Abstract
Objectives
There is mixed evidence on the relationship between physical activity and behavioural and mental health. We aimed to estimate the association between physical activity and risk of behavioural and mental health disorders in early school-aged children.
Design
A series of cross-sectional complete enumeration (census) surveys.
Settings
All primary schools in the Australian Capital Territory, 2014–2016.
Participants
All children enrolled in their first year of full-time primary education (kindergarten) were invited to participate. Of the 16 662 eligible kindergarten children, 15 040 completed the survey for the first time.
Outcome measures
Average daily physical activity participation and prevalence of risk of behavioural and mental health disorders derived from parent-reported data and the Strengths and Difficulties Questionnaire (SDQ). Characteristics associated with SDQ Total difficulties and subscales were estimated using logistic regression.
Results
8340 (61.7%) children met physical activity targets (60 min or more daily) and 709 (4.8%) were at clinically significant risk of behavioural and mental health disorders (Total difficulties).
Known sociodemographic correlates were also those variables associated with high risk of behavioural and mental health disorders (Total difficulties): Aboriginal and Torres Strait Islander status (OR 2.72, 95% CI 1.78–4.16), relative socioeconomic disadvantage (most disadvantaged vs least disadvantaged, OR 1.86, 95% CI 1.38–2.50) and male sex (OR 1.80, 95% CI 1.49–2.17). Average daily physical activity was not significant, despite the highest levels of physical activity (90 min or more daily) being reported in boys, Aboriginal and Torres Strait Islander children and those from more disadvantaged areas.
Conclusions
Our study provides comprehensive cross-sectional data on the relationship between physical activity participation and the risk of behavioural and mental health disorders in a large cohort of early school-aged Australian children. Aboriginal and Torres Strait Islander children, boys and those from the most disadvantaged socioeconomic group were at greatest risk of clinically significant behavioural and mental health disorders.
Keywords: public health, primary care, community child health, mental health
Strengths and limitations of this study.
The Kindergarten Health Check (KHC) has been conducted for several years and has excellent response rates.
There is a large sample for analysis.
The survey includes well-validated questions including the Strengths and Difficulties Questionnaire and measured anthropometric data.
The KHC is a series of cross-sectional surveys so we can demonstrate relationships between variables, but inference cannot be made about causality.
The survey includes parent-reported data on physical activity. The questions on physical activity had a lower response rate than other variables.
Introduction
Physical inactivity is associated with many potentially preventable chronic diseases1 and childhood is a key time for increasing participation in physical activity.2 The benefits of physical activity start in childhood with protective effects on cardiovascular and metabolic health.3 4 The importance of physical activity for school-aged children has been recognised by the WHO, and within Australia through the Australian 24-hour movement guidelines for children and young people (5 to 17 years ).5 6
The evidence on the association between physical activity and mental well-being and behavioural disorders in young children is mixed. Several studies have associated physical activity participation with lower rates of depression and anxiety, and improved self-esteem.7 8 However, mixed and contradictory results have been found and there is a paucity of information for younger children.7 9 10 In their systematic review of early childhood physical activity and psychosocial well-being, Hinkley et al 11 found supportive, null and even adverse associations between physical activity and a range of psychosocial well-being and behavioural outcomes. More recent systematic reviews continue to find mixed evidence. Carson et al 12 showed a favourable relationship between physical activity and psychosocial health in preschool-aged children based on an experimental study, while observational studies gave mixed results. Poitras et al 4 assessed the relationship between objectively measured physical activity and indicators such as behavioural conduct/prosocial behaviour, psychological distress and self-esteem in 5–17-year-olds, however, none of the included studies were for primary school-aged children. Nevertheless, physical activity may have a role in mitigating the increasing burden of mental health disorders in children. Anxiety, autism spectrum disorder, conduct disorder and depressive disorders ranked among the six largest contributors to the burden of disease for Australian boys and girls aged 5–14 years in 2011.1 The 2013–14 Australian Child and Adolescent Survey of Mental Health and Wellbeing (Young Minds Matter) reported a mental disorder in 14% of boys and 7% of girls in kindergarten or pre-primary.13
Despite the importance of physical activity, few children are meeting recommended targets. The 24-hour movement guidelines recommend Australian primary school-aged children get at least 60 min of moderate to vigorous intensity physical activity daily.6 The 2011–12 Australian Health Survey (AHS) found 36% of children aged 5–8 years met the recommended 60 min or more of physical activity on all 7 days prior to interview, with a further 34% meeting this target on 5–6 of the preceding 7 days.14 The Australian Capital Territory (ACT) General Health Survey found 44% of children aged 5–12 years were active for at least 60 min each day in 2015–2016.15
We know that fewer than half of young Australian children meet physical activity targets, including primary school-aged children in the ACT. It is also well known that sociodemographic characteristics play an important part in health and well-being. However, we lack information about children in early childhood, how their physical activity levels may relate to risk of mental and behavioural health disorders, and how sociodemographic factors may influence these for young children in the ACT.
The ACT Kindergarten Health Check (KHC) is offered to all children in the ACT in their first year of full-time primary school and collects information on risk of mental health and behavioural disorders and physical activity. Our study aimed to estimate the association between physical activity and risk of mental health and behavioural disorders and how this may differ for Aboriginal and Torres Strait Islander children, and those from different socioeconomic backgrounds.
