Abstract
Health care–associated infections (HCAIs) are a significant concern for both health care workers (HCWs) and patients. They are a major contributing factor of disease in industrialized countries, and are responsible for significant morbidity, mortality, and a direct annual financial loss of $6-7 billion in North America alone. They are an increasingly challenging health issue due to multidrug-resistant pathogens such as methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococci among others, along with an increasing number of susceptible patients. Over the last three decades, the risk of HCAIs has increased in the radiology department (RD) in part because of an increased number of patients visiting the department and an increase in the utilization of imaging modalities. In this review, we will discuss how patients and staff can be exposed to HCAIs in the RD, including contaminated inanimate surfaces, radiology equipment, and associated medical devices. As the role of medical imaging has extended from primarily diagnosis to include more interventions, the implementation and development of standardized infection minimization protocols and infection control procedures are vital in the RD, particularly in interventional radiology. With globalisation and the rapid movement of people regionally, nationally, and globally, there is greater risk of exposure to contagious diseases such as Ebola, especially if infected patients are undiagnosed when they travel. For effective infection control, advanced training and education of HCWs in the RD is essential.
The purpose of this article is to provide an overview of HCAIs as related to activities of the RD. We will discuss the following major topics including the variety of HCAIs commonly encountered, the role of the RD in HCAIs, transmission of infections to patients and HCWs in the RD, standard infection prevention measures, and the management of susceptible/infected patients in the RD. We shall also examine the role of, and the preparedness of, HCWs, including RD technologists and interventional radiologists, who may be exposed to undiagnosed, yet infected patients. We shall conclude with a brief discussion of the role of further research related to HCAIs.
Learning Objectives
After the completion of this review article, the readers will
• Understand the exposure and role of radiology department in health care–associated infections,
• Know the causes/modes/transmission of infections in radiology department,
• Be conscious of standard disinfection protocols,
• Be aware of current and future strategies required for the effective control of health care–associated infection in the radiology department.
This is a CME article and provides the equivalent of 2 hours of continuing education that may be applied to your professional development credit system. A 10-question multiple-choice quiz follows this reading. Please note that no formalized credit (category A) is available from CAMRT.
Keywords: medical imaging, pathogens, infection prevention, radiology equipment, interventional radiology
Introduction
Health care–associated infections (HCAIs), previously known as nosocomial infections, can be defined as those infections that are acquired within any health care setting including inpatient/outpatient, radiology department (RD), and emergency department (ED) [1].
In recent years, there has been a significant increase in morbidity and mortality related to HCAIs worldwide and they have become a priority rank in the World Health Organization (WHO) agenda. HCAIs are the 4th major cause of disease in developed countries [2]. Developing countries have much higher risks of HCAIs with a ratio of 20:1 as compared to the developed countries as studied by Hefzy [1].
The drastic increase in HCAIs has had major implications on hospital budgets. In 2000, HCAIs caused 5,000 deaths in the United Kingdom (UK) alone, causing a 1% increase in the total UK National Hospital budget [3]. The US Centers for Disease Control and Prevention estimated the total costs in North America to be in excess of $6 billion ($US) for treating HCAIs and their associated disabilities [4]. In Germany, it is estimated that approximately 2.4 billion € are spent annually for treatment of such infections [5].
There have been serious efforts to identify the route of transmission of HCAIs and to find effective measures to reduce them [6]. It has been estimated that depending on the type and route, 10%–70% of HCAIs can be controlled [7]. Previously, it was believed that HCAIs were only limited to inpatient hospital settings, where patients have their first encounters with the health care system when they are acutely ill. However, recent outbreaks have shown that a significant number of HCAIs are also experienced in the outpatient settings [1].
Since the RD is integral to the diagnosis and management of many diseased patients, patients and hospital staff within the RD may acquire HCAIs [8]. Radiologists and technologists and other support staff may be unaware of an infectious disease carried by the patient they are about to image or the variety of sources of potential infections they may be exposed to daily.
Important Features of Health Care–Associated Infections
It has been observed that over 55% of HCAIs are transmitted by health care workers (HCWs) providing medical and nursing care via colonized or infected hands, whereas over 28% of such infections are through direct body contact. Therefore, HCWs can be considered as a vector for the transmission of HCAIs to patients [9].Other modes of infection include contact with a contaminated surface, during transport of an infected patient, or during removal of personal protective equipment (PPE) [10]. HCWs are also potentially exposed to many bloodborne infections. As studied by Beltrami et al, the risk of transmission of bloodborne infections variably increases after percutaneous exposure. For example, the risk of transmission of hepatitis B virus is 6%–30%, hepatitis C virus is 1.8%, and human immunodeficiency virus is 0.3% [11]. Similarly, many respiratory diseases such as tuberculosis were common among HCWs, but a recent study in 2016 by Tiemersma has revealed that because of proper surveillance and use of protective equipment, the incidence of new cases of tuberculosis has declined to approximately 32% in the last 5 years (2010–2015) [12].
Types of Infections
Bloodborne infections are acquired through exposure to blood or blood derivatives (platelets, clotting factors) [11]. Respiratory infections are acquired through the inhalation of aerosolized agents and are responsible for 16% of the HCAIs [13].
Gastrointestinal infections cause 13% of the HCAIs and include Clostridium difficile (C diff) infections [14].
Biomedical devices in the vascular system, or other body cavities, can result in infections related to the implantation of these devices as part of an invasive radiology procedure In addition, drains in patients placed elsewhere or during surgery can also be a vector for colonization and transmission of infectious agents. Rutledge-Taylor found that bloodborne and biomedical device vectors constitute about 30% of total HCAIs [13].
Various catheters and stents are used in interventional procedures carried out in the RD; therefore, urinary tract infections, surgical site infections [13], and venous catheter-related infections are also potential causes of bacteremia. A prospective study by Bonnal et al showed that 32% of Staphylococcus aureus–related bacteremia originated from intravascular catheters. Of these catheter-related infections, 56% were due to peripheral vascular catheters and 34% were due to Central Venous Catheters (CVCs) [15]. However, during the same period, there was a decline in peripheral vascular catheters–related infections from 20 to 7%, demonstrating that with adherence to clinical guidelines and precautionary measures that rates of infection can be improved [16]. Common HCAIs, along with their precautionary measures, are described in Table 1 .
Table 1.
Common Health Care–Associated Infections and Transmission-Based Precautions [17]
| Modes of Transmission | Details | Precautionary Measures | Causative Organisms |
|---|---|---|---|
| Direct contact | Infections which transmit through direct contact with an infected patient either by physical touch or by direct droplet infection (sneeze, cough) |
|
|
| Airborne | Infection transmission through small respiratory droplets like sneeze, cough, laugh, exhale, etc. |
|
|
| Droplet | Infection transmission through large respiratory droplets including cough, sneeze or drip within 3 feet of patient |
|
|
| Enteric | Infection through exposure to infected body secretions including feces, vomit or contaminated food and water |
|
|
| Bloodborne infections | Infection that spread through contamination by blood and other body fluids |
|
|
Modes of Transmission of HCAIs
Those responsible for the transmission of an HCAI can be categorized as either infected or colonized individuals. Infected individuals typically have an active pathogen and manifest the signs and symptoms of disease related to the pathogen. By contrast, colonized individuals may have a pathogen but they do not show the signs or symptoms of disease; hence they can be a major, silent source of disease transmission [18].
