Summary
In 1915, a British medical officer on the Western Front reported on a soldier with relapsing fever, headache, dizziness, lumbago, and shin pain. Within months, additional cases were described, mostly in frontline troops, and the new disease was called trench fever. More than 1 million troops were infected with trench fever during World War 1, with each affected soldier unfit for duty for more than 60 days. Diagnosis was challenging, because there were no pathognomonic signs and symptoms and the causative organism could not be cultured. For 3 years, the transmission and cause of trench fever were hotly debated. In 1918, two commissions identified that the disease was louse-borne. The bacterium Rickettsia quintana was consistently found in the gut and faeces of lice that had fed on patients with trench fever and its causative role was accepted in the 1920s. The organism was cultured in the 1960s and reclassified as Bartonella quintana; it was also found to cause endocarditis, peliosis hepatis, and bacillary angiomatosis. Subsequently, B quintana infection has been identified in new populations in the Andes, in homeless people in urban areas, and in individuals with HIV. The story of trench fever shows how war can lead to the recrudescence of an infectious disease and how medicine approached an emerging infection a century ago.
Introduction
The Battle of the Aisne in France in September, 1914, marked the beginning of trench warfare on the Western Front. Within months, a network of 4000 miles of trenches extended from the English Channel to Switzerland and this was where millions of men would live, fight, and die during the next 4 years.1
In June, 1915, a British medical officer in Flanders, Major John Graham, reported: “A private [from] an infantry regiment was admitted to a casualty clearing station… suffering from a febrile illness of three days' duration… headache, dizziness, severe lumbago, a feeling of stiffness down the front of the thighs, and severe pains in the legs referred chiefly to the shins”. The private's fever resolved for several days, and then he had another bout of fever and the aforementioned symptoms. After the second round of fever, he recovered, except for fatigue. Graham remarked: “I have been receiving cases in considerable numbers presenting clinical features which do not differ… from those given above”.2, 3 Graham was describing what would become known as trench fever. This Historical Review will outline the 3-year quest to identify the epidemiology and cause of trench fever, an infection that would sap the manpower resources of both sides during World War 1. The discoveries of the mode of transmission and causative organism of trench fever represent triumphs of rigorous clinical investigation over the idle speculation that permeated medical discourse at that time. From this springboard, the evolution of our current understanding of trench fever is also described.
The investigations begin
The cases described by Graham were brought to the attention of Colonel Wilmot Herringham, consulting physician to the British First Army. Herringham invited Colonel William Leishman (advisor in pathology to the British Expeditionary Force) to consult on this seemingly new disease. The possibility that these cases were dengue or sandfly fever was entertained, but the new disease did not fit the descriptions of these afflictions.4 The disease took months to be recognised, partly because of the fragmented nature of military medical care.5 In June, 1915, Leishman wrote of the new ailment “I am doubtful whether it deserves serious attention”.1 In a meeting on June 21, with Lieutenant-General Alfred Keogh, Director-General of the Royal Army Medical Corps (RAMC), Leishman did not bother to mention the illness.1 Nevertheless, when he returned to France, Leishman promoted further investigations on the disease and, with Herringham, visited several hospitals that had cases. By August, 1915, Leishman shared Herringham's view that this illness was novel.1
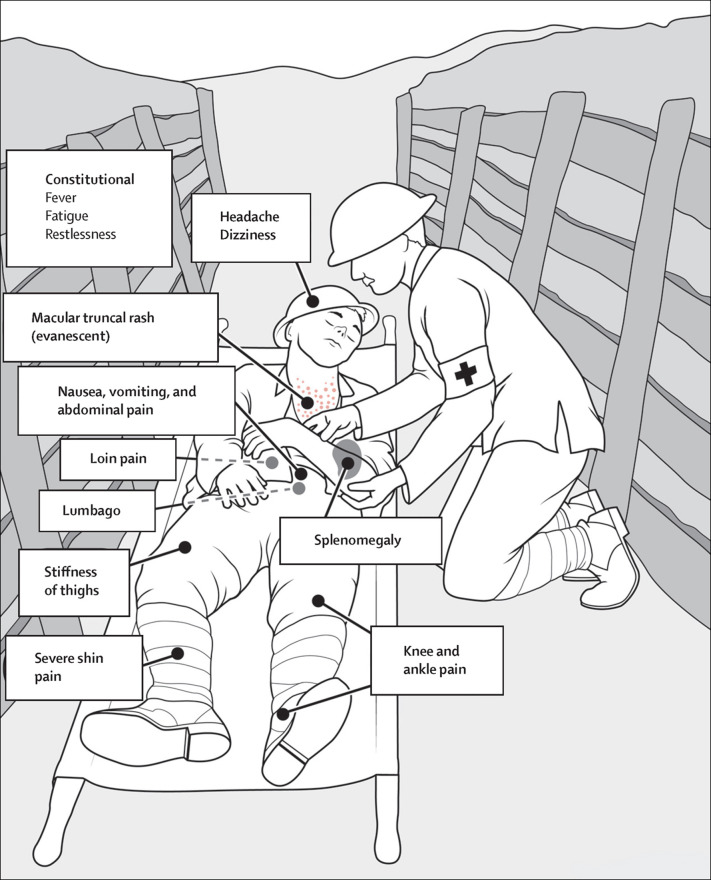
2 months after Graham's report, George Hunt of the RAMC and Allan Rankin of the Canadian Army Medical Corps (CAMC) reported on 30 patients with the following characteristics: headache, back and limb pain, without catarrh or gastrointestinal symptoms; slight constitutional disturbance, even with high fever (unlike typhus, typhoid, or relapsing fever); and the absence of rash (unlike dengue or typhus), splenic enlargement (unlike relapsing fever or malaria), and bronchitis (figure 1 ).6 In fact, patients with trench fever can present with splenomegaly and an evanescent rash resembling that of typhoid.7, 8 Attempts to culture the causative organism from blood, faeces, urine, and the nasopharynx failed. Blood films were also unrevealing.6 Hunt and Rankin proposed that this was a newly discovered disease and used the term trench fever for the first time in the scientific literature (although this name had already entered army vernacular).1
Figure 1.