Methods
The KHC is an annual cross-sectional survey of all children in the ACT in their first year of full-time primary education (kindergarten). All eligible children enrolled in ACT kindergartens are invited to participate in the survey; participation is voluntary. The KHC consists of a paper questionnaire completed by parents at the start of the school year, and a physical health check performed by the school health nurses during the school year for all children whose parents consent to their participation. More information on the KHC is included in online supplementary file 1. Our study analyses data from the 2014 to 2016 surveys. Children who were identified as repeating kindergarten within the ACT were excluded from the analysis for their second year.
bmjopen-2019-034847supp001.pdf (172.3KB, pdf)
The KHC collects demographic data (date of birth, sex, Aboriginal or Torres Strait Islander status, home address) and information on selected conditions and behaviours. Parents were asked to report on their child’s physical activity outside of school hours in terms of the number of school days and hours/minutes of activity on these days, and similar for weekend days. These were combined to determine the average daily activity of children and were assessed against the targets for moderate to vigorous physical activity from the Australian 24-hour movement guidelines for children aged 5–17 years.6 As our study population are children at school, we used the guidelines for school-aged children (5–17-year-olds), rather than those in early years including pre-school (0–5-year-olds). The KHC physical activity survey questions are included within the survey instrument, which is included as online supplementary file 2.
bmjopen-2019-034847supp002.pdf (110.5KB, pdf)
The parent-completed questionnaire includes the Strengths and Difficulties Questionnaire (SDQ). The SDQ contains 25 questions asking parents to assess their child’s behaviour and psychological traits over the previous 6 months. It is a well-validated behavioural screening questionnaire for children, adapted for use in Australia from the original developed by Goodman.16 The questions ask about positive and negative attributes which are used to calculate scores for emotional difficulties, conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behaviour. A Total difficulties score is calculated from all subscales except prosocial behaviour. Children are scored as close to average, slightly raised or high risk.
The physical health check includes measurement of height and weight by school health nurses. Body mass index was calculated and classified into weight categories based on age-specific and sex-specific cut-offs.17 Health concerns from either the questionnaire or health screen are communicated to the child’s primary carer and nominated general practitioner.
We linked the KHC with an indicator of socioeconomic disadvantage—the 2016 Index of Relative Socio-Economic Disadvantage (IRSD), one of the Socio-Economic Indexes for Areas (SEIFA) produced by the Australian Bureau of Statistics.18 IRSD was mapped to geocoded home addresses at the finest geographic level available, the Statistical Area Level 1 (SA1). We created quintiles of socioeconomic disadvantage for the ACT by ranking the IRSD scores for ACT SA1 regions and dividing them into five equal cohorts. These quintiles are specific to the ACT and differ from those based on the national profile. The ACT is relatively advantaged compared with the national average, with 78% of the ACT in the least disadvantaged quintile based on the national IRSD profile.18
Statistical analysis
Our analysis comprised of producing unweighted prevalence estimates and logistic regression analysis. CIs for prevalence estimates were calculated using binomial sampling. Logistic regression was performed with dependent variable Total difficulties (high vs slightly raised/average risk) and independent variables sex, Aboriginal and Torres Strait Islander status, relative socioeconomic disadvantage, total daily physical activity (minutes), body mass index and age (months). Average daily physical activity was skewed, so the cube root transformation was used. A sensitivity analysis was conducted with categories of physical activity participation in lieu of continuous data. Analysis was also run with SDQ subscales as the dependent variable.
Analysis was conducted in SPSS V.24. Missing data were excluded from the analysis.
Patient and public involvement
Patients and the public were not involved in the design of the study.
Results
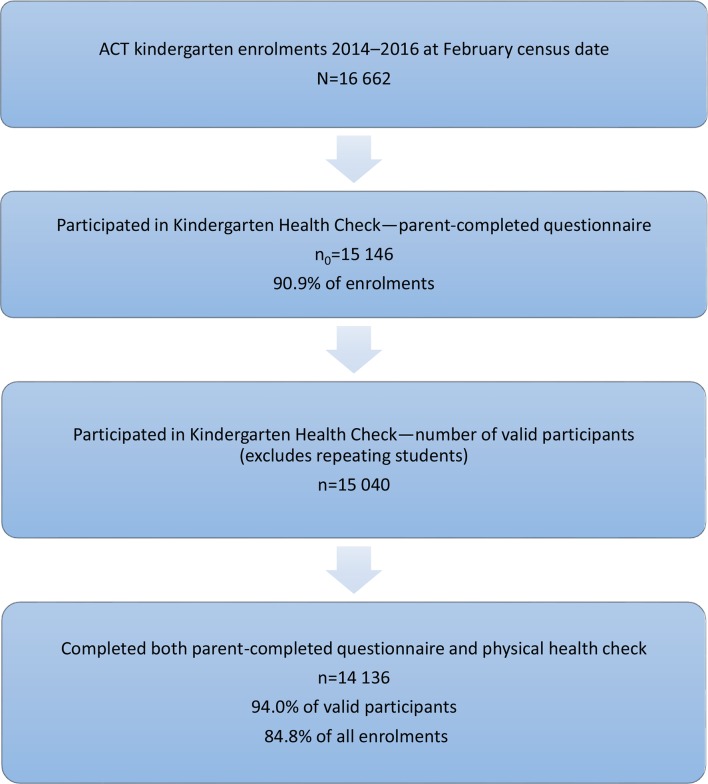
Of the 16 662 children enrolled in kindergarten in ACT schools during the study period, 15 146 (90.9%) participated in the KHC. Data for 106 children who were identified as repeating kindergarten within the ACT were excluded from the analysis for their second year of participation. Of the remaining 15 040 children, 94.0% participated in the health screen (figure 1). Overall, 14 136 (84.8% of enrolled children) participated in the KHC parent-completed questionnaire and physical health check for the first time.
