Abstract
Background
Healthcare personnel (HCP) are at risk of being exposed to or transmitting infections in hospitals, and vaccination against vaccine-preventable diseases (VPDs) is a well-known preventive strategy. Vaccination against influenza, hepatitis B virus, measles-mumps-rubella, varicella, and pertussis is recommended for HCP. However, there is no information on the current status of hospitals' vaccination policies for HCP in Korea.
Methods
We conducted a nationwide survey on hospital vaccination policies and barriers to implementing recommended vaccination programs in 2018. The online survey questionnaire was distributed to 652 hospitals, and 200 of them responded.
Results
Of the 200 surveyed hospitals, 151 (75.5%) conducted a pre-employment screening program for at least one VPD, and 196 (98%) had vaccination programs that included at least one vaccine. Influenza vaccine was most commonly included in their programs (97.5%, n = 195), followed by hepatitis B vaccines (69%, n = 138). However, < 25% of the hospitals included other vaccines in their policies (measles-mumps-rubella, 24.5%; varicella, 18.5%; pertussis, 11%). Only 13 hospitals (6.5%) included the five recommended vaccines for HCP in their policies. Influenza vaccination coverage had a mean of 89.9% and was significantly higher in hospitals fully funding the vaccination cost (91.8% vs. 80.4%, P < 0.001). Among hospitals funding influenza vaccines, the coverage was lower in hospitals with ≥ 700 beds (−6.5%, P = 0.003). Hospitals' financial burden was the most important barrier to implementing vaccination polices as recommended (78.6%, 121/154), followed by lack of awareness (21%) or campaign (21%) and lack of leadership (17%).
Conclusion
Despite the recommendations on vaccination for HCP, the vaccination policies for HCP differ in hospitals and appear to be insufficient to protect HCP and prevent nosocomial transmission. Strong leadership of each hospital to protect HCP and financial support from the government are required to implement appropriate vaccination policies in hospitals.
Keywords: Vaccine, Healthcare Personnel, Policy
Graphical Abstract
INTRODUCTION
Healthcare personnel (HCP) are at risk of exposure to and transmission of vaccine-preventable diseases (VPDs) in their occupational settings.1 Vaccinating HCP is one of the main strategies to protect them and prevent transmission of VPDs.
In Korea, the National Immunization Program (NIP) has long been established and has provided free vaccines against VPDs to children,2 and for the elderly population aged ≥ 65 years, influenza and pneumococcal vaccines are also provided. The coverage rates of vaccines included in the NIP were estimated to be high in children (average coverage, > 95%).3 However, because immunity against these VPDs decreases over time and vaccination does not always confer full protection against VPDs, the vaccination status of HCP should be up-to-date. In Korea, measles outbreaks were noted in hospitals in 2007, where 45% of the confirmed cases of measles resulted from nosocomial transmission.4 Recently, measles outbreaks occurred in Korean hospitals.5 A recent study showed the considerably low seroprevalence of measles in HCP in their twenties (60%).6 The seroprevalence of pertussis was also reported to be low among HCP (33.7%), proposing booster immunization of pertussis in HCP in Korea.7
The Korean Society of Infectious Diseases (KSID) and the Korean Centers for Disease Control and Prevention (KCDC) jointly recommend that HCP receive vaccines against seasonal influenza, measles-mumps-rubella (MMR), varicella, tetanus-diphtheria-pertussis (Tdap), and hepatitis B.8 However, a survey on physicians revealed that < 10% of physicians have knowledge of HCP vaccination, and vaccine coverage was also low.9 Moreover, there was no information on how vaccination programs have been implemented and which vaccines were recommended for HCP in Korean hospitals so far. Vaccination against seasonal influenza is recommended for HCP worldwide, yet vaccination uptake among HCP has not been described on the national level.
This study aimed to investigate the current status of hospital vaccination policies for HCP in Korea and identify the barriers to implementing recommended vaccination programs for HCP. Moreover, we surveyed influenza vaccination coverage among HCP and examined the factors associated with the coverage.
