Key points.
Severe community-acquired pneumonia (CAP) is associated with a high mortality rate and significant morbidity.
Of patients presenting to hospital with CAP, up to 10% will require critical care admission.
Streptococcus pneumoniae continues as the most common infective pathogen.
Staphylococcus aureus, Legionella, and gram-negative pathogens are increasingly frequent causative pathogens.
Combined viral and bacterial infections may induce a more severe spectrum of disease.
Severe community-acquired pneumonia (CAP) remains a frequent reason for admission to hospital. It is the most common cause of septic shock requiring escalation to treatment within an intensive care unit (ICU). Despite earlier recognition and recent advances in supportive care, severe CAP is still associated with substantial morbidity and mortality, more often seen in the elderly and those with considerable comorbidities.
Definition
CAP is defined as an acute infection of the pulmonary parenchyma, with symptom onset in the community. Diagnosis can still be made within 48 h of hospital admission to meet criteria for a community-acquired infection. Severe CAP is defined as a pneumonia requiring supportive therapy within a critical care environment, that is associated with a higher mortality rate. Severe CAP is frequently a multisystem disease and patients will often present with multiple organ failure.
Epidemiology
The annual incidence of CAP is 1.6–10.6 per 1000 adult population in Europe.1 Between 1.2% and 10% of patients requiring hospital admission to treat CAP will require ICU admission. The incidence of CAP increases with age, and more than 90% of deaths related to severe pneumonia occur in patients over the age of 70. The 28 day mortality rate in patients admitted to critical care is ∼17%, which increases to 24.4% in those requiring invasive mechanical ventilation and 28.8% in those that develop septic shock.1 Mortality rates in younger patients are more influenced by the severity of the infection rather than the presence of comorbidities. Even in the absence of comorbidities, severe CAP is associated with excess mortality over subsequent years among survivors independent of age.
Clinical features
CAP classically presents with a triad of infective signs (fever, leucocytosis), clinical signs and symptoms (sputum production, tachypnoea, cough, pleuritic chest pain), and a new or changed infiltrate as observed on radiography, for which there is no other explanation except infection. However, these clinical signs and symptoms may not be universally seen or present typically, particularly in the elderly or immunosuppressed. Diagnosis of CAP may be clouded or complicated by underlying disease states that affect cardiorespiratory function and by atypical or subacute presentations of infection.
Aetiology
Pneumonia develops when the defensive mechanisms within the lung become overwhelmed by a pathogen which has been either inhaled or aspirated. This is more likely to occur with more virulent pathogens and in patients with reduced host defences. Pathogens responsible for CAP are varied and wide-ranging in their capacity to cause severe disease and extra-pulmonary features (Table 1). The predominant pathogen throughout all age groups remains Streptococcus pneumoniae. Legionella, gram-negative bacilli, influenzae species, and Staphylococcus aureus are becoming increasingly common causes of severe CAP requiring critical care admission in comparison with CAP managed outside of critical care units. The frequency of other less prevalent causes of CAP such as Chlamydophilia psittaci, Coxiella burnetii, and Mycoplasma pneumoniae varies according to epidemiological setting and in part on the diagnostic techniques that are used. No causative organism is identified in up to 36% of cases of severe CAP.
Table 1.
