Abstract
Background
Crises affecting civilian infrastructure (including electricity supply, clean water, and access to institutional health services) may have an effect on the delivery of pharmacy services in the community.
Objectives
The objectives were to describe and analyze the impact of 2 major crises (the severe acute respiratory syndrome [SARS] outbreak, and the electrical system failure [“blackout”]) on pharmacy practice and pharmacists in Toronto, Canada.
Methods
An exploratory, qualitative study was undertaken. Pharmacists were recruited, provided informed consent, and were interviewed. Data from transcripts were coded and categorized to identify themes related to adaptive strategies undertaken by pharmacists during times of civil crisis.
Results
Five key themes emerged from this research: (1) during times of crisis, pharmacies become frontline health care facilities, (2) a vacuity of leadership/lack of utility of emergency preparedness guidelines and policies, (3) role of and reliance on experience and professional judgment, (4) importance of documentation, and (5) the importance of “teamness” in enabling successful adaptation during times of crisis.
Conclusions
Emergencies and civil crises will continue to occur. Findings of this study include the importance of effective documentation systems and teamwork practices, as well as confident reliance on professional judgment and experience, as determinants of successful adaptation to civil crises.
Keywords: Pharmacy practice, Emergency preparedness, Disaster readiness, Civil crisis
1. Background
Since the events of September 11, 2001 there has been an urgent need for all citizens to be adequately prepared for civil disasters or crises.1 Emergency preparedness, once the purview of elite teams of health care professionals or highly skilled individuals such as paramedics or firefighters, has now become an everyday preoccupation.2 A fundamental premise of such emergency preparedness that has now emerged is the understanding that “rescue” or relief will likely not come immediately and that individuals must, to a large degree, fend for themselves during the initial aftermath of any major catastrophic situation.3, 4
Health professionals, in general, may be somewhat more comfortable than most in dealing with or providing leadership during emergency situations, given the independent nature of health care work itself.5, 6 However, few health care professionals are prepared for the breakdown of the civilian infrastructure that supports their day-to-day practice.7, 8, 9, 10, 11 For example, prolonged absence of electricity (and commensurate problems with use of refrigerators or computers), potable water, and supplies and other events that may commonly occur during a natural or human-made disaster will fundamentally affect the way in which health care may be provided to patients. Of course, during such times of civil crisis, the general population's need for health care services may also be expected to rise significantly.2, 7
Within the profession of pharmacy, there has been some literature published related to disaster preparedness. In general, this consists of hypothetical legal-ethical debates or discussion, or policy documents published by professional or regulatory associations designed to provide pharmacists with guidelines for responding during times of civil crisis.12, 13, 14, 15 Of interest, there are few published reports outlining the real-world response of pharmacists during times of disaster. Teeter12 commented on the application of the Comprehensive Emergency Management model within the community pharmacy context, noting that “…only a few organizations…have made emergency management a priority,” and that “pharmacists…have little time available to devoted to preparing for disasters and terrorism.” Pedersen et al16 reported on results of a survey to identify pharmacists' opinions regarding their level of involvement in emergency preparedness, and noted that those who have previously been involved in emergency training or emergency situations place a higher premium on preparedness.
Sadly, over the past decade, there have been many circumstances that have resulted in the breakdown of civic and health system infrastructure. In Ontario, Canada, there have been two particularly noteworthy events—the severe acute respiratory syndrome (SARS) outbreak of 200317 and the electricity “blackout” of the Eastern Seaboard of North America in August 2004. These widely publicized and unpredicted events affected wide swaths of the population, and resulted in significant issues related to the delivery of health care services.
The SARS outbreak occurred over a 4-month period in the late winter and early spring of 2003. The pathogenesis and epidemiology of SARS have been described elsewhere18; briefly, it is believed that a single patient-vector transmitted the virus from Hong Kong to Canada, where it then spread rapidly through certain communities, resulting in over 50 deaths in the metropolitan Toronto area. Importantly, the disease was first isolated within health care institutions, and consequently some of those who died were health care professionals such as nurses and physicians. At its peak, the SARS crisis resulted in the World Health Organization (WHO) issuing a major travel advisory cautioning international visitors about visiting the city of Toronto, Canada. As Canada is a First World country priding itself upon its health care and civic infrastructure, the WHO directive was unprecedented—and reasonable given the lack of understanding of how the illness was spreading and what its implications may be.
