Abstract
Community acquired pneumonia (CAP) is a leading cause of childhood morbidity worldwide. Because of the rising antimicrobial resistance rates and adverse effects of childhood antibiotic use on the developing microbiome, rational prescribing of antibiotics for CAP is important. This review summarizes and critically reflects on the available evidence for the epidemiology, etiology and antimicrobial management of childhood CAP. Larger prospective studies on antimicrobial management derive mostly from low- or middle-income countries as they have the highest burden of CAP. Optimal antimicrobial management depends on the etiology, age, local vaccination policies and resistance patterns. As long as non-rapid surrogate markers are used to distinguish viral- from bacterial pneumonia, the management is probably suboptimal. For a young child with signs of non-severe pneumonia (with or without wheezing), watchful waiting is recommended because of probable viral etiology. For children with more severe CAP with fever, a five-day oral amoxicillin course would be the first choice therapy and dosage will depend on local resistance rates. There is no clear evidence yet for superiority of a macrolide-based regimen for all ages. For cases with CAP requiring hospitalization, several studies have shown that narrow-spectrum IV beta-lactam therapy is as effective as a broad-spectrum cephalosporin therapy. For most severe disease, broad-spectrum therapy with or without a macrolide is suggested. In case of empyema, rapid IV-to-oral switch seems to be equivalent to prolonged IV treatment.
Abbreviations: BD, bis in die/(two times a day); (RC)CAP, radiologically conformed community acquired pneumonia; HiB, Haemophilus influenza type B; HIV, human immunodeficiency virus; HRV, human rhinovirus; ICU, Intensive Care Unit; IV, intravenous; LMIC, low- and middle-income countries; LRT, lower respiratory tract; MIC, minimal inhibitory concentration; PCR, polymerase chain reaction; PCV, pneumococcal conjugate vaccine; RSV, respiratory syncytial virus; SP, Streptococcus pneumoniae; TID, ter in die (3 times a day); WHO, World Health Organization; URT, upper respiratory tract
Keywords: Pneumonia, Children, Epidemiology, Etiology, Antimicrobial treatment
Introduction
Pneumonia is a leading cause of childhood morbidity and mortality worldwide. The annual worldwide incidence of pneumonia in children <5 years old is estimated 120 million approximately, of which ∼1.3 million cases lead to death [1]. The world-wide case fatality ratio is estimated to be around 8.7% for severe pneumonia. Most mortality occurs in the younger age group. Specifically, 81% of all pneumonia deaths occur in children <2< years old [2]. These figures have largely improved since the eighties, when childhood respiratory tract infections accounted for 4–5 million childhood deaths per year [3].
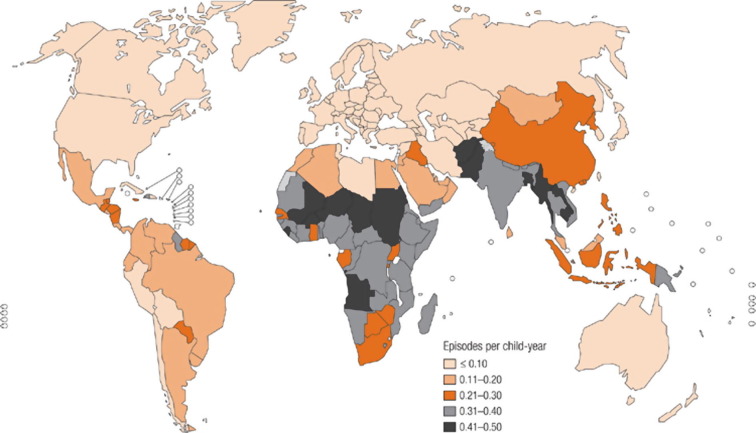
The epidemiology of childhood pneumonia varies widely between different regions of the world related to prevalence of risk factors and causative pathogens [4]. Most pneumonia episodes occur in Southeast Asia and Africa. Importantly, sub-Saharan Africa accounts for 43% of pneumonia deaths, despite only constituting 19% of the world's under-5 population [2], [5]. In low- and middle-income countries (LMIC), the incidence has been reduced to 25% over the last decade, now being ∼0.22 episodes per child year [6]. Figure 1 shows the worldwide incidence of pneumonia in children <5 years old.
Fig. 1.
Incidence of pneumonia in children <5 years. Rudan et al, WHO 2008 [4]. Reprinted with permission [4].
Increased hygiene, antibiotic therapy and vaccination against Streptococcus pneumoniae (SP) with pneumococcal conjugate vaccine (PCV), and Haemophilus influenzae type B (HiB) have largely decreased the morbidity in children in the developed world [7]. Especially the contribution of HiB CAP is falling quite rapidly because of widespread vaccination in the majority of LMIC. Only a few countries do not vaccinate against HiB; in 2012, 180 countries introduced HiB-vaccine and 86 countries PCV [1]. The estimated reduction of the HiB- and PCV on radiologically confirmed (RC) pneumonia is ∼18% and ∼26% respectively [8]. A recent Asian study noted a 39% decline in RCCAP in young children after HiB vaccination [9]. However, the HIV-epidemic has increased the incidence of childhood CAP again [1], [6].
Because of the large burden of pneumonia on child health and mortality, the optimal management of pneumonia is a ‘hot topic’. Optimal management comprises good accessibility to health care services, adequate diagnosis, and rational easily available inexpensive antimicrobial therapy. These lead to a fast resolution of symptoms in the majority of children with pneumonia. Resistance must be prevented by restricted use in general, and use of narrow-spectrum antibiotics. This review will describe the available evidence for the etiology and management of CAP in otherwise healthy children beyond the neonatal period.
Etiology of community acquired pneumonia in childhood
Methods
Microbiological methods to study the etiology are culture, polymerase chain reaction (PCR), direct immunofluorescence, antigen tests and (paired) serology. Upper respiratory tract (URT) samples (naso- or oropharyngeal swabs) are often used as surrogate markers for the lower respiratory tract (LRT) (sputum, pleural fluid, lung tap, broncho-alvealor lavage fluid, and biopsy). The positive predictive value and specificity of the URT samples might be limited for LRT, since many potential pathogenic organisms also colonize the URT [10].
Blood cultures
Blood cultures rarely add to the diagnosis of CAP (1–10%), and might lead to a prolonged hospitalization [11]. A targeted approach of identifying the patients with CAP at risk for bacteraemia might aid in the yield of positive blood cultures [12].
Lung aspirates, biopsy- and empyema studies
In the pre-vaccine era, 62% of pre-treated children from LMIC had bacteria detected in their lung aspirates, mainly SP and HiB. Viruses were present in 23% [3]. A post-mortem study of lung tissue samples from 98 Mexican children younger than 2 years who died of pneumonia, showed respiratory syncytial virus (RSV) in 30% of patients [13]. Bacterial PCR on post-mortem stored Chinese lung tissue samples from a 50-year period showed HiB as a causative pathogen for fatal CAP in 18% of children [14]. A recent systematic review series on incidence and pathogens in childhood CAP found HiB responsible for 16% of fatal cases, adjusted for HiB vaccination [6]. More data will be available in the future as the PERCH (Pneumonia Etiology Research for Child Health) project will study post-mortem samples combined with ante-mortum samples with modern techniques to define the cause of death in children with pneumonia in the vaccine-era [10], [15].
