Abstract
Measles is a viral infection that has a characteristic pattern of prodromal symptoms followed by a rash. Previously considered an inevitable childhood condition, measles is known as the “first” classic childhood exanthem. For most children, measles was a one-time, short-term illness; however, some children developed complications that led to severe sequelae and death. The introduction of the measles vaccine dramatically decreased the number of cases, but the current trend against vaccination has caused outbreaks of the condition. We propose the implementation of the AAA approach (assume, advise, and answer) as a way for providers to directly encourage the administration of the vaccine and prevent future cases of measles.
Keywords: Measles, vaccination
Introduction
Exanthems are cutaneous eruptions that arise abruptly and are often associated with viral infections. Exanthems are often the first sign of illness that prompts a medical evaluation. The skin eruptions can be nonspecific; however, some present with classic characteristic patterns and prodromal symptoms that can aid in determining a diagnosis (Paller et al., 2016). Recognizing these patterns is important for both specialists and general practitioners because childhood exanthems are one of the most common cutaneous reasons for urgent care visits (Biesbroeck and Sidbury, 2013). This article reviews the first classic childhood exanthem: measles.
Measles, or rubeola, is a highly contagious disease caused by an RNA virus from the paramyxoviridae family. Prior to the measles vaccine, measles was considered an inevitable childhood illness with approximately 30 million cases and > 2 million deaths worldwide yearly (Wolfson et al., 2007). The live measles vaccine, introduced in 1963, dramatically lowered these numbers. The vaccine was initially given as one dose; however, due to an epidemic in 1989 to 1990, a second dose for children ages 4 to 6 years became the standard of care (Centers for Disease Control and Prevention [CDC], 2004).
Measles is an airborne pathogen, spread by the inhalation of respiratory droplets (Paller et al., 2016). Smaller aerosols of these droplets can remain suspended for hours (Chen et al., 1989). The virus typically infects the nasopharyngeal epithelium and spreads to the lymphatics, where it multiplies, resulting in a disseminated viremia. The prodrome includes a fever above 101°F (38.3°C), the classic three C’s (cough, coryza, and conjunctivitis), and the pathognomonic enanthem, Koplik’s spots, with white to red buccal mucosa papules (Rota et al., 2016). The incubation period prior to the prodromal symptoms lasts approximately 10 days, and the exanthem follows approximately 2 to 4 days later with the cephalocaudal spread of a maculopapular or morbilliform eruption. The rash marks the initiation of humoral and cellular immune responses, and symptoms usually start to fade with recovery approximately 1 week later (Rota et al., 2016). Patients are contagious from the time of the prodrome symptoms until 4 days after the rash (CDC, 2018b).
Diagnosis in immunodeficient patients may be difficult because they may lack immune-mediated clearance and not develop cutaneous findings (Markowitz et al., 1988). Diagnosis of measles can be confirmed with antibody or polymerase chain reaction detection (Rota et al., 2016). Treatment is typically supportive with proper nutrition and hydration (Strebel et al., 2012). Particularly in areas of vitamin A deficiency, at the time of measles diagnosis, the World Health Organization recommends daily oral vitamin A supplementation of 200,000 IU (or 50,000–100,000 IU in infants) for 2 days to reduce the risk of overall and pneumonia-specific mortality and prevent severe symptoms, such as blindness, due to the immunomodulating properties of vitamin A (D’Souza and D’Souza, 2002, Rumore, 1993, World Health Organization/UNICEF/International Vitamin A Consultative Group Task Force, 1997). A few case reports have found that intravenous or aerosolized ribavirin may also help with severe disease (Forni et al., 1994, Krasinski and Borkowsky, 1989).
Historically for most children, measles was a one-time, short-term illness; however, some children have developed severe complications leading to permanent sequelae, such as blindness, deafness, intellectual disabilities, or death (Perry and Halsey, 2004). Tremendous progress has been made worldwide to eliminate measles, and fortunately the majority of dermatologists have never seen a case (Biesbroeck and Sidbury, 2013). However, measles is not completely eradicated, and continues to be a serious health threat that makes awareness critical. Although measles-related mortality in children younger than 5 years of age decreased from 7% in 1990 to 1% in 2008, measles continues to be a leading cause of mortality worldwide in this age group (van den Ent et al., 2011).
