Abstract
Steroid-resistant nephrotic syndrome (SRNS) is a common cause of chronic kidney disease in children, and a considerable number of patients progress to end-stage renal disease. SRNS is a highly heterogeneous disorder, both clinically and genetically, and more than 50 monogenic causes of SRNS, including isolated and syndromic forms, have been identified. Recent large-cohort studies indicate that at least 30% of childhood-onset SRNS cases are genetic. The benefits of definitive molecular diagnosis by genetic testing include the avoidance of unnecessary and potentially harmful diagnostic procedures (e.g., kidney biopsy) and treatment (e.g., steroid and immunosuppressants), detection of rare and potentially treatable mutations (e.g., coenzyme Q10 biosynthesis pathway defect), prediction of prognosis (e.g., posttransplant recurrence), and providing precise genetic counseling. Furthermore, the identification of novel disease-causing genes could provide new insights into the pathogenic mechanisms of SRNS. Therefore, whenever accessible and affordable, genetic testing is recommended for all pediatric patients with SRNS, and should certainly be performed in patients with a higher probability of genetic predisposition based on genotype-phenotype correlation data. The genetic testing approach should be determined for each patient, and clinicians should, therefore, be aware of the advantages and disadvantages of methods currently available, which include Sanger sequencing, gene panel testing, and whole-exome or whole-genome sequencing. Importantly, the need for precise and thorough phenotyping by clinicians, even in the era of genomics, cannot be overemphasized. This review provides an update on recent advances in genetic studies, a suggested approach for the genetic testing of pediatric patients with SRNS.
Keywords: High-throughput nucleotide sequencing, Phenocopy, Reverse phenotyping, Sanger sequencing, Steroid-resistant nephrotic syndrome
Introduction
The majority of pediatric patients with idiopathic nephrotic syndrome respond well to steroids. However, 10% to 20% of affected children have steroid-resistant nephrotic syndrome (SRNS) [1]. Most SRNS cases are accompanied by focal segmental glomerulosclerosis (FSGS) and progress to end-stage renal disease (ESRD). To date, more than 50 monogenic causes of SRNS/FSGS have been identified, and novel causative genes are continually being discovered [2].
Traditional Sanger sequencing, the classic chain-termination method of DNA sequencing, is the ‘gold standard’, providing high specificity and sensitivity in the genetic diagnosis of hereditary diseases. However, given the large genetic heterogeneity of SRNS, using Sanger sequencing entails significant cost and effort, unless a single or few disease-relevant genes can be identified clinically. However, recent advances in next-generation sequencing (NGS) have provided a revolutionary new approach for genetic diagnosis in terms of cost and effectiveness by allowing a panel of candidate genes or whole genes to be sequenced simultaneously. Mutations have been detected in approximately 30% of childhood-onset SRNS cases, according to large-cohort studies using NGS (Table 1) [2-7]. Thus, clinicians must select the best diagnostic tool for patients with a suspected genetic disorder.
Table 1.
Genetic studies in large cohorts of pediatric patients with steroid-resistant nephrotic syndrome
| Trautmann et al [5] (2015) | Sadowski et al[3] (2015) | Bierzynska et al[2] (2017) | Wang et al[6] (2017) | Warejko et al[4] (2018) | Nagano et al[7] (2020) | |
|---|---|---|---|---|---|---|
| Country | International | International | United Kingdom | China | International | Japan |
| Modality | GP (31 genes) | GP (27 genes) | WES (53 genes) | GP (28 genes) | WES | GP (60 genes) |
| Detection ratea | 277/1,174 (23.6) | 526/1,783 (29.5) | 49/187 (26.2) | 34/120 (28.3) | 85/300 (28.3) | 69/230 (30.0) |
| Commonly mutated genesb | NPHS2, 138/277 (49.8) | NPHS2, 177/526 (33.7) | NPHS1, 14/49 (28.6) | COQ8B, 8/34 (23.5) | NPHS1, 13/85 (15.3) | WT1, 17/69 (24.6) |
| WT1, 48/277 (17.3) | NPHS1, 131/526 (24.9) | NPHS2, 12/49 (24.5) | NPHS1, 7/34 (20.6) | PLCE1, 11/85 (12.9) | NPHS1, 8/69 (11.6) | |
| NPHS1, 41/277 (14.8) | WT1, 85/526 (16.2) | WT1, 4/49 (8.2) | WT1, 7/34 (20.6) | NPHS2, 8/85 (9.4) | INF2, 8/69 (11.6) | |
| SMARCAL1, 12/277 (4.3) | PLCE1, 37/526 (7.0) | NUP107, 4/49 (8.2) | NPHS2, 4/34 (11.8) | SMARCAL1, 8/85 (9.4) | TRPC6, 7/69 (10.1) | |
| PLCE1, 10/277 (3.6) | LAMB2, 20/526 (3.8) | TRPC6, 3/49 (6.1) | LMX1B, 2/34 (5.9) | LAMB2, 6/85 (7.1) | LAMB2, 6/69 (8.7) |
Data are presented as number/total number (%).
GP, gene panel; WES, whole-exome sequencing.
Overall mutation detection rate. bParentheses denote the percentage of total patients with mutations.
