Summary
The burden of pneumonia in Australian children is significant with an incidence of 5–8 per 1000 person-years. Pneumonia is a major cause of hospital admission in children less than 5 years of age. Indigenous children are at particular risk with a 10–20-fold higher risk of hospitalisation compared to non-Indigenous children. They also have longer admissions and are more likely to have multiple admissions with pneumonia. There are limited data on pathogen-specific causes of pneumonia, however Streptococcus pneumonia is the most common bacterial cause in children under 5 years of age and respiratory syncytial virus (RSV) and influenza are the predominant viral causes in young children. Pneumonia due to Haemophilus influenza type b (Hib) has been virtually eliminated by the introduction of universal Hib immunisation. Further studies are needed to accurately define the epidemiology of pneumonia due to specific pathogens to help target treatment and immunisation strategies.
Keywords: pneumonia, epidemiology, Australia, Indigenous child
INTRODUCTION AND DEMOGRAPHICS
The burden of respiratory and other infections in Australian children reflects the demography of the population, the variations in climate, patterns of migration and the proximity of countries from which less common pathogens may be imported. Australia is relatively unique amongst developed industrialised nations: it is comparatively sparsely populated, with the majority of the population concentrated around the southern and eastern seaboard. The total Australian population is approximately 20.2 million,1 predominantly urban and the majority descended from the European migration in the last 200 years. Indigenous Australians (Aboriginal Australians and Torres Strait Islanders) have inhabited the continent for at least 4000 years and comprise ∼2.5% of the total population.1 The majority of Indigenous Australians live in deprived socio-economic circumstances, often in remote rural locations. Indigenous Australians have some of the worst health indicators in the industrialised world.2 They bear a disproportionate burden of infectious diseases in childhood – and pneumonia is no exception.
Australia has a large migrant population with over 4.5 million individuals born overseas, equivalent to almost one quarter of the population.1
The majority of migrants are from other industrialised nations and the epidemiology of infectious diseases in these migrants is likely to be similar to that in non-Indigenous Australians. In addition, Australia currently accepts ∼12000 refugees under a humanitarian program and many more from refugee-like backgrounds under family reunification programs.3 The epidemiology of respiratory infections in this population is related to the country of origin or transit, previous limited access to adequate health care and the potentially poor vaccination coverage in refugee children.4
The climate of Australia ranges from temperate in the south to large areas of desert in the interior and tropical conditions in the north. The epidemiology of childhood respiratory infections partly reflects these differences, with familiar pathogens occurring frequently throughout the country, but with high incidences of bacterial pneumonia amongst Indigenous Australians and less familiar pathogens, such as meliodosis, occurring in the Northern Territory. The close proximity to South-east Asia has led to concern (to date largely unfulfilled) of the potential spread to Australia of ‘new’ respiratory diseases, such as Avian Influenza and Severe Acute Respiratory Syndrome (SARS).5
THE OVERALL BURDEN OF PNEUMONIA IN AUSTRALIAN CHILDREN
As in other industrialised nations, there has been a substantial decline in infectious disease mortality in Australia throughout the twentieth century. In 1907 the mortality rate across all ages from all infectious diseases was 258.9 per 100000 population; 90 years later it was 7.2 per 100000.6 Similar trends are evident in children and are attributed to improvements in sanitation, vaccination and the introduction of antibiotics. In 1996 communicable diseases accounted for 3% of the total disease burden in Australia.6 However, in children infections contribute significantly more to the burden of childhood diseases, although there are no national data. Respiratory infections have also declined substantially over the same time period.6
Australia (particularly in Western Australia) has an impressive resource of linked health-related databases, which provide detailed data on the overall epidemiology of children hospitalised with pneumonia. Clearly any data relating to the aetiology of pneumonia should be interpreted with a certain degree of caution, as the discharge diagnosis of pneumonia is usually made on clinical and/or radiological grounds, without microbiological confirmation of the aetiology.7 Much of the Australian epidemiological data spans a period where rapid diagnosis of respiratory viral pathogens was not available and diagnostic labels such as ‘bronchitis’ were more commonly applied than they are currently. However these studies provide useful insights into the overall burden of pneumonia in Australian children.