Figure 1.
Participation rates for the Kindergarten Health Check, 2014–2016. Source: ACT Education and Training Directorate37–39 and KHC 2014–2016. Note: Enrolment data derived from the February census within each year. ACT, Australian Capital Territory; KHC, Kindergarten Health Check.
Baseline characteristics of study participants are shown in table 1. Over 75% of children were of a healthy weight with 3.6% in the obese weight range and 6.0% considered underweight. Nearly two-thirds (61.7%) met physical activity targets of 60 min or more on average daily, however, 13% averaged less than 30 min daily. Five per cent of children had a high-risk Total difficulties score; that is, they were at significantly increased risk of clinically significant mental health and behavioural disorders. Analysis of the SDQ subscales showed that a higher proportion of children had high-risk scores for hyperactivity/inattention than for the other domains, and peer problems was the domain with the lowest proportion of high-risk scores.
Table 1.
Characteristics of children in the Kindergarten Health Check, 2014–2016
| Characteristic | Number | Per cent (95% CI) |
| Mean (SD) age on commencement (years) | 5.27 (0.31) | |
| Age at 30 April of enrolment year | ||
| <5 years | 91 | 0.6 (0.5–0.7) |
| 5 to <6 years | 13 947 | 92.7 (92.3–93.1) |
| 6 years or more | 1002 | 6.7 (6.3–7.1) |
| Sex | ||
| Male | 7754 | 51.6 (50.8–52.4) |
| Female | 7286 | 48.4 (47.6–49.2) |
| Indigenous status* | ||
| Aboriginal or Torres Strait Islander | 348 | 2.3 (2.1–2.6) |
| Not Aboriginal or Torres Strait Islander | 14 649 | 97.7 (97.4–97.9) |
| Socioeconomic status† | ||
| Most disadvantaged quintile (Q1) | 2676 | 18.5 (17.9–19.2) |
| Q2 | 2915 | 20.2 (19.5–20.8) |
| Q3 | 3166 | 21.9 (21.2–22.6) |
| Q4 | 2881 | 19.9 (19.3–20.6) |
| Least disadvantaged quintile (Q5) | 2805 | 19.4 (18.8–201) |
| School sector | ||
| Government school | 9773 | 65.0 (64.2–65.7) |
| Non-government school | 5267 | 35.0 (34.3–35.8) |
| Body mass index‡ | ||
| Underweight | 851 | 6.0 (5.6–6.4) |
| Healthy weight | 11 023 | 78.1 (77.4–78.7) |
| Overweight | 1736 | 12.3 (11.8–12.8) |
| Obese | 511 | 3.6 (3.3–3.9) |
| Mean (SD) daily physical activity participation (min)§ | 85.6 (66.51) | |
| Average daily physical activity participation§ | ||
| <30 min | 1782 | 13.2 (12.6–13.8) |
| 30 to <60 min | 3382 | 25.0 (24.3–25.8) |
| 60 to <90 min | 3392 | 25.1 (24.4–25.8) |
| ≥90 min | 4948 | 36.6 (35.8–37.8) |
| Strengths and Difficulties Questionnaire high-risk subscale scores¶ | ||
| Emotional difficulties | 915 | 6.1 (5.8–6.5) |
| Conduct problems | 1019 | 6.8 (6.4–7.3) |
| Hyperactivity/inattention | 1232 | 8.3 (7.8–8.7) |
| Peer problems | 101 | 0.7 (0.5–0.8) |
| Total difficulties | 709 | 4.8 (4.4– 5.1 ) |
| Prosocial | 421 | 2.8 (2.6–3.1) |
| All children | 15 040 | 100.0 |
*Excludes children for whom Indigenous status was not available.
†Socioeconomic status based on ACT quintiles of relative disadvantage from IRSD at SA1 level. Excludes children for whom socioeconomic status was not available.
‡Excludes those for whom body mass index not available.
§Excludes those for whom physical activity participation not available.
¶Each category excludes those children for which the reported measure is not available.
ACT, Australian Capital Territory; IRSD, Index of Relative Socio-Economic Disadvantage; SA1, Statistical Area Level 1 .
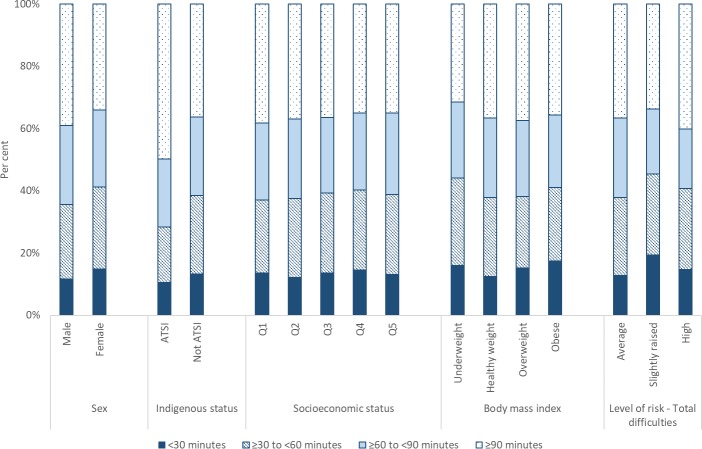
Figure 2 shows that children meeting physical activity target of 60 min or more daily were more likely to be of Aboriginal and Torres Strait Islander origin or boys. Children who were underweight were less likely than other children to participate in 60 min or more of physical activity daily. Aboriginal and Torres Strait Islander children had the highest level of reported activity, with half averaging 90 min or more daily.