In August 2004, a massive electricity blackout occurred over much of the Eastern Seaboard of the United States and several Canadian provinces. Once again, the city of Toronto and many parts of the province of Ontario were significantly affected. Although hydroelectric workers moved quickly to restore power within a reasonable period of time, parts of the city remained without electricity for close to a week. Even after restoration of power, there were ongoing concerns regarding the fragility of the electrical grid and rolling brownouts due to local electricity supply and distribution problems.
In the case of both SARS and the blackout, there was still an urgent need to ensure that health care services were available to the public. An important component of these health care services includes medication dispensing and pharmacy care services provided by pharmacists and pharmacies.19 Despite the widespread civic disaster represented in both cases, pharmacists were still required (arguably more than ever) to be “at their posts,” available and able to provide health care services.
2. Research objective
The objective of this research was to describe and examine the experience of pharmacists, in the Greater Toronto Area to 2 major civic crises affecting professional practice—the SARS outbreak of 2003 and the blackout of August 2004.
3. Research method
An exploratory, qualitative study was undertaken using a method described by Denzin.20 A semistructured interview protocol was developed and piloted using 4 volunteer participants. Upon revision, the protocol and study were reviewed by the Ethics Review Board, and approval was received to continue with the study. Pharmacists were recruited for this study through advertisements at local continuing professional development events, where a general description of the study objectives and processes was provided. Those who were interested in participating were contacted by a research assistant who provided further details regarding the study, explained confidentiality provisions, and then completed signed informed consent. After completion of the consent procedure, participants scheduled a 30- to 45-minute telephone-based interview time with a research assistant. All participants were assured that interviews were confidential, that no identifying data or names would be presented, and that their anonymity was ensured.
In order to participate in this study, pharmacists were required to have been practicing as a pharmacist in a direct patient-care setting in Toronto for at least 25 h/wk during March 2003 to June 2003 (SARS) and August 2004 (blackout). No exclusion criteria were established because the inclusion criteria were deemed to be clear and comprehensive enough.
All interviews were recorded using a digital recorder and were transcribed verbatim. An initial coding structure was developed by all investigators. Analysis proceeded using a method described by Chi21 for coding and categorization of qualitative data. Briefly, this method involved the use of interative analysis of a random sample representing approximately 10% of the data by 2 independent reviewers until agreement on a coding structure was achieved. Once an agreed-upon coding structure had been developed, 2 independent reviewers analyzed another sample of data representing approximately 10% of the data using the coding structure. Where disagreements in coding occurred, a third reviewer was available to adjudicate differences. On the basis of this analysis, revisions to the original coding structure were undertaken to allow for development of a final coding tree. All remaining transcripts (representing approximately 80% of the data) were subsequently read and reviewed by 2 independent investigators; where disagreements in coding occurred, a third researcher was available to adjudicate, using the agreed-upon coding structure. In this way, reliability of analysis is strengthened while minimizing the number of different reviewers required to analyze data. This method of analysis has been used to interpret data collected from a variety of different data-gathering methods, including focus groups and interviews. Data were managed and stored using the software program Knowledge Forum v3 (University of Toronto, Toronto, Canada).
4. Results and discussion
A total of 39 pharmacists responded to the invitation to participate in this study. Of those who responded, 28 met the inclusion criteria and agreed to participate. Individual interviews were then scheduled. One participant dropped out before the interview because of personal scheduling reasons; consequently, a total of 27 pharmacists were interviewed for this study. A demographic profile of these participants is provided in Table 1. As indicated, most of the participants involved in this study were community practitioners during the time of both SARS and the blackout.
Table 1.
Demographic profile of participants (n = 27)
| Male:female ratio | 15:12 (56%:44%) |
| Mean number of years of experience as a pharmacist at the time of SARS (2003) | 9.4 ± 3.8 (range, 4-26 years) |
| Mean number of years spent working at community pharmacy site at the time of SARS (2003) | 6.9 ± 1.8 (range, 2-26 years) |
| Mean pharmacist:technician ratio at community pharmacy site at the time of SARS (2003) | 1:1.9 (range, 1:0-1:4) |
| Mean pharmacist:technician ratio at community pharmacy site at the time of blackout (2004) | 1:2.1 (range, 1:0-1:4) |
| Hospital:community ratio (primary practice site during both crises) | 7:20 (26%:74%) |
SARS, severe acute respiratory syndrome.