This review gives an update on recent advances in genetic studies, provides a suggested approach for genetic testing, and describes the potential translation of genetic information into clinical diagnosis and treatment in pediatric patients with SRNS.
Genotype-phenotype correlations in monogenic SRNS
Currently, in the Online Mendelian Inheritance in Man database (OMIM, https://www.ncbi.nlm.nih.gov/omim), 21 genes are listed under the category of nephrotic syndrome (NPHS1-21) and nine genes are listed under the FSGS category (FSGS1-9) (Table 2). These genes are expressed either exclusively or predominantly by podocytes. Most diseases within the category of NPHS have an autosomal recessive mode of inheritance, high penetrance, and earlier disease onset. Conversely, most diseases within the category of FSGS have an autosomal dominant mode of inheritance, incomplete penetrance, and later disease onset. In addition, many other genes are listed as causative genes for isolated or syndromic forms of SRNS or FSGS (Table 3).
Table 2.
Diseases under categories of nephrotic syndrome (NPHS) and focal segmental glomerulosclerosis (FSGS) in the Online Mendelian Inheritance in Man (OMIM)
| Disease | Gene | Inheritance | OMIM numbera | Proteins |
|---|---|---|---|---|
| NPHS1 | NPHS1 | AR | 256300 | Nephrin |
| NPHS2 | PDCN | AR | 600995 | Podocin |
| NPHS3 | PLCE1 | AR | 610725 | Phospholipase c, epsilon-1 |
| NPHS4 | WT1 | AD | 256370 | WT1 transcription factor |
| NPHS5 | LAMB2 | AR | 614199 | Laminin, beta-2 |
| NPHS6 | PTPRO | AR | 614196 | Protein-tyrosine phosphatase, receptor-type, O |
| NPHS7 | DGKE | AR | 615008 | Diacylglycerol kinase, epsilon, 64-kDa |
| NPHS8 | ARHGDIA | AR | 615244 | Rho GDP-dissociation inhibitor alpha |
| NPHS9 | COQ8B | AR | 615573 | Coenzyme Q8B |
| NPHS10 | EMP2 | AR | 615861 | Epithelial membrane protein 2 |
| NPHS11 | NUP107 | AR | 616730 | Nucleoporin, 107-kDa |
| NPHS12 | NUP93 | AR | 616892 | Nucleoporin, 93-kDa |
| NPHS13 | NUP205 | AR | 616893 | Nucleoporin, 205-kDa |
| NPHS14 | SGPL1 | AR | 617575 | Sphingosine-1-phosphate lyase 1 |
| NPHS15 | MAGI2 | AR | 617609 | Membrane-associated guanylate kinase, WW and PDZ domain-containing, 2 |
| NPHS16 | KANK2 | AR | 617783 | KN motif- and Ankyrin repeat domain-containing protein 2 |
| NPHS17 | NUP85 | AR | 618176 | Nucleoporin, 85-kDa |
| NPHS18 | NUP133 | AR | 618177 | Nucleoporin, 133-kDa |
| NPHS19 | NUP160 | AR | 618178 | Nucleoporin, 160-kDa |
| NPHS20 | TBC1D8B | XL | 301028 | TBC1 domain family, member 8B |
| NPHS21 | AVIL | AR | 618594 | Advillin |
| FSGS1 | ACTN4 | AD | 603278 | Actinin, alpha 4 |
| FSGS2 | TRPC6 | AD | 603965 | Transient receptor potential cation channel, subfamily C, member 6 |
| FSGS3 | CD2AP | AR/AD | 607832 | CD2-associated protein |
| FSGS4 | APOL1 | AR | 612551 | Apolipoprotein L-I |
| FSGS5 | INF2 | AD | 613237 | Inverted formin 2 |
| FSGS6 | MYO1E | AR | 614131 | Myosin IE |
| FSGS7 | PAX2 | AD | 616002 | Paired box protein 2 |
| FSGS8 | ANLN | AD | 616032 | Actin binding protein anillin |
| FSGS9 | CRB2 | AR | 616220 | Crumbs cell polarity complex component 2 |
AD, autosomal dominant; AR, autosomal recessive.
Phenotype number.
Table 3.