Common pathogens implicated in severe CAP
| Pathogen | Risk factors | Other features |
|---|---|---|
| Streptococcus pnemoniae | Alcoholism, HIV, i.v. drug abuse, hyposplenism | Pleural effusion, empyema |
| Staphylococcus aureus | Structural lung disease, i.v. drug abuse, influenza | Pneumothoraces, cavitation |
| CA-MRSA | Influenza | Necrotizing pneumonia, cavitation, neutropenia, skin pustules |
| Legionella species | Smoking, foreign travel | Neurological symptoms, raised creatinine kinase, diarrhoea, transaminitis, relative bradycardia |
| Gram-negative bacilli | Structural lung disease, recent antibiotics, immunosuppression | |
| Klebsiella pneumoniae | Alcoholism, aspiration | Leucopenia, cavitation, empyema |
| Acinetobacter baumannii | Alcoholism, aspiration | |
| Pseudomonas aeruginosa | Smoking, aspiration, HIV, structural lung disease | |
| Haemophilus influenzae | Aspiration, COPD, smoking, HIV, i.v. drug abuse | |
| Moraxella catarrhalis | COPD, smoking | |
| Respiratory viruses | Viral pandemics | Interstitial infiltrates or normal chest radiography |
| Mycoplasma pneumoniae | Cyclical pandemics | Headache, erythema multiforme, positive cold agglutinin titres |
| Chlamydophilia | Interstitial infiltrates | |
| Pneumoniae | COPD, smoking | |
| Psittaci | Exposure to birds | Horder spots, transaminitis |
| Anaerobes | Alcoholism, aspiration, i.v. drug abuse | Cavitation |
| Mycobacterium tuberculosis | Alcoholism, HIV, i.v. drug abuse |
Streptococcus pneumoniae
Streptococcus pneumoniae is a gram-positive α-haemolytic capsulated organism. Infective risk is highest in the immunocompromised, elderly, and hyposplenic patients, although overall frequency is reducing due to vaccination against this pathogen. The clinical response after infection is related to pneumococcal virulence factors and the genetic background of the patient. These indices are believed to alter the systemic inflammatory response that is produced through pneumococcal infection. Although the overall incidence of penicillin resistance is reducing in adults, antibiotic-resistant S. pneumoniae may be seen in several patient groups including: severely ill patients admitted to ICU, those at the extremes of age, patients that have recently received β-lactam therapy, immunosuppressed patients, alcoholics, and patients with medical comorbidities.
Staphylococcus aureus
Staphylococcus aureus is a gram-positive aerobic coagulase-positive diplococcus. Resistant strains such as methicillin-resistant St. aureus (MRSA) are increasingly isolated in patients diagnosed with severe pneumonia, although surveillance and eradication among at-risk patients has been successful in reducing incidence. MRSA is treated with antibiotics such as vancomycin, linezolid, teicoplanin, and rifampicin, although resistance to vancomycin is increasing. Community-acquired MRSA (CA-MRSA) pneumonia may occur in previously healthy patients with no prior healthcare exposure, often after influenza and can predispose to severe necrotizing pneumonia. The incidence of CA-MRSA currently remains low but needs consideration in any younger patient requiring physiological support for severe CAP.
The Panton–Valentine leukocidin (PVL) exotoxin (also referred to as Toxigenic St. aureus) is strongly associated with virulent strains of St. aureus. The PVL gene is carried by both MRSA and methicillin-sensitive St. aureus (MSSA). Most PVL-SA strains are currently MSSA, although there is an increasing association with CA-MRSA infection. PVL-SA strains are usually associated with community-acquired infections, producing a particularly severe form of haemorrhagic pneumonia that is often preceded by a ‘flu-like’ illness or necrotizing soft tissue infection (Table 2). Antimicrobials such as linezolid and clindamycin are thought to be effective at suppressing toxin production.
Table 2.
Panton–Valentine leukocidin St. aureus pneumonia
| Epidemiology | Clinical signs | Investigations |
|---|---|---|
| Immunocompetent adults Community-acquired MSSA strains more common Preceding ‘flu-like’ illness or necrotizing skin infection Household history of PVL-SA skin sepsis Rapidly progressing infection with a high mortality rate |
Haemoptysis Profound hypotension Diarrhoea and vomiting Tachycardia >140 beats min−1 Tachypnoea Skin pustules |
Chest radiography may show multi-lobar infiltrates,
effusions, or cavitation Markedly elevated C-reactive protein Leucopenia Raised creatinine kinase Sputum Gram-film reveals multiple gram-positive cocci Negative pneumococcal and legionella urinary antigens |
Viral pneumonias
Viral infections are an increasingly common cause of severe CAP, accounting for up to 18–30% of cases. In recent years, we have seen the appearance of several virulent respiratory strains that can cause a severe pneumonic disease, progressing to multi-organ failure. These have included avian influenza A virus (H5N1), Middle East respiratory syndrome coronavirus (MERS-CoV), influenza A virus (H1N1), and severe acute respiratory syndrome. Viral pneumonias often have seasonal predilection and may be preceded by a viral prodrome inclusive of fever, myalgia, non-productive cough, and headache. Pregnancy, obesity, chronic disease, advanced age, and immunosuppression are risk factors for severe illness and development of complications.