In a study of all Western Australian live births in 1986, 5% of non-Indigenous and 17% of Indigenous children were admitted to hospital with a diagnosis of pneumonia in the first two years of life.8 Of the Indigenous children, 11% had repeated admissions with pneumonia. For all children, low or high birth weight, male sex and measures of social disadvantage (young or unmarried mothers or rural location) were significant risk factors for admission.8
Between 1988 and 1993 in Western Australia, there were 53311 admissions to hospital with respiratory diseases in children aged up to 14 years, of which 4293 (8.1%) were for pneumonia (Table 1 ).9 Pneumonia was second only to asthma as the most frequent admission diagnosis in children beyond one year of age. In Indigenous children, the rate of pneumonia was 10–20 times higher than non-Indigenous children (Table 1).9
Table 1.
Age-specific hospital admissions for pneumonia in children in Western Australia 1988–1993.
| Age | Indigenous |
Non-Indigenous |
|||
|---|---|---|---|---|---|
| Admissions | Ratea | Admissions | Ratea | RR (95% CI)b | |
| Infants (<1 year) | 573 | 6189 | 324 | 223 | 27.7 (24.2–31.8) |
| 1–4 years | 1194 | 3812 | 1052 | 184 | 20.7 (19.1–22.5) |
| 5–14 years | 406 | 667 | 744 | 52 | 12.8 (11.4–14.5) |
| 15–24 years | 401 | 691 | 446 | 29 | 23.8 (20.8–27.3) |
Data from Williams et al. (1997).9
Rate per 100 000 person-years.
RR (relative rate) is the ratio of the Indigenous to non-Indigenous rate. 95% CI is the 95% confidence interval for the relative rate.
More recent and partially overlapping data from Western Australia have examined the burden of childhood pneumonia in the first two years of life in all children born between 1990 and 2000 (K. Carville, D. Lehmann, R. Richmond, N. De Klerk and D. Burgner, unpublished results). In this cohort of 270068 singleton live births (17366 Indigenous births, 252702 non-Indigenous births), pneumonia accounted for 4518 hospital admissions, equivalent to 5.8% of all admissions with an infectious diagnosis. Almost half of admissions with pneumonia in the first two years of life were in Indigenous children, in whom pneumonia accounted for 12.2% of all infectious diagnoses. Not only was pneumonia far more common in Indigenous children (Fig. 1 ), these children were three times more likely than non-Indigenous children to have multiple admissions with this diagnosis. Indigenous children with pneumonia also had a longer hospital stay than non-Indigenous children, possibly reflecting more severe disease and logistic difficulties with returning families to their remote locations.
Figure 1.
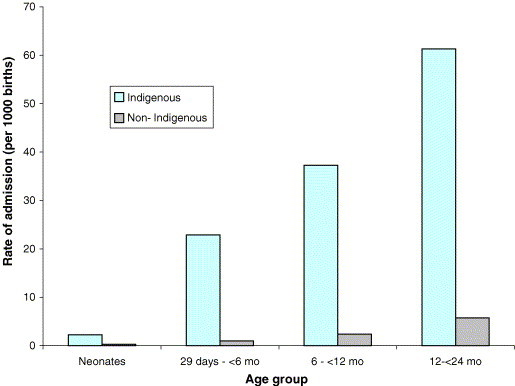
Rate of hospital admission with pneumonia from birth to 2 years in Western Australian children from 1990–2000. Data from K. Carville, D. Lehmann, R. Richmond, N. De Klerk and D. Burgner (unpublished results).
A retrospective study from suburban Sydney assessed the incidence and risk factors for all-cause pneumonia in over 2000 children aged 5–14 years by parental interview. In this predominantly non-Indigenous population the estimated incidence of pneumonia was 7.6 per 1000 person-years. This is comparable to the rate of 5.2 per 1000 person-years reported in non-Indigenous children of the same age in Western Australia. In the former study over 90% of children received antibiotic therapy and 41% were hospitalised. There appeared to be an association with a preceding diagnosis of asthma and increased risk of pneumonia.
PNEUMONIA DUE TO SPECIFIC PATHOGENS
With some notable exceptions, there is a lack of data on the epidemiology of pneumonia due to specific pathogens in Australian children. However, given the ethnic make-up of the Australian population, the climate and clinical experience, cautious generalisation of data from other countries is possible. There is increasing awareness that mixed infections, with more than one pathogen, may be important in the aetiology of childhood pneumonia,10 although this has not been investigated in Australia.