METHODS
Survey description
We conducted a cross-sectional, nationwide survey on vaccination policies of hospitals and influenza vaccination coverage in Korea in May 2018. The survey population included infection control practitioners or HCP in charge of infection prevention and control at their hospitals. We considered that all members at the time of survey (n = 1,717), and the hospitals where they currently worked (n = 652), were the survey targets, given that the majority of infection control practitioners and HCP in this field were enrolled in the Korean Society for Healthcare-associated Infection Control and Prevention (KOSHIC) which is the major professional society establishing infection prevention measures and providing education and training in Korea. Thus, all registered members of the KOSHIC were contacted via email. The survey web link was distributed to all members via email following the announcement that the survey on hospitals' vaccination policies for HCP would be conducted and participation was encouraged. In order to avoid possible selection bias, the details of specific survey topics were not mentioned in advance. They were asked to fill out a web-based, self-administered questionnaire on the hospital's vaccination policy. If multiple members worked at the same hospital, they were asked to answer only one survey questionnaire.
We designed the survey questions based on the KSID's recommendations with reference to the KCDC and CDC. The target individuals were HCP. The target vaccines were seasonal influenza, MMR, varicella, Tdap, and hepatitis B vaccines. Information on other vaccines included in hospitals' policies was also collected.
The questionnaire consisted of three main domains: 1) hospital's vaccination policy for HCP, 2) influenza vaccination coverage among HCP in the previous year and suggested strategies to improve influenza vaccination among HCP, and 3) barriers to implementing recommended vaccination policies. Survey questions were independently reviewed by three infection control experts (two infectious disease specialists and one infection preventionist) from the KOSHIC and the Korean Association of Infection Control Nurses.
Vaccination policies for each of the aforementioned vaccines were categorized as “recommended” or “not recommended.” Each facility's financial coverage for vaccine costs for HCP were classified as “fully covered,” “partially covered,” or “none.” The target HCP of vaccination was classified as “all HCP,” “HCP in direct contact with patients,” or “HCP in high-risk department.”
Strategies to improve influenza vaccine coverage were categorized as financial support, increase awareness with active campaign, education on HCP vaccination, vaccination at workplace, providing incentives to vaccinated HCP, and penalties for unvaccinated HCP. Participants were asked to choose more than one answer and were allowed to suggest other strategies. In terms of barriers to implementation of recommended vaccines, participants were also asked to give their opinions openly.
HCP were defined as all individuals employed in hospitals with or without direct patient care, including physicians, dentists, nurses, and paramedical, laboratory, and administrative personnel regardless of their employment status (permanent, temporary, or contract staff). HCP were also classified into four groups based on their job type: group 1, physicians; group 2, nurses and nurses' aides; group 3, technicians, therapists, emergency paramedical service personnel, laboratory personnel, and pharmacists; and group 4, administrators and other workers.
Statistical analysis
We calculated descriptive statistics for hospital characteristics (bed size, government-funded or private, teaching or non-teaching). The proportions for each vaccine and combination of vaccines implemented in hospitals' vaccination policies were also calculated. We examined the association between hospital characteristics and hospitals' vaccination policies using χ2 tests. Factors associated with influenza vaccination coverage were also investigated using simple and multiple linear regression analyses. A P value < 0.05 was considered significant. Statistical analyses were performed using Stata version 13.0 software (Stata Corporation, College Station, TX, USA).
Ethics statement
This study was approved by the Institutional Review Board of the Kyung Hee University Hospital with waiving the requirement to obtain any informed consent (KHUH 2018-10-032).
RESULTS
Characteristics of respondent hospitals
Of the 652 hospitals that received a survey questionnaire, 200 hospitals (30.1%) responded. These 200 surveyed hospitals were distributed in all 9 provinces and 6 metropolitan cities. The largest number of surveyed hospitals were in Seoul (18%, n = 36) and Gyeonggi (18.5%, n = 37). Considering the total number of healthcare facilities (acute care hospitals and long-term care facilities) in each region,10 the number of surveyed hospitals in each region ranged from 4.2% to 9.7% except for Jeju. The characteristics of surveyed hospitals are summarized in Table 1. A total of 172 hospitals (86.0%) answered that hospital committees for deciding the vaccination policy or similar committees existed. Planning and implementing vaccination programs for HCP was mainly conducted by the infection prevention and control department (53%, n = 106), followed by occupational health nurses (36.5%, n = 73).
