Abstract
Background
Domestic violence during pregnancy is a major public health concern. This preventable risk factor threatens both the mother and baby. Routine perinatal care visits offer opportunities for healthcare professionals to screen and refer abused women for effective interventions. It is, however, not clear which interventions best serve mothers during pregnancy and postpartum to ensure their safety.
Objectives
To examine the effectiveness and safety of interventions in preventing or reducing domestic violence against pregnant women.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (31 July 2014), scanned bibliographies of published studies and corresponded with investigators.
Selection criteria
We included randomised controlled trials (RCTs) including cluster‐randomised trials, and quasi‐randomised controlled trials (e.g. where there was alternate allocation) investigating the effect of interventions in preventing or reducing domestic violence during pregnancy.
Data collection and analysis
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy.
Main results
We included 10 trials with a total of 3417 women randomised. Seven of these trials, recruiting 2629 women, contributed data to the review. However, results for all outcomes were based on single studies. There was limited evidence for the primary outcomes of reduction of episodes of violence (physical, sexual, and/or psychological) and prevention of violence during and up to one year after pregnancy (as defined by the authors of trials). In one study, women who received the intervention reported fewer episodes of partner violence during pregnancy and in the postpartum period (risk ratio (RR) 0.62, 95% confidence interval (CI) 0.43 to 0.88, 306 women, moderate quality). Groups did not differ for Conflict Tactics Score ‐ the mean partner abuse scores in the first three months postpartum (mean difference (MD) 4.20 higher, 95% CI ‐10.74 to 19.14, one study, 46 women, very low quality). The Current Abuse Score for partner abuse in the first three months was also similar between groups (MD ‐0.12 lower, 95% CI ‐0.31 lower to 0.07 higher, one study, 191 women, very low quality). Evidence for the outcomes episodes of partner abuse during pregnancy or episodes during the first three months postpartum was not significant (respectively, RR 0.50, 95% CI 0.25 to 1.02, one study with 220 women, very low quality; and RR 0.60, 95% CI 0.35 to 1.04, one study, 271 women, very low quality). Finally, the risk for low birthweight (< 2500 g) did not differ between groups (RR 0.74, 95 % CI 0.41 to 1.32, 306 infants, low quality).
There were few statistically significant differences between intervention and control groups for depression during pregnancy and the postnatal period. Only one study reported findings for neonatal outcomes such as preterm delivery and birthweight, and there were no clinically significant differences between groups. None of the studies reported results for other secondary outcomes: Apgar score less than seven at one minute and five minutes, stillbirth, neonatal death, miscarriage, maternal mortality, antepartum haemorrhage, and placental abruption.
Authors' conclusions
There is insufficient evidence to assess the effectiveness of interventions for domestic violence on pregnancy outcomes. There is a need for high‐quality, RCTs with adequate statistical power to determine whether intervention programs prevent or reduce domestic violence episodes during pregnancy, or have any effect on maternal and neonatal mortality and morbidity outcomes.
Keywords: Female, Humans, Pregnancy, Domestic Violence, Domestic Violence/prevention & control, Domestic Violence/psychology, Pregnancy Outcome, Pregnant Women, Pregnant Women/psychology, Randomized Controlled Trials as Topic, Safety, Sex Offenses, Sex Offenses/prevention & control, Sex Offenses/psychology
Plain language summary
Preventing or reducing partner violence against women during pregnancy
Violence against women by partners during pregnancy is a major public health concern. It can cause physical and psychological harm to women and may lead to pregnancy complications and poor outcomes for babies. It is not clear what sort of intervention best serves women and infants during pregnancy and after giving birth to ensure their safety. Interventions that might work include counselling and psychological therapy to give women more confidence and to encourage them to make plans to avoid abuse. Referral to social workers, shelters and other community‐based resources may also help. For partners, referral can be made to 'batterer' treatment programs.
Routine prenatal care offers opportunities for healthcare staff to identify women at risk of being abused. In this review we included 10 randomised trials involving a total of 3417 women, seven of which studied pregnant women who were at high risk of partner violence. The interventions examined in the studies included a single brief individualised consultation, case management and referral to a social care worker, and multiple therapy sessions during pregnancy and after birth. Due to the lack of data, and the different way outcomes were reported, we were unable to identify interventions that worked better than others. Studies focused on different outcomes and we were not able to pool information to draw conclusions about the overall effectiveness of the interventions. Most of the studies did not report on whether or not there had been any reduction in episodes of violence. There was evidence from a single study that the total number of women reporting partner violence during pregnancy and after birth was reduced for women receiving a psychological therapy intervention. Several of the studies examined whether women who received interventions were less likely to have depression after the birth of the baby, but the evidence was not consistent. Other outcomes for the baby such as reduced birthweight and preterm birth were reported in only one study, and the intervention did not lessen the risk of preterm birth (< 2500 g). None of the studies reported results for important outcomes such as stillbirth, neonatal death, miscarriage, maternal deaths, antepartum haemorrhage, and placental abruption. More information is needed from well‐conducted trials before any particular interventional approach can be recommended.
Summary of findings
Summary of findings for the main comparison. Any intervention to prevent violence (all interventions) versus standard care for preventing or reducing domestic violence against pregnant women.
| Any intervention to prevent violence (all interventions) versus standard care for preventing or reducing domestic violence against pregnant women | ||||||
| Patient or population: all pregnant women Settings: three trials conducted in the USA Intervention: any intervention to prevent violence (all interventions) versus standard care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Any intervention to prevent violence (all interventions) versus standard care | |||||
| Partner abuse: episodes during pregnancy | Study population | RR 0.5 (0.25 to 1.02) | 220 (1 study) | ⊕⊝⊝⊝ very low1,2 | ||
| 182 per 1000 | 91 per 1000 (45 to 185) | |||||
| Partner abuse: episodes during the first 3 months postpartum | Study population | RR 0.6 (0.35 to 1.04) | 271 (1 study) | ⊕⊝⊝⊝ very low1,2 | ||
| 212 per 1000 | 127 per 1000 (74 to 220) | |||||
| Partner abuse: abuse score in the first 3 months postpartum (Conflict Tactics Score*) The CTS is a 19‐item self‐report scale listing behaviours that the respondent’s partner might use in conflicts. Women report the frequency of partner behaviours over the past year on a 7‐point scale where 0 = never and 6 = 20 or more times. | The mean partner abuse: abuse score in the first 3 months postpartum in the intervention groups was 4.2 higher (10.74 lower to 19.14 higher) | 46 (1 study) | ⊕⊝⊝⊝ very low1,3 | |||
|
Partner abuse in the first 3 months postpartum (Current Abuse Score**) The Current abuse score consists of 2 scales: 1) Abuse Assessment Screen (AAS) and 2) Prenatal Psychosocial Profile (PPP). |
The mean partner abuse in the first 3 months postpartum (current abuse score) in the intervention groups was 0.12 lower (0.31 lower to 0.07 higher) | 191 (1 study) | ⊕⊝⊝⊝ very low4,5 | |||
| Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum) | Study population | RR 0.62 (0.43 to 0.88) | 306 (1 study) | ⊕⊕⊕⊝ moderate1 | ||
| 378 per 1000 | 234 per 1000 (163 to 333) | |||||
| Number of low‐birthweight (< 2500 g) babies | Study population | RR 0.74 (0.41 to 1.32) | 306 (1 study) | ⊕⊕⊝⊝ low1,6 | ||
| 154 per 1000 | 114 per 1000 (63 to 203) | |||||
| *The Abuse Assessment Screen (AAS) tool was used to for screening. Respondents who answered ‘yes’ to being physically or emotionally hurt by someone or forced to have sexual activities within the last year were considered abused. These women, who responded "Yes" to AAS tool, were administered the Conflict Tactics Score (CTS).
**The AAS contains 4 questions on emotional, physical, and sexual abuse at any time during the woman’s life, within the previous year and during pregnancy. The severity of physical violence is classified from levels 1 to 5: level 1 = slapping to level 5 = wounding with a weapon. The PPP is a 44‐item Likert‐type scale that measures stress, social support from partner and from others and self‐esteem during pregnancy. Each 11 item sub‐scale asks women to rate their stress from no stress (1) to severe stress (4). RR: risk ratio; CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 All studies contributing data had design limitations. 2 Wide confidence crossing the line of no effect and small sample size. 3 Wide confidence interval crossing the line of no difference and small sample size. 4 All studies contributing data has serious design limitations. 5 Estimate based on small sample size. 6 Wide confidence interval crossing the line of no effect.
Background
Description of the condition
Violence against women and girls is a major health and human rights concern (Beydoun 2010). Women can experience physical or mental abuse throughout their lifecycle, in infancy, childhood, adolescence, during adulthood or older age (Parker 1994; Petersen 1997). Violence has severe health consequences (Feder 2009), and is a social problem that warrants an immediate co‐ordinated response from multiple sectors including healthcare providers and social workers (Goodwin 1990; Newberger 1992).
Violence against women by partners is referred to as domestic violence (DV), spousal assault, intimate partner violence (IPV), wife abuse, wife assault, and battered wife syndrome (Bohn 1996; McFarlane 1996). Most researchers define DV as threats of, or actual physical injury from hitting, slapping, punching, choking, kicking, injury with a weapon, or otherwise injuring an intimate partner (Browne 1997; Campbell 1992; Parker 2002; Stark 1999). Assault and coercive behaviours include physical, sexual, and psychological/emotional attacks, and threats against property, children and pets, economic coercion, and many more such acts. Some are injurious and criminal in nature, while others are not (Hedin 2000). The consequences of abuse are varied, and women suffering DV do not present with a particular set of symptoms. Given this variation, the concept of DV should not be conceptualised as a disease or syndrome, nor should it be considered as a specific health problem (e.g. injury or reproductive, physical, or mental health problem). In fact, more often than not, victims demonstrate strength and ability to take care of themselves and their infant in spite of often untenable situations. However, it is clear that abuse puts the victim at greatly increased risk of a multitude of physical and mental health problems (Howard 2010).
Although estimating the prevalence of DV is difficult (Ballard 1998) and estimates vary, especially during pregnancy, it is likely that most providers of women's healthcare services will encounter many pregnant women who are survivors of DV. For almost 30% of women who experience DV, the first incident occurs in pregnancy (Rodriguez 2001). The prevalence of physical abuse during pregnancy varies around the world: in Canada, reported prevalence ranges from 1.0% to 10.9% (Daoud 2012); in the United States, 0.9% to 20.1% (Gazmararian 1996 ); in the United Kingdom, 1.8% at booking, 5.8% at 34 weeks of gestation and 5.0% at 10 days postpartum (Bacchus 2004); in Sweden, 4.3% (Hedin 1999); in South Africa, 6.8% (Jewkes 2001); and Jejeebhoy 1998 has reported high rates of abuse in India. The prevalence of psychological and sexual maltreatment of women during pregnancy has also been reported at between 13% and 60% (Hedin 1999; Jahanfar 2007; Valladares 2005). DV is reported within all socio‐economic class groupings, but it is most prevalent within the working and lower middle socio‐economic classes (Babu 2009; Nagassar 2010).
Abuse during pregnancy is of particular concern because it is a threat to both maternal and child health (Lewis 2007; Lewis 2011; Shah 2010). It directly (e.g. via trauma to the abdomen) and indirectly affects the mortality and morbidity of fetus and mother. Other health‐related problems and adverse economic circumstances enhance the risk of adverse pregnancy outcomes. It is a chronic problem for mothers and infants as violence exposure tends to continue after pregnancy (Taft 2009b).
Studies to date have demonstrated that physical abuse before, during, and after pregnancy is associated with reproductive health problems such as sexually transmitted diseases (Rodriguez 2001), urinary tract infection (Gazmararian 1996), depression, substance abuse (Rose 2010) and other mental health problems (Browne 1997; Canterino 1999; El Kady 2005). Domestic violence is associated with a higher incidence of unwanted pregnancy (Browne 1997; Parker 2002) and intentional abortions (Canadian Centre for Justice Statistics 2000).
There are many negative effects of DV on pregnancy. The following harms have been clearly documented: maternal deaths (Lewis 2007; Lewis 2011; Saltzman 2003), low birthweight (Chamberlain 2000; Jewkes 2001; Lipsky 2003), placental abruption (Hedin 2000), preterm labour and delivery (Harwin 2006), fetomaternal haemorrhage, fetal death (Mezey 2000), intrauterine growth restriction (Janssen 2003), pregnancy complications due to trauma (Jejeebhoy 1998), miscarriage (Chamberlain 2000), maternal infections, and poor weight gain (Wiist 1999). In addition, DV negatively affects pregnant women's health behaviours (World Health Organization 2000) leading to delayed entry into prenatal care or to women seeking no care at all (Diaz‐Olavarrieta 2002), and increases behavioural risks such as the use of tobacco, alcohol, and illicit drugs, and poor maternal nutrition (Bacchus 2004; Family Violence Prevention Fund 1999; Ng 2005; Parsons 2000; Wathen 2003).
Physical injuries to fetuses and infants, such as bruising, broken bones, and stab wounds, as well as death, have also been described (Ezechi 2004; Valladares 2005). Child abuse is also reported more often among families with a history of DV (Feldhaus 1997) and antenatal violence is associated with an increased risk of child behavioural problems (Flach 2011).
Description of the intervention
There are a number of interventions that have been examined in relation to violence prevention for pregnant women. A review by Sharps 2008 suggested that perinatal home‐visiting programs are likely to reduce the incidence of physical abuse and improve pregnancy and infant outcomes. Another review by Van Parys 2014 stated that there is a lack of evidence as to which intervention is effective during the perinatal period. Nevertheless, some interventions such as home visitation programs and some multifaceted counselling interventions showed promising results. Several studies show that interventions such as wallet‐size cards with community resources listed, spending time in a shelter, individual counselling, and home social support programs, alone or in combination, may decrease physical abuse (McFarlane 2006; Parker 1999). A review focusing on women recruited in DV shelters or refuges suggests that intensive advocacy may reduce physical abuse one to two years after the intervention (Ramsay 2009). There is currently no systematic review examining interventions specifically focusing on pregnant women.
During routine prenatal checkups, the clinician has the opportunity to screen women and then refer to various intervention programs. For women, both screening and intervention programs could lead to referral of identified individuals to appropriate healthcare specialists or agencies for support such as referral to social workers, shelters, counselling or other community‐based resources. For partners, referral can be made to 'batterer' treatment programs. The effectiveness of these programs is not clear (Arias 2002).
Available studies to date have investigated the effectiveness of DV screening on reduction of violence or improving women's health outcomes (Feder 2009; Nelson 2012; Spangaro 2010), but these studies have not investigated pregnancy outcomes.
It is clear that unless DV risk is reduced, screening efforts are of little use. Thus reviews investigating the effectiveness of screening alone are relevant to the topic in hand and worth mentioning. Acceptability and effectiveness of screening for women presenting in prenatal clinics has been studied (Ramsay 2002) and findings suggest that screening programs in antenatal clinics generally increased rates of identification of women experiencing DV. More recent studies provide evidence that universal screening is associated with improved pregnancy outcomes (Coker 2012). Screening programs that took a comprehensive approach (i.e., incorporated multiple program components, including institutional support) were successful in increasing DV identification rates (O'Campo 2011). This evidence suggests that screening for DV may be a useful component of routine antenatal assessment (Janssen 2006).