Bacterial pathogens
Neonatal pneumonia – Streptococcus agalactiae
As in other industrialised countries, group B streptococcus (GBS) is the leading cause of early-onset neonatal infection.11 Pneumonia is the principal clinical manifestation, in contrast to late-onset GBS infection, when meningitis predominates.12 The incidence of early-onset GBS infection has fallen from 2 per 1000 live births in non-Indigenous Australians in 1991–1993, to 0.5 per 1000 in 1995–1997.11 The burden of early-onset GBS disease in Indigenous neonates was 2–3 times higher and also showed a similar decline.11 The fall in the incidence of GBS is due to the increasing introduction of universal screening late in the third trimester and widespread antibiotic prophylaxis, in accordance with international guidelines.13 Interestingly, although only 40% of neonatal GBS occurs in preterm infants, they carry about 80% of the mortality14 and will not benefit from the screening that occurs in the last few weeks of the third trimester.
Streptococcus pneumoniae
The pneumococcus is recognised as the most common bacterial cause of community-acquired pneumonia in children, responsible for approximately one third of cases.15, 16 Exact estimates of the burden of disease are hampered by lack of sensitive and specific diagnostic methods in children who have negative blood cultures.17 The highest incidence of pneumococcal pneumonia is common in children under 5 years of age although a significant proportion of cases occur in older children. In Australia, the majority of data relates to pneumococcal pneumonia with bacteraemia in children from the National enhanced invasive pneumococcal disease (IPD) surveillance program.18 The incidence of bacteraemic pneumococcal pneumonia (BPP) in children under 5 years of age in 2001 prior to the widespread introduction of pneumococcal conjugate vaccine (PCV) was 17.4 per 100000 population, representing 37% of cases of IPD in this age group.18 The proportion of IPD associated with pneumonia in Indigenous children was much higher (72%) compared to non-indigenous children (31%). The overall incidence of BPP in Indigenous children was approximately 15-fold higher than in non-indigenous children under 5 years of age. The serotypes responsible for IPD were more varied in Indigenous children, with approximately 55% being due to the seven serotypes in the licensed pneumococcal conjugate vaccine (Prevnar™) compared to 86% in non-Indigenous children under 2 years of age. BPP figures clearly underestimate the true burden of pneumococcal pneumonia. In undertaking a cost-effectiveness analysis of PCV in Australian children, Butler and colleagues estimated the incidence of moderate or severe pneumococcal pneumonia to be 100 per 100000 persons in children under 5 years.19 Vaccine efficacy studies also provide an estimate of the burden of disease. In the PCV efficacy study in northern California, the incidence of chest X-ray proven pneumonia was reduced by 17.7% (95% confidence interval (CI) = 4.8–28.9%) in the intention to treat analysis20 and a similar level of efficacy was seen in a study of 9-valent PCV in South Africa (25% in HIV negative children).21 The impact of universal PCV in both Indigenous and non-Indigenous Australian children is awaited with interest.
Haemophilus influenzae
The burden of pneumonia due to Haemophilus influenzae in Australia has not been well defined. The majority of data relates to bacteraemic pneumonia due to Haemophilus influenzae type b (Hib) in the prevaccination era. Hib pneumonia represented 4–8% of invasive Hib disease in non-Indigenous children in southeastern Australia22, 23 but up to 40% of invasive Hib disease in Indigenous children from the Northern Territory.24 The age of onset of bacteraemic pneumonia was much earlier in Indigenous children (majority <12 months of age). The epidemiology of bacteraemic Hib pneumonia in Indigenous children is similar to that in developing countries25 suggesting that Hib was responsible for approximately 20% of severe pneumonia in Indigenous children prior to Hib vaccination. Following the introduction of conjugate Hib vaccines, the incidence of bacteraemic Hib pneumonia has dramatically decreased in both populations.26
Mycoplasma pneumoniae and Chlamydia pneumoniae
There are few specific Australian data relating to the burden of M. pneumoniae respiratory infection in children. Studies from European countries indicate that this pathogen may be responsible for almost one-third of childhood admissions with pneumonia in Finland27 but is much less commonly identified in the UK28 and the USA.16 Anecdotally M. pneumoniae is thought to be one of the commonest causes of pneumonia in school-age Australian children and empiric macrolide antibiotics are widely used in this setting, but this is not evidence-based. Interestingly, an Australian study suggested that asymptomatic carriage of M. pneumoniae is widespread in children admitted to hospital with non-pneumonic diagnoses,29 although whether there is significant nosocomial transmission is unknown.