Syndromic forms of steroid-resistant nephrotic syndrome/focal segmental glomerulosclerosis
| Gene | Inheritance | OMIM numbera | Disease |
|---|---|---|---|
| ALG1 | AR | 608540 | Congenital disorder of glycosylation, type Ik |
| ARHGDIA | AR | 615244 | Seizures, cortical blindness |
| CD151 | AR | 609057 | Pretibial epidermolysis bullosa and deafness |
| COQ2 | AR | 607426 | Coenzyme Q10 deficiency, primary, 1; encephalopathy |
| COQ6 | AR | 614650 | Coenzyme Q10 deficiency, primary, 1; deafness |
| CUBN | AR | 261100 | Megaloblastic anemia-1, Finnish type |
| DGKE | AR | 615008 | Atypical hemolytic uremic syndrome |
| INF2 | AD | 614455 | Charcot-Marie-Tooth disease, dominant intermediate E |
| ITGA3 | AR | 614748 | Epidermolysis bullosa, interstitial lung disease |
| ITGB4 | AR | 226650 | Epidermolysis bullosa, junctional, non-Herlitz type |
| LAMB2 | AR | 609049 | Pierson syndrome |
| LAGE3 | XR | 301006 | Galloway-Mowat syndrome 2, X-linked |
| LCAT | AR | 245900 | Norum disease (classical familial lecithin:cholesterol acyltransferase deficiency) |
| LMNA | AD | 151660 | Lipodystrophy, familial partial, type 2 |
| LMX1B | AD | 161200 | Nail-patella syndrome |
| MAFB | AD | 166300 | Multicentric carpotarsal osteolysis |
| MTTL1 | Mt | 540000 | MELAS syndrome |
| MYH9 | AD | 155100 | Macrothrombocytopenia and granulocyte inclusions with or without nephritis or sensorineural hearing loss (Epstein syndrome, Fechtner syndrome) |
| NUP107 | AR | 618348 | Galloway-Mowat syndrome 7 |
| NUP133 | AR | 618349 | Galloway-Mowat syndrome 8 |
| NXF5 | XR | Co-segregating heart block | |
| OSGEP | AR | 617729 | Galloway-Mowat syndrome 3 |
| PAX2 | AD | 120330 | Papillorenal syndrome |
| PDSS2 | AR | 614652 | Coenzyme Q10 deficiency, primary, 3; Leigh syndrome |
| PMM2 | AR | 212065 | Congenital disorder of glycosylation, type Ia |
| PODXL | AR | Congenital omphalocele | |
| SCARB2 | AR | 254900 | Epilepsy, progressive myoclonic 4, with or without renal failure |
| SMARCAL1 | AR | 242900 | Schimke immuno-osseous dysplasia |
| TP53RK | AR | 617730 | Galloway-Mowat syndrome 4 |
| TPRKB | AR | 617731 | Galloway-Mowat syndrome 5 |
| WDR4 | AR | 618347 | Galloway-Mowat syndrome 6 |
| WDR73 | AR | 251300 | Galloway-Mowat syndrome 1 |
| WT1 | AD | 194080, 136680 | Denys-Drash syndrome, Frasier syndrome |
| ZMPSTE24 | AR | 608612 | Mandibuloacral dysplasia with type B lipodystrophy |
AD, autosomal dominant; AR, autosomal recessive; MELAS, mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes; Mt, mitochondrial; XR, X-linked recessive.
Phenotype number.
Age of onset
The likelihood of detecting a causative mutation is inversely related to the age of disease onset in patients with SRNS. In one large-cohort study [3], the mutational detection rate in patients with disease onset within the first 3 months of life (congenital nephrotic syndrome) and at age 4 to 12 months (infantile nephrotic syndrome) was 69.4% and 49.7%, respectively (61.3% in the first year combined). This fraction decreased to 25.3% at age 1 to 6 years, 17.8% at age 7 to 12 years, and 10.8% at age 13 to 18 years.
The major disease-causing genes for congenital nephrotic syndrome are NPHS1, NPHS2, WT1, and LAMB2, which account for 85% of patients in a European study and 93% in a Korean study [8,9]. PLCE1 is another gene that is often mutated in early-onset SRNS and is typically associated with histological lesions of diffuse mesangial sclerosis (DMS) [10].
NPHS2, which encodes podocin, is the gene most commonly mutated in patients with disease onset between 4 months and 18 years in most Western countries [2,3,11]. However, the rate of NPHS2 mutation as a cause for SRNS is rare in certain ethnic groups, including Korean, Chinese, and Japanese populations [6,12,13]. WT1 is also commonly mutated, accounting for approximately 6% of sporadic SRNS cases in childhood [12,14,15]. WT1 mutations can manifest at any age as either isolated or syndromic forms of SRNS [12,14]. One study found that mutations in WT1 show a biphasic distribution, with a large peak at 4 to 12 months age at onset and a second smaller peak beyond 18 years [3].
While most autosomal recessive SRNS cases manifest in early childhood, autosomal dominant SRNS typically present in adolescence or adulthood. The major dominant genes that manifest in late-onset SRNS include ACTN4, TRPC6, and INF2 [3]. In a study of adult patients with FSGS [16], the overall rate of genetic diagnosis was 11%, including 55% of the total detected with mutations in COL4A3-5, 40% in podocyte genes, and 5% in congenital anomalies of the kidney and urinary tract genes.
Renal pathology
Although most pediatric patients with SRNS display lesions of FSGS, other types of lesions may also be involved, such as minimal change lesions, mesangial proliferative glomerulonephritis, and DMS [5].
In a report from the SRNS Study Group [3], renal biopsy patterns were found to differ according to age group; DMS was a frequent finding (26.9%) in infants, whereas FSGS was seen in more than 90% of individuals with the onset of proteinuria at 7 to 25 years. In addition, in individuals with mutations in genes (WT1, PLCE1, LAMB2, and NPHS1) mostly detected in patients with earlier onset, DMS was frequent (23.1%, 17.8%, 13.6%, and 4.9% respectively), whereas mutations in other genes commonly detected in patients with later onset never led to DMS. These findings suggest that DMS, lying on the opposite side of FSGS on a spectrum of shared pathogenesis, represents a developmental glomerular phenotype of immature glomeruli [3,17].