How the intervention might work
Often, the goal of intervention is to reduce further abuse. Some interventions are designed to improve women's empowerment and to enhance their independence and control. Some attempt to keep women from danger of extreme violence and teach women how to stay safe. Generally, safeguarding women from harm, managing symptoms, conducting a safe communication with others when in an abusive relationship, increasing women's confidence, and improving family networks and relationships are the major objectives of interventional programs (Ford‐Gilboe 2011). Healthcare providers may make positive contributions to women's access to special services designed to reduce violence. These interventions may reduce women's exposure to violence and more generally improve women's health (Kramer 2004; McCloskey 2006). Reducing the contact between partners in violent relationships also reduces opportunities for further abuse and potential harmful activities (Dugan 2003).
Why it is important to do this review
Current literature on the subject is inconclusive (O'Reilly 2010). Some reviews have concluded that there is insufficient evidence to show whether or not interventions or screening are effective (Nelson 2012). Conversely, Horiuchi 2009 has suggested that screening and interventions for pregnant women would be beneficial. It is therefore necessary to obtain a more comprehensive review of the existing evidence to identify the benefit or harm attributed to commonly practiced interventions to prevent or reduce DV.
Moreover, pregnancy is a unique window of opportunity to screen for DV. Women may welcome the opportunity to be asked about DV (Gazmararian 1996), although they need to be able to trust the care giver and be assured of confidentiality of the information exchanged (Gazmararian 2000). Healthcare professionals are in a unique position to identify and assist women during pregnancy.
Objectives
The objective of this review was to examine the effectiveness and safety of interventions in preventing or reducing domestic violence against pregnant women.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials including cluster‐randomised trials and quasi‐randomised controlled trials (e.g. where there was alternate allocation) investigating the effect of interventions in preventing or reducing domestic violence during pregnancy.
Types of participants
Pregnant women of any age at any stage of pregnancy and their partners (if the intervention involved them). We planned to include studies that recruited both pregnant and non‐pregnant women, provided that data were reported separately for pregnant women, and would consider the data reported for pregnant women only in our analysis (no such studies were identified for this version of the review).
Types of interventions
Any intervention without screening or with screening (for those who screen positive) provided during pregnancy and aimed at preventing or reducing the number of episodes of domestic violence. Studies could include interventions carried out in any setting, including healthcare services and community‐based studies.
Types of outcome measures
Although we focused on interventions during pregnancy, violence during pregnancy has an impact on the longer‐term health of women and infants, and we have included some outcomes measured in the postnatal period.
Primary outcomes
Reduction of episodes of violence (physical, sexual, and/or psychological)
Prevention of violence during and up to one year after pregnancy as defined by the authors of trials
Secondary outcomes
Maternal and fetal outcomes
Depression including prenatal or postnatal depression
Miscarriage
Antepartum haemorrhage
Premature labour
Abruptio placenta
Maternal mortality
Neonatal outcomes
Birthweight
Apgar score first minute
Apgar score fifth minute
Stillbirth
Perinatal death
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We contacted the Trials Search Co‐ordinator to search the Cochrane Pregnancy and Childbirth Group’s Trials Register on 31 July 2014.
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of Embase;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We contacted organisations that work in the area of violence for further trials. We also checked references of retrieved articles.
We did not apply any language restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeJahanfar 2013.
For this update, the following methods, which are based on a standard template used by the Cochrane Pregnancy and Childbirth Group, were used for assessing the five reports that were identified as a result of the updated search.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether this would impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
For this update the quality of the evidence was assessed using the GRADE approach (Schunemann 2009). We assessed the quality of the body of evidence relating to the following outcomes for the comparison 'Any intervention to prevent violence (all interventions) versus standard care'.
Partner abuse: episodes during pregnancy
Partner abuse: episodes during the first three months postpartum
Partner abuse: score in the first three months postpartum (Conflict Tactics Scale)
Partner abuse in the first three months postpartum (Current abuse score)
Partner abuse: total episodes at final study assessment (pregnancy and to 10 weeks postpartum)
Number of low birthweight babies (< 2500 g)
GRADEprofiler (GRADE 2008) was used to import data from Review Manager (RevMan 2014) in order to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference with 95% confidence intervals.
Unit of analysis issues
Cluster‐randomised trials
For this update, there was one mixed‐methods trial identified (Sharps 2013). In this trial, one group of urban women were individually randomised to treatment and 12 rural sites were also randomised. The only outcome reported for this review was retention rates, and therefore no relevant analysis was undertaken. If in future updates we included more cluster‐randomised trials, we will adjust appropriate data using the methods described in the Handbook [Section 16.3.4 or 16.3.6] using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity or subgroup analysis to investigate the effects of the randomisation unit.
Cross‐over trials
This review does not include cross‐over trials. It is unlikely that cross‐over designs would be a relevant trial design for Cochrane Pregnancy and Childbirth Group reviews.
Other unit of analysis issues
We did not detect any studies with multiple pregnancies. It is unlikely that this target population will be studied as there are many complications due to other clinical issues such as birthweight discordance, twin‐to‐twin transfusion, higher risk of congential anomalies that impact on the birthweight and other pregnancy outcomes. Confounding factors are many. Thus we did not include twins in the review, given that it is unlikely multiple pregnancies would be included in randomised controlled trials of interventions to prevent or reduce domestic violence.
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if the I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. Had we identified substantial heterogeneity (above 30%), we planned to explore it by pre‐specified subgroup analysis.
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). Had we conducted pooled analyses in this review, we planned to use fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If we had pooled data and noted clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if we had detected substantial statistical heterogeneity, we planned to use random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. We would have treated the random‐effects summary as the average range of possible treatment effects, and discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we would not have combined trials.
If in future updates of this review we use random‐effects analyses, we will present the results as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
Where data were available, we planned to undertake analysis of subgroups by severity of violence. However, no such analyses were undertaken due to lack of data. We planned to assess subgroup differences by interaction tests available within RevMan (RevMan 2014) and to report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
We did not conduct pooled analyses in this review. If, in future updates, such pooled analyses are possible and heterogeneity is identified, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if so, we will used random‐effects analysis to produce it.
Sensitivity analysis
In future updates, if data allow, we plan to carry out sensitivity analyses to explore the effect of trial quality assessed by concealment of allocation, high attrition rates, or both, with poor quality studies being excluded from the analyses in order to assess whether this makes any difference to the overall result.
Results
Description of studies
Results of the search
The original search of the Pregnancy and Childbirth Group Trials Register retrieved 27 reports and, excluding duplicates, further searching identified an additional 10 reports for possible inclusion. A total of 27 trials (37 study reports) were assessed. After assessment we included nine trials and excluded 17. One study is awaiting further assessment (Loree 2008) and more information about this study is in the Characteristics of studies awaiting classification table.
For this update, we identified eight additional reports. One trial was included but with no relevant outcome data reported (Sharps 2013). One trial was an additional report for an included study (Kiely 2010), and one trial was excluded (Bhandari 2012). Five trials are ongoing studies (Feder 2013; Krishnan 2012; Sharma 2013; Taft 2009a; Temmerman 2010). The final numbers are 10 included studies, 18 excluded studies and six studies awaiting assessment or ongoing. We contacted the authors for additional information and data where possible. Only one author (Temmerman 2010) replied that no reportable data are available at this point in time because the study is ongoing.
Included studies
We included 10 randomised trials involving 3417 women. Seven of these trials (2629 women) contributed data to the review. The studies were predominantly carried out in the USA, although there was one trial in Peru (Cripe 2010) and one in Hong Kong (Tiwari 2005).
Participants
Eight of the 10 studies randomised women who were assessed during pregnancy and were identified as being at high risk of partner violence (Calderon 2008; Cripe 2010; Curry 2006; Kiely 2010; McFarlane 2000; Sharps 2013; Tiwari 2005; Zlotnick 2011). In the study by Olds 2004, the women recruited were not specifically at high risk of abuse; women were recruited if they were young (less than 19 years of age), unmarried or in receipt of Medicaid. In the Nagle 2002 trial, it was not clear that participants were at high risk of partner violence.
Interventions and comparisons
The interventions in the included trials varied considerably and ranged from single, brief sessions through to multiple intensive sessions during pregnancy and extending into the postnatal period.
Calderon 2008 described a single brief intervention that involved an interactive computer assessment and tailored advice encouraging women to seek help, and care providers were alerted of a high‐risk status.
In the trial by Cripe 2010, women received a single counselling session by social workers; Tiwari 2005 described a similar brief counselling intervention tailored specifically for Chinese women.
In the Curry 2006 study, women in the intervention group received video advice and then individually‐tailored case management by a nurse with referral as appropriate.
Two trials (Kiely 2010; Zlotnick 2011) described psychological therapy interventions involving multiple sessions during pregnancy with booster sessions in the postnatal period. In the Kiely 2010 trial, sessions were based on cognitive behavioural therapy, while Zlotnick 2011 examined an intervention underpinned by theory relating to interpersonal psychotherapy.
In a three‐arm trial McFarlane 2000 compared a brief intervention with a counselling intervention, or a counselling intervention plus home visits.
In Sharps 2013, the usual care (UC) group received the standard home visitation (HV) and the Domestic Violence Enhanced Home Visitation Program (DOVE) was the intervention. The DOVE intervention group received the standard HV and an additional three prenatal and three postnatal DOVE sessions.
Nagle 2002 examined home visits during pregnancy and the postnatal period as did Olds 2004, although in this latter study one group received visits from a nurse and one from para‐professionals.
The comparison groups mainly received usual care, although this may have included, or been supplemented by, written information on safety planning and, or a list of local resources where women could seek further help or advice on partner abuse.
Outcomes
A serious problem in this review was the lack of consistency in reported outcomes, and the limited range of outcomes reported, and the varied way that outcomes such as depression or experience of violence were measured. Only one of the included studies (Kiely 2010) reported episodes of partner abuse during pregnancy, while four studies (Curry 2006; Kiely 2010; Tiwari 2005; Zlotnick 2011) reported some data on partner abuse in the early postpartum period (up to three months after the birth), we were unable to combine data in a meta‐analysis as results from each study were reported in different ways. For example, while Tiwari 2005 and Zlotnick 2011 both reported scores on the Conflict Tactics Scale in the postnatal period, Zlotnick 2011 reported overall scores whereas Tiwari 2005 reported scores for separate dimensions, and we were unable to collapse these results into a single score. In a further study, results on partner abuse were not reported in a way that allowed us to include them in data and analysis tables (mean results were reported without standard deviations and there was insufficient information to allow us to impute values) (McFarlane 2000); this study also included some data on the use of community resources.
Several of the included studies did not report on episodes of abuse. Calderon 2008, for example, focused on whether or not women discussed partner violence with those providing care; it was not clear whether such discussions had any tangible effect. Nagle 2002 predominantly reported process outcomes, while Cripe 2010 focused on safety planning. Sharps 2013 reported only recruitment and retention rates. In the study by Olds 2004, a multiplicity of outcomes were reported over a series of papers. These included partner violence along with pregnancy outcomes and long‐term developmental outcomes in children, although it was not clear whether these outcomes were prespecified. Overall, there was little information on other review outcomes including depression and stress in pregnancy and the postnatal period, and outcomes for babies including birthweight and preterm birth.
Excluded studies
We excluded 18 studies. The main reason for excluding studies was that the interventions were not aimed at pregnant women. Three studies examined home visitation interventions to support women after the birth of the child; Armstrong 1999 focused on support by child health nurses, while Quinlivan 2003 examined visits by nurse‐midwives during the period following the birth; Bair‐Merritt 2010 looked at a parent support intervention over three years by para‐professionals. None of these trials specifically aimed to reduce or prevent partner violence during pregnancy. In the study by Eddy 2008 the intervention was aimed at professionals rather than pregnant women, and in the Koziol‐McLain 2010 trial, women were recruited in hospital emergency departments and were not necessarily pregnant. Miller 2011 focused on women attending family planning clinics and the aim of the intervention was to prevent reproductive coercion. The study by Taft 2009a focused on women at high risk of abuse but included women with children under five, pregnant women and other women who were perceived as being at risk. Separate results were not reported for pregnant women.
In five studies, while the focus was on partner violence, participants were not randomly allocated to groups (Janssen 2003; Lipsky 2003; Macy 2007; McFarlane 1996; Parker 1999). Bhandari 2012 conducted convenience sampling for a qualitative study.
The remaining studies were excluded because the intervention was not designed specifically to prevent or reduce abuse (Blackmore 2006; Bullock 2009; Marcenko 1994). While Kataoka 2010 did focus on partner violence, the aim of the intervention was to identify the best means of increasing disclosure of abuse by women rather than to prevent abuse. One of the reports identified by the search was a trial registration for a study that did not take place (Janssen 2011).
Risk of bias in included studies
The studies were mixed in terms of overall risk of bias; while many of the studies used methods of sequence generation and allocation concealment that were at low risk of bias, blinding and sample attrition were frequent problems. One of the studies contributing outcome data was considered to be of low risk of bias (Tiwari 2005).
Allocation
Six of the included studies used methods of sequence generation that we assessed as low risk of bias (Calderon 2008; Kiely 2010; Nagle 2002; Olds 2004; Tiwari 2005; Zlotnick 2011); methods included computer‐generated randomisation sequences, or the use of external randomisation services. In three trials, the methods for generating the randomisation sequence were not clear (Cripe 2010; Curry 2006, Sharps 2013), and in one study, the method was assessed as high risk of bias (McFarlane 2000), where group assignment was according to clinic.
Six studies were judged to use methods at low risk of bias for concealing allocation at the point of randomisation. Consecutively numbered opaque sealed envelopes were used in the trials by Tiwari 2005 and Zlotnick 2011, and external telephone randomisation services were utilised by Kiely 2010, Nagle 2002 and Olds 2004. In Calderon 2008, an automated interactive computer programme carried out randomisation. Methods were unclear for Cripe 2010, Sharps 2013, and Curry 2006, and the quasi‐randomisation approach used for sequence generation in the McFarlane 2000 trial meant that it was judged as high risk of bias for allocation concealment as it was possible that allocation could be anticipated by those carrying out randomisation.
Blinding
Blinding women, clinical staff, staff providing interventions, and those collecting outcome data is very difficult for this type of intervention. Blinding was not attempted or not mentioned in six of the included studies, although Cripe 2010, Kiely 2010, Olds 2004 and Tiwari 2005 all reported attempting to blind outcome assessment. It was not clear whether this was successful. The overall impact of lack of blinding in these studies is difficult to assess. It is possible that for outcomes such as self‐reported episodes of partner violence, the lack of blinding may have caused some response bias. For other outcomes, such as preterm birth, lack of blinding may have been less of a problem.
Incomplete outcome data
Loss of women to follow‐up did not appear to be a serious problem in the studies by Cripe 2010, Olds 2004, Tiwari 2005, and Zlotnick 2011, although there were missing data for some outcomes in the Olds 2004 trial, and Zlotnick 2011 did not provide information on reasons for loss to follow‐up. In the study by Curry 2006, more than 1000 women were randomised but results were reported only for the small sub‐sample assessed as being at high risk of DV. In the trials by McFarlane 2000 and Nagle 2002 there were high levels of sample attrition. Loss of women to follow‐up may be a serious problem even with low or modest sample attrition; it is possible that those women most at risk of poor outcomes (such as abuse) would be more likely than others to be lost to long‐term follow‐up (Higgins 2011).