Interviews were undertaken pursuant to the finalized semistructured protocol ( Fig. 1). In addition to audio recording of interviews, extensive field notes were maintained to provide clarification of transcripts.
Fig. 1.
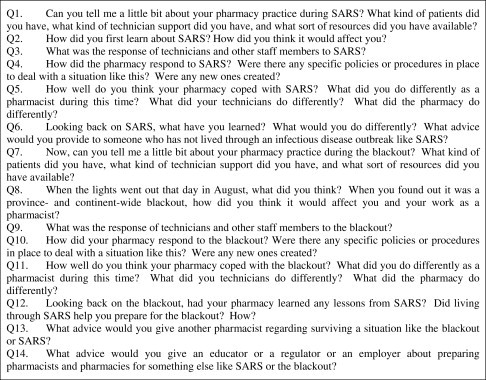
Interview schedule (excerpts).
Pharmacists who agreed to participate in this study represented both hospital and community practices. After iterative coding, categorization, analysis, and checking of data, 5 key themes emerged:
1. During times of civil crisis, pharmacies become frontline health care facilities
During the SARS crisis and the blackout, large institutional care centers, including large clinics and hospitals, were forced to remain closed, in an attempt to prevent the spread of the virus from institutions to the general community. As a result, during the SARS outbreak the health care system literally was suspended for many patients. Elective surgeries, new admissions, and even emergency care were redirected to other, nonaffected cities or centers where possible, or patients simply had to go without access to institutionally based physicians and nurses. During this time, study participants reported that their community pharmacies experienced a large increase in the number of patients they saw and an increase in the acuity level.
Roger: Where else are they supposed to go, right? The hospitals in quarantine, there's no clinics open…so they come to the pharmacy. It was really, really stressful—people were desperate and asking all kinds of questions because they had nowhere else to turn to. We were still open, we sell (medications) so they would come and ask us everything. I know we're not allowed to diagnose, but what choice do you have when everything else is closed?
Sandy: (I've been a pharmacist for 35 years.) The SARS time was probably the most rewarding time in my career, because for once the patients actually really really needed us. Any of them who had their doctors in the hospital, well, the hospitals were all closed, so they would come to us. I really think we shone, you know pharmacy real rose to the occasion and kept the (health care) system going.
Whereas some participants reported a sense of enthusiasm and excitement at being called upon to engage in frontline health care services such as this, other participants felt quite overwhelmed and very nervous.
Casey: How are we supposed to deal with this? If it was up to me, well, I know we couldn't really close up and go away but it was really stressful. We're pharmacists right, not doctors. But now all of sudden, they want me to diagnose things, or prescribe. It's hard to explain that I can't do that, it's against the law while I'm standing up beside all these shelves filled with drugs.
Karen: It was really unfair to us (during SARS). Here's this rampant infectious disease and, well it's bad enough they have to close all the hospitals down and then quarantine the staff, but the pharmacies, they're all open. So of course, what happens? Everyone goes to the pharmacy because the doctor is closed. We couldn't handle all the people, all the questions, it was way out of our scope. And patients got really pissed off of course because, well they need someone, but they can't get anyone and so we're it.
The traditional roles of pharmacists and pharmacies evolved considerably during times of crisis; for some pharmacists, this represented new opportunities to apply existing knowledge and skills, whereas for others it resulted in a daunting new reality, one that resulted in significant coping challenges.
2. The vacuity of leadership/lack of utility of emergency guidelines
A consistent theme across all interviews related to a commonly held sentiment—during times of crisis, one can only rely on oneself. During the SARS outbreak, the lack of understanding of the illness itself, coupled with disorganization and lack of communication from public health officials, resulted in individuals and groups seeking out leadership and decision making at the micro or local level:
Anne: It was just ridiculous. One day they said one thing, the next day the other. It was only when nurses started to die and there was still no “official” response that, well you take matters in your own hands, you know? You have to say, I don't know what's going on here, no one does, but I'm going to take care of myself. So I said, okay, we're going to wear gloves and masks when (we deal with our patients). I know they say that doesn't look professional, but it's safety first.
Interviewer: Did you receive any comments about this from your customers, or (head office)?