Interestingly, some patients with primary coenzyme Q10 deficiency (COQ2 or COQ6 mutations) show collapsing glomerulopathy [18-20].
Syndromic SRNS
Several different syndromic SRNS with typical extrarenal manifestations have been reported (Table 3). These diseases are typically due to mutations in genes that encode nuclear proteins/transcription factors (WT1, LMX1B, SMARCAL1, PAX2, LMNA, MAFB, and WDR73), glomerular basement membrane and adhesion proteins (LAMB2, ITGA3, and ITGB4), actin cytoskeleton components (MYH9 and INF2), lysosomal (SCARB2) proteins, and mitochondrial proteins (COQ2, COQ6, and PDSS2), but not slit diaphragm-associated proteins (NPHS1, NPHS2, PLCE1, and TRPC6) [21].
If a patient shows typical extrarenal manifestations, it is highly likely that the disease-relevant gene mutation will be identified. However, a significant fraction of patients with mutations in syndromic genes either do not manifest or manifest only mild or ambiguous extrarenal phenotypes. Thus, the absence of typical extrarenal manifestations does not guarantee an absence of syndromic gene mutations.
Mutations in at least eight genes (PDSS1, PDSS2, COQ2, COQ4, COQ6, COQ8A, COQ8B, and COQ9) have been reported to cause primary coenzyme Q10 deficiency in humans [22], and mutations in four of those genes can cause renal phenotypes, either syndromic SRNS (PDSS2, COQ2, and COQ6) [20,23,24] or isolated SRNS (COQ8B) [25]. Early and accurate diagnosis of primary coenzyme Q10 deficiency is vital because starting high-dose coenzyme Q10 supplementation at an early stage can result in remission or amelioration of proteinuria at least [23,25,26].
Ethnic differences
Similar to most genetic disorders, hereditary SRNS shows ethnic differences. Compared to other ethnicities, the most striking feature within the Korean populations is a very low prevalence of NPHS2 mutations [12]. This finding is also common in Chinese and Japanese populations [6,13]. On the other hand, mutations in NUP107, COQ8B, and COQ6 are relatively more common in Korea [19,27,28].
Benefits of genetic testing
Patients with a rare disease often face a difficult journey to diagnosis, commonly termed a ‘diagnostic odyssey’, which includes moving from clinician to clinician, multiple misdiagnoses, unnecessary tests, and incorrect treatment. An early genetic diagnosis may thus help to avoid this diagnostic odyssey [29]. Accurate genetic diagnosis in patients with SRNS can also be beneficial in several other ways. First, genetic diagnosis is essential for genetic counseling. Second, detection of certain mutations enables prediction and further screening of renal and extrarenal comorbidities that may have otherwise taken longer to diagnose, i.e. ‘reverse phenotyping’. Early detection and disease monitoring of certain extrarenal phenotypes may help to address the potential of serious complications, such as the development of Wilms’ tumor or gonadoblastoma in patients with WT1 mutations [14,30]. Third, genetic diagnosis affects the future treatment plan. Almost all genetic forms of SRNS do not respond to conventional steroids or immunosuppressants, therefore an accurate genetic diagnosis could make it possible to avoid such unnecessary and potentially harmful treatments. In addition, genetic testing can detect rare mutations that may be amenable to treatment such as mutations in the coenzyme Q10 biosynthesis pathway [23,25,26]. Finally, in patients preparing for a kidney transplant, the likelihood of posttransplant recurrence of FSGS can be predicted to be very low by the presence of genetic mutations [5,11,31]. However, it is known that the recurrence rate of proteinuria/nephrotic syndrome in a graft kidney is about 30% in patients homozygous for the Fin-major mutation in NPHS1, and approximately 70% of them have measurable anti-nephrin antibodies [32]. The Fin-major mutation in NPHS1 has never been reported in the Korean population. In addition, in patients with autosomal dominant mutations, family member kidney donor candidates should also undergo genetic testing because they could be harboring a disease-causing mutation despite being clinically asymptomatic, due to low penetrance of the mutated genes. These individuals could go on to develop clinical symptoms after kidney donation.
Indications for genetic testing
In clinical practice, a kidney biopsy is recommended for pediatric patients with nephrotic syndrome who do not respond to initial steroid treatment in order to achieve a pathological diagnosis and create an effective future treatment plan. A genetic diagnosis may provide a more clear-cut assessment of the disorder than a pathological diagnosis. Therefore, whenever accessible and affordable, genetic testing should be performed in conjunction with, or even instead of, a kidney biopsy in all pediatric SRNS patients. However, when such an inclusive approach is not possible, genetic testing should be performed as a priority on the basis of certain indications to stratify the likelihood of a genetic cause, after considering cost-effectiveness [20].
Although genetic testing is recommended for all pediatric patients with SRNS, it is frequently performed in clinical practice in those patients with 1) early age at onset, especially congenital (< 3 months of age) or infantile (4 month to 1 year of age) onset, 2) a family history of SRNS or consanguinity, 3) presence of typical extrarenal manifestations of syndromic diseases, 4) lack of response to multiple drugs, 5) progression to chronic kidney disease or ESRD, and 6) preoperative evaluation for kidney transplantation.