In recent childhood empyema studies PCR aided in the yield of pathogens. The majority of severe pneumonia cases were still caused by SP (non-vaccine types, ∼62%), followed by S. pyogenes (16%) [16], [17], [18]. However, concomitant viral infections were not investigated. Among cases with empyema from LMIC; SP, HiB and S. aureus play a major role [19], [20].
Induced sputum and URT-samples
Hospitalized pre-school Kenyan children with CAP underwent induced sputum for culture and/or PCR, blood culture and nasopharyngeal PCR. They had evidence of bacterial infection in 9%, viral in 53%, mixed viral-bacterial in 15%, and no pathogen was found in 22% [21]. The same type of study was performed in New Caledonia, showing probable pathogens in 90% of hospitalized cases. 82% of these were viruses (RSV and HRV being the most common) and 23% bacterial pathogens [22].
Induced sputum samples from hospitalized children (1–16 years) with radiologically confirmed (RC) CAP showed a pathogen in 97% of patients using viral antigen detection, PCR, and cultures. The majority of these children had a viral-bacterial co-infection (66%), followed by bacterial infection (25%) and viral infection (5%). Human rhinovirus (HRV)-SP was the most common co-infection detected [23]. Viral pathogens were more often detected in the post-PCV era compared to the pre-PCV era in British children with RCCAP, mainly because of new techniques, such as blood and nasopharyngeal swab PCR. Bacterial infection rates (mainly SP) were similar between the pre- and post PCV7 era (∼20%) [24]. Pavia reviewed etiologies from 4 recent studies in children hospitalized with CAP (Table 1 ). These 4 studies, using nasopharyngeal multiplex PCR and culture, had an average pathogen detection rate of about 80%, and in 40–60% of the samples one or more bacteria were found. Viruses were detected in 45–66% and co-infection in ∼23–33%. HRV and RSV were the major contributors. Although the methods were slightly different, the figures were quite comparable between the studies. Also, atypical bacteria were found in pre-school children [25].
Table 1.
Main pathogens causing childhood lower respiratory tract disease. Notably: HiB is virtually eliminated because of worldwide vaccination. Adapted from Pavia et al. [25].
| Lower respiratory disease | Etiologic agent |
|---|---|
| Bronchiolitis | RSV, human metapneumovirus, parainfluenzavirus, adenovirus, rhinovirus, coronavirus, influenzavirus, bocavirus, Mycoplasma- or Chlamydia pneumoniae |
| Wheezing | RSV, human metapneumovirus, rhinovirus, adenovirus, parainfluenzavirus, coronavirus, influenzavirus, bocavirus, Mycoplasma pneumoniae |
| Pneumonia | Influenzavirus, parainfluenzavirus, RSV, adenovirus, rhinovirus, human metapneumovirus, Streptococcus pneumoniae, Mycoplasma pneumoniae, Streptococcus pyogenes, Staphylococcus aureus |
A large USA study conducted in hospitalized children <18 years with RCCAP showed a pathogen (PCR of URT swab and serology, blood culture) in 81% of children. These were mostly single or multiple viruses (66%, the majority being RSV or HRV), followed by bacteria (8%) and co-infection (7%). However, 51% of these children had comorbidity (mainly asthma) thus this population cannot be fully compared with previously healthy children. This might also explain the low incidence of bacterial infection [26]. In a Chinese serological study aimed at determining viral and atypical bacterial respiratory infection in ∼10,000 hospitalized children, Mycoplasma pneumonia was found to be the main causative agent, followed by adenovirus and influenza B-virus. However, since only serology was used, many viral and bacterial organisms could not be found [27]. These figures were confirmed by another study using serology and PCR that found that 17.5% of CAP cases were caused by atypical pathogens [28].
Additionally, Staphylococcus aureus, Gram-negative bacilli (such as Klebsiella pneumoniae, non-typhoidal Salmonella spp.) and Mycobacterium tuberculosis have been involved in the etiology of acute pneumonia in LMIC. Influenza-associated severe S. aureus co-infection seemed to have increased recently, also in high-income countries [2], [29].
Treatment of community acquired childhood pneumonia
Antimicrobial agents
Almost all studies from an outpatient setting have been performed in LMIC using the WHO-definition (Table 2 ). This is a major limitation for the generalizability of the results in other settings. Therefore, studies from LMIC and industrialized countries are separately described.
Table 2.
WHO-definition of pneumonia.
| Diagnosis | Symptoms |
|---|---|
| Non-severe pneumonia | Cough and fast breathing |
| Severe pneumonia | Cough, fast breathing, lower chest indrawing |
| Very severe pneumonia | Cough, fast breathing, lower chest indrawing, grunting, inability to feed, central cyanosis, lethargy, convulsions |
LMIC studies – outpatient setting
In non-severe pneumonia, oral co-trimoxazole and normal dose amoxicillin (TID) seem to be equivalent with a failure rate of 12–13%. However, the primary endpoint was not clearly described. In severe pneumonia, amoxicillin seems to be superior to co-trimoxazole, as was shown by a prospective blinded study that showed an 18% failure versus 33% failure, respectively. In this study, 20–22% of children were bacteriaemic. HiB accounted for bacteriaemia in 14% and SP in 8%. Amoxicillin was successful in all children who had SP bacteriaemia, whereas co-trimoxazole failed in 28% children who had SP bacteraemia [30], [31]. In Pakistan, twice daily oral co-trimoxazole was prospectively and blindly compared with twice daily oral amoxicillin (50 mg/kg/d) in children with non-severe pneumonia. The endpoint was defined as normalization of breathing rate for age at day 5 [32]. Both antibiotics were equally effective but there was also a high failure rate for both (19% vs. 16%, respectively).
In 2 large (>8000 children) prospective Pakistani studies in preschool children with severe pneumonia, 1 dose of co-trimoxazole followed by referral for injectable penicillin (WHO guideline) was inferior to a 5–7 day high-dose oral amoxicillin course (BD), but the general evidence was of low-quality. The primary endpoint was treatment failure by day 6. Failure rate was 8–9% for the amoxicillin group and 13–18% for the control group. However, it is questionable whether the follow-up was adequate. In addition, many children in the control group did not receive injectable penicillin [33], [34], [35].
In Gambia, a 5-day course of co-trimoxazole and single penicillin injection followed by a 5-day course of oral ampicillin (unknown dose) in young children with severe pneumonia was studied. Clinical recovery after 2 weeks was comparable in both treatment arms [36].