In two studies, women were assessed for a broad range of risk factors including smoking and other factors associated with poor pregnancy outcomes (Calderon 2008; Kiely 2010). The women randomised to partner violence interventions may have formed only a small proportion of the total sample randomised, and women may have received interventions for more than one risk factor. The impact of this on particular outcomes was difficult to assess. Multiple interventions may have had a synergistic or interactive effect, and for some outcomes, if women had more than one intervention, it would be difficult to ascertain which intervention led to any possible differences between groups. For example, women may have smoked and have been at high risk for DV, and therefore received multiple interventions; under these circumstances it would not be easy to disentangle which intervention, if any, influenced outcomes such as infant birthweight or preterm birth.
Selective reporting
It was difficult to assess outcome reporting bias without access to trial registrations and study protocols and most studies were judged to be at unclear risk of bias because we only had access to published study reports. We have already mentioned the difficulty interpreting outcomes with stratified samples and multiple interventions in the studies by Calderon 2008 and Kiely 2010. Interpreting findings from the Olds 2004 study was also hampered by possible outcome reporting bias. Several papers have been published on this trial and different papers focus on different outcomes, it was not clear that all outcomes reported were pre‐specified, nor was it clear how different aspects of the interventions were associated with particular outcomes.
Other potential sources of bias
Most of the studies appeared to have comparable groups at baseline in terms of participant characteristics. Some of the studies provided little information on methods so assessment of overall risk of bias was difficult. We have set out findings for overall risk of bias in Figure 1 and for individual studies in Figure 2.
1.
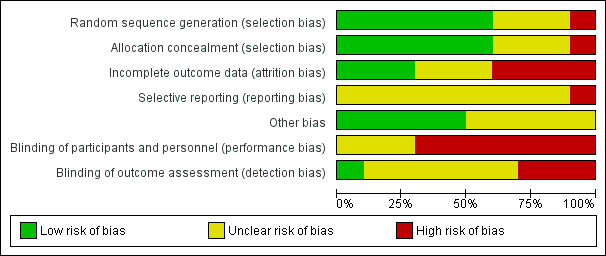
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
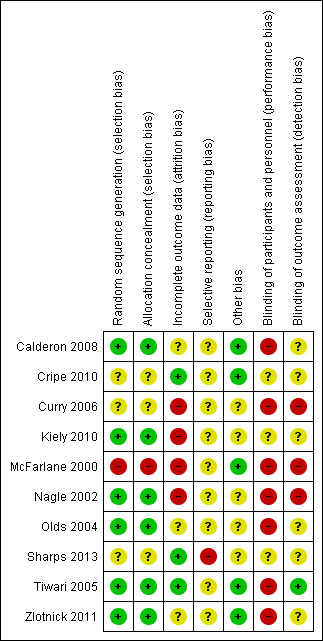
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1
Comparison: Any intervention to prevent violence (all interventions) versus standard care
Due to lack of consistency in the outcomes reported in included studies, we were unable to combine results from trials in meta‐analysis, and results are derived from single studies.
Primary outcomes
Kiely 2010 suggests that women randomised to the group receiving a psychological therapy intervention were less likely to have recurrent episodes of abuse during pregnancy compared with those receiving usual care, although the difference between groups did not reach statistical significance (risk ratio (RR) 0.50, 95% confidence interval (CI) 0.25 to 1.02, 220 women, very low quality) (Analysis 1.1). The protective effect of psychological therapy continued during the first three months of follow‐up postpartum although again, results were not statistically significant (RR 0.60, 95% CI 0.35 to 1.04, 271 women, very low quality) (Analysis 1.2). In this study there was a significant difference between groups in the total number of women reporting DV at any point during pregnancy and/or in the postnatal period, with women in the intervention group being less likely to report abuse (RR 0.62, 95% CI 0.43 to 0.88, 306 women, moderate quality) (Analysis 1.6).
1.1. Analysis.
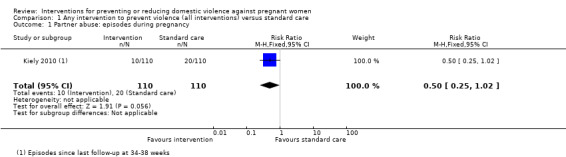
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 1 Partner abuse: episodes during pregnancy.
1.2. Analysis.
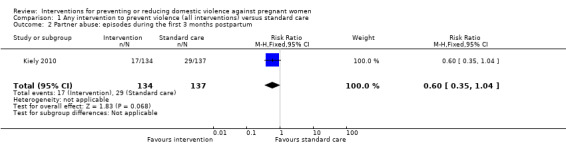
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 2 Partner abuse: episodes during the first 3 months postpartum.
1.6. Analysis.
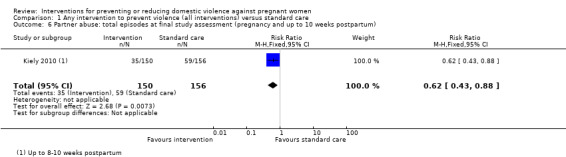
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum).
In other studies examining DV in the postnatal period, findings were inconsistent, and most of the results were not statistically significant. The Zlotnick 2011 study examined a psychotherapy intervention and DV in the first three months after the birth was measured using the Conflict Tactics Scale; the difference between the intervention and control group was not statistically significant (mean difference (MD) 4.20, 95% CI ‐10.74 to 19.14, 46 women, very low quality) (Analysis 1.3). Differences between group scores for DV in the first three months postpartum in the study by Curry 2006 had a MD of ‐0.12 (95% CI ‐0.31 to 0.07, 191 women, very low quality); the evidence of a difference between groups receiving nurse case management or usual care was not statistically significant (Analysis 1.5).
1.3. Analysis.
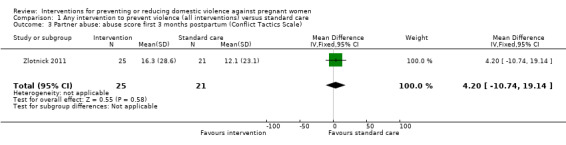
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale).
1.5. Analysis.
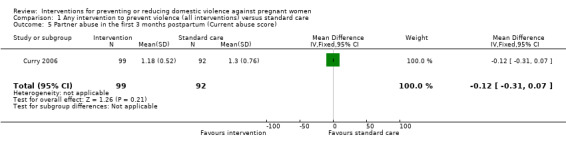
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 5 Partner abuse in the first 3 months postpartum (Current abuse score).
Tiwari 2005 also used the Conflict Tactics Scale to assess DV in the first three months postpartum following a brief antenatal counselling intervention that focused on improving relationships with partners and strengthening social networks. For this study, mean scores on subscales measuring psychological, physical (minor and severe) and sexual abuse were reported separately. The intervention appeared to be effective in reducing minor physical violence (MD ‐0.46, 95% CI ‐0.82 to ‐0.10) and psychological abuse (MD ‐0.81, 95% CI ‐1.45,to ‐0.17). Severe physical violence and sexual abuse scores were not significantly different between the intervention and control groups (MD 0.08, 95% CI ‐0.28 to 0.44, and MD ‐0.09, 95% CI ‐0.24 to 0.06, respectively) (Analysis 1.4).
1.4. Analysis.
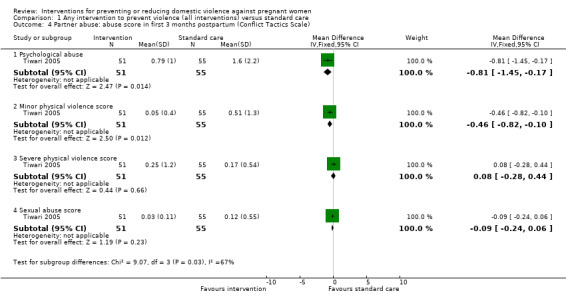
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale).
Nagle 2002 examined the effects of a nurse home‐visiting intervention and found no significant difference between groups for the number of women reporting DV at seven to eight months postpartum (Analysis 1.7).
1.7. Analysis.
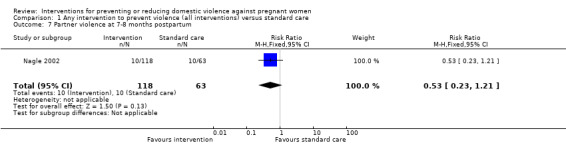
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 7 Partner violence at 7‐8 months postpartum.
In a study examining a counselling intervention with or without support from a mentor compared with a brief intervention, authors reported that the severity of abuse decreased over the study period in all groups. However, there were no clear differences between different intervention groups for mean physical violence scores at up to 18 months postpartum (McFarlane 2000). (We have not included data from this study in the data and analysis tables as standard deviations were not reported, and we did not have sufficient information to impute values.)
Secondary outcomes
There was no strong evidence that risk of a major depression episode during pregnancy was lower in the intervention group than in the control group in the study by Zlotnick 2011 (RR 0.42, 95% CI 0.04 to 4.31) (Analysis 1.8) and there was no statistically significant difference in the mean number of depression episodes (Psychiatric Status Rating) (MD ‐0.46, 95% CI ‐0.97 to 0.05) (Zlotnick 2011) (Analysis 1.9).
1.8. Analysis.
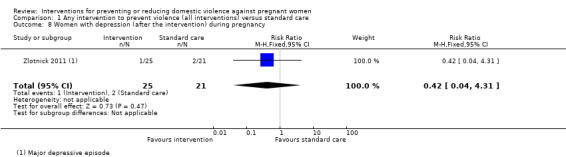
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 8 Women with depression (after the intervention) during pregnancy.
1.9. Analysis.
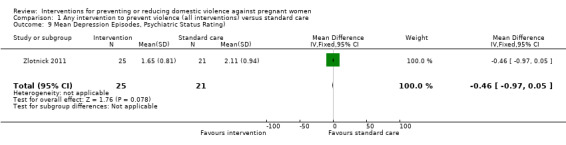
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 9 Mean Depression Episodes, Psychiatric Status Rating).
The number of women with depression at up to three months postpartum was reported in two studies examining empowerment training and interpersonal psychotherapy respectively (Tiwari 2005; Zlotnick 2011). In view of differences between the interventions and statistical heterogeneity in findings (I2 = 66%), we decided not to pool results from these studies and have reported sub‐totals only. Tiwari 2005 reported a positive treatment effect following a brief prenatal intervention (RR 0.39, 95% CI 0.20 to 0.75), whereas, an interpersonal psychotherapy intervention involving multiple sessions (Zlotnick 2011) did not appear reduce the number of women with depression (RR 1.40, 95% CI 0.38 to 5.18) (Analysis 1.11). Zlotnick 2011 also reported mean scores on the Edinburgh Postnatal Depression Scale at three months postpartum and identified no clear difference between groups (MD ‐1.88, 95% CI ‐5.24 to 1.48) (Analysis 1.12).
1.11. Analysis.
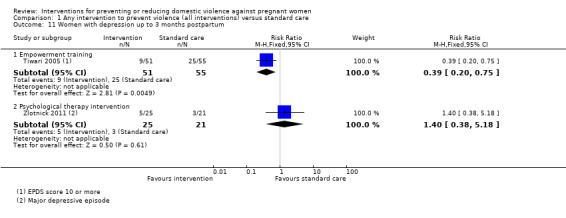
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 11 Women with depression up to 3 months postpartum.
1.12. Analysis.
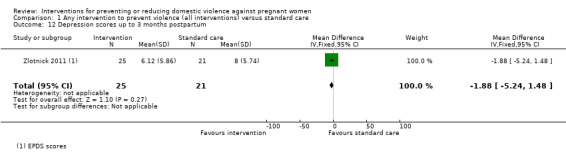
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 12 Depression scores up to 3 months postpartum.
Nagle 2002 reported the number of women with depression (scoring greater than 16 on the Beck Depression Inventory) and mean depression scores at seven to eight months postpartum; there was no strong evidence of differences between groups for either outcome (RR 0.85, 95% CI 0.37 to 1.98, and MD ‐0.65, 95% CI ‐2.41 to 1.11, respectively) (Analysis 1.13; Analysis 1.14).
1.13. Analysis.
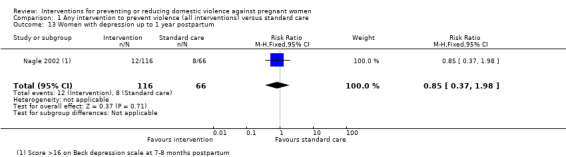
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 13 Women with depression up to 1 year postpartum.
1.14. Analysis.
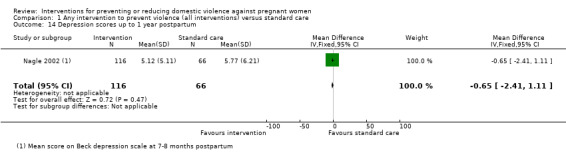
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 14 Depression scores up to 1 year postpartum.
The study by Kiely 2010 and colleagues examining the effectiveness of a psycho‐behavioural intervention was the only one that reported neonatal outcomes. Mean birthweight was similar for babies whose mothers were in the intervention group who received individually‐tailored therapy sessions compared with women receiving usual care (3139 g ± 593 versus 3098 g ± 717) (MD 41.00, 95% CI ‐106.19 to 188.19) (Analysis 1.23). The number of low birthweight babies (less than 2500 g) was also similar in the two groups (RR 0.74; 95% CI 0.41 to 1.32, 306 infants, low quality) (Analysis 1.24). The intervention was not associated with any significant reduction in the overall number of preterm births in this study (RR 0.69, 95% CI 0.40 to 1.20) (Analysis 1.25), although there was a significant increase in mean gestational age at delivery for women in the intervention group (MD 1.40 weeks, 95% CI 0.33 to 2.47) (non‐prespecified outcome, Analysis 1.26).
1.23. Analysis.
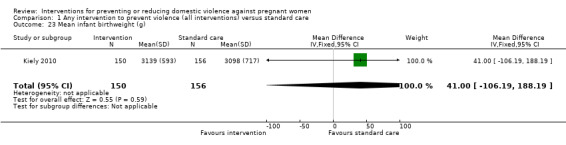
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 23 Mean infant birthweight (g).
1.24. Analysis.
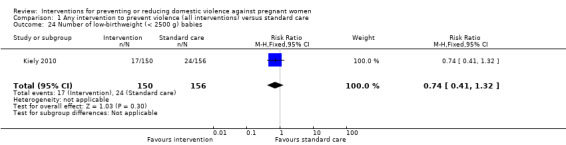
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 24 Number of low‐birthweight (< 2500 g) babies.
1.25. Analysis.
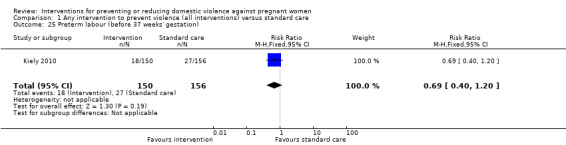
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 25 Preterm labour (before 37 weeks' gestation).
