Summary
The world is becoming urban. The UN predicts that the world's urban population will almost double from 3·3 billion in 2007 to 6·3 billion in 2050. Most of this increase will be in developing countries. Exponential urban growth is having a profound effect on global health. Because of international travel and migration, cities are becoming important hubs for the transmission of infectious diseases, as shown by recent pandemics. Physicians in urban environments in developing and developed countries need to be aware of the changes in infectious diseases associated with urbanisation. Furthermore, health should be a major consideration in town planning to ensure urbanisation works to reduce the burden of infectious diseases in the future.
Introduction
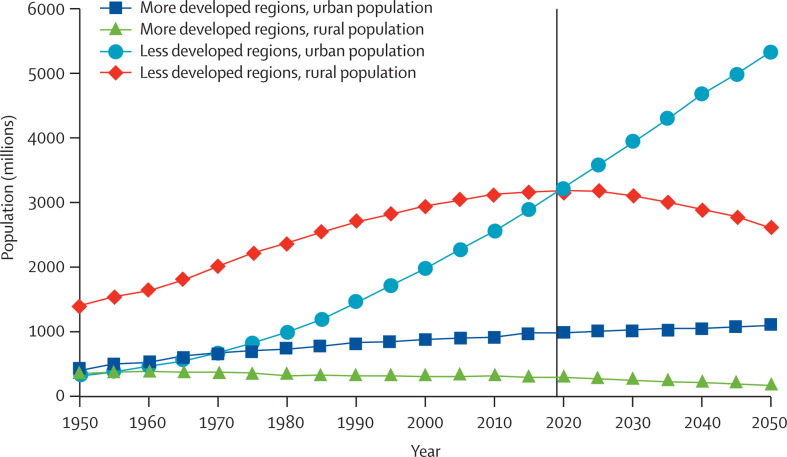
In 2009, more than 50% of the world's population were living in cities.1 Although most developed nations already show high rates of urbanisation (about 80%), tropical countries are experiencing a remarkable expansion of their urban agglomerations (figure 1 ). The population of Niamey, Niger, for example, increased from 250 000 people in the 1980s to almost 1 million today. By 2050, the world's urban population is expected to reach 6·3 billion. Almost all of this growth will be in low-income regions: in Africa the urban population is likely to triple, and in Asia it will more than double.1 Although Latin America became mostly urban in the early 1960s, sub-Saharan Africa remains mainly rural and is not expected to pass the urban tipping point before 2030.3 Although nearly half of the increase will be in small urban centres (less than 500 000 inhabitants), most mega-cities in Europe and northern America will grow by less than 0·5%. High-growth rates are expected in Lagos, Nigeria, Dhaka, Bangladesh, and Karachi, Pakistan. This worldwide increase in urban population results from a combination of factors including natural population growth, migration, government policies, infrastructure development, and other major political and economical forces, including globalisation.
Figure 1.
Evolution of urban and rural populations between 1950 and 20502
There is no universally accepted definition of what urban is. Some countries use a basic administrative definition (eg, living in the capital city); others use population measures (eg, size or density), or functional characteristics (eg, economic activities). Data are therefore difficult to extrapolate from one country to another. Moreover, there are few high-quality studies assessing urban health in tropical regions and most studies are cross-sectional. Most studies address differences between urban and rural settings and data are rarely disaggregated according to disparities within urban settings, which are therefore masked. Finally, urban growth might be driven by different forces in different cities, and the epidemiology of individual diseases might differ according to specific urban dynamics and contexts.4
In industrialised nations, urbanisation has contributed to an overall improvement of health and to a major shift in disease patterns towards a rise in chronic diseases. However, in many low-income countries, economic growth does not keep pace with the rise in urban populations. Many national and municipal governments do not have the resources to cope with the steady influx of migrants or with the explosive demographic growth of urban centres. The urban sector's share of the poor is therefore on the rise. In Sudan and Central African Republic, more than 94% of urban residents live in dismal conditions in shanty towns.5 In 2001, 924 million urban residents lived in slums and informal settlements. This number is expected to double to almost 2 billion by 2030.6 The health transition that has taken place in developed cities is still beyond reach for most low-income countries. Chronic illnesses have been increasing in importance, but infectious diseases remain a leading cause of mortality and morbidity.7, 8, 9 Furthermore, important socioeconomic disparities have emerged in urban centres mirrored by profound health inequalities.9, 10 Urbanisation of low-income countries raises new health challenges for the international community.9
Several rural pathogens have adapted to urban environments and others have emerged or re-emerged in urban areas. The heterogeneity in health of urban dwellers, increased rates of contact, and mobility of people, results in a high risk of disease transmission in large urban populations. Cities become incubators where all the conditions are met for outbreaks to occur. Although poor urban areas are typically affected first, infections have the potential to rapidly propagate to other parts of the city, including wealthy neighbourhoods and tourist areas. Additionally, in an interconnected world, cities become gateways for the worldwide spread of infections. These issues have substantial public-health implications, reshaping the epidemiology of both chronic and infectious diseases, with consequences worldwide. They also change the practice of physicians working in cities of tropical regions, and of travel doctors in developed nations. This Review will summarise how urbanisation influences the epidemiology of infectious diseases. We focus on low-income countries where most rapid urbanisation is taking place with important consequences because of the scarcity of resources.