Table 1. Characteristics of 200 surveyed hospitals.
| Characteristics | Values | |
|---|---|---|
| Location | ||
| Seoul | 36 (18.0) | |
| Other metropolitan cities | 57 (28.5) | |
| Gyeonggi | 37 (18.5) | |
| Other provinces | 70 (35.0) | |
| Bed size | ||
| < 200 | 62 (31.0) | |
| 200–499 | 90 (45.0) | |
| 500–699 | 17 (8.5) | |
| 700–899 | 20 (10.0) | |
| ≥ 900 | 11 (5.5) | |
| Hospital funding type | ||
| National | 52 (26.0) | |
| Private | 148 (74.0) | |
| Educational type | ||
| Teaching hospital | 77 (38.5) | |
| Non-teaching hospital | 123 (61.5) | |
| Department to implement vaccination programs | ||
| Infection prevention and control | 103 (53.0) | |
| Occupational health | 73 (36.5) | |
| Presence of decision-making committees | ||
| Committees dedicated to vaccination policies | 25 (12.5) | |
| Committees taking the similar role | 147 (73.5) | |
| None | 28 (14.0) | |
Data are presented as number (%).
Hospital vaccination policy for HCP
Of the 200 hospitals, 151 (75.5%) conducted a pre-employment screening program for vaccination status or immunity against at least one VPD. Hepatitis B (74%, n = 148) was the most commonly screened VPD, followed by rubella (19%, n = 38), measles (18%, n = 36), and mumps (17%, n = 34). Screening for Tdap or hepatitis A vaccination was only implemented in ≤ 6% of hospitals.
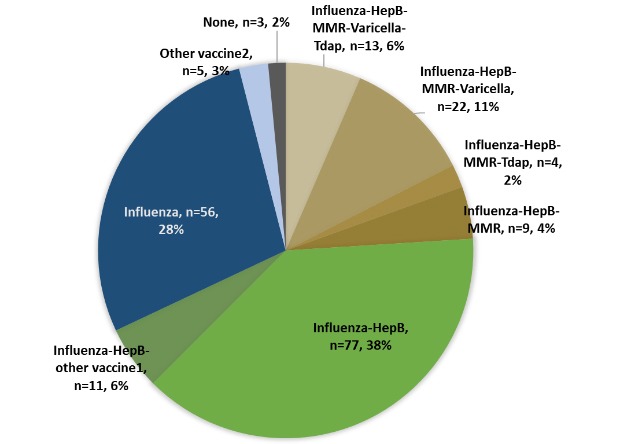
A total of 196 hospitals (98%) had hospital vaccination policies that included at least one vaccine. Influenza vaccine was most commonly included in their policies (97.5%, n = 195), followed by hepatitis B vaccines (69%, n = 138). However, < 25% of hospitals included other vaccines in their policies (MMR, 24.5%; varicella, 18.5%; Tdap, 11%). Only 13 hospitals included all five vaccines (influenza, hepatitis B, MMR, varicella, and Tdap) which are recommended for HCP by the KSID/KCDC in their policies (Table 2). Pre-vaccine screening for immunity against measles (36.7%, 18/49), mumps (30.6%, 15/49), and rubella (38.8%, 19/49) was performed in < 20 of the 49 hospitals that included MMR vaccine in their vaccination program.
Table 2. Vaccines included in hospital vaccination policies for healthcare personnel among 200 surveyed hospitals.
| Vaccination programs | Values |
|---|---|
| Influenza | 56 (28.0) |
| Hepatitis B | 2 (1.0) |
| Influenza-Hepatitis B | 77 (38.5) |
| Influenza-Hepatitis B + Other vaccinesa | 11 (5.5) |
| Influenza-Hepatitis B-MMR | 8 (4.0) |
| Influenza-Hepatitis B-MMR-Hepatitis A | 1 (0.5) |
| Influenza-Hepatitis B-MMR-Tdap | 1 (0.5) |
| Influenza-Hepatitis B-MMR-Tdap-Hepatitis A | 4 (2.0) |
| Influenza-Hepatitis B-MMR-Varicella | 9 (4.5) |
| Influenza-Hepatitis B-MMR-Varicella-Hepatitis A | 13 (6.5) |
| Influenza-Hepatitis B-MMR-Varicella-Tdap | 6 (3.0) |
| Influenza-Hepatitis B-MMR-Varicella-Tdap-Hepatitis A | 7 (3.5) |
| Other combination of vaccinesb | 3 (1.5) |
| None | 3 (1.5) |
Data are presented as number (%).