Major signs and symptoms of trench fever
© 2016 Sue Simon, UTHSCSA
Soon thereafter, the naysayers emerged. A letter to the editor followed Hunt and Rankin's report, challenging their assertion that trench fever was novel, and proposing paratyphoid as the cause.9 Hunt and Rankin countered that the bacterium causing paratyphoid is culturable.10 Another physician blamed trench fever on atmospheric conditions in the trenches, but this received no serious consideration.1 Trench fever was recognised soon after in French troops, and then in Greece, Mesopotamia, Italy, and on the Eastern Front.1, 11
In February, 1916, John McNee and Arnold Renshaw of the RAMC published a comprehensive account of trench fever and did the first experimental investigations.4 More than 100 attempts to culture the organism from blood were unsuccessful. Serological tests for typhoid, paratyphoid, and brucellosis were negative. Stool and urine cultures and blood smears were unrevealing. McNee and Renshaw reported that the malady occurred in frontline soldiers and their medical personnel and that the infection could be transmitted by the inoculation of blood from a case of trench fever. Thus, they proposed that the disease was most likely insect-borne, by flies, mosquitoes, midges, or lice.4 At a conference in May, 1916, Leishman presented an overview of trench fever and it was recognised in RAMC documents by August, 1916.1 Nevertheless, scepticism remained. In October, 1916, Sidney Dyke of the RAMC reported seeing 200 patients with fever in a field hospital; he doubted that these cases represented a new entity and ascribed the fevers to “nervous” influenza.12
There was enough early suspicion of an insect vector that in the autumn of 1915, entomologist Alexander Peacock was assigned to investigate the transmission of trench fever within the trenches. Peacock did a 6-month study of the body louse and published his notes on its natural history in 1916. Peacock also examined 274 soldiers and found that 95% were infested with body lice. After excluding those with more than 100 lice, the mean number of lice per man was 20 (range 10–30). About 5% of the soldiers were infested with more than 130 lice.13
In 1916, T Strethill Wright of the RAMC posited that because trench fever occurred throughout the winter, it was unlikely to be transmitted by flies or midges. He proposed the louse as the most likely vector;14 although mosquitos, fleas, and ticks had all been incriminated as vectors of infection before the 20th century, the relation of the body louse to typhus and relapsing fever had only been discovered within the previous decade.15 Wright also thought that rodents could harbour ectoparasites that might serve as vectors of trench fever.14 Arthur Hurst of the RAMC reasoned that because trench fever did not cause diarrhoea or catarrh, it must be insect-borne. Furthermore, he noted that lice were ubiquitous compared with other potential vectors.16 Evidence continued to mount that incriminated the louse—eg, trench fever was more common in units with higher rates of louse infestation.16, 17 In January, 1916, there was an outbreak of pyrexia of unknown origin among Allied troops in Salonika (now Thessaloniki, Greece), which continued into May. Meanwhile, to control louse infestation in Salonika, the barrel disinfector (originally used in Serbia to control typhus in 1915) was implemented and the incidence of pyrexia of unknown origin decreased substantially.18 In July, 1916, Hunt and McNee concluded that lice were responsible, on the basis of exposure histories of personnel at a casualty clearing station who had contracted trench fever.19 Nevertheless, in July, 1916, Herringham remained unconvinced of louse-borne transmission.20, 21 In September, 1916, William Rutherfurd and Basil Hughes of the RAMC blamed those ever-present denizens of the trenches, field voles and rats.22, 23 Later that year, John Muir disputed the term trench fever and the association with lice; he implicated a nasopharyngeal virus.24
The German experience
The first German report of trench fever was in 1916 by Wilhelm His Jr. He first observed the disease in a Russian prison in May, 1915, and then saw other cases in the autumn of 1915 in Wolhynia (Poland). At a meeting of military physicians in Warsaw in January, 1916, German hygienist Heinrich Werner reported similar cases. His termed the disease “Wolhynia fever”, whereas Werner called it “five-day fever”.25 His and Werner each published their findings in 1916.26, 27
The Commissions
In August, 1916, Leishman asked laboratorian Adrian Stokes to try to infect laboratory animals with trench fever by use of infected lice.1 However, these experiments failed because human body lice do not feed on non-primates and laboratory animals are generally not susceptible to trench fever.28 By this time, several British and German physicians had done self-inoculation studies using infected lice, but the results were inconsistent.21, 25, 29, 30 Thus, only experimentation with a larger number of participants would provide a definitive answer regarding louse-borne transmission. In Britain, Keogh established the War Office Trench Fever Investigation Commission (TFIC).1
The TFIC had its origins in studies of trench fever done by RAMC physician William Byam at Hampstead Heart Hospital in 1917. Byam noted an association between so-called disordered action of the heart and previous trench fever; he then tried to transmit trench fever to laboratory animals using blood from these patients. Byam's experiments came to the attention of the War Office, and the TFIC was formed.1 The commission was chaired by David Bruce (who had discovered the cause of brucellosis and African trypanosomiasis) and it held its first meeting in November, 1917. Bruce assembled a team of accomplished physicians and scientists that included three fellows of the Royal Society. The goal of the TFIC was “to make a complete investigation of the disease from every point of view”.31 The commission recruited more than 200 men, mostly unfit for military service, who volunteered to do their part for King and country.20, 31 Previously, McNee and Renshaw4 had shown that trench fever was transmissible by blood inoculation, so the investigators started from this point. On Feb 14, 1918, the TFIC announced that the human body louse (figure 2 ) is the vector of trench fever and that the inoculation of infected louse faeces into abraded skin or the conjunctivae is the means of transmission.32 The TFIC also made several salient observations (panel ).
Figure 2.
The human body louse Pediculus humanus corporis in the process of defecation
© 2016 Darlyne Murawski
Panel. Observations of the War Office Trench Fever Investigation Commission32.