Interestingly, a prospective double-blind study comparing an oral 3-day normal dose amoxicillin course with placebo in young Pakistani children with non-severe pneumonia did not show any difference in therapy failure at 72 h (7.2% vs 8.3%, p = 0.60). This highlights the mostly viral nature of lower respiratory infections in young children. Importantly, difficulty breathing and fever were identified as risk factors for failure by day 5 [37]. An Indian prospective double-blind study in young children with non-severe pneumonia and wheezing with persistent tachypnea after bronchodilator nebulization, studied 3-day low-to normal dose oral amoxicillin vs. placebo. Clinical failure defined as severe of very severe pneumonia, or oxygen saturation <90% before or on day 4, or fever or persistence of non-severe pneumonia on day 4 was observed in 24% in the placebo group and 19.9% in the amoxicillin group (p = 0.34, number needed to treat = 24) [38]. In almost all these studies, the etiology was not investigated.
LMIC studies – inpatient setting
A non-blinded study comparing IV vs. oral regimen in several LMIC countries showed equivalence for normal dose oral amoxicillin (TID) and injectable penicillin in children <5 years for severe pneumonia. The outcome ‘treatment failure’ (lower chest indrawing after 48 h) was 19% for both groups. Age younger than 11 months and hypoxia predicted treatment failure. Nasopharyngeal washes showed 25% RSV positivity in both groups, 27–29% SP and 20% HiB colonization. RSV-isolation was not associated with treatment failure. However, probably not all pneumonias were caused by the detected bacteria (of which 66% were SP and 30% HiB resistant to amoxicillin), since only nasopharyngeal wash was analyzed. Also, no high dose amoxicillin was used. It was not described whether resistant organisms predicted treatment failure [39]. A prospective study compared a 5-day high dose oral amoxicillin course (BD) vs. 2 days of IV ampicillin followed by 3 days of high dose amoxicillin for severe pneumonia in 2100 preschool children. The primary endpoint, treatment failure by day 6, was 7.5% vs. 8.6% respectively (risk difference 1.1, CI −1.3 to 3.5). A positive urine ‘antibacterial activity’ test was positive in 36–38% of tested patients [40]. In a small prospective non-blinded Pakistani study in hospitalized children with pneumonia, oral amoxicillin (dose unknown) was found to be equally effective as clarithromycin or oral cefuroxime (primary outcome clinical improvement at 48 h), but was more cost-effective [41].
The prospective open label SPEAR study showed superiority of 5 days of IV ampicillin/gentamicin compared to IV chloramphenicol in preschool children with very severe pneumonia. Strikingly, S. aureus was more often cultured than SP [42]. In an open label trial in young Papoean children comparing the same regimen, no significant differences were observed in the primary outcome ‘adverse outcome within 30 days’, being (22.1% vs 26.3%). Adverse outcome was defined as death, treatment failure requiring change of antibiotics, readmission with severe pneumonia within 1 month of discharge or absconding from hospital. Of note, this is an area with high penicillin resistance. The most commonly isolated bacteria were Pseudomonas aeruginosa, S. aureus, HiB, Enterobacter spp, SP, other Streptococcus spp, other enteric Gram-negative bacilli [43].
Industrialized country studies
No studies from high-income countries on antimicrobial management of WHO-defined non-severe pneumonia were found. A non-blinded study comparing 7 days of unknown dose oral amoxicillin with amoxicillin-clavulanic acid in children with clinical CAP showed superiority for amoxicillin-clavulanic acid. However, the endpoint was unclear and the confidence interval very broad (2.85–38.2) [44]. A small study comparing 1 dose of injectable penicillin with normal oral dose amoxicillin (50 mg/kg/d; TID) in children with RCCAP, did not find differences in fever, respiratory rate and general appearance scores after 24–36 h [45]. A retrospective cohort study showed beta-lactam monotherapy (unknown dose) to be as good as macrolide monotherapy for clinical CAP in children 1–18 years old, irrespective of their age. The primary outcome was treatment failure within 14 days leading to prescription of a new antibiotic [46]. Earlier, this author concluded that children >6 years with CAP might benefit from a combination of beta-lactam and macrolide therapy leading to a lower odds of treatment failure at day 7 and day 14, but also these data derived from a retrospective study. No etiologies were studied [47]. Other studies also described equal clinical effectiveness in children when comparing macrolides vs. amoxicillin or amoxicillin-clavulanic acid in RCCAP, but the studies were poorly designed and probably influenced by the pharmaceutical sponsor [48], [49].
The role for macrolide antibiotics in hospitalized children with CAP is unclear. A retrospective study compared ceftriaxone and macrolide versus ceftriaxone monotherapy and suggested combination therapy to decrease length of stay only for patients >5 years (RR 0,95). However, the number needed to treat resulting in 1 child hospital length of stay for 1 less day was 7 children. This is possibly not cost-effective. No etiologies were estimated [50]. Fluoroquinolones have hardly been studied in children. A multisite open non-inferiority study in children 0.5–16 years old with RCCAP compared levofloxacin with broad-spectrum beta-lactam therapy (<5 year) and clarithromycin or ceftriaxone/macrolide combination therapy (>5 year). The majority of the study group received levofloxacin for 10 days (546 vs. 182 patients). Clinical cure rates were identical for both groups (94%). Serology and sputum analysis (performed for some subjects) showed M. pneumonia as the major pathogen in all age groups. Viral causes were not investigated [51].
Clinical outcomes for children 2 months–18 years hospitalized with CAP were identical for narrow (ampicillin/penicillin) and broad-spectrum (2nd or 3rd generation cephalosporin) IV antibiotics, according to 3 large retrospective series. Primary outcomes were several clinical parameters, such as days of IV treatment, days of oxygen requirement days of hospitalization, and readmission rates [52], [53], [54]. This has been confirmed in prospective randomized observational studies in pediatric patients with proven lobar pneumonia looking at clinical, laboratory and radiological outcomes (penicillin vs. cefuroxime) [55]. For example, the PIVOT trial prospectively compared low dose oral amoxicillin (24 mg/kg/d; TID) with IV penicillin followed by low dose oral amoxicillin in 246 children hospitalized with RCCAP >6 months old in the United Kingdom. Oral amoxicillin was clinically equivalent to IV penicillin regarding the time to resolution of fever and hypoxia. The oral intervention was cost-effective [57]. However, children with most severe pneumonia were excluded. Naso- and oropharyngeal swabs were taken for viral PCR but no results were described [56]. In 104 children with very severe pneumonia, IV oxacillin/ceftriaxone combination therapy was prospectively compared with IV amoxicillin-clavulanic acid monotherapy (normal dose). The amoxicillin-clavulanic acid group did significantly better with respect to tachypnoea improvement and hospital length of stay [58]. The latter can probably be fully explained by the fact that IV amoxicillin-clavulanic acid was switched to oral amoxicillin-clavulanic acid after 48 h in case of improvement.