Anne: Nothing from the customers—I mean I think they probably thought it was a good idea too, right? Head office kept sending us e-mails saying there was no need to panic, and that we shouldn't wear masks because that would like send the wrong message and it wasn't needed. But then these nurses were dying. They were dying.
James: Our (regional manager) didn't know what to do…it's not his fault, I know. But how were we supposed to handle patients who were coughing, or who were sick. Rationally, well logically you know that not everyone who has a cold or a cough has SARS, right? But still, no one knew what was going on and no one could really tell us. So we had to make the decision ourself. We had to put the patients first, so of course we couldn't wear masks or gloves or anything while we were with them. Some of the technicians didn't like this, but, someone had to make a decision. And we used our common sense of course…we would clean up and sterilize the counters every half hour or so, limit contact with patients, all that sensible stuff.
Participants in the study were particularly critical of written policies, procedures, and guidelines that were developed under the auspices of “emergency preparedness.”
Karen: They were of no help at all. It was all so vague, and just kept on saying “use your professional judgment,” whatever that means. I know it's not possible to develop a policy and procedure for every single situation, and, well who could have predicted that there'd be SARS and the blackout. So I guess, well, these emergency guidelines aren't really ever much good.
Casey: It was a joke. I remember during the blackout, we were all scrambling around trying to figure what to do because we had no electricity. One of the technicians, she was looking through the policy manual we have, the one issued by (head office). She got to the section called Emergencies…and in the manual, she was referred to a Web site address! Yeah, in the middle of a blackout the information we need is on a Web site.
Tim: There were no lights, no electricity—even if we had an emergency plan, no one would have been able to find it because the computer wasn't working. You can't rely on guidelines or things like that when everything is falling apart…you've got to rely on yourself and your common sense.
Several participants noted that they had received “emergency preparedness training” of some sort, ranging from being required to read a policy/procedure/guideline to attendance at a workshop or lecture. All those who had received such training were unanimous in their belief that it simply did not (and likely could not) prepare them for the SARS outbreak or the blackout because these events were simply never conceived of nor discussed during training. Participants noted that the focus of their sessions tended toward bioterrorism or other similar situations, rather than the meltdown of the civilian infrastructure through an unpredictable event such as the blackout. Participants also noted that knowledge and skills gained from such training appeared to be of limited transferable utility in assisting them in coping with either crisis. Participants in this study were not asked to rate the quality of this prior training, nor to elaborate upon details.
3. The role of experience and professional judgment
Professional practice, at the best of times, is a highly context-sensitive and complex phenomenon, requiring individuals to make numerous microjudgments in a time-pressured environment. As practice has evolved, there has been increasing reliance on information and accessing information in electronic databases for decision support. During the blackout, lack of electricity meant that all electronic databases and records (including patients' profiles or drug information) were not available. Similarly, during SARS, there was virtually no information, studies, therapeutic guidelines, or other information that would assist pharmacists in making decisions.
Bill: It was supremely ironic actually. During the blackout, who do you think were the most valuable (pharmacists) I had? Not the young ones, the clinical hotshots. It was actually, the older ones, the ones who you know don't do pharmaceutical care, but actually know how to dispense, how to run a dispensary. They, well, the younger pharmacists, they didn't have a clue. They'd only ever known computerized patient records, and automatic allergy checking—most of them didn't even know how to hand-write a label! What got us through these crises—I know I'm not the only one who thinks this, I've talked with (other colleagues) too—it was the old guys, the ones that the young hotshots are always writing off as being out of date.
Karen: It wasn't any problem for me. When I first started working as a pharmacist, we didn't have any computers, just typewriters, so at least I knew how to produce a label, keep the dispensing record, all that stuff without computers. It was tough for everyone else, hard to get used to but in a strange way it was actually kind of fun for me.
James: Some of the younger pharmacists, I mean, well of course they're really bright and keen, right? But they would just get paralyzed, they just didn't know what to do. They were all ready to just close the store and say, sorry we can't help you and they expected that the customers would just understand that. Of course I had to explain, no, you can't do that. Whether there's SARS or a blackout or anything, people still need to get their drugs so we have to figure out a way to work around this problem. They just don't have the experience or the common sense sometimes.