There are two major modes of transmission for HCAIs; direct or indirect. Direct transmission occurs when pathogens are transferred from an infected, or colonized, subject to a noninfected or noncolonized individual, either through direct skin contact, blood, air droplets, or body secretions. Indirect transmission occurs when there is transfer via an infected or colonized individual to the surrounding environment, for example, linen, clothing, dust, surfaces, or devices, which can then potentially lead to an infection in a new subject.
Susceptible Individuals
With modern therapies, people are living longer and living with more chronic diseases, making them susceptible to infection. Susceptible individuals include immunocompromised patients such as those receiving stem-cell transplantation or chemotherapy for cancers, or patients with decreased immunity such as those with chronic liver or renal disease. Increasingly, people are becoming susceptible to infectious agents due to newer biologic medications that alter the immune system. This group of susceptible individuals may be patients or HCWs in the RD.
Drug Resistance
HCAIs are of great concern in this era of drug (multidrug)-resistant pathogens. The number of drug-resistant pathogens has been growing. Most common among these are methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococci, C diff, Acinetobacter baumannii, Klebsiella pneumoniae, and Pseudomonas aeruginosa [19]. Some of these pathogens are resistant to multiple antibiotics and antibiotic combinations, making prevention and infection control measures even more essential for the management of these HCAIs. Many resistant pathogens such as C diff inhabit the intensive care unit (ICU) environment [20]. Ventilation-associated pneumonias are also very common in ICUs leading to mortality rates of 9%–70% [21]. These factors lead to the increased cost of care because of prolonged hospitalization, intensive care admission, and treatment with newer and more complex antibiotic regimes. The incidence of HCAIs in ICU is significantly higher than for patients admitted to general inpatient wards [22]. Since imaging is often performed on multiple patients in ICU, in one general location, often with a single x-ray machine and digital cassette, heightened diligence is required to avoid the transmission of infectious agents [23].
Similarly, the risk of transmission of HCAIs to neonate and pediatric patients in neonatal intensive care unit (NICU) or pediatric intensive care unit is significantly higher than the general population [24]. Central line–associated bloodstream infections are especially prevalent in NICUs [25].
Role of Radiology Department in Managing HCAIs
RDs are a frequently utilized, shared referral location for patients in hospital for diagnosis and treatment. The RD has evolved from simply using x-ray machines to multiroom facilities using an array of imaging equipment, including magnetic resonance imaging (MRI), computerized tomography (CT), interventional radiology (IR), ultrasonography (US), and other modalities, and are commonly visited by numerous patients [16]. Colonized and infected patients waiting for different radiological tests may increase the chance of HCAIs [26].
Many reports have demonstrated deficiencies in disinfection and sterilization protocols within the RD including studies by Levin et al and Duszak et al, which illustrate the presence of the microorganisms on medical equipment and radiology work stations [23], [27]. Therefore, staff working in RDs including physicians, technologists, and nurses should have an up-to-date knowledge and standardized operating procedures to minimize HCAIs spread via personnel or radiology equipment [28].
A detailed summary of contamination sources and infectious pathogens in the RD is provided in Table 2 . Some common pathogens include Staphylococci, Bacilli, diphtheroids and fungal spores. These are usually found on lead aprons and almost 92% of radiological markers [40]. Ultrasound probes, especially when they come in contact with disrupted skin, may demonstrate Staphylococcus epidermidis (skin flora), Staphylococcus hominis, and few bacillus and gram-negative species. X-ray machines mostly carry gram-negative organisms, especially Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, and MRSA [23]. MRI machines are, however, more prone to MRSA colonization [34].
Table 2.
Reported Areas of Contamination in the Radiology Department (RD) Needs Full Forms of MRSA, VRE, and C diff
| Location | Susceptible Places | Causative Organisms | Reference |
|---|---|---|---|
| General usage areas |
|
|
|
| Patient waiting area |
|
|
|
| Imaging suite |
|
|
|
| Radiology equipment |
|
|
|
| Medical devices |
|
|
|
| Reporting areas |
|
|
|
| Radio pharmacy/Injection site |
|
|
|
| Conference room |
|
|
|
| Interventional radiology suite |
|
|
|
| Waste removal areas |
|
|
|
MRSA, methicillin-resistant Staphylococcus aureus; CT, computerized tomography; ECG, electrocardiogram; VRE, Vancomycin-resistant Enterococci.
Infectious Agents in the Radiology Department
There are many ways by which HCAIs can spread in the RD. They can be broadly categorized into areas within the RD imaging suites and those areas outside the imaging suites. Infection can be passed from patient to radiology HCW and vice versa.
Within the Radiology Suites
Imaging Suite
Imaging suites (rooms) serve as a major reservoir for HCAIs, as a wide variety of patients and medical radiation technologist use these suites for both inpatient and outpatient imaging. The same imaging room may be used for both patient subsets [26].
Hands
Contaminated hands can lead to transfer of infectious pathogen from one person to another and to adjacent surfaces and devices. HCWs (nurses, medical radiation technologists, porters, etc.) and patients can infected or be carriers of HCAIs [41].
Radiology Equipment and Devices
A wide range of microbial pathogens have been linked to different radiological devices and equipment [23]. Portable radiology units come in close proximity to pathogen-laden surfaces in the ICU and the ED. In addition, as the radiographer is required to place and then remove the cassette behind the patient back, so the cassette, portable radiographic machine, and radiographer's hands can become contaminated, an extensive study carried out by Lawlor et al on filmcards used in radiation therapy also shows the tendency of cross-contamination [42]. This may result in the transmission of HCAIs since portable x-rays are often performed on multiple patients at one time and one cassette may be used for multiple patients [43]. Giacometti et al observed that 41.7% of x-ray tubes, 91.7% of control panels and imaging plates, and 8% of x-ray cassettes in the RD imaging rooms were contaminated [33]. The machine control panels and working monitors were the most often contaminated items in the RD.
One study stated that 22.6% of the ultrasound probes were contaminated [44]. Nonbiopsy, endocavity probes which come in contact with mucous membrane and skin require a higher level of disinfection than noncavity ultrasound probes [45]. Ultrasound gel may also serve as a potential source of bacterial contamination such as Burkholderia cepacia and other harmful pathogens, possibly due to its bulk purchase and lack of attention to the expiry dates [46], [47].
The daily use of, and disposal of, a larger number of automated contrast injector system syringes in the CT area has been highlighted as a possible infection control issue [48]. The recurrent handling of the injector system during assembly and/or refilling has led to the contamination of injection tubing and syringes in the past [49].
Within MRI, the most common place for infection is the surface of the machine bore, and as this is a difficult place to access, it may be overlooked during routine cleaning and disinfection [34].
Adhesive tape, often used by radiographers for their radiographic markers (left vs. right, etc.) can also serve as a reservoir for HCAIs because of higher survival rate of bacteria on adhesive tape [50], [51].
