ABSTRACT |
Background:
Visual demands, especially for near vision, are becoming increasingly more frequent at the workplace, and might cause visual fatigue or asthenopia. The tasks performed by ophthalmologists involve visual effort, raising interest in their study within the context of occupational health.
Objectives:
To estimate the prevalence of visual complaints and its relationship to work demands among ophthalmologists at a university hospital in Lisbon.
Methods:
Occurrence of visual fatigue symptoms was assessed by means of a symptom questionnaire - College of Optometrists in Vision Development Quality of Life (COVD-QoL) - and through the identification of near points of accommodation and convergence. Schirmer’s test was used to assess tear production. The results were analyzed by means of descriptive statistics, Spearman’s coefficient and the Wilcoxon test for p<0.05.
Results:
Most among the 27 analyzed physicians reported visual fatigue (n=25), dry eyes and frequent blinking (n=27). Schirmer’s test evidenced differences at the end of the working day and the near points of accommodation and convergence indicated occurrence of visual fatigue.
Conclusions:
The results showed significant differences between the beginning and the end of the working day among ophthalmologists, with occurrence of visual fatigue at the end of the working day. These findings point to the need to implement a health surveillance program to prevent occupational visual disorders.
Keywords |: visual fatigue, occupational medicine, ophthalmology
RESUMO |
Contexto:
As exigências visuais, designadamente da visão ao perto, são cada vez mais frequentes no mundo do trabalho, podendo causar fadiga visual ou astenopia. Os médicos oftalmologistas exercem atividades que exigem esforço visual, o que determina o interesse no seu estudo pela saúde ocupacional.
Objetivos:
Identificar a prevalência das queixas visuais e a sua relação com as exigências do trabalho nos médicos oftalmologistas em um hospital universitário de Lisboa.
Métodos:
Avaliou-se a ocorrência de sintomas de fadiga visual por meio de um questionário de sintomas - Inventário de Eficiência Visual (IEV) - e pela determinação dos pontos próximos de acomodação e de convergência. Utilizou-se o teste de Schirmer para a avaliação da secreção lacrimal. Os resultados foram analisados com o auxílio da estatística descritiva, do coeficiente de Spearman e do teste de Wilcoxon para p<0,05.
Resultados:
Dos 27 médicos respondentes, a maioria refere fadiga visual (n=25), assim como a presença de olhos secos e o piscar frequentemente (n=27). Os resultados do teste de Shirmer evidenciam diferenças no final do dia de trabalho e os pontos próximos de acomodação e convergência evidenciam a presença de fadiga visual.
Conclusões:
Os resultados revelaram diferenças significativas entre o início e o final do dia de atividade profissional dos médicos oftalmologistas, indiciando a existência de fadiga visual ao final do dia de trabalho. Tal situação determina a necessidade de implementar um programa de vigilância da saúde para prevenir alterações visuais de natureza profissional.
INTRODUCTION
Work plays a central role in different societies independently from their degree of development. However, it is often performed under poor health and safety conditions1, while the main priority of workers is to keep their jobs2.
One among the most recent - and perhaps most evident - changes in the world of work is the increase of the visual demands (especially for near vision) under a broad range of working conditions3. The evaluation of lighting is often restricted to environmental aspects, with neglect of the individual characteristics of workers, changes inherent to aging and eventual vision problems.
Studies on “work” and “vision” predominantly address work accidents and the adverse effects of exposure to chemical and physical agents, such as eye injuries, lesions from contact with chemicals - as, e.g., retrobulbar neuritis caused by methanol or lead - and cataracts or maculopathy secondary to ionizing radiation4,5.
The deep transformations undergone by work environments in recent years, mainly derived from technologies based on the use of computers and information systems6, demand progressively higher efficiency of the eye and coordination of the eye movements4, resulting in increased interest in ergo-ophthalmology studies.
The Scientific Committee of the International Commission on Occupational Health (ICOH) defined ergo-ophthalmology as the scientific field aimed at analyzing, evaluating and designing working systems pertaining to the relationship between work and visual performance, by making use of knowledge from different scientific fields in order to obtain maximum efficiency and efficacy of visual function at work4.
Shift of fixation from a distant to a near object involves changes in the refractive power of the eye and in the relationship of the position of the visual axes to keep images clear in the retina and preserve binocular vision. The mechanism by which the eye changes its focus is known as accommodation, and the changes in the position of the visual axes as convergence. These two processes are essential for the preservation of binocular vision for near vision7.