Duration and dose
There are no data on short (2–3 days) versus longer course of IV antibiotics (5 days) for preschool children with severe pneumonia [59]. In preschool outpatients with RCCAP, a 5-day course with high dose amoxicillin (80 mg/kg/d; TID) was not inferior to a 10-day course. A 3-day course was associated with an unacceptable failure rate in this prospective study in a country with high penicillin resistance [60].
For non-severe pneumonia in under-fives, a short course (3 days) of antibiotics seems to be as effective as a long course (5 days), based on 4 prospective studies from LMIC. However, the WHO-definition of pneumonia was used in this study and therefore, many children with viral infections might have been included [61], [62]. In under-fives with RCCAP in a region with low pneumococcal penicillin resistance, oral amoxicillin (50 mg/kg/day) BD was as efficacious as TID dosing [63]. These results must be interpreted with caution, because of the impossibility to distinguish viral from bacterial pneumonia on chest radiograph. Twice daily normal dose amoxicillin was also used in comparative studies of amoxicillin with co-trimoxazole [32]. A pharmacokinetic study compared BD with TID dosing of 50 mg/kg/d amoxicillin in young children and concluded that the time above MIC was probably insufficient for higher concentration levels. Therefore, a 60–80 mg/kg/d dose should be considered in BD dosing [64].
Standard and double strength co-trimoxazole were equally effective in treating non-severe pneumonia with a treatment failure of about 20% in both groups (at 48 h) [65]. The absence of a difference and high treatment failure might be related to the (viral) etiology in non-severe pneumonia.
Adjunctive therapies
Corticosteroids
The role of systemic corticosteroids in pediatric CAP is far from clear. Two retrospective studies described an association with prolonged hospital stay and greater odds of re-hospitalization in cases with CAP without wheezing or asthma [66], [67]. In children with very severe pneumonia (ICU-setting), a 5-day methylprednisolone course with imipenem led to a faster resolution of symptoms compared to imipenem alone. This trial was small and not blinded [68]. Till now, systemic corticosteroids are not recommended in pediatric CAP without wheezing. Anecdotal reports describe fast improvement when adding steroids in severe pneumococcal CAP [69].
Oseltamivir
Retrospectively, there were no proven benefits for oseltamivir in hospitalized pediatric patients without underlying diseases or risk factors for developing a serious illness, including those with asthma [70]. Also the Cochrane meta-analysis, mainly based on 1 poorly designed study, described no significant benefit for oseltamivir treatment in children with pneumonia, although it might reduce the symptoms earlier, without other clinical relevance [71]. More well-designed studies are needed to study the role of oseltamivir in influenza pneumonia.
Specific circumstances
Pre-treated children
In previously healthy children hospitalized with CAP after oral antibiotic treatment, broad-spectrum showed better outcome compared to narrow-spectrum therapy in a retrospective study. Prospective studies are needed for appropriate recommendation [72].
Unvaccinated children
Most trials did not describe whether the included children were vaccinated against HiB. Beta-lactamase production by HiB may vary per region. According to local resistance patterns it should be decided to add a beta-lactamase inhibitor or prescribe 2nd/3rd generation cephalosporins [73].
Pleural empyema
Prolonged antimicrobial therapy is warranted, irrespective of additive treatment modalities such as video-assisted thoracoscopic surgery (VATS) or fibrinolysis. A retrospective study comparing outpatient IV versus oral treatment did not show differences in outcome, thus promoting oral treatment [74]. This was confirmed by another retrospective cohort study evaluating 2132 children with empyema. Treatment failure rates were identical in both groups: PICC 3.2%, and orally 2.6% [75]. Currently, there is no evidence recommending specific antimicrobial therapy. The majority of thoracic empyema is caused by SP (notably serotype 1), followed by S. aureus [76]. Antibiotic choice should be directed by culture or PCR and be as narrow as possible. In case of SP or S. aureus, additive clindamycin or rifampicin have been mentioned. Duration suggestions range from continuing antibiotics for 5–7 days after resolution of fever till extending the antibiotic course with 2–4 weeks after discharge [76], [77].
Discussion
The incomplete knowledge about the optimal treatment of CAP is defined by the fact that the etiology is difficult to establish and is often multifactorial: viral and bacterial. Pulmonary samples are hard to obtain, therefore surrogate markers from the upper respiratory tract are often used. The available etiologic studies are incomparable because of the different sampling methods, laboratory techniques, and definition of pneumonia among the studies. From the summarized studies, it seemed that in 15–25% bacterial etiology is probable, except for the study of Honkinen, who detected bacteria in the induced sputum of 91% of hospitalized children (culture and PCR) and the study of Pavia (40–60% nasopharyngeal bacteria, culture) [23], [25]. In the majority of children from the Honkinen study, the sputum was aspirated trough the nostrils, probably also retrieving nasopharyngeal pathogens. The positive predictive value of nasopharyngeal bacterial pathogens reflecting lower respiratory tract pathogens is not optimal. Therefore, it cannot be concluded whether nasopharyngeal pathogens are only colonizing the respiratory tract or also are the pneumonia-causing pathogen. Most etiology studies investigated clinical CAP-cases and might therefore not represent non-severe CAP. At a hospital level, there is a higher chance for a bacterial cause of CAP compared to the community level [6]. It is clear that viruses play an important role in the majority of childhood CAP, especially in the under-fives. Because viruses (mainly RSV, HRV and influenza) seem to play an important role in severe CAP, they might even play a more important role in non-severe CAP. However, respiratory viruses are also detected in the upper respiratory tract of healthy children, but with less frequency compared to cases [21], [26].
The therapeutic studies differed in settings, doses, outcomes and diagnosis (RC vs. WHO-definition). Moreover, resistance rates were highly diverse, if at all accounted for. The validity and generalizability of many trials is low, and composite endpoints were used in many trials, such as ‘treatment failure’ [78]. Etiologies were often not extensively studied and this might lead to a validity threat. Also, the trials comparing IV vs. oral regimens were not blinded because of ethical issues. In the large LMIC studies, antimicrobial pre-treatment was often not adjusted for. However, this was probably an important contributor for treatment failure. Most large studies derived from LMIC and are probably not representative for developed countries simply because the WHO-algorithm used for pneumonia at the local level health services is not used in developed settings. The treatment failure rates were diverse. Strikingly in non-severe pneumonia the failure rates were on average not lower compared to severe pneumonia, stressing the fact that the etiology might be non-bacterial (failure rates of ∼7–20%).
The specificity of the WHO criteria for RCCAP is low, about 20%. Adding fever to the WHO criteria improves the specificity substantially (∼45%) with a very small reduction in the sensitivity [79]. At a community and rural level these criteria can be used to identify a child at risk possibly needing live-saving treatment. But in an industrialized city setting, more experience and diagnostics are available to establish the severity of the clinical pneumonia. Unfortunately, a rapid and reliable test to distinguish viral- from bacterial pneumonia is still lacking in this setting; only then its treatment can be fully rationalized. Decision rules are currently being explored to decrease the number of children that are prescribed antibiotics in case of probable viral CAP (personal communication) [80].
