Summary
Although promotion of safe hygiene is the single most cost-effective means of preventing infectious disease, investment in hygiene is low both in the health and in the water and sanitation sectors. Evidence shows the benefit of improved hygiene, especially for improved handwashing and safe stool disposal. A growing understanding of what drives hygiene behaviour and creative partnerships are providing fresh approaches to change behaviour. However, some important gaps in our knowledge exist. For example, almost no trials of the effectiveness of interventions to improve food hygiene in developing countries are available. We also need to figure out how best to make safe hygiene practices matters of daily routine that are sustained by social norms on a mass scale. Full and active involvement of the health sector in getting safe hygiene to all homes, schools, and institutions will bring major gains to public health.
Introduction
Promotion of hygiene might be the single most cost-effective way of reducing the global burden of infectious disease.1 One might therefore expect hygiene to be the subject of multimillion dollar international initiatives like those for malaria or HIV/AIDS prevention. Perhaps because hygiene does not require clever new technologies or products, or perhaps because it is a domestic and personal issue largely affecting women and children, and perhaps because it concerns the neglected diarrhoeal and respiratory diseases (still the two biggest killers of children), hygiene is still very much overlooked in public health. There are signs that the situation is beginning to improve. Governments and funding agencies increasingly accept that hygiene promotion should play a part in health investments across the wider community, not just in health-care settings. Policy makers are also realising that the health benefits of increased investment in water and sanitation infrastructure are largely delivered through improvements in personal and domestic hygiene.2 Original approaches using new insights are modernising the hygiene sector, making it more attractive to investors.
Improved water supplies and sanitation facilities make it easier to practise hygiene, keeping children and adults safe from infection. But even without improved facilities, better hygiene can still make a huge difference to health. Although most sanitation and water supply programme implementers seek to improve hygiene alongside hardware, they rarely have the resources and professional support needed to do this effectively. Health professionals recognise the need for better hygiene, but too few are actually engaged in programmes to promote it.
In this Review we gather the facts about the importance of hygiene for public health and explore the scale of the problem. We set out what we know about hygiene and assess its promotion in the service of the Millennium Development Goals (MDGs) and beyond. Growing understanding of what shapes hygiene behaviour and creative partnerships are changing the way improvement is being approached. The evidence for giving hygiene a much higher priority is strong, and, to a large extent, we already know what needs to be done. The most important ingredient still missing is the full and active engagement of the health sector in improving global hygiene.
Improvements in hygiene, sanitation, and water can prevent several important infections, in addition to providing other benefits. Among these avoidable infections prevention of diarrhoeal diseases is most important. Because the source of infections is human faecal material, the most important hygiene behaviours are clearly those that keep faecal matter out of the domestic environment. Adequate handwashing after contact with faeces is also crucial (after one's own defecation, after handling the faeces of children, or after contact with a faeces-contaminated environment). Other ways of preventing the faecal–oral transmission of infections include keeping water, foods, and surfaces free of faecal contamination and preventing carriage by flies. Safe food handling and preparation is also important, especially for children, as is the avoidance of animal faeces and the safe storage and use of water.3 Other diseases that can be prevented by adequate hygiene include respiratory infections, trachoma, and skin infections. Endoparasites, such as roundworm and hookworm, and ectoparasites including scabies and fleas, can also be avoided.
Hygiene and health: the evidence
Public health practitioners commonly use information from four sources when weighing up the risk of infectious disease. First, they can assess the biological likelihood that a particular practice will place individuals at risk of infection. Second, they can use risk mapping—for example, modelling of the transfer of microbes between surfaces and hosts in homes and hospitals4 or use of the hazard analysis critical control points method for assessing risk in food preparation.5 However, these approaches depend on access to good estimates of environmental contamination, which are largely unavailable for developing countries. Third, health practitioners can use correlations between recorded practices and disease incidence from observational studies. These data are more readily available, but can be misleading.6 Hygiene behaviour is commonly associated with socioeconomic factors, such as wealth, education, access to water, and modern lifestyle attitudes,7 all of which influence the risk of infectious disease. Such strong socioeconomic confounding is difficult, if not impossible, to address analytically.8
The fourth source of information for public health policy making is randomised controlled trials (RCTs), which control for confounding. However, very few RCTs of hygiene promotion programmes have been undertaken in developing countries, and those that have been done have several methodological flaws. For example, the masking of participants to the intervention is difficult, and as a result, mothers who are grateful for an intervention may be less likely to report disease in their children, leading to inflated effect sizes.9 Bias is thus a serious issue in unblinded studies on diarrhoea.10
Given these caveats, what can we say about the prevention of diarrhoeal disease through hygiene? Table 1 draws together our assessment of the available evidence, from reviews and other key papers, concerning the four sources of information: biological plausibility, risk modelling, observational studies, and RCTs.
Table 1.
Evidence for the ability of specific hygiene practices to prevent diarrhoeal disease
| Specific behaviour | Biological plausibility | Risk modelling | Observational studies | RCTs | |
|---|---|---|---|---|---|
| Handwashing with soap by carers | After own or child's toilet, before eating | Strong | Strong | Large effect | Large effect |
| Safe food handling | Food preparation, storage Weaning food preparation, storage |
Strong Strong |
Strong in developed countries Some |
Inconclusive Inconclusive |
No studies Inconclusive |
| Safe stool disposal | Use of toilets, nappies, potties | Strong | No studies | Large effect | No studies |
| Surface cleansing | Kitchen and toilet cleaning | Plausible | Reasonable in developed countries | Inconclusive | Inconclusive |
| Solid waste disposal | Burning, disposal service | Plausible | Limited | Large effect | No studies |
| Fly control | Insecticiding, trapping | Strong | Some | Large effect | Large effect |
| Removing animal faecal matter | Restricting contact with chicken, pig, cow, buffalo excreta | Plausible | No studies | Large effect | No studies |
RCTs=randomised controlled trials.