The human vision tends to accommodate to any luminous stimulus. When it focuses on an object at infinite distance, the eye is “not accommodated”, and the mechanism of accommodation unfolds in a gradual manner proportional to the distance to the focused point8.
Non- or poorly corrected binocular vision disorders have direct impact on the signs and symptoms of visual fatigue.
Several factors might trigger (or increase) the occurrence of visual fatigue:
natural decline of vision as a function of aging - starting at about age 40 years old - and appearance of presbyopia due to loss of the lens elasticity;
eye pathological conditions, such as accommodation disorders, low fusion range and non-corrected ametropias;
wearing contact lenses and use of some medications9.
Asthenopia, defined as visual fatigue, is one among the most frequent vision disorders10. Term asthenopia is usually employed to designate any subjective symptom or discomfort associated with the use of the eye11, particularly headache around or above the eyes, tired eyes and eye discomfort.
Visual fatigue might also be described as a functional alteration caused by excessive and prolonged contraction of the ciliary muscle when focusing on an object. Ferguson et al. consider it is the main cause of visual fatigue when the muscles that control the fixation movements are vulnerable12.
Within the occupational setting, visual fatigue is one of the most prevalent eye disorders13,14,15,16,17.
To summarize, visual fatigue might be characterized as presence of one or more eye symptoms (tired eyes, feeling of pressure and itch, eye irritation, difficulty to maintain the focus on images, “redness” and “dry eyes”, frontal and occipital headache, among others) that might be triggered by the continuous use of the eye in long-lasting activities performed at a near distance.
Changes in work processes and increasing use of computers led to a progressive increase of the visual demands and of the activation of the components of the nervous system that coordinate the eye movements and accommodation4,18,19,20. In parallel, also the environmental conditions at work, its microclimate (relative humidity, air temperature and speed) and lighting, in particular, influence the visual system. The relative humidity decreases in enclosed environments, especially the ones with air conditioning systems, which potentiates the evaporation of tears. This situation might be made worse by the visual effort imposed by work at near distance over a long period of time, which unavoidably results in reduction of the blink rate21. Charpe and Kaushik22 reported that the blinking of eyes is 22 times per minute when reading on paper, to reduce to 7 blinks per minute when looking to a computer screen. Yan et al.23 observed that high mental concentration and use of computers cause changes in the tear dynamics with reduction of the spontaneous eye blink rate (SEBR) to 5-6 times per minute. In addition, the tear film - which is essential for the protection and efficiency of the eye surface structures - might considerably evaporate when the environmental humidity is low (especially below 40%).
The work of ophthalmologists is complex and comprises several tasks that involve visual effort. Among the activities they most frequently perform in enclosed environments with air conditioning systems, use of computers, slit lamp and surgical microscope stand out, in addition to tasks involving a high degree of responsibility, which are performed under variable external environmental conditions, such as a dark/poorly lit room. Also reduction of the blink rate, which unavoidably occurs when using computers and slit lamp, might cause changes in the tear secretion.
METHODS
The aim of the present study was to investigate the prevalence of visual complaints and their relationship with job demands among ophthalmologists from a university hospital in Lisbon.
We performed a brief analysis of the work performed by the physicians allocated to the outpatient department of a clinical hospital (n=37) to identify the main risk factors likely to have impact on visual complaints. Next we characterized the occurrence of symptoms related with visual fatigue through application of the Portuguese version of questionnaire College of Optometrists in Vision Development Quality of Life (COVDL-QoL) - Inventário de Eficiência Visual (IEV)24 - which includes the following aspects:
sociodemographic and occupational data;
information on the general state of health;
characterization of eye symptoms.
The participants were then subjected to ophthalmologic examination at the beginning and the end of a working day (average interval of 8 hours). Ophthalmologic examination included analysis of binocular vision parameters, such as near point of accommodation (NPA) and convergence (NPC) by means of the Royal Air Force (RAF) rule. Tear secretion was assessed also at the beginning and the end of the working day by means of Schirmer’s test25.
NPA and NPC are the nearest points on which the eyes are able to maintain focus and binocular fixation. They are measured with the RAF rule, which is placed below the patient’s eyes. The object to be focused on is slowly moved along the rule towards the eyes until focus is lost or one of the patient’s eyes stops fixating and deviates to one side. Normal values are 10 cm for NPC and 8 diopters for NPA, and decrease with age. The measure of the distance of the point on which reading is difficult without optical correction is indicative of presbyopia.