A web of interconnected determinants
Specificities of urban populations
The close proximity of people is a prominent urban factor. The world's densest cities are in Asia, and with almost 30 000 inhabitants per km2, Mumbai, India leads the way. Population density affects diseases, particularly those transmitted via respiratory and faecal–oral routes. Because of high-population density, an increased amount of shared airspace increases exposure to influenza, measles, and Mycobacterium tuberculosis. Urban centres usually have higher rates of tuberculosis infection than do rural areas.11 In impoverished suburban areas of Karachi, Pakistan, the prevalence of pulmonary tuberculosis is 329 per 100 000 people, much higher than the prevalence of 171 per 100 000 that was reported by Pakistan national statistics.12 Densely populated cities also provide favourable grounds for the spread of emerging diseases, as shown by the severe acute respiratory syndrome or the recent H1N1 influenza epidemics. Careful urban planning is crucial to restrict household overcrowding, and the provision of parks and open spaces relieves congestion.
In most low-income countries, urban expansion is due to natural population growth. However, migration of people from other urban centres or from rural areas contributes substantially to the growth of cities.1 Economic migration and forced displacement can contribute to population movements. In Amman, Jordan, at least 500 000 of the 2 million inhabitants have moved to the city seeking refuge from conflict or disaster.3 For urban growth, migration is generally more important in nations with low rates of natural increase. In China for example, the floating population of rural migrants moving to coastal cities is about 120 million. Large population movements are also occurring between cities, notably in Latin America and the Caribbean. In São Paulo, Brazil, a third of all urban growth can be attributed to migration from other cities.9 Migration affects the transmission of communicable diseases in several ways. First, cities might provide favourable conditions for the spread of germs that are imported by migrants. Schistosomiasis has established itself in urban areas most probably through infected migrants.13 The snail intermediate host of Schistosoma spp is present in urban water bodies, and endemic foci occur in large cities such as in Bamako, Mali, Dar el Salam, Tanzania, and Kampala, Uganda.14, 15, 16 Second, migrants who are infected might also increase the transmission of a disease that is already present in a city. In Kinshasa, Democratic Republic of Congo, the massive inflow of internally displaced persons from provinces where African trypanosomiasis is endemic, contributed to an increase of ten times in the number of cases reported.17 Finally, rural migrants travelling from non-endemic areas might also change the epidemiology of infectious diseases already present in cities. Many newcomers do not have the specific immunity for these diseases and are more susceptible to infections and more likely to develop severe forms than are residents.18, 19 Naive migrants also contribute to the spread of latent forms of the disease. In Kabul, Afghanistan, where cutaneous leishmaniasis is endemic, most of the population become infected and immune in early life. Since 1987, rural-to-urban population movements have substantially increased the risk of transmission among newcomers, and the spread of this disease has reached epidemic proportions.20
The physical environment of cities
According to WHO, almost 137 million people in urban populations have no access to safe drinking water, and more than 600 million urban dwellers do not have adequate sanitation.21 The situation is particularly alarming in congested cities of sub-Saharan Africa (figure 2 ). In Nigeria for example, only 3% of residents from Ibadan have access to piped water, and in Greater Lagos, only 9% of its 10 million residents have access.4 Unsafe water sources and inadequate sanitation and hygiene are prime contributors to diarrhoeal infections and might lead to cholera endemicity.22 The overall prevalence of diarrhoea can be very high in cities as shown by data from northern Jakarta, Indonesia, where prevalence is 50 per 1000 people.23 Inadequate sanitation also affects the transmission of soil-transmitted helminthiasis and intestinal parasites. Several surveys23, 24, 25, 26, 27 show a high prevalence of intestinal parasites among children—for example, 52·8% in Karachi, Pakistan.27 Finally, absence of sewerage systems can lead to the proliferation of rodents, as in El Salvador's slums, where rats carrying Leptospira interrogans proliferate.28 During the rainy season, open-drainage gutters tend to overflow, flooding streets and adjacent homes, and triggering outbreaks of leptospirosis.29, 30 Solutions to the urban transmission of water-borne diseases include improved water access, quality, and sanitation, and the promotion of personal hygiene practice. If continued political and financial commitment is made, these interventions might result in a high return on investment.31 In Beijing and Chongqing, China, alliances of several stakeholders were established to address long-term sustainability of urban water cycles. The doubling of Chongqing's population between 1995 and 2003 has resulted in water scarcity and serious environmental degradation. Recycling of waste water and initiatives for harvesting rainwater are under development.32
Figure 2.