Kelly: Some of the younger pharmacists, they were so worried about the rules and the laws. They were so paranoid, they wouldn't give another (salbutamol) inhaler to a patient, an asthma patient for years, because there were no refills! I'd say, well, the patient can't see the doctor because the office is closed, and they'd suggest the patient go to an emergency room, and well, most of them are closed too in the hospitals. And even if one was open—you know how busy they'd be? Why would you send someone there, to wait for hours and to clog up the system even more, when you can just bend the rule about repeats and deal with it after in some way. No one is going to complain and you're saving everybody here.
The more recent emphasis in pharmacy education on clinical skills and problem solving has, it may be argued, come at the expense of dispensing and practice management skills. Without a strong foundation in drug distribution systems management, it was consequently more difficult for newer graduates to adapt to the crisis situation and develop creative solutions to facilitate access to medications in the circumstance.
Jodi: I actually had to ask my mother…she was a nurse, but used to do a lot of dispensing of medications, so she was the one that gave some ideas about how to keep records about what was dispensed or what to do when you couldn't call the doctor, right, because she's so used to that. I know she thought it was cute, but it was actually kind of annoying to me that I really didn't have a clue what to do. I was supposed to be in charge here, and I couldn't think of anything besides closing the store!
Sandy: You feel like you're in a science fiction movie. It was like only about the bare basics, that's all anyone had time for, or that's all we could do because you had no computers. You actually don't realize how helpless you become without your computer. It was different in SARS because you could, well there just wasn't information or knowledge about it. But during the blackout, you couldn't get to information you knew was right in the computer and so, you just, well, like a deer in a headlight.
4. The importance of well-established documentation systems
A major theme for all participants related to their documentation practices during SARS and the blackout. In particular, there was recognition that these crises provoked responses by pharmacists that forced them to act in ways that may have been perilous from a medical legal perspective.
Tim: So if you've got this guy right there in front of you, and he's supposed to be getting (acetaminophen, caffeine, and codeine 30 mg) for his cancer, his pain, and he's telling you he's in pain, and he's got repeats left, but because of the blackout you can't open his file on the computer. What are you supposed to do? Tell him to come back next week when the Ohio Energy Authority restores some (power) line somewhere? You can't send him to a hospital. So you have to give him some, even though, if you're wrong, or he's lying or something that's like trafficking in narcotics, giving a drug without a prescription. So all you can do is give it to him, but write down everything you did and why and what happened.
Jerry: During SARS I called (the provincial regulatory body) for some advice about how to handle a situation. I was looking for them to say whether it was okay for me to do something or not. They just refused to say, they just kept saying use your professional judgment, but make sure you document what you did, why you did it, and what the outcome was. This was good advice I think because, really they shouldn't be making the decision for someone else.
As both the SARS crisis and the blackout continued, pharmacists noted how problematic deficiencies in documentation systems became over time:
Karen: I'm glad (the pharmacy I worked in) had a pretty good system of documenting, so that pharmacists from each shift to shift had a way of communicating with each other, passing messages along. Honestly, if we didn't have that, we'd have been sunk. Our (documentation log) was the, what, thread that connected all of us, so we could tell each other what was going on during different times of the day. I used to use this kind of logbook system when I (worked in a hospital pharmacy practice). Without that kind of communication and continuity of care you'd never know what was happening from morning to evening to night.
Kelly: If there was one thing I learned, it was how important it is to have some system to communicate between pharmacists in a store, so that something that happens in the morning, well if you need to leave a message for the evening guys they know what to expect. We didn't have any kind of system like this, and if the phone wasn't working or you couldn't get a message through—we had a lot of problems because of it.
Sarah: I've worked in some pharmacies where they have a really good method for pharmacists to communicate and document with each other, or with the doctors in the building. (During the blackout) the pharmacy I was working in—well, they really had nothing, nothing at all. And that's when problems happen—double doctoring, med errors, all sorts of things because you can't rely on your computer or your memory during something like this.
5. The role of “teamness” in successful adaptation
The literature on team effectiveness has demonstrated the importance of teamwork, particularly in high-stress,22 highly ambiguous situations.23, 24 Characteristics of high-performing teams include role flexibility, fluid boundaries, sense of shared purpose, and lack of rigid hierarchy.24, 25, 26 The value of teamwork in health care has frequently been described in terms of interdisciplinary teams in specific settings, for example, psychiatry,27 geriatrics,24 surgery,28 and emergency medicine.29 Within pharmacy, there is a paucity of literature and evidence regarding the value of “teams” in the community pharmacy setting. Such teams will generally consist of pharmacists, pharmacy technicians, students, and a variety of clerical and support staff.
