Abstract
The goal of this study was to assess the effect of college attendance on tobacco use among young adults and across subpopulations with disparities in tobacco use. Using a cohort of US youth (<18 years) who aged into young adulthood (18-24 years) in the Population Assessment of Tobacco and Health (2013-14, 2015-16, n=3619) and propensity score matching we estimated the effect of college attendance on past 30-day use of cigarettes, e-cigarettes, cigarillos, hookah and smokeless. In unmatched analysis, college attenders (vs. nonattenders) had lower risk of using any form of tobacco (RD: −10.0; 95% CI: −13.2, −7.0), cigarettes (RD: −13.0; 95% CI: −15.4, −10.5), e-cigarettes (RD: −4.1; 95% CI: −6.8, −1.7), cigarillos (RD: −5.7; 95% CI: −7.6, −3.8), and smokeless tobacco (RD: −2.0; 95% CI: −3.4, −0.6), but not hookah (RD: −0.2; 95% CI: −2.1, 1.6). In matched analysis, these associations were all near-null, with the exception of cigarettes (matched RD: −7.1; 95% CI: −10.3, −3.9). The effect of college attendance was stable for all subpopulations we assessed including among those identifying as non-Hispanic Black or Lesbian, Gay or Bisexual as well as among those living in the South, Midwest or whose parents did not attend college. The results suggest that college attendance may reduce young adults’ risk of cigarette smoking but may not reduce the risk of using other tobacco products.
Introduction
Since as early as the 1964 Surgeon General’s report,1 researchers have shown large differences in cigarette smoking across levels of education. In the United States (US), for example, the annual decline in smoking prevalence between 1974 and 1985 in the National Health Interview Survey was approximately five times higher among the most educated than among the least.2 Across the life course, differences in tobacco use by educational attainment diverge most pronouncedly in the transition to young adulthood, where adults who do not attend college are more than twice as likely to smoke and typically smoke at higher consumption-levels than their college attending counterparts.3-6 Moreover, the epidemiology of progression to regular smoking suggests that the typical college-aged period (18-24 years) represents a critical time when many individuals initiate smoking and experimenters transition to heavier patterns of use.7-9
Several studies have suggested that the effect of educational attainment on cigarette smoking could be causal.10-12 While causality is best established with experimental data,13 the impossibility of designing an experiment in the education setting necessitates the emulation of an experiment using observational data. A primary concern of observational studies of educational attainment and tobacco use are variables that are associated with both educational attainment and tobacco use, known as “confounding” variables. For instance, many known risk factors for tobacco use, such as poor academic performance,14 are also risk factors for not attending college and may also lead to disparities in use across socioeconomic groups. Past studies have exploited variables exogenous to the choice to attend college, such as twin or sibling pairing,10,11 to create matched comparisons that are assumed to be comparable, thus controlling for confounding with their study design. Confounding can also be addressed through analysis, when suspected confounders are observed and measured.15,16 The use of propensity score matching (PSM) allows for the control of identified and measured confounders while also checking if balance has been achieved across confounders. PSM mimics the balance achieved in randomized experiments by constructing groups that are similar with respect to measured confounders and thus improves the ability to make a balanced comparison of the effect of college attendance on the risk of tobacco use.17,18
As past studies of educational effects have focused on cigarette use, it is unclear whether the effects of college attendance extends to products like e-cigarettes and hookah, which are now used more frequently by US youth.19-21 In this manuscript, we use the nationally representative Population Assessment of Tobacco Health (PATH) Study to first assess whether college nonattenders are at higher risk for using cigarettes, e-cigarettes, cigarillos, hookah and smokeless tobacco in general. Second, we exploit the longitudinal cohort design of the PATH Study along with PSM to make estimates of the effect of college attendance on the risk for using each tobacco product. Third, because educational differences in part explain other disparities in smoking prevalence, such as racial/ethnic differences,22 we assess whether the effect of college attendance differed across various priority populations, including among young adults who are non-Hispanic Black (henceforth Black), identified as Lesbian, Gay or Bisexual (LGB), lived in the South or Midwest, and who had parents who did not attend college. Finally, we explored differences in the social-ecological environment of college attenders and nonattenders (e.g., time spent around smokers, perceived social norms of smoking, and exposure to tobacco advertising) as potential mechanisms for a “college effect”.23
Methods
Analytical Sample
Analyses were based on a cohort of Wave 1 youth (<18 years) who aged into young adulthood (18-24 years) by Wave 3 of the Population Assessment of Tobacco and Health (n=3619). The PATH study is an ongoing, nationally-representative, longitudinal cohort study of adults and youth in the US.24 Wave 1 interviews were conducted from September 12, 2013 to December 14, 2014 with a response rate of 78.4% to the youth interview and Wave 3 follow-up surveys were October 12, 2015 to December 14, 2016 with a follow-up response rate that was also 78.4% for the adult interview among Wave 1 survey completers. The PATH Study was conducted by Westat and approved by Westat’s institutional review board. Further design details are published.24
Measures
Outcome Variables
Tobacco use:
Participants were asked a series of questions about the types of tobacco products they used. Details of questions and responses are presented in Kasza et al.25 For our analyses, at Wave 3 we assessed past-30-day use of cigars, cigarettes, cigarillos, e-cigarettes, hookah, smokeless tobacco (excluding snus), and “any” tobacco products (i.e., any of the nine assessed in PATH) as the primary outcome variables. We also adjusted for Wave 1 past-30-day use of any tobacco products.