Modality of genetic testing
The modality of genetic testing is changing rapidly as a consequence of rapid advances in NGS. In addition to traditional Sanger sequencing, three NGS approaches for genetic diagnosis are now available in the clinical setting: 1) gene panels, 2) whole-exome sequencing (WES), and 3) whole-genome sequencing (WGS).
Sanger sequencing
Although there has been a rapid increase in the use of NGS, Sanger sequencing is still regarded as the gold standard, providing high specificity and sensitivity for genetic diagnosis. Sanger sequencing can be used very effectively with a single or few candidate genes, especially small-size genes, which are identified by genotype-phenotype correlation data. For example, mutational screening for four candidate genes (NPHS1, NPHS2, WT1, and LAMB2) will provide a genetic diagnosis in more than 85% of congenital nephrotic syndrome cases [8,9]. As another example, in ethnic groups with a higher prevalence of NPHS2 mutations, the sum of mutations in three common disease-causing genes (NPHS1, NPHS2, and WT1) account for over 70% of total mutations detected in pediatric patients with SRNS [3,5,33]. Given that NPHS1 mutations are predominantly associated with early-onset SRNS, pediatric patients with late-onset SRNS should be screened for NPHS2 (the entire coding sequence of 8 exons) and WT1 (exons 8 and 9, the hot spots for mutations) [34]. However, such recommendations cannot be applied in Korea, due to the very low prevalence of NPHS2 mutations [12]. Disease-relevant genes may also be suspected clinically in patients who present with a typical extrarenal phenotype associated with a syndromic form of SRNS (Table 3).
In addition, Sanger sequencing can be used to confirm variants detected by NGS and can complement NGS by filling in low-coverage and no-coverage regions due to sequence homology with pseudogenes, high guanine-cytosine (GC)-rich content, highly repetitive regions, and other sequence complexities [35].
Gene panel testing
SRNS is a highly heterogeneous disorder, with more than 60 known disease-causing genes. When a clinical evaluation of a patient with SRNS cannot elicit either a single or a few disease-relevant genes, gene-by-gene Sanger sequencing can be replaced by gene panel analysis, where all protein-coding exons of multiple candidate genes are tested simultaneously using high-throughput polymerase chain reaction amplification and sequencing approaches. The gene panel can be designed specifically as an indication-driven test by including genes known to be associated with a certain phenotype or disease group, such as SRNS or proteinuria. Gene panel analysis is currently considered the most cost-effective approach for indication-driven mutation analysis [36].
Gene panel testing can also be used to analyze genes, which are too large for Sanger sequencing, such as the COL4A3-5 genes that cause Alport syndrome. Importantly, mutations in syndromic genes are observed in a significant fraction of patients with no or mild/atypical extrarenal phenotypes. In these cases, the suspected underlying genetic syndrome cannot be identified clinically, but gene panel testing is able to detect the disease-causing mutations.
Compared to WES or WGS, the advantages of gene panel testing include lower cost, overall higher exon coverage, no incidental findings in genes unrelated to the disease of interest, and detection of fewer variants of unknown significance. However, to achieve 100% coverage, Sanger fill-in and/or complementary assays such as targeted gene arrays to detect deletions/duplications are required. The disadvantages of gene panel testing include rapidly outdated gene panels due to the continuous discovery of novel disease-causing genes, and the existence of novel or phenocopy genes that will not be included in the panel and therefore will not be detected. A phenocopy is defined as “a phenotypic trait or disease that resembles the trait expressed by a particular genotype, but in an individual who is not a carrier of that genotype” [37]. For example, patients with hereditary renal diseases not belonging to SRNS, such as Alport syndrome, Dent disease, renal-coloboma syndrome, and Fabry disease, can manifest proteinuria or SRNS as the only evident clinical sign at disease onset or even later [16,38-41]. These cases are often misdiagnosed as isolated SRNS, but gene panel testing for SRNS reveals a negative result. Such conditions are referred to as phenocopies of hereditary SRNS [42].
Whole-exome sequencing
WES refers to the sequencing of the entire exome, i.e., sequencing of all protein-coding regions that make up 1% to 2% of the whole genome. With continual reductions in sequencing cost and the development of bioinformatics, WES has become a more efficient and unbiased approach to genetic diagnosis than gene panel testing. Because WES covers not only known candidate genes but also whole genes, it can identify novel disease-causing genes and thus expand the genetic heterogeneity of SRNS.
