Abstract
Objectives
Ethnic enclaves are ethnically, spatially, and socially distinct communities that may promote health through access to culturally appropriate resources and reduced exposure to discrimination. This study examined ethnic enclave residence and pregnancy outcomes among Asian/Pacific Islander (API) women in the USA.
Design
We examined 9206 API births in the Consortium on Safe Labor (2002–2008). Ethnic enclaves were defined as hospital regions with high percentage of API residents (> 4%), high dissimilarity index (> 0.41; distribution of API and white residents within a geographic area), and high isolation index (> 0.03; interaction between API and white residents in an area). Gestational diabetes mellitus (GDM), preterm birth (PTB), small for gestational age (SGA), and smoking and alcohol use during pregnancy were reported in medical records supplemented with ICD-9 codes. Hierarchical logistic regression models estimated associations between ethnic enclaves and pregnancy outcomes, adjusted for maternal factors, area-level poverty, and air pollution.
Results
Women in enclaves had lower odds of GDM (OR 0.61; 95%CI 0.45, 0.82), PTB (OR 0.74; 95%CI 0.56, 0.99), and SGA (OR 0.68; 95%CI 0.52, 0.89) compared with women in non-enclaves. Prenatal smoking and alcohol use appeared less likely in enclaves, but estimates were imprecise. Within enclaves, about 10.5% of homes speak an API language, compared with 6.0% in non-enclaves. The mean percent of foreign-born API populations was 67.4% in enclaves and 68.8% in non-enclaves.
Conclusions
API women residing in ethnic enclaves had better pregnancy outcomes than API women residing in non-enclave areas. Access to culturally appropriate social supports and resources may be important for health promotion among API populations.
Keywords: Ethnic enclave, Asian/Pacific Islander, Gestational diabetes mellitus, Preterm birth, Small for gestational age, Health behaviors
Introduction
The Asian/Pacific Islander (API) population is the fastest growing racial/ethnic group in the USA [1], and over 65% of this population is foreign born [2]. Additionally, 95% of the US API population resides within metropolitan areas [3]. API residents of US metropolitan areas have historically been concentrated into “ethnic enclaves,” characterized by a high concentration of API residents of a similar ancestry and are socially and geographically distinct from the racial/ethnic majority population [4–6].
Despite the concentration of API residents in US metropolitan areas, our understanding of the potential health effects of ethnic enclaves is limited. The lived experiences of API residents within ethnic enclaves may differ from API residents of non-enclave areas, as API residents of ethnic enclaves may be exposed to less discrimination and have easier access to culturally relevant goods and services than API residents of non-enclave areas [4–6]. Thus, residing in ethnic enclaves may be associated with better outcomes. For example, API individuals residing in ethnic enclaves were found to have lower rates of cancer [7] and longer life spans [8]. However, evidence regarding pregnancy outcomes among API women residing in ethnic enclaves is limited. Given the large percentage of API individuals residing in US metropolitan areas [3], and the persistent health disparities of gestational diabetes mellitus (GDM) [9, 10] and small for gestational age (SGA) births [9–12] among US API populations, a greater focus on pregnancy outcomes among API residents of ethnic enclaves in the USA is warranted.
Current evidence regarding pregnancy outcomes and health behaviors among API women residing in ethnic enclaves is inconsistent. Residence in ethnic enclaves may be associated with lower rates of smoking during pregnancy [11, 13] and lower risk of delayed prenatal care [11], yet the association between ethnic enclaves and birth weight, preterm birth, and gestational diabetes mellitus is mixed and may vary according to the ancestry of the API population [9, 14].
Current studies of API ethnic enclaves lack recognition of ambient air pollution as a determinant of poor outcomes. API communities are exposed to high levels of air pollution [15], and API women may be uniquely susceptible to poor pregnancy outcomes when exposed to high levels of ambient air pollution [16]. Additionally, API communities experience high levels of area-level poverty [17]. Thus, accounting for ambient air pollution and area-level poverty may allow for a better understanding of the association between residence in an ethnic enclave and pregnancy and behavior outcomes.
Contributing to inconsistent results among current studies of API ethnic enclaves is a lack of consistent definition of what constitutes an ethnic enclave. Constructs used to identity ethnic enclaves include various measures of racial housing segregation and population density [5, 6, 9]. Variability in defining API ethnic enclaves does not allow for comparable results, further limiting our understanding of health outcomes associated with residence in an API ethnic enclave.
Current evidence of health outcomes among API residents of ethnic enclaves is limited due to scarcity of existing studies, a lack of multiple examinations of similar outcomes, no standard definition of what constitutes an ethnic enclave, and studies focused largely on a single geographic area. The aim of this study was to use a nationwide obstetric cohort to contribute additional evidence to the literature regarding ethnic enclaves as a determinant of health for pregnant API women. The study of the association between ethnic enclaves and multiple pregnancy and behavior outcomes among API women in multiple US metropolitan areas focused on recognized health disparities among pregnant API women: GDM, SGA, and other pregnancy and behavior outcomes examined in prior studies of API ethnic enclaves (preterm birth (PTB), smoking in pregnancy, and alcohol use in pregnancy). We hypothesized that API women residing in ethnic enclaves had lower risk for poor pregnancy and behavior outcomes compared with API women residing in non-enclave areas.