In young children, cough and fast breathing without fever do not justify antibiotics. Watchful waiting with a return visit is suggested. It is impossible to distinguish pneumonia from bronchiolitis or viral wheeze based on the WHO criteria alone. In case of clinical severe pneumonia with fever or RCCAP, oral amoxicillin is proven to be effective in the majority of children and equivalent or superior compared to co-trimoxazole. Oral amoxicillin is equivalent to IV narrow-spectrum beta-lactam, and IV narrow-spectrum beta-lactam treatment is not inferior to broad-spectrum beta-lactam antibiotics. The doses of amoxicillin used in the cited studies vary. Therefore, it is difficult to compare whether the clinical effect is depending on the dose. A normal dose (40–50 mg/kg/d; TID) would be sufficient in a setting with low levels of penicillin resistance. BD dosing is questioned because of failure of some patients to reach a concentration > MIC > 50% of time. In case of high-level penicillin resistance, BD dosing is not preferred. The duration for probable uncomplicated bacterial pneumonia should not extend 5 days. Based on small studies, macrolide antibiotics are not inferior to beta-lactam antibiotics, but also not proven to be superior, not even in older children. In addition, beta-lactam/macrolide combination therapy was never shown to be clearly beneficial but there is a lack of good studies. Because of the rapid development of macrolide resistance; small-spectrum beta-lactam antibiotics are preferred in case of CAP. There is no reason to initiate a second or third generation cephalosporin treatment in uncomplicated CAP in a vaccinated child without recent pretreatment. These might be indicated in case of suspected gram-negative or S. aureus after influenza infection, severe pneumonia or in children with a previous medical history. There is hardly evidence for adjunctive therapies in childhood CAP.
Conclusion
The optimal antimicrobial management of childhood CAP depends on the etiology, age, local vaccination policies and resistance patterns. As long as non-rapid surrogate markers are used to distinguish viral- from bacterial pneumonia, the management is probably suboptimal.
For a young child with signs of non-severe pneumonia (with or without wheezing) who is otherwise doing well, watchful waiting would be recommended because of probable viral etiology. For children with more severe CAP with fever, oral amoxicillin or narrow-spectrum IV beta-lactam therapy would be the first choice. There is no clear evidence for superiority of a macrolide-based regimen for all ages. Five days should be enough to treat uncomplicated pneumonia and the dosage will depend on local penicillin resistance rates. Broad-spectrum therapy covering beta-lactamase producing bacteria is warranted in the case of very severe disease or pre-treated children.
Financial support
The author is supported by grants from ESPID, Stichting Coolsingel and ZonMw. These sponsors had no involvement in the collection, analysis, and interpretation of data, or in the writing of the manuscript.
Compliance with ethical standards
This article does not contain any studies with human participants performed by any of the authors.
Educational aims
The reader will be able to
-
•
Understand the epidemiology of childhood CAP and effects of universal Hib- and pneumococcal vaccination.
-
•
Identify problems with establishing the causative pathogen for childhood CAP.
-
•
Recognize CAP in under-fives is often viral in origin, thus not needing antibiotics.
-
•
Prescribe adequate antimicrobial treatment (spectrum, route and duration) for uncomplicated and complicated childhood CAP.
-
•
Realize that the evidence for macrolide treatment in childhood CAP is scarce.
Future research directions
-
•
To create decision algorithms to help doctors rationally prescribe antibiotics for CAP.
-
•
To develop rapid markers, including transcriptomics, to distinguish between viral and bacterial etiology of childhood CAP.
-
•
To identify patients that might benefit from add-on macrolide therapy.
Acknowledgements
Prof. Andrew Cant provided some useful suggestions during the writing phase of this review
References
- 1.Walker C.L.F., Rudan I., Liu L., Nair H., Theodoratou E., Bhutta Z. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381:1405–1416. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliwa J., Karumbi J., Marais B., Madhi S., Graham S. Tuberculosis as a cause or comorbidity of childhood pneumonia in tuberculosis-endemic areas: a systematic review. Lancet Respir Med. 2015;3:235–243. doi: 10.1016/S2213-2600(15)00028-4. [DOI] [PubMed] [Google Scholar]
- 3.Shann F. Etiology of severe pneumonia in children in developing countries. Pediatr Infect Dis. 1986;5:247–252. doi: 10.1097/00006454-198603000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Rudan I., Boschi Pinto C., Biloglav Z., Mulholland K., Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86:408–416. doi: 10.2471/BLT.07.048769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu L., Johnson H., Cousens S., Perin J., Scott S., Lawn J. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 6.Rudan I., O'Brien K., Nair H., Liu L., Theodoratou E., Qazi S. Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J Glob Health. 2013;3:010401. doi: 10.7189/jogh.03.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenberg D., Givon Lavi N., Ben Shimol S., Ziv J., Dagan R. Impact of PCV7/PCV13 introduction on community-acquired alveolar pneumonia in children <5 years. Vaccine. 2015;33:4623–4629. doi: 10.1016/j.vaccine.2015.06.062. [DOI] [PubMed] [Google Scholar]