Figure 2.
Characteristics of children by average daily physical activity participation, 2014–2016. (a) Excludes children for whom Indigenous status was not available. (b) Socioeconomic status based on ACT quintiles of relative disadvantage from IRSD at SA1 level. Q1—most disadvantaged; Q5—least disadvantaged. Excludes children for whom socioeconomic status was not available. (c) Excludes those for whom body mass index not available. (d) Excludes those for whom physical activity participation not available. ACT, Australian Capital Territory; IRSD, Index of Relative Socio-Economic Disadvantage; SA1, Statistical Area Level 1.
The attributes of children with high-risk Total difficulties scores are shown in table 2. These children were more likely to be boys, of Aboriginal and Torres Strait Islander origin, or from the most disadvantaged socioeconomic groups. No increase in risk was seen based on average daily physical activity (figure 2).
Table 2.
Characteristics of children rated high risk for strengths and difficulties subscales, 2014–2016
| SDQ subscale§ | Sex | Indigenous status* | Socioeconomic status† | Body mass index‡ | |||||||||
| Male | Female | Aboriginal or Torres Strait Islander | Not indigenous | Q1 | Q2 | Q3 | Q4 | Q5 | Underweight | Healthy weight | Overweight | Obese | |
| Number (per cent) | |||||||||||||
| Total difficulties | 471 (6.1) | 238 (3.3) | 43 (12.5) | 663 (4.6) | 179 (6.8) | 165 (5.7) | 132 (4.2) | 130 (4.6) | 87 (3.1) | 35 (4.2) | 495 (4.5) | 79 (4.6) | 41 (8.1) |
| Emotional difficulties | 473 (6.2) | 442 (6.1) | 41 (11.9) | 871 (6.0) | 204 (7.7) | 196 (6.8) | 177 (5.6) | 153 (5.4) | 158 (5.7) | 52 (6.2) | 662 (6.1) | 100 (5.8) | 53 (10.5) |
| Conduct problems | 626 (8.2) | 393 (5.5) | 42 (12.2) | 976 (6.7) | 234 (8.8) | 228 (7.9) | 198 (6.3) | 172 (6.0) | 157 (5.6) | 35 (4.2) | 726 (6.6) | 135 (7.8) | 40 (7.9) |
| Hyperactivity/inattention | 827 (10.8) | 405 (5.6) | 59 (17.2) | 1167 (8.1) | 275 (10.4) | 276 (9.6) | 219 (7.0) | 217 (7.6) | 203 (7.3) | 57 (6.8) | 880 (8.1) | 145 (8.4) | 52 (10.3) |
| Peer problems | 77 (1.0) | 24 (0.3) | n.p. | n.p. | 22 (0.8) | 21 (0.7) | 20 (0.6) | 22 (0.8) | 13 (0.5) | 10 (1.2) | 59 (0.5) | 16 (0.9) | 6 (1.2) |
| Prosocial | 296 (3.9) | 125 (1.7) | 15 (4.4) | 405 (2.8) | 80 (3.0) | 73 (2.5) | 95 (3.0) | 90 (3.1) | 68 (2.4) | 26 (3.1) | 299 (2.7) | 44 (2.5) | 17 (3.4) |
n.p., not published due to small cell size.
*Excludes children for whom Indigenous status was not available.
†Socioeconomic status based on ACT quintiles of relative disadvantage from IRSD at SA1 level. Q1—most disadvantaged; Q5—least disadvantaged. Excludes children for whom socioeconomic status was not available.
‡Excludes those for whom body mass index not available.
§Each category excludes those children for which the reported measure is not available.
ACT, Australian Capital Territory; IRSD, Index of Relative Socio-Economic Disadvantage; SA1, Statistical Area Level 1; SDQ, Strengths and Difficulties Questionnaire .
Boys were more likely than girls to be rated high risk for conduct problems, hyperactivity/inattention and prosocial behaviour difficulties (table 2). Very few children (<1%) were rated high risk for peer problems. Aboriginal and Torres Strait Islander children were more likely than other children to be rated high risk for all subscales excluding peer problems. Children in the most disadvantaged two quintiles were more likely to be at high risk for emotional difficulties, conduct problems and hyperactivity/inattention.
Of the 15 040 children in the study, 12 097 (80.4%) were included in the main logistic regression model (dependent variable, high-risk Total difficulties score) (table 3). Aboriginal and Torres Strait Islander background was the strongest predictor of being at substantial risk of clinically significant problems (OR 2.72, 95% CI 1.78–4.16). Being from the most disadvantaged socioeconomic quintile was the next highest predictor of risk (OR 1.86, 95% CI 1.38–2.50). The risk of significant problems decreased with decreasing relative socioeconomic disadvantage, however, the ORs were significantly different for the two most disadvantaged quintiles only (table 3). Boys were more likely to be at high risk than girls (OR 1.80, 95% CI 1.49–2.17), and children who were obese were more likely to be at high risk than those of healthy weight (OR 1.86, 95% CI 1.27–2.72). Age at enrolment was weakly significant with a small impact on risk. Total daily physical activity and body mass index were not significant predictors in the model.
Table 3.