Methods
The Consortium on Safe Labor (CSL) was an electronic medical record-based retrospective cohort study from 2002 to 2008 which included 19 hospitals (8 university teaching hospitals, 9 community teaching hospitals, 2 community hospitals) in 15 hospital referral regions (HRR), catchment areas for tertiary care hospitals [18]. Hospitals were selected based on availability of electronic medical records and for geographic representation of the 9 American College of Obstetricians and Gynecologists districts [19]. Data extracted for births at 23 weeks or later included maternal sociodemographic characteristics; medical, reproductive, and prenatal history; and labor and delivery postpartum and newborn data. A total of 228,438 deliveries were included in the study. We excluded multifetal pregnancies (n = 5053; 2.21%) and singleton pregnancies with missing air pollution exposure information (n = 10; 0.004%). Including only Asian/Pacific Islander mothers resulted in an analytic sample of 9206 births to 8475 mothers. Institutional Review Boards at all sites approved the CSL and data are anonymous.
As individual-level addresses are not available in the CSL, residence was estimated using the HRR in which the birth occurred [20]. HRRs are comparable in geographic size to Metropolitan Statistical Areas [21] and are based on population centers of at least 120,000 residents [18].
We aggregated ZIP code tabulation area to provide HRR-level sociodemographic estimates as no available crosswalk aggregates smaller geographic units, like census tracts, to the HRR level [18, 21]. ZIP code tabulation area data was obtained from the 2000 Decennial Census, and the 2007–2011 5-year average of the American Community Survey (ACS) from the National Historical Geographic Information System [22]. CSL data was linked with contemporary sociodemographic data: births in 2002–2004 were linked with 2000 Census data, and births in 2005–2008 were linked with 2007–2011 ACS data [21].
Air pollution exposure data in the CSL are estimated using the Community Multiscale Air Quality Model, a 3-dimensional, multipollutant air quality model used to predict ambient pollutant levels using the National Emission Inventory emissions data and Weather Research Forecasting Model meteorological data. Exposure was based on the predicted hourly ambient pollutant concentrations within HRRs, weighted to reflect population concentration, and accounting for non-residential areas within an HRR, as previously described [20].
Outcome Variables
Gestational diabetes mellitus (GDM) was recorded in the medical record or discharge summaries using ICD-9 code 648.8. During the study period (2002–2008), it was typical for women to be screened for GDM between 24 and 28 weeks gestation using the Carpenter and Coustan criteria [23]. PTB was defined as births from 23 to less than 37 weeks of gestation, with gestational age as recorded in medical records using the best clinical estimate. SGA births were defined as infants born < 10th percentile of weight of infant sex and gestational age, based on internal reference [24]. We examined smoking and alcohol use as previous studies of ethnic enclave status among API women also examined health behaviors [11, 13]. Smoking and alcohol use during pregnancy was reported in medical records. As smoking during pregnancy (1.51%) and alcohol use during pregnancy (0.71%) were rare and are typically underreported in medical records [25], we also created a “smoking or alcohol use during pregnancy” variable.
Identifying Ethnic Enclaves
We identified ethnic enclaves at the HRR level, as HRRs are the smallest geographic area available in the CSL [20] yet are large enough geographic units to measure residential sorting by race/ethnicity [21]. We have previously measured residential segregation at the HRR level in the CSL [21],and previous studies have used counties [13] or Metropolitan Statistical Areas [26] to measure ethnic enclaves.
To the best of our knowledge no validated measure of ethnic enclaves exists in the current literature. Recent studies of ethnic enclaves in the USA used various geographic units of analysis, including census tracts [5, 9], ZIP codes [6], Metropolitan Statistical Areas [26], and counties [13]. As HRRs are centered on metropolitan areas with at least 120,000 residents, using HRRs to measure ethnic enclaves allows for a focus on urban centers where the majority of API populations reside in the USA [3]. However, the broader geographic coverage (average miles2 13,065; average population size in thousands 2026; Supplemental Table 1) of HRRs allows for inclusion of potential ethnic enclaves outside of urban centers that may be missed if using smaller geographic units of analysis [26].
Multiple constructs have been considered to represent ethnic enclaves, including population density [5, 9], measures of racial/ethnic segregation [13], or a combination of population density and racial/ethnic segregation [6]. Relying solely on population density to identify ethnic enclaves suggests a sufficiently large population to represent a potentially socially distinct area yet may not best capture the geographic distinction that is a key facet of ethnic enclaves. Identifying ethnic enclaves using racial/ethnic segregation better captures the geographic distinction of ethnic enclaves; however, small populations of a racial/ethnic group may be considered highly segregated yet not sufficiently large to represent a socially distinct area. Use of both racial/ethnic density measures and segregation measures may better represent the social and geographic distinction of an ethnic enclave which may alleviate concerns regarding use of a single measure [6]. Thus, we combined measures of API population density and racial/ethnic segregation to identify API ethnic enclaves for this analysis.
API population density, the percent of API individuals residing in an HRR, is a measure of social distinction. Racial/ethnic segregation is represented by two variables: API-white dissimilarity index, the differential distribution of APIs and whites within a geographic area [27, 28], and the API isolation index, the probability that a member of the API group will interact with a member of the same group [27, 28]; both are measures of geographic distinction. API density, API-white dissimilarity index, and API isolation index were calculated separately for census data and ACS data (Table 1).
Table 1.
Area-level measures used to identify ethnic enclaves
| Measure | Formula | Interpretation |
|---|---|---|
| API density Range 0–100 100 = high density |
Density = (AT/PT) × 100 | A score of 100 suggests all residents of an HRR are of API background. |
| Dissimilarity index Range 0–1 1 = high dissimilarity |
A score of 0.6 suggests 60% of API residents of an HRR would need to move to different ZIP codes within their HRR of residence in order for APIs and whites to be evenly dispersed in that HRR. | |
| Isolation index Score range 0–1 1 = high isolation |
If APIs make up 25% of the population of an HRR, but all APIs live in ZIP codes that are 100% black, the isolation index would be equal to 1 for that HRR. |
ai, number of API in the ZIP code
AT, number of API in the HRR
n, number of ZIP codes
PT, total population of the HRR
wi, number of whites in the ZIP code
WT, number of white in the HRR
Informed by previous work using population-based percentiles to identify ethnic enclaves [5, 6, 9], we identified tertiles (low, medium, high) for API density, API-white dissimilarity, and API isolation. An HRR was considered an ethnic enclave if it was in the high category for API density, API-white dissimilarity, and API isolation.
