Abstract
Armed conflict leads to increased risk of emotional distress among children and adolescents, and increased exposure to significant daily stressors such as poverty and community and family violence. Unfortunately, these increased risks usually occur in the context of largely unavailable mental health services. There is growing empirical support that evidence-based treatment techniques can be adapted and delivered by non-specialists with high fidelity and effectiveness. However, in order to improve feasibility, applicability, and outcomes, appropriate cultural and contextual adaptation is essential when delivering in different settings and cultures. This paper reports the adaptation process conducted on a new World Health Organization psychological intervention—Early Adolescent Skills for Emotions (EASE)—for use in the north of Lebanon. Lebanon is a middle-income country that hosts the largest number of refugees per capita globally. We conducted: i) a scoping review of literature on mental health in Lebanon, with a focus on Syrian refugees; ii) a rapid qualitative assessment with adolescents, caregivers, community members, and health professionals; iii) cognitive interviews regarding the applicability of EASE materials; iv) a psychologist review to reach optimal and consistent Arabic translation of key terms; v) “mock sessions” of the intervention with field staff and clinical psychology experts; vi) gathering feedback from the Training of Trainers workshop, and subsequent implementation of practice sessions; and vii) gathering feedback from the Training of Facilitators workshop, and subsequent implementation of practice sessions. Several changes were implemented to the materials—some were Lebanon-specific cultural adaptations, while others were incorporated into original materials as they were considered relevant for all contexts of adversity. Overall, our experience with adaptation of the EASE program in Lebanon is promising and indicates the acceptability and feasibility of a brief, non-specialist delivered intervention for adolescents and caregivers. The study informs the wider field of global mental health in terms of opportunities and challenges of adapting and implementing low-intensity psychological interventions in settings of low resources and high adversity.
Keywords: psychological intervention, cultural adaptation, low- and middle-income countries, humanitarian emergencies, armed conflict, adolescents
Introduction
There are over 25 million refugees worldwide, around half are children, and the majority (84%) are hosted in low- and middle-income countries (LMIC) (1). Children frequently experience significant stressors and barriers to healthy development during the refugee experience, including poverty, education interruptions, exposure to traumatic events, increased family and community violence, and child protection risks (2). These experiences contribute to a greatly increased risk for poor mental health (3). Host communities in LMICs also face similar stressors, associated with living in adversity, and these stressors impact significantly on child and adolescent mental health (3).
Alongside increased mental health needs in LMICs, a vast treatment gap exists, whereby the majority of individuals needing mental health treatment do not receive minimally adequate care (4, 5). Significant barriers to providing necessary support for children and adolescents in these settings include limited financial resources (4, 6, 7) and under-resourced professional mental health workforces. In low-income countries there are less than 2 mental health professionals per 100,000 population, compared with over 70 in high-income settings (8).
Accordingly, a large body of work has considered scalable psychological interventions to overcome the barriers to providing quality mental health care in LMICs. These interventions often utilize “task-shifting”, whereby non-specialists (people without professional clinical qualifications in mental health e.g. lay counselors, nurses, primary care providers, peers) are trained and supervised to deliver services that have historically been delivered by clinical professionals (9, 10). Furthermore, they may consist of briefer and simplified versions of existing evidence-based treatments, and reduce costs via alternative formats such as group-based implementation. Rather than developing disorder-specific intervention packages, focus has shifted to developing interventions that target underlying common symptoms and processes, and that are safe and effective for individuals with a range of disorders or sub-threshold distress. There is growing empirical support that these scalable low-intensity interventions can be implemented effectively by non-specialists in LMICs (11–13). The World Health Organization (WHO) is developing and testing the effectiveness of scalable psychological interventions that can be implemented by trained and supervised non-specialists in multiple cultural contexts (10). For example, Problem Management Plus, has shown efficacy in treating psychological symptoms and distress in adults, when delivered one-to-one, and in group format (14–16).
While these findings show promise for the feasibility of delivering evidence-based approaches in varying cultural settings, appropriate consideration of cultural factors is essential (17). There is evidence that culturally adapted treatments are more effective than non-adapted treatments (18–20). Although one recent meta-analysis of psychological interventions for depression in LMICs found no significant difference between adapted and non-adapted therapies (21), another meta-analysis of minimally guided treatments for depression found that treatment effects increased with additional cultural adaptations made (20). A barrier to adequately evaluating the empirical support for the process of cultural adaptation, is that the majority trials of psychological interventions in LMICs do not comprehensively outline adaptations made (22). Cultural adaptation commonly involves systematic modification of interventions and training materials to consider language, culture, and context, with the goal of ensuring that it is compatible with the client’s cultural patterns, meanings, and values (23). In order to maintain fidelity to the evidence-based treatment, it is generally recommended that the core intervention components are maintained, while other changes can be made to improve “fit,” in terms of acceptability, comprehensibility, relevance, and completeness (23). In a review of cultural adaptations of treatments for depression, Chowdhary and colleagues (24) found that the most common adaptations were made to language, context, and the person delivering the treatment, rather than to core intervention content.
War Child Holland is conducting an evaluation of a new potentially scalable intervention developed by the WHO, Early Adolescent Skills for Emotions (EASE), in Lebanon. Simultaneously it is being evaluated in three other sites: Tanzania, Pakistan, and Jordan. In Lebanon, the evaluation is part of the STRENGTHS project, that evaluates community-based mental health care implementation strategies to address the psychological needs of Syrian refugees in eight countries (25).
In this paper, we outline the process and results of formative research undertaken to culturally and contextually adapt the EASE intervention for use in the north of Lebanon. By sharing the lessons learned, we aim to contribute to a greater understanding of necessary considerations when adapting psychosocial interventions for use in new settings.
Methods
Setting
Lebanon, a middle-income country, has historically experienced significant conflicts, including a civil war from 1975 to 1990, the Hezbollah–Israel war in 2006, and internal conflicts. Additionally, Lebanon now hosts the highest number of refugees per capita globally—with an estimated 1.5 million Syrian refugees, plus large numbers of Palestinian refugees, and vulnerable Lebanese, from a total national population of 5.9 million (1, 26). As a result, there are significant challenges of limited basic infrastructure and the ability to meet educational, health, financial, and mental health needs of the entire population (26). It is estimated that over half of the individuals affected by the Syrian crisis are children; and approximately 1.4 million children in Lebanon are currently growing up at risk, with urgent unmet needs for basic services and protection (26). Most recent estimates indicate only 1.26 psychiatrists and 3.42 psychologists per 100,000 population, with only 3% working in the government sector, making mental health care often inaccessible to the most vulnerable (27).
