Abstract
Dysregulated type I interferon (IFN-I) expression can lead to severe pathology and disease. In this issue of Cell Host & Microbe, Channappanavar et al. (2016) use a SARS-coronavirus animal model to describe how rapid and robust virus replication with delayed IFN-I can lead to lung immunopathology, with fatal outcomes.
Dysregulated type I interferon (IFN-I) expression can lead to severe pathology and disease. In this issue of Cell Host & Microbe, Channappanavar et al. (2016) use a SARS-coronavirus animal model to describe how rapid and robust virus replication with delayed IFN-I can lead to lung immunopathology, with fatal outcomes.
Main Text
Type I interferons (IFNs-I) are important components of our innate immune system. Upon pathogen encounter, specific signatures named pathogen-associated molecular patterns (PAMPs) are recognized by host cell pathogen recognition receptors (PRRs) to induce the expression and secretion of IFN-I, other cytokines, and chemokines. This “first alarm” has two major consequences. First, IFN-I can bind its cellular receptor to induce a signaling cascade that culminates in the expression of hundreds of IFN-stimulated genes (ISGs), some of which are known to have antiviral effector function. ISG expression will turn our cells into the so-called “antiviral state,” which makes our cells more resistant to virus infection and thereby limits virus spread. Second, (pro)inflammatory cytokines and chemokines will attract a variety of immune cells, including macrophages, neutrophils, NK cells, dendritic cells, and others, that further combat virus infection locally and initiate the adaptive immune response.
Within the airways—the main entry port of respiratory viruses—innate immune responses are of particular importance. The epithelial layer is an important barrier to infection, and epithelial cells represent the first target cells of many human respiratory viruses. Limiting virus replication and spread is instrumental to secure lung epithelium integrity until the adaptive, more pathogen-specific immune response will come into play. Accordingly, viruses have evolved to evade innate immune responses. Their primary goal is to establish a robust infection in initial target cells in order to propagate and spread within the host and to transmit virus progenies to new hosts.
The Coronavirus family comprises viruses of veterinary and medical importance that are mainly associated with respiratory and enteric infection. Human respiratory coronaviruses have been known since the 1960s to circulate worldwide and to cause respiratory infection with rather mild symptoms (common cold), suggesting that they are well adapted to the human host. However, zoonotic coronaviruses, such as severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV), can cause severe respiratory tract infection with high mortality. Severe cases of SARS have been reported with high serum levels of proinflammatory cytokines, increased accumulation of monocyte-macrophages and neutrophils in the lung, and, accordingly, extensive lung damage. Notably, severe immunopathology driven by extensive inflammation is known from other coronaviruses, namely mouse hepatitis virus (MHV) and feline infectious peritonitis virus. However, the causes and consequences are still poorly understood, and therapeutic intervention is limited.
The work of Channappanavar et al. (2016) in this issue of Cell Host & Microbe presents how SARS-CoV can cause exuberant inflammatory host responses with consequences of severe lung pathology. They used a murine model of SARS with a mouse-adapted SARS virus (maSARS-CoV) (Roberts et al., 2007) and observed fast and robust virus replication accompanied by a delayed IFN-I response in BALB/c mice. Remarkably, the virus reached peak titers in the lung already at day 1 post-infection, a time point where coronavirus-induced IFN-I responses are only beginning to mount. Indeed, delayed IFN-I responses are well known for coronaviruses that efficiently evade PRR, namely MDA5, sensing. It has been shown by numerous studies in the MHV system that, following MHV infection, IFN-I expression is barely detectable in most cell types. Coronavirus IFN-I evasion is multifaceted, including sequestering and shielding dsRNA within double membrane vesicles, modification of viral mRNA 5′-cap structures, and specific targeting of antiviral cellular pathways, such as OAS-RNaseL, by viral accessory gene functions (Kindler and Thiel, 2014, Zhao et al., 2012). Plasmacytoid dendritic cells (pDCs) are a notable exception. They utilize TLR7 to sense viral nucleic acids and can induce robust IFN-I expression following coronavirus infection (Cervantes-Barragan et al., 2007). Channappanavar and colleagues noticed that pDCs also appear to be among the most important IFN-I-producing cell types in their murine model of SARS.