Nearly 20% of patients with CAP who have proven bacterial pneumonia are co-infected with a virus. It is often unclear if the viral organism is the primary causative pathogen or has predisposed the patient to secondary bacterial infection.2,3 Secondary bacterial infection was reported in 4–24% of patients requiring critical care admission during the H1N1 pandemic in 2009. Streptococcus pneumoniae, St. aureus, and H. influenzae were the more common pathogens isolated in these patients in addition to the virus. Mixed infections are thought to induce a more severe inflammatory response in comparison with an individual pathogen, with variable and overlapping signs and symptoms occurring. Although biomarkers such as C-reactive protein (CRP) are more significantly raised in bacterial disease, they are insufficiently sensitive or specific to be used as sole diagnostic indicators to aid differentiation between bacterial and viral pneumonias. Multiplex polymerase chain reaction (PCR) assays enable concurrent recognition of multiple viruses and is now the gold standard diagnostic test. Routine use of these assays has substantially progressed epidemiological knowledge of respiratory viruses. PCR may be performed on nose and throat swabs and nasopharyngeal and tracheal aspirates.
Healthcare-associated pneumonia
Infections with pathogens usually associated with hospital-acquired pneumonias (HAP) are an emerging cause of CAP. Healthcare-associated pneumonia (HCAP)—in which pneumonia develops in patients who have had recent contact with the healthcare system (Table 3)—is distinguished from CAP not just by the environment in which infections develop but also by the causative pathogens involved. HCAP is often caused by MRSA or multi-drug resistant (MDR) gram-negative pathogens such as Pseudomonas aeruginosa and Klebsiella pneumoniae. HCAP is associated with an increased severity of pneumonia and an excess mortality. This is due to the effects of infection with MDR pathogens and also the age, relatively poor functional status, and related treatment restrictions of those that tend to be affected.
Table 3.
Risk factors for healthcare-associated and MDR pneumonias
| Healthcare-associated pneumonia |
| Chronic haemodialysis |
| Residence in a nursing home or extended care facility |
| Contact with a family member with an MDR pathogen |
| Hospitalization for >2 days during the previous 90 days |
| I.V. antibiotics, chemotherapy, or wound care within previous 30 days |
| Immunosuppressive disease or immunomodulating therapy |
| Multi-drug-resistant organisms |
| Previous antibiotic therapy within 3 months |
| Recent hospitalization |
| Alcoholism |
| Immunosuppression |
| Multiple medical comorbidities (particularly structural lung disease) |
Investigations
General investigations are performed to aid diagnosis, identify the causative pathogen, assess severity, identify complications, and to monitor response to treatment. Investigations should be guided by the severity of pneumonia, previous antibiotic therapy, comorbid illness, and epidemiological factors.
Radiology
Chest radiography (CXR) is the first-line imaging modality in severe CAP. Bacterial and viral pathogens may both induce a wide range of CXR changes. Multi-lobar consolidation is often seen in—although not restricted to—pneumonia involving Legionella, Streptococci, and Staphylococci spp. Staphylococcus pneumonia may present with cavitation and pneumothoraces, whereas CA-MRSA may be associated with rapidly enlarging effusions. Chest ultrasound is useful in confirming the presence of an effusion or empyema and may also assist in identifying the presence of a pneumothorax or fluid overload. Computed tomography (CT) of the thorax should be considered in severe infection or if the patient fails to improve.
Microbiology
In at least 30% of cases, no causative pathogen is isolated. Routine microbiological investigations in severe CAP should include microscopy and quantitative culture of sputum samples, blood cultures, PCR, or direct immunofluorescence of respiratory tract samples, urinary Legionella and pneumococcal antigen tests. Serum pneumococcal antigen may also be detected with a reported sensitivity of 70–80%. Urine antigen tests are more sensitive than blood cultures and will remain positive even after the patient has been exposed to appropriate antibiotic therapy. It is, however, of note that Legionella urine antigen testing will only detect serogroup 1 which is responsible for 80–95% of CAP due to Legionella species and therefore may provide falsely reassuring information. As a general rule, urine antigen tests are most useful for ‘ruling in’ rather than ‘ruling out’ disease, as a negative test result for a specific pathogen may only have a sensitivity of 40–86% in early infection and thus false-negative results are not uncommon. If a patient is Legionella urine antigen-positive, sputum samples should be tested, so that the species of Legionella can undergo epidemiological matching. Bronchoscopy, bronchoalevolar lavage, protected specimen brushing, and thoracocentesis may aid identification of a causative agent when the diagnosis is not established or treatment is failing.