Outside the Imaging Suites
Waiting Areas
One of the most important factors in preventing the acquisition of HCAIs in RD is to reduce the patient's stay in the waiting area as much as possible. Prolonged exposure of patients with other patients, and family members, in the RD waiting room is raising a new concern, especially after the recent outbreaks of Ebola, and other highly contagious diseases. This emphasizes the possible need for appropriate use of patient isolation units and the need to follow proper protocols for patient transfer and imaging [52], [53] (Figure 1 ).
Figure 1.
Example of waiting area prone to spread infectious disease (thanks to Dr Amber Ilyas, Radiology Department in Mayo Hospital, Lahore, Pakistan).
Ready Rooms
The surfaces and devices used in the RD ready rooms can serves as a pool of potential pathogenic organisms, since they come in contact with the blood and other bodily secretions of infected patients. These devices include the box for sharp disposal containers with syringes and needles, as well as intravenous (IV) access catheters and an illuminated venipuncture-assist device (Vein finder) [54].
Technologist Working Areas
A study conducted by Duszak et al on RD work stations has shown that work stations used by physicians and imaging technologists to capture, edit, and save images can be contaminated with higher levels of microbial organisms than adjacent toilet seats and door knobs [27].
Equipment and People
Often, patients with bleeding wounds and surgical drains or draining abscesses may come in contact with the surfaces of imaging equipment leading to contamination. Other equipment including imaging tables, touch screens, keyboards, electrocardiogram leads, computer mouse, patient transfer devices, and immobilization straps can all be infected. This emphasizes the need to develop and use an appropriate disinfection procedure before and after every patient visit to RD [55].
Lead aprons are used as a protective gear by the radiology team especially in the fluoroscopy suites and interventional radiology theatres. It has been observed that the front of the apron is more colonized with bacteria as compared with the sides [40].
Radiographic markers can be involved in cross-contamination as they may come in contact with open wounds, as well as other potential sources of contaminations such as pens, note books, etc., in the radiographer's pockets that may then be carried outside the imaging suite [36], [48].
Hospital Environment
The hospital environment serves as a major reservoir of pathogens. Pathogens can survive for prolonged durations on hospital surfaces such as beds, bed rails, IV pumps, supply carts, and over-the-bed tables. They can contaminate the hands and gloves of HCWs, who can in turn transfer pathogens to other individuals and hospital surfaces [56], [57].
Section 4: Preventing Infection in the Radiology Department
Preventative measures should be taken at every level starting from general education and awareness to include proper disinfection of radiological equipment and more specific disinfection and sterilization protocols.
Hand Hygiene Protocols
The single most effective way to reduce HCAIs is to reduce microbial growth on the hands of workers. This is usually performed with alcohol hand sanitizers [26]. However, the use of alcohol is not very effective in enteric infections particularly with C diff and proper hand washing with soap and water is required. Special emphasis is required on hand hygiene while performing portable x-rays in the ED and other susceptible areas [41]. Additional precautionary measures include proper use of gloves while performing radiological examinations and when handling patients.
Sterilization and Disinfection of RD Equipment
Up to one-third of HCAIs can be prevented by proper cleaning of medical equipment [58]. A study by Carling et al shows that 88% of radiographers believed that the major reason for radiology equipment contamination is lack of proper disinfection on a regular basis [57]. It is recommended that all radiology surfaces including CT and MRI table tops, and the ultrasound table, etc., which come into direct contact with patients, must be covered with a replaceable sheet, and these sheets must be replaced after every patient. In addition, cleaning of radiology equipment and imaging equipment with alcohol wipes and chlorhexidine-based detergent between examinations has also shown beneficial results [34].
For the sterilization of radiographic markers, it is highly recommended that alcohol gel and disinfecting wipes along with proper hand washing techniques of the radiographer must be used to ensure contamination [59], [60]. Specific attention is required for ribbon markers which are the most difficult to disinfect [61].
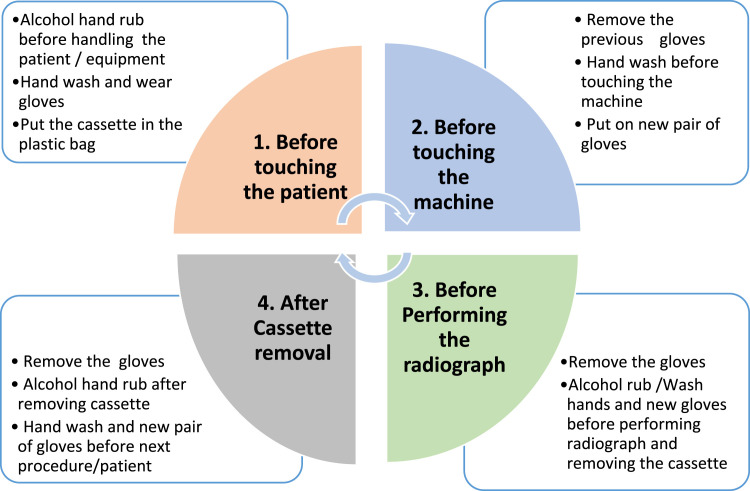
According to a study carried out by Kim et al. on contaminated x-ray cassettes in RD, alcohol wipes have been found to be more effective for the disinfection of x-ray equipment and cassettes as compared with soap and water. Specific disinfection protocol has been explained before touching the patient, before touching the machine, before performing the radiograph and after removing the cassette, to avoid contamination [62]. See Figure 2 .
Figure 2.
Recommended disinfection protocol before portable x-ray [61].
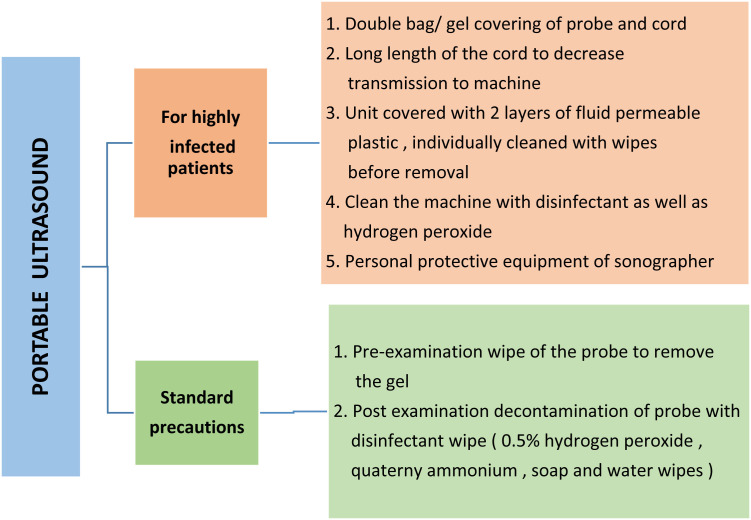
For ultrasound probes, the Canadian Society of Diagnostic Medical Sonographers suggests that sonographers first wipe nonendocavity probes to remove the ultrasound gel and later wipe it with a disinfecting wipe after each examination [63]. It has been observed that 0.5% accelerated hydrogen peroxide has better germicidal performance [64]. The American Institute of Ultrasound in Medicine advises the use of soap and water or spray/wipes of quaternary ammonium disinfectant [65]. See Figure 3 .
Figure 3.