Schirmer’s test is performed for cases of suspected aqueous-tear deficient dry eye. It consists in measuring the amount of moisture in a piece of special filter paper (Whatman 41) with 5 mm of width and 35 mm of length. When the test is performed under topical anesthesia it assesses the basal secretion. Before the test, the eyes are gently dried from excess tears. The filter paper is folded 5 mm from one of its margins and then placed on the point where the middle and external thirds of the lower lid meet. Patients are requested to close their eyes gently for 5 minutes. Then the paper is removed and the amount of moisture is measured. Values less than 6 mm of wetting are considered below the normal range.
Based on the analysis of binocular vision parameters at the beginning and the end of the working day, we investigated associations with asthenopia and dry eye complaints reported by the participants.
The results were first subjected to univariate analysis through descriptive statistics, and then to bivariate analysis by means of Spearman’s correlation coefficient and comparison of paired samples with the Wilcoxon test at p<0.05. The analysis was performed using software SPSS version 22.
RESULTS
Twenty-seven physicians (73% of the full staff) responded the questionnaire; most of them worked about 40 hours per week. The participants’ age ranged from 26 to 62 years old (mean about 40 years old). The sample included individuals aged 20 to 29 years old (n=29), men (n=15), with 0 to 9 years of activity (n=12) and having worked in the current position for less than 4 years (n=10).
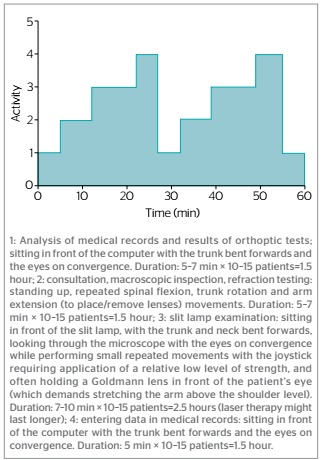
Analysis of the activities performed by the participants (Graphic 1) showed that most (n=14) were exposed to visual demands in association with use of computers or other information systems for more than 6 hours per day. The average length of the work cycles was 20 to 30 minutes. Within such context, visual effort was systematically required over more than 10 minutes (n=15).
Graphic 1. Activities performed by ophthalmologists along consultations.
Among the responses to the questionnaire the following stood out: lack of breaks (n=15), visual fatigue (n=25), mental fatigue (n=15) and physical fatigue (n=2).
Frequent occurrence of dry eye and frequent blinking was reported (n=27); 10 and 9 participants reported feeling the eyes dry “occasionally” and “frequently”, respectively.
Most respondents (n=16) reported having felt their eyes tired “frequently” in the past year. However, eye redness occurred only “seldom” (n=15) or “never” (n=8) in a regular week.
Along the past year and relative to a regular week at work, most participants reported having “occasionally” felt a strong discomfort that caused the “need to close the eyes” (n=20), as well as a feeling of pressure or pain in the eyes (n=14). Only one participant reported not to use artificial tears, while 13 used them “occasionally.” Upon being inquired on the effects of artificial tears, all responded they afford “relief.”
In regard to the aforementioned symptoms, almost all the participants (n=25) reported they had never occurred before the onset of their professional lives, and that they improved or disappeared when on leave/vacation (n=26). Similarly, 25 participants stated their symptoms became worse or reappeared on the first days after returning to work following leaves/holidays. Twenty-four among the latter reported that such complaints were associated with work-related risk factors, namely, use of computers, surgical work, long working hours demanding visual effort and work overload.
Analysis of association between work characteristics and visual fatigue showed that the latter had strong correlation with average duration of work on the computer (r=0.60; p<0.02) and use of medication for arterial hypertension (r=0.60; p<0.01) and moderate correlation with work outside the hospital (r=0.51; p<0.001) and perception of work as imposing visual demands (r=0.44; p<0.001). In addition, weaker correlation was found with lack of breaks during the working day (r=0.32; p<0.03). Use of artificial tears exhibited positive relationship with weekly working hours (r=0,45; p<0,001), average length of work on the computer (r=0.34; p<0.02) and wearing contact lenses (r=0.31; p<0.04) and negative correlation with reduced use on vacation (r=-0,37; p<0,01).