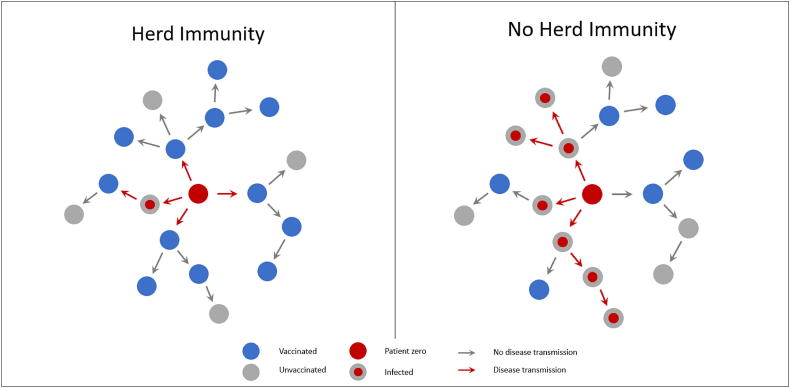
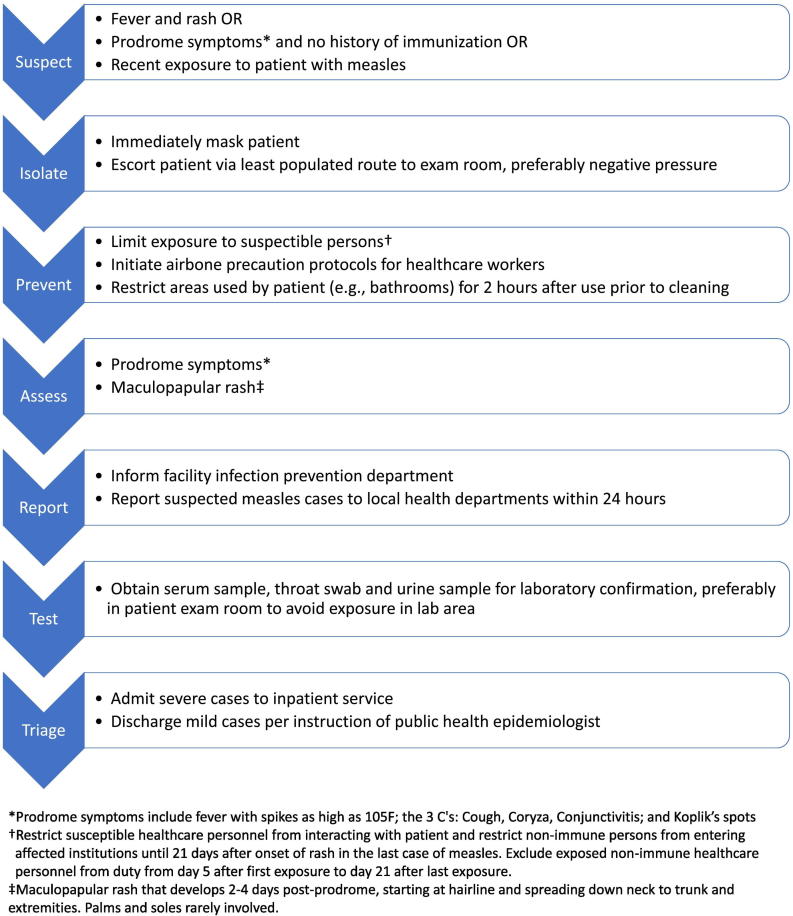
Given the highly contagious nature, herd immunity through measles vaccination is imperative to prevention. Herd immunity refers to the probability that an infectious individual will come in contact with an immunized person instead of a susceptible person at a rate that will not allow transmission of the disease through the population (Fig. 1). The herd immunity threshold is 89% to 94%, which means outbreaks can still occur in populations even with > 90% of vaccinated individuals (Thompson, 2016). If a patient is suspected of having measles, cautionary steps must be taken immediately to prevent an outbreak (Fig. 2).
Fig. 1.
Visual represenation of disease transmission in populations with and without herd immunity
Fig. 2.
Overview of general steps to manage patients with suspected measles (Centers for Disease Control and Prevention, 2018a, Centers for Disease Control and Prevention, 2018b, Centers for Disease Control and Prevention, 2019). Refer to individual institutions or state health departments for specific protocol and contact information.