- 8.Theodoratou E., Johnson S., Jhass A., Madhi S., Clark A., Boschi Pinto C. The effect of Haemophilus influenzae type b and pneumococcal conjugate vaccines on childhood pneumonia incidence, severe morbidity and mortality. Int J Epidemiol. 2010;39(Suppl 1):i172–i185. doi: 10.1093/ije/dyq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flasche S., Takahashi K., Vu D., Suzuki M., Nguyen T., Le H. Early indication for a reduced burden of radiologically confirmed pneumonia in children following the introduction of routine vaccination against Haemophilus influenzae type b in Nha Trang, Vietnam. Vaccine. 2014;32:6963–6970. doi: 10.1016/j.vaccine.2014.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner G.D.H., Bunthi C., Wonodi C., Morpeth S., Molyneux C., Zaki S. The role of postmortem studies in pneumonia etiology research. Clin Infect Dis. 2012;54(Suppl 2):S165–S171. doi: 10.1093/cid/cir1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCulloh R., Koster M., Yin D., Milner T., Ralston S., Hill V. Evaluating the use of blood cultures in the management of children hospitalized for community-acquired pneumonia. PLoS ONE. 2015;10:e0117462. doi: 10.1371/journal.pone.0117462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andrews A., Simpson A., Heine D., Teufel R. A cost-effectiveness analysis of obtaining blood cultures in children hospitalized for community-acquired pneumonia. J Pediatr. 2015 doi: 10.1016/j.jpeds.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 13.Bustamante Calvillo M.E., Velázquez F.R., Cabrera Munõz L., Torres J., Gómez Delgado A., Moreno J.A. Molecular detection of respiratory syncytial virus in postmortem lung tissue samples from Mexican children deceased with pneumonia. Pediatr Infect Dis J. 2001;20:495–501. doi: 10.1097/00006454-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Hu H., He L., Dmitriev A., Hu Y., Deng J., Zhang W. The role of Haemophilus influenzae type b in fatal community-acquired pneumonia in Chinese children. Pediatr Infect Dis J. 2008;27:942–944. doi: 10.1097/INF.0b013e3181757b32. [DOI] [PubMed] [Google Scholar]
- 15.Levine O., O'Brien K., Deloria Knoll M., Murdoch D., Feikin D., DeLuca A. The Pneumonia Etiology Research for Child Health Project: a 21st century childhood pneumonia etiology study. Clin Infect Dis. 2012;54(Suppl 2):S93–S101. doi: 10.1093/cid/cir1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pernica J., Moldovan I., Chan F., Slinger R. Real-time polymerase chain reaction for microbiological diagnosis of parapneumonic effusions in Canadian children. Can J Infect Dis Med Microbiol. 2014;25:151–154. doi: 10.1155/2014/757963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sakran W., Ababseh Z.E.D., Miron D., Koren A. Thoracic empyema in children: clinical presentation, microbiology analysis and therapeutic options. J Infect Chemother. 2014;20:262–265. doi: 10.1016/j.jiac.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 18.De Schutter I., Vergison A., Tuerlinckx D., Raes M., Smet J., Smeesters P. Pneumococcal aetiology and serotype distribution in paediatric community-acquired pneumonia. PLoS ONE. 2014;9:e89013. doi: 10.1371/journal.pone.0089013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lochindarat S., Teeratakulpisarn J., Warachit B., Chanta C., Thapa K., Gilbert G. Bacterial etiology of empyema thoracis and parapneumonic pleural effusion in Thai children aged less than 16 years. Southeast Asian J Trop Med Public Health. 2014;45:442–454. [PubMed] [Google Scholar]
- 20.Zampoli M., Kappos A., Wolter N., von Gottberg A., Verwey C., Mamathuba R. Etiology and incidence of pleural empyema in South African children. Pediatr Infect Dis J. 2015;34:1305–1310. doi: 10.1097/INF.0000000000000880. [DOI] [PubMed] [Google Scholar]
- 21.Hammitt L., Kazungu S., Morpeth S., Gibson D., Mvera B., Brent A. A preliminary study of pneumonia etiology among hospitalized children in Kenya. Clin Infect Dis. 2012;54(Suppl 2):S190–S199. doi: 10.1093/cid/cir1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mermond S., Zurawski V., D'Ortenzio E., Driscoll A., DeLuca A., Deloria Knoll M. Lower respiratory infections among hospitalized children in New Caledonia: a pilot study for the Pneumonia Etiology Research for Child Health Project. Clin Infect Dis. 2012;54(Suppl 2):S180–S189. doi: 10.1093/cid/cir1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Honkinen M., Lahti E., Österback R., Ruuskanen O., Waris M. Viruses and bacteria in sputum samples of children with community-acquired pneumonia. Clin Microbiol Infect. 2012;18:300–307. doi: 10.1111/j.1469-0691.2011.03603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elemraid M., Sails A., Eltringham G.J.A., Perry J., Rushton S., Spencer D. Aetiology of paediatric pneumonia after the introduction of pneumococcal conjugate vaccine. Eur Respir J. 2013;42:1595–1603. doi: 10.1183/09031936.00199112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pavia A. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. 2011;52(Suppl 4):S284–S289. doi: 10.1093/cid/cir043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jain S., Williams D., Arnold S., Ampofo K., Bramley A., Reed C. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu J., Ai H., Xiong Y., Li F., Wen Z., Liu W. Prevalence and correlation of infectious agents in hospitalized children with acute respiratory tract infections in Central China. PLoS ONE. 2015;10:e0119170. doi: 10.1371/journal.pone.0119170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lochindarat S., Suwanjutha S., Prapphal N., Chantarojanasiri T., Bunnag T., Deerojanawong J. Mycoplasma pneumoniae and Chlamydophila pneumoniae in children with community-acquired pneumonia in Thailand. Int J Tuberc Lung Dis. 2007;11:814–819. [PubMed] [Google Scholar]
- 29.Finelli L., Fiore A., Dhara R., Brammer L., Shay D., Kamimoto L. Influenza-associated pediatric mortality in the United States: increase of Staphylococcus aureus coinfection. Pediatrics. 2008;122:805–811. doi: 10.1542/peds.2008-1336. [DOI] [PubMed] [Google Scholar]
- 30.Straus W.L., Qazi S.A., Kundi Z., Nomani N.K., Schwartz B. Antimicrobial resistance and clinical effectiveness of co-trimoxazole versus amoxycillin for pneumonia among children in Pakistan: randomised controlled trial. Pakistan Co-trimoxazole Study Group. Lancet. 1998;352:270–274. doi: 10.1016/s0140-6736(97)10294-x. [DOI] [PubMed] [Google Scholar]
- 31.Lodha R., Kabra S., Pandey R. Antibiotics for community-acquired pneumonia in children. Cochrane Database Syst Rev. 2013;6:CD004874. doi: 10.1002/14651858.CD004874.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Catchup Study Group Clinical efficacy of co-trimoxazole versus amoxicillin twice daily for treatment of pneumonia: a randomised controlled clinical trial in Pakistan. Arch Dis Child. 2002;86:113–118. doi: 10.1136/adc.86.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Das R., Singh M. Treatment of severe community-acquired pneumonia with oral amoxicillin in under-five children in developing country: a systematic review. PLoS ONE. 2013;8:e66232. doi: 10.1371/journal.pone.0066232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bari A., Sadruddin S., Khan A., Khan Iu.H., Lehri I., Macleod W. Community case management of severe pneumonia with oral amoxicillin in children aged 2–59 months in Haripur district, Pakistan: a cluster randomised trial. Lancet. 2011;378:1796–1803. doi: 10.1016/S0140-6736(11)61140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Soofi S., Ahmed S., Fox M., MacLeod W., Thea D., Qazi S. Effectiveness of community case management of severe pneumonia with oral amoxicillin in children aged 2–59 months in Matiari district, rural Pakistan: a cluster-randomised controlled trial. Lancet. 2012;379:729–737. doi: 10.1016/S0140-6736(11)61714-5. [DOI] [PubMed] [Google Scholar]
