp.1307065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleisch AF, Kloog I, Luttmann-Gibson H, et al. Air pollution exposure and gestational diabetes mellitus among pregnant women in Massachusetts: a cohort study. Environ Health 2016;15:40 10.1186/s12940-016-0121-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu H, Ha S, Henderson BH, et al. Association of atmospheric particulate matter and ozone with gestational diabetes mellitus. Environ Health Perspect 2015;123:853–9. 10.1289/ehp.1408456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu M-C, Wang P, Cheng T-J, et al. Association of temporal distribution of fine particulate matter with glucose homeostasis during pregnancy in women of Chiayi City, Taiwan. Environ Res 2017;152:81–7. 10.1016/j.envres.2016.09.023 [DOI] [PubMed] [Google Scholar]
- 17.Malmqvist E, Jakobsson K, Tinnerberg H, et al. Gestational diabetes and preeclampsia in association with air pollution at levels below current air quality guidelines. Environ Health Perspect 2013;121:488–93. 10.1289/ehp.1205736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan S-C, Huang C-C, Lin S-J, et al. Gestational diabetes mellitus was related to ambient air pollutant nitric oxide during early gestation. Environ Res 2017;158:318–23. 10.1016/j.envres.2017.06.005 [DOI] [PubMed] [Google Scholar]
- 19.Pedersen M, Olsen SF, Halldorsson TI, et al. Gestational diabetes mellitus and exposure to ambient air pollution and road traffic noise: a cohort study. Environ Int 2017;108:253–60. 10.1016/j.envint.2017.09.003 [DOI] [PubMed] [Google Scholar]
- 20.Robledo CA, Mendola P, Yeung E, et al. Preconception and early pregnancy air pollution exposures and risk of gestational diabetes mellitus. Environ Res 2015;137:316–22. 10.1016/j.envres.2014.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen H-N, Hua S-Y, Chiu C-T, et al. Maternal exposure to air pollutants and risk of gestational diabetes mellitus in Taiwan. Int J Environ Res Public Health 2017;14:1604 10.3390/ijerph14121604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Hooven EH, Jaddoe VWV, de Kluizenaar Y, et al. Residential traffic exposure and pregnancy-related outcomes: a prospective birth cohort study. Environ Health 2009;8:59 10.1186/1476-069X-8-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choe S-A, Eliot MN, Savitz DA, et al. Ambient air pollution during pregnancy and risk of gestational diabetes in New York City. Environ Res 2019;175:414–20. 10.1016/j.envres.2019.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jo H, Eckel SP, Chen J-C, et al. Associations of gestational diabetes mellitus with residential air pollution exposure in a large southern California pregnancy cohort. Environ Int 2019;130:104933 10.1016/j.envint.2019.104933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stroup DF, Berlin JA, Morton SC, et al. Meta-Analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (moose) group. JAMA 2000;283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mishra S, Bhadoria AS, Kishore S, et al. Gestational diabetes mellitus 2018 guidelines: an update. J Family Med Prim Care 2018;7:1169–72. 10.4103/jfmpc.jfmpc_178_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 29.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bobrovitz N, Onakpoya I, Roberts N, et al. Protocol for an overview of systematic reviews of interventions to reduce unscheduled hospital admissions among adults. BMJ Open 2015;5:e008269 10.1136/bmjopen-2015-008269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen ZJ, Raaschou-Nielsen O, Ketzel M, et al. Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care 2012;35:92–8. 10.2337/dc11-1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu C, Ying Z, Harkema J, et al. Epidemiological and experimental links between air pollution and type 2 diabetes. Toxicol Pathol 2013;41:361–73. 10.1177/0192623312464531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rich DQ, Kipen HM, Huang W, et al. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA 2012;307:2068–78. 10.1001/jama.2012.3488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest 2006;116:1793–801. 10.1172/JCI29069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun Y, Taguchi K, Sumi D, et al. Inhibition of endothelial nitric oxide synthase activity and suppression of endothelium-dependent vasorelaxation by 1,2-naphthoquinone, a component of diesel exhaust particles. Arch Toxicol 2006;80:280–5. 10.1007/s00204-005-0043-3 [DOI] [PubMed] [Google Scholar]