We conducted our cultural adaptation process in the North governorate, mainly in two vulnerable areas—Beb el Tebbeneh and Hay el Tanak. These were selected as representative areas, given the high vulnerability, and a mix of cultural groups (e.g. Syrian, Lebanese, and Palestinian). When considering cultural and contextual adaptations for psychological interventions in Lebanon, it is important to note that there are vast cultural and contextual differences among different regions of Lebanon including wide variations in income, living conditions, type and opportunities of employment, religion, language, and attitudes toward mental health and associated interventions. Therefore, results of this adaptation process cannot be assumed to be nationally representative.
Intervention
EASE was developed to address internalizing problems (e.g. depression or anxiety symptoms) in 10- to 14-year-olds living in adversity (28). It consists of seven 90-min group-based sessions for adolescents focusing on four key empirically-supported strategies: understanding my feelings (emotion identification), calming my body (diaphragmatic breathing), changing my actions (behavioral activation), and solving my problems (problem solving). Additionally, three adjunctive caregiver sessions (initially developed to be 120 min each) aim to promote positive parenting practices to improve the caregiver–child relationship and enhance confidence when responding to adolescent distress. Intervention materials consist of: i) facilitator manual for delivering the sessions, ii) workbook for each adolescent to complete individual activities and home practice, iii) storybook to illustrate key concepts, iv) posters for adolescent sessions, and v) caregiver hand-outs.
Process
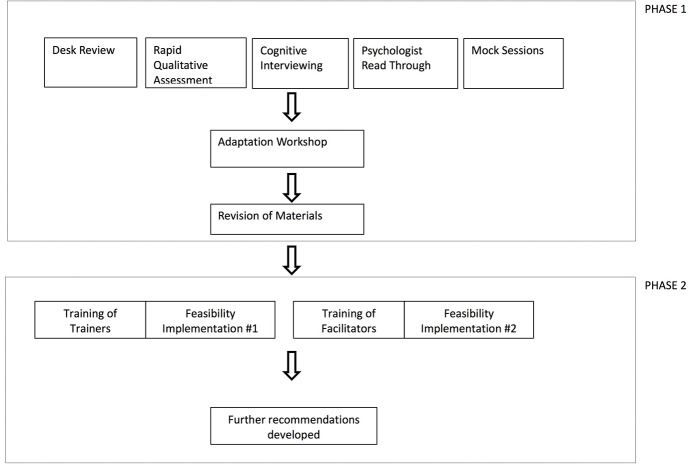
We followed an iterative adaptation process based on an internal WHO draft guidance on cultural adaptation of scalable psychological interventions (available on request), which draws from various resources (23, 29, 30). In the first phase, we conducted: i) literature reviews on mental health in Lebanon, with a focus on Syrian refugees; ii) a rapid qualitative assessment (RQA) with adolescents, caregivers, community members, and health professionals in Lebanon; iii) cognitive interviewing with EASE materials; iv) a psychologist Arabic read-through to reach optimal and consistent translation of key terms; and v) “mock sessions” of the intervention with field staff and clinical psychology experts. In an adaptation workshop, data from each of the five steps was reviewed to decide on necessary adaptations. Changes to materials were proposed to developers at WHO, and changes in line with the intervention model were implemented accordingly. The second phase involved: i) gathering data from the Training of Trainers workshop, and associated implementation of practice sessions; and ii) gathering data from the Training of Facilitators workshop, and associated implementation of practice sessions. Several recommendations were developed for further adaptations. This process is depicted in Figure 1. Ethical approval was obtained from Saint Joseph’s University, Beirut (USJ-2017-24).
Figure 1.
The adaptation process for Early Adolescent Skills for Emotions (EASE) in Lebanon.
Phase 1—Formative Research
Scoping Review of Literature
In order to learn from existing relevant literature, a two-part non-structured desk review was conducted. One part encompassed reviewing: i) an internal desk review conducted by partners in the STRENGTHS research consortium (available on request), investigating mental health of Syrian refugees in the Middle-East and Europe; ii) existing, known desk reviews pertaining to Syrian child and adolescent mental health (31, 32); and iii) recent internal needs assessments carried out by War Child in Lebanon, not specific to Syrian refugees. The other part took place after the RQA (described below), and further explored common issues identified in the assessment, via a non-structured literature search.
Rapid Qualitative Assessment
The aims of the RQA were to: i) understand all problems experienced by the community; ii) give insight into how problems related to mental health are expressed locally; iii) explore coping methods commonly used by adolescents, and community coping mechanisms; iv) explore awareness and communication around mental health in the community; v) map available mental health services; and vi) receive input on the planned EASE intervention delivery. The RQA took place in community centers where War Child Holland was implementing education activities.
First, free-listing interviews (29) were conducted with 11 adolescents (aged 10 to 14 years; 8 female, 3 male; 5 Syrian, 6 Lebanese), and 13 caregivers (12 female, 1 male; 4 Syrian, 9 Lebanese), invited through the community center coordinators, who were instructed to find a mixed gender sample that represented the wider community. Trained research assistants asked participants to provide information on the research question “What are all the problems that affect children and adolescents in this community?” with several probes to follow up. Responses were tallied, and the most commonly reported problems that were potentially able to be addressed via a psychological intervention, were then explored further through semi-structured interviews with different participants.
Semi-structured interviews were conducted in the format of four focus group discussions with adolescents (age 10–14, n = 15; 8 female, 7 male; 11 Syrian, 4 Lebanese); and individual key informant interviews with adolescents (age 10–14, n = 7; 3 female, 4 male; 5 Syrian, 4 Lebanese, 1 Palestinian), caregivers (n = 9; all female; 4 Syrian, 4 Lebanese, 1 Syrian-Lebanese), community members (n = 4; one community center director, one education officer, one football academy leader, and one other respected community member), and health care providers (n = 3; clinical psychologist and psychotherapist, psychologist, and social worker). The adolescents, caregiver, and community members were a purposive sample selected by community center coordinators to be either representative of the community (adolescents and caregivers) or knowledgeable about the mental health and psychosocial concerns within the community (community members). The mental health care providers were invited through sector networks in the region. Adolescent participants provided informed assent to participate and their caregivers provided informed written consent. Adult participants gave informed written consent to participate.
Interviews were audio recorded, and interviewers also took detailed notes. Interviews were transcribed verbatim and translated into English via a professional translator. At least 10% of transcripts were checked for quality and accuracy by a bilingual team member (KT). The data were analyzed through inductive thematic analysis to determine main themes and illustrative quotes (33). The results are reported in full elsewhere, but pertinent findings are reported here.