Exposure Variable
College Attendance:
So as to characterize differences in smoking between those who made any decision to attend college or not, we categorized “college attenders” as those who at Wave 3 were currently enrolled in a 2-year, 4-year or advanced degree program, had attended college but dropped out, or who had already received an associates, bachelors or advanced degree.12 “Nonattenders” were thus those who at Wave 3 were not currently enrolled a 2-or-4-year degree program and had never previously attended college.
Matching and Sub-Analysis Variables
Socio-demographic variables:
Questions assessing sex and race/ethnicity were administered at Wave 1 and Wave 1 Census Region was coded by Westat using the address for sampling. Missing data on age, sex, race, and Hispanic ethnicity were logically assigned from other survey data as described in the PATH Study User Guide.26 At Wave 1, respondents’ parents reported whether their own level of educational attainment, which we categorized to college attender vs. nonattender, and at Wave 3 respondents reported their sexual orientation, which we categorized to LGB vs. Straight.
Household to tobacco use:
At Wave 1, respondents were asked: “Does anyone who lives with you now use any of the following: [list of tobacco products],” which we categorized for any use vs. no use.
Use of other drugs or alcohol:
At Wave 1, ever use was ascertained for alcohol, marijuana, as well as for misuse of prescription drugs (i.e., Ritalin/ Adderall, painkillers, sedatives, tranquilizers), cocaine or crack, methamphetamine or speed, heroin, inhalants, solvents, and hallucinogens by a series of questions: “Have you ever used [substance]?” Substances were categories as “alcohol,” “marijuana,” or “any drugs, excluding marijuana.” Those who reported ever use were classified as “any use;” all others were classified as “no use.”
Psychosocial variables:
At Wave 1, mental health and substance use problems were assessed using scales from the Global Appraisal of Individual Needs–Short Screener.27 The internalizing subscale (Cronbach’s α = .81) included 4 items of depressive and anxiety symptoms. The externalizing subscale (Cronbach’s α = .72) included experience with 5 conduct and behavioral items. Adolescents were scored on how many items they had experienced in the past month or past 2 to 12 months.28,29 At Wave 1, sensations seeking (Cronbach’s α = .75) was assessed by 3 items modified from the Brief Sensation Seeking Scale.30 At Wave 1, high school scholastic performance was categorized in two levels (mostly B’s or greater vs. less than mostly B’s).
Self-reported Physical Health:
At Wave 1, respondents recorded their perceived physical health by responding to the question: “in general, would you say your overall health is….” with the response options “Excellent,” “Very Good,” “Good,” “Fair,” “Poor.”
Exploratory Measures of Social-Ecological Environment
Perceived social norms:
At Wave 3, respondents recorded the perceptions of norms regarding cigarette smoking in general, “In general, do you think most people disapprove of smoking cigarettes?” (“Definitely yes/Probably yes” vs. “Probably not/Definitely not”) and among people important to them, “Thinking about the people who are important to you, how would you describe their views on…. Smoking cigarettes” (“Very Negative/Negative” vs “Neither positive nor negative/Positive/ Very Positive”)
Time around smokers:
At Wave 3, respondents were asked, “during the past seven days, about how many hours were you around others who were smoking [whether or not you were smoking yourself]? Include time in your home, in a car, at work, or outdoors.” Responses were recorded in hours.
Friends who smoke:
At Wave 3, respondents were also asked whether people who they considered important to them used cigarettes (“Yes” vs. “No”).
Exposure to tobacco ads:
At Wave 3, respondents recorded exposure to different types of tobacco advertising using the question, “In the past 30 days, have you noticed cigarettes or other tobacco products (not including e-cigarettes or electronic nicotine products) being advertised in any of the following places? Choose all that apply.” Responses included “At gas stations, convenience stores,” “On billboards,” “In newspapers or magazines,” “On radio,” “On television,” “At events like fairs, festivals, or sporting events,” “At nightclubs, bars, or music concerts,” “On websites or social media sites,” “Somewhere else (SPECIFY).” We categorized responses as seeing “Any” vs. “No” advertising.
Managing missing data
Missing data were observed on several of the variables (Supplementary Table 1). These missing data were imputed using the Amelia II algorithm in R with 5 imputed datasets, and by assuming a missing at random pattern.31 Imputation diagnostics suggested the Amelia II algorithm provided imputed values that accurately predicted the observed values for the ordinal variables in our dataset and the majority of the continuous values (Supplementary Figure 1).