An HIV test should be considered in all patients who are positive for Streptococcus pneumoniae, in severe disease and when atypical features are present. Serological assays may aid in the diagnosis of less common pathogens such as C.burnetii and when PCR is not available. β-d-glucan forms part of the cell wall of fungi including Aspergillus and an assay is available as a means of diagnosing invasive fungal infection. Measurement of procalcitonin (PCT) may help to differentiate between infectious and non-infectious causes of respiratory failure, although must not be used in isolation. PCT can also be used to monitor the efficacy of antibiotic treatment.
Risk stratification
Timely recognition of high-risk patients with severe illness is essential in ensuring that appropriate antibiotic treatment is started promptly and physiological support continues within an appropriate setting. Traditionally, physicians have used clinical evaluation to define severity. Structured severity assessment tools have been developed to assist decision-making regarding critical care admission. They should be used in combination with clinical data, near-patient investigations, and biomarkers to assess severity. Risk stratification tools that are used regularly include the Pneumonia Severity Index (PSI), British Thoracic Society (BTS) CURB-65 score (Table 4), and Severe Community-Acquired Pneumonia Score (Table 5) jointly produced by the American Thoracic Society and Infectious Disease Society of America (ATS/IDSA).2 Both PSI and CURB-65 have been more extensively validated to recognize low-risk patients and are not as good at predicting need for critical care support. Other risk stratification scores have been developed, including SMART-COP (Table 6), which was created to help identify patients who may require invasive respiratory or vasopressor support.4 Both ATS/IDSA and SMART-COP perform well as risk stratification tools in identifying patients who require ICU admission, but further validation is required for both.
Table 4.
CURB-65 severity score
| Prognostic features |
| Confusion—abbreviated Mental Test Score ≤8, or new disorientation in person, place, or time |
| Blood urea >7 mmol litre−1 |
| Respiratory rate ≥30 bpm |
| Blood pressure—diastolic ≤60 mm Hg or systolic <90 mm Hg |
| Age ≥65 yr |
| Risk stratification (each prognostic feature present scores 1 point) |
| 0–1: Low risk (<3% mortality risk) |
| 2: Intermediate risk (3–15% mortality risk) |
| 3–5: High risk (>15% mortality risk) |
Table 5.
ATS/IDSA severe CAP score. A need for NIV can substitute for a respiratory rate ≥30 bpm or a ratio ≤250. The presence of one major, or three or more of nine minor criteria should warrant consideration for critical care admission
| Minor criteria |
| Respiratory rate ≥30 bpm |
| ratio ≤250 |
| Multilobar infiltrates |
| Confusion/disorientation |
| Urea ≥7.14 mmol litre−1 (≥20 mg dl−1) |
| Leukopenia (WBC count <4×109 cells litre−1) |
| Thrombocytopenia (count <100×109 platelets litre−1) |
| Hypothermia (core temperature <36°C) |
| Hypotension (SAP <90 mm Hg; requiring aggressive fluid resuscitation) |
| Major criteria |
| Invasive mechanical ventilation |
| Septic shock with the need for vasopressors |
Table 6.