Cognitive Interviewing
The aim of the cognitive interviewing exercise was to ensure that materials were easily understood, acceptable, and relevant to the population. Two groups of adolescents (n = 8) and two groups of caregivers (n = 8) were shown the Arabic intervention materials and asked questions about whether they were relevant, understandable, and acceptable, following a semi-structured guide. The materials shown were key intervention components, which were purposefully selected to include components hypothesized by the local team to be less understandable, acceptable, or relevant in Lebanon—talking to young people about suicide, the choice of activity in the story book of “bird watching,” and the explanation of the “Tired Cycle” of behavioral inactivation due to low mood. Data was collated per concept.
Psychologist Read-Through
The purpose of the read-through was to ensure consistency, accuracy, and appropriateness of Arabic wording and idioms. The manual was translated to a formal, yet simple, Arabic in order to be understood by Lebanese, Syrians, and Palestinians. Staff from War Child Holland (three psychosocial trainers, the regional psychosocial advisor, and the research coordinator) read through materials and discussed any translation issues together. An existing glossary of mental health idioms and terminology used by Syrians was used as a reference (31).
Mock Sessions
Mock sessions were conducted via live role-plays, to allow identification of any further necessary adaptations. Attendees included: three psychosocial trainers from Lebanon, the regional psychosocial advisor, three non-Lebanese psychologists, and two non-Lebanese researchers. Each session was role-played, followed by a discussion of comprehensibility, acceptance, completeness, and relevance. This was an addition to the WHO guidance, and recommended based on field experiences indicating that this would provide substantive suggestions for changes (34).
Adaptation Workshop
A 2-day adaptation workshop was attended by representatives from organizations involved in the STRENGTHS consortium. The aim of the workshop was to review all data from Phase 1, and determine recommendations for adaptations. Recommendations were compiled for suggested adaptations to the intervention materials, training materials, or implementation considerations, and were coded according to the Bernal framework for cultural adaptation of psychological interventions (23).
Phase 2—Implementation Data
Training of Trainers and Practice Cycle
An 8-day Training of Trainers workshop was held for two trainers from Lebanon (both psychologists). Three master trainers (MA, AM, FB) conducted the training, one of which (MA) is a psychologist from Lebanon.
The two trainers and one master-trainer (MA) each conducted a supervised “practice cycle” to prepare themselves to train and supervise non-specialists in the intervention. This involved delivering the EASE intervention to three groups: one group of females (n = 7), one group of males (n = 7), and one mixed group (n = 5; 3 boys, 2 girls). Adolescents were of mixed nationalities, including Lebanese, Syrian, and Palestinian. Qualitative feedback was gathered from the trainers via session notes, supervision notes, and a debrief session at the end of the implementation.
Training of Facilitators and Practice Cycle
Two separate trainings were held with facilitators. Training was 9 days, and followed the EASE Training of Facilitators manual. It was followed by a supervised practice cycle implementation, whereby facilitators delivered the intervention to a small number of adolescents. The first training was attended by eight facilitators, with six continuing to the practice cycles. The second training involved nine facilitators, with seven continuing to practice cycles. The non-specialist facilitators did not have any formal mental health qualifications, but all had previous group facilitation experience with children or adults.
During the two supervised practice cycles, 13 facilitators implemented the EASE intervention with a total of 37 adolescents aged 10 to 14 years old, in seven groups (group sizes ranging from 3 to 11 adolescents). Adolescents were not selected specifically for high levels of distress, given that this was the first time the program had been implemented by non-specialists in Lebanon. Facilitators collected attendance data, and completed self-report fidelity checklists of the major components of the sessions, including duration.
Trainers conducted 10 structured observations in total, whereby they rated facilitators on fidelity and competency, using a standardized observation tool developed specifically for EASE (35). Facilitators were rated on whether they completed each component of the session (yes or no), on how well they delivered each section of the session (done well, done partially, needs improvement), and two general competency items which assessed the use of group facilitation skills, and basic helping skills (done well, done partially, needs improvement). Two additional competency items were to be rated if they were applicable—managing an acutely distressed participant, and demonstrating basic safety skills—however these did not arise during any of the observations. Informal qualitative feedback was collected from adolescents, caregivers, and facilitators.
Results
Phase 1—Formative Research
Scoping Review of Literature
Our review highlighted that conflict-affected Syrians experience a wide range of mental health problems including newly emerged mental health conditions caused by conflict-related experiences, as well as issues related to living conditions (31). Children and adolescents report war-related anxiety, worries about the future, and other emotional distress including grief, frustration and hopelessness (31, 32, 36, 37). Several barriers to accessing health care exist, including language barriers, stigma, and perceived power-dynamics in the therapeutic relationship (31, 32, 36). Children and adolescents experience high rates of family violence, contributing to emotional distress (36). Furthermore, high rates of substance use among adolescents are reported (36, 37). A pervasive daily stressor is poverty, and this is known to affect many other aspects of child and adolescent well-being, including lack of basic needs, poor attendance at school, child labor, substance use, and criminal activity (31, 32, 36, 37). In Lebanon, 70% of Syrian refugees live below the poverty line (26) and reports indicate that poverty and associated experiences can exacerbate hopelessness and frustration, and pre-existing mental health concerns (31, 36). Needs assessments conducted in Lebanon by War Child Holland confirm these findings and highlight the importance of interventions targeting the specific mental health and psychosocial needs of vulnerable populations in Lebanon.
Rapid Qualitative Assessment
The most common concerns reported through free listing, that were considered potentially viable to be addressed in a psychological intervention, were: i) physical violence and abuse (among children and adolescents, and from caregivers or teachers toward children and adolescents); ii) neglect and emotional abuse from parents; iii) emotional abuse among children and adolescents (primarily bullying and teasing); and iv) substance use (alcohol, tobacco, and other drugs) among children and adolescents. The framework analysis resulted in seven themes, which are presented in Table 1.
Table 1.