Statistical analysis
To calculate prevalence estimates and their corresponding 95% CIs, we used the single-wave population and replicate weights for Wave 3, created by Westat using the Balanced Repeated Replication method with Fay’s adjustment (ρ=0.3) that when combined with the use of a probability sample allowed for computed estimates that were representative of the non-institutionalized, civilian US population of young adults.24,26
To calculate propensity scores, we first obtained imputed data sets, then estimated propensity scores, and finally averaged the propensity score for each individual across the imputed data sets.32 Separate logistic models were fitted for each of the imputed data sets, with college attendance set as the dependent variable and potential confounders entered as covariates in the regression model. We estimated each respondent’s propensity to attend college and averaged the final resulting propensity score for each individual across imputations. Using the resulting propensity scores, each college attender was matched to the closest nonattender(s) using the nearest-neighbor method with optimizations assessed for choice of matching ratios and caliper and by matching without replacement.33 Standardized mean differences of each covariate (before and after matching) were used to judge whether the matching improved balance across all imputed data sets. We chose the ratio and caliper that provided the lowest average imbalance across all imputed data sets and assured covariates had standardized mean differences that were <∣0.1∣, which in all cases was a 1:1 matching ratio with 0.1 caliper (Supplementary Tables 3-8). The final sample size for the resulting matched sample was n=2480. To explore whether the effect of college attendance on the risk of tobacco use was stable across subpopulations, we also performed the same methods just outlined separately in subsamples for each subpopulation of interest, resulting in additional matched subsamples.34 The subpopulations we focused on included young adults who identified as Black (matched sample n=350), LGB (matched sample n=240), who lived in the South (matched sample n=920) or Midwest (matched sample n=546), and whose parents did not attend college (matched sample n=1850), as there are known disparities in tobacco use among these subpopulations and there was sufficient sample size to make comparisons within these subpopulation.22,35 In a sensitivity analysis, we also assessed whether excluding those who had finished or dropped out of college affected the primary results of tobacco use (matched sample n=2200). After matched samples were obtained, we estimated the differences in the risk of using various forms of tobacco in young adulthood between college attenders and nonattenders in both the matched and unmatched datasets. Finally, we also explored potential mechanisms for the “college effect” by exploring differences in the socio-ecological environment between college attenders and nonattenders using logistic and linear regression in the full dataset.
Risk differences (RDs) were calculated using logistic regression, mean differences (MDs) using linear regression and their corresponding 95% CIs using 1,000 draws from the multivariate normal distribution with the mean vector equal to the model coefficients and the variance equal to the coefficient covariance matrix.36 All analyses were performed using R, version 3.5.2 (R Foundation for Statistical Computing).
Results
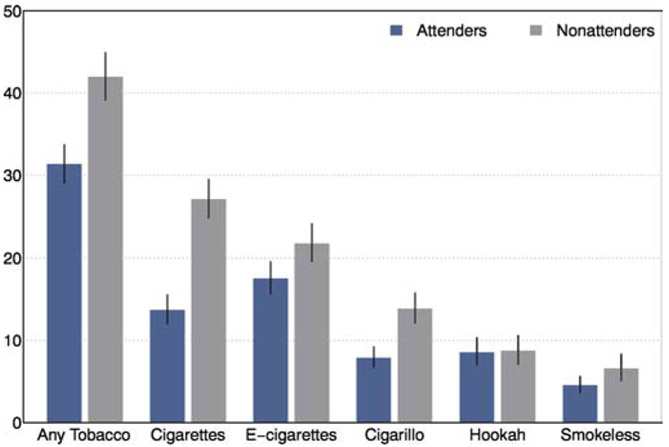
A total of 31.4% (95% CI: 29.0, 33.7) of the young adults who attended college used at least one form of tobacco at Wave 3 compared to 42.0% (95% CI: 39.1, 44.9) among those who did not attend. Among young adults who did not attend college, cigarettes (27.1%; 95% CI: 24.8, 29.5) were the most commonly used tobacco product (Figure 1), followed by e-cigarettes (21.8%; 95% CI: 19.6, 24.1), cigarillos (13.9%; 95% CI: 12.1, 15.8), hookah (8.7%; 95% CI: 7.0, 10.6), and smokeless tobacco (6.6%; 95% CI: 5.1, 8.4). Among young adults who attended college, e-cigarettes (17.5%; 95% CI: 15.6, 19.5) were the most commonly used tobacco product, followed by cigarettes (13.6%; 95% CI: 12.0, 15.5), hookah (8.5%; 95% CI: 7.0, 10.3), cigarillos (7.9%; 95% CI: 6.7, 9.2), and smokeless tobacco (4.5%; 95% CI: 3.6, 5.6).
Figure 1. Prevalence of tobacco product use at Wave 3 by college attendance among the cohort of youth (<18 years) who aged into early adulthood (18-24 years) between Waves 1 and 3 of the PATH Study, United States, 2013-14, 2015-16.
Notes: The bars indicate the prevalence of tobacco use among college attenders (blue) and nonattenders (grey) with their corresponding 95% CIs.