The best studied hygiene practice in developing countries is that of handwashing. Evidence from all four types of source is consistent, with RCTs of handwashing interventions showing reductions in diarrhoea of around 30%, and of 43–47% if soap is used.11, 12 Handwashing can also reduce other infections; one review suggested it could reduce respiratory infection by 16%,13 and a more recent cluster-randomised trial in Pakistan reported a reduction in acute lower respiratory tract infections of 50%.14 Handwashing also reduces neonatal mortality,15 trachoma,16 and parasitic worm infections.17 Face or whole-body washing are less well researched but might help to control skin infections and trachoma.18 An unclean face is associated with increased risk of trachoma,19, 20 and a randomised trial suggested that face washing reduces the risk of severe trachoma infection substantially.21 Handwashing with soap mitigated the severe acute respiratory syndrome epidemic22 and is one of the key practices recommended to counter possible influenza pandemics.23
Although food-borne infection is the main route of transmission of gastrointestinal infections in developed countries, their contribution to the burden of diarrhoea in low-income settings is unclear. Hot climates, poor storage facilities, and faecal contamination of the environment all make food-borne infection more likely. Therefore, food-borne infections are likely to play a major part in diarrhoeal disease transmission in low-income settings.24 Microbiological studies have shown the ability of many pathogens to grow quickly in food, especially in hot climates.24, 25 Contaminated weaning food, in particular, has been suggested as a major contributor to diarrhoea in low-income settings,26 although observational studies gave inconclusive results.24
Most of what we assume about food-borne infections in low-income settings is based on expert opinion and biological plausibility, rather than field data (eg, WHO's manual Five Keys to Safer Food).27 Several trials have assessed the effect of promoting exclusive breastfeeding on food-borne infections, with equivocal results.28, 29 Food hygiene interventions have rarely been systematically tested. In one of the very few intervention studies of improving childhood feeding practices, which included some food-hygiene education, Bhandari and colleagues30 found little effect on the nutritional status of children in rural India. The results of a recent trial done in Mali suggested that the microbiological safety of weaning food could be significantly improved with hazard-control principles in homes.31
Other routes of infection that could be removed by better hygiene are related to contact with child7, 32, 33 and animal faeces.34 A meta-analysis of observational studies of hygiene practices associated with child faeces found that failure to remove child faeces and unhygienic handling practices were associated with a 23% increased risk of diarrhoea.35 Other observational studies have reported that animals kept in shared outdoor living spaces (compounds) increase the risk of diarrhoea by over 50%.36, 37, 38 However, no studies that we know of have quantified the risks associated with the use of cow dung for fuel or in house maintenance. So far no intervention trials have aimed to reduce animal faecal contamination in domestic spaces. Neither are there any reports of trials of improving the disposal of child faeces by use of potties, nappies, or child-friendly toilets.
Household surfaces seem to play a major part in disease transmission, although most evidence is from developed countries,39, 40, 41 and few intervention studies have tested whether surface cleansing can reduce transmission in any setting. Larson and colleagues42 in the USA compared use of antibacterial cleaning products with similar products without an antibacterial agent, and found no additional benefit. However, a small study in a school setting suggested that regular cleaning of desks and other classroom surfaces reduces the risk of gastrointestinal illness.43
Epidemiological evidence of the health risk associated with solid-waste disposal in low-income settings is scarce. Observational studies have shown a strong link between environmental exposure to solid waste and diarrhoea,44 perhaps because waste heaps are sometimes used for open defecation and disposal of excreta. In addition to attracting insect vectors and flies, waste is associated with Lassa fever infection which is transmitted by rats.45 In some settings fly control might reduce diarrhoea risk by around 25%,46, 47, 48 and lessen the risk of trachoma.
Because there are multiple routes for the transmission of gastroenteric pathogens, many hygiene intervention studies have targeted several behaviours at once. Such an approach can dilute the effect of the intervention. For example, Haggerty and co-workers49 did a large cluster-randomised trial to test the effect of promoting four different hygiene behaviours (handwashing after faecal contact, handwashing before food contact, disposal of animal faeces, and disposal of child faeces). No effect on diarrhoea was reported in this study, perhaps suggesting that changing four distinct hygiene practices over a short time is unrealistic.
The biological plausibility of most hygiene interventions is high (table 1); there is, however, a major shortage of evidence from trials. Trials on this topic can be complex and the results misleading; it is hard to mask participants to the nature of the intervention, which can lead to bias in outcome reporting. One way to improve this situation is to use more objective outcome measures, such as health-care seeking, assessments by health-care workers masked to intervention status, or mortality. Future hygiene trials need to be larger to model full-scale programme implementation and more intensive (and therefore costly) than previous trials to objectively assess outcomes. Large, adequately funded trials are urgently needed to assess the effects of intervening to improve three key practices in particular: handwashing, safe disposal of child stools, and promotion of food hygiene.
The immediate question is what public health actions should be taken now? Whether an intervention can be recommended for implementation depends not only on the evidence of disease reduction, but also on its scalability, acceptability, and the risk of adverse effects.50 The weight of evidence suggests that hygiene promotion is effective in reducing disease, can be promoted both directly and by mass media programmes with relatively low expenditure per person targeted,1, 51 and has few adverse effects. Even if the true effect on disease in low-income settings is smaller than studies suggest, hygiene improvements will likely have an effect on disease control at large scale. Although additional intervention trials using improved outcome measures are urgently needed to confirm previous findings, hygiene promotion can already be recommended for large-scale implementation.
Hygiene behaviour
While surveys such as multiple indicator cluster surveys and demographic and health surveys systematically collect data on key health indicators, only recently have they begun to include data on hygiene practices. One reason for this is that questionnaire-based surveys are inadequate for gathering data about private and morally bound issues such as food and hand hygiene because they overestimate rates of handwashing, for example, by two to three times.52 Efforts are continuing to identify indicators of hygiene practice that are both valid and simple to collect.53, 54, 55
An article56 published in 2009 collated data about directly observed handwashing in 11 countries, and we identified another survey57 from Bangladesh in 2008 (table 2 ). Handwashing with soap by child carers at key moments, such as after using the toilet, was rare, varying from 3% in Ghana to 42% in Kerala, India. Handwashing with water alone happens on a further 45% of occasions, on average. Handwashing with soap was also rare after cleaning up children and before handling food. If these figures are a good guide, less than one in six children in developing countries is protected from disease by handwashing with soap at key moments. This contributes perhaps a million unnecessary deaths to the global toll.61
Table 2.
Handwashing with soap and water by mother or carer on key occasions56
| N | After toilet (%) | After cleaning child (%) | After cleaning up child stools (%) | Before feeding index child (%) | Before handling food (%) | Handwashing with water only after toilet (%) | |
|---|---|---|---|---|---|---|---|
| Ghana58, 59 | 500 | 3 | 2 | .. | 1 | .. | 39 |
| India, Kerala | 350 | 42 | .. | 25 | .. | .. | .. |
| Madagascar | 40 | 4 | .. | .. | 12 | .. | 10 |
| Kyrgyzstan60 | 65 | 18 | 0 | .. | .. | .. | 49 |
| Senegal | 450 | 23 | 18 | .. | .. | 18 | .. |
| Peru | 500 | 14 | .. | .. | 6 | .. | .. |
| Bangladesh57 | 1000 | 19 | 26 | 1 | 1 | 60 | |
| China, Sichuan | 78 | 13 | .. | 16 | 6 | .. | 87 |
| China, Shaanxi | 64 | 12 | .. | .. | 16 | .. | 14 |
| Tanzania | 30 | 13 | 13 | 13 | 4 | .. | 33 |
| Uganda | 500 | 14 | 19 | 11 | 6 | 8 | 44 |
| Vietnam | 720 | .. | 14 | 23 | 5 | .. | 51 |
| Kenya | 802 | 29 | 35 | 38 | 13 | 15 | 57 |
| Average | .. | 17 | 11 | 25 | 3 | 5 | 51 |
Data from reference 56, unless otherwise stated.
Handwashing behaviour is far from ideal in developed countries. In a motorway service station in the south of England, just 65% of women and 31% of men washed their hands with soap after using the toilet facilities,62 and a study in the north of England recorded that just 43% of mothers washed their hands with soap after changing a dirty nappy.63 A survey by Judah and co-workers64 reported that 28% of commuters in five UK cities had bacteria of faecal origin on their hands.