A current limitation in the clinical application of WES is that it cannot offer complete coverage of all exons, which results in the dropout of several critical exons. For instance, certain genomic regions, which have sequence homology with pseudogenes, high GC-rich content, highly repetitive regions, and other sequence complexities, are difficult to amplify, and analyzing such regions may give false-negative or false-positive results. Although the complementary Sanger fill-in of these genomic regions refractory to NGS confers high clinical sensitivity and specificity on gene panel testing, practically, such fill-in is not feasible for WES because the proportion of problematic regions increases significantly when a huge region is targeted (62 Mb; 1% to 2% of the whole genome) [36]. Another limitation that hinders the widespread application of WES is the generation of large amounts of data and insufficient bioinformatics support to manage the data. To overcome these limitations, filtering the exome information via analysis of an in silico panel of genes associated with the disease of interest will give similar results to gene panel testing. The analysis can then be extended in response to negative findings in the first-line analysis or to search for novel disease-causing genes [21,42]. In a recent study of 64 young patients diagnosed with SRNS by Landini et al [43], the exome results were filtered in silico for 298 genes related to chronic kidney disease, including but not limited to SRNS-related genes. They found disease-causing variants in podocytopathy genes typically associated with SRNS and FSGS in 19 patients (30%) as well as pathogenic mutations in phenocopy genes, including COL4A3-5 (Alport syndrome), CLCN5 (Dent disease), PAX2 (renal-coloboma syndrome), and GLA (Fabry disease), in 18 patients who were clinically diagnosed with, and treated for, SRNS. Post hoc thorough ‘reverse phenotyping’ revealed the presence of distinct extrarenal phenotypes typical of the genetic diagnoses in all patients and/or first-degree relatives [43]. In other words, the combination of a WES-based diagnostic workflow for an extended panel of nephropathy-related genes with reverse phenotyping of patients and their families doubled the diagnostic rate for genetic diagnosis underlying SRNS from 30% to 60% [43].
Whole-genome sequencing
WGS can provide the complete data set of an individual’s genome by sequencing the entire genome. Compared to WES, it has the advantage of potentially improving exon, regulatory, and intronic region coverage, and improving the analysis of copy number and structural rearrangements. However, due to the high cost and long analytic period with a substantial amount of data generation, WGS is currently recommended only as a second-line test. A similar approach to that used with WES can also be used with WGS, i.e., analyzing a panel of relevant genes only.
Algorithm for genetic testing
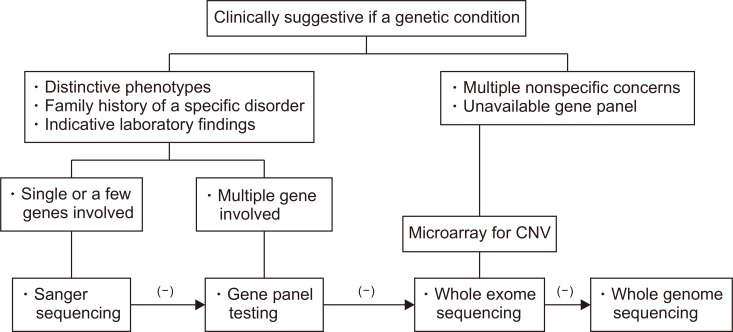
Currently, there are no universal guidelines for the mutation screening of children with SRNS. Clinicians should consider the clinical usefulness, relevance, availability, and cost-effectiveness when they direct genetic testing for pediatric patients with SRNS. Figure 1 shows an algorithm for genetic testing, which is modified from the study by Xue et al [35].
Figure 1.
Algorithm for the molecular genetic testing in pediatric patients with steroid-resistant nephrotic syndrome. This algorithm is modified from the study by Xue et al [35].
CNV, copy number variation.
Conclusions
SRNS is a genetically and phenotypically heterogeneous disorder, and more than 60 monogenic causes of SRNS have been identified. At least 30% of childhood-onset SRNS cases are caused by a genetic mutation. Currently used genetic testing methods for SRNS include Sanger sequencing, panel gene testing, WES, and WGS, each of which has advantages and disadvantages. At present, clinical phenotyping combined with targeted NGS panel analysis is the most cost-effective and clinically useful approach for the mutational screening of SRNS [21] and should be used whenever accessible and affordable. However, decisions should be made based on the specific patient and medical center. Most importantly, even in the era of genomics, precise and thorough phenotyping by clinicians remains essential for an accurate genetic diagnosis, including selection of the appropriate genetic testing method and interpretation of results [42].
Acknowledgments
This research was supported by a grant from the Korea Health Technology Research & Development Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI18C0013).
Footnotes
Conflicts of interest
The author has no conflicts of interest to declare.
