Abstract
This study assesses patterns of caregiving, death, and recovery after incident disability in older adults. We used the Health and Retirement Study to follow of a cohort of adults age ≥65 in the United States with incident disability in activities of daily living (ADLs) or instrumental activities of daily living (IADLs) (n=8,713). Rates of care and function state were assessed biennially: deceased, nursing home dwelling, at home with paid help, at home with both paid and unpaid help, at home with unpaid help, at home with no assistance and recovered. In the two years after incident disability, 22.1% recovered and 46.8% died. Transitions between care and function states occurred frequently, with more than 20% of the cohort living at home with no assistance despite disability at least once. This study demonstrates the high levels of care and function state fluctuation and unmet needs after functional disability.
BACKGROUND:
Over the last decade, healthcare expenditures in the United States have remained concentrated, with 50% of spending in the top 5% of the population (Mitchell & Agency for Healthcare Research and Quality, 2016). One segment of high cost older adults is those with functional disability (Aldridge & Kelley, 2014). They are more at risk for persistently high costs as well as potentially burdensome care patterns such as readmissions and hospitalization at the end of life (Depalma et al., 2013; Kelley, Ettner, Morrison, Du, & Sarkisian, 2012). Their functional disability makes them vulnerable to unmet caregiving needs requiring frequent transitions in care (Freedman & Spillman, 2014; Mor, 2014). Transitions, such as from home to an institutional setting, are associated with poor spousal outcomes as well as patient distress (Schulz et al., 2004).
Screening for changes in physical function in older adults is a potential approach to identify high-risk older adults (Fritz & Lusardi, 2009; Wells, Williams, Kennedy, Sawyer, & Brown, 2018). However, this is not routinely done outside of the nursing home setting (Hawes et al., 1995). The importance of function to target interventions has been well-studied (Tak, Kuiper, Chorus, & Hopman- Rock, 2013). We seek to assess the potential role of population-level functional disability screening using a nationally representative survey of aging in order to assess a population-based approach to identify high-risk older adults earlier in the course of illness.
METHODS:
This study used data from the Health and Retirement Study (HRS), a longitudinal, nationally representative panel survey of United States (US) adults aged ≥51 years and their spouses (Sonnega et al., 2014). The HRS conducts inperson or telephone surveys biennially, with initial response rates of 79% and follow-up rates of 85% to 91%. If individuals are unable to respond, proxy reporters are utilized. All participants provided informed consent and this study was determined by our institutional review board to be exempt from review.
Cohort:
We identified a cohort of HRS participants aged ≥65 years reporting incident ADL disability, IADL disability or both ADL and IADL disability between 2000 and 2012. Incident disability was defined as the first report of needing assistance or having difficulty with at least one ADL/IADL and a minimum lookback of 1 survey wave. ADLs include bathing, eating, dressing, walking across a room, and getting in/out of bed and toileting. IADLs included making hot meals, grocery shopping, using the telephone, taking medications and managing money. While ADLs occur later and are followed by higher mortality rates than IADLs (Lawton & Brody, 1969), we screened for both to identify disability earlier in order to best follow patterns over time.
We then created a subgroup of individuals with at least 10 years of follow up in order to assess how common and transitory different care and function states were for individuals. This subgroup therefore included individuals with incident ADL/IADL disability occurring in either 2000 or 2002.
Measurements:
The primary outcome measurement was the proportion of participants in each function and care state at follow-up relative to years since incident disability. The participants’ function and care states were determined at each follow-up assessment as: was the individual deceased; if not deceased, did he/she still have a disability; if so, did he/she reside in a nursing home or at home; and if at home, did he/she report assistance for that disability from unpaid (family or friend) or paid caregivers. This was ascertained from separate questions on death, disability, nursing home residence, and assistance with disabilities asked at each 2-year survey wave. Function and care states were thus defined as: (1) deceased, (2) disabled in a nursing home, (3) disabled at home with paid caregivers, (4) disabled at home with both paid and unpaid caregivers, (5) disabled at home with unpaid caregivers, (6) disabled at home with no assistance, or (7) recovered. In addition, demographics, self-reported illnesses and household characteristics as assessed by the HRS were included.