The results of Schirmer’s test (Graphic 2) performed at the beginning of the working day (n=20) were normal (score ≥12) for most participants (n=15). However, the results were different at the end of the working day, mainly reduction of values (n=12).
Graphic 2. Distribution of Schirmer’s test results before and after a working day.
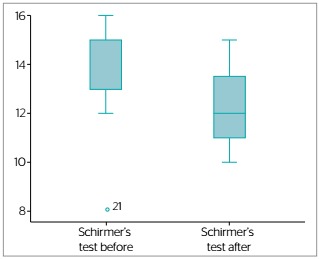
Analysis of Schirmer’s test results for both time-points by means of the Wilcoxon test and assuming that the median values were similar (H0) evidenced significant reduction of the values at the end of the working day, which might be considered to be an indicator of changes in the tear secretion.
Also the results for NPC at the beginning of the working day (n=25) were within the limits of normal. However, the NPC distance increased at the end of the working day (n=21) (Graphic 3).
Graphic 3. Results for near point of convergence before and after a working day.
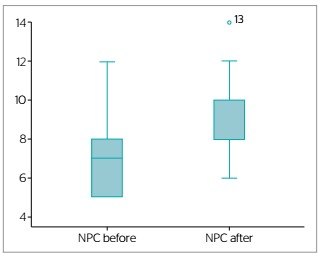
Analysis of NPC at both time-points by means of the Wilcoxon test revealed statistical difference indicative of presence of visual fatigue (p<0.002).
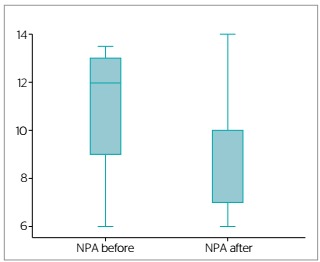
The results for NPA at the beginning of the working day (n=25) were adequate to the participants’ age range (Graphic 4). In turn, the results corresponding to the assessment at the end of the working day (n=21) evidenced reduction of the NPA value.
Graphic 4. Results for near point of accommodation before and after a working day.
DISCUSSION
The prevalence of visual fatigue and associated symptoms was high, especially in association with activities performed during consultations and surgery. The fact that most participants stated these symptoms had never occurred before the onset of their professional lives, that they improved (or even disappeared) while on leave and/or vacation, and became worse (or reappeared) along the first days after returning to work are seemingly indicative of a relationship with work-related activities. The environment, available technical resources and organizational demands and goals that determine the response of this professional category might influence the occurrence of eye disorders, such as visual fatigue. However, also aspects related to individual susceptibility, such as use of medications that interfere with the amount and/or quality of tears, working at a second job and quality of sleep and rest might certainly have impact on visual fatigue.
Most participants perceived a relationship between eye symptoms and occupational factors, particularly work on the computer, surgery work, use of microscope and ophthalmologic equipment, too long periods of work demanding visual effort and work overload, which agrees with the results of other studies on work involving use of information systems4,20.
When inquired on environmental factors that somehow influence their visual health, the participants reported that the main aspects to improve were: visual effort - 88.9% (n=24), time pressure - 81.5% (n=22), body posture - 59.3% (n=16), lighting - 51.6% (n=14) and salary and social benefits - 41.8* (n=13). Aspects rated better were relationship with colleagues - 70.4% (n=19) and supervisors - 44.4% (n=12) and ventilation - 25.9% (n=7).
In regard to self-perceived fatigue, 55.6% (n=15) of the participants reported occurrence of mental fatigue, which in turn might contribute to visual fatigue. Rocha and Debert-Ribeiro26 found association between complaints reported by workers with visual fatigue and high mental workload.
Among the main results of the present study, the ones of ophthalmologic tests stand out, because they are considered to be relevant for the assessment of visual fatigue25. We found significant difference in binocular vision and tear secretion between the initial (beginning of the working day) and final (end of the working day) time-points of assessment.