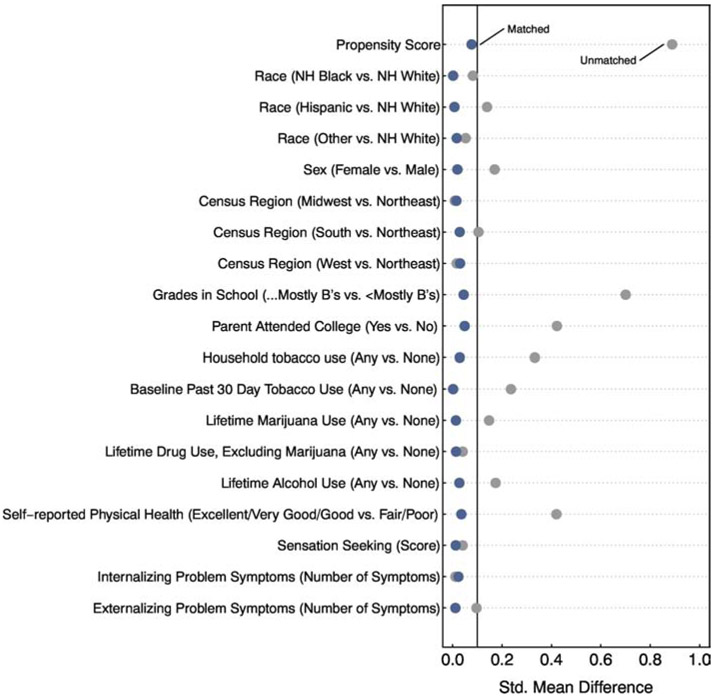
The balance assessment step of our PSM procedures (Figure 2) suggested imbalance between young adult college attenders and nonattenders—as indicated by standardized mean differences above ∣0.1∣—with respect to 10 of the 18 covariates that we assessed as well as the overall propensity score. The matched dataset resulting from the final matching algorithm improved balance on all variables, such that after matching all standardized mean differences were below ∣0.1∣ for each covariate and the overall propensity score. Additional analyses in the supplementary appendices also show that good balance was achieved among the various subsamples that we assessed the effect of college attendance among, with only minor exceptions among the LGB sub-sample (Supplementary Tables 3-7).
Figure 2. Standardized mean differences showing the balance improvement obtained by propensity score matching for college attendance and nonattendance, among the cohort of youth (<18 years) who aged into early adulthood (18-24 years) between Waves 1 and 3 of the PATH Study, United States, 2013-14, 2015-16.
Note: Each dot in the figure indicates the standardized mean difference of the covariate between attenders and nonattenders in either the unmatched sample (grey dots) or in the matched sample. Nearest-neighbor matching was used to balance the matched sample with a 1:1 matching ratio and a caliper of 0.1. Standardized mean difference values <∣0.1∣ indicate good balance.
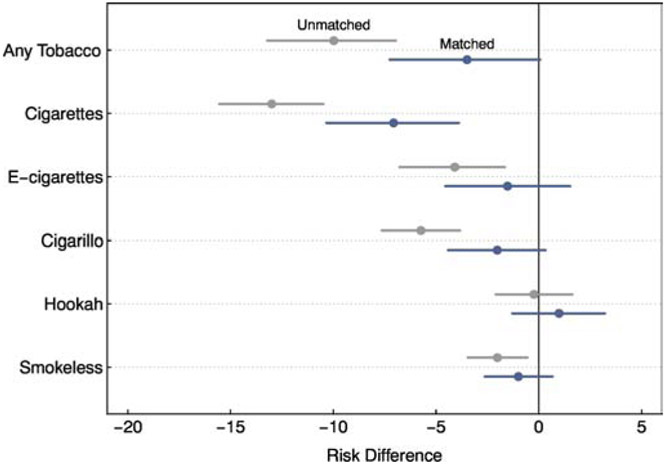
When using logistic regression models on the unmatched dataset (Figure 3), we observed differences between college attenders and nonattenders in terms of the risk of using any form of tobacco (RD (percentage points): −10.0; 95% CI: −13.2, −7.0), cigarettes (RD: −13.0; 95% CI: −15.4, −10.5), e-cigarettes (RD: −4.1; 95% CI: −6.8, −1.7), cigarillos (RD: −5.7; 95% CI: −7.6, −3.8), and smokeless tobacco (RD: −2.0; 95% CI: −3.4, −0.6), but comparable risk of using hookah (RD: −0.2; 95% CI: −2.1, 1.6). When using the balanced datasets there were no differences between college attenders and nonattenders in terms of the risk for using any form of tobacco (matched RD: −3.5; 95% CI: −7.3, 0.1), e-cigarettes (matched RD: −1.5; 95% CI: −4.6, 1.5), cigarillos (matched RD: −2.0; 95% CI: −4.4, 0.3), smokeless tobacco (matched RD: −1.0; 95% CI: −2.6, 0.7) and hookah (matched RD: 1.0; 95% CI: −1.3, 3.2). However, the differences between college attenders and nonattenders remained for cigarettes (matched RD: −7.1; 95% CI: −10.3, −3.9).