A slum of Kibera
Dwellers of slums live in dire, overcrowded environments, with no access to water or sanitation. In the slum of Kibera, Kenya the number of inhabitants is almost 1 million.
© 2011 Manoocher Deghati (www.irinnews.org)
Urbanisation also creates an increasing problem for the management of solid waste. The Asian Development Bank estimates that the waste quantities generated by Indian cities will increase from 46 million tonnes in 2001, to 65 million tonnes in 2010. In rural areas, most waste is reused as compost, burnt, or recycled to meet daily needs. In cities, this is rarely possible, and when municipal services are deficient, waste piles up in empty lots and street sides, leading to soil, air, and water pollution. This pollution might increase the prevalence of diarrhoeal and intestinal parasitic infections.33, 34 Accumulated waste can also be a breeding site for vectors. Phlebotomine sandflies—the main vectors for leishmania parasites—breed in organic waste from human beings and domestic animals. In Teresina, Brazil, the risk of contracting visceral leishmaniasis is six times higher for people living in houses with no regular rubbish collection than for people with regular rubbish collection.35 Aedes spp mosquitoes, which are vectors for dengue, yellow fever, and chikungunya, have adapted well to the urban environment and often breed in cans, plastic bottles, and tyres.36, 37 Accumulated waste also favours the swarming of rodents. The epicentre for plague outbreaks in Mahajanga, Madagascar, is a densely populated area including two large markets, which generate the town's largest amount of rubbish.38
Housing conditions are commonly better than in rural areas, with concrete floors and walls rather than houses built with leaves and mud. In many low-income countries, however, poor residents of slums generally build their own dwellings from flimsy, scrounged materials and with no concern for vector hygiene. In the suburbs of Arequipa, Peru, about half of the houses are infested with Triatoma infestans, which transmits Trypanosoma cruzi.39 Infestans were also found in peri-urban areas of Cochabamba, Bolivia.40 However, several municipalities have deployed large-scale efforts to upgrade shantytowns and other impoverished areas. A government programme in Mexico to replace dirt floors with cement floors in Mexico City led to a 78% reduction in parasitic protozoa infestations and a 49% reduction in diarrhoea among children.41
Social disparities drive health inequities in urban settings
Many social determinants interact to define individual exposure and vulnerability to disease.42 In urban settings, the most substantial factors include socioeconomic status, place of residence, race, ethnicity, gender, and education.43 Urbanisation contributes to economic growth and is generally a positive factor in overall poverty reduction. Cities provide opportunities for many rural migrants who are attracted by greater job prospects and higher salaries than those found in rural areas. Improved socioeconomic status results in improved health and health conditions are on average better in urban areas than in rural areas. However, in most cities in low-income countries, high inequities in economic, social, and living conditions are often noted, which are often mirrored by inequalities in health (figure 3 ).8, 44 In cities in Brazil, low income, unemployment, and material deprivation are associated with an increased risk of dengue, schistosomiasis, and leptospirosis.45, 46, 47, 48 In addition to individual-level factors, the socioeconomic characteristics of neighbourhoods also matter, and slum dwellers and informal settlers are the most vulnerable groups.42 In El Salvador, Brazil, the risk of acquiring severe leptospirosis is four times higher for residents of favelas than for other residents.30, 49 Similarly, education levels are higher on average in urban centres than in rural areas. Furthermore, urban residents have better access to mass media and are more exposed to campaigns for disease prevention. Knowledge and skills attained through education make people more receptive to health education. For example, knowledge of HIV and AIDS is better in