If improvement of hygiene practices, such as handwashing with soap, has the potential to be one of the most cost-effective ways in which public health can be improved in developing countries, how should we go about it? Though changing behaviour is difficult, we know a lot more about hygiene behaviour than we did 10 years ago and promising approaches to changing hygiene on a large scale are emerging.
Risky hygiene behaviours persist around the world because of a web of factors that can be hard to shift. Poor environmental conditions, such as lack of water, sanitation, and drainage, have a role. Other obstacles include the absence of hard surfaces that can easily be kept clean, unavailability of cleaning materials such as soap and surface cleansers, and limited access to hygiene aids, such as potties or nappies. Local social structures and cultural norms, as well as individual psychological factors, also help to keep present practices locked in place. For behaviour to change one, or several, of these factors will have to be addressed, but to do so will require a better understanding of them. Several formative research studies that aimed to provide an understanding to enable the design of effective handwash programmes have investigated the behavioural aspects of hygiene.65, 66, 67
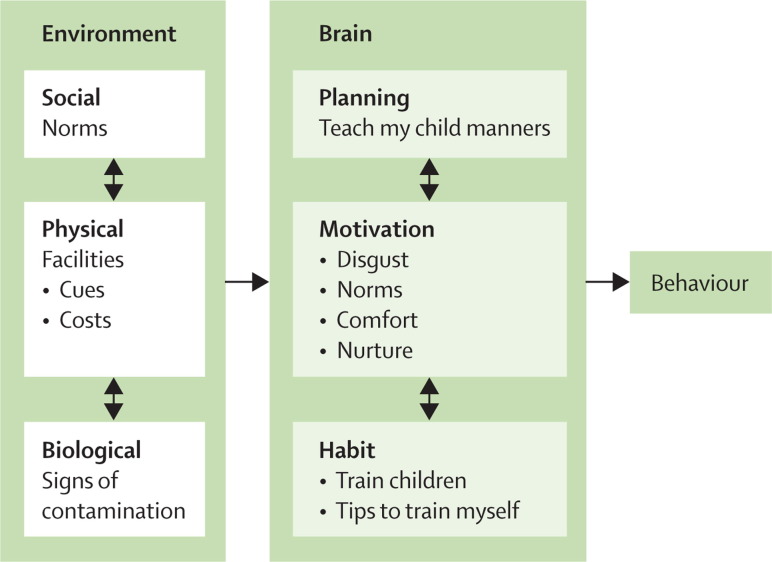
A review of 11 studies done in Africa, Asia, and Latin America concluded that, although there are local differences, common patterns exist. Three kinds of hygiene behaviour were identified: habitual, motivated, and planned.56 Hygiene habits were learnt at an early age, but soap use was rarely taught by parents or schools. Key motivations for handwashing were disgust of contamination on hands and to do what everyone else was perceived to be doing (social norms). Other motivations included comfort and nurturance (the desire to care for one's children). Planned handwashing, with the aim of preventing disease, took place rarely. Mothers did not find the threat of diarrhoeal disease particularly relevant and found the connection between handwashing and possible diarrhoea in children tenuous. Mothers did, however, plan to teach their children good manners, and they also planned to economise by ensuring that soap was not wasted. Aunger and colleagues68 observed that habit was the most powerful determinant of handwashing in Kenya, followed by several motives including disgust, and social norms, and cognitive plans to save money. An investigation into nurses' handwashing in Australia saw evidence of a similar distinction between planned and motivated or habitual handwashing behaviour.69 A study of routine behaviour and hygiene in rural India suggested that some handwashing behaviours are deeply embedded in daily routines and hence highly habitual, whereas others are motivated by the transient disgust or discomfort of having dirty hands.70
The psychological factors determining hygiene are related to factors in the environment. For example, when local social norms are the source of poor handwashing habits people commonly practise what they perceive everyone else to be doing, which reinforces the norm of not using soap. Lack of water and a perception that soap is too expensive for handwashing could also constrain handwashing (though this might be post-rationalisation because one review suggested that soap was present in 97% of all households in a review, but it was used mainly for clothes, body, and dish washing).56 Finally, fear of epidemics such as cholera or severe acute respiratory syndrome (but not of endemic diarrhoeas that cause far more deaths) could also lead to improved hygiene.56
Although an understanding of the determinants of handwashing behaviour is helpful, how such insight can be used in behaviour change programmes is not always obvious. The figure summarises the psychological and environmental factors that are likely to determine hygiene behaviour.56 If much handwashing is habitual, then the cues that trigger these habits need to be found and the habits established at an early age. Environmental changes that make handwashing easier and cheaper, such as the introduction of simple water-saving technologies (eg, so-called tippy taps), could be helpful (although how their use could become widespread is unclear), as could information suggesting that handwashing with soap is a desirable social norm where it is not one.
Figure.
Hypotheses about the most effective ways of changing handwashing behaviour
Some of these hypotheses have already been tested. An experimental study71 in Australia recently reported that promoting disgust led to increased handwashing in a public toilet, as it did in a service station intervention in the UK.62 A national handwash programme in Ghana that used disgust and nurture to motivate handwashing increased self-reported handwashing before eating by 41% and after defecation by 13%.51 Disgust was also used humorously in an urban social marketing programme in Burkina Faso. The project increased observed handwashing with soap by mothers from 1% to 17% after using the toilet and from 13% to 31% after cleaning up a child (panel 1 ).72 A norms-based message, “Is the person next to you washing with soap?”, worked best to encourage handwashing in a motorway service station in the south of England.62 Other promising approaches, such as trying to establish hygiene habits in schools, are thought to be effective. Unpublished evidence from Kenya, Peru, and Uganda suggests that working through schools might have a double advantage: children take up what they are taught and might also take messages home, hence influencing their families.
Panel 1. Programme Saniya in Burkina Faso.
Programme Saniya aimed to improve handwashing and stool disposal behaviour in the town of Bobo-Dioulasso in Burkina Faso. Based on principles of social marketing, including use of existing respected in-depth research, the programme was tailored to local customs and targeted specific types of behaviour, built on existing motivations for hygiene (social and aesthetic rather than health-based), and used locally appropriate channels of communication, including neighbourhood committees, street theatre, schools, and local radio. After the programme had run for 3 years, three-quarters of the mothers targeted had been involved with programme activities and half could cite the two main messages of the programme correctly. Although the safe disposal of children's stools changed little between 1995 and 1998 (80% before intervention and 84% after), handwashing with soap after cleaning a child's bottom rose from 13% to 31%. The proportion of mothers who washed their hands with soap after using the latrine increased from 1% to 17%.2 The estimated household and societal cost savings associated with the programme far outweighed its costs.4
The standard approach to hygiene promotion, whether through schools, clinics, or health outreach programmes, has, until recently, been educational. However, knowledge about possible long-term health effects does not necessarily translate into practice. There is little proof that such educational approaches are effective, either in developing,73, 74 or developed countries.75 In the past two decades an approach known as PHAST (participatory hygiene and sanitation transformation) has become the predominant model among non-government organisations. Although it is an imaginative attempt to involve communities in solving their own hygiene problems, PHAST is mostly an educational approach, is heavily reliant on the skills of trained facilitators, and is difficult to implement on a large scale. There are no rigorously collected data to support the effectiveness of PHAST programmes, and some evidence from Tanzania and Uganda indicates that the approach has limited effect on hygiene behaviour. Community health clubs were successful and cost effective in promoting sanitation and hygiene in two districts of Zimbabwe (panel 2 ),76 largely because communal activities can change local norms.