Covariates
Individual-level covariates included maternal age, marital status (married, single, divorced, missing), insurance status (public, private, other), pre-pregnancy body mass index (BMI, < 18.5, 18.5 ≤ 224.9, 25 ≤ 29.9, ≥ 30), parity (nulliparous or multiparous), and preconception chronic disease (asthma, hypertension, diabetes). Insurance status (reflecting access to resources) [29] and marital status (married couples typically have higher income compared to other families) [30] are proxies of socioeconomic status as family income is not available in CSL data. BMI was imputed to account for high degree of missingness.
HRR-level covariates included area-level poverty (proportion of residents in the HRR living below federal poverty thresholds), hospital type (university affiliated teaching hospital, community teaching hospital, community non-teaching hospital), and ambient air pollution [16, 31–33] (GDM: benzene, sulfur dioxide, nitrous oxide; PTB: carbon monoxide, nitrous oxide, sulfur dioxide; SGA: particulate matter 10, sulfur dioxide). Specific air pollutants were chosen based on previous studies of the association between ambient air pollutants and the outcome of interest [16, 31–33]. HRR-level poverty and air pollution were treated as continuous. Covariates included in analysis were informed by previous studies [9, 11, 12, 14, 16, 31–33].
Statistical Analysis
Prevalence of pregnancy and behavior outcomes and maternal characteristics were reported by ethnic enclave residence.
Two-level hierarchical logistic regression models, women nested within HRRs, with robust standard errors to account for repeated births within the same mother (n = 731, 7.9% of births) were fit to estimate odds ratio (OR) and 95% confidence intervals for the association between residence in an ethnic enclave and pregnancy and behavioral outcomes. A separate model was used for each outcome variable: GDM, SGA, PTB, smoking, alcohol, and smoking/alcohol. Residence in a non-enclave area served as the reference.
As the potential protective effect of residence in an ethnic enclave may be related to the distinct social environment of ethnic enclaves, we conducted post hoc analysis to compare the HRR-level percent foreign-born API residents and percent households speaking an API language of ethnic enclaves and non-enclave areas, obtained from 2000 Census and 2007–2011 ACS data.
Results
Table 2 includes prevalence of outcomes and maternal characteristics by ethnic enclave status. Of the 9206 API women in the sample, 1924 (20.8%) resided in an ethnic enclave, while 7282 (79.2%) resided outside an ethnic enclave. Women residing in ethnic enclaves had lower prevalence of SGA, GDM, and PTB (p < 0.05) compared with women in non-enclave areas, and differences in prevalence of smoking, alcohol use, or smoking/alcohol use were not statistically significant. Women residing in ethnic enclaves were more likely to be over the age of 30, be married, and have no prior births (Table 2). Women residing in non-enclave areas were more likely to have private insurance and be admitted to community hospitals for delivery (Table 2).
Table 2.
Frequency (and percent) of outcomes and demographic characteristics by Asian/Pacific Islander ethnic enclave status in the Consortium on Safe Labor among Asian/Pacific Islander women (n = 9206)
| Residing in ethnic enclave |
p valuesa | ||
|---|---|---|---|
| Yes (n = 1924) | No (n = 7282) | ||
| Pregnancy outcomes | |||
| Gestational diabetes mellitusb | 142 (7.5) | 757 (10.5) | p < 0.01 |
| Preterm birth | 140 (7.3) | 631 (8.6) | p = 0.03 |
| Small for gestational age | 193 (10.0) | 1025 (14.0) | p < 0.01 |
| Behavior outcomes | |||
| Smoking | 25 (1.3) | 114 (1.5) | p = 0.40 |
| Alcohol | 17 (0.6) | 48 (0.8) | p = 0.33 |
| Smoking/alcohol | 38 (1.9) | 147 (2.0) | p = 0.94 |
| Maternal age | p < 0.01 | ||
| < 20 years | 13 (0.68) | 155 (2.13) | |
| 20–24 years | 72 (3.74) | 1223 (16.79) | |
| 25–29 years | 363 (18.87) | 2467 (33.88) | |
| 30–34 years | 801 (41.63) | 2213 (30.39) | |