- 36.Rao X, Montresor-Lopez J, Puett R, et al. Ambient air pollution: an emerging risk factor for diabetes mellitus. Curr Diab Rep 2015;15:603 10.1007/s11892-015-0603-8 [DOI] [PubMed] [Google Scholar]
- 37.Chuang K-J, Yan Y-H, Cheng T-J. Effect of air pollution on blood pressure, blood lipids, and blood sugar: a population-based approach. J Occup Environ Med 2010;52:258–62. 10.1097/JOM.0b013e3181ceff7a [DOI] [PubMed] [Google Scholar]
- 38.Upadhyay D, Panduri V, Ghio A, et al. Particulate matter induces alveolar epithelial cell DNA damage and apoptosis: role of free radicals and the mitochondria. Am J Respir Cell Mol Biol 2003;29:180–7. 10.1165/rcmb.2002-0269OC [DOI] [PubMed] [Google Scholar]
- 39.Luo B, Shi H, Wang L, et al. Rat lung response to PM2.5 exposure under different cold stresses. Int J Environ Res Public Health 2014;11:12915–26. 10.3390/ijerph111212915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Araujo JA, Barajas B, Kleinman M, et al. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res 2008;102:589–96. 10.1161/CIRCRESAHA.107.164970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yi L, Wei C, Fan W. Fine-particulate matter (PM2.5), a risk factor for rat gestational diabetes with altered blood glucose and pancreatic GLUT2 expression. Gynecol Endocrinol 2017;33:611–6. 10.1080/09513590.2017.1301923 [DOI] [PubMed] [Google Scholar]
- 42.Brook RD, Xu X, Bard RL, et al. Reduced metabolic insulin sensitivity following sub-acute exposures to low levels of ambient fine particulate matter air pollution. Sci Total Environ 2013;448:66–71. 10.1016/j.scitotenv.2012.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bass V, Gordon CJ, Jarema KA, et al. Ozone induces glucose intolerance and systemic metabolic effects in young and aged brown Norway rats. Toxicol Appl Pharmacol 2013;273:551–60. 10.1016/j.taap.2013.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krishna MT, Madden J, Teran LM, et al. Effects of 0.2 PPM ozone on biomarkers of inflammation in bronchoalveolar lavage fluid and bronchial mucosa of healthy subjects. Eur Respir J 1998;11:1294–300. 10.1183/09031936.98.11061294 [DOI] [PubMed] [Google Scholar]
- 45.Kelishadi R, Mirghaffari N, Poursafa P, et al. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis 2009;203:311–9. 10.1016/j.atherosclerosis.2008.06.022 [DOI] [PubMed] [Google Scholar]
- 46.Lee H, Myung W, Jeong B-H, et al. Short- and long-term exposure to ambient air pollution and circulating biomarkers of inflammation in non-smokers: a hospital-based cohort study in South Korea. Environ Int 2018;119:264–73. 10.1016/j.envint.2018.06.041 [DOI] [PubMed] [Google Scholar]
- 47.Yang B-Y, Qian ZM, Li S, et al. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 communities Chinese Health study. Lancet Planet Health 2018;2:e64–73. 10.1016/S2542-5196(18)30001-9 [DOI] [PubMed] [Google Scholar]
- 48.Hesterberg TW, Bunn WB, McClellan RO, et al. Critical review of the human data on short-term nitrogen dioxide (NO2) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol 2009;39:743–81. 10.3109/10408440903294945 [DOI] [PubMed] [Google Scholar]
- 49.Cappuccio FP, D'Elia L, Strazzullo P, et al. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:414–20. 10.2337/dc09-1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cupul-Uicab LA, Skjaerven R, Haug K, et al. In utero exposure to maternal tobacco smoke and subsequent obesity, hypertension, and gestational diabetes among women in the MobA cohort. Environ Health Perspect 2012;120:355–60. 10.1289/ehp.1103789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2019-000937supp001.pdf (334.2KB, pdf)