Successful implementation of the measles vaccine has dramatically lowered the number of measles cases without significant complications (Demicheli et al., 2012). One dose of the measles, mumps, and rubella (MMR) vaccine is at least 95% effective in preventing clinical measles (Demicheli et al., 2012). With the aid of the vaccine, the annual reported measles incidence has decreased worldwide by 87% from 2000 to 2014 (Dabbagh et al., 2017). One of the primary concerns with regard to the safety of the MMR vaccine stems from a 1998 research study in which Andrew Wakefield implicated the MMR vaccine as the cause of autism in 12 pediatric patients via histologic samples from colonoscopies. He alleged that the tissue indicated “a pattern of colitis and ileal-lymphoid-nodular hyperplasia,” connecting the use of the vaccine and the development of autism (Wakefield et al., 1998). However, after further investigation by the General Medical Council, evidence was found to indicate that Wakefield had falsified information in an attempt to discredit the pharmaceutical company producing the MMR vaccine (Boseley, 2010). Wakefield had been secretly funded more than £400,000 (Deer, 2006) by lawyers representing a soon-to-be-established company, Immunospecifics Biotechnologies Ltd., hoping to market a safer single measles shot and a diagnostic test for inflammatory bowel disease (Deer, 2011). The attempted financial venture began to unravel as it became apparent that Wakefield’s initial paper was fraudulent (Triggle, 2010). Nonetheless, the damage had been done. From 1992 to 2004, immunization rates fell from 91.6% to 78.9% (Deer, 2012).
Societal perception with regard to the risks of vaccines has continued to the present day and has led many parents to withhold vaccinations from their children. The anti-vaccine movement has swelled, in part due to several prominent groups that perpetuate unfounded safety concerns. Both the American Chiropractic Association and the International Chiropractic Association support individual exemptions to standard vaccinations (Campbell et al., 2000). The founder of chiropractic, Daniel Palmer, believed that vaccines were ineffective vials filled with “filthy animal poison” (Busse et al., 2005). In addition, a survey of practitioners of homeopathy indicated that 83% do not recommend vaccinations (Ernst, 2001). These alternative medicine associations in combination with outspoken celebrity “antivaxxers” have resulted in a community encouraging the resurgence of unvaccinated children (Roberts, 2018).
Approximately 1.3% of children born in 2015 had not received a vaccine by the age of 2 years compared with approximately 0.9% of children born in 2011 (Mellerson et al., 2018). The decrease in vaccination rates has contributed to numerous outbreaks across the United States. A recent outbreak in Clark County, Washington State, identified 71 confirmed measles cases (Clark County Public Health, 2019). From January 1 to May 24, 2019, 940 individual cases have been confirmed in 26 states, the highest number reported in the United States since 1994 (CDC, 2019).
Practical intervention
Recognizing the signs of measles is important for early diagnosis and prevention of disease spread. For every isolated case of measles, a rapid and aggressive public health response is required to identify, educate, quarantine, immunize and to protect susceptible contacts. Contacts prior to the development of symptoms must be considered because the measles-infected patient was contagious days before recognizable symptoms appeared (Rota et al., 2016).
To further prevent measles outbreaks, vaccination is imperative. Strategies to increase public education on the safety and impact of vaccination rates are being implemented at multiple levels. On the legislative level, the Washington State House Committee recently passed a bill to ban personal and philosophical vaccine exemptions (Gstalter, 2019). On an individual level, providers have the opportunity to directly encourage the administration of vaccines to prevent and even eradicate diseases such as smallpox (Conis, 2019). The CDC has provided a systematic approach that can be employed with each patient CDC, 2018a. The recommended stepwise strategy can be easily remembered with the mnemonic AAA: assume, advise, and answer.
Assume: When discussing vaccines with parents, it is best to begin with the assumption that they are planning on accepting the vaccine for their child. Parents are more likely to appropriately vaccinate their children if the provider assumes that vaccines will be given (Opel et al., 2015).
Advise: If resistance is met, the next step is to advise parents with a strong recommendation to vaccinate their children (CDC, 2018a).
Answer: Finally, if there is continued resistance to administering the vaccine, providers should listen to and answer any questions or concerns the parents may have (CDC, 2018a). For reluctant parents, the use of motivational interviewing techniques may be helpful. The strategy should be to avoid adversarial instruction and overt persuasion in favor of a guiding style to help parents identify their own motivations to vaccinate (Leask et al., 2012).
Measles is a candidate for eradication (Rota et al., 2016), which means that this is a valuable opportunity to educate parents and pursue complete elimination through vaccination. Worldwide unification can ensure that no child suffers the devastating outcome of preventable diseases.
Conflict of Interest
None
Funding
None.