| 35+ years | 671 (34.88) | 1222 (16.78) | |
| Unknown/missing | 4 (0.21) | 2 (0.03) | |
| Body mass index | p < 0.01 | ||
| ≥ 30 | 40 (2.08) | 408 (5.60) | |
| 25–29.9 | 188 (9.77) | 574 (7.88) | |
| 18.5–24.9 | 199 (10.34) | 425 (5.84) | |
| 11.2–18.49 | 1247 (64.81) | 2270 (31.17) | |
| Unknown | 250 (12.99) | 3605 (49.51) | |
| Insurance type | p < 0.01 | ||
| Private | 800 (41.58) | 5665 (77.79) | |
| Public | 47 (2.44) | 1253 (17.21) | |
| Self-pay | 5 (0.26) | 194 (2.66) | |
| Other | 1072 (55.72) | 170 (2.33) | |
| Marital status | p < 0.01 | ||
| Married | 1766 (91.79) | 5998 (82.37) | |
| Single | 146 (7.59) | 1106 (15.19) | |
| Divorced | 8 (0.42) | 48 (0.66) | |
| Unknown | 4 (0.21) | 130 (1.79) | |
| Prior births | p < 0.01 | ||
| 0 | 1118 (58.11) | 3373 (46.32) | |
| ≥ 1 | 806 (41.89) | 3909 (53.68) | |
| Hospital type | p < 0.01 | ||
| University affiliated | 1827 (94.96) | 1986 (27.27) | |
| Community: teaching | 97 (5.04) | 4889 (67.14) | |
| Community: non-teaching | 0 (0) | 407 (5.59) | |
p values obtain using generalized estimating equations to account for women who had more than one pregnancy in the study
Excluded women with preconception diagnosis of diabetes from analysis
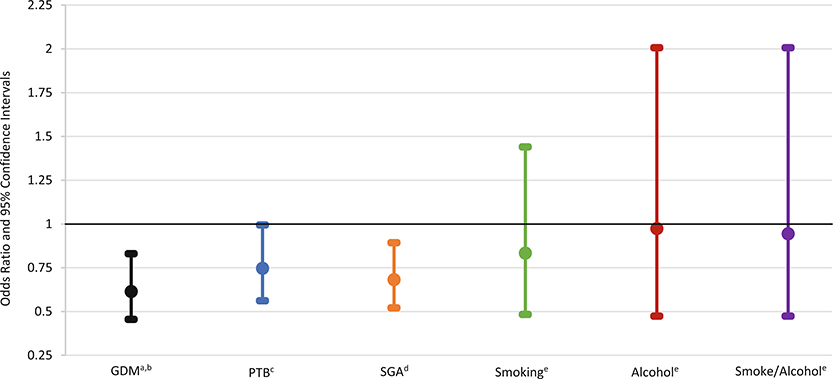
In hierarchical logistic regression models, women residing in ethnic enclaves had lower odds of poor pregnancy outcomes than women residing in non-enclave areas (Fig. 1). More specifically, women in ethnic enclaves had 39% (OR 0.61; 95%CI 0.45, 0.83) lower odds of GDM, 26% (OR 0.74; 95%CI 0.56, 0.99) lower odds of PTB, and 32% (OR 0.68; 95% CI 0.52, 0.89) lower odds of SGA. Results for smoking, alcohol use, and smoking or alcohol use suggest ethnic enclaves may be protective against poor health behaviors, but the confidence intervals were imprecise (Fig. 1).
Fig. 1.
Adjusted odds of pregnancy and behavior outcomes among Asian/Pacific Islander women residing in Asian/Pacific Islander ethnic enclaves in the Consortium on Safe Labor 2002–2008. aN = 9068; women with preconception diagnosis of diabetes excluded from analysis. bModel included maternal age, insurance status, preconception body mass index, marital status, parity, chronic disease status, area-level poverty, ambient sulfur dioxide, ambient nitrous oxide, and ambient benzene. cModel included maternal age, insurance status, preconception body mass index, marital status, parity, chronic disease status, area-level poverty, ambient carbon monoxide, ambient nitrous oxide, and ambient sulfur dioxide. dModel included maternal age, insurance status, preconception body mass index, marital status, parity, chronic disease status, area-level poverty, ambient particulate matter 10, and ambient sulfur dioxide. eModel included maternal age, insurance status, preconception bodymass index,marital status, parity, and chronic disease status
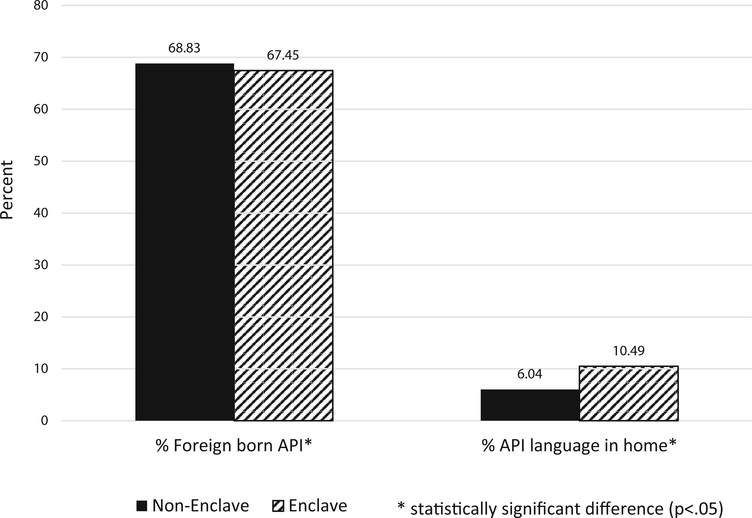
In post hoc analysis, we observed the percent foreign born in API ethnic enclaves, and non-enclaves were similar, but slightly higher in non-enclaves (67.4% in enclaves and 68.8% in non-enclaves (Fig. 2). API ethnic enclaves had a higher percentage of API languages spoken in homes (10.5%) compared with non-enclaves (6.0%) (Fig. 2).
Fig. 2.
Percent foreign born and percent Asian/Pacific Islander language spoken in home by ethnic enclave status in the Consortium on Safe Labor 2002–2008
Discussion
In this study of pregnancy and behavior outcomes among API women residing in ethnic enclaves across 15 US metropolitan areas, we found that API women residing in ethnic enclaves had lower odds of adverse pregnancy outcomes of GDM, PTB, and SGA than API women residing in non-enclave areas. Our results also suggest women residing in ethnic enclaves may also have had lower risk of smoking and alcohol use during pregnancy. These results are in line with our hypothesis that API women residing in ethnic enclaves will have better pregnancy and behavior outcomes than API women residing in non-enclave areas.