Figure 3. Differences in the risk of using tobacco by college attendance in the full unmatched sample and the propensity score matched sample, among the cohort of youth (<18 years) who aged into early adulthood (18-24 years) between Waves 1 and 3 of the PATH Study, United States, 2013-14, 2015-16.
Notes: Each dot in the figure indicates the difference in risk of using the specific tobacco product corresponding to the row between college attenders and nonattenders and line segments indicate 95% CIs for those risk difference estimates. Negative values indicate lower risk among college attenders vs. nonattenders while values at 0 indicate no difference. Grey dots and segments were estimated using the full unmatched sample and blue dots and segments were estimated using the matched sample. Nearest-neighbor matching was used to balance the matched sample with a 1:1 matching ratio and a caliper of 0.1.
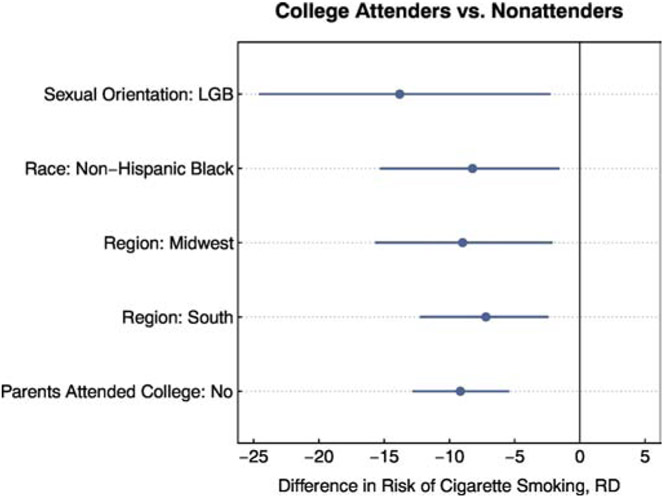
Moreover, the effect of college attendance on the risk for cigarette use was stable across the sociodemographic subpopulations that we assessed (Figure 4). Specifically, the risk of cigarette use was 13.8 percentage points (matched RD; 95% CI: −24.5, −2.3) lower among college attenders who identified as LGB than among nonattenders who identified as LGB, 8.2 percentage points (matched RD; 95% CI: −15.7, −1.6) lower among college attenders who identified as Black than among nonattenders who identified as Black, and 9.2 percentage points (matched RD; 95% CI: −12.8, −5.5) lower among first-generation college attenders than among nonattenders whose parents were also nonattenders. Further, when looking across geographic locations with a high prevalence of cigarette use, the risk of cigarette use was 9.0 percentage points (matched RD; 95% CI: −15.6, −2.2) lower among college attenders from the Midwest than among nonattenders from the Midwest and 7.2 percentage points (matched RD; 95% CI: −12.2.2.5) lower among college attenders from the South than among than nonattenders from the South.
Figure 4. Differences in the risk of using tobacco by college attendance in propensity score matched samples, among subpopulations of the cohort of youth (<18 years) who aged into early adulthood (18-24 years) between Waves 1 and 3 of the PATH Study, United States, 2013-14, 2015-16.
Notes: RD = Risk Difference; Each dot in the figure indicates the difference in risk of using cigarettes between college attenders and nonattenders and line segments indicate 95% CIs for those risk difference estimates. Negative values indicate lower risk among college attenders vs. nonattenders while values at 0 indicate no difference. Each risk difference was estimated in a separate subsample corresponding with subpopulation specified in the row. Nearest-neighbor matching was used within this subsample to balance the covariates. All matched samples were balanced with a 1:1 matching ratio and a caliper of 0.1
When comparing how the socio-ecological environment differed between college attenders and nonattenders (Table 1), we found that college attenders had a lower probability of knowing someone who they perceived to be important to them who smoked cigarettes than nonattenders (RD: −8.6; 95% CI: −11.9, −5.3) and of being exposed to tobacco advertising (RD: −7.3; 95% CI: −10.7, −4.1). College attenders also had a higher probability of perceiving social disapproval of cigarette smoking in general (RD: 7.2; 95% CI: 4.3, 10.0) and from people they perceived to be important to them (RD: 17.6; 95% CI: 14.8, 20.4). College attenders also spent less time with smokers (MD (hours): −3.1, 95% CI: −4.1, −2.2) than nonattenders.
Table 1.