Similarly, there are no specific studies of C. pneumoniae in Australian children. European data suggest this pathogen may be an important cause of pneumonia, especially in children >10 years.30 A small study of pneumonia in both adults and children from Northern Australia failed to identify C. pneumoniae.31 It is likely that this pathogen is underestimated as a cause of pneumonia in Australian children.
Staphylococcus aureus
This is an important cause of severe pneumonia, particularly in Indigenous children. In one study, from Western Australia, 69 cases were admitted over a 20 year period, with a decreasing but significant mortality over the study period.32 There is an increasing prevalence of methicillin-resistant S. aureus (MRSA: both ‘local’ strains and ‘imported’ multi-resistant strains), particularly in Indigenous children,33, 34 which has clear implications for antibiotic therapy for this pathogen.
Mycobacterium tuberculosis
Although tuberculosis (TB) is the world's most prevalent infectious disease, Australia has continued to have one of the world's lowest rates.35 The majority of TB disease occurs in migrants and less commonly in Indigenous Australians and is predominantly a disease of the aged.36 TB is reported in few Australian children but this is likely to represent a gross under-estimate, given the extreme difficulties in confirming the diagnosis microbiologically in paediatric patients.37 The prevalence of latent TB, as measured by positive Mantoux reactivity, is high, especially in migrants from countries where TB is endemic. In a study of 12–14 year-old Sydney children, 2% of the Australian-born and 27% of the overseas-born children had a positive Mantoux test.38 The risk of developing TB disease following latent infection may be extremely high in early childhood39 and remains significant through later childhood and adulthood.40 Active identification of latent TB in recent migrants to Australia, especially in children, although not universally performed, would seem prudent.39, 41
Other bacterial pathogens
Streptococcus pyogenes
This is a prevalent pathogen in Indigenous children from Northern Australia, who have some of the highest rates of rheumatic fever in the world.42, 43 Streptococcus pyogenes may, therefore, represent a more common cause of pneumonia in this population than appreciated, although there are no epidemiological studies of its role in pneumonia.
Burkholderia pseudomallei
Melioidosis is an important pathogen in South-east Asia and Northern Australia.44 In the Northern Territory the incidence is 5.8 per 100000 population, increasing to 25.5 per 100000 in Indigenous Australians.45 It causes pneumonia and septicaemia, together with abscesses in a variety of organs, including the lungs.44 Most infections occur in those with predisposing risk factors, such as diabetes,44 but it is reported in children from tropical Northern Australia.46
Viral pathogens
The epidemiology of the major paediatric respiratory viruses is generally similar in Australian children to that observed in Europe and the USA.
Respiratory syncytial virus
In industrialised nations, respiratory syncytial virus (RSV) is the predominant cause of viral lower respiratory tract infection in infancy.47 Studies48, 49 and clinical experience suggest that the same is true in Australia. The primary pathology is bronchiolitis, rather than pneumonia. RSV infection is associated with considerable morbidity and mortality, especially in high-risk groups.47 The epidemiology of RSV appears to be related to meteorological conditions in Australia49 and in neighbouring South-east Asian countries.50
Influenza
Influenza is an important cause of lower respiratory tract infection in Australian children, although precise data regarding the size of the problem are lacking. Retrospective data suggest that the pattern of epidemics do not necessarily correlate closely with European and USA epidemiology.51 Australia is part of the WHO global influenza surveillance network (FluNet: http://rhone.b3e.jussieu.fr/flunet/www/), which tracks influenza activity from active reporting from sentinel general practices and publishes regular local and national updates.52, 53 A recent London study indicated that influenza A caused one-third of viral community-acquired pneumonia and 16% of all community-acquired pneumonia.54 An Australian paediatric study suggested that influenza is also an important cause of hospital admission and morbidity and that influenza A affected younger children, whereas influenza B tended to affect those with underlying medical problems.55
‘New’ viral infections – severe acute respiratory syndrome (SARS) and avian influenza
The proximity of Australia to the epicentres of newly recognised viral infections (severe acute respiratory syndrome (SARS) and avian influenza), has created considerable concern that these infections may become major public health issues in Australia.