- 36.Campbell H., Byass P., Forgie I.M., O'Neill K.P., Lloyd Evans N., Greenwood B.M. Trial of co-trimoxazole versus procaine penicillin with ampicillin in treatment of community-acquired pneumonia in young Gambian children. Lancet. 1988;2:1182–1184. doi: 10.1016/s0140-6736(88)90244-9. [DOI] [PubMed] [Google Scholar]
- 37.Hazir T., Nisar Y., Abbasi S., Ashraf Y., Khurshid J., Tariq P. Comparison of oral amoxicillin with placebo for the treatment of world health organization-defined nonsevere pneumonia in children aged 2–59 months: a multicenter, double-blind, randomized, placebo-controlled trial in Pakistan. Clin Infect Dis. 2011;52:293–300. doi: 10.1093/cid/ciq142. [DOI] [PubMed] [Google Scholar]
- 38.Awasthi S., Agarwal G., Kabra S., Singhi S., Kulkarni M., More V. Does 3-day course of oral amoxycillin benefit children of non-severe pneumonia with wheeze: a multicentric randomised controlled trial. PLoS ONE. 2008;3:e1991. doi: 10.1371/journal.pone.0001991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Addo Yobo E., Chisaka N., Hassan M., Hibberd P., Lozano J., Jeena P. Oral amoxicillin versus injectable penicillin for severe pneumonia in children aged 3 to 59 months: a randomised multicentre equivalency study. Lancet. 2004;364:1141–1148. doi: 10.1016/S0140-6736(04)17100-6. [DOI] [PubMed] [Google Scholar]
- 40.Hazir T., Fox L., Nisar Y., Fox M., Ashraf Y., MacLeod W. Ambulatory short-course high-dose oral amoxicillin for treatment of severe pneumonia in children: a randomised equivalency trial. Lancet. 2008;371:49–56. doi: 10.1016/S0140-6736(08)60071-9. [DOI] [PubMed] [Google Scholar]
- 41.Aurangzeb B., Hameed A. Comparative efficacy of amoxicillin, cefuroxime and clarithromycin in the treatment of community -acquired pneumonia in children. J Coll Physicians Surg Pak. 2003;13:704–707. [PubMed] [Google Scholar]
- 42.Asghar R., Banajeh S., Egas J., Hibberd P., Iqbal I., Katep Bwalya M. Chloramphenicol versus ampicillin plus gentamicin for community acquired very severe pneumonia among children aged 2–59 months in low resource settings: multicentre randomised controlled trial (SPEAR study) BMJ. 2008;336:80–84. doi: 10.1136/bmj.39421.435949.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duke T., Poka H., Dale F., Michael A., Mgone J., Wal T. Chloramphenicol versus benzylpenicillin and gentamicin for the treatment of severe pneumonia in children in Papua New Guinea: a randomised trial. Lancet. 2002;359:474–480. doi: 10.1016/S0140-6736(02)07677-8. [DOI] [PubMed] [Google Scholar]
- 44.Jibril H.B., Ifere O.A., Odumah D.U. An open, comparative evaluation of amoxycillin and amoxycillin plus clavulanic acid (‘Augmentin’) in the treatment of bacterial pneumonia in children. Curr Med Res Opin. 1989;11:585–592. doi: 10.1185/03007998909112675. [DOI] [PubMed] [Google Scholar]
- 45.Tsarouhas N., Shaw K.N., Hodinka R.L., Bell L.M. Effectiveness of intramuscular penicillin versus oral amoxicillin in the early treatment of outpatient pediatric pneumonia. Pediatr Emerg Care. 1998;14:338–341. [PubMed] [Google Scholar]
- 46.Ambroggio L., Test M., Metlay J., Graf T., Ann Blosky M., Macaluso M. Comparative effectiveness of beta-lactam versus macrolide monotherapy in children with pneumonia diagnosed in the outpatient setting. Pediatr Infect Dis J. 2015;34:839–842. doi: 10.1097/INF.0000000000000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ambroggio L., Test M., Metlay J., Graf T., Blosky M., Macaluso M. Beta-lactam versus beta- lactam/macrolide therapy in pediatric outpatient pneumonia. Pediatr Pulmonol. 2015 doi: 10.1002/ppul.23312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wubbel L., Muniz L., Ahmed A., Trujillo M., Carubelli C., McCoig C. Etiology and treatment of community-acquired pneumonia in ambulatory children. Pediatr Infect Dis J. 1999;18:98–104. doi: 10.1097/00006454-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Kogan R., Martínez M.A., Rubilar L., Payá E., Quevedo I., Puppo H. Comparative randomized trial of azithromycin versus erythromycin and amoxicillin for treatment of community-acquired pneumonia in children. Pediatr Pulmonol. 2003;35:91–98. doi: 10.1002/ppul.10180. [DOI] [PubMed] [Google Scholar]
- 50.Leyenaar J., Shieh M., Lagu T., Pekow P., Lindenauer P. Comparative effectiveness of ceftriaxone in combination with a macrolide compared with ceftriaxone alone for pediatric patients hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2014;33:387–392. doi: 10.1097/INF.0000000000000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bradley J., Arguedas A., Blumer J., Sáez Llorens X., Melkote R., Noel G. Comparative study of levofloxacin in the treatment of children with community-acquired pneumonia. Pediatr Infect Dis J. 2007;26:868–878. doi: 10.1097/INF.0b013e3180cbd2c7. [DOI] [PubMed] [Google Scholar]
- 52.Dinur Schejter Y., Cohen Cymberknoh M., Tenenbaum A., Brooks R., Averbuch D., Kharasch S. Antibiotic treatment of children with community-acquired pneumonia: comparison of penicillin or ampicillin versus cefuroxime. Pediatr Pulmonol. 2013;48:52–58. doi: 10.1002/ppul.22534. [DOI] [PubMed] [Google Scholar]
- 53.Queen M., Myers A., Hall M., Shah S., Williams D., Auger K. Comparative effectiveness of empiric antibiotics for community-acquired pneumonia. Pediatrics. 2014;133:e23–e29. doi: 10.1542/peds.2013-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams D., Hall M., Shah S., Parikh K., Tyler A., Neuman M. Narrow vs broad-spectrum antimicrobial therapy for children hospitalized with pneumonia. Pediatrics. 2013;132:e1141–e1148. doi: 10.1542/peds.2013-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Amarilyo G., Glatstein M., Alper A., Scolnik D., Lavie M., Schneebaum N. IV Penicillin G is as effective as IV cefuroxime in treating community-acquired pneumonia in children. Am J Ther. 2014;21:81–84. doi: 10.1097/MJT.0b013e3182459c28. [DOI] [PubMed] [Google Scholar]
- 56.Atkinson M., Lakhanpaul M., Smyth A., Vyas H., Weston V., Sithole J. Comparison of oral amoxicillin and intravenous benzyl penicillin for community acquired pneumonia in children (PIVOT trial): a multicentre pragmatic randomised controlled equivalence trial. Thorax. 2007;62:1102–1106. doi: 10.1136/thx.2006.074906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lorgelly P.K., Atkinson M., Lakhanpaul M., Smyth A.R., Vyas H., Weston V. Oral versus i.v. antibiotics for community-acquired pneumonia in children: a cost-minimisation analysis. Eur Respir J. 2010;35:858–864. doi: 10.1183/09031936.00087209. [DOI] [PubMed] [Google Scholar]