1.26. Analysis.
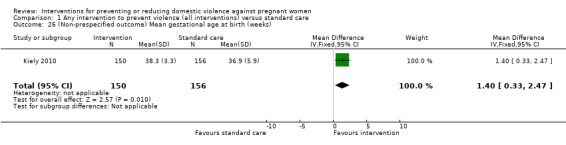
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks).
Other secondary outcomes
None of the studies reported results for several of our secondary outcomes: Apgar score less than seven at one minute, and five minutes; stillbirth, neonatal death, miscarriage, maternal mortality, antepartum haemorrhage, and placental abruption.
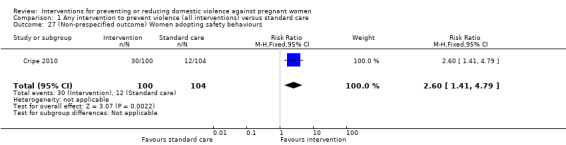
Non‐prespecified outcomes
Several studies reported data on outcomes that we had not prespecified. Cripe 2010 examined an empowerment intervention in pregnancy compared with usual care. Results showed that women in the intervention group were more likely to make plans to avoid abuse by adopting safety behaviours (RR 2.60, 95% CI 1.41 to 4.79) (Analysis 1.27).
1.27. Analysis.
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 27 (Non‐prespecified outcome) Women adopting safety behaviours.
Curry 2006 investigated active case management by nurses aiming to reduce stress among pregnant women, and reported some reduction in stress scores for women receiving the intervention (MD ‐2.06, 95% CI ‐3.34 to 0.78) (Analysis 1.28).
1.28. Analysis.
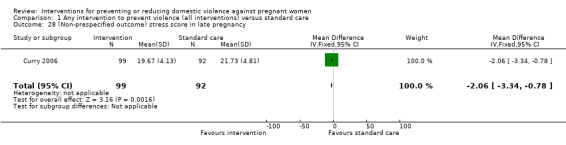
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 28 (Non‐prespecified outcome) stress score in late pregnancy.
Calderon 2008 examined an intervention that aimed to increase identification of women suffering violence in pregnancy and reported that the intervention led to more women discussing abuse with their healthcare providers (Analysis 1.29).
1.29. Analysis.
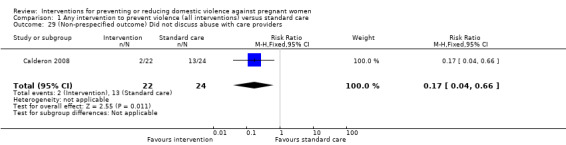
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 29 (Non‐prespecified outcome) Did not discuss abuse with care providers.
Women were followed up over several years following home visits by public health nurses during pregnancy and the postnatal period in the study by Olds 2004. It was not clear in this study whether or not prevention or reduction of DV was a pre‐specified outcome, nor whether the intervention was tailored for women at risk of abuse. The number of women reporting violence two to four years after the birth was not significantly different in the intervention and control groups (Analysis 1.30).
1.30. Analysis.
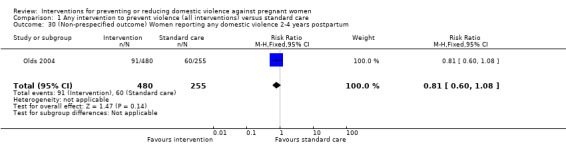
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum.
Sharps 2013 compared the usual care (UC) group, who received the standard home visitation (HV), with the Domestic Violence Enhanced Home Visitation Program (DOVE), which was the intervention. The DOVE intervention group received the standard HV in addition to the DOVE IPV intervention. Women in the DOVE intervention group received three prenatal and three postnatal DOVE sessions in addition to their HV protocols. The recruitment and retention rates were reported. Women who received the DOVE intervention had a higher retention rate.
Discussion
Summary of main results
Our review set out to examine the effectiveness of interventions in preventing or reducing domestic violence (DV) against pregnant women. In this review, there were 10 identified studies of prevention of DV in pregnancy (Calderon 2008; Cripe 2010; Curry 2006; Kiely 2010; McFarlane 2000; Nagle 2002; Olds 2004; Sharps 2013; Tiwari 2005; Zlotnick 2011), eight of which studied pregnant women who were at high risk of partner violence (all except Nagle 2002 and Olds 2004). Six of these studies reported on at least one of our pre‐specified outcomes (Cripe 2010; Curry 2006; Kiely 2010; Nagle 2002; Tiwari 2005; Zlotnick 2011). The interventions examined in the studies varied significantly and included a single brief individualised consultation, case management and referral to social care workers, and multiple therapy sessions during pregnancy and postpartum.
Results for many outcomes were not consistent and most differences between groups were not statistically significant. We were not able to combine results from different studies, in the hope of identifying patterns among study results, source of disagreement (if any) among results, or other interesting relationships that may appear in the context of a meta‐analysis. Due to the lack of data and the disparate way outcomes were reported, we were unable to single out one intervention that works better than the others.
In one study, compared with women receiving usual care, women receiving a psychological therapy intervention were less likely to report DV at any point during pregnancy and/or in the postnatal period (Kiely 2010). An intervention which aimed to improve women's relationships with their partners and strengthen social networks slightly reduced psychological abuse and minor physical violence scores, but had no significant effect on severe physical violence scores (Tiwari 2005). There was no strong evidence that an educational video focusing on abusive relationships along with tailored case management was effective in reducing intimate partner abuse in the first three months postpartum.
Several trials examined the effects of interventions on postpartum depression but results were inconsistent.
There was very little information on outcomes relating to pregnancy complications and neonatal outcomes. The non‐significant effect of psycho‐behavioural intervention on birthweight or preterm birth could be due to the reported effect measures being unadjusted for the confounding effect of gestational age (Kiely 2010).
We did not find any evidence that interventions had a negative, harmful effect.
Overall completeness and applicability of evidence
There was a limited range and lack of consistency in the outcomes reported in the studies included in the review, and in cases where studies measured and reported similar outcomes (such as frequency of violence or depression), they were measured with various tools and at different time points. This meant we were unable to carry out meta‐analysis and this limited our ability to draw conclusions about the overall effect of interventions.
We also noted the paucity of data on various important outcomes that should be the centre of attention for healthcare providers during pregnancy. Only one study investigated outcomes related to newborn babies (Kiely 2010) and none investigated maternal pregnancy outcomes such as miscarriage, maternal mortality, antepartum haemorrhage, and placental abruption.
Quality of the evidence
The risk of bias of the included trials was mixed.
Only six of the included studies used adequate randomisation techniques or allocation concealment. The nature of interventions was such that they did not allow for blinding of women and the staff providing care, thus compromising the validity of study results (i.e. lack of blinding may have led to response bias for outcomes such depression or frequency of DV episodes). Loss of follow‐up was not a major problem in trials for pregnant women as the clinicians had enough time to assess the risk of DV, implement interventions and collect outcome data during routine prenatal and postpartum visits, although sample attrition was a source of concern in some of the included studies (Curry 2006; Kiely 2010; McFarlane 2000; Nagle 2002).
Outcome data for partner abuse episodes during pregnancy and during the first three months postpartum were graded of very low quality, as were the data for the current abuse score and the Conflict Tactics Score. The assessments of very low quality were due to imprecise effect estimates, high risk of bias in the study contributing data, and small sample size. Outcome data for the Conflict Tactics score, broken down into four components, was considered to be of moderate quality, due primarily to the low risk of bias for the study contributing data. Evidence for the outcome of the number of low birthweight babies was graded as of low quality.
Potential biases in the review process
We are aware that there was a risk of introducing bias at all stages of the review process and we took various steps to minimise this. Two review authors assessed eligibility, risk of bias and carried out data extraction and a third author checked assessments. Data were entered by one review author and were checked by a second review author. However, assessing risk of bias, for example, requires individual judgement about the impact of bias on outcomes, so it is possible that a different review team may not have agreed with all of our assessments.
Agreements and disagreements with other studies or reviews
Our conclusions are compatible with the only review (O'Reilly 2010) that appraised both the effect of screening and preventive interventions for DV. The latter part of the review looked at four studies (El‐Mohandes 2008; McFarlane 2000; Parker 1999; Tiwari 2005) focusing on the effectiveness of interventions on prevention of DV. We did not include one of these trials in this review for methodological reasons (Parker 1999).
Authors' conclusions
Implications for practice.
There was so much variation in the study outcomes examined that we were unable to combine study findings to develop a summary measure of the effectiveness and safety of interventions to prevent or reduce violence against pregnant women. None of the studies reported neonatal mortality and important morbidity outcomes.
Implications for research.
The studies included in our analysis examined different interventions, reported on a limited range of outcomes, and varied in the way in which outcomes were measured, and we were unable to conduct a meta‐analysis. With so few good quality research studies on the topic, it is evident that more high‐quality studies are required.
What's new
| Date | Event | Description |
|---|---|---|
| 7 August 2014 | New search has been performed | Search updated. Eight new reports identified. We included one new study (Sharps 2013); excluded one new study (Bhandari 2012); added one additional report for a previously included study (Kiely 2010); added five ongoing studies (Feder 2013; Krishnan 2012; Sharma 2013; Taft 2012; Temmerman 2010). Methods updated and 'Summary of findings' table added. |
| 7 August 2014 | New citation required but conclusions have not changed | Review updated. |
Acknowledgements
Review authors would like to thank Dr Mark Fitzgerald at Vancouver General Hospital, University of British Columbia for providing information and advice at the protocol stage.
As part of the pre‐publication editorial process, the Jahanfar 2013 review was commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
Therese Dowswell for her contributions to the earlier version of this review (Jahanfar 2013).
Nancy Medley's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication.
Data and analyses
Comparison 1. Any intervention to prevent violence (all interventions) versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Partner abuse: episodes during pregnancy | 1 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.25, 1.02] |
| 2 Partner abuse: episodes during the first 3 months postpartum | 1 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.35, 1.04] |
| 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale) | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 4.20 [‐10.74, 19.14] |
| 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Psychological abuse | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐1.45, ‐0.17] |
| 4.2 Minor physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.82, ‐0.10] |
| 4.3 Severe physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.28, 0.44] |
| 4.4 Sexual abuse score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.06] |
| 5 Partner abuse in the first 3 months postpartum (Current abuse score) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.31, 0.07] |
| 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum) | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.43, 0.88] |
| 7 Partner violence at 7‐8 months postpartum | 1 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.23, 1.21] |
| 8 Women with depression (after the intervention) during pregnancy | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.31] |
| 9 Mean Depression Episodes, Psychiatric Status Rating) | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.97, 0.05] |
| 10 Depression scores (after the intervention) during pregnancy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Women with depression up to 3 months postpartum | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Empowerment training | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.20, 0.75] |
| 11.2 Psychological therapy intervention | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.38, 5.18] |
| 12 Depression scores up to 3 months postpartum | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐1.88 [‐5.24, 1.48] |
| 13 Women with depression up to 1 year postpartum | 1 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.98] |
| 14 Depression scores up to 1 year postpartum | 1 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐2.41, 1.11] |
| 15 Apgar score less than 7 at 1 minute | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Apgar score less than 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Stillbirth | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Neonatal death | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Miscarriage (up to 20 weeks) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Antepartum haemorrhage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Placental abruption | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Mean infant birthweight (g) | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 41.0 [‐106.19, 188.19] |
| 24 Number of low‐birthweight (< 2500 g) babies | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.41, 1.32] |
| 25 Preterm labour (before 37 weeks' gestation) | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.40, 1.20] |
| 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks) | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.33, 2.47] |
| 27 (Non‐prespecified outcome) Women adopting safety behaviours | 1 | 204 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.6 [1.41, 4.79] |
| 28 (Non‐prespecified outcome) stress score in late pregnancy | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐2.06 [‐3.34, ‐0.78] |
| 29 (Non‐prespecified outcome) Did not discuss abuse with care providers | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.66] |
| 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum | 1 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.60, 1.08] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Calderon 2008.
| Methods | Stratified RCT. Women were stratified by risk factor combination (1 of 15 possible combinations of 4 risk behaviours (IPV, alcohol, drugs, smoking)). | |
| Participants | Women attending 5 prenatal clinics in the San Francisco bay area (USA). Only women with risk factors were randomised. 37 women experiencing DV were randomised. Inclusion criteria: women less than 26 weeks’ gestation, English speaking, aged 18 years or older, not attending for first prenatal visit who screened positive for one (or more than one) of 4 risk factors (smoking, alcohol, drug use or DV). Exclusion criteria: women who had no risk factors were not randomised. |
|
| Interventions | Experimental intervention: video doctor‐assessment with appropriate messages for risk factor (e.g. encouraging women to discuss problem) and healthcare staff were alerted and given a cueing sheet to discuss risk factor (DV). (20 women randomised to the intervention group.) Control/Comparison intervention: all women had video doctor‐assessment but healthcare staff did not receive cueing sheet. Women randomised to the control group received usual care and any discussion of risk was at the discretion of healthcare staff. (17 women randomised to control condition.) |
|
| Outcomes | This study examined whether discussions re DV occurred and women’s views of the discussion (acceptability and helpfulness). No other outcome data were reported. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was by a computer programme, however, it was not clear how stratification affected the randomisation process as some women may have had several risk factors (it was not clear whether these women would then receive several intervention messages and several staff cueing forms). |
| Allocation concealment (selection bias) | Low risk | By computer programme. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 37 women experiencing DV were randomised and data appear available for all women at the immediate post‐intervention assessment. There were some missing data at follow‐up (32 were followed up at 2 months) but all women were included in a sensitivity analysis (those lost to follow‐up were assumed to have had no discussion of DV). |
| Selective reporting (reporting bias) | Unclear risk | Results for women assessed with a single risk factor were reported but it seems that women may have had multiple risk factors and multiple interventions and there may have been some interaction effect (it is possible that if a woman had multiple risk factors then she was more likely than those with a single risk factor to have discussions with healthcare staff). |
| Other bias | Low risk | Other bias not apparent. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Staff would have been aware of group assignment because the interview would have been conducted according to the intervention cue sheet for the intervention group. It is unclear whether women would have been aware of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Staff would have been aware of group assignment because the interview would have been conducted according to the intervention cue sheet for the intervention group. It is unclear whether women would have been aware of group assignment. Outcomes are self‐reported, so it is unclear whether these would have been shaped by knowledge of group assignment. |
Cripe 2010.