MMR = measles-mumps-rubella, Tdap = tetanus-diphtheria-pertussis.
aOther vaccines were Tdap (n = 4), varicella vaccine (n = 2), and hepatitis A vaccine (n = 7); bOther vaccines were influenza-Tdap (n = 1), influenza-MMR (n = 1), and influenza-hepatitis A (n = 1).
Vaccines included in the hospital vaccination policies significantly depended on hospital size. Hospitals with ≥ 500 beds were more likely to include MMR (P < 0.001), varicella (P < 0.001), hepatitis B (P = 0.04), and hepatitis A vaccines (P < 0.001) in their hospital policies and fully fund vaccination costs for HCP (Table 3).
Table 3. Vaccines included in the hospital vaccination policies according to the hospital characteristics and target HCP for each vaccine.
| Hospital characteristics | Influenza | Hepatitis B | MMR | Varicella | Tdap | Hepatitis A | |
|---|---|---|---|---|---|---|---|
| No. of hospitals | 195 (97.5) | 138 (69.0) | 49 (24.5) | 37 (18.5) | 22 (11.0) | 32 (16.0) | |
| Full financial support | 155 (79.5) | 78 (56.5) | 32 (65.3) | 19 (51.4) | 13 (59.1) | 11 (34.4) | |
| Bed size | |||||||
| < 200 (n = 62) | 61 (98.4) | 38 (61.3) | 5 (8.1) | 6 (9.7) | 8 (12.9) | 5 (8.1) | |
| 200–499 (n = 90) | 87 (96.7) | 59 (65.6) | 11 (12.2) | 13 (14.4) | 7 (7.8) | 11 (12.2) | |
| 500–699 (n = 17) | 16 (94.0) | 13 (76.5) | 2 (11.8) | 7 (41.2) | 2 (11.8) | 3 (17.6) | |
| 700–899 (n = 20) | 20 (100) | 17 (85.0) | 12 (60.0) | 15 (75.0) | 2 (10.0) | 8 (40.0) | |
| ≥ 900 (n = 11) | 11 (100) | 11 (100) | 7 (63.6) | 8 (72.7) | 3 (27.3) | 5 (45.5) | |
| Hospital funding types | |||||||
| Public (n = 52) | 51 (98.1) | 31 (59.6) | 8 (15.4) | 15 (28.8) | 10 (19.2) | 11 (21.2) | |
| Private (n = 148) | 144 (97.3) | 107 (72.3) | 29 (19.6) | 30 (20.3) | 12 (8.1) | 21 (14.2) | |
| Educational types | |||||||
| Teaching (n = 77) | 11 (100) | 60 (77.9) | 27 (35.1) | 36 (46.8) | 11 (14.3) | 20 (26.0) | |
| Non-teaching (n = 123) | 118 (95.7) | 78 (63.4) | 10 (8.1) | 16 (13.0) | 11 (8.9) | 12 (9.8) | |
| Target HCP for each vaccine | |||||||
| No. of responding hospitals | 186 (95.4) | 119 (86.2) | 35 (71.4) | 27 (73) | 12 (54.5) | 21 (65.6) | |
| All HCP | 184 (98.9) | 63 (52.9) | 8 (22.9) | 8 (29.6) | 4 (33.3) | 8 (38.1) | |
| HCP in direct patient care | 2 (1.1) | 41 (34.5) | 10 (28.6) | 9 (33.3) | 2 (16.7) | 8 (38.1) | |
| HCP in high-risk department | - | 15 (12.6) | 17 (48.6) | 10 (37.0) | 6 (50.0) | 5 (23.8) | |
Data are presented as number (%).
HCP = healthcare personnel, MMR = measles-mumps-rubella, Tdap = tetanus-diphtheria-pertussis.
Of the 197 responding hospitals, 43 events of exposure to VPDs among susceptible HCP occurred in 2017, and exposure to varicella (n = 15) or hepatitis B (n = 11) was the most common.