SMART-COP score of 3 or more points identifies 92% of those who will require intensive respiratory support
| Variable | Points |
|---|---|
| Systolic arterial pressure <90 mm Hg | 2 |
| Multi-lobar involvement on chest radiography | 1 |
| Albumin level <35 g litre−1 | 1 |
| Respiratory rate | 1 |
| 50 yr and younger: ≥25 bpm | |
| Older than 50 yr: ≥30 bpm | |
| Tachycardia (≥125 beats min−1) | 1 |
| New onset confusion | 1 |
| Oxygen level | 2 |
| 50 yr and younger: <70 mm Hg, oxygen saturation ≤93%, or ratio <333 | |
| Older than 50 yr: <60 mm Hg, oxygen saturation ≤90%, or ratio <250 | |
| Arterial pH<7.35 | 2 |
In an aim to improve simplicity through the use of a single stratification tool, NICE have recommended that CURB-65 be used in combination with clinical judgement and arterial blood gas analysis to guide need for critical care admission.5 An approach using early warning scores, a risk stratification tool, and a resuscitation bundle could potentially reduce ICU admissions and mortality.6,7
Management
Diagnosis and aggressive interventions at a very early stage of disease presentation may prevent progression on to multi-organ involvement. Early appropriate parenteral antibiotic administration has been demonstrated to improve patient outcomes, particularly in patients at a higher risk of death.8 The majority of patients that die with severe CAP tend to do so from complications of multi-organ failure rather than from primary respiratory failure alone and often require renal replacement therapy, invasive circulatory monitoring, and support. Adherence to protocols such as those produced by the BTS or IDSA/ATS is associated with a reduction in overall mortality.2,9
Respiratory
Patients with respiratory failure despite high-flow oxygen therapy can be managed with non-invasive ventilation (NIV) or invasive ventilation.10 NIV is of particular benefit in those patients who are immunosuppressed, have underlying obstructive lung disease or Pneumocystis jiroveci infection. A lower ratio and bilateral alveolar infiltrates suggesting acute respiratory distress syndrome (ARDS) are independent predictors of NIV failure and in such patient groups, progression to invasive mechanical ventilation should be considered at an early stage. Early identification of a failed NIV trial is important as several trials have demonstrated poorer outcomes in patients requiring intubation after a prolonged unsuccessful NIV trial. Most patients with severe CAP will require intubation and mechanical ventilation, particularly in the presence of persistent hypoxaemia, severe acidosis, depressed consciousness, or progressive hypercapnia. These patients should be managed with a lung-protective ventilation strategy using low tidal volumes (6 ml kg−1 predicted body weight) and plateau airway pressures <30 cm H2O. Although high PEEP levels may improve oxygenation, there is no mortality difference in comparison with ventilation using low PEEP except in ARDS with a ratio <200 mm Hg.11
Advanced respiratory rescue techniques including prone ventilation, extra-corporeal carbon dioxide removal (ECCO2R), and extra-corporeal membranous oxygenation (ECMO) should be considered in cases of refractory hypoxaemia or symptomatic hypercarbia.12
Cardiovascular
Hypotension should be managed according to the Surviving Sepsis Guidelines of 2012.13 Fluid resuscitation, vasopressor, and inotropic support is guided by clinical assessment in combination with dynamic flow monitoring, including pulse contour analysis devices (LiDCO™, PiCCO™, Vigileo™), transoesophageal Doppler, and transthoracic echocardiography.
Supportive treatment
Standard care for all patients should include adherence to ventilator-acquired pneumonia and catheter-related bloodstream infection bundles, nutritional support, deep venous thrombosis, and gastric ulcer prophylaxis and chest physiotherapy. Steroids are not routinely recommended as adjunctive therapy in hypoxaemic respiratory failure except in P. jiroveci pneumonia. There is currently insufficient evidence to support the use of either G-CSF or statins.
Antimicrobials
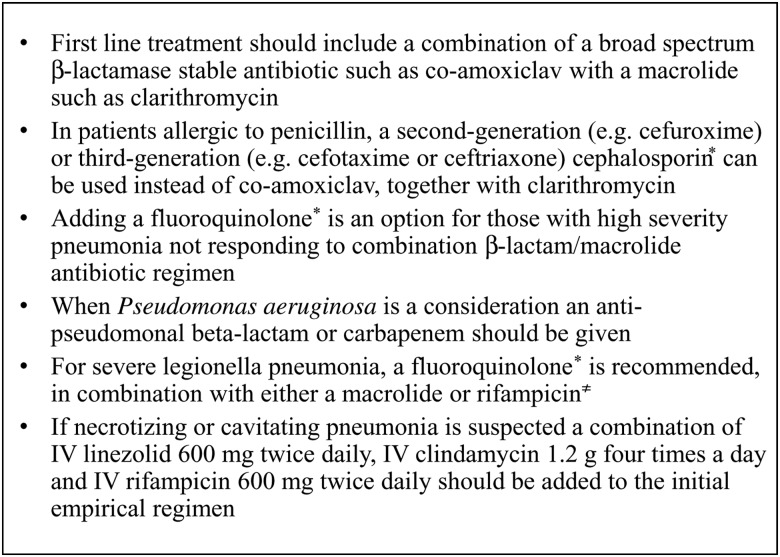
Antibiotic therapy is usually begun on an empirical basis based on severity of illness (often guided by severity scoring such as CURB-65), the BTS (Fig. 1) and NICE guidelines, patient risk factors, and local epidemiology of resistant organisms.5,9 Initial treatment is broad spectrum, aiming to provide cover for S. pneumoniae, St. aureus, Legionella, and gram-negative bacteria. Coverage for atypical bacteria and MDR pathogens should be considered if risk factors for these pathogens are present (Table 2). Atypical and MDR pathogens are more common in patients requiring ICU care. Patients with severe CAP treated with combination antibiotic therapy including a macrolide have an improved survival rate compared with monotherapy. Empirical macrolide monotherapy should be avoided due to emerging pneumococcal resistance. Once a pathogen is identified, antibiotic coverage should be narrowed unless there are concerns about dual pathogen infection. This approach is associated with fewer complications, reduced risk of Clostridium difficile infection, and minimizes development of antibiotic resistance. In severe disease, septic shock or in a non-responding patient, continuous infusions of time-dependent antibiotics such as β-lactams and carbapenems may improve outcome. There is however an elevated risk of both line-related infections and thrombophlebitis, both of which are more prevalent in immunosuppressed patients.14
Fig 1.