Study Approval
NA.
References
- Biesbroeck L., Sidbury R. Viral exanthems: An update. Dermatol Ther. 2013;26(6):433–438. doi: 10.1111/dth.12107. [DOI] [PubMed] [Google Scholar]
- Boseley S. Lancet retracts 'utterly false' MMR paper [Internet] 2010. https://www.theguardian.com/society/2010/feb/02/lancet-retracts-mmr-paper [cited 2019 February 22]. Available from:
- Busse J.W., Morgan L., Campbell J.B. Chiropractic antivaccination arguments. J Manipulative Phsiol Ther. 2005;28(5):367–373. doi: 10.1016/j.jmpt.2005.04.011. [DOI] [PubMed] [Google Scholar]
- Campbell J.B., Busse J.W., Injeyan H.S. Chiropractors and vaccination: A historical perspective. J Pediatr. 2000;105(4):E43. doi: 10.1542/peds.105.4.e43. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Epidemiology of measles--United States, 2001-2003. MMWR Morb Mortal Wkly Rep. 2004;53(31):713–716. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Talking with parents about vaccines for infants [Internet] 2018. https://www.cdc.gov/vaccines/hcp/conversations/talking-with-parents.html [cited 2019 February 22]. Available from:
- Centers for Disease Control and Prevention Transmission of measles [Internet] 2018. https://www.cdc.gov/measles/about/transmission.html [cited 2019 May 27]. Available from:
- Centers for Disease Control and Prevention Measles cases and outbreaks [Internet] 2019. https://www.cdc.gov/measles/cases-outbreaks.html [cited 2019 May 27]. Available from:
- Chen R.T., Goldbaum G.M., Wassilak S.G., Markowitz L.E., Orenstein W.A. An explosive point-source measles outbreak in a highly vaccinated population. Modes of transmission and risk factors for disease. Am J Epidemiol. 1989;129(1):173–182. doi: 10.1093/oxfordjournals.aje.a115106. [DOI] [PubMed] [Google Scholar]
- Clark County Public Health Measles investigation. Public health [Internet] 2019. https://www.clark.wa.gov/public-health/measles-investigation [cited 2019 May 27]. Available from:
- Conis E. Measles and the modern history of vaccination. Public Health Rep. 2019;134(2):118–125. doi: 10.1177/0033354919826558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabbagh A., Patel M.K., Dumolard L., Gacic-Dobo M., Mulders M.N., Okwo-Bele J.M. Progress toward regional measles elimination - Worldwide, 2000-2016. MMWR Morb Mortal Wkly Rep. 2017;66(42):1148–1153. doi: 10.15585/mmwr.mm6642a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deer B. MMR doctor given legal aid thousands [Internet] 2006. https://briandeer.com/mmr/st-dec-2006.htm Available from:
- Deer B. Secrets of the MMR scare. How the vaccine crisis was meant to make money. BMJ. 2011;342:c5258. doi: 10.1136/bmj.c5258. [DOI] [PubMed] [Google Scholar]
- Deer B. MMR shot statistics, England & Wales [Internet] 2012. https://briandeer.com/solved/mmr-stats-england.htm [cited 2019 May 27]. Available from:
- Demicheli V., Rivetti A., Debalini M.G., Di Pietrantonj C. Vaccines for measles, mumps and rubella in children. Cochrane Database Syst Rev. 2012;2 doi: 10.1002/14651858.CD004407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Souza R.M., D’Souza R. Vitamin A for treating measles in children. Cochrane Database Syst Rev. 2002;1 doi: 10.1002/14651858.CD001479. [DOI] [PubMed] [Google Scholar]
- Ernst E. Rise in popularity of complementary and alternative medicine: Reasons and consequences for vaccination. Vaccine. 2001;15(20) doi: 10.1016/s0264-410x(01)00290-0. Suppl 1:S90–3; discussion S89. [DOI] [PubMed] [Google Scholar]
- Forni A.L., Schluger N.W., Roberts R.B. Severe measles pneumonitis in adults: Evaluation of clinical characteristics and therapy with intravenous ribavirin. Clin Infect Dis. 1994;19(3):454–462. doi: 10.1093/clinids/19.3.454. [DOI] [PubMed] [Google Scholar]
- Gstalter M. Washington State House Committee passes bill to ban personal, philosophical vaccine exemptions [Internet] 2019. https://thehill.com/homenews/state-watch/430333-washington-state-house-committee-passes-bill-to-ban-vaccine-exemptions [cited 2019 February 22]. Available from:
