Abstract
Objective
This study sought to evaluate the sustained value of an early pregnancy assessment clinic (EPAC) in the management of early pregnancy complications and its effect on the incidence emergency room (ER) visits.
Methods
A 10-year retrospective study (January 2006 to December 2015) was conducted. The number of patients assessed, sources and reasons for referral, and treatments provided were reviewed. The numbers of ER assessments and reassessments for abortion, hemorrhage, and ectopic pregnancy from January 2004 to December 2005 (pre-EPAC) and January 2006 to December 2015 (post-EPAC) were also reviewed.
Results
There were 11 349 new referrals and 10 764 follow-up visits. The reasons for referral were threatened miscarriage (n = 3568, 31.4%), missed miscarriage (n = 3056, 26.9%), incomplete miscarriage (n = 1064, 9.4%), complete miscarriage (n = 991, 8.7%), ectopic pregnancy (n = 857, 7.6%), hyperemesis gravidarum (n = 139, 1.2%), and others (n = 1674, 14.8%). There has been a significant decreasing trend (tau = −0.60, P = 0.0127) and a significant decrease in the post-EPAC rate of ER reassessments (P = 0.0396) for hemorrhage, with a concomitant decrease in EPAC visits for hemorrhage. In addition, there has been a significant increasing trend (tau = 0.64, P = 0.0081) and a significant increase in the post-EPAC rate of ER assessments (P = 0.00001) for ectopic pregnancies.
Conclusion
Over the 10-year period, the EPAC has remained a vital service for managing early pregnancy complications for women. However, the clinic has not yet had a sustained impact on ER visits for miscarriage, ectopic pregnancy, and hemorrhage. It is possible that a reduction in ER assessments and reassessments for early pregnancy complications can be achieved through a clinic with daily access.
Key Words: Early pregnancy complications, miscarriage, hemorrhage, ectopic
Résumé
Objectif
Cette étude visait à évaluer la valeur à long terme d'une clinique d'évaluation précoce de la grossesse (EPAC) dans la prise en charge des complications en début de grossesse ainsi que l'incidence sur les visites aux urgences.
Méthodologie
Nous avons mené une étude rétrospective sur 10 ans (de janvier 2006 à décembre 2015). Nous nous sommes penchés sur le nombre de patientes examinées à l'EPAC, les sources et les motifs de recommandation et les traitements prodigués. Nous avons également examiné le nombre d'évaluations et de réévaluations aux urgences pour un avortement, des saignements et une grossesse extra-utérine de janvier 2004 à décembre 2005 (avant l'EPAC) ainsi que de janvier 2006 à décembre 2015 (après la mise en place de l'EPAC).
Résultats
Pendant la période à l'étude, il y a eu à l'EPAC 11 349 nouvelles recommandations et 10 764 visites de suivi. Voici les motifs des recommandations : risque de fausse couche (n = 3 568; 31,4 %), fausse couche asymptomatique (n = 3 056; 26,9 %), fausse couche incomplète (n = 1 064; 9,4 %), fausse couche complète (n = 991; 8,7 %), grossesse extra-utérine (n = 857; 7,6 %), hyperemesis gravidarum (n = 139; 1,2 %) et autres (n = 1 674; 14,8 %). On notait une importante tendance à la baisse (tau = −0,60; P = 0,0127) et une baisse significative dans le taux de réévaluations faites aux urgences (P = 0,0396) pour des saignements après la mise en place de l'EPAC, de même qu'une baisse des visites à l'EPAC pour le même motif. En outre, on observait une importante tendance à la hausse (tau = 0,64; P = 0,0081) et une hausse significative des taux d'évaluation aux urgences après la mise en place de l'EPAC (P = 0,00001) pour une grossesse extra-utérine.
Conclusion
Pendant les 10 années de l'étude, l'EPAC est demeurée un service essentiel pour la prise en charge des complications en début de grossesse. Cette approche n'a toutefois pas entraîné d'effet durable sur les visites aux urgences pour une fausse couche, une grossesse extra-utérine ou des saignements. Il se pourrait qu'un accès quotidien à une EPAC permette une réduction des évaluations et des réévaluations aux urgences pour des complications en début de grossesse.