-
•
The human body louse is the vector of trench fever and the inoculation of infected louse faeces into abraded skin or the conjunctivae is the means of transmission
-
•
The average incubation period is 7·7 days
-
•
The gut contents of one infected louse is sufficient for transmission
-
•
The bite does not cause transmission because there is no salivary gland involvement or regurgitation
-
•
The causative organism is within the blood plasma
-
•
Patients with trench fever are capable of infecting lice for at least 443 days from the onset of illness
-
•
Louse faeces are not infective via nasal or oral routes
-
•
The faeces become infective 5 days after the louse feeds on a patient with trench fever
-
•
The organism is not passed from infected lice to their offspring
-
•
Head lice can also transmit the infection
-
•
Infected faeces remain infectious for at least 4 months
-
•
The infection is likely to be rickettsial31
The group also learned much about louse behaviour.33 By experimental inoculation, they recorded the characteristics of trench fever more accurately than under chaotic field conditions. In 200 cases, they recorded headache (74%); pain in the shins (46%), loins (31%), knees (22%), ankles (20%), thighs (20%), calves (13%), and shoulders or arms (8%); chills (26%); sweating (19%); frequent urination (13%); dizziness (12%); nausea and vomiting (11%); abdominal pain (8%); and diarrhoea (6%). Patients also frequently reported restlessness and inability to find a position of comfort.20
Meanwhile, in mid-1917, the British Expeditionary Force Pyrexia of Unknown Origin Inquiry Sub-committee was established to study trench fever at an RAMC Hospital near Saint-Pol-sur-Ternoise, France.34 In October, 1917, the American Red Cross set up the Medical Research Committee (MRC) to study military medical problems. The MRC was chaired by physician Richard Strong, who had directed the International Sanitary Commission that suppressed an epidemic of typhus in Serbia in 1915. Other members of the MRC were recruited primarily from American medical academia.7
Strong attended a meeting of the British Expeditionary Force Medical Investigation Committee on Dec 8, 1917, with Herringham and Leishman in attendance.1 There, it was agreed that the MRC should investigate the mode of transmission of trench fever and the infectious properties of the blood.11 At that point in the war, trench fever was second only to scabies in terms of its detrimental effect on military manpower.1, 7
The MRC did 103 human experiments, focusing on transmission by blood, blood constituents, lice, urine, faeces, and sputum; and determination of the pathogen.7 In January, 1918, it was arranged for the MRC to do its investigations at Saint-Pol-sur-Ternoise, to have access to cases of trench fever at an early stage.7 The British had no soldiers to spare, so the US Army supplied hundreds of volunteers, with 82 being selected.7, 34
According to Herringham, the British and American medical personnel got along well: “I should like to say a few words, if without impertinence, on the good feeling and good fellowship which existed between us and the Americans”. Herringham described Strong as “a wise quiet man, with a dry smile, well known for his pathologic discoveries, whose one care, as he said himself, was to carry out his work in such a way that it would not have to be done again… His second in command [Homer Swift] gave us to understand that to take part in the elucidation of a new disease was a greater fortune than he had ever hoped and that he would now die a happy man”.34
The MRC released its findings on March 9, 1918, and they mostly mirrored the findings of the War Office, although the MRC erroneously reported that the louse might transmit trench fever by its bite.7 However, later in March, a German attack forced the MRC team to abandon its work at the hospital at Saint-Pol-sur-Ternoise and they retreated to Paris to continue their studies. When the hospital resumed operations in the summer of 1918, the number of cases of trench fever was greatly diminished; the warm weather and louse control measures reduced louse infestation among the Allied troops and the cases of trench fever dropped accordingly.34
The work of the MRC received high praise from the medical community. William Osler stated: “the [MRC] has done a splendid service… We may join heartily in the thanks which the Commission offers to the men who endured so patiently the many trials of the experiment. To Maj Strong and his able colleagues we may offer our warmest congratulations”.35 Bruce declared “the louse at last has emerged from its seclusion and [is] crawling in the full light of notoriety”.21 Nevertheless, Bruce claimed primacy of the TFIC over the MRC for the discovery of the mode of transmission of trench fever,20 but his team had the advantages of a head start in the research and the ready means to publish first because they were based in London. Some commentators have argued that both the TFIC and the MRC should have received equal credit for this discovery.36
Nevertheless, on the basis of unsuccessful self-infection experiments, in March, 1918, Charles Sundell and Austin Nankivell of the RAMC still doubted louse-borne transmission.29 Dyke also discounted the louse because trench fever occasionally occurred in people without obvious louse exposure.12 However, the results of the two commissions firmly established louse-borne transmission of the disease.
The work of the commissions has been criticised for coming too late; perhaps if the studies had been done earlier, the number of cases of trench fever would have been substantially lower.3 Medical historian Frederick Holmes stated that “the complicated bureaucratic research efforts to find the cause and cure of trench fever were late and feeble”.37 However, once the commissions were established, they quickly produced sterling bodies of work, characterising a disease unknown to science less than 5 years earlier, at a time of low technological sophistication, manpower shortages, and other pressing priorities. Most of their conclusions have withstood the test of time and were a valuable contribution to understanding this disease.