In terms of barriers to implementing the vaccination policy for HCP as recommended, 154 hospitals (77%) responded to this question. Among these responding hospitals, 78.6% of them (121/154) answered that the hospitals' financial burden for the costs of vaccines and serologic tests was the most important barrier, followed by lack of awareness among HCP (21%, 32/154) or campaign about vaccination (21%, 32/154), and lack of leadership (17%, 26/154).
Influenza vaccination
The influenza vaccination program for HCP was implemented in 195 hospitals. Of these, 155 hospitals (111 hospitals with < 500 beds) provided free influenza vaccines to HCP, and the proportion of hospitals providing free vaccines increased with hospital size: < 200 beds, 72.1% (n = 44); 200–499 beds, 77.0% (n = 67); 500–699 beds, 81.3% (n = 13); and ≥ 700 beds, 100% (n = 31).
The mean vaccination coverage in all surveyed hospitals was 89.9% ± 12.7%, and 77 hospitals answered that the coverage reached up to > 90% in all job types. However, the coverage widely ranged from 22% to 100%. Among the other 118 hospitals whose coverage failed to reach ≥ 90%, 58 hospitals answered that physicians had the lowest coverage, and 19 hospitals answered that administrative personnel had the lowest coverage.
The influenza vaccine coverage was significantly higher in hospitals providing free influenza vaccines and in public hospitals. Interestingly, the vaccine coverage tended to decrease with the hospital size. In a multivariable analysis, full funding for influenza vaccine was the significant factor associated with high vaccine coverage. The vaccine coverage increased by 12.7% (95% confidence interval [CI], 8.0%–17.4%) in hospitals providing free influenza vaccine than in those providing partial or no support (Table 4). We also separately performed multivariable analyses according to the vaccine funding status. Among the hospitals fully funding influenza vaccines, the vaccine coverage significantly decreased with the increase in hospital size (−6.5%, −4.9% and −0.7% in hospitals with ≥ 700 beds, with 500–699 beds, and 200–499 beds respectively, compared to that of hospitals with < 200 beds) and tended to be lower in private hospitals than public hospitals by 4.8%. In contrast, among the hospitals which did not fund or partially fund vaccine costs, there were no differences according to the hospital size, hospital funding type, or education type (Supplementary Table 1).
Table 4. Factors associated with the influenza vaccine coverage among healthcare personnel.
| Factors | Coverage, % | Univariable | P value | Multivariable | P value | |
|---|---|---|---|---|---|---|
| Hospital size, beds | ||||||
| < 200 | 91.5 ± 12.8 | Ref. | Ref. | |||
| 200–499 | 89.3 ± 16.1 | −2.2 (−6.7, 2.2) | 0.33 | −2.5 (−6.2, 2.1) | 0.33 | |
| 500–699 | 88.5 ± 5.3 | −3.1 (−10.7, 4.6) | 0.44 | −3.7 (−11.2, 3.8) | 0.34 | |
| ≥ 700 | 86.9 ± 7.6 | −3.4 (−10.5, 1.2) | 0.12 | −6.1 (−12.6, 0.3) | 0.06 | |
| Funding types | ||||||
| National | 93.1 ± 6.4 | Ref. | Ref. | |||
| Private | 88.3 ± 14.9 | −4.8 (−9.1, −0.5) | 0.03 | −3.2 (−7.4, 0.9) | 0.13 | |
| Education type | ||||||
| Teaching | 88.3 ± 12.6 | Ref. | Ref. | |||
| Non-teaching | 90.4 ± 13.9 | 2.1 (−1.8, 6.0) | 0.30 | 2.5 (−1.9, 7.0) | 0.26 | |
| Financial support for vaccination | ||||||
| Fully funded | 91.8 ± 8.1 | Ref. | Ref. | |||
| Partial or none | 80.4 ± 23.5 | −11.4 (−16.0, −6.9) | 0.00 | −12.7 (−17.4, −8.0) | 0.00 | |
Values are expressed as mean ± standard deviation or coefficient (95% confidence interval).
Among the 199 responding hospitals, funding for vaccine cost (51.7%) was most commonly answered as one of the best strategies to improve vaccine coverage, especially in hospitals with < 500 beds (84.5%, 87/103). A total of 66 hospitals (33.1%) answered a multimodal strategy including financial support, campaign and education, and vaccination at worksite as the best one.