Differences in socio-environmental risk and protective factors between college attenders and nonattenders among the cohort of youth (<18 years) who aged into early adulthood (18-24 years) between Waves 1 and 3 of the PATH Study, United States, 2013-14, 2015-16, n=3619
| Variable | RD or MD | 95% CI | |
|---|---|---|---|
| Perceived norm of cigarette smoking (general) | 7.2 | 4.2 | 10.0 |
| Perceived norm of cigarette smoking (among people important) | 17.6 | 14.8 | 20.4 |
| Has friends who smoke | −8.6 | −11.9 | −5.3 |
| Exposed to tobacco advertising in past 30 days | −7.3 | −10.7 | −4.1 |
| Hours spent around smokers while they were smoking in past 7 days | −3.1* | −4.1 | −2.2 |
Value is Mean Difference; MD = Mean Difference; RD = Risk difference
Note: Higher RD and MD values favor college nonattenders while lower values favor college attenders
A sensitivity analysis revealed that including or excluding those who had graduated or dropped-out of college did not qualitatively impact the results or interpretation of the results (Supplementary Figure 2).
Discussion
In this nationally representative cohort of US young adults, we found that college attendance reduced the risk of cigarette smoking but not the risk of using other tobacco products. For cigarette use, the protective effect of college attendance extended across populations with noted tobacco disparities, highlighting the potential that increacing access to college education could have on reducing disparities in cigarette smoking. College attenders perceived stronger norms against smoking cigarettes, had fewer friends who smoked and were less likely to be exposed to other smokers or to tobacco advertising, which may help to explain the effect of college attendance on the risk of cigarette smoking.
The finding that college attendance reduces the risk for cigarette smoking is consistent with past studies that relied on other methodological approaches.10-12 We add to this literature in several unique ways. Most notably, we found that although the prevalence of e-cigarette, cigarillo and smokeless tobacco use was lower among college attenders, these differences were explained by differences in pre-college risk factors suggesting the absence of a “college effect.” Moreover, cigarettes were the most frequently used product among college non-attenders, while e-cigarettes were the most frequently used product among college attenders and there was no difference between college attenders and nonattenders in terms of the risk of using hookah. One possible explanation for these results is that there are fewer prevention and health education mechanisms in place that discourage use of e-cigarettes and hookah among college attenders. For instance, there is a common misconception that e-cigarettes and hookah are safer than cigarettes, and this is associated with use;37 hookah lounges are highly prevalent around college campuses;38 and less than half of colleges include restrictions on hookah smoking in their smoke-free air laws.39 Scaling out interventions that focus on such intermediary variables may increase the potency of the college effect on reducing use of non-cigarette tobacco products.
We also found that the effects of college attendance on the risk of cigarette use extended across populations with smoking-related disparities. This finding substantiates past studies that have shown that differences in education attainment can help explain other smoking-related disparities22 by suggesting with that these differences in the case of college attendance may be causal. By extension, this suggests that raising college attendance among populations vulnerable to smoking may improve health outcomes in those populations by reducing the risk of smoking. Where sample size allows, future studies should also investigate whether the effect of college attendance extends to other populations with notable disparities in tobacco use, such as Americans Indians and Alaskan Natives.22,40
When considering the potential mechanism by which college might prevent cigarette smoking we found evidence suggesting that differences in the social-ecological environment between attenders and nonattenders may at least partially play a part.23 In our results, college attenders were more likely to perceive strong anti-smoking norms, less likely to socialize with smokers and were exposed to fewer tobacco advertisements. Continuing to scale out policies that make college campuses less amenable to smoking, such as smoke-free air laws, as well as considering policies that govern the quantity, type and location of retailer outlets and marketing41 around college campuses may further increase the effect that college attendance has on tobacco use.
There is also a need for tobacco prevention efforts that reach beyond the college campus to impact nonattending tobacco users who use tobacco at higher rates. Comprehensive tobacco control programs that reach both college attenders and non-attenders should be applied in all state and local jurisdictions.42 Increasing the minimum age of tobacco sales to 21 could reduce both youth and young adult tobacco use regardless of college attendance; however, coverage of this policy remains low.43 Targeted interventions that focus on places where nonattending populations congregate should become a programmatic focus. For instance, some tobacco control interventions targeting young adults have been implemented in bars and could be applied more broadly.44 Additionally, ensuring that broader implementation of effective workplace-focused cessation programs at workplaces that employ a large number of young adults may improve cessation outcomes among smokers in these organizations
While our study has many strengths, there are some limitations that should be noted. Although follow-up rates were relatively high for the PATH Study, the nonresponse to the follow-up survey could impact our results. Also, although matching drastically improved balance on the many potential confounders that were included in the PATH Study, there is always a potential that additional unmeasured confounders are driving the observed associations. However, these would need to be substantial and operate in the opposite direction of the observed confounders to bring back any effect of college attendance on the risk of using e-cigarettes, cigarillos, hookah or smokeless tobacco . Thirdly, while capturing the most inclusive definition of college attendance, our measure may suppress further variation between college attenders that could not be captured due to the short time window of the study and merit future research. For instance, there may be differences between 2-year and 4-year degree programs,12 public or private universities, or between schools that have stronger or weaker tobacco control policies. Finally, given the small sample size of LGB young adults, we had relatively low power to detect the effects of college attendance on cigarette use among this subsample; however, despite the small sample and associated low precision, the effect was comparable in magnitude and did not cross the null.