The results of Schirmer’s test at the beginning of the working day were rated normal for most participants (score ≥12). However, substantial changes were found at the end of the working day, with significant (p<0.03) reduction of the score (n=12) compared to the earliest assessment, which might be considered to be indicative of changes in tear secretion. The visual demands imposed by the professional activity of ophthalmologists over long periods of time, involving computers, slit lamp and microscope, unavoidably cause reduction of the blink rate21. Yan et al.23 consider that also high mental concentration and use of computers cause considerable changes in the tear dynamics, i.e., reduced SEBR. These factors might lead to the development of the dry eye syndrome, and the associated complaints probably are the main reason for physicians to self-prescribe artificial tears. The universal use of artificial tears by the participants does not allow infer whether dry eye syndrome could have occurred were this medication not to have been used.
The results for NPC at the beginning of the working day (n=25) might be categorized as within the normal range. The same was not the case on the assessment at the end of the working day. The results (n=21) indicated significant (p<0.002) increase of the NPC distance.
The results for NPA at the beginning of the working day (n=25) were adequate to the participants’ age range. The assessment at the end of the working day (n=21) evidenced significant (p<0.07) reduction of the NPA values. Although the investigated binocular vision parameters were within the normal range at the end of the day, they exhibited a clear trend to come close to the lower limits of normal. These parameters probably undergo changes due to a functional modification caused by excessive and prolonged contraction of the ciliary muscle when focusing on objects. According to Ferguson et al.12, the main cause of visual fatigue is vulnerability of the image focusing system and of the muscles that control the eye fixation, which might be triggered by continued and prolonged use of the eyes in activities at near distance.
The results of the present study allow inferring that work at near distance, which is a part of the professional routine of ophthalmologists, reduces NPC, NPA and tear secretion, with possible relevant implications for visual comfort and the professionals’ performance. These observations are confirmed by other studies conducted with workers who perform activities that impose high visual demands16,17,20,27.
While the results evidenced occurrence of visual fatigue, one of the main limitations of the present study is due to the sample size.
CONCLUSIONS
In the present study we found high prevalence of visual fatigue among the analyzed ophthalmologists (92.6%) which manifested through a set of self-reported symptoms occurring more frequently at the end of the working day.
Almost all the participants reported to use artificial tears, which variable exhibited positive correlation with weekly working hours, average length of work on the computer, wearing contact lenses and reduction of symptoms during vacation.
The complaints were largely related to some risk factor at work, especially work on the computer, surgery work, use of ophthalmologic equipment, long working hours demanding visual effort and work overload.
The results of the ophthalmologic tests evidenced significant differences between the beginning and the end of the working day, to wit, reduced tear secretion, increased NPC distance and reduced NPA values. These findings clearly point to occurrence of visual fatigue among ophthalmologists at the end of the working day.
Study performed at National Public Health School, New University of Lisbon - Lisbon, Portugal.
Funding: none
REFERENCES
- 1.Sousa-Uva A, Serranheira F. Saúde, Doença e Trabalho: ganhar ou perder a vida a trabalhar? Loures: Diário de Bordo; 2013. [Google Scholar]
- 2.Ferreira-Junior M. Ferreira-Junior M. Saúde no trabalho: temas básicos para o profissional que cuida da saúde dos trabalhadores. São Paulo: Roca; 2000. Saúde no trabalho: temas básicos para o profissional que cuida da saúde dos trabalhadores. [Google Scholar]
- 3.Anshel J. Visual ergonomics in the workplace. Am Associat Occup Health Nurses J. 2007;55(10):414–420. doi: 10.1177/216507990705501004. [DOI] [PubMed] [Google Scholar]