Analysis:
We described the demographics, self-reported illnesses and household characteristics at baseline for each individual in the incident ADL/IADL disability cohort. We then calculated proportions of individuals in each function and care state relative to years since incident disability.
Next, we assessed patterns of function and care state transitions for individuals, using the subgroup of individuals with 10 years of follow up. In order to assess both how common and how transitory each function and care state is, we measured the proportion of individuals ever experiencing each state and the average amount of time spent in it.
All proportions and lengths of time were adjusted for survey weighting and sampling strategy. We applied subjects’ last available survey weights for individuals who were deceased or residing in nursing homes. Analysis was performed using Stata (StataCorp), version 14.0.
RESULTS:
The characteristics of the 8,713 older adults with incident ADL/IADL impairment are shown in Table 1. The cohort’s mean age was 78 years. Notably, 17.8% of the cohort reported themselves to be in poor health and an additional 31.9% described their health as fair. Rates of comorbidities were high, with 71.7% having arthritis, 37.7% reporting that they have heart disease and 53.1% reporting they had 3 or more comorbidities. A large number (37.4%) lived alone, nearly the same as the proportion that had children living within ten miles (37.9%).
Table 1.
Baseline cohort characteristics of those with incident ADL/IADL impairment (n = 8,713).
| Demographics | |
| Female | 52.7% |
| Age, M (SD) | 78.0 (0.15) |
| Race | |
| White | 87.4% |
| Black | 9.5% |
| Other | 3.1% |
| Hispanic | 5.5% |
| Net worth, M (SD) | US$387,655 (US$19,452) |
| Self-reported health | |
| Excellent | 3.7% |
| Very good | 15.4% |
| Good | 31.2% |
| Fair | 31.9% |
| Poor | 17.8% |
| Proxy reporter | 45.7% |
| Prevalence of select conditions | |
| Arthritis | 71.7% |
| Stroke | 14.6% |
| Heart disease | 37.7% |
| Lung disease | 14.4% |
| Cancer | 20.4% |
| Diabetes | 22.6% |
| Hypertension | 62.8% |
| Household characteristics | |
| Live alone | 37.4% |
| Children within 10 miles | 37.9% |
Source. Health and Retirement Study, 2000–2012.
Note. Net worth is derived from multiple assessments of household assets and reported in 2012 USD. ADL = activities of daily living; IADL = instrumental activities of daily living.
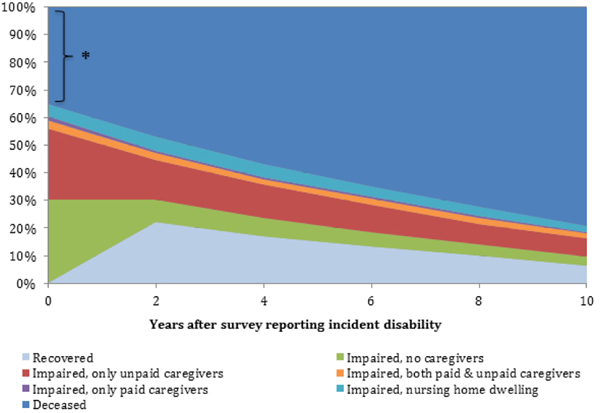
Individuals with incident ADL/IADL disability had mean follow-up of 4.2 biennial survey waves, representing 8 years of follow-up on average. Two years after onset of ADL or IADL disability, 46.8% of individuals in the cohort were deceased and by 10 years 79.4% were deceased (Figure 1). While 22.1% of individuals were recovered 2 years after onset of disability, only 6.43% remained without disability 10 years later.
Figure 1.
Proportion of older adults with incident disability in each function and care state over 10 years of follow-up (n=8,713)
*Individuals with both incident disability and death before the next HRS survey wave.