Introduction
Early pregnancy complications are common scenarios accounting for about 15% to 20% of all pregnancies.1, 2 The causes of early pregnancy loss include fetal chromosomal abnormalities, maternal conditions, intrauterine infections, maternal-fetal incompatibilities, and unknown causes.1 The early pregnancy assessment clinic (EPAC) model has been shown to provide improved efficiency and quality of care in the management of early pregnancy complications.3 EPACs are not common in Canada; however, they are becoming increasingly popular. In Vancouver, British Columbia, patients reported satisfaction with the emotional support and care provided at an EPAC,4 and in Halifax, Nova Scotia, an early pregnancy complications clinic provides care to women with early pregnancy losses.5
An EPAC at North York General Hospital in Toronto, Ontario was established in August of 2005. The clinic continues to serve women from anywhere in central Toronto and the greater Toronto area of Ontario. The model of the clinic was described in our previous study in 2009.6 Since then the hours of the clinic have remained the same, and over 20 000 visits were made between August 2005 and 2015. The aim of the present study was to assess whether the EPAC has had a sustained impact over the 10 years of the study period on the management of early pregnancy complications and on the number of assessments and reassessments in the emergency room (ER).
Methods
The clinic data from the EPAC database and patients' records from Powerchart between January 2006 and December 2015 (years 1–10) were reviewed. The number of women assessed, the sources of referral, the reasons for referral, the final diagnoses, and the treatments provided at the clinic were analyzed. The total number of ER visits per year, the number of initial consultations, and repeat assessments within 30 days for abortion, hemorrhage, and ectopic pregnancy were obtained from the health records department. The ER data were obtained between January 2004 (year −1) to December 2005 (year 0) before and just after the opening of EPAC (pre-EPAC) and between January 2006 and December 2015 (years 1–10) after the opening of EPAC (post-EPAC). The classification of these selected pregnancy-related complications determined on the basis of ICD 10 classification: abortion/miscarriage (codes 002 and 003), early pregnancy hemorrhage (code 020), and ectopic pregnancy (code 000). The code 020 for early pregnancy hemorrhage includes threatened abortion and other hemorrhage in early pregnancy.
Statistical Analysis
ER assessment and reassessment rates of each early pregnancy complication (miscarriage, ectopic pregnancy, and hemorrhage) were calculated by setting the denominator as the child-bearing (aged 15 to 49) female population in each corresponding year. This population was used because of the lack of availability of data on pregnant women population sizes. The child-bearing female population statistics for the catchment area of the hospital (previously described) were obtained from the Census Program of Statistics Canada,7 which releases data every 5 years. The census data for the years 2001, 2006, 2011, and 2016 were used. The child-bearing female population sizes for the remaining years (2004–2005, 2007–2010, and 2012–2015) were predicted using linear regression of child-bearing population on year from the 2001 to 2016 census data.
Exploratory Analysis
An exploratory data analysis was conducted on both ER assessment and ER reassessment data sets by calculating the assessment and reassessment rates for each of the three early pregnancy complications.
Pre-EPAC and Post-EPAC Comparison
Next, the difference between the average pre-EPAC and the average post-EPAC ER assessment and reassessment rates for each early pregnancy complication was tested by a chi-square test.
Trend Analysis of ER Assessments and Reassessments
Finally, because of limited pre-EPAC data, a rank-based nonparametric Mann-Kendall test8, 9, 10 was used to detect monotonic trends in rates of ER assessments and reassessments for miscarriage, ectopic pregnancy, and hemorrhage since the implementation of the EPAC. The Mann-Kendall test was applied specifically to test the data against a null hypothesis of no monotonic trend against an alternative hypothesis of downward monotonic trend between 2005 and 2015 (years 1–10).
All statistical and graphic analyses were performed using R statistical software version 3.3.3 (The R Project for Statistical Computing, Vienna, Austria; www.r-project.org/). The trend analysis was conducted by the package “trend” in R to detect trends in assessment and reassessment rates over 10 years. Graphs were made using the library ggplot2 (www.ggplot2.org). Statistical significance was decided at a 5% significance level.
The study was approved by the Ethics Review Board of North York General Hospital, a community hospital affiliated with the University of Toronto.