Our observations are in line with recent evidence regarding pregnancy and behavior outcomes among pregnant API women, with the most consistent evidence suggesting ethnic enclaves are associated with lower risk of smoking during pregnancy. In New Jersey, among a sample of immigrant women from India, a 60% lower risk of smoking during pregnancy among women residing in ethnic enclaves compared with women residing in non-enclave areas was observed [11]. In a national sample of racially/ethnically diverse US women, lower probability of interaction with white residents (a measure of racial/ethnic density and segregation) was associated with decreased smoking during pregnancy among API women [13]. A protective effect of ethnic enclaves among API populations has also been observed in the UK, where Pakistani women residing in ethnic enclaves had lower risk of smoking during pregnancy than women residing outside ethnic enclaves [34]. Limitations of using medical records to determine smoking during pregnancy likely contributed to our lack of a statistically significant association between ethnic enclave residence and smoking during pregnancy [25], our results suggest a potentially protective effect (Fig. 1).
Our findings of lower risk of PTB among API women residing in ethnic enclaves are largely in line with extant evidence, though few statistically significant associations have been reported. Lower risk of PTB has been observed among Indian mothers in the USA [11] and among Bangladeshi, Indian, and Pakistani mothers in the UK-based Millennium Cohort [14]. However, in the Bradford cohort, another UK cohort, an increased risk of PTB was observed among Pakistani mothers residing in ethnic enclaves [34].
Evidence regarding fetal growth is inconsistent and may vary by ancestry within the broader API population. Among Indian mothers in the USA, evidence suggests a reduced risk of low birth weight among women residing in ethnic enclaves [11]. Evidence from the Millennium Cohort suggests residence in an ethnic enclave increased risk of low birth weight among Bangladeshi and Indian mothers, while a reduced risk of low birth weight was observed among Pakistani mothers [14]. Contrasting the results from the Millennium Cohort, the Bradford cohort found infants born to Pakistani mothers residing in ethnic enclaves had greater risk of low birth weight [34]. However, none of these observations were statistically significant [11, 14, 34].
Ancestry-specific risk of GDM was reported among API women in New York [9]. South Central Asian women residing in ethnic enclaves had a 20–40% increased risk of GDM compared with South Central Asian women residing in non-enclave areas. In contrast, Chinese women residing in ethnic enclaves had an approximate 4%decreased risk of GDM compared with Chinese women residing in non-enclave areas.
These ancestry-specific findings are important to note given that individuals of multiple ancestries are often aggregated into a single API population. This masks potential differences in health risk. For instance, women of Asian ancestry may have different risks for developing GDM than do women of Pacific Islander ancestry [35, 36]. Thus, differing findings by ancestry within the broader API population highlight the need for future studies to consider ancestry to best understand health outcomes among the broader API population.
In the current study, the potentially protective effect of residing within an ethnic enclave was observed after adjustment for a range of individual-level factors, including socioeconomic status and medical risks. Area-level factors were also adjusted for. This is the first study of ethnic enclaves to also account of air pollution exposure, noteworthy as API communities have high levels of air pollution [15], and API women may be at higher risk of poor pregnancy outcomes when exposed to air pollution than women from other racial/ethnic groups [16]. We also adjusted for area-level poverty, which is linked with racial/ethnic disparities in pregnancy outcomes [37]. Thus, the benefit of residing in an ethnic enclave may be greater than any detrimental effect of exposure to areas with poor air quality or areas of high poverty.
The health benefits for API residents residing within an API ethnic enclave may relate to increased culturally relevant social and economic connectivity. Social cohesion and social networks allow for greater political participation/representation, community organizations, and civic participation [5, 6, 11, 38]. These social supports may buffer residents from exposure to and consequences of discrimination, leading to reduced uptake of unhealthy coping mechanisms like smoking and alcohol use [5, 6, 11]. The reduced uptake of unhealthy coping mechanisms is partially supported by our findings suggesting potentially lower rates of smoking and alcohol use in pregnancy among women residing in ethnic enclaves (Table 2; Fig. 1). Additionally, the social climate of ethnic enclaves may mitigate negative effects of poverty and unsafe physical activity spaces that are associated with areas of high concentration of racial/ethnic minorities and immigrant communities [39–41].
As a majority of US API residents are immigrants [1], API ethnic enclaves may allow for more successful adaptation to life in the USA as health-relevant goods and services cater to the specific ethnic community of the enclave. For example, access to ethnic grocery stores in ethnic enclaves may increase access and boost adherence to traditional diets which are healthier than a typical American diet [5, 6]. Additionally, API residents of ethnic enclaves may have greater access to health care providers of similar ancestry and culturally specific health information, and these services may be provided in language native to the resident population [42].
Examining the foreign-born status and the languages spoken at home of the API populations reflected in the CSL allowed us to determine if socially/culturally lived experiences differed by enclave status. In post hoc analysis, API populations in ethnic enclaves and non-enclave areas have a similarly high percent of foreign-born residents, yet ethnic enclaves have a higher percentage of homes speaking a native API language than do non-enclave areas (Fig. 2). This greater use of API language suggests the social environments of the ethnic enclaves identified in the current study may provide a more culturally relevant experience for API residents leading to better health outcomes. Additionally, API foreign-born status and API language spoken in homes in the present study mirror national estimates [1]. While the CSL is not a nationally representative sample, the API population in the CSL reflected a similar population percentage as that in the overall US API population. For example, according to the 2000 Decennial Census, the API population in the USA was about 3.5%, and according to the 2010 Decennial Census, the API population in the USA was about 5% [43]. The API population in the CSL (sampled between 2002 and 2008) is approximately 4% (9206 of 228,438). Additionally, given the majority of the US API population resides in metropolitan areas [3], and the CSL sampled from 15 metropolitan areas, the lived experiences of the API population in the CSL may be a good approximation of the lived experiences of the broader US API population.