ORs from logistic regression analyses
| SDQ subscale† | Logistic regression independent variables* | ||||||||||
| Sex | Indigenous status | Socioeconomic status‡ Q1 | SES Q2 | SES Q3 | SES Q4 | Physical activity | Underweight§ | Overweight§ | Obese§ | Age | |
| OR (95% CI) | |||||||||||
| Total difficulties | 1.80 (1.49–2.17) | 2.72 (1.78–4.16) | 1.86 (1.38–2.50) | 1.50 (1.11–2.03) | 1.30 (0.96–1.77) | 1.29 (0.95–1.76) | 0.96 (0.88–1.04) | 1.05 (0.72–1.53) | 1.05 (0.79–1.38) | 1.86 (1.27–2.72) | 1.03 (1.00–1.05) |
| Emotional difficulties | 0.97 (0.83–1.13) | 1.98 (1.30–3.01) | 1.26 (0.99–1.60) | 1.09 (0.86–1.38) | 0.96 (0.75–1.22) | 0.91 (0.71–1.16) | 0.94 (0.87–1.01) | 0.98 (0.70–1.36) | 0.94 (0.74–1.20) | 1.78 (1.28–2.47) | 1.03 (1.01–1.06) |
| Conduct problems | 1.57 (1.35–1.82) | 1.66 (1.09–2.54) | 1.48 (1.17–1.87) | 1.32 (1.05–1.67) | 1.08 (0.85–1.37) | 0.98 (0.77–1.25) | 0.99 (0.93–1.07) | 0.58 (0.39–0.85) | 1.29 (1.05–1.59) | 1.15 (0.79–1.68) | 1.02 (1.00–1.04) |
| Hyperactivity/inattention | 2.02 (1.75–2.33) | 1.85 (1.26–2.72) | 1.35 (1.09–1.67) | 1.27 (1.03–1.57) | 0.91 (0.73–1.13) | 1.05 (0.84–1.30) | 0.97 (0.91–1.04) | 0.91 (0.67–1.22) | 1.09 (0.89–1.34) | 1.41 (1.02–1.94) | 1.01 (0.99–1.02) |
| Peer problems | 2.73 (1.61–4.64) | 1.43 (0.35–5.91) | 1.67 (0.74–3.73) | 1.22 (0.53–2.84) | 1.70 (0.78–3.70) | 1.78 (0.82–3.86) | 0.78 (0.62–0.98) | 2.42 (1.18–4.98) | 1.90 (1.02–3.52) | 1.93 (0.69–5.41) | 1.03 (0.97–1.10) |
| Prosocial | 2.49 (1.94–3.19) | 0.66 (0.24–1.80) | 1.27 (0.87–1.85) | 1.14 (0.78–1.66) | 1.36 (0.95–1.93) | 1.28 (0.89–1.84) | 0.78 (0.70–0.87) | 1.07 (0.68–1.68) | 1.13 (0.81–1.58) | 1.03 (0.56–1.91) | 1.00 (0.97–1.03) |
*Reference categories: girls, non-Indigenous, Q5—least disadvantaged, healthy weight (BMI); physical activity and age are continuous.
†Each category excludes those children for which the reported measure is not available.
‡Socioeconomic status (SES) based on ACT quintiles of relative disadvantage from IRSD at SA1 level. Q1—most disadvantaged; Q5—least disadvantaged.
§Based on BMI.
ACT, Australian Capital Territory; BMI, body mass index; IRSD, Index of Relative Socio-Economic Disadvantage; SA1, Statistical Area Level 1; SDQ, Strengths and Difficulties Questionnaire.
Logistic regression was also undertaken for the SDQ subscales (table 3). ORs were significant for boys for all domains other than emotional difficulties. Aboriginal and Torres Strait Islander children were at increased risk for emotional difficulties, conduct problems and hyperactivity/inattention, however, they were not at increased risk for peer problems or prosocial behaviour difficulties. Being from the most disadvantaged socioeconomic quintile was associated with increased odds of conduct problems and hyperactivity/inattention. Obesity was associated with increased odds of emotional difficulties. Physical activity was associated with lower odds of peer problems and prosocial behaviour difficulties.
Logistic regression analyses for Total difficulties and the SDQ subscales where physical activity was included as a categorical variable were done as part of a sensitivity analysis (online supplementary file 3). ORs for independent variables, other than physical activity, showed only minor differences from those in the models where physical activity was included as a continuous variable. For Total difficulties and hyperactivity/inattention, 60 to <90 min of daily physical activity was significant in the models (baseline,<30 min daily). For prosocial behaviour, all categories were significant compared with baseline. Physical activity was not significant for the remaining SDQ subscales.
bmjopen-2019-034847supp003.pdf (273.8KB, pdf)
Discussion
Our study found nearly two-thirds of ACT kindergarten children were meeting physical activity targets of 60 min or more daily. These children were more likely to be boys, of Aboriginal or Torres Strait Islander background, or from the most disadvantaged socioeconomic areas.
The 2011–12 AHS found similar proportions of boys (36%) and girls (35%) aged 5–8 years met the recommended 60 min or more of physical activity on all 7 days prior to interview.14 However, similar to our study, boys undertook more daily exercise. Boys aged 5–17 years spent an average of 78 min in moderate to vigorous activity daily, compared with 67 min for girls. There were no statistically significant differences in the proportion of children aged 5–17 years meeting physical activity targets based on socioeconomic status (IRSD).