Results
From January 2006 to December 2015, there were 11 349 new referrals and 10 764 follow-up visits to the EPAC. A total of 5069 referrals (44.7%) were from the ER, 3024 referrals (26.6%) were from family physicians, 2140 referrals (18.9%) were from obstetrician-gynaecologists, 242 referrals (2.1%) were from midwives, and 874 referrals (7.7%) were from other sources. The reasons for referral were threatened miscarriage (3568 patients, 31.4%), missed miscarriage (3056, 26.9%), incomplete miscarriage (1064, 9.4%), complete miscarriage (991, 8.7%), ectopic pregnancy (857, 7.6%), hyperemesis gravidarum (139, 1.2%), and others (1674, 14.8%). The final diagnoses of patients referred are shown in Table 1 . The clinic arranged dilatation and curettage for 2169 women (19.1% of referred patients), and 1451 women (12.8%) were administered misoprostol to induce miscarriage. A total of 231 women (2%) with ectopic pregnancy were administered methotrexate.
Table 1.
Final diagnoses of patients referred to the early pregnancy assessment clinic
| Diagnosis | n (%) |
|---|---|
| Missed miscarriage | 2758 (24.3) |
| Threatened miscarriage | 2170 (19.1) |
| Complete miscarriage | 1959 (17.3) |
| Incomplete miscarriage | 1522 (13.4) |
| Ectopic gestation | 680 (6.0) |
| Hyperemesis gravidarum | 139 (1.2) |
| Others | 2058 (18.1) |
| Lost to follow-up | 63 (0.6) |
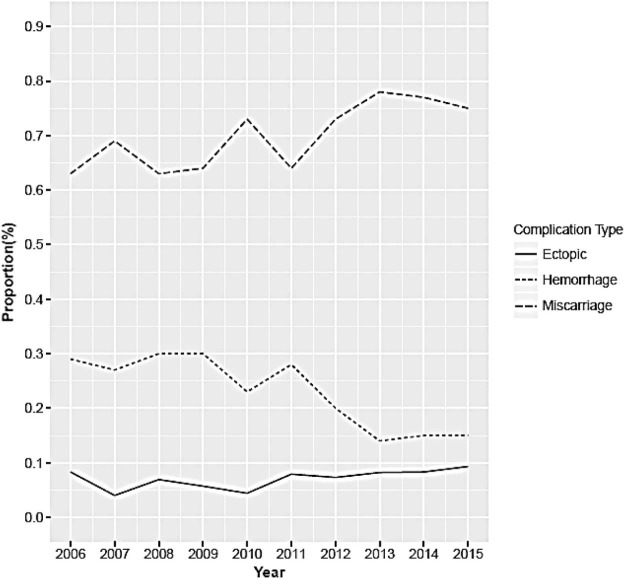
The trends in EPAC visits for early pregnancy complications during the 10-year period are shown in the Figure . There has been an increasing trend in the number of EPAC visits for miscarriage and ectopic pregnancy since the opening of the clinic, whereas there has been a decreasing trend in the number of visits for hemorrhage.
Figure.
Trend in early pregnancy assessment clinic visits for miscarriage, hemorrhage, and ectopic pregnancy.
Exploratory Analysis
The numbers of ER assessments and reassessments for these early pregnancy complications are shown in Table 2 . During the 2 years before the establishment of the EPAC (pre-EPAC: year −1 to year 0), there was a total of 126 540 ER visits, of which 1897 visits were for hemorrhage, 899 were for miscarriage, and 118 were for ectopic pregnancy. There were 599, 162, and 39 ER reassessments for these diagnoses, respectively. During the 10-year period after the opening of the EPAC (post-EPAC: years 1–10), there was a total of 850 051 ER visits, of which 10 262 visits were for hemorrhage, 5818 were for miscarriage, and 1413 were for ectopic pregnancy. There were 2610, 935, and 335 ER reassessments for these diagnoses, respectively.
Table 2.