IFN-I expression and signaling is absolutely essential for survival of mice following MHV infection (Cervantes-Barragan et al., 2007), an observation that has been made for many viruses. However, IFN-I can also have immunosuppressive potential, accompanied with chronic immune activation during persistent lymphocytic choriomeningitis virus infection (Teijaro et al., 2013, Wilson et al., 2013), or pathogenic potential, manifested by increased lung damage during acute influenza virus infection (Davidson et al., 2014). Channappanavar et al. have observed that IFN-I expression can actually also be detrimental during acute SARS-CoV infection. Compared to MHV, an important difference appears to be the extremely rapid replication of maSARS-CoV in BALB/c mice that, together with the upcoming—but delayed—IFN-I response, orchestrated extensive lung inflammation. This was accompanied by influx of inflammatory monocyte-macrophages (IMMs), which were attracted by inflammatory mediators. Detrimentally, IMMs themselves additionally produced (through IFN-I stimulation) high levels of inflammatory mediators, such as CCL2, CCL7, and CCL12, resulting in further IMM influx and massive accumulation of pathogenic inflammatory IMMs that increased the severity of SARS. Finally, to complete the picture of IFN-I-induced immune dysregulation, Channappanavar et al. observed that also T cells, which would normally promote virus clearance, are sensitized by IFN-I to apoptosis, resulting in reduced numbers of virus-specific CD8 and CD4 T cells.
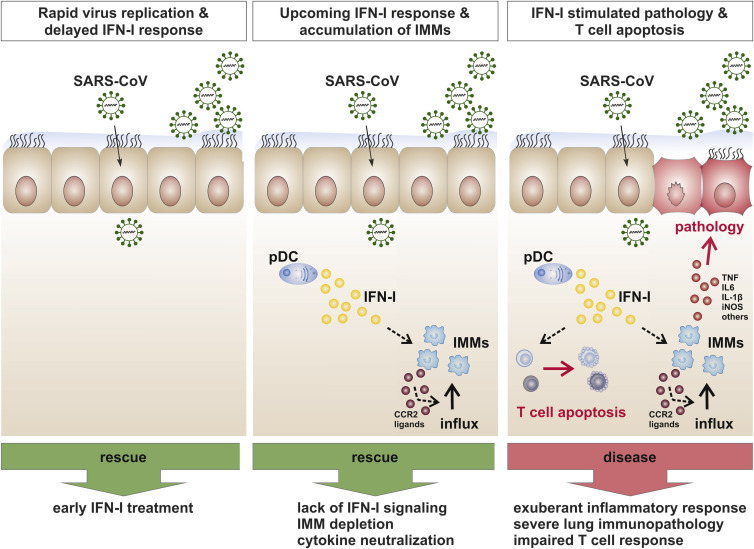
What we can learn from this work is that antiviral innate immune responses can, under certain circumstances, get out of balance and become immunopathogenic. In the case of SARS, the important parameters of the delicate balance of virus-host interactions are: (1) fast and robust initial virus replication while IFN-I expression is delayed, (2) recruitment of immunopathogenic immune cells by inflammatory mediators, and (3) impairment of T cell responses (Figure 1 ). However, this work also pinpoints possible avenues for preventive or therapeutic intervention. IFN-I is in fact protective if applied very early after infection. At later time points, when IFN-I and inflammatory cytokines become pathogenic, depletion of IFN-I and/or inflammatory cytokines, inhibition of IFN-I/cytokine signaling, or depletion of IFN-I/cytokine-producing cells may be valid treatment options to bring the exaggerating immune response back to balance.
Figure 1.