These findings have implications beyond pregnancy, as GDM may increase the risk of future maternal, fetal, and childhood health risks [44], and PTB [45] and SGA [46] may increase the risk of poor developmental and physical health outcomes among offspring. Exposure to smoking and alcohol during pregnancy is associated with poor health outcomes across the lifespan [47, 48]. Furthermore, API ethnic enclaves may be protective against cancer and overall mortality risk [7, 8], suggesting the culturally relevant experience of residing in an ethnic enclave may provide benefits across the life span.
Our findings are notable for several reasons. The large amount of data available in the CSL allowed us to examine multiple pregnancy and behavior outcomes, providing consistent evidence of the potentially protective effect of residence in an ethnic enclave among pregnant API women. This is the first study to account for both ambient air pollution and area-level poverty when examining the association between residence in an ethnic enclave and health outcomes among pregnant API women. Our analysis of 15 metropolitan areas across the USA captured geographic variability not present in studies of single metropolitan areas; thus, residence in an ethnic enclave may have potentially beneficial effects for API populations across the USA.
This study should be considered in the context of its limitations. Our measure of ethnic enclaves has not been validated against other potential measures of ethnic enclaves. Given the geographic limitations of our data, our approach to measuring ethnic enclaves was informed by previous studies in an attempt to best capture the geographic and social distinctions that are unique to ethnic enclaves. Future studies are needed to validate measures of ethnic enclaves using various geographic levels and social constructs. Next, the CSL aggregates API women into a single category; thus, we were unable to examine API women by ancestry. Risk of poor pregnancy outcomes and effect of residence in an ethnic enclave may differ by ancestry [9, 14]; however, the majority of the API population in the CSL may be of Asian ancestry [16]. We do not have immigration history for women within the CSL; thus, assessment of potential acculturation is limited. The API population in the CSL is over 65% foreign born (Fig. 2), suggesting that acculturation to US health behaviors may relate to health outcomes among API women. However, the potentially protective effect of residence in ethnic enclaves suggests that women residing in ethnic enclaves may be more likely to adhere to cultural norms and health behaviors of their country of origin than women in non-enclave areas. The CSL lacks maternal residence history, limiting our ability to assess our knowledge of their length of exposure to ethnic enclaves. Most residential relocations during pregnancy occur within a similar geographic area, and cross-sectional data may allow for approximate understanding of exposure to contextual social exposures over time [49].
With electronic medical record data, potential unmeasured confounders that may increase risk of poor outcomes were unaccounted for. However, the richness of our data allowed us to control for maternal socioeconomic status, medical history, area-level poverty, and air pollution exposures associated with poor pregnancy outcomes [16, 31–33, 37, 50]. As the CSL sampled primarily from teaching hospitals, our sample may include a higher proportion of women with high-risk pregnancies. However, rates of GDM among API women in the CSL (9.7%) are lower than reported rates in the 2010 PRAMS data (16.3%) [51]. API women in the CSL had a lower rate of obesity (BMI ≥ 30) than API women in the USA [52]. The API women in the CSL may have been of similar or better health status for several reasons. First, on average, Asian adults have lower rates of obesity than Pacific Islander adults in the USA [53]. Second, evidence suggests US Asian women have better pregnancy outcomes than US Pacific Islander women [54]. Lastly, the API population of the metropolitan areas represented in the CSL is, on average, 93.4% Asian and 6.6% Pacific Islander [16].
As HRR is the geographic level of analysis in the CSL, we were unable to identify localized ethnic enclaves or spatial variation within HRRs. Identifying localized ethnic enclaves may provide a better understanding of ancestry-specific associations which is needed considering the ethnic variation within the broader US API population. However, measuring ethnic enclaves at a macro-level geography aligns with previous analyses [13, 26], includes potential ethnic enclaves that may exist outside of urban centers [26], and allows for identification of ethnic enclaves and non-enclave areas.
Conclusions
We observed decreased risk of GDM, PTB, and SGA among API women residing in API ethnic enclaves across multiple metropolitan areas in the USA. These ethnic enclaves may be socially distinct areas which allow API women better access to culturally specific resources, increased social cohesion, and reduced exposure to discrimination, leading to better pregnancy outcomes. This evidence suggests culturally appropriate social supports and resources may be an important factor to consider for health promotion among API populations in the USA. Additional research is warranted to better understand these factors among the diverse API populations in the USA.
Supplementary Material
Acknowledgments
Funding Information This research was supported by the Intramural Research Program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), including the funding for the Consortium on Safe Labor (Contract No. HHSN267200603425C) and the Air Quality and Reproductive Health Study (Contract No. HHSN275200800002I, Task Order No. HHSN27500008). This paper has been cleared for publication by the NICHD but the funding source had no role in the design, analysis, interpretation, or writing of the manuscript. The ZIP code–HRR crosswalk data was obtained from The Dartmouth Atlas, which is funded by the Robert Wood Johnson Foundation and the Dartmouth Clinical and Translational Science Institute, under the award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH).
Footnotes
Conflict of Interest The authors declare that they have no conflicts of interest.