Findings From the Rapid Qualitative Assessment in Lebanon.
| Theme | Key findings | Quote |
|---|---|---|
| 1. Emotional abuse, bullying, and physical violence |
|
Of course, emotional abuse. There is no tenderness from the mother, there is beating from the father, there is domination from the brother … What would all this do to the child? (Community member, female, Lebanese) |
| 2. Substance use |
|
I mean there is smoking. You feel like there is smoking. You find many people are … I mean I know a kid who is now 14 years old and he smokes, and he has been smoking for about 5 years. I mean it’s not recent. (Mother, Syrian) One of its causes is that there are young people who did not continue their studies, they dropped out of school and they have no job, they live in an area where there are no jobs, and they are not studying … one of its results is that they have no money, they become jobless, they drink and do drugs, they behave badly, not to mention that they might also steal. (Community member, female, Lebanese) |
| 3. Poverty |
|
Yes, it’s true. We have children in school who are no longer in school because their father is not present, and they can’t, so their mother stopped sending them to school, boys in our class, and now they work. (FGD girls, Syrian) |
| 4. Other problems reported |
|
… I am telling you I now have a complex from the word “That Syrian” and “Those Syrians,” as if “those” are stupid animals, and you don’t feel like a Syrian. We don’t feel like it is a nationality anymore. (Mother, Syrian) |
| 5. Community awareness of mental health and coping mechanisms |
|
They talk to their friends and parents the most, but they don’t talk to a hospital, and there are no such centers here (Boy, Lebanese) |
| 6. Mental health service mapping |
|
I mean, they need more than just a session, they need more. I mean, more than just a referral to an association that may or may not help them. There are many lacking services. (Service provider, female, Lebanese) |
| 7. Input on Early Adolescent Skills for Emotions implementation strategies |
|
So, we used to check … we used to ask them about the timing of their school, or if they studied in centres, or if they worked … such things. (Service provider, female, Lebanese) |
Cognitive Interviewing
Results of the cognitive interviewing indicated that the content was relevant and comprehensible, and the language was simple and easy to understand. Importantly, several findings informed intervention delivery. Adolescents commonly endorsed that psychosocial problems occurred for friends or neighbors, rather than reporting that these problems occurred in their own life. The local team perceived this to be due to a cultural expectation that events occurring within the family home should not be discussed with others. Furthermore, thorough explanation of the EASE strategies was required in order for adolescents to fully grasp them. For the Tired Cycle in particular, explanation on the linkages between mood and behaviors, and the directional nature of the cycle needed to be expanded.
Caregivers were talkative and liked the opportunity to share experiences. Caregivers were worried that suicide would be discussed with their children, as this was perceived to increase the risk of suicide. When they were asked if it is acceptable to talk about suicide, one caregiver said: “With the parents yes, but with the child, no.” Another caregiver further explained: “No because the child will have this idea in their head and they will want to do it!” This highlighted the need for thorough explanation about the reasons for discussing suicide with young people. Physical punishment was openly discussed by caregivers, and reportedly very common, with many stating that it was necessary because they had no other options. Additionally, caregivers recognized the need for taking care of themselves, but found it hard to implement. This highlighted that discussing these topics would be suitable in the intervention, but with sensitivity.
Psychologist Read-Through
The language of the EASE materials was generally perceived to be understandable, and several revisions were made for consistency, accuracy, and simplifying terminology. One example was a change in the word for “emotional problems” in Arabic from “mashakel 3atifiah” (i.e. emotional problems) to “mashakel nafsiah” (i.e. psychological problems), as the first had connotations of “romantic problems.” Furthermore, the concept of suicidality was introduced via a culturally appropriate phrase: “Sometimes people have thoughts that their life is not worth living or they wish they would fall asleep and not wake up.”
Mock Sessions
Overall the experience of the mock sessions indicated that the content and ideas were largely relevant, acceptable, and understandable in the Lebanese context. Several suggested edits to the original version were identified, to improve facilitators’ ease of use of the manual and increase participant engagement more generally across all contexts. Furthermore, several cultural adaptations were identified for use in Lebanon.
Adaptation Workshop
All recommendations for changes from the previous five steps were summarized and discussed, and the changes implemented are shown in Table 2. One substantial change to EASE content was adapting the “Tired Cycle” for behavior activation, which previously focused on the inactivity associated with depression. Given the critical prevalence and impact of aggression and violence in the communities, this was adapted to the “Vicious Cycle,” with examples provided for how behavioral cycles can also work to maintain anxiety and anger, and prevent engagement in personally valued activities.
Table 2.
Adaptations Made in Phase 1 for Early Adolescent Skills for Emotions (EASE) Materials and Implementation in Lebanon (Coded by Bernal Framework).
| Adaptation Principle | Change implemented to EASE | Information/Rationale | Source |
|---|---|---|---|
| LANGUAGE | |||
| Translation into local language |
|
Consistency will enhance understanding. | Mock Read |
| Use of local idioms |
|
Ensures that materials are accessible and easily understood by participants. | Read |
| Technical terms replaced by colloquialisms |
|
These terms were identified as most relatable and appropriate in the context, especially given the stigma around mental health interventions. There is stigma and suspicion around mental health services, and a belief that it is better treated within the community. |
Mock Read |
| PEOPLE | |||
| Therapist-patient matching |
|
Traditions of gender segregation are common. | RQA |
| Cultural competency of therapists |
|
It is important that they are well respected, especially given stigma, and reported distrust of NGOs and health services. Adolescents do not often discuss what happens at home outside the home, and often report that these things happen to “other people” |
RQA CI |
| Therapist–patient relationship |
|
Caregivers enjoyed the opportunity to speak about their concerns. Due to stigma, need to ensure confidentiality of adolescent sessions and ensure they are comfortable to disclose issues. |
Mock CI |
| METAPHORS | |||
| Use of material with cultural relevance | Several changes were made to the story to increase cultural relevance.