ER assessments and reassessments data for three early pregnancy complications
| Year | Total ER Assessments | Miscarriage |
Ectopic pregnancy |
Hemorrhage |
|||
|---|---|---|---|---|---|---|---|
| Assessments | Reassessments | Assessments | Reassessments | Assessments | Reassessments | ||
| 2004 | 61 155 | 466 | 90 | 54 | 15 | 924 | 286 |
| 2005 | 65 385 | 433 | 72 | 64 | 24 | 973 | 313 |
| 2006 | 67 932 | 438 | 55 | 58 | 14 | 963 | 285 |
| 2007 | 70 509 | 462 | 78 | 62 | 9 | 1079 | 297 |
| 2008 | 72 440 | 550 | 85 | 114 | 28 | 1171 | 292 |
| 2009 | 78 650 | 589 | 104 | 187 | 53 | 1166 | 225 |
| 2010 | 80 291 | 707 | 126 | 163 | 34 | 1267 | 245 |
| 2011 | 85 331 | 602 | 97 | 137 | 33 | 967 | 251 |
| 2012 | 91 770 | 625 | 106 | 144 | 31 | 959 | 300 |
| 2013 | 96 476 | 654 | 112 | 175 | 45 | 888 | 275 |
| 2014 | 101 250 | 598 | 92 | 170 | 30 | 875 | 233 |
| 2015 | 105 402 | 593 | 80 | 203 | 58 | 927 | 207 |
ER: emergency room.
The incidence rates of ER assessment and reassessment rates for miscarriage, ectopic pregnancy, and hemorrhage between 2004 and 2015 (during the pre-EPAC and post-EPAC periods) are presented in Table 3 .
Table 3.
Incidence ratesa for miscarriage, ectopic pregnancy, and hemorrhage at ER assessments and reassessments
| Year (year defined) | Child-bearing population | Miscarriage rate per 1000 females |
Ectopic pregnancy rate per 1000 females |
Hemorrhage rate per 1000 females |
|||
|---|---|---|---|---|---|---|---|
| Assessments | Reassessments | Assessments | Reassessments | Assessments | Reassessments | ||
| 2004 (year −1) | 1 442 356 | 0.32 | 0.062 | 0.037 | 0.010 | 0.64 | 0.20 |
| 2005 (year 0) | 1 456 220 | 0.30 | 0.049 | 0.044 | 0.016 | 0.67 | 0.21 |
| 2006 (year 1) | 1 481 565 | 0.30 | 0.037 | 0.039 | 0.009 | 0.65 | 0.19 |
| 2007 (year 2) | 1 483 949 | 0.31 | 0.053 | 0.042 | 0.006 | 0.73 | 0.20 |
| 2008 (year 3) | 1 497 813 | 0.37 | 0.057 | 0.076 | 0.019 | 0.78 | 0.19 |
| 2009 (year 4) | 1 511 677 | 0.39 | 0.069 | 0.124 | 0.035 | 0.77 | 0.15 |
| 2010 (year 5) | 1 525 541 | 0.46 | 0.083 | 0.107 | 0.022 | 0.83 | 0.16 |
| 2011 (year 6) | 1 565 970 | 0.38 | 0.062 | 0.087 | 0.021 | 0.62 | 0.16 |
| 2012 (year 7) | 1 553 270 | 0.40 | 0.068 | 0.093 | 0.020 | 0.62 | 0.19 |
| 2013 (year 8) | 1 567 134 | 0.42 | 0.071 | 0.112 | 0.029 | 0.57 | 0.18 |
| 2014 (year 9) | 1 580 998 | 0.38 | 0.058 | 0.108 | 0.019 | 0.55 | 0.15 |
| 2015 (year 10) | 1 594 862 | 0.37 | 0.051 | 0.127 | 0.036 | 0.58 | 0.13 |
ER: emergency room.
Rates were calculated using child-bearing age women population of the corresponding year as the denominator.
Pre-EPAC and Post-EPAC Comparison
The average rates of ER visits for early pregnancy complications compared between the pre-EPAC and post-EPAC periods are presented in Table 4 . There was a significant increase in the post-EPAC rate compared with the pre-EPAC rate of ER assessments for miscarriage (P = 0.0016) and ectopic pregnancy (P = 0.00001). There was no significant difference in the post-EPAC and pre-EPAC rates of ER assessment for hemorrhage.
Table 4.
| Mean incidence rate per 1000 women |
||||
|---|---|---|---|---|
| Complication | Pre-EPAC | Post-EPAC | Difference (95% CI) | P valuec |
| ER assessments | ||||
| Miscarriage | 0.31 | 0.38 | −0.07 (−0.11, −0.03) | 0.0016 |
| Ectopic pregnancy | 0.041 | 0.091 | −0.05 (−0.07, −0.03) | 0.00001 |
| Hemorrhage | 0.65 | 0.67 | −0.02 (−0.06, 0.03) | 0.4783 |
| ER reassessments | ||||
| Miscarriage | 0.056 | 0.061 | −0.005 (−0.027, 0.017) | 0.7031 |
| Ectopic pregnancy | 0.013 | 0.022 | −0.009 (−0.021, 0.003) | 0.1725 |
| Hemorrhage | 0.21 | 0.17 | 0.04 (0.02, 0.07) | 0.0396 |
EPAC: early pregnancy assessment clinic; ER: emergency room.