Most of the flux in caregiving states occurred in the two years after disability. Over these two years, the proportion of disabled older adults with no caregivers fell from 46.8% to 26.2%, some of which was due to recovery. At the same time, there was an increase in the proportion reporting unpaid caregiving, from 39.8% to 45.9%. There was also an increase in nursing home care from 7.0% to 16.4%. Over the entire decade, those reporting concurrent paid and unpaid caregiving increased, from 4.3% to 13.2%.
The second stage of the analysis examined the individual patterns of caregiving for ADL/IADL disabilities for those with a potential observation period of at least 10 years. Table 2 demonstrates the proportion of individuals experiencing each function and care state over the next decade, and the mean years spent in each state for those who experienced it. Death was the most common state following disability, with deceased individuals dying a mean of 1.14 years after onset of disability. The next most commonly experienced state was unpaid care (40.1%), with individuals reporting unpaid care for a mean of 3.89 years, followed by no assistance (36.0%), reported on average for 3.37 years. The state that individuals experience for the shortest length of time was receiving both paid and unpaid home-based care, with individuals in this state for a mean of 2.93 years, followed by paid home-based care, with the average individual in this state for a mean of 2.93 years.
Table 2.
Transition between and mean time in function and care states during the 10 years after incident ADL/IADL disability.
| Death | Unpaid home-based care | No care, living at home | Recovery | Nursing home care | Both paid and unpaid home-based care | Paid home-based care | |
|---|---|---|---|---|---|---|---|
| Proportion experiencing each state over the 10 years after disability | 79.4% | 40.1% | 36.0% | 29.0% | 13.8% | 9.5% | 3.9% |
| Mean years in each statea | 8.86b | 3.89 | 3.37 | 4.77 | 3.29 | 2.59 | 2.93 |
Note. ADL = activities of daily living; IADL = instrumental activities of daily living.
Mean years in each state was assessed only for those reporting the specific state at least once.
This indicates that deceased individuals died a mean of 1.14 years after the first report of disability.
DISCUSSION:
This study demonstrates patterns of recovery, death, and caregiving following incident disability in a nationally representative sample of older adults in the United States. While recovery was common, especially in the 2 years after onset of disability, death and recurrent or persistent disability were more likely. Caregiving patterns demonstrated significant numbers of transitions among caregiving arrangements over time.
This study suggests people experience significant fluctuations in disability, caregiving, and overall health in the first years after the onset of disability. For individuals following incident ADL/IADL disability, 22.1% have recovered by year two (although fewer than half of these will still be without disability 6 years later) and 46.9% have died. The rate of durable recovery that we find is lower than in other studies (Hardy & Gill, 2004). This is likely because we are likely missing more transient, minor episodes of disability occurring and resolving between HRS survey waves. The proportion receiving both paid and unpaid care at home as well as nursing home care increases by more than 100% over the first two years after incident disability. Most states of care measured are short-term with only 20.0% of those receiving paid home based care and 23.1% receiving both paid and unpaid care at home in the same situation two years later.
The number of individuals reporting no assistance despite disability is sizable and deserves further study. For those surviving individuals who were disabled, 46.8% reported no assistance although this declined to 26.2% two years later. It will be important to understand the factors underlying this lack of assistance and the health outcomes of these individuals. Other literature has demonstrated the health consequences of having unmet caregiving needs. Our population-level estimates of the size of this population indicate unmet care needs is a major public health issue.
This study has several limitations. While the HRS is advantageous in that it allows following individuals for over a decade, it is conducted biennially; therefore, there may be transitions in care, recovery, and disability occurring between survey waves. In addition, the HRS describes caregiving as assistance with ADL and IADLs while other types of support such as emotional support, companionship, and assisting with medical care are not captured. In order to define caregiving states as relatively few categories, we do not include the range of variation within each state, such as caregiving hours or number of caregivers. Understanding how caregiving networks change over time is a separate and valuable research area. Although the HRS utilizes proxy respondents for cognitively impaired individuals, there is evidence that this contributes little bias (Weir, Faul, & Langa, 2014). Finally, this study describes the population-level patterns after disability. Further work will determine the individual clinical (comorbidities, dementia), household (caregiver presence and wealth) and regional (health system and wealth) factors that influence outcomes after disability.