SARS is a newly described coronavirus infection, with a high mortality rate.56 Active SARS surveillance has been undertaken in Australia since 2003. Of the 138 individuals in Australia investigated during this period, 111 had ‘suspect’ and 27 ‘probable’ infection; five of the latter group were reported to the WHO as likely cases, after other diagnoses were excluded.5 None of these were children, but given the significant paediatric morbidity reported from neighbouring countries,57 there is the potential for SARS becoming a significant paediatric infection in Australia.
Avian influenza, a viral infection spread from infected birds and poultry, has caused significant morbidity and mortality in Asian countries.58 To date no human cases have been reported in Australia but there is considerable potential risk through migration and, to a lesser extent, through adoption of children from overseas.59
CONCLUSIONS AND SUGGESTIONS FOR FUTURE RESEARCH
Pneumonia is a common disease in Australian children and a frequent cause of admission to hospital. Whilst Australian children suffer from a range of pathogens similar to those experienced by children in industrialised countries in the Northern Hemisphere, there are several important caveats. In tropical Australia, unusual pathogens are encountered and there is the additional risk posed by imported respiratory infections from neighbouring countries. Indigenous Australians bear a hugely disproportionate burden of many diseases and have a much higher incidence of pneumonia compared to non-Indigenous children. The introduction of conjugate Hib vaccines decreased the burden of Hib pneumonia in both Indigenous and non-Indigenous children highlighting the importance of vaccination in reducing the burden of pneumonia.
The important issues in reducing the burden of pneumonia in Australia relate to (1) the impact of newly introduced vaccines, such as the conjugate pneumococcal vaccine, (2) the development of novel vaccines and therapies, especially against common viral pathogens and (3) understanding the causal pathways (and in particular the gene – environment interactions) that underlie the differential severity of essentially ubiquitous pathogens. Australia has an impressive epidemiological infrastructure and surveillance networks that will be crucial in addressing these key questions.
References
- 1.Australian Bureau of Statistics. Vol. 2004. Canberra: ABS, 2004.
- 2.Gracey M. Australian Aboriginal child health. Ann Trop Paediatr. 1998;18(Supplement):S53–S59. doi: 10.1080/02724936.1998.11747981. [DOI] [PubMed] [Google Scholar]
- 3.Davidson N., Skull S., Burgner D. An issue of access: delivering equitable health care for newly arrived refugee children in Australia. J Paediatr Child Health. 2004;40:569–575. doi: 10.1111/j.1440-1754.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- 4.Davidson N., Skull S., Chaney G. Comprehensive health assessment for newly arrived refugee children in Australia. J Paediatr Child Health. 2004;40:562–568. doi: 10.1111/j.1440-1754.2004.00465.x. [DOI] [PubMed] [Google Scholar]
- 5.Fielding J.E., Yohannes K., Vally H., Spencer J.D. Severe acute respiratory syndrome surveillance in Australia. Commun Dis Intell. 2004;28:181–186. [PubMed] [Google Scholar]
- 6.Bi P., Whitby M., Walker S., Parton K.A. Trends in mortality rates for infectious and parasitic diseases in Australia: 1907–1997. Intern Med J. 2003;33:152–162. doi: 10.1046/j.1445-5994.2003.00354.x. [DOI] [PubMed] [Google Scholar]
- 7.Isaacs D. Problems in determining the etiology of community-acquired childhood pneumonia. Pediatr Infect Dis J. 1989;8:143–148. [PubMed] [Google Scholar]