Years −1 to 0, byears 1–10, cChi-square test.
There were also no significant differences in the post-EPAC and pre-EPAC rates of ER reassessments for miscarriage and ectopic pregnancy. Conversely, there was a significant decrease in the average rate of post-EPAC reassessments for hemorrhage compared with pre-EPAC reassessment (0.17 vs. 0.21, P = 0.0396).
Trend Analysis of ER Assessments and Reassessments
The results of the trend analysis of ER assessments and reassessments for early pregnancy complications since the opening of the EPAC are presented in Table 5 . There was a significant increasing trend in the percentage of ER assessments for ectopic pregnancy and a non-significant increasing trend in the percentage of ER assessments for miscarriage. There were increasing trends in ER reassessments for miscarriage and ectopic pregnancy that were non-significant. There was a significant decreasing trend in ER reassessments for hemorrhage (tau = −0.60, P = 0.127) and a non-significant decreasing trend in ER assessments for hemorrhage.
Table 5.
Trend analysis of the percentage of ER assessments and reassessments from 2005 to 2015
| Complication | ER assessment |
ER reassessment |
||
|---|---|---|---|---|
| Tau | P valuea | Tau | P valuea | |
| Miscarriage | 0.42 | 0.0868 | 0.31 | 0.2129 |
| Ectopic pregnancy | 0.64 | 0.0081 | 0.46 | 0.0617 |
| Hemorrhage | −0.46 | 0.0617 | −0.60 | 0.0127 |
ER: emergency room.
Mann-Kendall trend test for downward monotonic trend.
Discussion
Early pregnancy complications occur in about 15% to 20% of all pregnancies,1, 2 and they can result in significant psychiatric morbidity.11 After a miscarriage, women can experience increased anxiety, which can persist for several weeks after the pregnancy loss,11 and they can also experience emotions of grief, dysphoria, and guilt.12 Often women experiencing a miscarriage receive care in the ER, where they frequently can be faced with long wait times and fragmented care from several health care providers.13 These women can also feel that their experiences of loss are not adequately acknowledged in the ER and that there is a lack of clear discharge education and follow-up instructions, all of which can leave them feeling marginalized.14 Despite this, the ER remains the first contact for these women.
It has been shown that patient satisfaction with the medical care received after a miscarriage is improved when there is a follow-up appointment soon after the loss, with sufficient time to discuss patients' feelings and questions.12 EPACs provide a resource for women to receive treatment for pregnancy complications, as well as the appropriate follow-up appointments, thus enhancing the efficiency and quality of care provided.3
In addition, several studies have shown that the implementation of an EPAC can significantly reduce the admissions rate for early pregnancy complications from the ER.15, 16, 17, 18 However, there are fewer studies exploring the effect of the EPAC model of care on the number of assessments and reassessments in the ER for early pregnancy complications. An Australian study found that following the establishment of an early pregnancy problem service clinic, there was a significant reduction in the median length of stay in the ER for women experiencing pain or bleeding in early pregnancy; however, there was a non-significant reduction in the proportion of assessments and reassessments in the ER.19 Another study found that implementing the use of a gynaecology outpatient clinic decreased the proportion of ER assessments for miscarriages from 31% in 2001 to 17% in 2009.20
Our study showed that throughout a 10-year period, the EPAC has continued to provide care to women with early pregnancy complications; however, there has not been an impact in reducing the number of ER assessments and reassessments for miscarriage and ectopic pregnancy. The significant decreasing trend seen in the percentage of ER reassessments for hemorrhage is likely not a result of the EPAC because there was a concomitant decrease in EPAC visits for hemorrhage during the same period.