Panel 2. Community health clubs in Zimbabwe.
The innovative method of community health clubs used in Zimbabwe significantly changed hygiene behaviour and built rural demand for sanitation.76 Villagers were invited to a series of weekly sessions where one health topic was debated and then action plans formulated. These proved highly popular with mothers. In 1 year in Makoni District, 1244 health sessions were held by 14 trainers, costing an average of US$0·21 per beneficiary and involving 11 450 club members. In Tsholotsho District, 2105 members participated in 182 health promotion sessions held by three trainers which cost $0·55 for each beneficiary. Club members' hygiene was significantly different (p<0·0001) from a control group regarding 17 key hygiene practices including toilet building and handwashing. The authors of the study concluded that if a strong community structure is developed and the norms of a community are altered, sanitation and hygiene behaviour are likely to improve.76
Many programmes promote hygiene in schools. Although evidence of effect is scarce, data from a water-treatment and handwashing intervention in Kenya and an intensive handwashing educational programme in Chinese primary schools showed a reduction in absenteeism.77, 78 The biggest obstacle to school hygiene might be the shortage of facilities; for example, studies in Kenya and Senegal showed that only 5–10% of schools had soap available for children to use.79
Although all of these programmes might have helped to improve hygiene behaviour in their target communities, proven approaches to hygiene promotion that are effective on the large scale and that will help meet the Millennium Development Goals for child survival are needed. The most promising approach is that developed by the Global Public–Private Partnership for Handwashing with Soap (panel 3 ).
Panel 3. The Global Public–Private Partnership for Handwashing with Soap.
Conceived as a way of combining the expertise and resources of the private and public sectors, the Global Public–Private Partnership for Handwashing with Soap (PPP-HW) has been building coalitions and national programmes in over 17 developing countries. Usually based out of ministries of health, the programmes aim to work at national scale. The use of formative research to investigate the determinants of handwashing behaviour,1 use of professional creative agencies to design coherent, attractive, and outstanding national communications strategies with advice from industrial marketers, and attempts to evaluate programmes rigorously are also key features. Good preliminary results were achieved after 1 year of programme activities in Ghana and the model is convincing and innovative enough to have attracted substantial funds, but questions about effectiveness remain.
In Ghana, Peru, and Senegal public health authorities and soap companies were not always easy bedfellows, and national partnerships can be hard to sustain for longer than just one campaign. Partnerships require constant attention from a full-time coordinator skilled in reconciling public and private stakeholders. Coordinators must be able to secure commitment for the approach at the highest levels and keep the vision alive through constant change of personnel in both sectors (for example, from 2003 to 2009: Peru had six ministers of health).
It is a key objective of these partnerships to gather rigorous public domain evidence about the effectiveness of large-scale handwashing promotion efforts. However, gathering such data is proving challenging, especially when interventions cannot be centrally controlled because they depend on the goodwill of various partners.
For the future, some of the most promising initiatives arising from the PPP-HW's work are coming from the soap companies themselves. Unilever, for example, has made handwashing part of the social mission of the Lifebuoy brand and has pledged to bring handwashing to one billion people by 2012. Procter & Gamble and its Safeguard brand has reached 35 million children with one-on-one, school-based handwashing education and is planning to reach 100 million more by 2012.8 Colgate runs a “Clean Hands–Good Health” campaign in many countries to promote proper handwashing practices among school children with developmentally appropriate materials and a classroom curriculum. Local soap companies such as GeTrade in Ghana are also contributing their efforts. If promoting hygiene in emerging markets makes good business sense to private companies, because they can improve sales and enhance their reputations, this could lead to sustained long-term improvements in public health, as it has in developed countries.9
Policy issues—what the health sector needs to do
Far more is known about hygiene now than a decade ago. We understand the need to invest in hygiene and the key practices that require change, and we have appealing new ways of promoting hygiene. If hygiene promotion is truly the most cost-effective intervention for preventing disease in developing countries,1 then it is extraordinary that hygiene features so seldom in international public health efforts. What then holds back major investment in the improvement of hygiene?
The health sector needs to address four major challenges for hygiene to take its rightful place as a major issue within global public health. First, governments and ministries have to stop merely talking about the need for hygiene and instead act, investing in programmes that can actually change hygiene behaviour in villages and towns where children are dying from neglected diseases. Second, hygiene promotion has to figure in the job description for health agents, from the heads of health services to the most remote rural community health worker. Third, massive efforts need to be made to train health workers in the skills of hygiene promotion. This is important because otherwise they will continue to use outdated methods and health education approaches that are demotivating because they are ineffective. Fourth, although we know enough to act now, gaps in our knowledge exist. Health research funders need to make up for some of the decades of underinvestment in hygiene. Support is needed for the research that will allow us to say with more certainty how to change hygiene behaviour on a large scale, what improved hygiene will cost, and what the financial returns will be.
There are encouraging signs that, although investment still remains low, the topic of hygiene is moving up the political agenda. As pointed out by the former director of the World Bank Jim Wolfenson, hygiene is no longer seen as a joke. Inspired advocacy events, such as the Global Handwashing Day organised by the Global PPP-HW, have enhanced the global profile of hygiene. Celebrated every year on October 15, the day involves imaginative high-profile activities organised by public and private players from around the world. To become the focus of real investment, rather than good intentions, hygiene needs champions at all levels: from global, right through to village, and especially national ministries of health. Hygiene needs to find a place in national health plans and in poverty reduction strategies. Donors need to actively solicit hygiene promotion programmes and bring companies interested in promoting hygiene into the public health fold, rather than treating them with suspicion, as is sometimes the case.
Coordination is a key issue in hygiene improvement; each country needs to designate a focal point to provide effective management of diverse efforts. Greater impact could be achieved if the many agencies, donors, non-governmental organisations, companies, and government and citizen institutions with hygiene in their mandates could agree upon a few simple principles and harmonise their approaches. Every mother who has contact with a health worker during pregnancy or in the neonatal period needs to learn about the importance of hygiene, and handwashing in particular. Similarly, every family member who prepares food needs to know a few basic rules of food hygiene. If the coordination of outreach to the community is seen as crucial to efforts to combat HIV and malaria, the same should also be true for hygiene promotion.
In increasingly decentralised countries, policy building work needs to take place at national, regional, and provincial level. Creating this framework is challenging given competition for attention in the relevant ministries, their limited human and logistic resources, and shortage of skills. These problems are often worst in the remote and poverty-stricken areas that would benefit most from improved hygiene. Global leaders need to get involved to help show that hygiene is not a dirty contaminated topic, but one that can be attractive and popular, increasing votes, attention, and resources.