- 4.Piccoli B. A critical appraisal of current knowledge and future directions of ergophthalmology: consensus document of the ICOH Committee on "Work and Vision". Ergonomics. 2003;46(4):384–406. doi: 10.1080/0014013031000067473. [DOI] [PubMed] [Google Scholar]
- 5.Zenz C. Occupational medicine. Chicago: Year Book; 1975. [Google Scholar]
- 6.Pacheco W, Pereira C, Jr., Pereira V, Pereira H., Filho A era da tecnologia da informação e comunicação e a saúde do trabalhador. Rev Bras Med Trab. 2005;3(2):114–122. [Google Scholar]
- 7.Borrás M. Visión binocular: diagnóstico y tratamiento. Buenos Aires: Alfaomega; 2000. [Google Scholar]
- 8.Steinman S, Steinman B, Garzia R. Foundation of binocular vision: a clinical perspective. Washington: McGraw Hill Professional; 2000. [Google Scholar]
- 9.Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Survey Ophthalmol. 2005;50(3):253–262. doi: 10.1016/j.survophthal.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Ramalho A. Dicionário de oftalmologia. Lisboa: LIDEL; 2013. [Google Scholar]
- 11.Alves M, Polati M, Sousa S. Refratometria ocular e a arte da prescrição médica. Rio de Janeiro: Cultura Médica, Guanabara Koogan; 2009. [Google Scholar]
- 12.Ferguson D, Major G, Keldoulis T. Visual defect and the visual demands of tasks. Appl Ergon. 1974;5(2):84–93. doi: 10.1016/0003-6870(74)90084-2. [DOI] [PubMed] [Google Scholar]
- 13.David EV. Fadiga visual em operadores de VDU na Mobil Oil Portuguesa: avaliação subjetiva e análise ergoftalmológica. Lisboa: ENSP; 1992. 34.º Curso de Medicina do Trabalho. [Google Scholar]
- 14.Jain G, Shetty P. Occupational concerns associated with regular use of microscope. Int J Occup Med Environ Health. 2014;27(4):591–598. doi: 10.2478/s13382-014-0288-2. [DOI] [PubMed] [Google Scholar]
- 15.Flavin RJ, Guerin M, O'Briain DS. Occupational problems with microscopy in the pathology laboratory. Virchows Archiv. 2010;457(4):509–511. doi: 10.1007/s00428-010-0965-x. [DOI] [PubMed] [Google Scholar]
- 16.Frango G. Health disorders and ergonomic concerns from the use of microscope: A voice from the past. Am J Clin Pathol. 2011;135:170–171. doi: 10.1309/AJCPUYF00YHFHTHJ. [DOI] [PubMed] [Google Scholar]
- 17.Almeida C, Pagliuca L. Saúde ocular de laboratoristas leitores de lâminas. Rev RENE. 2002;3(1):104–110. [Google Scholar]
- 18.Hayes J, Sheedy JE, Stelmack JA, Heaney CA. Computer use, symptoms and quality of life. Optom VisSci. 2007;84(8):738–744. doi: 10.1097/OPX.0b013e31812f7546. [DOI] [PubMed] [Google Scholar]
- 19.Kanitkar K, Carlson A, Richard Y. Ocular problems associated with computer use. Rev Ophthalmol. 2005 Available from: http://www.revophth.com/content/d/ features/i/1317/c/25354/ [Google Scholar]
- 20.Agarwal S, Goel D, Sharma A. Evaluation of the factors which contribute to the ocular complaints in computer users. J Clin Diagn Res. 2013;7(2):331–335. doi: 10.7860/JCDR/2013/5150.2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaefer TM. Análise das alterações do piscar, do filme lacrimal e da superfície ocular induzidas pelo uso de monitor de computador. São Paulo: Faculdade de Medicina da Universidade de São Paulo; 2009. thesis. [Google Scholar]
- 22.Charpe N, Kaushik V. Computer Vision Syndrome (CVS): Recognition and control in software professionals. J Hum Ecol. 2009;28(1):67–69. [Google Scholar]
- 23.Yan Z, Hu L, Chen H, Lu F. Computer Vision Syndrome: a widely spreading but largely unknown epidemic among computers users. Comp Hum Behav. 2008;24:2026–2042. [Google Scholar]
- 24.Alves M. Tradução e validação para língua portuguesa do questionário Dry Eye Questionnaire. Covilhã: Universidade da Beira Interior; 2012. dissertation. [Google Scholar]
- 25.Kanski J, Bowling B. Oftalmologia clínica: uma abordagem sistemática. 7. Rio de Janeiro: Elsevier; 2012. [Google Scholar]
- 26.Rocha L, Debert-Ribeiro M. Working conditions, visual fatigue and mental health among systems analysts in São Paulo, Brazil. Occup Environ Med. 2004;61:24–32. [PMC free article] [PubMed] [Google Scholar]
- 27.Antunes J, Ferreira MH, Lopes M, Lança CC, Costa AM, Oliveira M, Mendanha L. Avaliação da visão binocular e da secreção lacrimal nos técnicos de farmácia em contexto de produção de nutrição parentérica [poster]; Encontro Nacional das Ciências e das Tecnologias da Saúde, 6; Lisboa. 2011; Lisboa: Escola Superior de Tecnologia da Saúde de Lisboa; 2011. Available from: http://repositorio.ipl.pt//handle/10400.21/311. [Google Scholar]