Compliance with Ethical Standards
Data Availability Consortium on Safe Labor data is publicly available at https://dash.nichd.nih.gov/. Geographic identifying information is not publicly available; please see http://grants.nih.gov/grants/policy/data_sharing/ for National Institutes of Health data sharing policy. Census and American Community Survey data is publicly available from American Fact Finder at https://factfinder.census.gov. Dartmouth Atlas of Healthcare geographic crosswalks are publicly available at http://www.dartmouthatlas.org/tools/downloads.aspx?tab=39.
Code Availability Please contact corresponding author for the analytic file and code.
Ethical approval This article does not contain any studies with human participants performed by any of the authors. Institutional Review Boards at all sites approved the CSL, and data are anonymous.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lopez G, Ruiz N, and Patten E. Key facts about Asian Americans, a diverse and growing population Fact Tank: News in the Numbers. Pew Research Center; Washington, DC: 2017. [cited 2019 3/27/2019]; Available from: https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asianamericans/. [Google Scholar]
- 2.Bureau, U.S.C Place of birth (Asian alone) in the United States universe: Asian alone population in the United States more information 2013–2017 American Community Survey 5-year estimates. 2019; Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid = ACS_17_5YR_B06004D&prodType=table. [Google Scholar]
- 3.Bureau, U.S.C Race and Hispanic or Latino: 2010 - United States – urban/rural and inside/outside metropolitan and micropolitan area more information 2010 Census Summary File 1. 2019; Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid = DEC_10_SF1_GCTP3. US26&prodType=table. [Google Scholar]
- 4.Liu M, Geron K. Changing neighborhood: ethnic enclaves and the struggle for social justice. Soc Justice. 2008;35(2 (112)):18–35. [Google Scholar]
- 5.Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Soc Sci Med. 2009;69(1):110–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim S, Yi SS, Lundy de la Cruz N, Trinh-Shevrin C. Defining ethnic enclave and its associations with self-reported health outcomes among Asian American adults in New York city. J Immigr Minor Health. 2017;19(1):138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glaser SL, Chang ET, Clarke CA, Keegan TH, Yang J, Gomez SL. Hodgkin lymphoma incidence in ethnic enclaves in California. Leuk Lymphoma. 2015;56(12):3270–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Von Behren J, et al. The influence of neighborhood socioeconomic status and ethnic enclave on endometrial cancer mortality among Hispanics and Asian Americans/Pacific Islanders in California. Cancer Causes Control. 2018;29(9):875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janevic T, Borrell LN, Savitz DA, Echeverria SE, Rundle A. Ethnic enclaves and gestational diabetes among immigrant women in New York City. Soc Sci Med. 2014;120:180–9. [DOI] [PubMed] [Google Scholar]
- 10.Deputy NP, et al. Prevalence and changes in preexisting diabetes and gestational diabetes among women who had a live birth - United States, 2012–2016. MMWR Morb Mortal Wkly Rep 2018;67(43):1201–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kane JB, Teitler JO, Reichman NE. Ethnic enclaves and birth outcomes of immigrants from India in a diverse U.S. state. Soc Sci Med. 2018;209:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y, Luo Z, Holzman C, Liu H, Margerison CE. Paternal race/ethnicity and risk of adverse birth outcomes in the United States, 1989–2013. AIMS Public Health. 2018;5(3):312–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang TC, Shoff C, Noah AJ, Black N, Sparks CS. Racial segregation and maternal smoking during pregnancy: a multilevel analysis using the racial segregation interaction index. Soc Sci Med. 2014;107:26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickett KE, et al. Ethnic density effects on maternal and infant health in the Millennium Cohort Study. Soc Sci Med. 2009;69(10):1476–83. [DOI] [PubMed] [Google Scholar]
- 15.Grineski SE, Collins TW, Morales DX. Asian Americans and disproportionate exposure to carcinogenic hazardous air pollutants: a national study. Soc Sci Med 2017;185(Supplement C):71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams AD, Grantz KL, Zhang C, Nobles C, Sherman S, Mendola P. Ambient volatile organic compounds and racial/ethnic disparities in gestational diabetes mellitus: are Asian/Pacific Islander women at greater risk? Am J Epidemiol. 2019;188(2): 389–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ishimatsu J Spotlight on Asian American and Pacific Islander poverty: a demographic profile. Washington, DC: National Coalition for Asian Pacific American Community Development; 2013. [Google Scholar]
- 18.DAHC. Dartmouth Atlas of health care: geographic crosswalks and research files. Lebanon, NH: Dartmouth College; 2013. [Google Scholar]
- 19.Zhang J, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203(4):326.e1–326.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen G, Li J, Ying Q, Sherman S, Perkins N, Sundaram R, et al. Evaluation of observation-fused regional air quality model results for population air pollution exposure estimation. Sci Total Environ. 2014;485–486:563–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams AD, Wallace M, Nobles C, Mendola P. Racial residential segregation and racial disparities in stillbirth in the United States. Health Place. 2018;51:208–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manson S, et al. IPUMS National Historical Geographic Information System: version 12.0 [database]. Minneapolis: University of Minnesota; 2016. [Google Scholar]
- 23.ADA. Gestational diabetes mellitus. Diabetes Care. 2003;26(suppl 1):s103–5. [DOI] [PubMed] [Google Scholar]