| Methods | RCT. 2‐arm trial with individual randomisation. | |
| Participants | Setting: public hospital in Lima, Peru, providing services to low‐income women living in Lima. Recruitment in 2007. Inclusion criteria: 220 pregnant women (gestational age between 12 and 26 weeks’ gestation) attending for care in the study hospital who screened positive for DV on the modified Abuse Assessment screen and able to speak and understand Spanish. (Women screened positive if they said yes to any of the following in the past year – been pushed, shoved, slapped, hit, kicked or otherwise physically hurt or been forced into sexual activity by a former or current partner.) |
|
| Interventions | Experimental intervention: (110 randomised) empowerment intervention during pregnancy which included standard care (a card with information about agencies providing IPV support). Women in the empowerment intervention received supportive counselling and education, and advice in the areas of safety by a trained social worker lasting about 30 minutes. Interviewers listened empathetically to the women and acknowledged their perceptions and feelings. Interviewers also helped women understand the cycle of violence and reviewed components of the safety plan including behaviours indicated in the Safety Behavior Checklist. For example, women were asked how they might secure and hide money and important documents such as birth certificates. Interviewers helped women develop a code to use with family and trusted friends to signal the need for assistance and/or to mentally plan their escape when needed. Women were given a brochure with a 13‐item safety plan to reinforce safety behaviours. To make the safety plan brochure less conspicuous, other prenatal brochures on topics such as breastfeeding or nutrition were also offered to the women. Interviewers also provided a list of community resources, such as emergency shelter, legal aid, law enforcement, and counselling, and strategies for seeking help from these resources. As part of the intervention, interviewers also offered to assist women with telephone calls to social service agencies or women's groups who could act as advocates for abused women. At the conclusion of the empowerment intervention session, interviewers helped women determine if it was safe for her to keep the safety plan brochure and the referral card. Women were free to discuss the pros and cons of leaving the abuser, reporting the abuser to law enforcement, or applying for a protection order. Control/Comparison intervention: (110 randomised) women randomised to receive standard care received a wallet‐size referral card listing agencies that provide DV services to abused women (e.g., legal, social services,and law enforcement). No counselling, advocacy, education, or other services were offered to women in this group during pregnancy. However, they were provided the empowerment intervention, specifically supportive counselling and education, and advice in the areas of safety by a trained social worker at the conclusion of the study during the 6th week postpartum visit. |
|
| Outcomes | Physical, functional and emotional functioning at follow‐up as compared with baseline. Use of community resources and safety behaviours. Episodes of violence in the past year were reported at baseline but data on this outcome were not reported at follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Assignment was by a “randomised block design” but how the sequence was generated and block size were not stated. |
| Allocation concealment (selection bias) | Unclear risk | Methods used to allocate women to groups at the point of randomisation were not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Sixteen women (7.3%) were lost to follow‐up. 220 women were randomised and follow‐up data were available for 204. |
| Selective reporting (reporting bias) | Unclear risk | Episodes of violence at follow‐up were not reported in this paper (it may be that these outcomes will be addressed in future papers). |
| Other bias | Low risk | Groups were reported to be similar at baseline and there was no other bias apparent. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Women and staff would be aware of the purpose of the study and which group they were assigned to. Post‐intervention interviews were carried out by a different interviewer than those who carried out the pre‐intervention ones to reduce bias. It was not clear what impact lack of blinding would have on the outcomes reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Women and staff would be aware of the purpose of the study and which group they were assigned to. Post‐intervention interviews were carried out by a different interviewer than those who carried out the pre‐intervention ones to reduce bias. It was not clear what impact lack of blinding would have on the outcomes reported. |
Curry 2006.
| Methods | RCT, 2 arms with individual randomisation (2 sites). | |
| Participants | 1000 women who spoke English and were 13 to 23 weeks pregnant at the time of recruitment. At the completion of the first assessment, women were randomised to 1 of the 2 groups, 501 to the control group and 499 to the treatment group. Prenatal Psychosocial Profile test was used to estimate women's stress level. After women at risk of abuse with high level of stress were identified, 106 were in the intervention group and 101 in the control group. Study carried out in two prenatal clinics of a Health Maintenance Organisation in the USA (clinics both served what was described as a geographically, culturally and economically diverse group). Each clinic enrolled 500 women over the period 2001‐2003. Exclusion criteria: adolescents for whom consent was not available. |
|
| Interventions | Experimental intervention: standard care plus video about abuse (watched by < 30%), 24/7 access to Nurse Case Management. Women were contacted by phone by nurse who actively managed their care. The intervention was intended to provide support and was individually tailored to women’s needs. Control/Comparison intervention: standard care which involved written information on community and health services resources for abused women. (Women assessed as being in danger were provided with safety planning and the offer of referral to the clinic social worker.) |
|
| Outcomes | Process outcomes (number of contacts, etc). The outcomes reported in this paper related to stress scores on Prenatal Psychosocial Profile measure (it was not clear what other outcome information was collected). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1000 women were enrolled on the study. 106 women in the intervention group and 101 women in the control group were assessed as being at high risk at the first study assessment and results were only provided for the high‐risk group (i.e. approximately 20% of those randomised). Of the high‐risk groups 99 of the high‐risk intervention group and 92 of the high‐risk control group provided follow‐up data. |
| Selective reporting (reporting bias) | Unclear risk | It was not clear what outcome data were collected. |
| Other bias | Unclear risk | There was very little information on methods and there may be further outcome data not published in this paper. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described. It is likely that women and staff were aware of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not described. It is likely that outcome assessors were aware of group assignment. |
Kiely 2010.
| Methods | A complex RCT with several arms and 4 different interventions targeting women with risk factors (depression, smoking, passive smoking and IPV). Women may have had more than 1 risk factor and may have been randomised to receive more than 1 intervention. Women at risk of IPV were randomised into intervention and control arms. | |
| Participants | Setting: 6 community prenatal clinics serving mainly African‐American women in Washington DC. July 2001‐2003. Inclusion criteria: women from minority groups (mainly African‐American) aged at least 18 years, 28 weeks pregnant or less, English speaking and resident in the study area. Exclusion criteria: women who were identified as suicidal at baseline or follow‐up were excluded. |
|
| Interventions | Experimental intervention: cognitive behavioural intervention focusing on 4 risk factors (smoking, passive smoking, depression and DV). Women received an intervention specifically focusing on their individual risk factors (most women had more than one risk factor and would receive more than 1 intervention component. 336 women reported DV and 169 were randomised to the DV intervention group. The intervention was delivered as part of routine prenatal visits by psychologists or social workers. The intervention was based on empowerment theory and emphasised safety planning and behaviours and a list of phone numbers for community resources was provided. The intervention took place over several sessions lasting about 30 minutes and women received a small incentive for attending sessions. There were 2 postpartum booster sessions to reinforce messages. 51% of women in the intervention group received 4 or more sessions and a quarter attended none. Comparison group: 167 of the women reporting DV received standard care according to protocols at each clinic. |
|
| Outcomes | DV was identified by Abuse Assessment Screen at baseline. Follow‐up sessions used Conflict Tactics Scale to identify women at risk. Episodes of DV during pregnancy and in the early postpartum period (minor and severe and sexual violence). Low and very low birthweight, gestational age at delivery, preterm and very preterm birth. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation scheme with site and risk specific permuted block randomisation with investigators and staff blinded to block size. |
| Allocation concealment (selection bias) | Low risk | Allocation by external data co‐ordinating centre by telephone. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 1000 women were recruited to this trial and randomised. Randomisation was stratified according to baseline risk and only those women with DV risk were randomised for the DV intervention. (In this review we have reported findings for those women identified at risk of DV and randomised to receive or not receive the DV intervention; If we carried out analysis using all women randomised any intervention effect would be diluted considerably). 336 with DV risk had baseline data but there were considerable amounts of missing data at follow‐up, although there were some outcome data for at least 1 of the follow‐up interviews for 306 women and outcome data for babies were available for 306 women. It was reported that women were analysed by randomisation group whether or not they received the planned intervention. |
| Selective reporting (reporting bias) | Unclear risk | Most women had more than 1 risk factor and were likely to receive different interventions – the interventions may have had some synergistic or interactive effect. But results are reported only by single risk factors – i.e. this paper only focuses on women reporting DV at baseline. |
| Other bias | Unclear risk | Intervention and control group characteristics appeared similar at baseline. It was no clear how many woman received multiple interventions or whether women in the control group received other interventions to address risk factors other than DV. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Women and staff delivering intervention would be aware of group assignment. Telephone interviewers were reported to be blind to allocation but it was not clear whether this was successful (women may have revealed their allocation during interviews). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Women and staff delivering intervention would be aware of group assignment. Telephone interviewers were reported to be blind to allocation but it was not clear whether this was successful (women may have revealed their allocation during interviews). |
McFarlane 2000.
| Methods | 3‐arm trial. Quasi‐randomisation (clinics rotated through different interventions; “monthly sequential assignment. | |
| Participants | Setting: 2 prenatal clinics in SW USA. Each clinic served 2000‐3000 pregnant women each year and 97% were Hispanic. Inclusion criteria: women who reported abuse in the year prior to or during current pregnancy by current or former male partner (mean gestational age at recruitment 18 weeks). Exclusion criteria: not described. |
|
| Interventions | 335 women agreed to participate. 96% women Hispanic – and only results for these 329 women are reported in this paper. 3 interventions:
|
|
| Outcomes | Follow‐up at 2, 6, 12 and 18 months post‐intervention (i.e. after delivery). Outcomes were reported abuse and use of resources. Abuse on Severity of Violence against Women Scale (SVAWS) a 46 item scale; 19 items on threats of violence and 21 items on physical violence and 6 items on sexual violence with 4 point response re how often the behaviour occurred – never (1) to many times (4). Possible scores 19‐76 on threats and 27‐108 on violence. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Women were allocated by clinic. |
| Allocation concealment (selection bias) | High risk | Women were allocated by clinic; it is possible that women attending the different clinics were different and the order in which staff delivered the interventions may have had an effect. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Results only reported for Hispanic women in the sample. Results by intervention group were available for 259/329 women (79%) (> 20% missing data). |
| Selective reporting (reporting bias) | Unclear risk | Results in this paper for Hispanic women only – while they were 96% of the population it is not clear why other women were excluded or whether they were balanced across groups. Results are reported by gestational age at recruitment and over time – so there were a large number of possible correlations. |
| Other bias | Low risk | Groups were described as similar at baseline. Other bias not apparent. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of blinding; lack of blinding may have affected responses and other aspects of care. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of blinding; lack of blinding may have affected responses and other aspects of care. |
Nagle 2002.
| Methods | 3‐arm RCT. Individual women randomised. | |
| Participants | Setting: pregnant women attending state public health clinics in 3 parishes in Louisiana USA 1999‐2000. Inclusion criteria: pregnant women less than 28 weeks’ gestation with no previous live births and Medicaid eligible. |
|
| Interventions | Experimental intervention: 2 intervention arms that were combined in the results.
Control/Comparison intervention: usual care (not clearly described). |
|
| Outcomes | This thesis mainly reports on participation and adherence. Long‐term outcomes included child development, abuse and neglect, injury, subsequent pregnancy, mother‐child interaction and maternal employment. At follow‐up in the third trimester (28‐34 weeks) and at 6‐8 months postpartum results were described for depression (Beck Depression Inventory) and for partner violence (current and previous) (partner violence interview) with 13 items on physical violence (0 – never experienced, 1 – has experienced) (the time frame for reporting violence was not described). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by an external agency. |
| Allocation concealment (selection bias) | Low risk | It was stated that the nurses carrying out recruitment had no influence over randomisation which was carried out by an external agency (allocations were obtained by telephone). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 357 women consented to participation and were randomised (241 in intervention groups and 116 controls). There was considerable loss to follow‐up and deviations from protocol. 19.5% of intervention women received no intervention. 32.8% did not complete the first follow‐up interview at 28‐34 weeks, and an additional 9% of the women did not have this interview until after the birth of the baby and data were therefore not included in the analysis (206 followed up at interview one and 181 available at the postpartum follow‐up). Loss was balanced across groups but this loss to follow‐up and the large number of women not receiving the allocated intervention means that results are difficult to interpret. |
| Selective reporting (reporting bias) | Unclear risk | This thesis concentrated on only a limited part of the overall research project. The large number of analyses means that some significant results may have occurred by chance. |
| Other bias | Unclear risk | There was little information on some aspects of the trial design. We are not aware that other results from this trial have been published. Groups appeared similar at baseline. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and staff were aware of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants and staff were aware of group assignment. Knowledge of treatment group may have affected reporting of outcomes. |
Olds 2004.
| Methods | RCT, 3‐arm trial, individual randomisation. | |
| Participants | Low‐income, pregnant women with no previous live births referred to antenatal clinic in Denver (n = 735) were included in this study. These women were either qualified for Medicaid or had no private insurance. Setting: 21 public and private healthcare settings in Denver, Colorado USA 1994‐5. Inclusion criteria: low‐income women with no previous live births and qualified for Medicaid or had no private medical insurance. |
|
| Interventions | Home visits were provided from pregnancy through to child age 2 years. The home‐visiting program had 3 broad goals, (1) to improve maternal and fetal health during pregnancy by helping women improve their health‐related behaviours; (2) to improve children’s health and development by helping parents provide more competent care; and (3) to enhance mothers’ personal development by promoting planning of future pregnancies and helping women continue their education and find work. The visitors helped women accomplish these goals by promoting the adaptive behaviours specified above, by helping them improve their relationships with key family members and friends (especially their mothers and boyfriends), and by promoting women’s use of health and human services. Nurse home visitors were required to have a degree and experience in community or maternal and child health nursing, whereas para‐professionals were expected to have a high school education, no college preparation in the helping professions, and strong people skills. Women were randomised into 3 groups: Women in treatment 1 (n = 255) were provided with free developmental screening and referral for their children at 6, 12, 15, 21, and 24 months of age. Women in treatment 2 (n = 245) were provided with the screening offered in treatment 1 plus para‐professional home visiting during pregnancy and the child’s first 2 years of life. Women in treatment 3 (n = 235) were provided with the screening offered in treatment 1 plus nurse home visiting during pregnancy and the child's first 2 years. |
|
| Outcomes | Outcomes consisted of maternal reports of subsequent pregnancies, participation in education and work, use of welfare, marriage, cohabitation, experience of domestic violence, mental health, substance use, and sense of mastery; observations of mother‐child interaction and the home environment; tests of children’s language and executive functioning; and mothers’ reports of children’s externalising behaviour problems. A large number of outcomes were reported in this study where follow‐up continued into late childhood. The paper relating to the follow‐up when the child was four years old collected data relating to child development, subsequent pregnancies, drug and alcohol use and episodes of DV during previous 6 months and since the child was 2 years (i.e. 3.5 years and 2‐4 years postpartum). |
|
| Notes | The data reported in this review were from a paper reporting a follow‐up study of mothers and children in their homes near the child’s fourth birthday, 2 years after the end of the program. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation by computer by external operations office. |
| Allocation concealment (selection bias) | Low risk | External randomisation service. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 735 women randomised and 695 followed up at 4 years. There were missing data for some variables. |
| Selective reporting (reporting bias) | Unclear risk | It was not clear that all outcomes had been prespecified before the onset of the study. The study resulted in multiple publications. |
| Other bias | Unclear risk | Groups appeared comparable at baseline and follow‐up rates were relatively high. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Women and staff were aware of treatment group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was reported that follow‐up data were collected by investigators who were blind to group assignments. |
Sharps 2013.