|
Some aspects of the story were not culturally appropriate. Some adaptations made to increase sensitivity to experiences in this context. |
|
| Use of idioms/symbols |
|
Some adolescents may not related to these, some adolescents may not associate only “bright” colors with being happy. | Mock |
| CONTENT | |||
| Incorporation of local practices into treatment |
|
Encouraging adolescents to point out others’ mistakes is not appropriate in this context. Physical punishment is common in this context, and it is not advisable to tell parents that it is not acceptable, without also including alternative discipline methods. Celebrations are customary in the context. |
Mock CI |
| Addition of therapy modules to address cultural factors |
|
Grief, abuse, and substance use are common. They are not addressed anywhere specifically in the manual. Children are not used to discussing their emotions, and need some time and introductory activities to feel comfortable. |
Mock Lit RQA |
| Addressing stressors | Incorporated anger/externalizing problems and aggression throughout. For example:
|
Physical violence, anger, aggression, and bullying are common problems. We heard examples of negative coping mechanisms in the RQA, but understanding of mental health concerns is lacking, and there are high levels of stigma. |
Mock RQA Lit |
| GOALS | |||
| Client derived goals |
|
Poverty and crowded living spaces are pervasive, and children may already be working, therefore suitable enjoyable or meaningful activities may vary. Children have many problems, and many of them are out of their control. |
RQA Mock |
| Clarifying goals |
|
Coping strategies may vary in the context. Need to consider and encourage broader coping strategies. | RQA Mock |
| METHODS | |||
| Adaptation of training and supervision methods |
|
Facilitators will be non-specialist and will therefore need more detailed training. Facilitators need core understanding and knowledge of children’s well-being and positive parenting. Abuse is common in the community. Parents were very talkative in formative research, and liked the chance to share experiences. |
Mock RQA CI |
| Client engagement adaptations |
|
In this context, adolescents often do not have space to play and do not attend school. Externalizing problems are also common. Therefore keeping sessions active will increase engagement. Inclusion of interactive group activities will also reduce the individual focus, and broaden the concepts to cover social interactions which are important in this context. Consideration of gender is needed. The children and caregivers will have low literacy and education, and likely will have trouble engaging with lengthy sessions if they are didactic. Concepts should be presented as simply as possible. |
RQA CI Lit Mock |
| Structural adaptations | Scheduling needs to be around school activities, and prayer times. | ||
| Adaptation to techniques used to deliver treatment |
|
This should be added to end the sessions positively. The story telling element should be strengthened in the story. The amount of homework builds up from each session, so that at the end the child is doing many different things, which will likely be too much for children in this context. |
|
| CONTEXT | |||
| Increase accessibility and ensure feasibility |
|
Poverty is pervasive and families are often large, and living in crowded spaces. One-on-one quality time for lengthy periods is unlikely to be possible. In the RQA, intergroup tensions were identified, as well as mistrust of NGOs, and belief that problems are best dealt with by community. Families have many children, and experience poverty, therefore childcare is likely to be a barrier for caregiver attendance. |
Mock RQA Lit |
| Ensure acceptability |
|
Parents may be worried about us talking to children about suicide, when suicide is raised in parent session. Parents say that it’s acceptable to talk about, but worry that might be danger for children. Suicide is a sensitive topic as it is taboo, therefore there needs to be a good link to starting the discussion on suicide. Need to be sensitive to issues of poverty and food shortages. |
Mock CI RQA Lit |
| SECURITY | |||
| Specific adaptation relating to conflict-affected setting |
|
Vulnerable areas in Lebanon are unpredictable in terms of security concerns. | Mock RQA |
Mock, mock sessions; RQA, rapid qualitative assessment; CI, cognitive interviewing; Lit, scoping literature review; Read, read through.
Translation of Revised Materials
Professional translators translated the revised materials into English. We intended to translate the storybook into simplified, local language. However, based on feedback from trainers and facilitators, it was translated to simple, yet formal written Arabic, and facilitators could adapt the language during delivery. The glossary of key terms in Arabic for EASE, plus common terms for idioms of distress in Syrian Arabic, were provided to facilitators and they were encouraged to use them in their delivery of sessions as appropriate.
Phase 2—Implementation Data
Training of Trainers and Practice Cycles
Through this implementation, it was determined that separation of groups by gender (as recommended by the EASE manual) is beneficial to promote comfort and openness. Similarly siblings and relatives should be separated, where possible, to prevent reticence when discussing personal details. Further, it was determined that the presence of a male facilitator (alongside a female facilitator) was accepted by female adolescents. Significant behavior problems (for example leaving the classroom, and bullying) were experienced in the male group, such that the group was discontinued and individual support provided to interested adolescents. This supports the RQA findings that externalizing problems are salient in this population, and highlights the importance of training facilitators in additional behavioral management strategies in Lebanon. Specific feedback and recommendations for future adaptations to the intervention and implementation are collated in Table 3.
Table 3.
Feedback gathered from Training of Facilitators and Training of Trainers practice cycles and recommendations for further adaptations to Early Adolescent Skills for Emotions materials and implementation in Lebanon.
| Implementation considerations | ||
|---|---|---|
| Topic | Information | Recommendation for implementation in this setting |
| Literacy |
|
|
| More interaction and active learning |
|
|
| Addressing suicide |
|
|
| Confidentiality |
|
|
| Referrals |
|
|
| Group management and behavior management |
|
|
| Simplification of manual |
|
|
| Poor attendance |
|
|
| Session length |
|
|
| Comfort around discussion of emotions |
|
|
| Homework challenges |
|
|
| Requests for celebration |
|
|
| Group compositions |
|
|
| Delivery of specific strategies |
|
|
Training of Facilitators and Practice Cycles
On average, session duration was between 1.5 and 2 h. Attendance was variable, particularly for later children and caregivers sessions, ranging between an average of 53% and 89% per session. Facilitator-reported fidelity to the major components of the intervention was generally high, with low-fidelity reported for some specific sessions, sometimes due to the shortening of session time due to practical issues, or only one participant attending and therefore some group activities not being completed.
Trainer-observed fidelity was slightly lower, however overall, most facilitators were implementing the majority of the components in most sessions. Some items were not completed due to lack of time. Competency ratings for delivery of EASE content were rated high, and the majority of ratings on the core competencies of group facilitation and basic helping skills were the highest possible score.
Facilitators gathered and documented feedback from adolescents and caregivers at the end of the program. Overall, feedback was positive. Adolescents found the problem-solving strategy (managing my problems) most useful, and were commonly practicing diaphragmatic breathing. Some adolescents could not personally relate to the vicious cycle, which described the link between mood and detrimental behavior patterns that took them away from meaningful activities. In cases where children could not identify meaningful activities that were being impacted, facilitators asked children to use the behavioral activation strategy (changing my actions) to increase pleasurable activities, or improve everyday planning. Caregivers reported finding the diaphragmatic breathing strategy, and the exercise about caregiver strengths useful and felt that they were using more supportive and less harsh parenting techniques. Caregivers reported challenges around the implementation of quality time, given the large family sizes and time limitations and facilitators handled this as specified in the manual in terms of emphasizing brief moments. Specific feedback and recommendations for future adaptation to be implemented by WHO, are collated in Table 3.
Discussion
The aim of this study was to culturally and contextually adapt the EASE program for young adolescents in the north of Lebanon. We conducted a scoping review of the literature, RQA, cognitive interviewing, psychologist read-through, and mock sessions, and gathered data and feedback during training and practice cycles. Based on the findings, we made several minor and several more substantial adaptations to the materials and implementation methods.