In our study, the groups of children with higher daily physical activity also had a higher risk of behavioural and mental health disorders, with boys having double the rate of high-risk Total difficulties scores as girls (6.1% vs 3.3%). Aboriginal and Torres Strait Islander children had more than double the proportion at high risk compared with non-indigenous children (12.5% vs 4.6%), and children from the most disadvantaged socioeconomic group were also over-represented. Children who were obese were more likely to have high-risk Total difficulties score, but there was no significant difference in their physical activity participation compared with other children.
Our results are consistent with SDQ data for Australian children aged 4–12 years; higher rates of high-risk Total difficulties were seen for boys compared with girls (12.7% vs 7.7%) and children in the most disadvantaged socioeconomic groups (15.6% in the lowest socieconomic status (SES) quintile vs 7.2% in the highest SES quintile).19 Aboriginal and Torres Strait Islander children have also been shown elsewhere to have higher SDQ scores than the Australian average.20
Boys in our study were more likely to be at high risk for conduct problems, hyperactivity/inattention, peer problems and prosocial behaviour difficulties. They were equally likely as girls to be high risk for emotional problems.
Children of Aboriginal and Torres Strait Islander background and children with relative socioeconomic disadvantage were more likely to be at high risk for emotional problems, conduct problems and hyperactivity/inattention.
The Australian Early Development Census (AEDC) is a 3-yearly census of children in their first year of full-time primary education. Data from the 2018 AEDC found similar patterns to our study. Boys were more likely to be developmentally vulnerable than girls; including the social competence and emotional maturity domains.21 Aboriginal and Torres Strait Islander children were more likely to be developmentally vulnerable than other children, as were children from the most disadvantaged socioeconomic groups.
We did not demonstrate an association between physical activity and high-risk Total difficulties score in our study, despite other research linking physical activity participation with reduced depressive symptoms. Our study considered all physical activity together and it may be that different forms of physical activity provide different benefits. For example, Eime et al 22 propose that participation in sport may have psychological benefits beyond that from other forms of physical activity. We did find that increased physical activity participation was associated with lower odds of peer problems and prosocial behaviour difficulties. In their systematic review, Hinkley et al 11 found supportive associations between physical activity with conduct problems, emotional competence, emotional symptoms, hyperactivity/inattention and peer relationships, but conversely also found studies with adverse associations between physical activity with conduct problems and hyperactivity/inattention. Many more studies showed no significant associations.
The ratio of boys to girls at high risk for Total difficulties in our study is consistent with findings from Young Minds Matter, however, our estimates are lower than their reported prevalence of mental health disorders (13.6% of boys and 7.1% of girls).13 Two factors that may explain the difference are the survey scope and survey tools used. The KHC surveys children attending schools in the ACT only, and uses the SDQ to assign risk of mental health disorders. Young Minds Matter assessed children across Australia and used the Diagnostic Interview Schedule for Children Version IV to identify mental health disorders.13
In our study, boys were at higher risk than girls for all subscales of the SDQ other than emotional difficulties. Boys in kindergarten or pre-primary in Young Minds Matter had a higher prevalence of all and different types of mental disorders, compared with girls of the same age.13 Among primary school-aged children they found a higher prevalence of anxiety disorders, attention deficit hyperactivity disorder (ADHD) and conduct disorders for boys, and a higher prevalence of major depressive disorder for girls. However, for high school-aged children, boys had higher rates of ADHD and conduct disorders, but girls had a greater prevalence of major depressive disorder and anxiety disorders. The 2017–18 National Health Survey found that among adults, women report higher rates of psychological distress than men.23 This begs the question as to whether risks and prevalence of behavioural and mental health disorders are becoming more common for men, whether men are more vulnerable only in the younger age groups or whether risk varies for different conditions.
Aboriginal and Torres Strait Islander children in our study had the highest reported levels of physical activity. Despite the potential benefits of physical activity, these children also had the highest levels of risk for behavioural and mental health disorders overall (Total difficulties), emotional difficulties, conduct problems and hyperactivity/inattention. High risk of mental illness has been reprised elsewhere and has in part been attributed to the impacts of intergenerational trauma.24 It is well known that Aboriginal and Torres Strait Islanders have poorer health outcomes than other Australians, and these data have been extensively reported elsewhere.25
Despite the ACT being a fairly homogenous jurisdiction with respect to socioeconomic advantage, degrees of relative disadvantage were found in our study. Children from the two most disadvantaged quintiles were significantly more likely to be at high risk of behavioural and mental health disorders than those from less disadvantaged areas. The relationship between lower socioeconomic status and poorer health outcomes has been seen in numerous settings. The WHO’s report Closing the gap in a generation presents comprehensive and compelling data demonstrating poorer health outcomes both between and within countries based on different elements of social and economic disadvantage.26 In all countries, people in the least socioeconomically advantaged groups have poorer health outcomes. An independent report commissioned by the British Government—The Marmot Review—noted that health inequalities arise secondary to societal inequalities, and that to reduce health inequality society needs to reduce social gradients affecting children.27 The Australian Children’s Headlines Indicators show that across the board children of the least socioeconomic advantage have poorer outcomes than those from the highest.19
Strengths and limitations
The KHC has a number of strengths. It has been conducted for several years, is offered to all children and thus not subject to sampling error and has excellent response rates, providing a large sample for analysis. It includes well-validated questions including the SDQ. It includes measured anthropometric data, which is known to be more accurate than self-reported data.28
The KHC is a series of cross-sectional surveys; we can therefore demonstrate relationships between variables, but inference cannot be made about causality. Despite the high overall response rate, some questions were subject to lower participation. This includes physical activity, which was one of the key variables in our study.