- 8.Read A.W., Gibbins J., Stanley F.J. Hospital admissions for lower respiratory tract illness before the age of two years in western Australia. Paediatr Perinat Epidemiol. 1996;10:175–185. doi: 10.1111/j.1365-3016.1996.tb00041.x. [DOI] [PubMed] [Google Scholar]
- 9.Williams P., Gracey M., Smith P. Hospitalization of aboriginal and non-aboriginal patients for respiratory tract diseases in Western Australia, 1988–1993. Int J Epidemiol. 1997;26:797–805. doi: 10.1093/ije/26.4.797. [DOI] [PubMed] [Google Scholar]
- 10.Korppi M. Mixed microbial aetiology of community-acquired pneumonia in children. APMIS. 2002;110:515–522. doi: 10.1034/j.1600-0463.2002.11007801.x. [DOI] [PubMed] [Google Scholar]
- 11.Isaacs D., Royle J.A. Intrapartum antibiotics and early onset neonatal sepsis caused by group B Streptococcus and by other organisms in Australia, Australasian Study Group for Neonatal Infections. Pediatr Infect Dis J. 1999;18:524–528. doi: 10.1097/00006454-199906000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Smaill F. Intrapartum antibiotics for group B streptococcal colonisation. Cochrane Database Syst Rev. 2000:2. doi: 10.1002/14651858.CD000115. [DOI] [PubMed] [Google Scholar]
- 13.Schrag S., Gorwitz R., Fultz-Butts K., Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep. 2002;51:1–22. [PubMed] [Google Scholar]
- 14.Berner R. Group B streptococci during pregnancy and infancy. Curr Opin Infect Dis. 2002;15:307–313. doi: 10.1097/00001432-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Virkki R., Juven T., Rikalainen H., Svedstrom E., Mertsola J., Ruuskanen O. Differentiation of bacterial and viral pneumonia in children. Thorax. 2002;57:438–441. doi: 10.1136/thorax.57.5.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wubbel L., Muniz L., Ahmed A. Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J. 1999;18:98–104. doi: 10.1097/00006454-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 17.McIntosh K. Community-acquired pneumonia in children. N Engl J Med. 2002;346:429–437. doi: 10.1056/NEJMra011994. [DOI] [PubMed] [Google Scholar]
- 18.Roche P., Krause V. Invasive pneumococcal disease in Australia, 2001. Commun Dis Intell. 2002;26:505–519. [PubMed] [Google Scholar]
- 19.Butler J.R., McIntyre P., McIntyre C.R., Gilmour R., Howarth A.L., Sander B. The cost-effectiveness of pneumococcal conjugate vaccination in Australia. Vaccine. 2004;22:1138–1149. doi: 10.1016/j.vaccine.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 20.Black S., Shinefield H., Fireman B. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J. 2000;19:187–195. doi: 10.1097/00006454-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Klugman K.P., Madhi S.A., Huebner R.E. A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med. 2003;349:1341–1348. doi: 10.1056/NEJMoa035060. [DOI] [PubMed] [Google Scholar]
- 22.Gilbert G. Epidemiology of Haemophilus influenzae type b disease in Australia and New Zealand. Vaccine. 1991;9:S10–S13. doi: 10.1016/0264-410x(91)90173-4. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert GL., Johnson P.D., Clements D.A. Clinical manifestations and outcome of Haemophilus influenzae type b disease. J Paediatr Child Health. 1995;31:99–104. doi: 10.1111/j.1440-1754.1995.tb00755.x. [DOI] [PubMed] [Google Scholar]
- 24.Hanna J. The epidemiology and prevention of Haemophilus influenzae infections in Australian Aboriginal children. J Paediatr Child Health. 1992;28:354–361. doi: 10.1111/j.1440-1754.1992.tb02691.x. [DOI] [PubMed] [Google Scholar]
- 25.Mulholland E.K., Adegbola R.A. The Gambian Haemophilus influenzae type b vaccine trial: what does it tell us about the burden of Haemophilus influenzae type b disease? Pediatr Infect Dis J. 1998;17:S123–S125. doi: 10.1097/00006454-199809001-00006. [DOI] [PubMed] [Google Scholar]
- 26.Herceg A. The decline of Haemophilus influenzae type b disease in Australia. Commum Dis Intell. 1997;21:173–176. [PubMed] [Google Scholar]