| Methods | Study described as multi‐stage, longitudinal and randomised. Mixed‐methods trial. An urban sample of women was individually randomised to treatment groups (n = 92); 12 rural county health departments were randomised by site, 6 to treatment and 6 to placebo (cluster‐randomisation, n = 147). | |
| Participants | Participants were English speaking women, 31 weeks’ gestation and higher reporting abuse within the last 12 months, those registered in health department perinatal home visitation programs. | |
| Interventions | The usual care (UC) group received the standard home visitation (HV) and the Domestic Violence Enhanced Home Visitation Program (DOVE) was the intervention.DOVE intervention group received the standard HV in addition to the DOVE IPV intervention. Women in the DOVE intervention group received 3 prenatal and 3 postnatal DOVE sessions in addition to their HV protocols. | |
| Outcomes | Recruitment rate and retention rate. | |
| Notes | None of these outcomes are relevant to our review but future studies may report our primary and secondary outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised. Sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Unclear risk. Allocation concealment not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A total of 339 abused pregnant women were eligible for randomisation; 42 women refused, and 239 women were randomly assigned (124 DOVE; 115 usual care), resulting in a 71% recruitment rate. Retention rates from baseline included 93% at delivery, 80% at 3 months, 76% at 6 months, and 72% at 12 months. |
| Selective reporting (reporting bias) | High risk | No original outcome is reported in this publication. |
| Other bias | Unclear risk | Unknown. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not clear, blinding not mentioned. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not clear, blinding not mentioned. |
Tiwari 2005.
| Methods | RCT. 2‐arm trial with individual randomisation. | |
| Participants | Setting: public hospital in Hong Kong, May 2002–June 2003. Inclusion criteria: 110 women identified as abused by intimate partner. Pregnant women over 18 and less than 30 weeks’ gestation attending for first antenatal visit. Women had “answered ‘yes’ to being physically or emotionally abused by someone or forced to have sexual activities within the last year” (Abuse Assessment Screen). Exclusion criteria: no reported abuse or abused by someone other than their partner. |
|
| Interventions | Experimental intervention: 55 women (51 followed up) Intervention based on empowerment and empathic understanding. The aim of the intervention was to enhance independence and control. In a 30‐minute interview with a midwife researcher women were advised on safety and problem solving (the intervention was tailored for use with Chinese women). Women were also given a brochure (it was not clear whether this intervention was in addition to standard care. Control/Comparison intervention: 55 women (all followed up). Standard care. Women were given written information about community resources to support abused women. |
|
| Outcomes | Conflict Tactics scale (CTS) mean scores (with scores for minor and severe physical violence and psychological and sexual abuse); General Health scores; EPDS; and satisfaction with intervention. Women were followed up by telephone interview at 6 weeks postpartum. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation schedule was generated by a computer. |
| Allocation concealment (selection bias) | Low risk | Allocation was “concealed in consecutively numbered sealed envelopes” by a researcher not involved in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 110 women were randomised (55 in each group). 4 women were lost to follow‐up and it was stated that an intention‐to‐treat analysis was carried out although it was not clear what this meant. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study report. |
| Other bias | Low risk | No other sources of bias identified. There did appear to be differences between groups at baseline but it is not clear whether or to what extent baseline differences influenced results. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Women and care providers would not be blind to randomisation group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was stated that outcome assessment was carried out by researchers unaware of allocation and that women did not reveal their group until the end of the follow‐up interview. |
Zlotnick 2011.
| Methods | RCT. 2 arms with individual randomisation. | |
| Participants | Women attending for prenatal care were recruited from 2 primary care clinics and a private clinic in Rhode Island (USA). Inclusion criteria: 54 pregnant women aged between 18 and 40 years who screened positive for recent (past year) DV on the Revised Conflict Tactics Scale. (Gestational age at recruitment not clear.) Exclusion criteria: women with a current affective disorder, post‐traumatic stress disorder or current substance abuse were excluded and referred for appropriate treatment. |
|
| Interventions | Experimental intervention: (28 women randomised.) an intervention based on principles of interpersonal psychotherapy which aimed to enhance social support as a means of reducing depression, encouraging service use and reducing partner violence. The intervention also included empowerment and stabilisation components. The intervention involved four 60‐minute individual, scripted sessions during pregnancy and a booster session within 2 weeks of the birth; delivered by 2 trained staff. Control/Comparison intervention: (26 women randomised.) usual medical care which included educational material and list of resources for DV. Women in both groups received financial compensation for completing assessments. |
|
| Outcomes | Assessed at baseline, 5‐6 weeks after recruitment, 2 weeks after the birth and 3 months postpartum. Physical, sexual and psychological attacks measured on Revised Conflict Tactic scale (at baseline and then since last assessment). Major depressive disorder (assessed on Longitudinal Interval Follow‐up Examination (LIFE)). Postnatal depression score on EPDS. Post traumatic stress (on Davidson Trauma scale). History of trauma. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated schedule. |
| Allocation concealment (selection bias) | Low risk | Allocations concealed in consecutively numbered, sealed envelopes; allocation was by an investigator blind to baseline assessments. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 54 women were randomised and there were outcome data for 46 (85%). Information on women lost to follow‐up was not provided. It was stated that analyses were by intention‐to‐treat. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study reports. |
| Other bias | Low risk | No other bias is apparent. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding women, staff providing care and staff delivering the intervention to this type of intervention is not feasible. It is not clear how outcome data were collected |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is not clear how outcome data were collected. |
DV: domestic violence EPDS: Edinburgh Postnatal Depression Scale IPV: intimate partner violence RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Armstrong 1999 | The population in this study were not pregnant women.This was a trial examining an intervention in the postnatal period. There was no intervention in pregnancy and women were not recruited until after the birth. The intervention was delivered by child health nurses who offered weekly visits to support mothers and enhance parenting confidence with advice on child development and behaviour and facilitate access to other services. Individually tailored to family circumstances. |
| Bair‐Merritt 2010 | Women recruited to this study were not pregnant. The trial examined early childhood home visits to improve family functioning and reduce child maltreatment. Para‐professionals gave advice on child development and parenting and offered support. The first visit was scheduled within a week of the birth and visits were thereafter scheduled weekly at first then tapering off for up to 3 years (mean of 13 visits in first year). |
| Bhandari 2012 | This study used samples from RCT study of Domestic Violence Enhanced Home Visitation (DOVE) to conduct a qualitative study. Reported depression scores are based on correlation with relationship with mother. This study does not fit with our review objectives. |
| Blackmore 2006 | This study examined whether an antenatal health assessment form identified women with risk factors for postnatal depression (including DV). There was no intervention to prevent or reduce IPV. |
| Bullock 2009 | This study had an DV component but the objective did not meet this review criteria as it was looking into the effect of intervention on smoking cessation and DV reported as a part of secondary outcome. |
| Eddy 2008 | Target populations were not pregnant women. They were facilitators and trainers from various countries (n = 21). |
| Janssen 2003 | This is a descriptive population based study with important findings on the effect of DV on pregnancy outcome. However, it is not a RCT. |
| Janssen 2011 | This was a proposal for a study reported in a trial registration; the planned trial did not take place. |
| Kataoka 2010 | This study did not examine interventions to prevent IPV rather it compared 2 different methods of increasing disclosure about DV. |
| Koziol‐McLain 2010 | Women in this study were not pregnant. Participants included 399 English‐speaking women aged 16 years and older who referred to emergency department, |
| Lipsky 2003 | This cohort study investigates the effect of police report on pregnancy outcome of women suffering DV. |
| Macy 2007 | This was a longitudinal study with no randomisation and blinding. |
| Marcenko 1994 | Intervention involved consultation pertaining to DV prevention but none of the our priori outcome of interest was reported. |
| McFarlane 1996 | This study was not a RCT. |
| Miller 2011 | The participants in this study were women attending family planning clinics; the women were not pregnant. The study was looking at reproductive coercion. |
| Parker 1999 | This was not a RCT. |
| Quinlivan 2003 | Women were recruited to this study during pregnancy but were not randomised until after delivery and the intervention did not start until the postnatal period. The intervention was a postnatal home‐visiting service by nurse‐midwives aimed at “reducing adverse neonatal outcomes and in improving knowledge about contraception, vaccination schedules, and breastfeeding in teenage mothers younger than age 18 years” Structured home visits at 1, and 2 weeks and 1, 2, 4 and 6 months after the birth. Each visit lasted 1‐4 hours. Content of visits included infant feeding advice and support, information on vaccinations and to facilitate attendance for vaccinations, discussion of mood disorders and information on parenting. Follow‐up of any issues (which could include violence) raised at 2 months postpartum, discussion of issues re drugs and alcohol and advice on contraception. |
| Taft 2009a | The women recruited to this study were not all pregnant. The sample included women who were pregnant, who had a child under 5 or who otherwise were at high risk of IPV. Women in the intervention arm received up to 12 months support from trained and supported non‐professional mentor mothers. Women in the intervention arm received up to 12 months support from a trained mentor. (No separate breakdown for pregnant women experiencing DV). |
DV: domestic violence IPV: intimate partner violence RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Loree 2008.
| Methods | RCT. |
| Participants | Participants were adolescent couples; women were pregnant at recruitment. |
| Interventions | A counselling intervention was compared with routine care. |
| Outcomes | Outcomes were episodes of violence within couples. It was not clear whether women or their partners were the victims of the violence; authors report that much of the violence was reciprocal. |
| Notes | We have contacted the authors to see if we can obtain data for women only. paulf@ewm.edu (author contacted 20th June 2012). |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Feder 2013.
| Trial name or title | Enhanced Nurse Home Visitation Program To Prevent Intimate Partner Violence |
| Methods | RCT. |
| Participants | Women during pregnancy and postpartum. 250 women referred to the Multnomah County Health Department will be randomised to the experimental (NFP plus ECI) or control condition (NFP) and visited according to the regular NFP schedule during pregnancy and until the infant is 24 months old. |
| Interventions | Enhanced Nurse Home Visitation Program To Prevent Intimate Partner Violence. It is based on a choice or empowerment model whereby women can choose among interventions related to her goal for her current intimate relationship.The intervention concentrated on the prenatal and immediate (first 6 months) postpartum period with regular IPV, emotional abuse and controlling behaviour assessments throughout the study period. |
| Outcomes | Baseline and outcome measurement (CTS2, WEB, TPMI, depression ‐ Edinburgh, & parenting stress), screened at 3 months before delivery, 9 months and 21 months postpartum. |
| Starting date | January 2007 start date. End date October 2010. |
| Contact information | Principal Investigator: Lynette F Feder, PhD University of Central Florida, lynette.feder@ucf.edu Principal Investigator: Phyllis Niolin, PhD Centers for Disease Control and Prevention |
| Notes | We have been unable to find any additional reports on this trial to confirm that the study has been completed. We emailed the author on 18/8/2014, but we have had no reply. |
Krishnan 2012.
| Trial name or title | The Dil Mil trial |
| Methods | RCT using a parallel comparison. |
| Participants | Young married pregnant women (18 to 30 years old) with a history of domestic violence in the first or second trimester of pregnancy (daughter‐in‐laws (DILs) and their mother‐in‐laws' (MILs). |
| Interventions | Intervention consists of 2 half‐day group sessions with DILs, 5 half‐day group sessions with MILs, and 1 joint half‐day session with DILs and MILs. |
| Outcomes | Domestic violence incidence, related health outcomes (perceived quality of life, psychosocial status, and maternal and infant health), knowledge of links between GBV and health, gender‐equitable attitudes, relationship with DILs (communication social support, support of freedom of movement), reduction in GBV perpetration, resistance to GBV inflicted by son, knowledge of safety and the links between GBV and health, gender‐equitable attitudes, decision‐making skills, freedom of movement, resistance to GBV by husband. |
| Starting date | Starting date unclear. |
| Contact information | Suneeta Krishnan, skrishnan@rti.org. |
| Notes | This study is at recruitment stage. No results were available at the time of review update. |
Sharma 2013.
| Trial name or title | Impact of Women's Empowerment Program for Abused Pregnant Women |
| Methods | RCT with parallel assignment. |
| Participants | Abused pregnant women aged 18 to 35 years of age with a history of suffering from physical abuse. |
| Interventions | Behavioural intervention aiming to empower women. The one‐our intervention, delivered over a 11‐week period, consisted of an empowerment and additional components adapted from freedom program run to support domestic abused women. The control arm received standard care, which was routine check ups with care provided by healthcare professionals. |
| Outcomes | Rate of episode of domestic violence, health status and safety behaviour. |
| Starting date | January 2013. Completion August 2013 with June 2013 final data collection date for primary outcome measure. |
| Contact information | Neha Sharma, PhD, Macmillan research group UK. (No email published on protocol.) |
| Notes | It is unclear whether this trial has been completed. |
Taft 2012.
| Trial name or title | MOVE, a cluster‐randomised trial of screening and referral in primary health care |
| Methods | A cluster‐randomised trial. |
| Participants | Nurses and pregnant mothers. |
| Interventions | IPV screening. |
| Outcomes | 1. For nurses: whether nurses inquire about IPV among their client population, referring women experiencing IPV to services, Inquire about the safety of women and children in the relationship. 2. For pregnant women:whether women are asked about IPV, disclose/discuss any abuse and are satisfied with the quality of care and support they receive. 3. Proportion of MCH clients who have ever, or who are currently, experiencing IPV and those abused when pregnant. |
| Starting date | Start and completion dates unclear. |
| Contact information | Angela J Taft (a.taft@latrobe.edu.au) |
| Notes | This report is a protocol for the MOVE, a cluster‐randomised trial of screening and referral in primary health care. |
Temmerman 2010.
| Trial name or title | Intimate Partner Violence and Pregnancy, a Perinatal Care Intervention Study (MOM) |
| Methods | A single‐blind randomised controlled trial with parallel assignment. |
| Participants | Pregnant victims of partner violence (n = 150) |
| Interventions | Perinatal Care Intervention study that looks into the Impact of a resource card. The intervention group will receive an envelope with a gift voucher and a resource card (wallet size card with on the one side safety measures and on the other side contact details of resources for violence).The control group will receive the same envelope with a gift voucher and a letter of thanks. |
| Outcomes | Evolution of partner violence, help‐seeking behaviour of the pregnant victims of partner violence. |
| Starting date | June 2010. Estimated completion date March 2014. |
| Contact information | An‐Sofie Van Parys, Universiteit Gent, ansofie.vanparys@ugent.be |
| Notes | The contact author was emailed on 21/08/2014; data are not yet available because women are still being interviewed. Data may be available for next update. |
CTS: Conflict Tactics Scale IPV: intimate partner violence RCT: randomised controlled trial
Contributions of authors
Shayesteh Jahanfar wrote the protocol, conducted an additional search, extracted the data, assessed risk of bias, analysed data, wrote the discussion and abstract and edited the results section. Patricia Janssen commented on the protocol and edited the review. Louise Howard commented on the protocol, extracted data, assessed risk of bias and read and edited the review. Therese Dowswell was involved in data extraction, assessing risk of bias, data analysis and drafting text of the review.
For the 2014 update, Shayesteh Jahanfar and Nancy Medley assessed the new papers for eligibility, extracted data and assessed risk of bias. Shayesteh Jahanfar updated the text of the review. Nancy Medley prepared the 'Summary of findings' table. Louise Howard commented on the updated review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research, UK.