While considering these important limitations, our study suggests that increasing access to college in the US could have a positive effect on reducing cigarette smoking, including by addressing tobacco-related disparities. Strengthening existing tobacco control efforts on college campuses—e.g., by ensuring all tobacco products are included in smoke-free air laws—and creating new policies to counteract other environmental exposures, such as the proliferation of hookah lounges, may further strengthen the “college effect” on cigarettes and other tobacco products. Interventions that reach beyond the college campus must be considered to address the higher use rates among nonattending young adults.
Supplementary Material
Highlights.
Overall, college attenders had lower risk for using tobacco products
When accounting for pre-college risk factors, attendance only reduced the risk of cigarette use
The reduced risk for cigarette use extended across subpopulations with known disparities in use
College attenders had socio-ecological environments that were less conducive to cigarette use
Acknowledgments
Funding Details: This work was supported by grant 1R01CA234539-01 from the National Cancer Institute at the National Institutes of Health and grant 28IR-0066 from the Tobacco Related Diseases Research Program. The study sponsors took no part in the study design; collection, analysis and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None to Declare
References
- 1.United States. Surgeon General’s Advisory Committee on Smoking. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. US Department of Health, Education, and Welfare, Public Health Service; 1964. [Google Scholar]
- 2.Pierce JP, Fiore MC, Novotny TE, Hatziandreu EJ, Davis RM. Trends in cigarette smoking in the United States. Educational differences are increasing. JAMA. 1989;261(1):56–60. [PubMed] [Google Scholar]
- 3.Hu M-C, Davies M, Kandel DB. Epidemiology and Correlates of Daily Smoking and Nicotine Dependence Among Young Adults in the United States. Am J Public Health. 2006;96(2):299–308. doi: 10.2105/AJPH.2004.057232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Green MP, McCausland KL, Xiao H, Duke JC, Vallone DM, Healton CG. A closer look at smoking among young adults: where tobacco control should focus its attention. Am J Public Health. 2007;97(8):1427–1433. doi: 10.2105/AJPH.2006.103945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United States Public Health Service: Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (U.S.) Office on Smoking and Health. Preventing Tobacco Use among Youth and Young Adults. We Can Make the next Generation Tobacco-Free: A Report of the Surgeon General. Atlanta, Ga. Washington, D.C: U.S. Dept. of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 2012:16 p. [Google Scholar]
- 6.Rath JM, Villanti AC, Abrams DB, Vallone DM. Patterns of tobacco use and dual use in US young adults: the missing link between youth prevention and adult cessation. J Environ Public Health. 2012;2012:679134. doi: 10.1155/2012/679134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chassin L, Presson CC, Sherman SJ, Edwards DA. The natural history of cigarette smoking: predicting young-adult smoking outcomes from adolescent smoking patterns. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 1990;9(6):701–716. [DOI] [PubMed] [Google Scholar]
- 8.Trinidad DR, Pierce JP, Sargent JD, et al. Susceptibility to tobacco product use among youth in wave 1 of the population Assessment of tobacco and health (PATH) study. Prev Med. 2017;101:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addict Abingdon Engl. 2001;96(2):313–323. doi: 10.1080/09652140020021053 [DOI] [PubMed] [Google Scholar]
- 10.Gilman SE, Martin LT, Abrams DB, et al. Educational attainment and cigarette smoking: a causal association? Int J Epidemiol. 2008;37(3):615–624. doi: 10.1093/ije/dym250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujiwara T, Kawachi I. Is education causally related to better health? A twin fixed-effect study in the USA. Int J Epidemiol. 2009;38(5):1310–1322. doi: 10.1093/ije/dyp226 [DOI] [PubMed] [Google Scholar]
- 12.Heckman JJ, Humphries JE, Veramendi G. Returns to Education: The Causal Effects of Education on Earnings, Health and Smoking. National Bureau of Economic Research;2016. doi: 10.3386/w22291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubin DB. Estimating causal effects of treatments in randomized and nonrandomized studies. J Educ Psychol. 1974;66(5):688. [Google Scholar]
- 14.DeBerard MS, Spielmans GI, Julka DL. Predictors of academic achievement and retention among college freshmen: A longitudinal study. Coll Stud J. 2004;38(1):66–80. [Google Scholar]
- 15.Greenland S Causation and Causal Inference. Springer;2011. [Google Scholar]
- 16.Hernan MA, Robins JM. Estimating causal effects from epidemiological data. J Epidemiol Community Health. 2006;60(7):578–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal. 2007;15(3):199–236. [Google Scholar]
- 19.Wang TW, Asman K, Gentzke AS, et al. Tobacco Product Use Among Adults — United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. doi: 10.15585/mmwr.mm6744a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jamal A, Phillips E, Gentzke AS, et al. Current Cigarette Smoking Among Adults — United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53–59. doi: 10.15585/mmwr.mm6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students — United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276–1277. doi: 10.15585/mmwr.mm6745a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agaku IT, Odani S, Okuyemi KS, Armour B. Disparities in current cigarette smoking among US adults, 2002–2016. Tob Control. May 2019:tobaccocontrol-2019-054948. doi: 10.1136/tobaccocontrol-2019-054948 [DOI] [PubMed] [Google Scholar]
- 23.Sallis JF, Owen N, Fisher E. Ecological models of health behavior. Health Behav Theory Res Pract. 2015;5:43–64. [Google Scholar]
- 24.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. August 2016. doi: 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. doi: 10.1056/NEJMsa1607538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westat. PATH Study Public Use Files User Guide. https://goo.gl/B2uj9G. Published 2017. Accessed January 31, 2018.