Clinical controversies
In the early 20th century, fever curves were scrutinised to discern patterns that might aid diagnosis. For trench fever, several groups of investigators proposed characteristic fever patterns.21, 29 The McNee team and Hurst described long and short forms.4, 16 The MRC recognised three patterns: relapsing, one short episode, and protracted.8 Sundell and Nankivell maintained that the long form was the only true pattern,29 but the TFIC stated that neither periodic fevers nor shin pain were the sine qua non of a trench fever diagnosis.21
Although these fever classifications were devised to assist diagnosis, there were too many variations to be useful; however, a relapsing pattern occurred with few other diseases (eg, relapsing fever, malaria, rat bite fever, brucellosis, leptospirosis, typhoid). The relapsing pattern occurred in about half of cases, and typically there were three to five relapses.7 In any case, fever records were often lost during the hectic process of transferring sick and wounded soldiers, further limiting their usefulness.8
No case definition was ever agreed on and so trench fever was diagnosed clinically and by ruling out other infections.5 Trench fever was distinguished from influenza by the absence of rhinorrhoea or cough. Malaria could be diagnosed by a blood smear and its course was modified by quinine. For louse-borne relapsing fever, the initial febrile period was longer than in trench fever and usually there was a single relapse. Jaundice, hepatomegaly, and albuminuria accompanied louse-borne relapsing fever, and shin pain was not prominent. Also, in louse-borne relapsing fever the spirochete is visible in the blood during the fever.11 Leptospirosis presents with nephritis and jaundice.7
Trench fever was also held responsible for disordered action of the heart, which presented as exhaustion, dyspnoea, palpitations, precordial pain, giddiness, and fainting.38 Some investigators claimed that up to 50% of cases of disordered action of the heart were caused by trench fever.39 Whether this was a true physiological sequela of trench fever, a manifestation of post-traumatic stress, or malingering was uncertain. Hurst opined that disordered action of the heart was not caused by trench fever, and he recommended only short periods of convalescence: “Patients with trench fever who were kept in the hospital too long, especially if they were transferred to hospitals in England, showed a great tendency to become chronic invalids”.11 The MRC did not diagnose any cases of disordered action of the heart after experimental infection.40 However, Everard Grieveson of the RAMC, himself a victim of trench fever, reported that 1 month after his first attack he experienced breathlessness and tachycardia with exertion; he had a second attack, and “as I found it impossible to walk 20 yards over rough ground without breathlessness I was evacuated to England”.17
The TFIC reported that trench fever caused arrhythmias in response to exercise, which they ascribed to vagal effects; thyroid extract was said to be beneficial.21 Sundell and Nankivell reported that “during convalescence a rhythmic irregularity… is common, and [with] exercise his pulse-rate is very easily quickened… this undisciplined action of the heart is not usually of serious import. The treatment… is graduated exercise… not… indiscriminate drugging with digitalis and bromides”.29 In a post-war study, Venning reported that trench fever accounted for only 3·2% of cases of disordered action of the heart and that “trench fever… [does not] produce disordered action of the heart of great or lasting severity”.39
Another puzzling symptom was the prominent shin pain of trench fever. Some physicians argued that the tibial pain seen in trench fever was not more common than in other infections, whereas Robert Rudolf (consultant to the CAMC) commented: “I think few physicians of experience will deny that the shin pains are peculiarly common and agonizing in trench fever”.40 Graham Chambers of the CAMC argued that “trench shin” was an infection distinct from trench fever.41
In 1921, Arthur Bacot reported on shin pains as part of the misery associated with an attack of trench fever that he had in Poland: “The shin pains were again more intense than those in the other bones, and with each recurrence this feature became more apparent… causing restlessness and preventing sleep”.42 Overwhelming fatigue could also be a consequence of trench fever. Bacot had a reputation for relentless hard work, but when he contracted trench fever even “he was very much impressed by the inertia and mental depression induced in himself by the illness”.43 In 1920, 6000 British war veterans still attributed their disability to trench fever and received state pensions.3
Attempts at treatment during World War 1
In 1916, Hunt and McNee reported that quinine, salvarsan (arsphenamine), antimony, mercury ointment, eusol, and convalescent serum were all ineffective treatments for trench fever.19 Colloidal silver had its proponents and sceptics.21, 44 Sundell and Nankivell noted no improvement with salicylate, bromides, butyl chloral, urotropine (methenamine), or tincture of gelsemium, but aspirin and phenacetin or topical menthol provided pain relief.29 Hurst recommended magnesium sulfate compresses for the pain.11 Byam reported that a lumbar puncture relieved the leg pain, even though the cerebrospinal fluid was non-inflammatory.21 The TFIC reported that acriflavine and trypan red (both used to treat trypanosomiasis), galyl and ortho-aminothiobenzene (antisyphilitic drugs), sulphur, iodine, manganese, rhodium, methylene blue (antimalarial drug), and killed intravenous Salmonella spp afforded no benefit.21 Hughes claimed that a concoction of quinine, salicylate, iron, arsenic, and strychnine was curative and that liniment of turpentine soothed the shin pain.23 However, neither of these interventions was corroborated nor supported by trial data.
Dealing with the louse
Early in World War 1, the lousicide NCI, consisting of naphthalene, creosote, and iodoform, was developed at the RAMC College at Millbank (London, UK), by Percy Lelean.45 NCI was effective against adult lice, but was not ovicidal.46 Furthermore, the British military was unable to procure adequate supplies of NCI, because naphthalene was obtained from coal tar, most of which was allocated to the production of explosives.47 The War Office asked Bacot to determine the efficacy of other chemicals against lice, but none proved superior to NCI.45 The Germans used cyclohexanone, cyclohexanol, cresol soap, and diphenylamine.48, 49 French soldiers wore sachets of sawdust impregnated with naphthalene, camphor, and benzene to ward off lice.1
Until 1916, there was little instruction on pediculosis within the British Expeditionary Force. In that year, Peacock and Hurst published reports on louse infestation in the army.13, 16 The War Office thereby issued a pamphlet on the louse problem. During the winter of 1916–17, schools of sanitation for medical officers were established, with weekly lectures on pediculosis. Similar schools were later started for other personnel engaged in sanitary duties. In May, 1918, a brochure on disinfestation was issued by the Director-General of Medical Services. However, the practical results of these efforts were uncertain. The medical officers simply had too many other responsibilities and received inadequate resources for delousing.47, 50
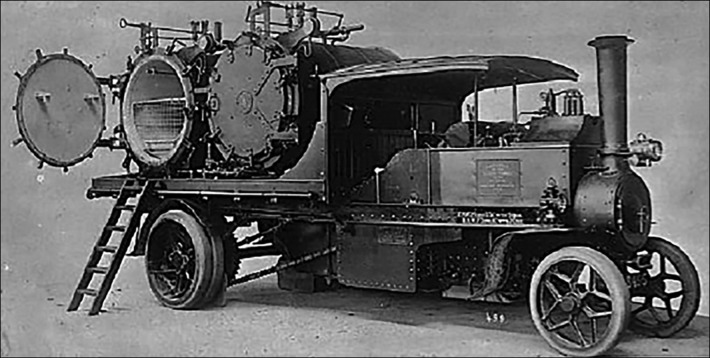
In the British Expeditionary Force, facilities were “not quite adequate”47 for bathing and the disinfestation of underclothing, and wholly wanting for the disinfestation of outer garments, even though infested khaki and cardigans were the main sources of lice. The central dilemma was that soldiers' clothing required frequent disinfestation. In 1915, the usual complement of disinfestation apparatus per division rarely exceeded one Foden Thresh (steam-propelled) disinfector (Figure 3, Figure 4 ) and two horse-drawn threshes. However, three disinfectors for one division were not even adequate to treat all the underwear. In 1915, there was an attempt to disinfest uniforms by ironing, but this was too labour intensive.47 In the absence of adequate resources for louse control, soldiers often resorted to manual disinfestation (figure 5 ). However, after the release of the TFIC and MRC reports in the spring of 1918, the British Expeditionary Force allocated more resources to louse control.1, 50
Figure 3.