NIHR Programme of centrally‐managed pregnancy and childbirth systematic reviews of priority to the NHS and users of the NHS: 10/4001/02
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Louise Howard is funded by a National Institute for Health Research Programme Grant for Applied Research on Improving the Healthcare Response to Domestic Violence and is a member of the WHO Guideline Development Group and the NICE/SCIE Guideline Development Group developing guidelines on the preventing and reducing domestic violence.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Calderon 2008 {published data only}
- Calderon SH, Gilbert P, Jackson R, Kohn MA, Gerbert B. Cueing prenatal providers effects on discussions of intimate partner violence. American Journal of Preventive Medicine 2008;34(2):134‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. The health in pregnancy (HIP) study. http://clinicaltrials.gov/ct2/show/NCT00540319 (accessed 20 February 2008).
- Humphreys J, Tsoh JY, Kohn MA, Gerbert B. Increasing discussions of intimate partner violence in prenatal care using Video Doctor plus Provider Cueing: a randomized, controlled trial. Womens Health Issues 2011;21(2):136‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cripe 2010 {published data only}
- Cripe SM, Sanchez SE, Sanchez E, Ayala Quintanilla B, Hernandez Alarcon C, Gelaye B, et al. Intimate partner violence during pregnancy: a pilot intervention program in Lima, Peru. Journal of Interpersonal Violence 2010;25(11):2054‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Curry 2006 {published data only}
- Curry MA, Durham L, Bullock L, Bloom T, Davis J. Nurse case management for pregnant women experiencing or at risk for abuse. Journal of Obstetric, Gynecologic and Neonatal Nursing 2006;35(2):181‐92. [DOI] [PubMed] [Google Scholar]
Kiely 2010 {published data only}
- El‐Khorazaty MN, Johnson AA, Kiely M, El‐Mohandes AAE, Subramanian S, Laryea HA, et al. Recruitment and retention of low‐income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC: Public Health 2007;7:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Mohandes A, Kiely M, El‐Khorazaty N, Gantz M, Blake S, Subramanian S. Reduction of intimate partner violence in pregnancy: the effect of an integrated intervention in an African‐American low income population [abstract]. Pediatric Academic Societies Annual Meeting; 2005 May 14‐17; Washington DC, USA. 2005:Abstract no: 2402.
- El‐Mohandes AA, Kiely M, Gantz MG, El‐Khorazaty MN. Very preterm birth is reduced in women receiving an integrated behavioral intervention: a randomized controlled trial. Maternal & Child Health Journal 2011;15(1):19‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Mohandes AA, Kiely M, Joseph JG, Subramanian S, Johnson AA, Blake SM, et al. An intervention to improve postpartum outcomes in African‐American mothers: a randomized controlled trial. Obstetrics & Gynecology 2008;112(3):611‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Mohandes AAE, for the NIH‐DC initiative to reduce infant mortality. An integrated psycho‐behavioral intervention during pregnancy has significant effects in reducing risks during the post‐partum period in African‐American women. Pediatric Academic Societies Annual Meeting; 2005 May 14‐17; Washington DC, USA. 2005:Abstract no: 39.
- Joseph JG, El‐Mohandes AA, Kiely M, El‐Khorazaty MN, Gantz MG, Johnson AA, et al. Reducing psychosocial and behavioral pregnancy risk factors: results of a randomized clinical trial among high‐risk pregnant African American women. American Journal of Public Health 2009;99(6):1053‐61. [PUBMED: 19372532] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiely M, El‐Mohandes AA, El‐Khorazaty MN, Gantz MG. An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstetrics & Gynecology 2010;115(2 Pt 1):273‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Katz KS, Rodan M, Gantz MG, El‐Khorazaty NM, Johnson A, et al. An integrated randomized intervention to reduce behavioral and psychosocial risks: pregnancy and neonatal outcomes. Maternal and Child Health Journal 2012;16(3):545‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
McFarlane 2000 {published data only}
- McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nursing 2000;17(6):443‐51. [DOI] [PubMed] [Google Scholar]
Nagle 2002 {published data only}
- Nagle GA. Maternal participation, depression and partner violence in a state run child abuse prevention program: Louisiana nurse home visitation 1999‐2002 [thesis]. Louisiana: Tulane University, 2002. [Google Scholar]
Olds 2004 {published data only}
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow‐up results of a randomized trial. Pediatrics 2004;114(6):1560‐8. [PUBMED: 15574615] [DOI] [PubMed] [Google Scholar]
Sharps 2013 {published data only}
- Sharps P, Alhusen L, Bullock L, Bhandari S, Ghazarian S, Udo E, et al. Engaging and retaining abused women in perinatal home visitation programs. Pediatrics 2013;132:S134‐S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tiwari 2005 {published data only}
- Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOG: an international journal of obstetrics and gynaecology 2005;112(9):1249‐56. [DOI] [PubMed] [Google Scholar]
Zlotnick 2011 {published data only}
- Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low‐income pregnant women with intimate partner violence: a pilot study. Archives of Women's Mental Health 2011;14(1):55‐65. [PUBMED: 21153559] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Armstrong 1999 {published data only}
- Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. Journal of Paediatrics and Child Health 1999;35(3):237‐44. [PUBMED: 10404442] [DOI] [PubMed] [Google Scholar]
Bair‐Merritt 2010 {published data only}
- Bair‐Merritt MH, Jennings JM, Chen R, Burrell L, McFarlane E, Fuddy L, et al. Reducing maternal intimate partner violence after the birth of a child: a randomized controlled trial of the Hawaii healthy start home visitation program. Archives of Pediatrics & Adolescent Medicine 2010;164(1):16‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhandari 2012 {published data only}
- Bhandari S, Bullock LF, Bair‐Merritt M, Rose L, Marcantonio K, Campbell JC, et al. Pregnant women experiencing IPV: Impact of supportive and non‐supportive relationships with their mothers and other supportive adults on perinatal depression: A mixed methods analysis. Issues in Mental Health Nursing 2012;33(12):827‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blackmore 2006 {published data only}
- Blackmore ER, Carroll J, Reid A, Biringer A, Glazier RH, Midmer D, et al. The use of the Antenatal Psychosocial Health Assessment (ALPHA) tool in the detection of psychosocial risk factors for postpartum depression: a randomized controlled trial. Journal of Obstetrics and Gynaecology Canada: JOGC 2006;28(10):873‐8. [DOI] [PubMed] [Google Scholar]
- Carroll JC, Reid AJ, Biringer A, Midmer D, Glazier RH, Wilson L, et al. Effectiveness of the antenatal psychosocial health assessment (ALPHA) form in detecting psychosocial concerns: A randomized controlled trial. Canadian Medical Association Journal 2005;173(3):253‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bullock 2009 {published data only}
- Bullock L, Everett KD, Mullen PD, Geden E, Longo DR, Madsen R. Baby BEEP: A randomized controlled trial of nurses' individualized social support for poor rural pregnant smokers. Maternal and Child Health Journal 2009;13(3):395‐406. [PUBMED: 18496746] [DOI] [PubMed] [Google Scholar]
Eddy 2008 {published data only}
- Eddy T, Kilburn E, Chang C, Bullock L, Sharps P. Facilitators and barriers for implementing home visit interventions to address intimate partner violence: town and gown partnerships. Nursing Clinics of North America 2008;43(3):419‐35, ix. [PUBMED: 18674673] [DOI] [PMC free article] [PubMed] [Google Scholar]
Janssen 2003 {published data only}
- Janssen PA, Holt VL, Sugg NK, Emanuel I, Critchlow CM, Henderson AD. Intimate partner violence and adverse pregnancy outcomes: a population‐based study. American Journal of Obstetrics and Gynecology 2003;188(5):1341‐7. [DOI] [PubMed] [Google Scholar]
Janssen 2011 {published data only}
- Janssen P. Can safety planning improve perinatal outcome among pregnant women exposed to intimate partner violence?. http://clinicaltrials.gov/ct2/show/NCT00831831 (accessed 15 February 2011).
Kataoka 2010 {published data only}
- Kataoka Y, Yaju Y, Eto H, Horiuchi S. Self‐administered questionnaire versus interview as a screening method for intimate partner violence in the prenatal setting in Japan: a randomised controlled trial. BMC Pregnancy and Childbirth 2010;10:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koziol‐McLain 2010 {published data only}
- Koziol‐McLain J, Garrett N, Fanslow J, Hassall I, Dobbs T, Henare‐Toka TA, et al. A randomized controlled trial of a brief emergency department intimate partner violence screening intervention. Annals of Emergency Medicine 2010;56(4):413‐23.e1. [PUBMED: 20538369] [DOI] [PubMed] [Google Scholar]
Lipsky 2003 {published data only}
- Lipsky S, Holt VL, Easterling TR, Critchlow CW. Impact of police‐reported intimate partner violence during pregnancy on birth outcomes. Obstetrics & Gynecology 2003;102(3):557‐64. [DOI] [PubMed] [Google Scholar]
Macy 2007 {published data only}
- Macy RJ, Martin SL, Kupper LL, Casanueva C, Guo S. Partner violence among women before, during, and after pregnancy: multiple opportunities for intervention. Women's Health Issues : official publication of the Jacobs Institute of Women's Health 2007;17(5):290‐9. [PUBMED: 17659882] [DOI] [PubMed] [Google Scholar]
Marcenko 1994 {published data only}
- Marcenko MO, Spence M. Home visitation services for at‐risk pregnant and postpartum women: a randomized trial. American Journal of Orthopsychiatry 1994;64(3):468‐78. [PUBMED: 7977669] [DOI] [PubMed] [Google Scholar]
McFarlane 1996 {published data only}
- McFarlane J, Parker B, Soeken K. Physical abuse, smoking and substance use during pregnancy: prevalence, interrelationships and effects on birth weight. Journal of Obstetric, Gynecologic and Neonatal Nursing 1996;25:313‐20. [DOI] [PubMed] [Google Scholar]
Miller 2011 {published data only}
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception 2011;83(3):274‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 1999 {published data only}
- Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Research in Nursing & Health 1999;22(1):59‐66. [PUBMED: 9928964] [DOI] [PubMed] [Google Scholar]
Quinlivan 2003 {published data only}
- Quinlivan JA, Box H, Evans SF. Postnatal home visits in teenage mothers: a randomised controlled trial. Lancet 2003;361(9361):893‐900. [PUBMED: 12648967] [DOI] [PubMed] [Google Scholar]
Taft 2009a {published data only}
- Taft A, Small R, Hegarty K, Lumley J, Watson L. Mosaic: the development phase of a randomised community intervention trial to reduce intimate partner abuse and depression in women pregnant or with children under five. [abstract]. Perinatal Society of Australia and New Zealand 7th Annual Congress; 2003 March 9‐12; Tasmania, Australia. 2003:A30.
- Taft AJ, Small R, Hegarty KL, Lumley J, Watson LF, Gold L. MOSAIC (MOthers' Advocates In the Community): protocol and sample description of a cluster randomised trial of mentor mother support to reduce intimate partner violence among pregnant or recent mothers. BMC Public Health 2009;9:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft AJ, Small R, Hegarty KL, Watson LF, Gold L, Lumley JA. Mothers' AdvocateS In the Community (MOSAIC)‐‐non‐professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. BMC Public Health 2011;11:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Loree 2008 {published data only}
- Loree A, Ondersma SJ, Beatty JR, Tzilos G, Chase SK, Schuster CR. Brief, universal intervention for child maltreatment prevention among high‐risk parents: effects on substance use, mental health, and intimate partner violence. Proceedings of the 70th Annual Scientific Meeting of the College on Problems of Drug Dependence; 2008 June 14‐19; San Juan, Puerto Rico, USA. 2008:11.
References to ongoing studies
Feder 2013 {published data only}
- Feder L. Enhanced nurse home visitation to prevent intimate partner violence. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed July 2014). NCT01811719 2013.
Krishnan 2012 {published data only}
- Krishnan S, Subbiah K, Chandra P, Srinivasan K. Minimizing risks and monitoring safety of an antenatal care intervention to mitigate domestic violence among young Indian women: The Dil Mil trial. BMC Public Health 2012;12:943. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharma 2013 {published data only}
- Sharma N. Impact of women's empowerment program for abused pregnant women: A randomized controlled trial. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 5 February 2014). NCT01933555 2013.
Taft 2012 {published data only}
- Taft AJ, Small R, Humphreys C, Hegarty K, Walter R, Adams C, et al. Enhanced maternal and child health nurse care for women experiencing intimate partner/family violence: protocol for MOVE, a cluster randomised trial of screening and referral in primary health care. BMC Public Health 2012;12(1):811. [DOI] [PMC free article] [PubMed] [Google Scholar]
Temmerman 2010 {published data only}
- Temmerman M. Intimate partner violence and pregnancy, a perinatal care intervention study (MOM). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed July 2014). NCT01158690 2010.