Anti-microbial recommendations, amended from BTS Guidelines 2009.9 *Associated with hospital-acquired infections such as Clostridium difficile;≠potential small risk of cardiac electrophysiological abnormalities with quinolone–macrolide combinations.
In patients admitted to ICU, the ideal duration of antibiotic therapy remains uncertain. The BTS and NICE guidelines suggest 7–10 days antibiotic treatment initially. If infection with St. aureus or a gram-negative bacilli is suspected or confirmed, antibiotic therapy should be continued for 14–21 days.9 Cavitating pneumonias and lung abscesses are usually treated for several weeks. Short-course antimicrobial therapy has the potential to improve efficacy and minimize the emergence of resistant organisms. The use of biomarkers such as highly sensitive PCT or CRP may help to reduce the duration of antibiotic treatment without an increase in either mortality or treatment failure.
Treatment for most viral pneumonias is primarily supportive, apart from in patients with severe influenza and patients at high risk of complications. Depending on current local influenza rates, anti-viral therapy may be started empirically while awaiting viral PCR results. Treatment with oseltamivir or zanamivir is recommended for Influenza A infection, and if started within 48 h of symptom onset may reduce the duration of symptoms, severity of disease, and risk of complications. Aerosolized ribavirin may be of benefit in treating respiratory syncytial virus, human metapneumovirus, and parainfluenza infections in immunocompromised patients.
Complications
Patients with severe CAP often have prolonged critical care admissions and are at risk of developing severe septic shock, renal and hepatic failure, coagulopathy, and central nervous system problems including vascular events, encephalopathy, meningitis, and convulsions. Pulmonary-related complications are frequent and depend on the infecting pathogen.
Parapneumonic effusions and empyemas are seen in up to 60% of patients with severe pneumonia. Although many pleural effusions will resolve with appropriate antimicrobial therapy, ultrasound-guided fluid aspiration and analysis should be performed if an effusion is present. Diagnostic aspiration yielding pus, pleural fluid with a pH <7.2, or a positive gram stain or culture are all indications for a tube thoracostomy and drainage of the effusion. Thoracoscopic decortication and drainage should be considered in the presence of an organized empyema or treatment failure.
ARDS. Treatment is primarily supportive using a lung-protective ventilatory strategy. Prone ventilation may be used in severe ARDS with a ratio <150 mm Hg and of at least 0.6.12 Early use of neuromuscular blockers in patients with severe ARDS improves 90 day survival and ventilator-free days.15
Lung cavitation and abscess formation are associated with infection from St. aureus, gram-negative bacilli, Aspergillus, Mycobacterium, and Nocardia species. Failure to respond to antibiotic therapy may raise the possibility of a non-infectious underlying cause such as vasculitis, bronchial obstruction, or infection with a resistant bacteria, mycobacteria, or fungi.
Bacterial and influenza pneumonias are associated with cardiac-related complications including myocardial infarction, arrhythmias, and decompensated cardiac failure. Pulmonary inflammation is thought to trigger cytokine release that up-regulate the inflammation of atherosclerotic plaques, decreasing plaque stability and increasing the risk of rupture. Cardiac events are associated with a substantial increase in mortality.