- 27.Korppi M., Heiskanen-Kosma T., Kleemola M. Incidence of community-acquired pneumonia in children caused by Mycoplasma pneumoniae: serological results of a prospective, population-based study in primary health care. Respirology. 2004;9:109–114. doi: 10.1111/j.1440-1843.2003.00522.x. [DOI] [PubMed] [Google Scholar]
- 28.Drummond P., Clark J., Wheeler J., Galloway A., Freeman R., Cant A. Community acquired pneumonia—a prospective UK study. Arch Dis Child. 2000;83:408–412. doi: 10.1136/adc.83.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldwater P.N., Martin A.J., Ryan B. A survey of nosocomial respiratory viral infections in a children's hospital: occult respiratory infection in patients admitted during an epidemic season. Infect Control Hosp Epidemiol. 1991;12:231–238. doi: 10.1086/646330. [DOI] [PubMed] [Google Scholar]
- 30.Heiskanen-Kosma T., Korppi M., Laurila A., Jokinen C., Kleemola M., Saikku P. Chlamydia pneumoniae is an important cause of community-acquired pneumonia in school-aged children: serological results of a prospective, population-based study. Scand J Infect Dis. 1999;31:255–259. doi: 10.1080/00365549950163536. [DOI] [PubMed] [Google Scholar]
- 31.Thompson J.E. Community acquired pneumonia in north eastern Australia—a hospital based study of aboriginal and non-aboriginal patients. Aust N Z J Med. 1997;27:59–61. doi: 10.1111/j.1445-5994.1997.tb00915.x. [DOI] [PubMed] [Google Scholar]
- 32.Knight G.J., Carman P.G. Primary staphylococcal pneumonia in childhood: a review of 69 cases. J Paediatr Child Health. 1992;28:447–450. doi: 10.1111/j.1440-1754.1992.tb02715.x. [DOI] [PubMed] [Google Scholar]
- 33.Torvaldsen S., Roberts C., Riley T.V. The continuing evolution of methicillin-resistant Staphylococcus aureus in Western Australia. Infect Control Hosp Epidemiol. 1999;20:133–135. doi: 10.1086/501594. [DOI] [PubMed] [Google Scholar]
- 34.Munckhof W.J., Schooneveldt J., Coombs G.W., Hoare J., Nimmo G.R. Emergence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection in Queensland. Australia. Int J Infect Dis. 2003;7:259–264. doi: 10.1016/s1201-9712(03)90104-4. [DOI] [PubMed] [Google Scholar]
- 35.Lumb R., Bastian I., Dawson D. Tuberculosis in Australia: bacteriologically confirmed cases and drug resistance. Commun Dis Intell. 2003;27:173–180. [PubMed] [Google Scholar]
- 36.Miller M., Lin M., Spencer J. Tuberculosis notifications in Australia. Commun Dis Intell. 2002;26:525–536. [PubMed] [Google Scholar]
- 37.Shingadia D., Novelli V. Diagnosis and treatment of tuberculosis in children. Lancet Inf Dis. 2003;3:624–632. doi: 10.1016/s1473-3099(03)00771-0. [DOI] [PubMed] [Google Scholar]
- 38.Alperstein G., Fett M.J., Reznik R., Thomas M., Senthil M. The prevalence of tuberculosis infection among Year 8 schoolchildren in inner Sydney in. Med J Aust. 1994;160:197–201. [PubMed] [Google Scholar]
- 39.Blyth C., Waring J., Burgner D. Inconspicuous consumption: disseminated tuberculosis following untreated latent infection. J Paediatr Child Health. 2004;40:227–229. doi: 10.1111/j.1440-1754.2004.00343.x. [DOI] [PubMed] [Google Scholar]
- 40.Marks G.B., Bai J., Simpson S.E., Sullivan E.A., Stewart G.J. Incidence of tuberculosis among a cohort of tuberculin-positive refugees in Australia: reappraising the estimates of risk. Am J Respir Crit Care Med. 2000;162:1851–1854. doi: 10.1164/ajrccm.162.5.2004154. [DOI] [PubMed] [Google Scholar]
- 41.MacIntyre C.R., Plant A.J., Yung A., Streeton J.A. Missed opportunities for prevention of tuberculosis in Victoria. Australia. Int J Tuberc Lung Dis. 1997;1:135–141. [PubMed] [Google Scholar]