A key finding of this study suggests that a determinant of successful adaptation to both the SARS and blackout situations was the level of “teamness” that existed before the crisis erupted:
Keith: We always knew we were a good group of people to work with—I mean, well you know how it is when everyone just is able to get along, know what to do, and help out along the way? We were always like that, we always worked together really well. The technicians would know exactly what to do, what they could handle, and then pass it on to the pharmacist next. When (SARS) hit, it really wasn't a big deal for us. We all, well, it was just like another new thing, you know? We were just able to roll with it because everyone pitched in, everyone knew what needed to be done.
Tim: The first thing, well, it was quite good really. One of the technicians was about 3 months pregnant for the first time, and well everyone knew her and knew they'd be trying for a couple of years and all that. So when (SARS) started, the other technicians they figured out how to let (this pregnant technician) take over all the ordering, receiving, and other jobs so she wouldn't have to come into contact with anyone. They just did it on their own, and presented (the management) with their plan and how it would work. They all knew they would need to work harder, work more even just to protect (the pregnant technician).
Sandy: It really comes down to this. If you were working well together before SARS or the blackout or god knows what else will come our way, well then, yeah it's tough and weird and different but you can all figure it out together. Because, I know it's corny, but two heads are better than one, and ten heads are better than two. Everyone was used to working together, we weren't really big on formal roles or who's the boss that kind of stuff—so it made it really easy for everyone to figure out how we were going to handle this situation and make sure things kept moving.
Pharmacies where teamwork was less evident, or where hierarchies and clear lines of authority were more prevalent experienced more difficulty in coping with the challenges introduced by these extraordinary events:
Karen: We always had a system where the pharmacist was in charge. I mean, really in charge, so that everything had to go through the pharmacist—verbal prescriptions, repeats, even simple OTC questions. So when (SARS) hit and the lights went out, no one knew how to do anything different. Everything just kept on piling up on the pharmacist and that's way too much work for one person to handle. They even tried to bring in extra pharmacists to help out, but it was the same problem. Even (the pharmacists who were brought in) kept on referring everything to the pharmacist so it really didn't help. The problem was that no one had any initiative before (SARS) so they sure weren't going to get it while everything was happening.
Paul: It was really too bad for us, because we didn't have a clue what to do. We had so many locums (relief pharmacists) and high school kids working as technicians—the whole setup was bad. When everything started to fall apart there was no give, there was just no ability on anyone's part do anything more—they didn't know how to cope because they never had to before.
Particular features of “teamness” that appeared relevant to successful adaptation in the face of crisis included role flexibility, personal accountability, and lack of rigid hierarchy:
Sarah: I was the pharmacist on shift when the lights went out. It was really weird, because at first you think, okay, it's just a power outage and it'll be okay soon, but then customers start coming in and the whole story was clear. No computer, no radio to find out what's happening in the world. A fridge full of drugs that'll go bad soon. I was so lucky; my technician and my front shop manager, they just handled all the technical stuff so I could concentrate on the customers. They had no more training in how to handle something like this than I did, but we all, well we all just figured out what needed to be done without a lot of yackety-yack, and then we just all did it and checked in with each other to see how everyone was doing. No one was the boss of anyone else, everyone just knew that something bad was happening and we had to get through it all together.
Grace: I wish—well, we should have learned our lesson, you know? We lived through SARS which was such a disaster because no one knew what to do and no one was talking to anyone else and thought that, okay, someone will just tell me what I'm supposed to do, right? Well, that didn't pan out. So when the blackout happened—it was exactly the same. We should have learned that we would have to take care of ourselves, work together, and not rely on some knight in shining armor to come to the rescue. No—no guideline or policy or anything like that—you can't predict what's going to happen. So you have to figure out how to work with each other or you just won't get through it.
5. Limitations
As a qualitative study, this report does not purport to be generalizable to all circumstances or situations; however, as an exploratory examination of an important and complex phenomenon, this study does provide important insights into how pharmacists and pharmacies respond during times of civil disaster, and provides background for future research activities.