DISCUSSION
This study demonstrated that hospitals' vaccination policies for HCP were diverse depending on hospital characteristics and that only 13% of hospitals included all vaccines recommended for HCP. Financial burden of vaccination and serology tests appeared to significantly influence hospitals' decision on which vaccines to include in their program.
In Korea, studies have shown that immunity against VPDs was insufficient to protect HCP in hospital settings. The seroprevalence of hepatitis B in HCP based on HBs antibody was 76.9% in 2003, which was similar to that in the general Korean population.11 The seroprevalence of pertussis was 33.7% in HCP (134/398, age 21–67 years) in one Korean hospital in 2011.7 The varicella seropositivity rate in HCP was 96% in a single hospital study.12 However, our survey showed that HCP remained at an increased risk of being exposed to varicella-zoster virus considering that HCP exposure to varicella was the most frequent event in 2017.
The seroprevalence of measles in HCP was alarmingly low in Korea.6,13 One study demonstrated that the seroprevalence of measles in HCP born after 1994 was as low as 40% in 2014–2016, which is similar to that in the general population.13 Measles outbreaks in healthcare facilities have been reported even during the post-elimination era worldwide.14,15 In Korea, there have been major measles outbreaks in the community in 2007 and 2014, which ultimately led to multiple nosocomial outbreaks in the same year.4,16 Despite the recent nosocomial outbreaks of measles, this survey showed that < 25% of hospitals included MMR vaccine in their hospital vaccination policy for HCP in 2018. Such a low proportion of hospitals implementing MMR vaccination could be a possible cause of a high number of HCP infected with measles in the 2019 measles outbreak in Korea. During the 2019 outbreak, HCP comprised 32.7% (n = 32) of the 98 outbreak-associated cases.5 The seropositivity rate of measles in young HCP from 6 hospitals in Daegu widely differed from 47% to 85.5%, depending on the hospital vaccination policy.6 This suggested that hospitals should screen HCP for immunity against measles and have their vaccination status up-to-date. The efforts to prevent in-hospital transmission of VPDs need to be made from the stage of healthcare professional schools because medical or nursing students or trainees can encounter similar risks of acquiring VPDs and can be a source of transmission during their training in healthcare settings and they become HCP in the future.17 Therefore, vaccination against airborne VPDs such as measles or varicella needs to be implemented not only in HCP but also in medical, nursing students or other students from healthcare schools.
The KSID/KCDC jointly published vaccination recommendations for HCP in 2012 and 2018.8,18 Vaccinating HCP against varicella, measles, and pertussis was included as one of the quality indicators of neonatal intensive care units in 2018.19 Based on the regulations of the Occupational Safety and Health Act, hospitals are required to provide appropriate vaccination for HCP to prevent infections and screen HCP for immunity against airborne pathogens and provide appropriate vaccines as medically indicated.20 However, recommended vaccination programs were not uniformly implemented in all hospitals. Vaccination policies for HCP substantially differed. According to this survey, the major hindrance to implementing the recommended vaccination policy was hospitals' financial burden. In Korea, the National Health Insurance System (NHIS) has long been established as a single healthcare insurer, covering almost the entire Korean population. However, cost for neither vaccination nor serologic tests for screening immunity against VPDs for HCP is reimbursed by the NHIS even though vaccines are officially recommended for HCP by the KSID/KCDC, which could contribute to hospitals' reluctance to accept the recommended vaccination policy up to a point. Thus, the government effort to reduce hospitals' financial burden might help lower the barrier to implementing recommended vaccinations in hospitals. Moreover, strong leadership and increased awareness of HCP on vaccination are crucial to improve vaccination coverage.
The overall influenza vaccine coverage in HCP was 89.9% during the 2017–2018 influenza season, which was higher than that in other target populations (adults ≥ 65 years, 79.8%) in Korea.21 Despite this, the vaccine coverage widely differed depending on the financial support by hospitals. However, this study also showed that the vaccine coverage was lower in large hospitals although these hospitals provided free influenza vaccine to all HCP. These findings indicate that, along with financial support, a multifaceted strategy including active campaign and continued education, worksite vaccination, incentives, and regulations is needed to improve the influenza vaccination coverage, and such strategy can be applied to promote vaccination against other VPDs.22,23,24
There are some limitations in this study. Firstly, because not all Korean hospitals responded to the survey, there could be selection bias. It is possible that responding hospitals are more likely to have their own vaccination policy and provide free vaccines to HCP. Thus, the number of vaccines included in hospital policies and vaccine coverage might have been overestimated, and the higher proportion of HCP could be vulnerable to VPDs in Korean hospitals. Secondly, information of hospitals vaccination policies was self-reported and difficult to validate externally.