The increase in ER assessments and reassessments for miscarriage and ectopic pregnancy is mirrored by an increase in EPAC clinic visits for these conditions. Therefore, the EPAC is continuing to manage these early pregnancy complications successfully in response to population trends and needs. However, it is speculated that the lack of impact on ER visits could reflect the clinic's limited hours of operation, which has remained unchanged since its implementation at 3 half-days a week. The Royal College of Obstetricians and Gynaecologists in the United Kingdom recommended that early pregnancy units should be easily accessible and available to patients on a daily basis during the normal working week for the service to be effective.21 Thus, for there to be an improvement in the impact of the EPAC at North York General Hospital, it would be important for the clinic to open daily to increase access for patients and reduce ER visits. This would improve the efficiency of the service.
Furthermore, with greater awareness about the EPAC service over the 10-year study period, there has been an increase in referrals for early pregnancy complications that likely would not have come to North York General Hospital otherwise. Therefore, it is possible that the increasing number of ER visits reflects patients presenting to the ER as a means of being referred to the EPAC and/or patients who were seen at the EPAC and decided to return specifically to the North York General Hospital ER for new concerns. The increase in ER visits could also reflect the appropriateness of the counselling provided to patients at EPAC. The ability of staff to counsel patients properly on what to expect with different types of management (i.e., misoprostol vs. expectant management for miscarriage) and when they should go the ER can also affect the trend in ER visits. In the future, as patient counselling improves and other EPACs are implemented, it is likely that ER visits for early pregnancy complications will be reduced.
There are several limitations to our study. When analyzing the pre-EPAC data, we were able to obtain data only from 1 year (2004) before the implementation of the EPAC, for two reasons: First, the National Ambulatory Care Reporting System coding that we used to extract ER early pregnancy complications data was not implemented until April 2002. Second, in 2003, as a result of the outbreak of severe acute respiratory syndrome, the number of ER visits was significantly low during the summer months; therefore, the 2003 data were not used in our analysis. The limited pre-EPAC data reduced the effectiveness of evaluating the sustainability of EPAC (comparing pre-EPAC with post-EPAC average ER visit rates) and also restricted the use of more appropriate statistical analysis such as an interrupted time-series analysis. If there had been more pre-EPAC data, it is possible that different trends may have been seen in ER visits for early pregnancy complications. Because of these limitations, a Mann-Kendall test was used to detect any monotonic trends in ER assessment rates and reassessment rates for early pregnancy complications after the EPAC opened. Furthermore, covariates such as patients' age, GA, infections in pregnancy, education, and socioeconomic status were not included in the trend and pre-EPAC vs post-EPAC analyses. These covariates may affect the number of ER assessments and reassessments. In addition, we did not have a link between the ER data and the EPAC data to determine whether patients seen in the ER were being followed up in the EPAC.
Conclusion
We hope that in the future, with expanded clinic operating hours, the EPAC will go beyond providing care for women and will represent an improved efficient pathway in the management of early pregnancy complications and in reducing the ER workload. Our study demonstrates the value of providing standardized care for women undergoing early miscarriage through the implementation and funding of EPAC models where one-stop comprehensive care can be offered. We hope that the findings of our study will inform stakeholders and policy makers in making the care of women undergoing early pregnancy loss a priority in Ontario and in Canada as a whole.
Acknowledgements
This study was funded by a grant from the Sheila Cohen Foundation and North York General Hospital Foundation. A special thank you goes to Dr Adrian Brown for helping to facilitate the funding. Acknowledgement also goes to bio-statistician Dushanthi Pinnaduwage, PhD, for performing the statistical analysis. We would also like to thank Michael Misinai, an Application Consultant at North York General Hospital for his assistance in working with the database. Finally, the authors would like to thank all their colleagues who have worked tirelessly to make the EPAC a success.
Footnotes
Competing interests: See Acknowledgements.