Development of Lethal Pneumonia by Dysregulated IFN-I and Exaggerated Inflammatory Responses in SARS-CoV-Infected Mice
Robust early SARS-CoV replication in the lung and delayed IFN-I expression (left panel) initiate a cascade of IFN-I mediated immune dysregulation. The upcoming IFN-I and cytokine response leads to recruitment of inflammatory monocyte-macrophages (IMMs) that, stimulated by pDC-derived IFN-I, release inflammatory mediators (CCR2 ligands; middle panel). This results in increased IMM influx, exuberant inflammation, and severe lung immunopathology. T cell responses are reduced through IFN-I-mediated T cell apoptosis (right panel). Possible preventive or therapeutic treatment options are early IFN-I treatment (left panel), inhibition of IFN-I signaling, IMM depletion, or cytokine neutralization (middle panel).
SARS was a zoonotic disease, and the observed immune dysregulation is probably not uncommon when viruses cross the species barrier. There are many examples of avian influenza virus strains that cause severe disease in humans. In fact, it has been proposed that one important factor for the high pathogenicity of the influenza virus strain causing the Spanish flu pandemic was the fast virus replication kinetics (Tumpey et al., 2005). Evolutionarily, however, viruses are well adapted to their natural host, and severe disease is the exception rather than the rule for many virus infections. Successful transmission is an important driving force for virus evolution and adaptation to the host. We have also seen that the mortality rate of SARS infections was declining at later stages during the SARS outbreak, suggesting that the virus was adapting to the new host. Thus, it is actually favorable for viruses to leave a window of opportunity for the host to clear virus infection, as long as transmission is granted. Nevertheless, one important parameter that made it possible to eventually halt the SARS outbreak was that disease symptoms become apparent before patients were infectious. This made the containment of infected individuals and vigorous contact tracing a successful strategy to interrupting infection chains. While we still don’t know which viral functions contribute to SARS-CoV-induced immune dysregulation, we observe that other human coronaviruses usually cause only mild disease. This is in fact also true for MERS-CoV in its natural host, the dromedary camel (Adney et al., 2014). Whether a similar type of IFN-I-driven immune dysregulation may apply to MERS-CoV infections in humans remains to be determined.
Acknowledgments
This work was supported by the Swiss National Science Foundation (SNF project 149784).
References
- Adney D.R., van Doremalen N., Brown V.R., Bushmaker T., Scott D., de Wit E., Bowen R.A., Munster V.J. Emerg. Infect. Dis. 2014;20:1999–2005. doi: 10.3201/eid2012.141280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes-Barragan L., Züst R., Weber F., Spiegel M., Lang K.S., Akira S., Thiel V., Ludewig B. Blood. 2007;109:1131–1137. doi: 10.1182/blood-2006-05-023770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channappanavar R., Fehr A.R., Vijay R., Mack M., Zhao J., Meyerholz D.K., Perlman S. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson S., Crotta S., McCabe T.M., Wack A. Nat. Commun. 2014;5:3864. doi: 10.1038/ncomms4864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindler E., Thiel V. Curr. Opin. Microbiol. 2014;20:69–75. doi: 10.1016/j.mib.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A., Deming D., Paddock C.D., Cheng A., Yount B., Vogel L., Herman B.D., Sheahan T., Heise M., Genrich G.L. PLoS Pathog. 2007;3:e5. doi: 10.1371/journal.ppat.0030005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teijaro J.R., Ng C., Lee A.M., Sullivan B.M., Sheehan K.C., Welch M., Schreiber R.D., de la Torre J.C., Oldstone M.B. Science. 2013;340:207–211. doi: 10.1126/science.1235214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumpey T.M., Basler C.F., Aguilar P.V., Zeng H., Solórzano A., Swayne D.E., Cox N.J., Katz J.M., Taubenberger J.K., Palese P., García-Sastre A. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- Wilson E.B., Yamada D.H., Elsaesser H., Herskovitz J., Deng J., Cheng G., Aronow B.J., Karp C.L., Brooks D.G. Science. 2013;340:202–207. doi: 10.1126/science.1235208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L., Jha B.K., Wu A., Elliott R., Ziebuhr J., Gorbalenya A.E., Silverman R.H., Weiss S.R. Cell Host Microbe. 2012;11:607–616. doi: 10.1016/j.chom.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]