Disinfection protocol for ultrasound [65].
Decontamination protocols for MRI machines are difficult to follow because of difficult access to its bore [34]. Therefore, it is suggested that MRI should be disinfected with a solution of 1,000 parts of hypochlorite by a million part of chloride [60].
Environment Infection Control
Some pathogens, especially Staphylococci, can survive for prolonged periods and can be strongly adherent to the plastic and metal components of medical imaging devices [51]. Bacillus species are also very common in the soil and dust. Owing to high likelihood of pathogens in the hospital environment, the (Good Water supply, Sanitation and Hygiene) WASH protocol is also recommended for proper disinfection [3].
It has been observed that during any change in hospital infrastructure or renovation, the rate of HCAIs increases (up to 60%, particularly blood stream infections rise up to 31%) [66]. In addition, pathogen-laden waste material which is produced as a result of patient handling can also be responsible for HCAIs [39].
Management of Infected Patients in the RD
Standard Infection Control Measures
General precautionary measures should be used for every patient. They are required to avoid transmission. These precautions are often known as universal or standard precautions. Standard precautions are augmented with additional precautions in patients with known enteric, air borne, or other specific transmission hazards; these are described in detail in Table 3 .
Table 3.
Standard Precautionary Measures for Infection Control
| Hand hygiene |
|
| General education/hygiene |
|
| Use of personal protective equipment |
|
| Patient handling |
|
| Isolation protocols |
|
| Disposal precautions |
|
| Needles/sharps handling |
|
| Equipment disinfection |
|
| Environmental hygiene |
|
Contagious Diseases
A contagious disease is any disease, which can be transmitted to other persons, either by physical contact with the person suffering the disease or by casual contact with their secretions or objects touched by them or by airborne route. Some of these highly contagious diseases that can have an impact on the RD are mentioned in the following.
Severe Acute Respiratory Syndrome
Severe acute respiratory syndrome (SARS) was a highly virulent respiratory infection, which resulted in a pandemic in 2003. The high droplet transmission rate of SARS posed an immense threat to HCWs, especially in the RD. As radiological workup of suspected SARS patients typically included a chest x-ray or CT, these patients would need to come to the RD for initial and follow-up imaging [67]. Although there have been no new reported cases of SARS after 2004, a lasting beneficial legacy of this pandemic has been the development of isolation protocols, proper configuration of the RD, cleaning of radiology equipment, along with patient and HCWs safety protocols that will be available if a future, similar outbreak occurs [68].
Middle East Respiratory Syndrome
Another highly contagious disease which has spread globally is Middle East respiratory syndrome. By 2015, it had spread to 26 countries because of its respiratory transmission pathway [69]. Therefore, proper guidelines for quarantine and precautions for airborne diseases, including the isolation of infected and susceptible patients, are critical for both patients and HCWs [70].
Ebola
On 8th August 2014, WHO declared an Ebola epidemic and a Public Health Emergency of International Concern [71]. Ebola virus disease (EVD) emerged as a threat to emergency health care treatment facilities. WHO declared that 10% of the EVD infections involved HCWs [72]. Because a large number of patients with EVD were undiagnosed before their first hospital admission, the rate of transmission to HCWs was significant, reaching almost 95% at the local hospital setting. However, if HCWs adhered to isolation and disinfection protocols, then the risk of HCAIs dramatically dropped to 10.7% [10].
Many advanced radiology procedures such as MRI, CT, or positron emission tomography have not shown any clinical importance in diagnosing patients with EVD [72]. Therefore, advanced imaging should be avoided unless absolutely necessary because of the risk of exposure for other patients and HCWs, as described by a study on cross-infection by Lawlor et al [42].
Portable x-ray and ultrasound are frequently performed for the diagnosis, and management, of infected patients. The use of portable ultrasound and x-ray in the EVD setting should be limited to emergency and isolation units. For such patients, strategies such as wireless, or robotic, imaging may help to further decrease transmission of infection [72].
Proper triage of suspected EVD patients presenting to the ED and use of isolation units can result in a marked reduction of HCAIs [73]. Because EVD disease transmission is through the infected patient's body fluid, good environmental hygiene is very important [74]. In addition to extensive disinfection of radiology equipment, environmental hydrogen peroxide vapor disinfection and disinfection of soiled surfaces are required while dealing with EVD patients [75], [76].
Role of Radiology Department Personnel
The spread of HCAIs is not limited to doctors or nurses, but involves all radiology personnel, including support personnel, and imaging technologists (US, CT, x-ray, etc.). Technologists working in the ICU, or EDs, are often not considered as part of the “local team”, and as such, they may fall through the cracks with respect to infection control resulting in their exposure to infected patients and contributing to the spread of HCAIs [23].
The prevention of HCW-associated transmission of pathogens to radiology department technologists (RDTs) include the use of systematic vaccinations against preventable diseases, prevention of needlestick injuries, proper education, hand hygiene surveillance, and adequate staff resources, as shown by Syrjanen et al [9]. If successfully trained, RDTs have the ability to break the chain of infection emerging in radiology suites and RD [28].
Protection of Radiology Staff
Intensified training and awareness programs for HCWs are required to increase their knowledge of occupational infections [77]. A recent study by Bello et al. in Ghana, revealed the alarming result of only half of local RDTs being aware of standard imaging guidelines, and they had only intermediate knowledge of infection control measures that were taught during their formal training program [78]. Most of the RDTs in this study stated that there was a lack of resources and materials for infection prevention.
Many HCWs are at risk for needlestick injuries (NSIs). These NSIs significantly increase the chances of bloodborne infections. These injuries can be avoided by eliminating the unnecessary use of needles and using safety devices [79]. A recent study carried out by Ballout reviewed the efficacy and safety of using safety-engineered IV and phlebotomy devices [79]. These devices have been shown to reduce the risk of NSIs in HCWs. However, after any NSIs, there must be proper follow-up and vaccination program against bloodborne diseases such as hepatitis B and C.
Organizations such as WHO have made recommendations about the need for screening of susceptible patients and early detection of possible infectious disease outbreaks. Such protocols include good infrastructure and communication with HCWs about contagious diseases and essential support services to the HCWs. These precautions also include careful screening of patients, a limit to the number of staff entering a patient's room. Imaging should be limited to the bedside with proper awareness of isolation unit protocols and use of personal protective equipment (PPEs) while dealing with the critical and undiagnosed patients [72].
PPEs are very important for HCWs working in isolation units and dealing with infected patients. For infections such as EVD, heightened PPE includes full-body coveralls, 2 pairs of nitrile gloves, powered air respirators or N95 respirator, fluid-impermeable apron, and shoe covers with, or without, leg covers [76].
HCAIs and Interventional Radiology
The IR suite can be considered to be a ‘‘very high risk area’’ for the transmission of HCAIs [33], [80]. Reduction of infection in IR requires the appropriate use of antibiotic prophylaxis [81], [82], identification of risk factors, and the appropriate pre-, intra-, and post-procedural care of the patients undergoing interventions. The Society of Interventional Radiology Clinical Practice Guidelines provides advice on the effective antibiotic prophylaxis for vascular and IR depending on the causative pathogens, procedure-specific likelihood of infection risks, and appropriate coverage [19].