For action on hygiene to become part of the remit of health workers, greatly increased investment in the development of capacity is needed. Training in up-to-date methods of communication is lacking at all levels in health ministries. Tertiary institutions that can provide this training need training themselves, and this is an area that could be addressed by external funders; although for some reason funding such skills development has, unfortunately, not been a priority for donors in recent years. Marketing expertise from the private sector has been helping to fill the skills gap, by designing state-of-the-art hygiene communication programmes and helping to train health officials in the techniques of marketing. Links between government health bodies and private organisations could be developed on a wider and more formal basis. The interface between programmes and health research is also problematic, as it is for health development in general. Local universities are the obvious institutions for designing and evaluating hygiene promotion programmes, but very few have that capacity at present.
Another question for policy makers is whether hygiene should be promoted alone or in concert with efforts to improve water and sanitation infrastructure. The introduction of a new water supply to a community is a perfect opportunity to raise the issue of hygiene. However, large-scale engineering programmes are rarely equipped to handle what they call the software (ie, the behavioural) side of development. Equally, the most effective use of a hygiene budget might be to cover larger areas by use of mass media, rather than to restrict efforts to villages in the process of acquiring new water facilities. Hygiene messages should always be integral to efforts promoting improved sanitation. Ministries of health can play a part by insisting that it is not acceptable to build toilets in schools, health facilities, workplaces, and homes without appropriate handwashing facilities.
Finally, good professional practice requires continual advancement in a feedback loop of learning and knowledge development whilst doing. Much can be done now. Far more could be done with serious investment to fill some of the important knowledge gaps about hygiene that still remain. Panel 4 sets out crucial questions that need answering urgently if we are to be able to deliver better hygiene programming in the future.
Panel 4. Research priorities.
Trials of interventions to change key hygiene practices
Randomised controlled trials are needed to test interventions to improve hygiene practices, including handwashing, safe stool disposal and food hygiene. Such studies should use objective outcomes such as clinical infection or mortality.
Testing of hygiene interventions
Small-scale testing of approaches in a laboratory or community setting, as well as large-scale screening, can provide answers about what works best to change hygiene behaviour and assurance of effectiveness before interventions are rolled out at a large scale.
The effectiveness, cost-effectiveness, and differential impact of different channels?
An analysis of the different routes of communication used in the Ghana PPP-HW campaign suggested that TV and radio had greater reach and impact than community events. Further analytical studies into the effectiveness and cost-effectiveness of different channels of communication are needed. We need to know more about the differential impact of different approaches on the low-income sections of society, which are at greatest risk of death from diarrhoeal disease and have fewer resources to commit to hygiene.80 We also need data to calculate dose-response curves: how much intervention produces how much behaviour change, and hence what level of investment is most cost effective?
Designing effective interventions
The process of turning insight about behaviour into effective behaviour-changing communication is still more of an art than a science. More needs to be understood about what makes communications attention-grabbing and memorable, as well as motivating. Habit clearly has an important role in hygiene and many other health behaviours, but the topic of how to create and change habits has been little studied.6, 7
Methods and models for hygiene promotion at different scales
Proven model approaches to hygiene promotion are badly needed by decentralised authorities and non-government organisations. Such agencies are often willing to implement hygiene promotion, but rarely have the specific expertise or capacity to develop the approaches themselves. Several examples of simple, effective, attractive, and costed activities and materials that have been tested and have been shown to work, are needed so that organisations can adapt these to local circumstances.
Sustaining improvements
Even when we are successful in changing hygiene behaviours we still do not know how persistent such changes are,11, 12 or the sort of investment that is needed to maintain the gains in a given population. Perhaps the most important tasks facing hygiene promoters and soap manufacturers are to work out how to make hygiene a matter of habit and a social norm. Once hygiene is established, improvements in behaviours will be truly sustainable.
Measuring hygiene behaviour
If we cannot accurately measure changes in hygiene behaviour we cannot measure the effectiveness of interventions in trials or evaluate the delivery of behaviour change in programmes. Because hygiene behaviour is private and morally loaded, simple questionnaire surveys give overestimates of behaviours such as handwashing, whereas direct observation is cumbersome and intrusive, and technological fixes, such as Smart Soap (containing accelerometers that record usage) have drawbacks too.14 Simple, cheap, and widely applicable methods of measuring hygiene behaviour change are still needed.
Technological, consumer, and business model innovation
Although simple technologies, such as water-saving taps, nappies, potties, and child-friendly toilets, can help families to live more hygienically, little effort has been made to develop and market hygiene-helping products that are appropriate for the consumers with low income. Three things are needed: exploration of the design space for the products that the poorest consumers need and want,16 the adaptation or creation of technologies, products, and services that meet those needs, and the development of business models that can operate profitably and be sustained on a large scale.
Hygiene: a roadmap to success
Though the evidence base is far from complete, the information we do have strongly suggests a need to improve handwashing behaviour, stool disposal practices, and food hygiene in particular when weaning. We know that hygiene can be promoted successfully through conventional health channels, water and sanitation initiatives, schools, and by commercial companies.
The first priority for any new resources allocated to hygiene is the design, management, and rigorous evaluation of large-scale hygiene promotion programmes (using randomised trials, where possible).
Second, we need more medium-scale programmes, operating at rural or urban district level. Such programmes provide the opportunity to learn more of the basics of hygiene promotion, how to turn insight about hygiene into effective promotional campaigns, how to invest to get the most behavioural change, which channels to use, how best to reach the most vulnerable, how often and how much to intervene and how to sustain behavioural changes. The capacity to implement medium-scale programmes needs to be built through learning by doing. Programmes of research led by local universities, with international support where needed, can begin to tackle these multiple issues. Because there are many different ways to promote hygiene, having more diverse and properly evaluated programmes will build a body of knowledge as to what works best in changing these persistent habitual behaviours.
Third, we need more dedicated epidemiological research funded by international donors and research councils. Many RCTs investigating efficacy and effectiveness are needed to provide rigorous evidence of the importance of improving individual hygiene practices. Food hygiene has the best claim to be tackled first, but all of the hygiene practices we have discussed have been neglected relative to the efforts for malaria or HIV research. For example, there is no evidence to indicate whether the practice of using animal dung to smooth floors and walls (common in Asia) is injurious to family health.
Fourth, we need to set new and more ambitious targets for the coming decades. It is unacceptable that, in the 21st century, most schools in developing countries still do not have sanitation and hygiene facilities, or that health centres, hospitals, maternity facilities, workplaces, and public institutions still cannot offer water and soap to their users. It is unacceptable that birth attendants and outreach workers are not always trained to wash hands with soap and do not systematically promote handwashing and hygiene to mothers. Handwashing and hygiene should be promoted at least as aggressively as vaccination. For the future every child should have the right to live in a household that is protected from disease by good hygiene.
In the next 5–10 years we have a window of opportunity to develop the high impact programmes which will bring about mass scale changes. If these programmes are successful in leading the members of all societies to adopt hygienic habits as a matter of course, then hygiene will be able to take its rightful place as one of the foundation stones of global health.