Despite these limitations, this survey provided valuable information on the current status of hospitals' vaccination policies for HCP in Korea and suggested possible solutions to overcome the barriers to improve vaccination policies for HCP. Exposure to VPDs in hospitals can lead to detrimental consequences. Exposed susceptible HCP can be infected and transmit infections to coworkers or patients, and they need to be isolated during the designated duration depending on the pathogens. This results in significant disruption in hospital functions and, consequently, substantial response costs. Also, VPD transmission in hospitals often poses a threat to public health. Thus, not only the hospitals but also the government should take the initiative to improve the vaccination status for HCP. Moreover, individual efforts of HCP to comply with the vaccination recommendations for HCP are necessary for their safety and the safety of patients.
ACKNOWLEDGMENTS
Authors thank all participating infection control practitioners for answering the survey and deeply appreciate the support of the Korean Society of Healthcare-associated Infection Control and Prevention.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Lee MS, Park SH, Kwak YG, Kim SR.
- Data curation: Lee MS, Park SH.
- Formal analysis: Lee MS, Park SH.
- Investigation: Lee MS, Park SH, Kwak YG, Kim SR.
- Methodology: Lee MS, Park SH, Kwak YG, Kim SR.
- Writing - original draft: Park SH.
- Writing - review & editing: Lee MS, Park SH, Kwak YG, Kim SR.
SUPPLEMENTARY MATERIAL
Factors associated with influenza vaccine coverage among healthcare personnel according to the vaccine funding status
References
- 1.Sydnor E, Perl TM. Healthcare providers as sources of vaccine-preventable diseases. Vaccine. 2014;32(38):4814–4822. doi: 10.1016/j.vaccine.2014.03.097. [DOI] [PubMed] [Google Scholar]
- 2.Yun JW, Noh JY, Song JY, Chun C, Kim Y, Cheong HJ. The Korean Influenza National Immunization Program: history and present status. Infect Chemother. 2017;49(4):247–254. doi: 10.3947/ic.2017.49.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korea Centers for Disease Control and Prevention. National Childhood Vaccination Coverage among Children Aged 3 Years in Korea, 2016. Cheongju, Korea: Korea Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 4.Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, et al. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis. 2011;204 Suppl 1:S483–S490. doi: 10.1093/infdis/jir087. [DOI] [PubMed] [Google Scholar]
- 5.Shin NR, Choi S, Jung YH, Kim H, Jung CW, Om J, et al. Measles outbreak and response from December 2018 to May 2019. Public Health Wkly Rep. 2019;12(30):1016–1025. [Google Scholar]
- 6.Chang HH, Kim SW, Kwon KT, Kim HI, Kim MJ, Ryu SY, et al. Preliminary report of seroprevalence of anti-measles immunoglobulin G among healthcare workers of 6 teaching hospitals of Daegu, Korea in 2019. Infect Chemother. 2019;51(1):54–57. doi: 10.3947/ic.2019.51.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi WS, Kim SH, Park DW. Seroprevalence of pertussis in healthcare workers without adult pertussis vaccine use at a university hospital in Korea. J Korean Med Sci. 2018;33(50):e321. doi: 10.3346/jkms.2018.33.e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korea Centers for Disease Control and Prevention. Guidelines for Adult Immunization. 2nd ed. Cheongju, Korea: Korea Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 9.Ko K, Kim S, Kim SH, Son KY, Lee J, Lee DR. Knowledge, current status, and barriers toward healthcare worker vaccination among family medicine resident participants in a web-based survey in Korea. Korean J Fam Med. 2017;38(1):21–27. doi: 10.4082/kjfm.2017.38.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.KOrean Statistical Information Service (KOSIS) Report on healthcare facilities by types and regions, South Korea. [Accessed July 6, 2019]. http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_MIRE01&vw_cd=MT_OTITLE&list_id=354_MT_DTITLE&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K2&path=%252Fcommon%252Fmeta_onedepth.jsp.