The situations reported in this study were somewhat unique, but are representative of different types of commonly occurring civic disasters (eg, infectious disease outbreak and a failure of civilian infrastructure). The participants in this study, however, are not necessarily representative of the general population of pharmacists or pharmacies in Ontario, because they were all volunteers. Self-selection bias may have resulted in a particular type of participant, one who is likely more interested in the topic, more willing to disclose personal anecdotes, and perhaps more interested in “pleasing” the interviewer(s).
Although attempts were made to ensure reliability of data analysis, through double-checking of all interview transcripts and coding, there is still the possibility that such analysis was somewhat skewed toward identifying certain phenomena. Wherever possible, we have attempted to provide extensive excerpts of transcripts, both to confirm the themes we have identified, and to allow the reader to draw his/her own conclusions regarding the experience of pharmacists in Toronto during these extraordinary circumstances. Most importantly, this has given those who lived through the experience and continued to serve on the front lines an opportunity to share their stories to allow others to be prepared.
6. Conclusions
The need for pharmacists and pharmacy services continues and likely increases during times of civic disaster, yet the basic infrastructure necessary to support these services may be severely compromised or nonexistent. The reality of emergencies and disasters, however, is that they are frequently unpredictable and of a scale and magnitude that defies imagination or preplanning. The likelihood of accurately predicting and planning for such emergencies may therefore be very low. Specific emergency policies and procedures may be drafted after-the-fact in light of learned experiences; however, the next emergency may bear no similarity to the previous one, and consequently such policies may be of limited utility, as pointed out by study participants.
All pharmacies and pharmacists must be vigilant and prepared, and expect the unexpected. Beyond such platitudes, however, sober realities exist. First, during times of crisis, pharmacies become more important than ever, and pharmacists begin to assume a variety of duties and responsibilities beyond their traditional scope of practice. Second, normal managerial reporting channels may become inoperable, and pharmacies must expect to have to weather the initial shock of the disaster alone, with limited guidance or direction from above. Finally, and perhaps most importantly, “teamness” (the ability of a group to function cohesively, flexibly, and in an interdependent manner) appears to be an important predictor of successful adaptation to crises.
According to reports from participants in this study, this last point may be of greatest importance. Factors influencing a team's sense of cohesion are myriad, and will differ based on context and experience. Nonetheless, the ability of the team to adapt to unforeseen situations and circumstances appears to be an important determinant of how effectively each individual member of that team will function during times of crisis. Though data from this exploratory study are only preliminary, this is clearly an area for further research.
Sadly, since completion of this research, there have been many more opportunities to examine pharmacists' responses during times of civil crisis. The nature of modern life suggests that, whether urban or rural, such crises will continue to emerge. Further research is required to examine how successful adaptation strategies can become more widespread within the pharmacy community, to ensure the public remains well served even during times of civil crisis.
References
- 1.Gordon J. Rothstein Associates; Brookfield, CT: 2002. Comprehensive Emergency Management for Local Governments: Demystifying Emergency Planning. [Google Scholar]
- 2.United States Department of Health and Human Services Centers for Disease Control and Prevention Public health emergency preparedness and response. http://www.bt.cdc.gov/planning/ Available at: Accessed 11.11.05.
- 3.National Association of Chain Drug Stores Emergency preparedness and counterterrorism. http://www.nacds.org/wmspage.cfm?parm1 = 1795 Available at: Accessed 11.11.05.
- 4.Mileti D. Joseph Henry Press; Washington, DC: 1999. Disasters by Design: A Reassessment of Natural Hazards in the United States. [Google Scholar]
- 5.Center for the Study of Bioterrorism at St. Louis School of Public Health www.slu.edu/colleges/sph/csbei/bioterrorism/index.html Available at: Accessed 11.11.05.
- 6.Seattle and King County Department of Public Health http://www.metrokc/gov/health/bioterrorism/index.htm Available at: Accessed 11.11.05.
- 7.John Hopkins University Center for Civilian Biodefense Studies http://www.fhma.com/bioterror.htm Available at: Accessed 11.11.05.
- 8.Food and Drug Administration information on bioterrorism. http://www.fda.gov/oc/opacom/hottopics/bioterrorism.html Available at: Accessed 11.11.05.