Failure to respond to treatment
Patients who do not demonstrate improvement within 72 h of commencing antibiotics and supportive care should be considered non-responders. If a patient requires critical care admission, the risk of failure to respond to treatment may be as high as 40% with a mortality that is increased several-fold. Independent risk factors for failure to respond include multi-lobar infection, presence of cavitation or pleural effusions, liver disease, and leucopenia. The efficacy of empirical antimicrobials may be reduced through emerging resistant pathogens such as CA-MRSA, Extended Spectrum β-lactamase-producing organisms, and Carbapenemase-producing Enterobacteriaceae. Failure to respond to treatment should result in re-evaluation of initial microbiological results, supplementary diagnostic testing, and either an escalation or change in antibiotic therapy. Alternative diagnoses such as an eosinophilic or organizing pneumonia need also be considered in patients who are slow or fail to respond to conventional treatment. The possibility of undiagnosed immunosuppression should be investigated and further history explored.
Summary
Despite the advancements in supportive care, severe CAP remains a common reason for critical care admission that is associated with a high mortality. Streptococcus pneumoniae remains the most common pathogen. However, disease due to gram-negative organisms is more frequent in patients requiring critical care admission and are increasingly MDR, despite antibiotic stewardship and increasing surveillance. Further research is needed to elucidate the extent to which viruses are involved in the pathogenesis of severe CAP. Viral and bacterial infections may co-exist, but it is unclear to what extent these organisms are causing the disease or have predisposed the patient to secondary infection. Future developments within this field are likely to concentrate on diagnostics and the ability to identify a causative pathogen within a shorter timeframe.
Declaration of interest
None declared.
MCQs
The associated MCQs (to support CME/CPD activity) can be accessed at https://access.oxfordjournals.org by subscribers to BJA Education.
References
- 1. Walden AP, Clarke GM, McKechnie S et al. Patients with community acquired pneumonia admitted to European Intensive Care Units: an epidemiological survey of the GenOSept cohort. Crit Care 2014; 18: R58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia. Clin Infect Dis 2007; 44(Suppl. 2): S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arnold FW, Summersgill JT, Lajoie AS et al. A worldwide perspective of atypical pathogens in community-acquired pneumonia. Am J Crit Care Med 2007; 175: 1086–93 [DOI] [PubMed] [Google Scholar]
- 4. Charles PG, Wolfe R, Whitby M et al. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis 2008; 47: 375–84 [DOI] [PubMed] [Google Scholar]
- 5. National Institute for Health and Care Excellence. Diagnosis and management of community- and hospital-acquired pneumonia in adults. Clinical guideline 191. December 2014 [PubMed]
- 6. Espana PP, Capelastegui A, Gorordo I et al. Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med 2006; 174: 1249–56 [DOI] [PubMed] [Google Scholar]
- 7. Barochia AV, Cui X, Vitberg D et al. Bundled care for septic shock: an analysis of clinical trials. Crit Care Med 2010; 38: 668–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frei CR, Attridge RT, Mortensen EM et al. Guideline-concordant antibiotic use and survival among patients with community-acquired pneumonia admitted to the intensive care unit. Clin Ther 2010; 32: 293–9 [DOI] [PubMed] [Google Scholar]
- 9. Lim WS, Baudouin SV, George RC et al. Guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 2009; 64(Suppl. III): iii1–iii55 [DOI] [PubMed] [Google Scholar]
- 10. Carrillo A, Gonzalez-Diaz G, Ferrer M et al. Non-invasive ventilation in community-acquired pneumonia and severe acute respiratory failure. Intensive Care Med 2012; 38: 458–66 [DOI] [PubMed] [Google Scholar]
- 11. Briel M, Meade M, Mercat A et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome. J Am Med Assoc 2010; 303: 865–73 [DOI] [PubMed] [Google Scholar]
- 12. Guerin C, Reignier J, Richard JC et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013; 368: 2159–68 [DOI] [PubMed] [Google Scholar]
- 13. Dellinger RP, Levy MM, Rhodes A et al. Surviving sepsis campaign: international guidelines for the management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 2013: 580–637 [DOI] [PubMed] [Google Scholar]
- 14. Kasiakou SK, Sermaides GJ, Michalopoulos A, Soteriades ED, Falagas ME. Continuous versus intermittent intravenous administration of antibiotics: a meta-analysis of randomized controlled trials. Lancet Infect Dis 2005; 5: 581–9 [DOI] [PubMed] [Google Scholar]
- 15. Papazian L, Forel JM, Gacouin A et al. ACURASYS Study Investigators. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010; 363: 1107–16 [DOI] [PubMed] [Google Scholar]