References
- 1.Alberman E. Spontaneous abortion: epidemiology. In: Stabile S., Grudzinkas G., Chard T., editors. Spontaneous abortion: diagnosis and treatment. Springer; London: 1992. pp. 9–20. [Google Scholar]
- 2.Wilcox A.J., Weinberg C.R., O'Connor J.F. Incidence of early loss of pregnancy. N Engl J Med. 1988;319:189–194. doi: 10.1056/NEJM198807283190401. [DOI] [PubMed] [Google Scholar]
- 3.Bigrigg M.A., Read M.D. Management of women referred to early pregnancy assessment unit: care and effectiveness. Br Med J. 1991;302:577–579. doi: 10.1136/bmj.302.6776.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhone S.A., Hodgson Z.G., Moshrefzadeh A. A Canadian urban early pregnancy assessment clinic: a review of the first year of operation. J Obstet Gynaecol Can. 2010;34:243–249. doi: 10.1016/S1701-2163(16)35184-2. [DOI] [PubMed] [Google Scholar]
- 5.Lu-Olaco E., Baskett T.F. 2011. Outcomes in an early pregnancy complications clinic: a five year audit, 2005–2009. Abstract presented at the 25th Annual Resident Research Day, Department of Obstetrics, Dalhousie University. Halifax, NS. [Google Scholar]
- 6.Tunde-Byass M., Cheung V.T.Y. The value of the early pregnancy assessment clinic in the management of early pregnancy complications. J Obstet Gynaecol Can. 2009;31:841–844. doi: 10.1016/S1701-2163(16)34302-X. [DOI] [PubMed] [Google Scholar]
- 7.Statistics Canada Population Estimates and Projections. http://www.statcan.gc.ca/eng/subjects/population_and_demography/population_estimates_and_projections Available at:
- 8.Mann H.B. Nonparametric tests against trend. Econometrica. 1945;13:245–259. [Google Scholar]
- 9.Kendall M.G. 4th ed. Griffin; London: 1975. Rank correlation methods. [Google Scholar]
- 10.Gocic M., Trajkovic S. Analysis of changes in meteorological variables using Mann-Kendall and Sen's Slope estimator statistical tests in Serbia. Glob Planet Change. 2013;100:172–182. [Google Scholar]
- 11.Thapar A.K., Thapar A. Psychological sequelae of miscarriage: a controlled study using the general health questionnaire and hospital anxiety and depression scale. Br J Gen Pract. 1992;42:94–96. [PMC free article] [PubMed] [Google Scholar]
- 12.Brier N. Understanding and managing the emotional reactions to a miscarriage. Obstet Gynecol. 1999;93:151–155. doi: 10.1016/s0029-7844(98)00294-4. [DOI] [PubMed] [Google Scholar]
- 13.Baciadore V., Warren N., Chaput C. A collaborative framework for managing pregnancy loss in the emergency department. J Obstet Gynecol Neonatal Nurs. 2009;38:730–738. doi: 10.1111/j.1552-6909.2009.01075.x. [DOI] [PubMed] [Google Scholar]
- 14.MacWilliams K., Hughes J., Aston M. Understanding the experience of miscarriage in the emergency department. J Emerg Nurs. 2016;42:504–512. doi: 10.1016/j.jen.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Sørensen J.L., Bødker B., Vejerslev L.O. [An outpatient unit for early pregnancy. Establishment and effects on the pattern of hospital admissions] Ugeskr Laeger. 1999;161:158–161. in Danish. [PubMed] [Google Scholar]
- 16.van den Berg M.M., Goddijn M., Ankum W.M. Early pregnancy care over time: should we promote an early pregnancy assessment unit? Reprod Biomed Online. 2015;31:192–198. doi: 10.1016/j.rbmo.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Wendt K., Crilly J., May C. An outcomes evaluation of an emergency department early pregnancy assessment service and early pregnancy assessment protocol. Emerg Med J. 2014;31:e50–e54. doi: 10.1136/emermed-2013-202887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rotheray K.R., Woo W.W., Graham C.A. An early pregnancy assessment clinic combined with emergency physician ultrasound reduces admissions [letter] Emerg Med Australas. 2010;22:194. doi: 10.1111/j.1742-6723.2010.01278.x. [DOI] [PubMed] [Google Scholar]
- 19.Brownlea S., Holdgate A., Thou S.T. Impact of an early pregnancy problem service on patient care and emergency department presentations. Aust N Z J Obstet Gynaecol. 2005;45:108–111. doi: 10.1111/j.1479-828X.2005.00351.x. [DOI] [PubMed] [Google Scholar]
- 20.Adolfsson A., Tullander-Tjörnstrand K., Larsson P.G. Decreased need for emergency services after changing management for suspected miscarriage. Acta Obstet Gynecol Scand. 2011;90:921–923. doi: 10.1111/j.1600-0412.2011.01144.x. [DOI] [PubMed] [Google Scholar]
- 21.Royal College of Obstetricians and Gynaecologists . 2006. The management of early pregnancy loss. Green-top guideline No. 25. London: Royal College of Obstetricians and Gynaecologists. [Google Scholar]