References
- 1.Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet. 2018;392:61–74. doi: 10.1016/S0140-6736(18)30536-1. [DOI] [PubMed] [Google Scholar]
- 2.Bierzynska A, McCarthy HJ, Soderquest K, et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney Int. 2017;91:937–947. doi: 10.1016/j.kint.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 3.Sadowski CE, Lovric S, Ashraf S, et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J Am Soc Nephrol. 2015;26:1279–1289. doi: 10.1681/ASN.2014050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warejko JK, Tan W, Daga A, et al. Whole exome sequencing of patients with steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol. 2018;13:53–62. doi: 10.2215/CJN.04120417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trautmann A, Bodria M, Ozaltin F, et al. PodoNet Consortium. Spectrum of steroid-resistant and congenital nephrotic syndrome in children: the PodoNet registry cohort. Clin J Am Soc Nephrol. 2015;10:592–600. doi: 10.2215/CJN.06260614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang F, Zhang Y, Mao J, et al. Spectrum of mutations in Chinese children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. 2017;32:1181–1192. doi: 10.1007/s00467-017-3590-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagano C, Yamamura T, Horinouchi T, et al. Comprehensive genetic diagnosis of Japanese patients with severe proteinuria. Sci Rep. 2020;10:270. doi: 10.1038/s41598-019-57149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hinkes BG, Mucha B, Vlangos CN, et al. Arbeitsgemeinschaft für Paediatrische Nephrologie Study Group. Nephrotic syndrome in the first year of life: two thirds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2) Pediatrics. 2007;119:e907–e919. doi: 10.1542/peds.2006-2164. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Han KH, Lee H, et al. Genetic basis of congenital and infantile nephrotic syndromes. Am J Kidney Dis. 2011;58:1042–1043. doi: 10.1053/j.ajkd.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Gbadegesin R, Hinkes BG, Hoskins BE, et al. Mutations in PLCE1 are a major cause of isolated diffuse mesangial sclerosis (IDMS) Nephrol Dial Transplant. 2008;23:1291–1297. doi: 10.1093/ndt/gfm759. [DOI] [PubMed] [Google Scholar]
- 11.Santín S, Tazón-Vega B, Silva I, et al. FSGS Spanish Study Group. Clinical value of NPHS2 analysis in early- and adult-onset steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol. 2011;6:344–354. doi: 10.2215/CJN.03770410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho HY, Lee JH, Choi HJ, et al. WT1 and NPHS2 mutations in Korean children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. 2008;23:63–70. doi: 10.1007/s00467-007-0620-1. [DOI] [PubMed] [Google Scholar]
- 13.Sako M, Nakanishi K, Obana M, et al. Analysis of NPHS1, NPHS2, ACTN4, and WT1 in Japanese patients with congenital nephrotic syndrome. Kidney Int. 2005;67:1248–1255. doi: 10.1111/j.1523-1755.2005.00202.x. [DOI] [PubMed] [Google Scholar]
- 14.Lipska BS, Ranchin B, Iatropoulos P, et al. PodoNet Consortium. Genotype-phenotype associations in WT1 glomerulopathy. Kidney Int. 2014;85:1169–1178. doi: 10.1038/ki.2013.519. [DOI] [PubMed] [Google Scholar]
- 15.Ruf RG, Schultheiss M, Lichtenberger A, et al. Members of the APN Study Group. Prevalence of WT1 mutations in a large cohort of patients with steroid-resistant and steroid-sensitive nephrotic syndrome. Kidney Int. 2004;66:564–570. doi: 10.1111/j.1523-1755.2004.00775.x. [DOI] [PubMed] [Google Scholar]
- 16.Yao T, Udwan K, John R, et al. Integration of genetic testing and pathology for the diagnosis of adults with FSGS. Clin J Am Soc Nephrol. 2019;14:213–223. doi: 10.2215/CJN.08750718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hildebrandt F, Heeringa SF. Specific podocin mutations determine age of onset of nephrotic syndrome all the way into adult life. Kidney Int. 2009;75:669–671. doi: 10.1038/ki.2008.693. [DOI] [PubMed] [Google Scholar]
- 18.Barisoni L, Diomedi-Camassei F, Santorelli FM, et al. Collapsing glomerulopathy associated with inherited mitochondrial injury. Kidney Int. 2008;74:237–243. doi: 10.1038/sj.ki.5002767. [DOI] [PubMed] [Google Scholar]
- 19.Park E, Ahn YH, Kang HG, et al. COQ6 mutations in children with steroid-resistant focal segmental glomerulosclerosis and sensorineural hearing loss. Am J Kidney Dis. 2017;70:139–144. doi: 10.1053/j.ajkd.2016.10.040. [DOI] [PubMed] [Google Scholar]
- 20.Diomedi-Camassei F, Di Giandomenico S, Santorelli FM, et al. COQ2 nephropathy: a newly described inherited mitochondriopathy with primary renal involvement. J Am Soc Nephrol. 2007;18:2773–2780. doi: 10.1681/ASN.2006080833. [DOI] [PubMed] [Google Scholar]
- 21.Preston R, Stuart HM, Lennon R. Genetic testing in steroid-resistant nephrotic syndrome: why, who, when and how? Pediatr Nephrol. 2019;34:195–210. doi: 10.1007/s00467-017-3838-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desbats MA, Lunardi G, Doimo M, Trevisson E, Salviati L. Genetic bases and clinical manifestations of coenzyme Q10 (CoQ 10) deficiency. J Inherit Metab Dis. 2015;38:145–156. doi: 10.1007/s10545-014-9749-9. [DOI] [PubMed] [Google Scholar]