Search strategy and selection criteria
We searched Medline, from 1970 to 2009, regardless of language, using the search terms “[diarrh(o)ea AND hygiene]”, “[respiratory AND hygiene]”, “[food AND hygiene]”, “[pneumonia AND hygiene]”, “[stool AND disposal]”, “[waste AND hygiene]”, and “[animal faeces AND diarrh(o)ea]”. We searched the reference lists of relevant articles and contacted authors and experts for further identification of articles. Table 1 draws together our assessment of the available evidence from available reviews (and other key papers) concerning the four sources of evidence, biological plausibility, risk modelling, observational studies, and randomised controlled trials.
Acknowledgments
Acknowledgments
Thanks to: Robert Aunger, Jamie Bartram, Sandy Cairncross, Richard Carter, Lisa Danquah, Therese Dooley, Matt Freeman, Rhona MacDonald, Claudio Lanata, Rick Rheingans, Beth Scott, and several anonymous reviewers.
Contributors
VC wrote the first draft and subsequent drafts, revised and finalised the paper. SL made substantial contributions to the content and conclusions of the paper, reviewing and finalising. WS made contributions to the content, reviewing and finalising. RF made contributions to the content, especially concerning policy issues. OT made contributions to the content in the food hygiene section. AB made contributions to the structure of the paper.
Conflicts of interest
VC has received a research grant from Unilever, has been a consultant in a think tank on hygiene for Kimberly Clark, and has been a consultant for a hygiene resource for health workers at Colgate Palmolive. AB has receiveda grant from Unilever to evaluate a hygiene intervention. RF, SL, WS, and OT declare that they have no conflicts of interest.
References
- 1.Jamieson D, Bremen J, Measham A, Alleyne G, Claeson M. Disease control priorities in developing countries. Oxford University Press; Oxford: 2006. [PubMed] [Google Scholar]
- 2.Cairncross S, Valdmanis V. Water supply, sanitation and hygiene promotion. In: Jamison D, Breman J, Measham A, editors. Disease control priorities in developing countries. 2nd edn. The World Bank; Washington, DC: 2006. pp. 771–792. [Google Scholar]
- 3.Curtis VA, Cairncross S, Yonli R. Domestic hygiene and diarrhoea, pinpointing the problem. Trop Med Int Health. 2000;5:22–32. doi: 10.1046/j.1365-3156.2000.00512.x. [DOI] [PubMed] [Google Scholar]
- 4.Haas C, Rose J, Gerba C, editors. Quantitative microbial risk assessment. John Wiley and Sons; San Francisco: 1999. [Google Scholar]
- 5.Ehiri JE, Azubuike MC, Ubbaonu CN, Anyanwu EC, Ibe KM, Ogbonna MO. Critical control points of complementary food preparation and handling in eastern Nigeria. Bull World Health Organ. 2001;79:423–433. [PMC free article] [PubMed] [Google Scholar]
- 6.Blum D, Feachem RG. Measuring the impact of water supply and sanitation investments on diarrhoeal diseases: problems of methodology. IntJ Epidemiol. 1983;12:357–365. doi: 10.1093/ije/12.3.357. [DOI] [PubMed] [Google Scholar]
- 7.Curtis V, Kanki B, Mertens T. Potties, pits and pipes: explaining hygiene behaviour in Burkina Faso. Soc Sci Med. 1995;41:383–393. doi: 10.1016/0277-9536(94)00341-p. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 9.Wood L, Egger M, Gluud LL. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt W, Cairncross S. Household water treatment in poor populations: is there enough evidence for scaling up now? Environ Sci Technol. 2009;43:986–992. doi: 10.1021/es802232w. [DOI] [PubMed] [Google Scholar]
- 11.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3:275–281. doi: 10.1016/s1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 12.Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev. 2008;1 doi: 10.1002/14651858.CD004265.pub2. CD004265. [DOI] [PubMed] [Google Scholar]
- 13.Rabie T, Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health. 2006;11:258–267. doi: 10.1111/j.1365-3156.2006.01568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luby SP, Agboatwalla M, Feikin DR. Effect of handwashing on child health: a randomised controlled trial. Lancet. 2005;366:225–233. doi: 10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]
- 15.Rhee V, Mullany L, Khatry S, Katz J. Maternal and birth attendant hand washing and neonatal mortality in southern Nepal. Arch Pediatr Adolesc Med. 2008;162:603–608. doi: 10.1001/archpedi.162.7.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emerson PM, Cairncross S, Bailey RL, Mabey DCW. A review of the evidence for the ‘F’ and ‘E’ components of the SAFE strategy for trachoma control. Trop Med Int Health. 2000;5:515–527. doi: 10.1046/j.1365-3156.2000.00603.x. [DOI] [PubMed] [Google Scholar]
- 17.Fung IH, Cairncross S. Ascariasis and handwashing. Trans RSoc Trop Med Hyg. 2009;103:215–222. doi: 10.1016/j.trstmh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Ngondi J, Gebre T, Shargie E. Evaluation of three years of the SAFE strategy (Surgery, Antibiotics, Facial cleanliness and Environmental improvement) for trachoma control in five districts of Ethiopia hyperendemic for trachoma. Trans R Soc Trop Med Hyg. 2009;10:1001–1010. doi: 10.1016/j.trstmh.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 19.Schemann JF, Sacko D, Malvy D. Risk factors for trachoma in Mali. Int J Epidemiol. 2002;31:194–201. doi: 10.1093/ije/31.1.194. [DOI] [PubMed] [Google Scholar]
- 20.Emerson PM, Bailey RL, Mahdi OS, Walraven GE, Lindsay SW. Transmission ecology of the fly Musca sorbens, a putative vector of trachoma. Trans R Soc Trop Med Hyg. 2000;94:28–32. doi: 10.1016/s0035-9203(00)90427-9. [DOI] [PubMed] [Google Scholar]
- 21.West SK, Munoz B, Lynch M. Impact of face-washing on trachoma in Kongwa, Tanzania. Lancet. 1995;345:155–158. doi: 10.1016/s0140-6736(95)90167-1. [DOI] [PubMed] [Google Scholar]
- 22.Fung ICH, Cairncross S. Effectiveness of handwashing in preventing SARS: a review. Trop Med Int Health. 2006;11:1749–1758. doi: 10.1111/j.1365-3156.2006.01734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jefferson T, Foxlee R, Mar CD. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2008;336:77–80. doi: 10.1136/bmj.39393.510347.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lanata CF. Studies of food hygiene and diarrhoeal disease. Int J Environ Health Res. 2003;13:S175–S183. doi: 10.1080/0960312031000102921. [DOI] [PubMed] [Google Scholar]
- 25.Islam MS, Hasan MK, Khani SI. Growth and survival of Shigella flexneri in common Bangladeshi foods under various conditions of time and temperature. Appl Environ Microbiol. 1993;59:652–654. doi: 10.1128/aem.59.2.652-654.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Motarjemi Y, Kaferstein F, Moy G, Quevedo F. Contaminated weaning food: a major risk factor for diarrhoea and associated malnutrition. Bull World Health Organ. 1993;71:79–92. [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization Prevention of Foodborne Disease: Five Keys to Safer Food. http://wwwwhoint/foodsafety/consumer/5keys/en (accessed Jan 10, 2009).