- 9.Food and Drug Administration drug preparedness and response to bioterrorism. http://www.fda.gov/cder/drugprepare/default.htm Available at: Accessed 11.11.05.
- 10.Delehanty R. The emergency nurse and disaster medical assistance teams. J Emerg Nurs. 1999;22:184–186. doi: 10.1016/s0099-1767(96)80103-6. [DOI] [PubMed] [Google Scholar]
- 11.American Society of Health System Pharmacists Homeland security formalizes pharmacist response teams. ASHP Midyear Clinical Meeting News and Views. 2003 (Dec 9):1–3. [Google Scholar]
- 12.Teeter D. Disaster preparedness and pharmacy. US Pharmacist. 2004;29:97–102. [Google Scholar]
- 13.American Society of Health System Pharmacists Emergency Preparedness-Counterterrorism Resource Centre http://ashp.org/emergency/ Available at: Accessed 11.11.05.
- 14.American Pharmacists' Association Pharmacist Resource Center http://www.aphanet.org/pharmcare/ResponseCenter.htm Available at: Accessed 11.11.05.
- 15.Academy of Managed Care Pharmacy Emergency Preparedness Center http://amcp.org/emergency/index.asp Update: Severe Acute Respiratory Syndrome. Available at: Accessed 11.11.05.
- 16.Pedersen C.A., Canaday B.R., Ellis W.M. Pharmacists' opinions regarding level of involvement in emergency preparedness and response. J Am Pharm Assoc (Wash DC) 2003;43:694–701. doi: 10.1331/154434503322642624. [DOI] [PubMed] [Google Scholar]
- 17.United States Department of Health and Human Services Centers for Disease Control and Prevention. MMWR Weekly: Update: Severe Acute Respiratory Syndrome—Toronto, Canada, 2003. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5223a4.htm. Accessed 13.02.05.
- 18.Wysong P. Imaging triage of SARS: Toronto in the crucible. Medscape Radiology. 2003. Available at: http://www.medscape.com/viewarticle/455444. Accessed 13.02.05.
- 19.American Society of Health Systems Pharmacists statement on the role of the health system pharmacist in emergency preparedness, statements on medication therapy and patient care. http://www.ashp.org/bestpractices/MedTherapy/Specific_St_EmergPrep.pdf Available at: Accessed 11.11.05.
- 20.Denzin N.K. 3rd ed. Sage Publications Inc.; Thousand Oaks, CA: 2005. The SAGE Handbook of Qualitative Research. [Google Scholar]
- 21.Chi M. Quantifying qualitative analyses of verbal data: a practical guide. J Learn Sci. 1997;6:271–315. [Google Scholar]
- 22.Kwan D., Barker K., Austin Z. Effectiveness of a faculty development program on interprofessional education: a randomized controlled trial. J Interprof Care. 2006;20:314–316. doi: 10.1080/13561820500518712. [DOI] [PubMed] [Google Scholar]
- 23.Davies H., Nutley S., Mannion R. Organisational culture and quality health care. Qual Health Care. 2000;9:111–119. doi: 10.1136/qhc.9.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. 2005;19(Suppl 1):188–196. doi: 10.1080/13561820500081745. [DOI] [PubMed] [Google Scholar]
- 25.Freeth D., Hammick M., Koppel I. LTSN; London: 2002. A Critical Review of Evaluations of Interprofessional Education. [PubMed] [Google Scholar]
- 26.Lichtenstein R., Alexander J., Jinnett K. Embedded intergroup relations in interdisciplinary teams: effects on perceptions of level of team integration. J Appl Behav Sci. 1997;33:413–435. [Google Scholar]
- 27.Hong G.-Y. Front line care providers' professional worlds: the need for qualitative approaches to cultural interfaces. Forum: Qual Soc Res. 2001;2:1–15. [Google Scholar]
- 28.Irvine R., Kerridge I., McPhee J. Interprofessionalism and ethics: consensus or clash of cultures? J Interprof Care. 2002;16:199–210. doi: 10.1080/13561820220146649. [DOI] [PubMed] [Google Scholar]
- 29.Degeling P., Kennedy J., Hill M. Mediating the cultural boundaries between medicine, nursing, and management: the central challenge in hospital reform. Health Serv Manage Res. 2001;14:36–48. doi: 10.1177/095148480101400105. [DOI] [PubMed] [Google Scholar]