Guidelines for the IR suites include control of patient transfer and movement to IR suite, limited exposure to infected patients, quarantine of those with high-risk infection, good flooring and infrastructure of IR suites, and appropriate disinfection protocols of radiology equipment and devices. In addition, RDTs and HCWs education, use of PPEs, and environmental disinfection is also required [38], [83].
Tools have been created to assess the rate of occurrence and the risk of infections for various IR procedures. Vascular access tracking system is a customized web-based system created to provide a site for data storage, and analysis, for catheter placement and infection-related information [35]. Another useful tool is mandatory electronic communication tool, it facilitates early communication and allows for the evaluation of complications related to peripherally inserted central catheters inserted by a venous access team [84].
Insertion site infection after an interventional procedure is one of the major cause of HCAIs in IR. In the NICU, the incidence of such infections is 4.3/100 interventional procedure [85]. Use of antibiotic is recommended but their effectiveness is still unknown.
Modern Radiology Technologies
There are many advanced technologies which are developing in the department of radiology; most common among these are robotic imaging and wireless radiology. Few studies have mentioned the use of robot-assisted imaging modalities in many interventional procedures including use of robotics for the ultrasound-guided venipuncture, robot-assisted MRI-guided liver ablation, and ultrasound-assisted robotic prostate brachytherapy [86], [87], [88]. Similarly, wireless imaging has been utilized in few settings such as the use of wireless x-ray output analyzer system, wireless transponder tracking system for ablative radiotherapy of the liver, and use of wireless intraoral coils for dental MRI [17], [89], [90]. However, it is very crucial to investigate in detail the need to update the departmental protocols based on literature findings in the areas of these modern technologies related to the RD.
Conclusion
In conclusion, HCAIs are a critical and overlooked threat in the hospitals, and to avoid such HCAIs, adherence to disinfection protocols and infection prevention precautions is highly recommended. As discussed in this review article, there are multiple resources through which HCAIs can be acquired in the RD and numerous precautionary steps are required to avoid HCAIs in the RD. However, many deficiencies are still present in terms of readiness of HCWs in the RD for epidemics and emergent infections disease outbreaks. Future studies are required in infection control practices related to IR procedures including the use of prophylactic antibiotics. In addition, further research on the use of more advance radiological technologies, such as wireless and portable imaging machines, especially in ED and during epidemics are required to reduce the risk of HCAIs in the RD. Because RDs are exposed to both direct and indirect modes of HCAIs, it is prudent to investigate further to avoid the exposure to both patients as well as HCWs.
Footnotes
Contributors: All authors contributed to the conception or design of the work, the acquisition, analysis, or interpretation of the data. All authors were involved in drafting and commenting on the paper and have approved the final version.
Competing interests: All authors declare: no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Appendix. CME Article Multiple-Choice Questions
-
1.The infections acquired within health care system are called
-
a)Health care–associated infection
-
b)Stomach infection
-
c)Urinary tract infection
-
d)Septicemia
-
a)
-
2.The hospital department where imaging (x-ray, CT, MRI, etc) of patients is done is known as the
-
a)Laboratory
-
b)Blood bank
-
c)Radiology department
-
d)Pharmacy
-
a)
-
3.The group of individuals exposed to health care–associated infections include
-
a)Immunocompromised patients
-
b)Cancer patients
-
c)Individuals with chronic disease
-
d)Health care workers
-
e)All of the above
-
a)
-
4.The set of protocols followed to reduce contamination and to avoid the spread of the infection within the health care settings are called
-
a)Laundry
-
b)Disinfection protocols
-
c)Phlebotomy
-
d)Chemotherapy
-
a)
-
5.WASH protocol (Good Water supply, Sanitation and Hygiene protocol) is recommended for proper disinfection of
-
a)Kitchen utensils
-
b)House carpets
-
c)Hospital environment
-
d)Laboratory shelves
-
a)
-
6.Any disease transmitted from one infected individual to another person, by physical contact, their secretions, or by airborne route is called
-
a)Pathogen
-
b)Contagious disease
-
c)Environmental contamination
-
d)Catheter infection
-
a)
-
7.SARS is an Abbreviation of
-
a)Middle East Respiratory Syndrome
-
b)Personal Protective Equipment
-
c)Intensive Care Unit
-
d)Severe Acute Respiratory Syndrome
-
a)
-
8.The globally renowned organization, which impose health care–related rules, regulation and legislation is
-
a)WHO (World Health Organization)
-
b)UN (United Nations)
-
c)World Bank
-
d)ILO (International Labour Organization)
-
a)
-
9.Personal Protective Equipment required for the prevention of Health care associated infections is called
-
a)EVD
-
b)CT
-
c)MRI
-
d)PPE
-
a)
-
10.The subspecialty of Radiology related to interventional procedures is called
-
a)Interventional Radiology (IR)
-
b)Computerized Tomography
-
c)Ultrasound
-
d)Magnetic Resonance Imaging (MRI)
-
a)
References
- 1.Hefzy E.M., Wegdan A.A., Abdel Wahed W.Y. Hospital outpatient clinics as a potential hazard for healthcare associated infections. J Infect Public Health. 2015;9(1):88–97. doi: 10.1016/j.jiph.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Guggenbichler J.P., Assadian O., Boeswald M., Kramer A. Incidence and clinical implication of nosocomial infections associated with implantable biomaterials - catheters, ventilator-associated pneumonia, urinary tract infections. GMS Krankenhhyg Interdiszip. 2011;6(1):18. doi: 10.3205/dgkh000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waite R.C., Velleman Y., Woods G., Chitty A., Freeman M.C. Integration of water, sanitation and hygiene for the control of neglected tropical diseases: a review of progress and the way forward. Int Health. 2016;8(Suppl 1):i22–i27. doi: 10.1093/inthealth/ihw003. [DOI] [PubMed] [Google Scholar]
- 4.NNIS Nosocomial infection rates for interhospital comparison: limitations and possible solutions. A Report from the National Nosocomial Infections Surveillance (NNIS) System. Infect Control Hosp Epidemiol. 1991;12(10):609–621. [PubMed] [Google Scholar]
- 5.Frank U., Chojnacki T., Dettenkofer M., Daschner F.D. Cost-effectiveness of an antiseptic-impregnated central venous catheter in the ICU. Intensive Care Med. 2003;29(1):139. doi: 10.1007/s00134-002-1559-0. [DOI] [PubMed] [Google Scholar]