The KHC data are subject to non-response and other non-sampling error. All kindergarten children in all ACT schools were invited to participate, with an overall response rate of 90.9%. The characteristics of children who did not participate in the survey may have been different to those that did. As the response rates were high, any effects of non-response were considered unlikely to be significant. If outcomes were correlated within schools, this may cause clustering which would impact error estimates. For the purposes of our study, this was considered unlikely to be significant. All data are subject to non-sampling error. An example of this is the physical activity measure, which is derived from parent-reported data. As with anthropometric data, measured, objective, physical activity data are more accurate than parent-reported activity.29
Our study did not measure screen time, which is a proxy measure for inactivity, and it may be that high screen time negates the benefits of physical activity or may be an independent risk factor.30 31 The Australian 24-hour movement guidelines for children and young people (5 to 17 years) recommend limiting sedentary recreational screen time to no more than 2 hours/day, and breaking up long periods of sitting as often as possible.6 The Canadian review of evidence for 5–17-year-olds found that increased sedentary behaviour was associated with unfavourable health outcomes a range of indicators.32 The KHC questionnaire will include parental report of screen time from 2019.
We undertook the logistic regression using standard categories for degree of risk from the SDQ. It is possible that different relationships may have been observed if the raw scores were used, as was done in the study by Griffiths et al.9
A potential limitation of using the area-based IRSD to create quintiles of socioeconomic disadvantage for our analysis is that this reflects the area children live in rather than their personal attributes.
Disadvantage in the ACT is found when looking at very small areas, which area-based measures such as SEIFA may miss.33 34 An alternative school-based measure, the Index of Community Socio-Educational Advantage, was considered as the school a child attends may better reflect their level of socioeconomic disadvantage than the suburb they live in. However, its derivation includes the proportion of indigenous students at the school.35 If a sub-population of interest is used in the creation of an area-based measure, it may introduce bias into the results.36 We had geocoded data and we were able to use IRSD at the finest available level—SA1—which overcomes some of the limitations of using area-based measures.
Conclusion
Increased risk of clinically significant behavioural and mental health disorders was seen for boys, Aboriginal and Torres Strait Islander children and those from socioeconomically disadvantaged areas. Despite evidence that physical activity is protective for mental health, we did not find that children who participated in more physical activity had different levels of overall risk than other children. Lower levels of physical activity were associated with being at high risk for peer relationship problems or prosocial behaviour difficulties.
Boys in early childhood are at higher risk of developing clinically significant behavioural and mental health disorders, compared with girls of the same age. Programmes or tailored supports may be needed for boys in this age group.
Health inequalities due to socioeconomic disadvantage are evident from a young age. Interventions that focus on addressing inequity and the impacts of intergenerational trauma, rather than promoting healthy lifestyles, are likely to have greater impact on young children’s mental well-being.
Supplementary Material
Footnotes
Contributors: KO, JA and KAD conceived the original idea and structure of the paper. KO, JA, KC and KAD planned the analysis. KC cleaned and provided the de-identified data. KO prepared the final dataset and undertook the data analysis. KO wrote the paper with significant structural and content input from JA, KC and KAD. All authors approved submission of the manuscript for publication.
Funding: This research project is supported by the Royal Australian College of General Practitioners with funding from the Australian Government under the Australian General Practice Training program. The Kindergarten Health Check is conducted by ACT Health (Canberra Health Services Division of Women, Youth & Children).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: The data collection and consent process has been granted ethics approval through the ACT Health Human Research Ethics Committee (ETHLR.13.316). Ethics approval for our study was granted by the ACT Health Human Research Ethics Committee’s Low Risk Sub-Committee (ETHLR.17.080).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. No additional data available for this study. The Kindergarten Health Check is an ACT health database. Access can be applied for by emailing: augp@anu.edu.au.
References
- 1. Australian Institute of Health and Welfare Australian burden of disease study: impact and causes of illness and death in Australia 2011. 4 Canberra, 2016. [Google Scholar]
- 2. Keegan RJ, Keegan SL, Daley S, et al. Getting Australia moving: establishing a physically literate and active nation (game plan). Canberra: University of Canberra, 2013. [Google Scholar]
- 3. US Department of Health and Human Services (DHHS) Physical activity guidelines Advisory Committee report. Washington DC, 2008. [Google Scholar]
- 4. Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab 2016;41:S197–239. 10.1139/apnm-2015-0663 [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization Physical activity and young people. Available: <https://www.who.int/dietphysicalactivity/factsheet_young_people/en/> [Accessed 2019 Nov 27].