- 58.Ribeiro C., Ferrari G., Fioretto J. Antibiotic treatment schemes for very severe community-acquired pneumonia in children: a randomized clinical study. Rev Panam Salud Publica. 2011;29:444–450. [PubMed] [Google Scholar]
- 59.Lassi Z., Imdad A., Bhutta Z. Short-course versus long-course intravenous therapy with the same antibiotic for severe community-acquired pneumonia in children aged two months to 59 months. Cochrane Database Syst Rev. 2015;6:CD008032. doi: 10.1002/14651858.CD008032.pub2. [DOI] [PubMed] [Google Scholar]
- 60.Greenberg D., Givon Lavi N., Sadaka Y., Ben Shimol S., Bar Ziv J., Dagan R. Short-course antibiotic treatment for community-acquired alveolar pneumonia in ambulatory children: a double-blind, randomized, placebo-controlled trial. Pediatr Infect Dis J. 2014;33:136–142. doi: 10.1097/INF.0000000000000023. [DOI] [PubMed] [Google Scholar]
- 61.Haider B., Saeed M., Bhutta Z. Short-course versus long-course antibiotic therapy for non-severe community-acquired pneumonia in children aged 2 months to 59 months. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD005976.pub2. [DOI] [PubMed] [Google Scholar]
- 62.Pakistan Multicentre Amoxycillin Short Course Therapy (MASCOT) pneumonia study group Clinical efficacy of 3 days versus 5 days of oral amoxicillin for treatment of childhood pneumonia: a multicentre double-blind trial. Lancet. 2002;360:835–841. doi: 10.1016/S0140-6736(02)09994-4. [DOI] [PubMed] [Google Scholar]
- 63.Vilas Boas A., Fontoura M., Xavier Souza G., Araújo Neto C., Andrade S., Brim R. Comparison of oral amoxicillin given thrice or twice daily to children between 2 and 59 months old with non-severe pneumonia: a randomized controlled trial. J Antimicrob Chemother. 2014;69:1954–1959. doi: 10.1093/jac/dku070. [DOI] [PubMed] [Google Scholar]
- 64.Fonseca W., Hoppu K., Rey L., Amaral J., Qazi S. Comparing pharmacokinetics of amoxicillin given twice or three times per day to children older than 3 months with pneumonia. Antimicrob Agents Chemother. 2003;47:997–1001. doi: 10.1128/AAC.47.3.997-1001.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rasmussen Z., Bari A., Qazi S., Rehman G., Azam I., Khan S. Randomized controlled trial of standard versus double dose cotrimoxazole for childhood pneumonia in Pakistan. Bull World Health Organ. 2005;83:10–19. [PMC free article] [PubMed] [Google Scholar]
- 66.Ambroggio L., Test M., Metlay J., Graf T., Blosky M., Macaluso M. Adjunct systemic corticosteroid therapy in children with community-acquired pneumonia in the outpatient setting. J Pediatric Infect Dis Soc. 2015;4:21–27. doi: 10.1093/jpids/piu017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weiss A., Hall M., Lee G., Kronman M., Sheffler Collins S., Shah S. Adjunct corticosteroids in children hospitalized with community-acquired pneumonia. Pediatrics. 2011;127:e255–e263. doi: 10.1542/peds.2010-0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nagy B., Gaspar I., Papp A., Bene Z., Voko Z., Balla G. Efficacy of methylprednisolone in children with severe community acquired pneumonia. Pediatr Pulmonol. 2013;48:168–175. doi: 10.1002/ppul.22574. [DOI] [PubMed] [Google Scholar]
- 69.Lavi E., Shoseyov D., Simanovsky N., Brooks R. Systemic steroid treatment for severe expanding pneumococcal pneumonia. Case Rep Pediatr. 2015;2015:186302. doi: 10.1155/2015/186302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bueno M., Calvo C., Méndez Echevarría A., de José M., Santos M., Carrasco J. Oseltamivir treatment for influenza in hospitalized children without underlying diseases. Pediatr Infect Dis J. 2013;32:1066–1069. doi: 10.1097/INF.0b013e31829be4bc. [DOI] [PubMed] [Google Scholar]
- 71.Jefferson T., Jones M., Doshi P., Spencer E., Onakpoya I., Heneghan C. Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments. BMJ. 2014;348:g2545. doi: 10.1136/bmj.g2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Breuer O., Blich O., Cohen Cymberknoh M., Averbuch D., Kharasch S., Shoseyov D. Antibiotic treatment for children hospitalized with community-acquired pneumonia after oral therapy. Pediatr Pulmonol. 2015;50:495–502. doi: 10.1002/ppul.23159. [DOI] [PubMed] [Google Scholar]
- 73.Esposito S., Cohen R., Domingo J., Pecurariu O., Greenberg D., Heininger U. Antibiotic therapy for pediatric community-acquired pneumonia: do we know when, what and for how long to treat? Pediatr Infect Dis J. 2012;31:e78–e85. doi: 10.1097/INF.0b013e318255dc5b. [DOI] [PubMed] [Google Scholar]
- 74.Stockmann C., Ampofo K., Pavia A., Byington C., Sheng X., Greene T. Comparative effectiveness of oral versus outpatient parenteral antibiotic therapy for empyema. Hosp Pediatr. 2015 doi: 10.1542/hpeds.2015-0100. [DOI] [PubMed] [Google Scholar]
- 75.Shah S.S., Srivastava R., Wu S., Colvin J.D., Williams D.J., Rangel S.J. Intravenous versus oral antibiotics for postdischarge treatment of complicated pneumonia. Pediatrics. 2016;138:e20161692. doi: 10.1542/peds.2016-1692. Epub 2016 Nov 17. [DOI] [PubMed] [Google Scholar]
- 76.Proesmans M., De Boeck K. Clinical practice: treatment of childhood empyema. Eur J Pediatr. 2009;168:639–645. doi: 10.1007/s00431-009-0929-9. [DOI] [PubMed] [Google Scholar]
- 77.Walker W., Wheeler R., Legg J. Update on the causes, investigation and management of empyema in childhood. Arch Dis Child. 2011;96:482–488. doi: 10.1136/adc.2009.165357. [DOI] [PubMed] [Google Scholar]
- 78.Hibberd P., Patel A. Challenges in the design of antibiotic equivalency studies: the multicenter equivalency study of oral amoxicillin versus injectable penicillin in children aged 3–59 months with severe pneumonia. Clin Infect Dis. 2004;39:526–531. doi: 10.1086/422453. [DOI] [PubMed] [Google Scholar]
- 79.Cardoso M., Nascimento Carvalho C., Ferrero F., Alves F., Cousens S. Adding fever to WHO criteria for diagnosing pneumonia enhances the ability to identify pneumonia cases among wheezing children. Arch Dis Child. 2011;96:58–61. doi: 10.1136/adc.2010.189894. [DOI] [PubMed] [Google Scholar]
- 80.Ferrero F., Adrián Torres F., Domínguez P., Ossorio M. Efficacy and safety of a decision rule for using antibiotics in children with pneumonia and vaccinated against pneumococcus. A randomized controlled trial. Arch Argent Pediatr. 2015;113:397–403. doi: 10.5546/aap.2015.eng.397. [DOI] [PubMed] [Google Scholar]