Additional references
Arias 2002
- Arias I, Dankwort J, Douglas U, Dutton MA, Stein K. Violence against women: the state of batterer prevention programs. Journal of Law, Medicine & Ethics 2002;30(3 Suppl):157‐65. [PUBMED: 12508520] [PubMed] [Google Scholar]
Babu 2009
- Babu BV, Kar SK. Domestic violence against women in eastern India: a population‐based study on prevalence and related issues. BMC Public Health 2009;9:129. [PUBMED: 19426515] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bacchus 2004
- Bacchus L, Mezey G, Bewley S, Haworth A. Prevalence of domestic violence when midwives routinely enquire in pregnancy. BJOG: an international journal of obstetrics and gynaecology 2004;111(5):441‐5. [DOI] [PubMed] [Google Scholar]
Ballard 1998
- Ballard TJ, Saltzman LE, Gazmararian JA, Spitz AM, Lazorick S, Marks JS. Violence during pregnancy: measurement issues. American Journal of Public Health 1998;88(2):274‐6. [PUBMED: 9491021] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beydoun 2010
- Beydoun HA, Al‐Sahab B, Beydoun MA, Tamim H. Intimate partner violence as a risk factor for postpartum depression among Canadian women in the Maternity Experience Survey. Annals of Epidemiology 2010;20(8):575‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohn 1996
- Bohn D, Holz K. Sequel of abuse. Journal of Nursing and Midwifery 1996;41(6):442‐56. [DOI] [PubMed] [Google Scholar]
Browne 1997
- Browne A. When Battered Women Kill. 2nd Edition. Australia: Collier MacMillan Publication, 1997:232. [Google Scholar]
Campbell 1992
- Campbell J, Poland M, Waller J, Ager J. Correlates of battering during pregnancy. Research in Nursing & Health 1992;15:219‐26. [DOI] [PubMed] [Google Scholar]
Canadian Centre for Justice Statistics 2000
- Canadian Centre for Justice Statistics. Family violence in Canada: a statistical profile. Cat no 85‐224‐XIE. Ottawa: Statistics Canada, 2000. [Google Scholar]
Canterino 1999
- Canterino JC, VanHorn LG, Harrigan JT, Ananth CV, Vintzileos AM. Domestic abuse in pregnancy: a comparison of a self‐completed domestic abuse questionnaire with a directed interview. American Journal of Obstetrics and Gynecology 1999;181(5 Pt 1):1049‐51. [DOI] [PubMed] [Google Scholar]
Chamberlain 2000
- Chamberlain L, Perham‐Hester KA. Physicians' screening practices for female partner abuse during prenatal visits. Maternal and Child Health Journal 2000;4(2):141‐8. [DOI] [PubMed] [Google Scholar]
Coker 2012
- Coker AL, Garcia LS, Williams CM, Crawford TN, Clear ER, McFarlane J, et al. Universal psychosocial screening and adverse pregnancy outcomes in an academic obstetric clinic. Obstetrics and Gynecology 2012;119(6):1180‐9. [PUBMED: 22617583] [DOI] [PubMed] [Google Scholar]
Daoud 2012
- Daoud N, Urquia ML, O'Campo P, Heaman M, Janssen PA, Smylie J, et al. Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. American Journal of Public Health 2012;102(10):1893‐901. [PUBMED: 22897526] [DOI] [PMC free article] [PubMed] [Google Scholar]
Diaz‐Olavarrieta 2002
- Diaz‐Olavarrieta C, Ellertson C, Paz F, Leon SP, Alarcon‐Segovia D. Prevalence of battering among 1780 outpatients at an internal medicine institution in Mexico. Social Science & Medicine 2002;55(9):1589‐602. [DOI] [PubMed] [Google Scholar]
Dugan 2003
- Dugan L, Nagin DS, Rosenfeld R. Do domestic violence services save lives?. National Institute of Justice Journal 2003;250:20‐5. [Google Scholar]
El Kady 2005
- Kady D, Gilbert WM, Xing G, Smith LH. Maternal and neonatal outcomes of assaults during pregnancy. Obstetrics & Gynecology 2005;105(2):357‐63. [DOI] [PubMed] [Google Scholar]
El‐Mohandes 2008
- El‐Mohandes AA, Kiely M, Joseph JG, Subramanian S, Johnson AA, Blake SM, et al. An intervention to improve postpartum outcomes in African‐American mothers: a randomized controlled trial. Obstetrics and Gynecology 2008;112(3):611‐20. [PUBMED: 18757660] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ezechi 2004
- Ezechi OC, Kalu BK, Ezechi LO, Nwokoro CA, Ndububa VI, Okeke GC. Prevalence and pattern of domestic violence against pregnant Nigerian women. Journal of Obstetrics and Gynaecology 2004;24(6):652‐6. [DOI] [PubMed] [Google Scholar]
Family Violence Prevention Fund 1999
- Family Violence Prevention Fund. Preventing Domestic Violence: Clinical Guidelines on Routine Screening. US Department of Health and Human Services, 1999. [Google Scholar]
Feder 2009
- Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al. How far does screening women for domestic (partner) violence in different health‐care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria. Health Technology Assessment 2009;13(16):iii‐iv, xi‐xiii, 1‐113, 137‐347. [DOI] [PubMed] [Google Scholar]
Feldhaus 1997
- Feldhaus KM, Koziol‐McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA 1997;277(17):1357‐61. [PubMed] [Google Scholar]
Flach 2011
- Flach C, Leese M, Heron J, Evans J, Feder G, Sharp D, et al. Antental domestic violence, maternal mental health and subsequent child behaviour: a cohort study. BJOG: an international journal of obstetrics and gynaecology 2011;118(11):1383‐91. [DOI] [PubMed] [Google Scholar]
Ford‐Gilboe 2011
- Ford‐Gilboe M, Merritt‐Gray M, Varcoe C, Wuest J. A theory‐based primary health care intervention for women who have left abusive partners. ANS. Advances in Nursing Science 2011;34(3):198‐214. [PUBMED: 21654310] [DOI] [PubMed] [Google Scholar]
Gazmararian 1996
- Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. JAMA 1996;275(24):1915‐20. [PubMed] [Google Scholar]
Gazmararian 2000
- Gazmararian JA, Petersen R, Spitz AM, Goodwin MM, Saltzman LE, Marks JS. Violence and reproductive health: current knowledge and future research directions. Maternal and Child Health Journal 2000;4(2):79‐84. [PUBMED: 10994575] [DOI] [PubMed] [Google Scholar]
Goodwin 1990
- Goodwin T, Breen M. Pregnancy outcome and fetomaternal hemorrhage after noncatastrophic trauma. American Journal of Obstetrics and Gynecology 1990;162:665‐71. [DOI] [PubMed] [Google Scholar]
GRADE 2008
- GRADEpro [Computer program]. Jan Brozek, Andrew Oxman, Holger Schünemann. Version 3.6 for Windows 2008.
Harwin 2006
- Harwin N. Putting a stop to domestic violence in the United Kingdom: challenges and opportunities. Violence Against Women 2006;12(6):556‐67. [DOI] [PubMed] [Google Scholar]
Hedin 1999
- Hedin LW, Grimstad H, Moller A, Schei B, Janson PO. Prevalence of physical and sexual abuse before and during pregnancy among Swedish couples. Acta Obstetricia et Gynecologica Scandinavica 1999;78(4):310‐5. [PubMed] [Google Scholar]
Hedin 2000
- Hedin LW, Janson PO. Domestic violence during pregnancy. The prevalence of physical injuries, substance use, abortions and miscarriages. Acta Obstetricia et Gynecologica Scandinavica 2000;79(8):625‐30. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Horiuchi 2009
- Horiuchi S, Yaju Y, Kataoka Y, Grace Eto H, Matsumoto N. Development of an evidence‐based domestic violence guideline: supporting perinatal women‐centred care in Japan. Midwifery 2009;25(1):72‐8. [PUBMED: 17399864] [DOI] [PubMed] [Google Scholar]
Howard 2010
- Howard LM, Trevillion K, Agnew‐Davies R. Domestic violence and mental health. International Review of Psychiatry 2010;22(5):525‐34. [DOI] [PubMed] [Google Scholar]
Jahanfar 2007
- Jahanfar S, Kamarudin EB, Sarpin MA, Zakaria NB, Abdul Rahman RB, Samsuddin RD. The prevalence of domestic violence against pregnant women in Perak, Malaysia. Archives of Iranian Medicine 2007;10(3):376‐8. [PUBMED: 17604477] [PubMed] [Google Scholar]
Janssen 2006
- Janssen P, Dascal‐Weichhendler H, McGregor M. Assessment for intimate partner violence: where do we stand?. Journal of the American Board of Family Medicine: JABFM 2006;19(4):413‐5. [PUBMED: 16809657] [DOI] [PubMed] [Google Scholar]
Jejeebhoy 1998
- Jejeebhoy SJ. Associations between wife‐beating and fetal and infant death: impressions from a survey in rural India. Studies in Family Planning 1998;29(3):300‐8. [PubMed] [Google Scholar]
Jewkes 2001
- Jewkes R, Penn‐Kekana L, Levin J, Ratsaka M, Schrieber M. Prevalence of emotional, physical and sexual abuse of women in three South African provinces. South African Medical Journal 2001;91(5):421‐8. [PubMed] [Google Scholar]
Kramer 2004
- Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Women's Health Issues 2004;14(1):19‐29. [PUBMED: 15001185] [DOI] [PubMed] [Google Scholar]
Lewis 2007
- Lewis G, editor. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2003–2005. London: CEMACH, 2007. [Google Scholar]
Lewis 2011
- Lewis G, editor. The Eighth Report of the Confidential Enquiries into Maternal Deaths 'Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2006‐2008. London: National Patient Safety Agency, Scottish Programme for Clinical Effectiveness in Reproductive Health, Department of Health, Social Services and Public Safety of Northern Ireland and the States of Jersey and Guernsey, and Isle of Man, 2011. [Google Scholar]
McCloskey 2006
- McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women's receipt of interventions and improved health. Public Health Reports (Washington, D.C.: 1974) 2006;121(4):435‐44. [PUBMED: 16827445] [DOI] [PMC free article] [PubMed] [Google Scholar]
McFarlane 2006
- McFarlane JM, Groff JY, O'Brien JA, Watson K. Secondary prevention of intimate partner violence: a randomized controlled trial. Nursing Research 2006;55(1):52‐61. [PUBMED: 16439929] [DOI] [PubMed] [Google Scholar]
Mezey 2000
- Mezey G, Bewley S, Bacchus L, Haworth A. Prevalence of domestic violence during pregnancy in a UK population: impact on maternal health and obstetric outcome: research briefing. Royal College of Obstetricians and Gynaecologists London 2000.
Nagassar 2010
- Nagassar RP, Rawlins JM, Sampson NR, Zackerali J, Chankadyal K, Ramasir C, et al. The prevalence of domestic violence within different socio‐economic classes in Central Trinidad. West Indian Medical Journal 2010;59(1):20‐5. [PUBMED: 20931908] [PubMed] [Google Scholar]
Nelson 2012
- Nelson HD, Bougatsos C, Blazina I. Screening Women for Intimate Partner Violence and Elderly and Vulnerable Adults for Abuse. Systematic Review to Update the 2004 U.S. Preventive Services Task Force Recommendation. Evidence Syntheses, No. 92. Rockville (MD): Agency for Healthcare Research and Quality (US), 2012. [PUBMED: 22675737] [PubMed] [Google Scholar]
Newberger 1992
- Newberger E, Barkan S, Lieberman E. Abuse of pregnant women and adverse birth outcome. JAMA 1992;267:2370‐2. [PubMed] [Google Scholar]
Ng 2005
- Ng C, Peterson T. The Ninth Malaysia Plan: gender, rights and development. Universiti Malaya and UN Malaysia Conference on Progress and Challenges in Human Development in Malaysia: Ideas for the Ninth Malaysia Plan; 2005 July 11‐12; Kuala Lumpur, Malaysia. 2005:Abstract no: 1290.
O'Campo 2011
- O'Campo P, Kirst M, Tsamis C, Chambers C, Ahmad F. Implementing successful intimate partner violence screening programs in health care settings: evidence generated from a realist‐informed systematic review. Social Science & Medicine 2011;72(6):855‐66. [PUBMED: 21330026] [DOI] [PubMed] [Google Scholar]
O'Reilly 2010
- O'Reilly R, Beale B, Gillies D. Screening and intervention for domestic violence during pregnancy care: a systematic review. Trauma, Violence & Abuse 2010;11(4):190‐201. [PUBMED: 20688785] [DOI] [PubMed] [Google Scholar]
Parker 1994
- Parker B, McFarlane J, Soeken K. Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstetrics & Gynecology 1994;84:323‐8. [PubMed] [Google Scholar]
Parker 2002
- Parker B, Chouaf K. Intimate partner violence following pregnancy. Archives of Pediatrics & Adolescent Medicine 2002;156(4):313‐4. [DOI] [PubMed] [Google Scholar]
Parsons 2000
- Parsons L, Goodwin MM, Petersen R. Violence against women and reproductive health: toward defining a role for reproductive health care services. Maternal and Child Health Journal 2000;4(2):135‐40. [DOI] [PubMed] [Google Scholar]
Petersen 1997
- Petersen R, Gazmararian J, Spitz A. Violence and adverse pregnancy outcomes. American Journal of Violence 1997;13(5):366‐73. [PubMed] [Google Scholar]
Ramsay 2002
- Ramsay J, Richardson J, Carter YH, Davidson LL, Feder G. Should health professionals screen women for domestic violence? Systematic review. BMJ (Clinical research ed.) 2002;325(7359):314. [PUBMED: 12169509] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramsay 2009
- Ramsay J, Carter Y, Davidson L, Dunne D, Eldridge S, Hegarty K, et al. Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well‐being of women who experience intimate partner abuse. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD005043.pub2] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodriguez 2001
- Rodriguez E, Lasch KE, Chandra P, Lee J. The relation of family violence, employment status, welfare benefits, and alcohol drinking in the United States. Western Journal of Medicine 2001;174(5):317‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rose 2010
- Rose L, Alhusen J, Bhandari S, Soeken K, Marcantonio K, Bullock L, et al. Impact of intimate partner violence on pregnant women's mental health: mental distress and mental strength. Issues in Mental Health Nursing 2010;31(2):103‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saltzman 2003
- Saltzman LE, Johnson CH, Gilbert BC, Goodwin MM. Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Maternal and Child Health Journal 2003;7(1):31‐43. [DOI] [PubMed] [Google Scholar]
Schunemann 2009
- Schunemann HJ. GRADE: from grading the evidence to developing recommendations. A description of the system and a proposal regarding the transferability of the results of clinical research to clinical practice [GRADE: Von der Evidenz zur Empfehlung. Beschreibung des Systems und Losungsbeitrag zur Ubertragbarkeit von Studienergebnissen]. Zeitschrift fur Evidenz, Fortbildung und Qualitat im Gesundheitswesen 2009;103(6):391‐400. [PUBMED: 19839216] [DOI] [PubMed] [Google Scholar]
Shah 2010
- Shah PS, Shah J. Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta‐analyses. Journal of Women's Health 2010;19(11):2017‐31. [PUBMED: 20919921] [DOI] [PubMed] [Google Scholar]
Sharps 2008
- Sharps PW, Campbell J, Baty ML, Walker KS, Bair‐Merritt MH. Current evidence on perinatal home visiting and intimate partner violence. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2008;37(4):480‐90; quiz 490‐1. [PUBMED: 18754987] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spangaro 2010
- Spangaro JM, Zwi AB, Poulos RG, Man WY. Who tells and what happens: disclosure and health service responses to screening for intimate partner violence. Health & Social Care in the Community 2010;18(6):671‐80. [PUBMED: 20637041] [DOI] [PubMed] [Google Scholar]
Stark 1999
- Stark E, Flitcraft A. Frazier W. Medicine and patriarchal violence: the social construction of a "private" event. International Journal of Health Services 1999;9:461‐93. [DOI] [PubMed] [Google Scholar]
Taft 2009b
- Taft AJ, Small R, Hegarty KL, Lumley J, Watson LF, Gold L. MOSAIC (MOthers' Advocates In the Community): protocol and sample description of a cluster randomised trial of mentor mother support to reduce intimate partner violence among pregnant or recent mothers. BMC Public Health 2009;9:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valladares 2005
- Valladares E, Pena R, Persson LA, Hogberg U. Violence against pregnant women: prevalence and characteristics. A population‐based study in Nicaragua. BJOG: an international journal of obstetrics and gynaecology 2005;112(9):1243‐8. [DOI] [PubMed] [Google Scholar]
Van Parys 2014
- Parys AS, Verhamme A, Temmerman M, Verstraelen H. Intimate partner violence and pregnancy: a systematic review of interventions. PloS One 2014;9(1):e85084. [PUBMED: 24482679] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wathen 2003
- Wathen CN, MacMillan HL. Interventions for violence against women: scientific review. JAMA 2003;289(5):589‐600. [DOI] [PubMed] [Google Scholar]
Wiist 1999
- Wiist WH, McFarlane J. The effectiveness of an abuse assessment protocol in public health prenatal clinics. American Journal of Public Health 1999;89(8):1217‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
World Health Organization 2000
- World Health Organization. National Report on Violence and Health, Malaysia. WHO, Center for Health Development, Kobe, Japan report (WHO/WKC/Tech.Se./05.2). Geneva: WHO, 2000. [Google Scholar]
References to other published versions of this review
Jahanfar 2011
- Jahanfar S, Janssen PA, Howard L. Interventions for preventing or reducing domestic violence against pregnant women. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD009414] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jahanfar 2013
- Jahanfar S, Janssen PA, Howard LM, Dowswell T. Interventions for preventing or reducing domestic violence against pregnant women. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD009414.pub2] [DOI] [PubMed] [Google Scholar]