The Foden Thresh steam disinfector
The Foden lorry was steam powered and thus was able to supply steam to the Thresh disinfector (this image is reproduced from Richard Peskett51 for non-commercial research purposes as permitted under the Copyright, Designs and Patents Act 1988, as amended and revised).
Figure 4.
The Foden Thresh steam disinfector at work
© 2016 sciencephoto.com
Figure 5.
German troops in a trench, manually picking lice and eggs from their clothing
© 2016 Alamy Limited
The search for the causative organism
After the unsuccessful investigations of the teams headed by Hunt and McNee, the quest for the microbiological cause of trench fever continued apace. In 1916, one group reported a bacterium (Micrococcus spp) in the blood cultures,52 but this finding was not replicated. Enterococcus spp was grown from the urine of patients with trench fever in 1916, and claimed as the causative organism,53 but this bacterium is a common urinary tract pathogen unrelated to trench fever. In 1917, Lyn Dimond of the RAMC reported a protozoal cause, but his work was discredited because contaminated water was used.54 Alwin Pappenheimer of the MRC proposed another protozoan, but he later recanted.55 A spirochete was proposed by H Moreland McCrea of the London Military Hospital, because of the presence of periostitis of the shins (analogous to syphilis).56 Werner also speculated that trench fever was caused by a spirochete because its recurrent course resembled relapsing fever.7
In 1916, German microbiologist Hans Toepfer found that lice that had fed on patients with trench fever contained “Rickettsia bodies”.57 Toepfer reported that he could morphologically differentiate these organisms from those causing typhus (Rickettsia prowasekii). His work was replicated by Fritz Munk and Henri da Rocha Lima of the Institute for Maritime and Tropical Diseases in Hamburg, who observed that R prowasekii invaded the epithelial cells of the louse gut, whereas the organisms causing trench fever did not,58 explaining why R prowasekii was lethal for the louse, whereas infection with the trench fever organism was not.
Byam presented the findings of the TFIC at a meeting of the Royal Society of Medicine, UK, in 1919, stating that the cause of trench fever was still unknown.33 Joseph Arkwright of the Lister Institute was then invited to elaborate on the possible causal role of “rickettsial bodies”, based on his investigations with Bacot and Duncan.59 The circumstantial evidence implicating rickettsiae was compelling; these organisms were abundant in the gut and faeces of lice that had fed on patients with trench fever. The organisms, which they named Rickettsia quintana, were similar to those seen in lice infected with R prowasekii. By contrast, R quintana was absent from lice that had fed on healthy controls or patients with other infections. However, Arkwright was unable to grow the organism in culture (as with R prowasekii). Despite Arkwright's evidence, scepticism remained. Percy Bassett-Smith of the Royal Navy stated that a spirochetal cause had not been disproven.33 Previously, at a meeting of the Society of Tropical Medicine and Hygiene in 1918, Bruce stated that he was unconvinced that bacteria of “that almost mythical genus Rickettsia” were the cause of trench fever. Also in attendance, Leishman opined that a protozoan was responsible.21 In Strong's assessment, trench fever was caused by a virus.7 With the inability to culture R quintana, controversy regarding the nature of the rickettsial bodies persisted into the 1920s; they were postulated by Swift to be “a granular stage [of] some other micro-organism” or “[a viral] inclusion”.5
Perhaps the greatest failing of the commissions was this inability to establish the causative organism. Medicine had just passed through the “golden age of bacteriology”, in which 20 pathogens had been cultured and identified.60 Thus, at the time of the commissions, medical bacteriology was mired in adherence to Koch's postulate that the causative bacterium must be cultured. However, even in the absence of fulfilment of Koch's postulates, by the early 1920s there was general acceptance of the role of R quintana in the genesis of trench fever.61
The impact of trench fever during World War 1
Trench fever had a major effect on the manpower resources of both the Allies and the Central Powers. An estimated 800 000 cases occurred among the Allies on the Western Front during World War 1.33 Trench fever caused a fifth to a third of all illnesses in the British Army and a fifth in the armies of the Central Powers.7 However, these are estimates, because no official records were kept.11 Each soldier affected by trench fever was typically unfit for duty for 60–70 days. Hurst was unable to find any accounts of trench fever by World War 1 Russian physicians, but he contended that it must have been common in their troops as well.11
Was trench fever a new disease?