- 11.Shin BM, Yoo HM, Lee AS, Park SK. Seroprevalence of hepatitis B virus among health care workers in Korea. J Korean Med Sci. 2006;21(1):58–62. doi: 10.3346/jkms.2006.21.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang JH, Park YS, Park SY, Kim SB, Ko KP, Seo YH. Varicella seroprevalence among health care workers in Korea: validity of self-reported history and cost-effectiveness of prevaccination screening. Am J Infect Control. 2014;42(8):885–887. doi: 10.1016/j.ajic.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Jung J, Kim SK, Kwak SH, Hong MJ, Kim SH. Seroprevalence of measles in healthcare workers in South Korea. Infect Chemother. 2019;51(1):58–61. doi: 10.3947/ic.2019.51.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fiebelkorn AP, Redd SB, Kuhar DT. Measles in healthcare facilities in the United States during the postelimination era, 2001–2014. Clin Infect Dis. 2015;61(4):615–618. doi: 10.1093/cid/civ387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Botelho-Nevers E, Gautret P, Biellik R, Brouqui P. Nosocomial transmission of measles: an updated review. Vaccine. 2012;30(27):3996–4001. doi: 10.1016/j.vaccine.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 16.Park SH, Lee DH, Jin JY, Shin YL, Shin M, Kim SS, et al. Measles outbreaks in the Kyeongin area of the Republic of Korea, 2013–2014: a single-center experience in a country of measles elimination. Asian Pac J Trop Med. 2017;10(1):69–74. doi: 10.1016/j.apjtm.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Dolan SB, Libby TE, Lindley MC, Ahmed F, Stevenson J, Strikas RA. Vaccination policies among health professional schools: evidence of immunity and allowance of vaccination exemptions. Infect Control Hosp Epidemiol. 2015;36(2):186–191. doi: 10.1017/ice.2014.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korea Centers for Disease Control and Prevention. Guidelines for Adult Immunization. 1st ed. Cheongju, Korea: Korea Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 19.Health Insurance Review & Assessment Service (HIRA) Plans on assessing the quality of neonatal intensive care units. [Accessed July 6, 2019]. http://www.hira.or.kr/bbsDummy.do;INTERSESSIONID=pq7LU3viAUEciE0KZE2PqjV_u3wU_TAishVzOrWCc5IQNL8G52bh!517654625!1150782201?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=6811&pageIndex=1#none.
- 20.National Law Information Center. Regulations of Occupational Safety and Health Act [Enforced on March 30, 2018] [Updated 2018]. [Accessed July 6, 2019]. http://www.law.go.kr/%EB%B2%95%EB%A0%B9/%EC%82%B0%EC%97%85%EC%95%88%EC%A0%84%EB%B3%B4%EA%B1%B4%EA%B8%B0%EC%A4%80%EC%97%90%EA%B4%80%ED%95%9C%EA%B7%9C%EC%B9%99.
- 21.Byeon KH, Kim J, Choi B, Choi BY. The coverage rates for influenza vaccination and related factors in Korean adults aged 50 and older with chronic disease: based on 2016 Community Health Survey data. Epidemiol Health. 2018;40:e2018034. doi: 10.4178/epih.e2018034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yue X, Black C, Ball S, Donahue S, De Perio MA, Laney AS, et al. Workplace interventions associated with influenza vaccination coverage among health care personnel in ambulatory care settings during the 2013–2014 and 2014–2015 influenza seasons. Am J Infect Control. 2017;45(11):1243–1248. doi: 10.1016/j.ajic.2017.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.To KW, Lai A, Lee KC, Koh D, Lee SS. Increasing the coverage of influenza vaccination in healthcare workers: review of challenges and solutions. J Hosp Infect. 2016;94(2):133–142. doi: 10.1016/j.jhin.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Jung Y, Kwon M, Song J. Stepwise intervention including 1-on-1 counseling is highly effective in increasing influenza vaccination among health care workers. Am J Infect Control. 2017;45(6):635–641. doi: 10.1016/j.ajic.2016.11.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Factors associated with influenza vaccine coverage among healthcare personnel according to the vaccine funding status