- 6.Umscheid C.A., Mitchell M.D., Doshi J.A., Agarwal R., Williams K., Brennan P.J. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32(2):101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- 7.Harbarth S., Sax H., Gastmeier P. The preventable proportion of nosocomial infections: an overview of published reports. J Hosp Infect. 2003;54(4):258–266. doi: 10.1016/s0195-6701(03)00150-6. [DOI] [PubMed] [Google Scholar]
- 8.Marcel J.P., Alfa M., Baquero F., et al. Healthcare-associated infections: think globally, act locally. Clin Microbiol Infect. 2008;14(10):895–907. doi: 10.1111/j.1469-0691.2008.02074.x. [DOI] [PubMed] [Google Scholar]
- 9.Huttunen R., Syrjanen J. Healthcare workers as vectors of infectious diseases. Eur J Clin Microbiol Infect Dis. 2014;33(9):1477–1488. doi: 10.1007/s10096-014-2119-6. [DOI] [PubMed] [Google Scholar]
- 10.Olu O., Kargbo B., Kamara S., et al. Epidemiology of Ebola virus disease transmission among health care workers in Sierra Leone, May to December 2014: a retrospective descriptive study. BMC Infect Dis. 2015;15:416. doi: 10.1186/s12879-015-1166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beltrami E.M., Williams I.T., Shapiro C.N., Chamberland M.E. Risk and management of blood-borne infections in health care workers. Clin Microbiol Rev. 2000;13(3):385–407. doi: 10.1128/cmr.13.3.385-407.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiemersma E.W., Huong N.T., Yen P.H., et al. Infection control and tuberculosis among health care workers in Viet Nam, 2009-2013: a cross-sectional survey. BMC Infect Dis. 2016;16(1):664. doi: 10.1186/s12879-016-1993-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutledge-Taylor K., Matlow A., Gravel D., et al. A point prevalence survey of health care-associated infections in Canadian pediatric inpatients. Am J Infect Control. 2012;40(6):491–496. doi: 10.1016/j.ajic.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Brkic S., Pellicano R., Turkulov V., Radovanovic M., Abenavoli L. Prevention program for Clostridium difficile infection: a single-centre Serbian experience. Minerva Med. 2016;107(3):131–139. [PubMed] [Google Scholar]
- 15.Bonnal C., Birgand G., Lolom I., et al. Staphylococcus aureus healthcare associated bacteraemia: An indicator of catheter related infections. Med Mal Infect. 2015;45(3):84–88. doi: 10.1016/j.medmal.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Shagam J.Y. The radiology department and nosocomial infections. Radiol Technol. 1999;70(5):418–430. [PubMed] [Google Scholar]
- 17.Ludwig U., Eisenbeiss A.K., Scheifele C., et al. Dental MRI using wireless intraoral coils. Sci Rep. 2016;6:23301. doi: 10.1038/srep23301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mirza S.K., Tragon T.R., Fukui M.B., Hartman M.S., Hartman A.L. Microbiology for Radiologists: How to Minimize Infection Transmission in the Radiology Department. Radiographics. 2015;35(4):1231–1244. doi: 10.1148/rg.2015140034. [DOI] [PubMed] [Google Scholar]
- 19.Venkatesan A.M., Kundu S., Sacks D., et al. Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. Written by the Standards of Practice Committee for the Society of Interventional Radiology and Endorsed by the Cardiovascular Interventional Radiological Society of Europe and Canadian Interventional Radiology Association [corrected] J Vasc Interv Radiol. 2018;21(11):1611–1630. doi: 10.1016/j.jvir.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Bouza E., Rodriguez-Creixems M., Alcala L., et al. Is Clostridium difficile infection an increasingly common severe disease in adult intensive care units? A 10-year experience. J Crit Care. 2015;30(3):543–549. doi: 10.1016/j.jcrc.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Cunnion K.M., Weber D.J., Broadhead W.E., Hanson L.C., Pieper C.F., Rutala W.A. Risk factors for nosocomial pneumonia: comparing adult critical-care populations. Am J Respir Crit Care Med. 1996;153(1):158–162. doi: 10.1164/ajrccm.153.1.8542110. [DOI] [PubMed] [Google Scholar]
- 22.Brunelli S.M., Turenne W., Sibbel S., Hunt A., Pfaffle A. Clinical and economic burden of bloodstream infections in critical care patients with central venous catheters. J Crit Care. 2016;35:69–74. doi: 10.1016/j.jcrc.2016.04.035. [DOI] [PubMed] [Google Scholar]
- 23.Levin P.D., Shatz O., Sviri S., et al. Contamination of portable radiograph equipment with resistant bacteria in the ICU. Chest. 2009;136(2):426–432. doi: 10.1378/chest.09-0049. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira J., Bouzada M.C., Jesus L.A., et al. Evaluation of national health-care related infection criteria for epidemiological surveillance in neonatology. J Pediatr (Rio J) 2014;90(4):389–395. doi: 10.1016/j.jped.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Ista E., van der Hoven B., Kornelisse R.F., et al. Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(6):724–734. doi: 10.1016/S1473-3099(15)00409-0. [DOI] [PubMed] [Google Scholar]
- 26.Ustunsoz B. Hospital infections in radiology clinics. Diagn Interv Radiol. 2005;11(1):5–9. [PubMed] [Google Scholar]
- 27.Duszak R., Jr., Lanier B., Tubbs J.A., Ogilvie M., Thompson-Jaeger S. Bacterial contamination of radiologist workstations: results of a pilot study. J Am Coll Radiol. 2014;11(2):176–179. doi: 10.1016/j.jacr.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt J.M. Stopping the chain of infection in the radiology suite. Radiol Technol. 2012;84(1):31–48. [PubMed] [Google Scholar]
- 29.Russotto V., Cortegiani A., Raineri S.M., Giarratano A. Bacterial contamination of inanimate surfaces and equipment in the intensive care unit. J Intensive Care. 2015;3:54. doi: 10.1186/s40560-015-0120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Catalano M., Quelle L.S., Jeric P.E., Di Martino A., Maimone S.M. Survival of Acinetobacter baumannii on bed rails during an outbreak and during sporadic cases. J Hosp Infect. 1999;42(1):27–35. doi: 10.1053/jhin.1998.0535. [DOI] [PubMed] [Google Scholar]
- 31.Rutala W.A., White M.S., Gergen M.F., Weber D.J. Bacterial contamination of keyboards: efficacy and functional impact of disinfectants. Infect Control Hosp Epidemiol. 2006;27(4):372–377. doi: 10.1086/503340. [DOI] [PubMed] [Google Scholar]
- 32.Lestari T., Ryll S., Kramer A. Microbial contamination of manually reprocessed, ready to use ECG lead wire in intensive care units. GMS Hyg Infect Control. 2013;8(1) doi: 10.3205/dgkh000207. Doc07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giacometti M., Gualano M.R., Bert F., et al. Microbiological contamination of radiological equipment. Acta Radiol. 2014;55(9):1099–1103. doi: 10.1177/0284185113512481. [DOI] [PubMed] [Google Scholar]