McNee believed that trench fever was introduced by colonial troops serving in the British Expeditionary Force.7 By 1920, trench fever was suspected to be identical to “febris Wolhynica” known in pre-war Poland.33 In retrospect, the “five-day fever” in the Russian medical literature of the 1800s and the Moldavia fever of the Russo-Turkish war of 1877 were probably trench fever.11 Hurst has proposed that in early 1915 louse-infested German soldiers conveyed trench fever from the Eastern Front to the Western Front, whereupon it spread to the British and French.11 Definitive evidence that trench fever was present in Europe centuries before World War 1 has been obtained by paleomicrobiological investigations. Analysis of DNA extracted from dental pulp has provided evidence of B quintana infection in Napoleon's soldiers at a Lithuanian gravesite (dated to 1812) and several French gravesites dating from 300 to 4000 years ago.62
The aftermath
Despite the return of millions of troops during and after World War 1, trench fever was not a problem for British civilians, although it was reported in soldiers who were quartered with returning troops.11 Within months of the armistice, trench fever disappeared from the British Army on the continent.11 The Allies implemented rigorous disinfestation procedures at French ports to prevent lice from returning with the troops.1 Trench fever was seen in post-war Poland and was common among German troops on the Eastern Front during World War 2.11, 63 However, multifront outbreaks of trench fever were not reported during World War 2. More effective lousicides were used early in the war by most of the combatants.15 By 1944, DDT, the lousicide par excellence, was also adopted by both sides.15 Furthermore, because of the mobile nature of tactics in World War 2, soldiers were not generally crowded closely together for prolonged periods, as in World War 1. After World War 2, trench fever was reported sporadically from Poland, USSR, Ethiopia, Mexico, and China.64
The trench fever organism was grown in culture in 1961, by J William Vinson of Harvard University and Henry Fuller of Walter Reed Army Institute of Research, and this permitted the first antibiotic susceptibility testing.65 Vinson and coworkers subsequently infected volunteers with the in-vitro isolates, producing trench fever and at last fulfilling Koch's postulates.66 Because it could be cultured, the organism was moved to the genus Rochalimaea in 1961.67 In 1993, Rochalimaea was unified with Bartonella.68 In 2004, the genomes of Bartonella quintana and Bartonella henselae (which causes cat scratch disease) were sequenced; B quintana has extensive genomic reduction compared with B henselae, because of its exquisite adaptation to its human host.69
Since the 1990s, a series of investigations altered traditional views of the epidemiology and pathogenesis of B quintana infection. In 1999, a serosurvey in the Peruvian Andes showed a 12% rate of exposure to B quintana, the first evidence of this pathogen in South America.70 Surprisingly, trench fever has been reported in homeless people in multiple cities in high-income countries.71
Novel manifestations of B quintana infection have also been described, including endocarditis, bacillary angiomatosis, lymphadenitis, and peliosis hepatis.72 From the 1980s, individuals with HIV infection have represented a new group that is highly susceptible to Bartonella spp infection. Two features of Bartonella spp pathogenesis remain to be explained: the organism's ability to cause persistent bacteraemia and to induce vasculoproliferative lesions, such as bacillary angiomatosis.72 The current treatment for trench fever is gentamicin for 2 weeks, followed by doxycycline for 4 weeks; for bacillary angiomatosis, erythromycin is preferred.72
The human head louse, cat flea, bed bug, and pigeon mite have also been implicated as vectors.73, 74, 75 People were thought to be the only reservoir for B quintana, but recently it was discovered that macaques and cats can harbour the organism.76, 77
Conclusions
With rapid response teams and the techniques of tissue culture, electron microscopy, microarrays, serological testing, and genomic amplification, modern scientists can elucidate the causes and epidemiological characteristics of a new infection in months;78 examples include hantavirus pulmonary syndrome, severe acute respiratory syndrome, and Middle East respiratory syndrome. Dissecting the epidemiology and aetiology of trench fever took years; it posed a particular challenge because there were no pathognomonical laboratory or clinical findings and the causative organism could not be cultured.8
Six factors lead to the emergence of new infectious disease: changes in human demographics and behaviour; travel and commerce; the breakdown of public health infrastructure; new technologies; economic development and changes in land use; and microbial adaptation.79 For trench fever during World War 1, the first three factors were operative. The epidemic of trench fever shows how war can act as a catalyst for the recrudescence of an infectious disease;80 other examples include malaria in World War 1, leishmaniasis during the Sudanese civil war, and epidemic typhus during the Burundian civil war. The story of trench fever also shows the methods used by physicians a century ago to deal with an emerging disease threat and scientific discourse in the early age of medical microbiology.81
Search strategy and selection criteria
I searched PubMed for articles published from Jan 1, 1915, to Feb 1, 2016 using the terms “trench fever”, “Rickettsia quintana”, and “Bartonella quintana”. Additional references were obtained by bibliographic branching and Google searches with identical terms. References published in English and German were examined.
Acknowledgments
Acknowledgments
I thank Robert Atenstaedt, who greatly enriched my understanding of this historic problem by combing through the archives of the Royal Army Medical Corps, as presented in his publications cited herein.
Contributors
I am sole author and contributor.
Declaration of interests
I declare no competing interests.
References
- 1.Atenstaedt RL. The medical response to the trench diseases in World War One. Cambridge Scholars Publishing; Newcastle upon Tyne: 2011. [Google Scholar]
- 2.Graham JHP. A note on a relapsing febrile illness of unknown origin. Lancet. 1915;186:703–704. [Google Scholar]
- 3.Atenstaedt RL. Trench fever: the British medical response in the Great War. J R Soc Med. 2006;99:564–568. doi: 10.1258/jrsm.99.11.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McNee JW, Renshaw A. “Trench fever”: a relapsing fever occurring with the British forces in France. Br Med J. 1916;1:225–234. [Google Scholar]