- 27.McDonell MG, Comtois KA, Voss WD, Morgan AH, Ries RK. Global Appraisal of Individual Needs Short Screener (GSS): psychometric properties and performance as a screening measure in adolescents. Am J Drug Alcohol Abuse. 2009;35(3):157–160. doi: 10.1080/00952990902825421 [DOI] [PubMed] [Google Scholar]
- 28.Conway KP, Green VR, Kasza KA, et al. Co-occurrence of tobacco product use, substance use, and mental health problems among youth: Findings from wave 1 (2013-2014) of the population assessment of tobacco and health (PATH) study. Addict Behav. 2018;76:208–217. doi: 10.1016/j.addbeh.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green VR, Conway KP, Silveira ML, et al. Mental Health Problems and Onset of Tobacco Use Among 12- to 24-Year-Olds in the PATH Study. J Am Acad Child Adolesc Psychiatry. 2018;57(12):944–954.e4. doi: 10.1016/j.jaac.2018.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stephenson MT, Hoyle RH, Palmgreen P, Slater MD. Brief measures of sensation seeking for screening and large-scale surveys. Drug Alcohol Depend. 2003;72(3):279–286. doi: 10.1016/J.Drugalcdep.2003.08.003 [DOI] [PubMed] [Google Scholar]
- 31.Honaker J, King G, Blackwell M. Amelia II: A Program for Missing Data. J Stat Softw. 2011;45(7). doi: 10.18637/jss.v045.i07 [DOI] [Google Scholar]
- 32.Myers AE, Hall MG, Isgett LF, Ribisl KM. A comparison of three policy approaches for tobacco retailer reduction. Prev Med. 2015;74:67–73. doi: 10.1016/j.ypmed.2015.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med. 2007;26(4):734–753. [DOI] [PubMed] [Google Scholar]
- 34.Green KM, Stuart EA. Examining Moderation Analyses in Propensity Score Methods: Application to Depression and Substance Use. J Consult Clin Psychol. 2014;82(5):773–783. doi: 10.1037/a0036515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CDCTobaccoFree. Burden of Tobacco Use in the U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html. Published February 28, 2019. Accessed June 12, 2019.
- 36.King G, Tomz M, Wittenberg J. Making the Most of Statistical Analyses: Improving Interpretation and Presentation. Am J Polit Sci. 2000;44(2):347. doi: 10.2307/2669316 [DOI] [Google Scholar]
- 37.Strong DR, Leas E, Elton-Marshall T, et al. Harm perceptions and tobacco use initiation among youth in Wave 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Prev Med. 2019;123:185–191. doi: 10.1016/j.ypmed.2019.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kates FR, Salloum RG, Thrasher JF, Islam F, Fleischer NL, Maziak W. Geographic Proximity of Waterpipe Smoking Establishments to Colleges in the U.S. Am J Prev Med. 2016;50(1):e9–e14. doi: 10.1016/j.amepre.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang TW, Tynan MA, Hallett C, et al. Smoke-Free and Tobacco-Free Policies in Colleges and Universities — United States and Territories, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(24):686–689. doi: 10.15585/mmwr.mm6724a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luke DA, Hammond RA, Combs T, et al. Tobacco Town: Computational Modeling of Policy Options to Reduce Tobacco Retailer Density. Am J Public Health. 2017;107(5):740–746. doi: 10.2105/AJPH.2017.303685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U.S. Department of Health and Human Services. Best Practices for Comprehensive Tobacco Control Programs. http://www.cdc.gov/tobacco/stateandcommunity/best_practices/pdfs/2014/comprehensive.pdf. Published 2014. Accessed February 25, 2019.
- 42.Leas EC, Schliecher N, Recinos A, Mahoney M, Henriksen L. State and regional gaps in coverage of ‘Tobacco 21’ policies. Tob Control. April 2019:tobaccocontrol-2019-054942. doi: 10.1136/tobaccocontrol-2019-054942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ling PM, Lee YO, Hong J, Neilands TB, Jordan JW, Glantz SA. Social branding to decrease smoking among young adults in bars. Am J Public Health. 2014;104(4):751–760. doi: 10.2105/AJPH.2013.301666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Syamlal G, King BA, Mazurek JM. Workplace Smoke-Free Policies and Cessation Programs Among U.S. Working Adults. Am J Prev Med. 2019;56(4):548–562. doi: 10.1016/j.amepre.2018.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.