- 23.Heeringa SF, Chernin G, Chaki M, et al. COQ6 mutations in human patients produce nephrotic syndrome with sensorineural deafness. J Clin Invest. 2011;121:2013–2024. doi: 10.1172/JCI45693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rötig A, Appelkvist EL, Geromel V, et al. Quinone-responsive multiple respiratory-chain dysfunction due to widespread coenzyme Q10 deficiency. Lancet. 2000;356:391–395. doi: 10.1016/S0140-6736(00)02531-9. [DOI] [PubMed] [Google Scholar]
- 25.Ashraf S, Gee HY, Woerner S, et al. ADCK4 mutations promote steroid-resistant nephrotic syndrome through CoQ10 biosynthesis disruption. J Clin Invest. 2013;123:5179–5189. doi: 10.1172/JCI69000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montini G, Malaventura C, Salviati L. Early coenzyme Q10 supplementation in primary coenzyme Q10 deficiency. N Engl J Med. 2008;358:2849–2850. doi: 10.1056/NEJMc0800582. [DOI] [PubMed] [Google Scholar]
- 27.Park E, Ahn YH, Kang HG, Miyake N, Tsukaguchi H, Cheong HI. NUP107 mutations in children with steroid-resistant nephrotic syndrome. Nephrol Dial Transplant. 2017;32:1013–1017. doi: 10.1093/ndt/gfw103. [DOI] [PubMed] [Google Scholar]
- 28.Park E, Kang HG, Choi YH, et al. Focal segmental glomerulosclerosis and medullary nephrocalcinosis in children with ADCK4 mutations. Pediatr Nephrol. 2017;32:1547–1554. doi: 10.1007/s00467-017-3657-9. [DOI] [PubMed] [Google Scholar]
- 29.Bergmann C. Advances in renal genetic diagnosis. Cell Tissue Res. 2017;369:93–104. doi: 10.1007/s00441-017-2636-6. [DOI] [PubMed] [Google Scholar]
- 30.Harita Y. Application of next-generation sequencing technology to diagnosis and treatment of focal segmental glomerulosclerosis. Clin Exp Nephrol. 2018;22:491–500. doi: 10.1007/s10157-017-1449-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jungraithmayr TC, Hofer K, Cochat P, et al. Screening for NPHS2 mutations may help predict FSGS recurrence after transplantation. J Am Soc Nephrol. 2011;22:579–585. doi: 10.1681/ASN.2010010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuusniemi AM, Qvist E, Sun Y, et al. Plasma exchange and retransplantation in recurrent nephrosis of patients with congenital nephrotic syndrome of the Finnish type (NPHS1) Transplantation. 2007;83:1316–1323. doi: 10.1097/01.tp.0000262569.27890.64. [DOI] [PubMed] [Google Scholar]
- 33.Trautmann A, Lipska-Ziętkiewicz BS, Schaefer F. Exploring the clinical and genetic spectrum of steroid resistant nephrotic syndrome: the PodoNet registry. Front Pediatr. 2018;6:200. doi: 10.3389/fped.2018.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lipska BS, Iatropoulos P, Maranta R, et al. PodoNet Consortium. Genetic screening in adolescents with steroid-resistant nephrotic syndrome. Kidney Int. 2013;84:206–213. doi: 10.1038/ki.2013.93. [DOI] [PubMed] [Google Scholar]
- 35.Xue Y, Ankala A, Wilcox WR, Hegde MR. Solving the molecular diagnostic testing conundrum for Mendelian disorders in the era of next-generation sequencing: single-gene, gene panel, or exome/genome sequencing. Genet Med. 2015;17:444–451. doi: 10.1038/gim.2014.122. [DOI] [PubMed] [Google Scholar]
- 36.Lovric S, Ashraf S, Tan W, Hildebrandt F. Genetic testing in steroid-resistant nephrotic syndrome: when and how? Nephrol Dial Transplant. 2016;31:1802–1813. doi: 10.1093/ndt/gfv355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Cancer Institute. NCI dictionary of genetics terms [Internet] National Cancer Institute; Bethesda (USA): c2019. [cited 2019 Dec 27]. Available from: https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/phenocopy. [Google Scholar]
- 38.Gast C, Pengelly RJ, Lyon M, et al. Collagen (COL4A) mutations are the most frequent mutations underlying adult focal segmental glomerulosclerosis. Nephrol Dial Transplant. 2016;31:961–970. doi: 10.1093/ndt/gfv325. [DOI] [PubMed] [Google Scholar]
- 39.Wang X, Anglani F, Beara-Lasic L, et al. Investigators of the Rare Kidney Stone Consortium. Glomerular pathology in dent disease and its association with kidney function. Clin J Am Soc Nephrol. 2016;11:2168–2176. doi: 10.2215/CJN.03710416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barua M, Stellacci E, Stella L, et al. Mutations in PAX2 associate with adult-onset FSGS. J Am Soc Nephrol. 2014;25:1942–1953. doi: 10.1681/ASN.2013070686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jaurretche S, Antongiovanni N, Perretta F. Fabry nephropathy. Role of nephrologist and clinical variables associated with the diagnosis. Nefrologia. 2019;39:294–300. doi: 10.1016/j.nefro.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 42.Schaefer F. "It's in your genes": exome sequencing enables precision diagnostics in proteinuric kidney diseases. Clin J Am Soc Nephrol. 2020;15:10–12. doi: 10.2215/CJN.14241119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Landini S, Mazzinghi B, Becherucci F, et al. Reverse phenotyping after whole-exome sequencing in steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol. 2020;15:89–100. doi: 10.2215/CJN.06060519. [DOI] [PMC free article] [PubMed] [Google Scholar]