- 5.Swift H. Trench fever. Arch Intern Med. 1920;26:76–98. [Google Scholar]
- 6.Hunt GH, Rankin AC. Intermittent fever of obscure origin, occurring among British troops in France. The so-called trench fever. Lancet. 1915;186:1133–1136. [Google Scholar]
- 7.Strong RP, Swift HF, Opie EL. Trench fever. Report of Commission. Medical Research Committee. Oxford University Press; American Red Cross, Oxford: 1918. [Google Scholar]
- 8.Swift HF. Trench fever in the American Expeditionary Forces. JAMA. 1919;73:807–812. [Google Scholar]
- 9.Robinson H. So-called “trench fever”. Lancet. 1915;186:1214–1215. [Google Scholar]
- 10.O'Connell MD, Hunt GH, Rankin AC. Trench fever. Lancet. 1915;186:1368–1369. [Google Scholar]
- 11.Hurst A. Medical diseases of war. Williams and Wilkins; Baltimore (MD): 1944. [Google Scholar]
- 12.Dyke SC. Trench pyrexias. Lancet. 1916;188:767–768. [Google Scholar]
- 13.Peacock A, Pearson W. The Peacock versus the louse (pediculus humanis corporis): one soldier's contribution to combating trench fever in the First World War. J R Coll Physicians Edinb. 2010;40:256–262. doi: 10.4997/jrcpe.2010.315. [DOI] [PubMed] [Google Scholar]
- 14.Wright TS. Some notes on trench fever. Br Med J. 1916;2:136–138. doi: 10.1136/bmj.2.2900.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Busvine JR. Disease transmission by insects. Its discovery and 90 years of efforts to prevent it. Springer-Verlag; Berlin: 1993. [Google Scholar]
- 16.Hurst AF. Trench fever: a relapsing fever occurring among the British troops in France and Salonica. Lancet. 1916;188:671–675. doi: 10.1136/jramc-2014-000305. [DOI] [PubMed] [Google Scholar]
- 17.Grieveson ER. Some observations on trench fever. Lancet. 1917;190:84–86. [Google Scholar]
- 18.Hunter W. A lecture on the prevention and arrest of lice-borne diseases by new methods of disinfection. Lancet. 1918;192:377–378. [Google Scholar]
- 19.Hunt GH, McNee JW. Further observations on trench fever. Q J Med. 1915-16;9:442–449. [Google Scholar]
- 20.Byam W, Carroll JH, Churchill JH. Trench fever, a louse-borne disease. Oxford University Press; London: 1919. [Google Scholar]
- 21.Byam W, Carroll JH, Churchill JH, Dimond L, Lloyd Ll, Sorapure VE. Trench fever—a louse-borne disease. Trans Soc Trop Med Hyg. 1917-18;11:237–245. [Google Scholar]
- 22.Rutherfurd WJ. Trench fever. The field vole a possible origin. Br Med J. 1916;2:386–387. doi: 10.1136/bmj.2.2907.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes B. Trench pyrexias; their prevention and treatment. Lancet. 1916;188:474–475. [Google Scholar]
- 24.Muir J. “Pyrexia” or “trench fever”. Br Med J. 1916;2:641–645. doi: 10.1136/bmj.2.2915.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.His W., Jr . A German doctor at the front. National Service Publishing Co; Washington, DC: 1933. [Google Scholar]
- 26.His W. A new period fever disease (Wolhynica fever) Berl Klin Wochensch. 1916;27:738–739. (in German). [Google Scholar]
- 27.Werner H. About a particular disease, called the five-day fever. Berl Klin Wochenschr. 1916;53:204. (in German). [Google Scholar]
- 28.Arkwright JA, Bacot A, Duncan FM. The association of rickettsia with trench fever. J Hyg. 1919;19:76–96. doi: 10.1017/s0022172400007397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sundell CE, Nankivell AT. Trench fever. Lancet. 1918;191:399–403. [Google Scholar]
- 30.Davies FC, Weldon RP. A preliminary contribution on “P.U.O. (trench fever).”. Lancet. 1917;189:183–184. [Google Scholar]
- 31.Bruce D. Trench fever. Final report of the War Office Trench Fever Investigation Committee. J Hyg (Lond) 1921;20:258–288. doi: 10.1017/s0022172400034008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.War Office Trench Fever Investigation Commission Transmission of trench fever by the louse. Br Med J. 1918;1:354–355. [Google Scholar]
- 33.Byam W, Lloyd LI. Trench fever: its epidemiology and endemiology. Proc R Soc Med. 1920;13:1–27. [PMC free article] [PubMed] [Google Scholar]
- 34.Herringham WP. A physician in France. Edward Arnold; London: 1919. https://archive.org/details/physicianinfranc00herr (accessed April 26, 2016). [Google Scholar]
- 35.Osler W. Trench fever: a critical analysis of the report of the American Commission. Lancet. 1918;192:496–498. [Google Scholar]
- 36.Bean CEW, ed. Official history of Australia in the War of 1914–1918. Australian War Memorial, 1921–1943. https://www.awm.gov.au/collection/RCDIG1069708/ (accessed April 26, 2016).
- 37.Holmes F. Trench fever in the First World War. http://www.kumc.edu/wwi/index-of-essays/trench-fever.html (accessed April 26, 2016).
- 38.Murray LM. The common factor in disordered action of the heart. Br Med J. 1918;2:650–665. doi: 10.1136/bmj.2.3024.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Venning JA. The etiology of disordered action of the heart. A report on 7,803 cases. Br Med J. 1919;2:337–339. doi: 10.1136/bmj.2.3063.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rudolf RD. Trench fever. Med Record. 1919;96:414–422. [Google Scholar]
- 41.Chambers G. Trench shin an infectious fibrositis. Lancet. 1917;189:752–755. [Google Scholar]
- 42.Bacot A. On the probable identity of Rickettsia pediculi with Rickettsia quintana. Br Med J. 1921;1:156–157. doi: 10.1136/bmj.1.3135.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenwood M, Arkwright JA. The life and scientific work of Arthur William Bacot. J Hyg. 1924;22:265–304. doi: 10.1017/s0022172400008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lloyd JH. Colloidal silver in trench fever. Lancet. 1919;193:583. [Google Scholar]
- 45.Bacot AW. The louse problem. Proc R Soc Med. 1917;10:61–94. [PMC free article] [PubMed] [Google Scholar]
- 46.Lelean PS. Sanitation in war. 2nd edn. P Blakiston's Son and Co; Philadelphia: 1917. [Google Scholar]
- 47.Peacock AD. Generalia of the louse problem at the Western Front. Lancet. 1921;198:1067–1077. [Google Scholar]
- 48.Beyer HG. On the etiology of typhus fever and louse extermination, from the point of view of the sanitarian. Milit Surg. 1916;38:483–491. [Google Scholar]
- 49.Weindling P. Epidemics and genocide in Central Europe, 1890–1945. Oxford University Press; Oxford: 2000. [Google Scholar]
- 50.MacPherson WG, Herringham WP, Elliott TR, Balfour A, editors. Vol I. His Majesty's Stationery Office; London: 1922. http://www.archive.org/stream/medicalservicesd01macpuoft/medicalservicesd01macpuoft_djvu.txt (Medical services. Diseases of war). (accessed April 26, 2016). [Google Scholar]
- 51.Peskett R. Historic military vehicle forum. 2015. http://hmvf.co.uk/forumvb/showthread.php?32602 (accessed June 1, 2015).