- 42.Carapetis J., Gardiner D., Currie B., MAthews J.D. Multiple strains of Streptococcus pyogenes in skin sores of aboriginal Australians. J Clin Microbiol. 1995;33:1471–1472. doi: 10.1128/jcm.33.6.1471-1472.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carapetis J.R., Walker A.M., Hibble M., Sriprakash K.S., Currie B.J. Clinical and epidemiological features of group A streptococcal bacteraemia in a region with hyperendemic superficial streptococcal infection. Epidemiol Infect. 1999;122:59–65. doi: 10.1017/s0950268898001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.White N.J. Melioidosis. Lancet. 2003;361:1715–1722. doi: 10.1016/s0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 45.Cheng A.C., Hanna J.N., Norton R. Melioidosis in northern Australia, 2001–02. Commun Dis Intell. 2003;27:272–277. [PubMed] [Google Scholar]
- 46.Currie B.J., Brewster D.R. Childhood infections in the tropical north of Australia. J Paediatr Child Health. 2001;37:326–330. doi: 10.1046/j.1440-1754.2001.00661.x. [DOI] [PubMed] [Google Scholar]
- 47.Hall C.B. Respiratory syncytial virus: a continuing culprit and conundrum. J Pediatr. 1999;135:2–7. [PubMed] [Google Scholar]
- 48.McIntosh E.D., De Silva L.M., Oates R.K. Clinical severity of respiratory syncytial virus group A and B infection in Sydney, Australia. Pediatr Infect Dis J. 1993;12:815–819. doi: 10.1097/00006454-199310000-00004. [DOI] [PubMed] [Google Scholar]
- 49.De Silva L.M., Hanlon M.G. Respiratory syncytial virus: a report of a 5-year study at a children's hospital. J Med Virol. 1986;19:299–305. doi: 10.1002/jmv.1890190402. [DOI] [PubMed] [Google Scholar]
- 50.Chew F.T., Doraisingham S., Ling A.E., Kumarasinghe G., Lee B.W. Seasonal trends of viral respiratory tract infections in the tropics. Epidemiol Infect. 1998;121:121–128. doi: 10.1017/s0950268898008905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Viboud C., Boelle P.Y., Pakdaman K., Carrat F., Valleron A.J., Flahault A. Influenza epidemics in the United States, France, and Australia, 1972–1997. Emerg Infect Dis. 2004;10:32–39. doi: 10.3201/eid1001.020705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Broom A.K., David W.S. The Influenza Surveillance Program in Western Australia. Commun Dis Intell. 2004;28:169–174. [PubMed] [Google Scholar]
- 53.Yohannes K., Roche P., Hampson A., Miller M., Spencer J. Annual report of the National Influenza Surveillance Scheme, 2003. Commun Dis Intell. 2004;28:160–168. [PubMed] [Google Scholar]
- 54.Laundy M., Ajayi-Obe E., Hawrami K., Aitken C., Breuer J., Booy R. Influenza A community-acquired pneumonia in East London infants and young children. Pediatr Infect Dis J. 2003;22:223–227. doi: 10.1097/01.inf.0000092192.59459.8b. [DOI] [PubMed] [Google Scholar]
- 55.Daley A.J., Nallusamy R., Isaacs D. Comparison of influenza A and influenza B virus infection in hospitalized children. J Paediatr Child Health. 2000;36:332–335. doi: 10.1046/j.1440-1754.2000.00533.x. [DOI] [PubMed] [Google Scholar]
- 56.Guan Y., Peiris J.S., Zheng B. Molecular epidemiology of the novel coronavirus that causes severe acute respiratory syndrome. Lancet. 2004;363:99–104. doi: 10.1016/S0140-6736(03)15259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leung C.W., Kwan Y.W., Ko P.W. Severe acute respiratory syndrome among children. Pediatrics. 2004;113:e535–e543. doi: 10.1542/peds.113.6.e535. [DOI] [PubMed] [Google Scholar]
- 58.Stephenson I., Nicholson K.G., Wood J.M., Zambon M.C., Katz J.M. Confronting the avian influenza threat: vaccine development for a potential pandemic. Lancet Infect Dis. 2004;4:499–509. doi: 10.1016/S1473-3099(04)01105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krilov L.R. Emerging infectious disease issues in international adoptions: severe acute respiratory syndrome (SARS), avian influenza and measles. Curr Opin Infect Dis. 2004;17:391–395. doi: 10.1097/00001432-200410000-00002. [DOI] [PubMed] [Google Scholar]