- 6. Australian Government Department of Health Australian 24-hour movement guidelines for children and young people (5 to 17 years): an integration of physical activity, sedentary behaviour, and sleep. Canberra, 2019. [Google Scholar]
- 7. Biddle SJH, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med 2011;45:886–95. 10.1136/bjsports-2011-090185 [DOI] [PubMed] [Google Scholar]
- 8. Brown HE, Pearson N, Braithwaite RE, et al. Physical activity interventions and depression in children and adolescents : a systematic review and meta-analysis. Sports Med 2013;43:195–206. 10.1007/s40279-012-0015-8 [DOI] [PubMed] [Google Scholar]
- 9. Griffiths L, Geraci M, Cortina-Borja M, et al. Associations between children’s behavioural and emotional development and objectively measured physical activity and sedentary time: Findings from the UK Millennium Cohort Study. Longit Life Course Stud 2016;7:124–43. 10.14301/llcs.v7i2.353 [DOI] [Google Scholar]
- 10. Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med 2019;49:1383–410. 10.1007/s40279-019-01099-5 [DOI] [PubMed] [Google Scholar]
- 11. Hinkley T, Teychenne M, Downing KL, et al. Early childhood physical activity, sedentary behaviors and psychosocial well-being: a systematic review. Prev Med 2014;62:182–92. 10.1016/j.ypmed.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 12. Carson V, Lee E-Y, Hewitt L, et al. Systematic review of the relationships between physical activity and health indicators in the early years (0-4 years). BMC Public Health 2017;17:854 10.1186/s12889-017-4860-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goodsell B, Lawrence D, Ainley J, et al. Child and adolescent mental health and educational outcomes. An analysis of educational outcomes from young minds matter: the second Australian child and adolescent survey of mental health and wellbeing. Perth, Australia: Graduate School of Education, The University of Western Australia, 2017. [Google Scholar]
- 14. ABS Australian health survey: physical activity, 2011–12. Australia, 2013. [Google Scholar]
- 15. ACT Health, Healthy Canberra . Australian Capital Territory Chief Health Officer’s Report 2018. Canberra, 2018. [Google Scholar]
- 16. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6. 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- 17. Cole TJ, Lobstein T. Extended International (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012;7:284–94. 10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed] [Google Scholar]
- 18. Australian Bureau of Statistics Socio-Economic indexes for Australia (SEIFA) 2016. Canberra, 2018. [Google Scholar]
- 19. AIHW Children’s Headline Indicators. Available: < https://www.aihw.gov.au/reports/children-youth/childrens-headline-indicators/data> [Accessed 10 Aug 2018].
- 20. Department of Social Services Footprints in time: the longitudinal study of Indigenous Children—Report from wave 5, 2015. [Google Scholar]
- 21. Commonwealth of Australia Australian early development census national report 2018. A snapshot of early childhood development in Australia, 2019. [Google Scholar]
- 22. Eime RM, Young JA, Harvey JT, et al. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act 2013;10:98 10.1186/1479-5868-10-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Australian Bureau of Statistics 4364.0.55.001 - National Health Survey: First Results, 2017-18. Canberra, 2019. https://www.abs.gov.au/AUSSTATS/abs@.nsf/ProductsbyCatalogue/F6CE5715FE4AC1B1CA257AA30014C725?OpenDocument [Google Scholar]
- 24. Dudgeon P, Milroy H, Walker R, Working together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. Canberra: Commonwealth of Australia, 2014. [Google Scholar]
- 25. AIHW Indigenous Australians. Available: < https://www.aihw.gov.au/reports-statistics/population-groups/indigenous-australians/overview> [Accessed 10 Aug 2018].
- 26. Commission on Social Determinants of Health (CSDH) CSDH final report: closing the gap in a generation: health equity through action on the social determinant of health. Geneva, Switzerland: World Health Organization, 2008. [Google Scholar]
- 27. Strategic Review of Health Inequalities in England post-2010 Committee (SRHIEPC) Fair Society, healthy lives (the Marmot review). strategic review of health inequalities in England post-2010, 2010. [Google Scholar]
- 28. Wang Z, Patterson CM, Hills AP. A comparison of self-reported and measured height, weight and BMI in Australian adolescents. Aust N Z J Public Health 2002;26:473–8. 10.1111/j.1467-842X.2002.tb00350.x [DOI] [PubMed] [Google Scholar]
- 29. Sarker H, Anderson LN, Borkhoff CM, et al. Validation of parent-reported physical activity and sedentary time by accelerometry in young children. BMC Res Notes 2015;8:735 10.1186/s13104-015-1648-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act 2011;8:98 10.1186/1479-5868-8-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Trinh L, Wong B, Faulkner GE. The independent and interactive associations of screen time and physical activity on mental health, school connectedness and academic achievement among a population-based sample of youth. J Can Acad Child Adolesc Psychiatry 2015;24:17–24. [PMC free article] [PubMed] [Google Scholar]
- 32. 24-Hour Movement Guidelines Leadership Group Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Guideline development report. Ottawa, Canada: Canadian Society for Exercise Physiology, 2016. [Google Scholar]
- 33. ACT Community Services Directorate Detecting disadvantage in the act. comparative analysis of SEIFA IRSD and SEIFI IRSD in the act. Canberra, Australia: ACT Government, 2012. [Google Scholar]
- 34. Tanton R, Miranti R, Vidyattama Y. Hidden disadvantage in the act: report for act Anti-Poverty week. Canberra, Australia: University of Canberra: National Centre for Social and Economic Monitoring (NATSEM) & Institute for Governance and Policy Analysis (IGPA), 2017. [Google Scholar]
- 35. Australian Curriculum Assessment and Reporting Authority (ACARA) Guide to understanding 2013 index of community Socio-educational advantage (ICSEA) values. ACARA, 2014. [Google Scholar]
- 36. Australian Bureau of Statistics Information paper: measures of socioeconomic status. Canberra, 2011. https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 [Google Scholar]
- 37. ACT Education and Training Directorate Canberra school census, 2014. [Google Scholar]
- 38. ACT Education and Training Directorate Canberra school census, 2015. [Google Scholar]
- 39. ACT Education and Training Directorate Canberra school census, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-034847supp001.pdf (172.3KB, pdf)
bmjopen-2019-034847supp002.pdf (110.5KB, pdf)
bmjopen-2019-034847supp003.pdf (273.8KB, pdf)