- 52.Birks AH, Thornley RT, Fawcus RA. Septicaemia due to micrococcus tetragenis as a cause of pyrexia at the front. Q J Med. 1916–1917;10:1–6. [Google Scholar]
- 53.Houston T, McCloy JM. The relation of the enterococcus to “trench fever” and allied conditions. Lancet. 1916;188:632–638. [Google Scholar]
- 54.Henry H. The haemogregarine of trench fever. Br Med J. 1917;2:739–740. [Google Scholar]
- 55.Pappenheimer AM. The etiology of trench fever. Br Med J. 1917;2:568. doi: 10.1136/bmj.2.2963.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McCrea HM. Trench fever. Is this condition a spirochaetosis? Lancet. 1917;189:796. [Google Scholar]
- 57.Toepfer HW. For the cause and transmission of Wolhynia fever. Munch Med Wochenschr. 1916;63:1495–1496. (in German). [Google Scholar]
- 58.Munk F, da Rocha Lima H. Clinic and etiology of so-called Volhynian fever. II. Results of etiological studies and their relations with the typhus research. Munch Med Wochenschr. 1917;30:1422–1433. (in German). [Google Scholar]
- 59.Arkwright JA, Bacot A, Martin Duncan F. Preliminary note on the association of rickettsial bodies in lice with trench fever. Br Med J. 1918;2:307–309. doi: 10.1136/bmj.2.3012.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Blevins SM, Bronze MS. Robert Koch and the ‘golden age’ of bacteriology. Int J Infect Dis. 2010;14:e744–e751. doi: 10.1016/j.ijid.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 61.Anon Typhus fever and its martyrs. JAMA. 1922;78:1054–1055. [Google Scholar]
- 62.Fournier PE, Drancourt M, Aboudharam G, Raoult D. Paleomicrobiology of Bartonella infections. Microbes Infect. 2015;17:879–883. doi: 10.1016/j.micinf.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 63.Zdrodovskii PF, Golinevich HM. The rickettsial diseases. Pergamon; London: 1960. [Google Scholar]
- 64.Vinson JW. In vitro cultivation of the rickettsial agent of trench fever. Bull World Health Organ. 1966;35:155–164. [PMC free article] [PubMed] [Google Scholar]
- 65.Vinson JW, Fuller HS. Studies on trench fever. I. Propagation of rickettsia-like from a patient's blood. Pathol Microbiol. 1961;24:152–166. [PubMed] [Google Scholar]
- 66.Vinson JW, Varela G, Molina-Pasquel C. 1969. Trench fever. III. Induction of clinical disease in volunteers inoculated with R quintana propagated on blood agar. Am J Trop Med Hyg. 1969;18:713–722. [PubMed] [Google Scholar]
- 67.Krieg A. Grundlagen der Insektenpathologie. Viren-, Rickettsien-, und Bakterien-Infektionen. Steinkopff; Darmstadt: 1961. [Google Scholar]
- 68.Brenner DJ, O'Connor SP, Winkler HH, Steigerwalt AG. Proposals to unify the genera Bartonella and Rochalimaea, with descriptions of Bartonella quintana comb. nov., Bartonella aii comb. nov., Bartonella henselae comb. nov., and Bartonella elizabethae comb. nov., and to remove the family Bartonellaceae from the order Rickettsiales. Int J Syst Bacteriol. 1993;43:777–786. doi: 10.1099/00207713-43-4-777. [DOI] [PubMed] [Google Scholar]
- 69.Alsmark CM, Frank AC, Karlberg EO. The louse-borne human pathogen Bartonella quintana is a genomic derivative of the zoonotic agent Bartonella henselae. Proc Natl Acad Sci USA. 2004;101:9716–9721. doi: 10.1073/pnas.0305659101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Raoult D, Birtles RJ, Montoya M. Survey of three bacterial louse-associated diseases among rural Andean communities in Peru: prevalence of epidemic typhus, trench fever, and relapsing fever. Clin Infect Dis. 1999;29:434–436. doi: 10.1086/520229. [DOI] [PubMed] [Google Scholar]
- 71.Bonilla DL, Kabeya H, Henn J, Kramer VL, Kosoy MY. Bartonella quintana in body lice and head lice from homeless persons, San Francisco, California, USA. Emerg Infect Dis. 2009;15:912–915. doi: 10.3201/eid1506.090054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Angelakis E, Raoult D. Pathogenicity and treatment of Bartonella infections. Int J Antimicrob Agents. 2014;44:16–25. doi: 10.1016/j.ijantimicag.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 73.Kernif T, Leulmi H, Socolovschi C, Berenger JM. Acquisition and excretion of Bartonella quintana by the cat flea, Ctenocephalides felis felis. Mol Ecol. 2014;23:1204–1212. doi: 10.1111/mec.12663. [DOI] [PubMed] [Google Scholar]
- 74.Leulmi H, Bitam I, Berenger JM. Competence of Cimex lectularis bed bugs for the transmission of Bartonella quintana, the agent of trench fever. PLoS Negl Trop Dis. 2015;9:e0003789. doi: 10.1371/journal.pntd.0003789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Melter O, Arvand M, Votypka J, Hulinska D. Bartonella quintana transmission from mite to family with high socioeconomic status. Emerg Infect Dis. 2012;18:163–165. doi: 10.3201/eid1801.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li H, Bai JY, Wang LY. Genetic diversity of Bartonella quintana in macaques suggests zoonotic origin of trench fever. Mol Ecol. 2013;22:2118–2127. doi: 10.1111/mec.12261. [DOI] [PubMed] [Google Scholar]
- 77.La VD, Tran-Hung L, Aboudharam G, Raoult D, Drancourt M. Bartonella quintana in domestic cat. Emerg Infect Dis. 2005;11:1287–1289. doi: 10.3201/eid1108.050101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gerberding JL. Faster… but fast enough? Responding to the epidemic of severe acute respiratory syndrome. N Engl J Med. 2003;348:2030–2031. doi: 10.1056/NEJMe030067. [DOI] [PubMed] [Google Scholar]
- 79.Institute of Medicine . Emerging infections: microbial threats to health in the United States. National Academy Press; Washington, DC: 1991. [PubMed] [Google Scholar]
- 80.Smallman-Raynor MR, Cliff AD. War epidemics. An historical geography of infectious diseases and military conflict and civil strife, 1850–2000. Oxford University Press; Oxford: 2004. [Google Scholar]
- 81.Atenstaedt RL. The response to the trench diseases in World War I: a triumph of public health science. Public Health. 2007;121:634–639. doi: 10.1016/j.puhe.2006.12.014. [DOI] [PubMed] [Google Scholar]