- 28.Bolam A, Manandhar DS, Shrestha P, Ellis M, Costello AM. The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised controlled trial. BMJ. 1998;316:805–811. doi: 10.1136/bmj.316.7134.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jakobsen MS, Sodemann M, Biai S, Nielsen J, Aaby P. Promotion of exclusive breastfeeding is not likely to be cost effective in West Africa. A randomized intervention study from Guinea-Bissau. Acta Paediatr. 2008;97:68–75. doi: 10.1111/j.1651-2227.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- 30.Bhandari N, Mazumder S, Bahl R, Martines J, Black RE, Bhan MK. An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. J Nutr. 2004;134:2342–2348. doi: 10.1093/jn/134.9.2342. [DOI] [PubMed] [Google Scholar]
- 31.Touré O. Implementation of the Hazard Analysis Critical Control Points (HACCP) method to improve microbiological food safety in peri-urban Mali. PhD thesis. London School of Hygiene and Topical Medicine; 2009. p. 105. [Google Scholar]
- 32.Huttly SR, Lanata CF, Yeager BA, Fukumoto M, del Aguila R, Kendall C. Feces, flies, and fetor: findings from a Peruvian shantytown. Rev Panam Salud Publica. 1998;4:75–79. doi: 10.1590/s1020-49891998000800001. [DOI] [PubMed] [Google Scholar]
- 33.Yeager BA, Huttly SR, Bartolini R, Rojas M, Lanata CF. Defecation practices of young children in a Peruvian shanty town. Soc Sci Med. 1999;49:531–541. doi: 10.1016/s0277-9536(99)00119-7. [DOI] [PubMed] [Google Scholar]
- 34.Black RE, de Romana G Lopez, Brown KH, Bravo N, Bazalar OG, Kanashiro HC. Incidence and etiology of infantile diarrhea and major routes of transmission in Huascar, Peru. Am J Epidemiol. 1989;129:785–799. doi: 10.1093/oxfordjournals.aje.a115193. [DOI] [PubMed] [Google Scholar]
- 35.Gil A, Lanata C, Kleinau E, Penny M. Children's feces disposal practices in developing countries and interventions to prevent diarrheal diseases. A literature review. Instituto de Investigacion Nutricional (Peru); Washington, DC: 2004. [Google Scholar]
- 36.Bukenya GB, Nwokolo N. Compound hygiene, presence of standpipe and the risk of childhood diarrhoea in an urban settlement of Papua New Guinea. Int J Epidemiol. 1991;20:534–539. doi: 10.1093/ije/20.2.534. [DOI] [PubMed] [Google Scholar]
- 37.Grados O, Bravo N, Black RE, Butzler JP. Paediatric campylobacter diarrhoea from household exposure to live chickens in Lima, Peru. Bull World Health Organ. 1988;66:369–374. [PMC free article] [PubMed] [Google Scholar]
- 38.Huttly SR, Blum D, Kirkwood BR, Emeh RN, Feachem RG. The epidemiology of acute diarrhoea in a rural community in Imo State, Nigeria. Trans R Soc Trop Med Hyg. 1987;81:865–870. doi: 10.1016/0035-9203(87)90055-1. [DOI] [PubMed] [Google Scholar]
- 39.Barker J, Bloomfield SF. Survival of Salmonella in bathrooms and toilets following salmonellosis. J Appl Microbiol. 2000;89:137–144. doi: 10.1046/j.1365-2672.2000.01091.x. [DOI] [PubMed] [Google Scholar]
- 40.Cozad A, Jones R. Disinfection and the prevention of infectious disease. Am J Infect Control. 2003;31:243–254. doi: 10.1067/mic.2003.49. [DOI] [PubMed] [Google Scholar]
- 41.Cogan TA, Slader J, Bloomfield SF, Humphrey TJ. Achieving hygiene in the domestic kitchen: the effectiveness of commonly used cleaning procedures. J Appl Microbiol. 2002;92:885–892. doi: 10.1046/j.1365-2672.2002.01598.x. [DOI] [PubMed] [Google Scholar]
- 42.Larson EL, Lin SX, Gomez-Pichardo C, Della-Latta P. Effect of antibacterial home cleaning and handwashing products on infectious disease symptoms: a randomized, double-blind trial. Ann Intern Med. 2004;140:321–329. doi: 10.7326/0003-4819-140-5-200403020-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sandora TJ, Shih MC, Goldmann DA. Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatrics. 2008;121:e1555–e1562. doi: 10.1542/peds.2007-2597. [DOI] [PubMed] [Google Scholar]
- 44.Rego RF, Barreto ML, Santos R, de Oliveira NF, Oliveira S. Rubbish index and diarrhoea in Salvador, Brazil. Trans R Soc Trop Med Hyg. 2007;101:722–729. doi: 10.1016/j.trstmh.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 45.Bonner PC, Schmidt WP, Belmain SR, Oshin B, Baglole D, Borchert M. Poor housing quality increases risk of rodent infestation and Lassa fever in refugee camps of Sierra Leone. Am J Trop Med Hyg. 2007;77:169–175. [PubMed] [Google Scholar]
- 46.Chavasse DC, Shier RP, Murphy OA, Huttly SR, Cousens SN, Akhtar T. Impact of fly control on childhood diarrhoea in Pakistan: community-randomised trial. Lancet. 1999;353:22–25. doi: 10.1016/s0140-6736(98)03366-2. [DOI] [PubMed] [Google Scholar]
- 47.Emerson PM, Bailey RL. Trachoma and fly control. J Comm Eye Health. 1999;12:57. [PMC free article] [PubMed] [Google Scholar]
- 48.Emerson PM, Lindsay SW, Walraven GE. Effect of fly control on trachoma and diarrhoea. Lancet. 1999;353:1401–1403. doi: 10.1016/S0140-6736(98)09158-2. [DOI] [PubMed] [Google Scholar]
- 49.Haggerty PA, Muladi K, Kirkwood BR, Ashworth A, Manunebo M. Community-based hygiene education to reduce diarrhoeal disease in rural Zaire: impact of the intervention on diarrhoeal morbidity. Int J Epidemiol. 1994;23:1050–1059. doi: 10.1093/ije/23.5.1050. [DOI] [PubMed] [Google Scholar]
- 50.Ross DA, Wight D, Dowsett G, Buve A, Obasi AI. The weight of evidence: a method for assessing the strength of evidence on the effectiveness of HIV prevention interventions among young people. World Health Organ Tech Rep Ser. 2006;938:79–102. discussion 317–41. [PubMed] [Google Scholar]
- 51.Scott B, Schmidt W, Aunger R, Garbrah-Aidoo N, Animashaun R. Marketing hygiene behaviours: the impact of different communications channels on reported handwashing behaviour of women in Ghana. Health Educ Res. 2007;22:225–233. doi: 10.1093/her/cym056. [DOI] [PubMed] [Google Scholar]
- 52.Curtis V, Cousens S, Mertens T, Traoré E, Kanki B, Diallo I. Structured observations of hygiene behaviours in Burkina Faso, validity, variability and utility. Bull World Health Organ. 1993;71:23–32. [PMC free article] [PubMed] [Google Scholar]
- 53.Biran A, Rabie T, Hirve S, Schmidt W, Curtis V. Comparing the performance of indicators of hand-washing practices in rural Indian households. Trop Med Int Health. 2008;13:278–285. doi: 10.1111/j.1365-3156.2007.02001.x. [DOI] [PubMed] [Google Scholar]