- Krasinski K., Borkowsky W. Measles and measles immunity in children infected with human immunodeficiency virus. JAMA. 1989;261(17):2512–2516. [PubMed] [Google Scholar]
- Leask J., Kinnersley P., Jackson C., Cheater F., Bedford H., Rowles G. Communicating with parents about vaccination: A framework for health professionals. BMC Pediatr. 2012;12:154. doi: 10.1186/1471-2431-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz L.E., Chandler F.W., Roldan E.O., Saldana M.J., Roach K.C., Hutchins S.S. Fatal measles pneumonia without rash in a child with AIDS. J Infect Dis. 1988;158(2):480–483. doi: 10.1093/infdis/158.2.480. [DOI] [PubMed] [Google Scholar]
- Mellerson J.L., Maxwell C.B., Knighton C.L., Kriss J.L., Seither R., Black C.L. Vaccination coverage for selected vaccines and exemption rates among children in kindergarten - United States, 2017-18 school year. MMWR Morb Mortal Wkly Rep. 2018;67(40):1115–1122. doi: 10.15585/mmwr.mm6740a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel D.J., Mangione-Smith R., Robinson J.D., Heritage J., DeVere V., Salas H.S. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am J Public Health. 2015;105(10):1998–2004. doi: 10.2105/AJPH.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paller A., Mancini A.J., Hurwitz S. 5th ed. Elsevier Saunders; New York, NY: 2016. Exanthematous diseases of childhood Hurwitz clinical pediatric dermatology; pp. 382–386. [Google Scholar]
- Perry R.T., Halsey N.A. The clinical significance of measles: A review. J Infect Dis. 2004;189:S4–16. doi: 10.1086/377712. Suppl 1. [DOI] [PubMed] [Google Scholar]
- Roberts K. When it comes to vaccines, celebrities often call the shots [Internet] 2018. https://www.nbcnews.com/health/health-care/when-it-comes-vaccines-celebrities-often-call-shots-n925156 [cited 2019 May 27]. Available from:
- Rota P.A., Moss W.J., Takeda M., de Swart R.L., Thompson K.M., Goodson J.L. Measles. Nature Rev Dis Primers. 2016;2 doi: 10.1038/nrdp.2016.49. [DOI] [PubMed] [Google Scholar]
- Rumore M.M. Vitamin A as an immunomodulating agent. Clin Pharm. 1993;12(7):506–514. [PubMed] [Google Scholar]
- Strebel P.M., Papania M.J., Fiebelkorn A.P., Halsey N.A. Vaccines. 6th ed. Elsevier; New York, NY: 2012. Measles vaccine; pp. 352–387. [Google Scholar]
- Thompson K.M. Evolution and use of dynamic transmission models for measles and rubella risk and policy analysis. Risk Anal. 2016;36(7):1383–1403. doi: 10.1111/risa.12637. [DOI] [PubMed] [Google Scholar]
- Triggle N. MMR doctor struck from register [Internet] 2010. http://news.bbc.co.uk/2/hi/health/8695267.stm [cited 2019 February 22]. Available from:
- van den Ent M.M., Brown D.W., Hoekstra E.J., Christie A., Cochi S.L. Measles mortality reduction contributes substantially to reduction of all cause mortality among children less than five years of age, 1990-2008. J Infect Dis. 2011;204(Suppl. 1):S18–S23. doi: 10.1093/infdis/jir081. [DOI] [PubMed] [Google Scholar]
- Wakefield A.J., Murch S.H., Anthony A., Linnell J., Casson D.M., Malik M. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351(9103):637–641. doi: 10.1016/s0140-6736(97)11096-0. [DOI] [PubMed] [Google Scholar]
- World Health Organization/UNICEF/International Vitamin A Consultative Group Task Force . 2nd ed. World Health Organization; Geneva, Switzerland: 1997. Vitamin A supplements: A guide to their use in the treatment and prevention of vitamin A deficiency and xerophthalmia. [Google Scholar]
- Wolfson L.J., Strebel P.M., Gacic-Dobo M., Hoekstra E.J., McFarland J.W., Hersh B.S. Has the 2005 measles mortality reduction goal been achieved? A natural history modelling study. Lancet. 2007;369(9557):191–200. doi: 10.1016/S0140-6736(07)60107-X. [DOI] [PubMed] [Google Scholar]