Given the high cost of medical and institutional care for disabled older adults, it is critical to understand how caregiving context and patterns change over time. This study demonstrates significant flux in the care patterns of older adults following disability. Future research will be needed to link the observed patterns to patient and caregiver reported quality of care. Furthermore, a sizable portion of individuals die in the years following report of new ADL or IADL disability and yet disability is not systematically screened for in health care settings or captured consistently in medical records. While previous work has contextualized functional disability in a context of recovery or rehabilitation, the magnitude of death and caregiver burden indicate that there is need for support and palliation for this population as well. In particular, efforts by health insurers to consider both the caregiving and support as well as health care needs for this population is a promising direction to better address the needs of older adults with functional disability. Future work to explore the benefits and implementation of screening for disability will be a critical step to improve quality of care for all older adults.
References
- Aldridge MD, & Kelley AS (2014). Epidemiology of Serious Illness and High Utilization of Healthcare, Appendix E In Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Institute of Medicine of the National Academies. [Google Scholar]
- Depalma G, Xu H, Covinsky KE, Craig BA, Stallard E, Thomas J, & Sands LP (2013). Hospital readmission among older adults who return home with unmet need for ADL disability. Gerontologist, 53(3), 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, & Spillman BC (2014). Disability and care needs among older Americans. The Milbank Quarterly, 92(3), 509–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz S, & Lusardi M (2009). Walking speed: the sixth vital sign. Journal of Geriatric Physical Therapy, 32(2), 1–5. [PubMed] [Google Scholar]
- Hardy SE, & Gill TM (2004). Recovery from disability among community dwelling older persons. JaMa, 291(13), 1596–1602. [DOI] [PubMed] [Google Scholar]
- Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, & Nonemaker S (1995). Reliability estimates for the Minimum Data Set for nursing home resident assessment and care screening (MDS). Gerontologist, 35(2), 172–178. [DOI] [PubMed] [Google Scholar]
- Kelley AS, Ettner SL, Morrison RS, Du Q, & Sarkisian C. a. (2012). Disability and decline in physical function associated with hospital use at end of life. Journal of General Internal Medicine, 27(7), 794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of Older People: Self- Maintaining and Instrumental Activities of Daily Living. The Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Mitchell EM, & Agency for Healthcare Research and Quality. (2016). Statistical Brief #497: Concentration of Health Expenditures in the U.S. Civilian Noninstitutionalized Population, 2014. Retrieved from https://meps.ahrq.gov/data_files/publications/st497/stat497.pdf [PubMed]
- Mor V (2014). The adverse consequences of unmet need among older persons living in the community: dual-eligible versus Medicare-only beneficiaries. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69, S51–S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Belle SH, Czaja SJ, Mcginnis KA, Stevens A, & Zhang S (2004). Long-term Care Placement of Dementia Patients and Caregiver Health and Well-being. JAMA, 292(8), 961–967. [DOI] [PubMed] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, & Weir DR (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tak E, Kuiper R, Chorus A, & Hopman-Rock M (2013). Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: A meta-analysis. Ageing Research Reviews, 12(1), 329–338. [DOI] [PubMed] [Google Scholar]
- Weir DR, Faul JD, & Langa KM (2014). Proxy interviews and bias in the distribution of cognitive abilities due to non-response in longitudinal studies: a comparison of HRS and ELSA. Longit Life Course Stud., 2(2), 170–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells EU, Williams CP, Kennedy RE, Sawyer P, & Brown CJ (2018). Factors That Contribute to Recovery of Community Mobility After Hospitalization Among Community-Dwelling Older Adults. Journal of Applied Gerontology, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]