- 54.Luby SP, Halder AK. Associations among handwashing indicators, wealth, and symptoms of childhood respiratory illness in urban Bangladesh. Trop Med Int Health. 2008;13:835–844. doi: 10.1111/j.1365-3156.2008.02074.x. [DOI] [PubMed] [Google Scholar]
- 55.Webb A, Stein A, Ramakrishnan U, Hertzberg V, Urizar M, Martorell R. A simple index to measure hygiene behaviours. Int J Epidemiol. 2006;35:1469–1477. doi: 10.1093/ije/dyl165. [DOI] [PubMed] [Google Scholar]
- 56.Curtis V, Danquah L, Aunger R. Planned, motivated and habitual hygiene behaviour: an eleven country review. Health Educ Res. 2009;24:655–673. doi: 10.1093/her/cyp002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Luby SP, Halder AK, Tronchet C, Akhter S, Bhuiya A, Johnston RB. Household characteristics associated with handwashing with soap in rural Bangladesh. Am J Trop Med Hyg. 2009;81:882–887. doi: 10.4269/ajtmh.2009.09-0031. http://www.ajtmh.org/cgi/reprint/81/5/882 (accessed Jan 19, 2011). [DOI] [PubMed] [Google Scholar]
- 58.Scott BE, Schmidt WP, Aunger R, Garbrah-Aidoo N, Animashaun R. Marketing hygiene behaviours: the impact of different communication channels on reported handwashing behaviour of women in Ghana. Health Educ Res. 2008;23:392–401. doi: 10.1093/her/cym056. [DOI] [PubMed] [Google Scholar]
- 59.Scott BE, Lawson DW, Curtis V. Hard to handle: understanding mothers' handwashing behaviour in Ghana. Health Policy Plan. 2007;22:216–224. doi: 10.1093/heapol/czm014. [DOI] [PubMed] [Google Scholar]
- 60.Biran A, Tabyshalieva A, Salmorbekova A. Formative research for hygiene promotion in Kyrgystan. Health Policy Plan. 2005;20:213–221. doi: 10.1093/heapol/czi024. [DOI] [PubMed] [Google Scholar]
- 61.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3:275–281. doi: 10.1016/s1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 62.Judah G, Aunger R, Schmidt WP, Michie S, Granger S, Curtis V. Experimental pretesting of hand-washing interventions in a natural setting. Am J Public Health. 2009;99:S405–S411. doi: 10.2105/AJPH.2009.164160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Curtis VA, Biran A, Deverell K, Hughes C, Bellamy K, Drasar B. Hygiene in the home: relating bugs to behaviour. Soc Sci Med. 2003;57:657–672. doi: 10.1016/s0277-9536(02)00409-4. [DOI] [PubMed] [Google Scholar]
- 64.Judah G, Donachie P, Cobb E, Schmidt W, Holland M, Curtis V. Dirty hands: bacteria of faecal origin on commuters' hands. Epidemiol Infect. 2009;138:409–414. doi: 10.1017/S0950268809990641. [DOI] [PubMed] [Google Scholar]
- 65.Biran A, Tabyshalieva A, Salmorbekova Z. Formative research for hygiene promotion in Kyrgyzstan. Health Pol Plan. 2005;20:213–221. doi: 10.1093/heapol/czi024. [DOI] [PubMed] [Google Scholar]
- 66.Curtis V, Kanki B, Cousens S, Sanou A, Diallo I, Mertens T. Dirt and diarrhoea: formative research for hygiene promotion programmes. Health Plan. 1997;12:122–131. doi: 10.1093/heapol/12.2.122. [DOI] [PubMed] [Google Scholar]
- 67.Young DR, Johnson CC, Steckler A. Data to action: using formative research to develop intervention programmes to increase physical activity in adolescent girls. Health Educ Behav. 2006;33:97–111. doi: 10.1177/1090198105282444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aunger R, Schmidt W, Ranpura A. Three kinds of psychological determinants for hand-washing behaviour in Kenya. Soc Sci Med. 2010;70:383–391. doi: 10.1016/j.socscimed.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 69.Whitby M, McLaws ML, Ross MW. Why healthcare workers don't wash their hands: a behavioral explanation. Infect Control Hosp Epidemiol. 2006;27:484–492. doi: 10.1086/503335. [DOI] [PubMed] [Google Scholar]
- 70.Aunger R, Curtis V. Lifebuoy five occasions study. PhD thesis, London School of Hygiene and Tropical Medicine; 2009. [Google Scholar]
- 71.Porzig-Drummond R, Stevenson R, Case T, Oaten M. Can the emotion of disgust be harnessed to promote hand hygiene? Experimental and field-based tests. Soc Sci Med. 2009;68:1006–1012. doi: 10.1016/j.socscimed.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 72.Curtis V, Kanki B, Cousens S. Evidence for behaviour change following a hygiene promotion programme in West Africa. Bull World Health Organ. 2001;79:518–527. [PMC free article] [PubMed] [Google Scholar]
- 73.Loevinsohn BP. Health education interventions in developing countries: a methodological review of published articles. Int J Epidemiol. 1990;19:788–794. doi: 10.1093/ije/19.4.788. [DOI] [PubMed] [Google Scholar]
- 74.Bolam A, Manandhar D, Shrestha P, Ellis M, Costello A. The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised controlled trial. BMJ. 1998;316:805–811. doi: 10.1136/bmj.316.7134.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Naikoba S, Hayward A. The effectiveness of interventions aimed at increasing handwashing in healthcare workers—a systematic review. J Hosp Infect. 2001;47:173–180. doi: 10.1053/jhin.2000.0882. [DOI] [PubMed] [Google Scholar]
- 76.Waterkeyn J, Cairncross S. Creating demand for sanitation and hygiene through Community Health Clubs: a cost-effective intervention in two districts in Zimbabwe. Soc Sci Med. 2005;61:1958–1970. doi: 10.1016/j.socscimed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 77.Bowen A, Ma H, Ou J. A cluster-randomized controlled trial evaluating the effect of a handwashing promotion program in Chinese primary schools. Am J Trop Med Hyg. 2007;766:1166–1173. [PubMed] [Google Scholar]
- 78.O'Reilly CE, Freeman MC, Ravani M. The impact of a school-based safe water and hygiene programme on knowledge and practices of students and their parents: Nyanza Province, western Kenya. Epidemiol Infect. 2008;136:80–91. doi: 10.1017/S0950268807008060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sidibe M. Can hygiene be cool and fun? Understanding school children's motivations to use their school toilets and wash their hands with soap in Dakar, Senegal. London School of Hygiene and Tropical Medicine; London: 2007. [Google Scholar]
- 80.Schmidt WP, Aunger R, Coombes Y. Determinants of handwashing practices in Kenya: the role of media exposure, poverty and infrastructure. Trop Med Int Health. 2009;14:1303–1314. doi: 10.1111/j.1365-3156.2009.02404.x. [DOI] [PubMed] [Google Scholar]