Our study lends support to the utility of conducting a careful and rigorous adaptation process before delivering an intervention in a new setting. We identified several important adaptations to key components of EASE that enhanced relevance and completeness in addressing the common experiences of adolescents in this community. First, the most substantial change to content of adolescent EASE sessions was the incorporation of examples of anger and bullying throughout the materials, given the high prevalence and impact. This notably included adapting the inactivity cycle of depression, to the broader “vicious cycle” which incorporates processes maintaining a spectrum of emotional distress behaviors (including anger and anxiety). Behavior activation is considered to be an effective and cost-effective technique suitable for wide-scale dissemination by non-specialists (38). However, while the strategy is commonly used to address inactivity associated with depressed mood, it has been previously noted that expanding the focus away from depressed mood and toward encompassing a broader concept of maladaptive behavior patterns interfering with valued activities, may reduce the impact of stigma related to depression, and increase cross-cultural applicability and relevance (39). This is in line with evidence that presentations of depression symptoms vary in different cultural contexts, and also in populations exposed to trauma (40). It also corresponds to adaptations made to an online psychological intervention for adults in Lebanon, where the focus was shifted away from inactivity as a symptom of depressed mood, with emphasis instead on increasing pleasurable activities to lift mood (41). Second, given the number and intensity of problems faced by adolescents in this context, with many outside the adolescents’ personal control (e.g. poverty, community violence), facilitators were required to more actively support adolescents to identify and prioritize appropriate problems for the problem-solving strategy. Third, the most significant change to the caregiver EASE content was the consideration of large families and limited physical space for the quality time strategy. Facilitators encouraged parents to keep quality time brief, and to accommodate for times where other siblings will also be present, by ensuring that individual attention is provided to each child. Fourth, given parents’ low literacy and education background, the amount of session content was reduced in order to retain only the key strategies and concepts.
Several changes were also recommended for session delivery. Given that adolescents often had a lack of opportunity for active play, and often had interruptions to schooling which meant that they were not accustomed to attending for long periods, there was a need for activities to be more physically active and interactive in order to maintain focus and engagement. Specific guidance should be given for facilitators on setting up group rules, and coaching children in group and pair work. Similarly for caregivers, it was recommended to increase interaction and reduce didactic presentations.
The types of adaptations made for EASE, are similar to adaptations made in other cultural adaptations in the mental health field. A recent systematic review of depression interventions for adults found that the most commonly adapted components were related to: language, facilitator, and context (24). EASE content was already simplified with non-specialists in mind, however gender matching of facilitators was carefully considered. Additional training for non-specialist providers was developed, covering topics of behavior management, and responding to disclosure of grief, substance use, and abuse. Significant adaptations were made based on context, including considerations around requirement of resources such as colored pencils, balloons, and costumes.
Based on our experiences, we provide several key recommendations for the process of cultural and contextual adaptation of psychological interventions. Firstly, when developing psychological interventions for use across contexts, material should consider low literacy and education levels of participants, low resources available, and non-specialist training of providers. Additionally, while materials will never be devoid of culture, several features can be incorporated to enable easier adaptation in new contexts, including: i) explicit mention of origin of materials including evidence for the use of each strategy; ii) specification of discrete sections that will likely need cultural adaptation (e.g. case stories that can be easily replaced); or iii) developing materials such that they are relevant in several different cultural contexts (e.g. key characters and illustrations used in the material are gender-neutral, age-ambivalent, without culturally important details that are not significant for the message that is being conveyed). Secondly, the mock sessions gleaned numerous useful suggestions for cultural adaptation as well as improvement of materials more broadly, and therefore are recommended as an important and cost-effective step, prior to training of facilitators and translation of final products.
We experienced several significant challenges during the adaptation process. Foremost, we had challenges relating to using formal written Arabic compared to colloquial versions. Initially we intended to translate materials into simplified and more local language, however facilitators reported a unanimous preference to receive the materials in simple, formal written Arabic, and would adapt the language during delivery to suit participants. Some facilitators were Lebanese and others were Syrian, while many of the adolescents in the program were Syrian. Therefore, exact matching of accent and colloquial terms used between facilitator and adolescents was not achievable. It is important to further note that Arabic dialects vary by region and by socio-economic status in Lebanon. Future work in Lebanon should aim to engage bilingual individuals with a strong mental health background as well as extensive knowledge of local languages, in order to optimally adapt terminology to be understood by facilitators, adolescents, and caregivers in these diverse communities.
One of our major challenges, relating to uptake and attendance at sessions, was scheduling implementation of EASE sessions around school and work commitments. The Ministry of Education and Higher Education in Lebanon has implemented double-shift schools in Lebanon, in a response to vastly increased numbers of school-age children and adolescents following the Syrian crisis, meaning that children were attending school at different times of the day. Additionally, high rates of child labor presented a significant challenge for attendance. Unfortunately, literature indicates that child labor is a risk factor for increased psychological distress and other protection needs (3). Our experience supports a need for integrated multi-sector programming that includes efforts to reduce child labor within communities, as well as providing multiple options for mental health services, to ensure that the most vulnerable children and adolescents are being reached. This may include flexible one-to-one sessions for those that cannot attend group sessions, or online or telephone options. A group format was selected for EASE in order to reduce resources needed for delivery and increase coverage, however future implementation research should evaluate cost-effectiveness, taking into account attendance rates in different settings, and the likely consequent attenuated impact associated with poorer attendance.
Our experience during the adaptation process conducted for EASE elucidates a core dilemma in delivering culturally sensitive treatments. On the one hand, there are significant cost-benefits and quality assurance advantages to maintaining core base materials for scalable interventions, which can be readily adapted to new contexts and cultures, and this may be a pre-requisite for replication of evidence-based treatments. Furthermore, developing consistent core intervention materials for use across various contexts, more readily enables development of global training and supervision networks, and effective integration of improvements and lessons learned from different settings. On the other hand, Kirmayer (17) argues that the evidence underlying evidence-based treatments is grounded in particular cultural assumptions that are deeply embedded in our diagnostic frameworks, interventions, and measured outcomes, and therefore does not adequately address cultural diversity. From this view, a more ground-up approach may be preferable for optimally incorporating cultural understandings and processes of illness and healing into our practice (17, 42). Rousseau and Kirmayer (42) caution against attributing the efficacy of culturally adapted treatments solely to the underlying psychotherapeutic framework, and instead encourage evaluation of the added cultural elements as explicit active ingredients for change themselves.