- 34.Shelly M.J., Scanlon T.G., Ruddy R., Hannan M.M., Murray J.G. Meticillin-resistant Staphylococcus aureus (MRSA) environmental contamination in a radiology department. Clin Radiol. 2011;66(9):861–864. doi: 10.1016/j.crad.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Morrison J., Kaufman J. Vascular Access Tracking System: a Web-Based Clinical Tracking Tool for Identifying Catheter Related Blood Stream Infections in Interventional Radiology Placed Central Venous Catheters. J Digit Imaging. 2016;29:737–741. doi: 10.1007/s10278-016-9891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buerke B., Puesken M., Mellmann A., et al. Automatic MDCT injectors: hygiene and efficiency of disposable, prefilled, and multidosing roller pump systems in clinical routine. AJR Am J Roentgenol. 2011;197(2):W226–W232. doi: 10.2214/AJR.10.5924. [DOI] [PubMed] [Google Scholar]
- 37.Teng S.O., Lee W.S., Ou T.Y., Hsieh Y.C., Lee W.C., Lin Y.C. Bacterial contamination of patients' medical charts in a surgical ward and the intensive care unit: impact on nosocomial infections. J Microbiol Immunol Infect. 2009;42(1):86–91. [PubMed] [Google Scholar]
- 38.Baffroy-Fayard N. [Infection control in interventional radiology: good practice guideline] J Radiol. 2002;83(3):351–359. [PubMed] [Google Scholar]
- 39.Sozzi E., Fabre K., Fesselet J.F., Ebdon J.E., Taylor H. Minimizing the Risk of Disease Transmission in Emergency Settings: Novel In Situ Physico-Chemical Disinfection of Pathogen-Laden Hospital Wastewaters. PLoS Negl Trop Dis. 2015;9(6):e0003776. doi: 10.1371/journal.pntd.0003776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boyle H., Strudwick R.M. Do lead rubber aprons pose an infection risk? Radiography. 2010;16(4):297–303. [Google Scholar]
- 41.Aso M., Kato K., Yasuda M., et al. [Hand hygiene during mobile X-ray imaging in the emergency room] Nihon Hoshasen Gijutsu Gakkai Zasshi. 2014;67(7):793–799. doi: 10.6009/jjrt.67.793. [DOI] [PubMed] [Google Scholar]
- 42.Lawlor D., Cannon K., Duan Q., Jensen K. Filmcards Used in Radiation Therapy: Are They a Potential Source of Cross-infection? J Med Imaging Radiat Sci. 2012;43(1):52–59. doi: 10.1016/j.jmir.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Neely A.N. A survey of gram-negative bacteria survival on hospital fabrics and plastics. J Burn Care Rehabil. 2000;21(6):523–527. doi: 10.1097/00004630-200021060-00009. [DOI] [PubMed] [Google Scholar]
- 44.Chu K., Obaid H., Babyn P., Blondeau J. Bacterial contamination of ultrasound probes at a tertiary referral university medical center. AJR Am J Roentgenol. 2014;203(5):928–932. doi: 10.2214/AJR.13.12407. [DOI] [PubMed] [Google Scholar]
- 45.Gray R.A., Williams P.L., Dubbins P.A., Jenks P.J. Decontamination of transvaginal ultrasound probes: review of national practice and need for national guidelines. Clin Radiol. 2012;67(11):1069–1077. doi: 10.1016/j.crad.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 46.Wooltorton E. Medical gels and the risk of serious infection. CMAJ. 2004;171(11):1348. doi: 10.1503/cmaj.1041684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hutchinson J., Runge W., Mulvey M. Burkholderia cepacia infections associated with intrinsically contaminated ultrasound gel: the role of microbial degradation of parabens. Infect Control Hosp Epidemiol. 2004;25(4):291–296. doi: 10.1086/502394. [DOI] [PubMed] [Google Scholar]
- 48.Buerke B., Mellmann A., Stehling C., Wessling J., Heindel W., Juergens K.U. Microbiologic contamination of automatic injectors at MDCT: experimental and clinical investigations. AJR Am J Roentgenol. 2008;191(6):W283–W287. doi: 10.2214/AJR.07.3954. [DOI] [PubMed] [Google Scholar]
- 49.Buerke B., Sonntag A.K., Fischbach R., Heindel W., Tombach B. [Automatic injectors in magnetic resonance imaging and computed tomography: pilot study on hygienic aspects] Rofo. 2004;176(12):1832–1836. doi: 10.1055/s-2004-813520. [DOI] [PubMed] [Google Scholar]
- 50.Hodges A. Radiographic markers: friend or fomite? Radiol Technol. 2001;73(2):183–185. [PubMed] [Google Scholar]
- 51.Lawson S.R., Sauer R., Loritsch M.B. Bacterial survival on radiographic cassettes. Radiol Technol. 2002;73(6):507–510. [PubMed] [Google Scholar]
- 52.Busi Rizzi E., Puro V., Schinina V., Nicastri E., Petrosillo N., Ippolito G. Radiographic imaging in Ebola Virus Disease: protocol to acquire chest radiographs. Eur Radiol. 2015;25(11):3368–3371. doi: 10.1007/s00330-015-3748-6. [DOI] [PubMed] [Google Scholar]
- 53.Vogl T.J., Martin S., Brodt H.R., Keppler O., Zacharowski K., Wolf T. The Frankfurt Ebola patient. Rofo. 2015;187(9):771–776. doi: 10.1055/s-0035-1553130. [DOI] [PubMed] [Google Scholar]
- 54.O'Grady N.P., Alexander M., Dellinger E.P., et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51(RR-10):1–29. [PubMed] [Google Scholar]
- 55.Hubble W.L., Turner J.A., Heuertz R. Effectiveness of Current Practices for Disinfecting Medical Equipment in a Radiology Department. Radiol Technol. 2016;87(3):250–260. [PubMed] [Google Scholar]
- 56.Li J.T., Li Y., Wang J. [Surveillance on gram-positive bacteria isolated from patients with hospital acquired infections or community acquired infections] Zhonghua Yi Xue Za Zhi. 2003;83(5):365–374. [PubMed] [Google Scholar]
- 57.Carling P.C., Parry M.F., Von Beheren S.M. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(1):1–7. doi: 10.1086/524329. [DOI] [PubMed] [Google Scholar]
- 58.Wenzel R.P., Edmond M.B. The impact of hospital-acquired bloodstream infections. Emerg Infect Dis. 2001;7(2):174–177. doi: 10.3201/eid0702.010203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aziz A.M. Clostridium difficile infection: A critical analysis of the guidance. Br J Nurs. 2009;18(21):1328–1332. doi: 10.12968/bjon.2009.18.21.45367. [DOI] [PubMed] [Google Scholar]
- 60.Health, P.H.E.A.D.O. 2009. Clostridium difficile infection: How to deal with the problem.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/340851/Clostridium_difficile_infection_how_to_deal_with_the_problem.pdf Available at: [Google Scholar]
- 61.Tugwell J., Maddison A. Radiographic markers – A reservoir for bacteria? Radiography. 2011;17(2):115–120. [Google Scholar]
- 62.Kim J.S., Kim H.S., Park J.Y., et al. Contamination of X-ray cassettes with methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus haemolyticus in a radiology department. Ann Lab Med. 2012;32(3):206–209. doi: 10.3343/alm.2012.32.3.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sonography, C.S.O.D.M. Professional Practice Guidelines and Policy statements for canadian sonograph. 2014. http://www.sonographycanada.ca/Apps/Sites-Management/FileDownload/DataDownload/6945/CSDMS_ProfessionalPractice_E_/pdf/1/1033 Available at:
- 64.Virox Technologies, I. Accelerated Hydrogen Peroxide® (AHP®) Technology. 2016. http://info.virox.com/accel-ahp-disinfectants-medical-reprocessing-canada Available at: Accessed June 2009.