- 24.Mannisto T, et al. Neonatal outcomes and birth weight in pregnancies complicated by maternal thyroid disease. Am J Epidemiol. 2013;178(5):731–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howland RE, Mulready-Ward C, Madsen AM, Sackoff J, Nyland-Funke M, Bombard JM, et al. Reliability of reported maternal smoking: comparing the birth certificate to maternal worksheets and prenatal and hospital medical records, New York City and Vermont, 2009. Matern Child Health J 2015;19(9):1916–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allen J, Turner E. Ethnic residential concentrations in United States metropolitan areas. Geogr Rev. 2005;95(2):267–85. [Google Scholar]
- 27.Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces. 1988;67(2):281–315. [Google Scholar]
- 28.Reardon SF, O’Sullivan D. Measures of spatial segregation. Sociol Methodol 2004;34(1):121–62. [Google Scholar]
- 29.Cohen RA. Impact of type of insurance plan on access and utilization of health care services for adults aged 18–64 years with private health insurance: United States, 2007–2008. NCHS Data Brief. 2010(28):1–8. [PubMed] [Google Scholar]
- 30.Semega JL, Fontenot KR, Kollar MA. Income and poverty in the United States: 2016, in Current Population Reports. Washington, DC: U.S. Census Bureau; 2017. p. 60–259. [Google Scholar]
- 31.Robledo CA, et al. Preconception and early pregnancy air pollution exposures and risk of gestational diabetes mellitus. Environ Res. 2015;137(Supplement C):316–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mendola P, et al. Preterm birth and air pollution: critical windows of exposure for women with asthma. J Allergy Clin Immunol. 2016;138(2):432–440.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ha S, Zhu Y, Liu D, Sherman S, Mendola P. Ambient temperature and air quality in relation to small for gestational age and term low birthweight. Environ Res. 2017;155:394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uphoff EP, Pickett KE, Crouch S, Small N, Wright J. Is ethnic density associated with health in a context of social disadvantage? Findings from the born in Bradford cohort. Ethn Health. 2016;21(2):196–213. [DOI] [PubMed] [Google Scholar]
- 35.Bhopal RS. A four-stage model explaining the higher risk of Type 2 diabetes mellitus in South Asians compared with European populations. Diabet Med. 2013;30(1):35–42. [DOI] [PubMed] [Google Scholar]
- 36.Zimmet P, Whitehouse S, Kiss J. Ethnic variability in the plasma insulin response to oral glucose in Polynesian and Micronesian subjects. Diabetes. 1979;28(7):624–8. [DOI] [PubMed] [Google Scholar]
- 37.Lorch SA, Enlow E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr Res.2015;79: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou M, Cho M. Noneconomic effects of ethnic entrepreneurship: a focused look at the Chinese and Korean enclave economies in Los Angeles. Thunderbird Int Bus Rev. 2010;52(2):83–96. [Google Scholar]
- 39.Osypuk TL, et al. Quantifying separate and unequal: racial-ethnic distributions of neighborhood poverty in Metropolitan America. Urban Aff Rev (Thousand Oaks, Calif). 2009;45(1):25–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity–related facilities and neighborhood demographic and socioeconomic characteristics: a national study. Am J Public Health. 2006;96(9):1676–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brewer M, Kimbro RT. Neighborhood context and immigrant children’s physical activity. Soc Sci Med. 2014;116:1–9. [DOI] [PubMed] [Google Scholar]
- 42.Choi JY. Negotiating old and new ways: contextualizing adapted health care-seeking behaviors of Korean immigrants in Hawaii. Ethn Health. 2013;18(4):350–66. [DOI] [PubMed] [Google Scholar]
- 43.Humes KR, Jones NA, Ramirez RR. Overview of Race and Hispanic Origin: 2010 2010 Census Briefs. US Census Bureau; Washington, DC: 2011. [cited 2019 3/15/2019]; Available from: https://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. [Google Scholar]
- 44.ACOG. Practice Bulletin No. 180: gestational diabetes mellitus. Obstet Gynecol. 2017;130(1):e17–37. [DOI] [PubMed] [Google Scholar]
- 45.Luu TM, Rehman Mian MO, Nuyt AM. Long-term impact of preterm birth: neurodevelopmental and physical health outcomes. Clin Perinatol. 2017;44(2):305–14. [DOI] [PubMed] [Google Scholar]
- 46.Hong YH, Chung S. Small for gestational age and obesity related comorbidities. Ann Pediatr Endocrinol Metab. 2018;23(1):4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kataria Y, Gaewsky L, Ellervik C. Prenatal smoking exposure and cardio-metabolic risk factors in adulthood: a general population study and a meta-analysis. Int J Obes. 2018. 43(4)763–73. [DOI] [PubMed] [Google Scholar]
- 48.Paintner A, Williams AD, Burd L. Fetal alcohol spectrum disorders– implications for child neurology, part 1: prenatal exposure and dosimetry. J Child Neurol. 2012;27(2):258–63. [DOI] [PubMed] [Google Scholar]
- 49.Osypuk TL. Invited commentary: integrating a life-course perspective and social theory to advance research on residential segregation and health. Am J Epidemiol. 2013;177(4):310–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kramer MS, Séguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14(3):194–210. [DOI] [PubMed] [Google Scholar]
- 51.DeSisto CL, Kim SY, Sharma AJ. Prevalence estimates of gestational diabetes mellitus in the United States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2007–2010. Prev Chronic Dis 2014;11:E104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fryer CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1990–1962 through 2015–2016 Health e-stats. National Center for Health Statistics Hyattsville, MD: [cited 2019 2/16/2019] Available from: https://www.cdc.gov/nchs/data/hestat/obesity_adult_15_16/obesity_adult_15_16.pdf. [Google Scholar]
- 53.Nam S. Obesity and Asian Americans in the United States: systematic literature review. Osong Public Health Res Perspect. 2013;4(4): 187–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schempf AH, Mendola P, Hamilton BE, Hayes DK, Makuc DM. Perinatal outcomes for Asian, Native Hawaiian, and other Pacific Islander mothers of single and multiple race/ethnicity: California and Hawaii, 2003–2005. Am J Public Health. 2010;100(5):877–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.