The EASE intervention was developed primarily for internalizing symptoms of depression and anxiety, and therefore during our adaptation process there was limited scope to add alternative strategies or significant focus on the problems reported during our formative work in vulnerable communities in Lebanon (e.g. significant prevalence of externalizing symptoms). Conversely, there is significant comorbidity between externalizing and internalizing problems, and increasing evidence for transdiagnostic approaches to address both (43). In the Lebanon context, where externalizing problems may be prominent, it will be important to understand the impact of the transdiagnostic components in EASE on both externalizing and internalizing symptoms. An additional key recommendation for future implementation and research is that early formative work in a new setting (including literature reviews and RQAs) should be conducted prior to selecting or developing new interventions to adapt and apply, based on identified context-specific priorities and understandings. It is imperative that flexible funding structures allow for such careful cultural enquiry prior to the selection of evidence-based approaches to implement.
Overall, our experience with adaptation of the EASE program in the north of Lebanon is promising and indicates the suitability of a brief, non-specialist delivered intervention for adolescents and caregivers. The research informs the wider field of global mental health in terms of opportunities and challenges of implementing psychological interventions in diverse settings of low resources and high adversity, and the potential to contribute to closing the global treatment gap (4). Child and adolescent mental health continues to be an area lacking sufficient attention, especially in under-resourced settings (7), and the results of this formative work, and forthcoming pilot trial and randomized controlled trial will provide further evidence on effective strategies to address this global issue (35).
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved. Ethical approval was obtained from Saint Joseph’s University, Beirut (USJ-2017-24). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
The overall process for the adaptation of EASE was designed by FB and MJ, with contributions from all authors. FS, MB, and PH contributed to the Desk Review. The Rapid Qualitative Assessment was overseen by FB and MJ, with FB and FS responsible for training research assistants, FS and KT responsible for data collection, FS contributing to data analysis alongside a master’s student, and field support provided by MA. The cognitive interviewing was overseen by FB and MJ, with KT responsible for data collection and analysis, and support provided by MA and FS. The psychologist read-through was coordinated by KT, with support from MA, and other staff members. Mock sessions were coordinated by FB; were conducted by FB, MA, AM, and PH; and attended by FS, KT, and MB. The adaptation workshop was coordinated by FB, and attended by MA, AM, PH, MB, MJ, FS, KT, and RC. Several authors (AM, KD, SW, FB, MA, PH) contributed to edits to materials, with WHO technical staff in Geneva providing the final sign-off. Training of Trainers (TOT) was conducted by MA, FB, and AM. MA and two other trainers implemented TOT practice cycles and shared valuable feedback. TOF was conducted by MA, and two trainers. MA and FB were responsible for supervision and collecting all field data and recommendations from the TOF practice cycle, with support from trainers and KT. MA, FB, and AM provided “master supervision” and collected feedback throughout. MS led the development of the overall STRENGTHS consortium plan, including cultural adaptation components. All authors critically reviewed and approved the manuscript for publication.
Funding
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 73337.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to foremost acknowledge the families, community members, professionals, community center staff, War Child Holland staff, and facilitators that took part in and supported our research activities and practice cycles—their time, effort, and feedback was invaluable in improving our services for vulnerable adolescents in Lebanon. Furthermore we would like to thank the EASE team at World Health Organization, led by Mark van Ommeren and Chiara Servili, for providing the EASE materials, leading the adaptations based on recommendations, and providing technical input to our project. We would like to thank all members of the STRENGTHS consortium for collegial support and input to the process. The STRENGTHS project is funded under Horizon 2020—the Framework Programme for Research and Innovation (2014-2020). The content of this article/poster/etcetera reflects only the authors’ views and the European Community is not liable for any use that may be made of the information contained therein.
References
- 1. UNHCR Global trends forced displacement in 2018. Geneva: UNHCR; (2019). [Google Scholar]
- 2. Tol WA, Rees S, Silove D. Broadening the scope of epidemiology in conflict-affected settings: opportunities for mental health prevention and promotion. Epidemiol Psychiatr Sci (2013) 22(3):197–203. 10.1017/S2045796013000188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet (2011) 378(9801):1515–25. 10.1016/S0140-6736(11)60827-1 [DOI] [PubMed] [Google Scholar]
- 4. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet (2018) 392(10157):1553–98. 10.1016/S0140-6736(18)31612-X [DOI] [PubMed] [Google Scholar]
- 5. Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry (2017) 210(2):119–24. 10.1192/bjp.bp.116.188078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gilbert BJ, Patel V, Farmer PE, Lu C. Assessing development assistance for mental health in developing countries: 2007–2013. PloS Med (2015) 12(6):e1001834. 10.1371/journal.pmed.1001834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lu C, Li Z, Patel V. Global child and adolescent mental health: the orphan of development assistance for health. PloS Med (2018) 15(3):e1002524. 10.1371/journal.pmed.1002524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO WHO Mental Health Atlas 2017. Geneva: WHO; (2018). [Google Scholar]
- 9. Kakuma R, Minas H, Van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, et al. Human resources for mental health care: current situation and strategies for action. Lancet (2011) 378(9803):1654–63. 10.1016/S0140-6736(11)61093-3 [DOI] [PubMed] [Google Scholar]
- 10. WHO Scalable psychological interventions for people in communities affected by adversity: A new area of mental health and psychosocial work at WHO. Geneva: WHO; (2017). [Google Scholar]
- 11. van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera SM, Pian J, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database Syst Rev (2013) 11:CD009149. 10.1002/14651858.CD009149.pub2 [DOI] [PubMed] [Google Scholar]
- 12. Singla DR, Kohrt B, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low- and middle-income countries. Annu Rev Clin Psychol (2017) 13:149–81. 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Purgato M, Gross AL, Betancourt T, Bolton P, Bonetto C, Gastaldon C, et al. Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. Lancet Global Health (2019) 6(4):e390–400. 10.1016/S2214-109X(18)30046-9 [DOI] [PubMed] [Google Scholar]