- 65.Shokoohi H., Amstrong P., Tansek R. Emergency department ultrasound probe infection control: challenges and solutions. Open Access Emerg Med. 2015;2015(7):1–9. doi: 10.2147/OAEM.S50360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Taylor G.D., McKenzie M., Kirkland T., Buchanan-Chell M., Wiens R. The impact of health care restructuring on nosocomially acquired blood stream infections. Can J Infect Dis. 2000;11(1):34–37. doi: 10.1155/2000/869091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ketai L., Paul N.S., Wong K.T. Radiology of severe acute respiratory syndrome (SARS): the emerging pathologic-radiologic correlates of an emerging disease. J Thorac Imaging. 2006;21(4):276–283. doi: 10.1097/01.rti.0000213581.14225.f1. [DOI] [PubMed] [Google Scholar]
- 68.Tsou I.Y., Goh J.S., Kaw G.J., Chee T.S. Severe acute respiratory syndrome: management and reconfiguration of a radiology department in an infectious disease situation. Radiology. 2003;229(1):21–26. doi: 10.1148/radiol.2291030789. [DOI] [PubMed] [Google Scholar]
- 69.Koenig K.L. Identify-Isolate-Inform: A Modified Tool for Initial Detection and Management of Middle East Respiratory Syndrome Patients in the Emergency Department. West J Emerg Med. 2015;16(5):619–624. doi: 10.5811/westjem.2015.7.27915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barbisch D., Koenig K.L., Shih F.Y. Is There a Case for Quarantine? Perspectives from SARS to Ebola. Disaster Med Public Health Prep. 2015;9(5):547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- 71.Team, W.E.R. Ebola virus disease in West Africa--the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371(16):1481–1495. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bluemke D.A., Meltzer C.C. Ebola virus disease: radiology preparedness. Radiology. 2015;274(2):527–531. doi: 10.1148/radiol.14142502. [DOI] [PubMed] [Google Scholar]
- 73.Brett-Major D.M., Jacob S.T., Jacquerioz F.A., et al. Being ready to treat Ebola virus disease patients. Am J Trop Med Hyg. 2015;92(2):233–237. doi: 10.4269/ajtmh.14-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Poliquin P.G., Vogt F., Kasztura M., et al. Environmental Contamination and Persistence of Ebola Virus RNA in an Ebola Treatment Center. J Infect Dis. 2016;214:S145–S152. doi: 10.1093/infdis/jiw198. [DOI] [PubMed] [Google Scholar]
- 75.Auffermann W.F., Kraft C.S., Vanairsdale S., Lyon G.M., 3rd, Tridandapani S. Radiographic imaging for patients with contagious infectious diseases: how to acquire chest radiographs of patients infected with the Ebola virus. AJR Am J Roentgenol. 2015;204(1):44–48. doi: 10.2214/AJR.14.14041. [DOI] [PubMed] [Google Scholar]
- 76.Mollura D.J., Palmore T.N., Folio L.R., Bluemke D.A. Radiology preparedness in ebola virus disease: guidelines and challenges for disinfection of medical imaging equipment for the protection of staff and patients. Radiology. 2015;275(2):538–544. doi: 10.1148/radiol.15142670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wicker S., Rabenau H.F., Schachtrupp A., Schalk R. Gesundheitswesen; Germany: 2016. [Viral Infections Among the Nursing Personnel - a Survey] [DOI] [PubMed] [Google Scholar]
- 78.Bello A.I., Asiedu E.N., Adegoke B.O., Quartey J.N., Appiah-Kubi K.O., Owusu-Ansah B. Nosocomial infections: knowledge and source of information among clinical health care students in Ghana. Int J Gen Med. 2011;4:571–574. doi: 10.2147/IJGM.S16720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ballout R.A., Diab B., Harb A.C., Tarabay R., Khamassi S., Akl E.A. Use of safety-engineered devices by healthcare workers for intravenous and/or phlebotomy procedures in healthcare settings: a systematic review and meta-analysis. BMC Health Serv Res. 2016;16:458. doi: 10.1186/s12913-016-1705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Huang S.Y., Philip A., Richter M.D., Gupta S., Lessne M.L., Kim C.Y. Prevention and management of infectious complications of percutaneous interventions. Semin Intervent Radiol. 2015;32(2):78–88. doi: 10.1055/s-0035-1549372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sutcliffe J.A., Briggs J.H., Little M.W., et al. Antibiotics in interventional radiology. Clin Radiol. 2015;70(3):223–234. doi: 10.1016/j.crad.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 82.Khan W., Sullivan K.L., McCann J.W., et al. Moxifloxacin prophylaxis for chemoembolization or embolization in patients with previous biliary interventions: a pilot study. AJR Am J Roentgenol. 2011;197(2):W343–W345. doi: 10.2214/AJR.10.6019. [DOI] [PubMed] [Google Scholar]
- 83.Abi-Jaoudeh N., Walser E.M., Bartal G., et al. Ebola and Other Highly Contagious Diseases: Strategies by the Society of Interventional Radiology for Interventional Radiology. J Vasc Interv Radiol. 2016;27(2):200–202. doi: 10.1016/j.jvir.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 84.Kim-Saechao S.J., Almario E., Rubin Z.A. A novel infection prevention approach: Leveraging a mandatory electronic communication tool to decrease peripherally inserted central catheter infections, complications, and cost. Am J Infect Control. 2016;44:1335–1345. doi: 10.1016/j.ajic.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 85.Clements K.E., Fisher M., Quaye K., O'Donnell R., Whyte C., Horgan M.J. Surgical site infections in the NICU. J Pediatr Surg. 2016;51:1405–1408. doi: 10.1016/j.jpedsurg.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 86.Balter M.L., Chen A.I., Maguire T.J., Yarmush M.L. Adaptive Kinematic Control of a Robotic Venipuncture Device Based on Stereo Vision, Ultrasound, and Force Guidance. IEEE Trans Ind Electron. 2016;64(2):1626–1635. doi: 10.1109/TIE.2016.2557306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Franco E., Ristic M., Rea M., Gedroyc W.M. Robot-assistant for MRI-guided liver ablation: A pilot study. Med Phys. 2016;43(10):5347. doi: 10.1118/1.4961986. [DOI] [PubMed] [Google Scholar]
- 88.Zhang S., Jiang S., Yang Z., Liu R., Yang Y., Liang H. An ultrasound image navigation robotic prostate brachytherapy system based on US to MRI deformable image registration method. Hell J Nucl Med. 2016;19(3):223–230. doi: 10.1967/s002449910404. [DOI] [PubMed] [Google Scholar]
- 89.Akaishi H., Takeda H., Kanazawa Y., Yoshii Y., Asanuma O. [Development of a Lead-covered Case for a Wireless X-ray Output Analyzer to Perform CT Half-value Layer Measurements] Nihon Hoshasen Gijutsu Gakkai Zasshi. 2016;72(3):244–250. doi: 10.6009/jjrt.2016_JSRT_72.3.244. [DOI] [PubMed] [Google Scholar]
- 90.James J., Cetnar A., Dunlap N.E., et al. Technical Note: Validation and implementation of a wireless transponder tracking system for gated stereotactic ablative radiotherapy of the liver. Med Phys. 2016;43(6):2794. doi: 10.1118/1.4948669. [DOI] [PubMed] [Google Scholar]