- 14. Bryant RA, Schafer A, Dawson KS, Anjuri D, Mulili C, Ndogoni L, et al. Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: a randomised clinical trial. PloS Med (2017) 14(8):e1002371. 10.1371/journal.pmed.1002371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rahman A, Hamdani SU, Awan NR, Bryant RA, Dawson KS, Khan MF, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA (2016) 316(24):2609–17. 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- 16. Rahman A, Khan MN, Hamdani SU, Chiumento A, Akhtar P, Nazir H, et al. Effectiveness of a brief group psychological intervention for women in a post-conflict setting in Pakistan: a cluster randomized controlled trial. Lancet (2019) 393:1733–44. 10.1016/S0140-6736(18)32343-2 [DOI] [PubMed] [Google Scholar]
- 17. Kirmayer LJ. Cultural competence and evidence-based practice in mental health: Epistemic communities and the politics of pluralism. Soc Sci Med (2012) 75(2):249–56. 10.1016/j.socscimed.2012.03.018 [DOI] [PubMed] [Google Scholar]
- 18. Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. J Couns Psychol (2011) 58(3):279–89. 10.1037/a0023626 [DOI] [PubMed] [Google Scholar]
- 19. Griner D, Smith TB. Culturally adapted mental health intervention: A meta-analytic review. Psychother: Theor Res Pract Training (2006) 43(4):531. 10.1037/0033-3204.43.4.531 [DOI] [PubMed] [Google Scholar]
- 20. Harper Shehadeh M, Heim E, Chowdhary N, Maercker A, Albanese E. Cultural adaptation of minimally guided interventions for common mentaldisorders: a systematic review and meta-analysis. J Med Internet Res Ment Health (2016) 3(3):e44. 10.2196/mental.5776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cuijpers P, Karyotaki E, Reijnders M, Purgato M, Barbui C. Psychotherapies for depression in low-and middle-income countries: a meta-analysis. World Psychiatry (2018) 17(1):90–101. 10.1002/wps.20493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jordans MJD, Pigott H, Tol WA. Interventions for children affected by armed conflict: a systematic review of mental health and psychosocial support in low- and middle-income countries. Curr Psychiatry Rep (2016) 18(1):9. 10.1007/s11920-015-0648-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bernal G, Jiménez-Chafey MI, Domenech Rodríguez MM. Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Prof Psychol: Res Pract (2009) 40(4):361–8. 10.1037/a0016401 [DOI] [Google Scholar]
- 24. Chowdhary N, Jotheeswaran A, Nadkarni A, Hollon S, King M, Jordans M, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. psychol Med (2014) 44(6):1131–46. 10.1017/S0033291713001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sijbrandij M, Acarturk C, Bird M, Bryant RA, Burchert S, Carswell K, et al. Strengthening mental health care systems for Syrian refugees in Europe and the Middle East: integrating scalable psychological interventions in eight countries. Eur J Psychotraumatol (2017) 8(sup2):1388102. 10.1080/20008198.2017.1388102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Government of Lebanon and United Nations Lebanon Crisis Response Plan 2017-2020 (2019 update). Beirut: Government of Lebanon; (2019). [Google Scholar]
- 27. World Health Organization and Ministry of Public Health Lebanon WHO-AIMS report on the mental health system in Lebanon. Beirut: World Health Organization and Ministry of Public Health; (2015). [Google Scholar]
- 28. Dawson KS, Watts S, Carswell K, Shehadeh MH, Jordans MJD, Bryant RA, et al. Improving access to evidence-based interventions for young adolescents: Early Adolescent Skills for Emotions (EASE). World Psychiatry (2019) 18(1):105–7. 10.1002/wps.20594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Applied Mental Health Research Group Johns Hopkins University Bloomberg School of Public Health. Design Implementation, Monitoring, and Evaluation of Mental Health and Psychosocial Assistance Programs for Torture Survivors in Low Resource Countries. Baltimore: Johns Hopkins University Bloomberg School of Public Health; (2018). [Google Scholar]
- 30. van Ommeren M, Sharma B, Thapa S, Makaju R, Prasain D, Bhattarai R, et al. Preparing instruments for transcultural research: use of the translation monitoring form with nepali-speaking bhutanese refugees. Transcult Psychiatry (1999) 36(3):285–301. 10.1177/136346159903600304 [DOI] [Google Scholar]
- 31. Hassan G, Kirmayer LJ, Mekki-Berrada A, Quosh C, El Chammay R, Deville-Stoetzel J-B, et al. Culture, context and the mental health and psychosocial wellbeing of Syrians: A review for mental health and psychosocial support staff working with Syrians affected by armed conflict. Geneva: UNHCR; (2015) p. 14–5. [Google Scholar]
- 32. Davis C, Wanninger A. Mental Health and Psychosocial Support Considerations for Syrian Refugees in Turkey: Source of Distress, Coping Mechanisms, & Access to Support. Los Angeles, CA: International Medical Corps; (2017). [Google Scholar]
- 33. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Method (2013) 13(1):117. 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tol W, Augustinavicius J, Carswell K, Brown F, Adaku A, Leku M, et al. Translation, adaptation, and pilot of a guided self-help intervention to reduce psychological distress in South Sudanese refugees in Uganda. Global Ment Health (2018) 5:e25. 10.1017/gmh.2018.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Brown FL, Steen F, Taha K, Aoun M, Bryant RA, Jordans MJD, et al. Early Adolescent Skills for Emotions (EASE) intervention for the treatment of psychological distress in adolescents: Study protocol for randomised controlled trials in Lebanon and Jordan. Trials (2019) 20(1):545. 10.1186/s13063-019-3654-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Save the Children Invisible Wounds: The impact of six years of war on the mental health of Syria’s children London UK: Save the Children. (2017).
- 37. Pfortmueller CA, Schwetlick M, Mueller T, Lehmann B, Exadaktylos AK. Adult asylum seekers from the Middle East including Syria in Central Europe: what are their health care problems? PloS One (2016) 11(2):e0148196. 10.1371/journal.pone.0148196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet (2016) 388(10047):871–80. 10.3310/hta21460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kanter JW, Puspitasari AJ. Global dissemination and implementation of behavioural activation. Lancet (2016) 388(10047):843–4. 10.1016/S0140-6736(16)31131-X [DOI] [PubMed] [Google Scholar]
- 40. Haroz E, Ritchey M, Bass J, Kohrt B, Augustinavicius J, Michalopoulos L, et al. How is depression experienced around the world? A systematic review of qualitative literature. Soc Sci Med (2017) 183:151–62. 10.1016/j.socscimed.2016.12.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ramia JA, Shehadeh MH, Kheir W, Zoghbi E, Watts S, Heim E, et al. Community cognitive interviewing to inform local adaptations of an e-mental health intervention in Lebanon. Global Ment Health (2018) 5:e39. 10.1017/gmh.2018.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rousseau C, Kirmayer L. Cultural adaptation of psychological trauma treatment for children. J Am Acad Child Adolesc Psychiatry (2009) 48(954):9555. 10.1097/CHI.0b013e3181b21669 [DOI] [PubMed] [Google Scholar]
- 43. Hersh J, Metz KL, Weisz JR. New frontiers in transdiagnostic treatment: Youth psychotherapy for internalizing and externalizing problems and disorders. Int J Cogn Ther (2016) 9(2):140–55. 10.1521/ijct.2016.9.2.140 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.