many cities than in rural areas, and urban dwellers generally use condoms more frequently.50 In urban Bangladesh, access to education and mass media are among the strongest predictors of health outcomes in women.51 Educated mothers are more aware of the importance of breast feeding, immunisation, and simple hygienic measures;52 but huge intraurban disparities persist. A study comparing rural, urban, and slum residents in India, found that literacy rates were higher in rural areas (80·6% literacy) and other urban areas (94·3%) than in slums (65·3%). Immunisation coverage, contraceptive use, and antenatal care were poorer in slums than in other urban districts.53
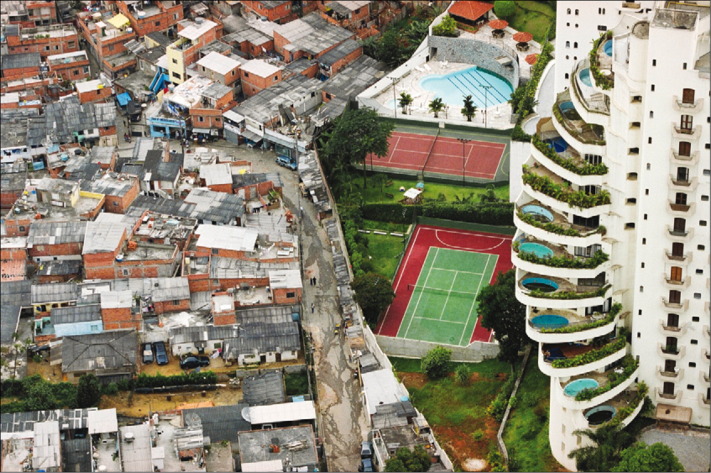
Figure 3.
Socioeconomic disparities in Paraisopolis, Sãu Paulo
The urban environment is characterised by important socioeconomic disparities and geographical heterogeneity. In Paraisopolis, São Paulo, Brazil, high-income housing is just two steps away from the favela shacks.
© 2011 Tuca Vieiria
Socioeconomic disparities also determine differential access to, and use of health care, with a substantial effect on prevention, treatment, and survival. In the city of Chandigarh, India, despite the presence of tertiary-care hospitals, multispeciality hospitals, and a network of public dispensaries and private clinics, coverage indicators for reproductive and child health are inferior in impoverished neighbourhoods.53 In the slums of Nairobi, Kenya, tumbledown, private-owned, and unlicensed clinics might be the only health facilities to which residents have access.54 Access to vaccination is also an issue for poorer urban residents, and in sub-Saharan Africa, rapid rates of urbanisation are associated with negative outcomes in access to vaccination.55 Differential access to medication might result in the emergence of resistance in the urban environment, (eg, malaria resistance to chloroquine56). The number of cases of multidrug-resistant (MDR) tuberculosis is also rapidly increasing in several cities.57 For Baku, Azerbaijan, this increase is particularly daunting: among newly diagnosed cases of tuberculosis, the proportion of single-drug resistant and MDR tuberculosis are 56·3% and 22·3%, respectively. Surveys have also reported alarming rates of MDR tuberculosis in Tashkent, Uzbekistan, Mumbai, India, Dhaka, Bangladesh, and Cape Town, South Africa.57, 58, 59
Finally, the urban environment results in many changes in human behaviour that affect transmission risks, in particular, for sexually transmitted diseases. Decreased social cohesion, new family structures, and the relaxation of traditional cultural norms yield new patterns of behaviour, including changes in sexual activity and the use of drugs.60, 61 Young people are particularly at risk. In Kampala, Uganda, a survey done among adolescents showed that 20·6% of the girls and 13·2% of the boys had at least one sexually transmitted disease.62 Migrants are also a particularly vulnerable group, because they are often young, single, and living away from their relatives. The 120 million migrants of China have been identified as the tipping point for the country's AIDS epidemic and several reports have underlined the high prevalence of high-risk sexual behaviours among this floating population.63, 64, 65, 66, 67 Risk perception about sexually transmitted diseases and HIV and AIDS is profoundly changed in rural-to-urban migrant populations;64, 65 however, the link between health behaviour and transmission of sexually transmitted diseases remains complex. A study comparing behaviours in Cotonou, Benin, Yaoundé, Cameroon, Kisumu, Kenya, and Ndola, Zambia, found that high-risk sexual behaviour was not more common in cities with the highest HIV prevalences than in others.68 Furthermore, some studies show that the sexual behaviour of young adults might be more high-risk in rural areas than in cities.69, 70
Important infectious diseases in tropical urban environments
Several infectious diseases have emerged or re-emerged in urban areas.71 Some that were traditionally thought of as rural, have adapted to the urban environment and are now common in cities. Others have acquired the potential to start sudden epidemics. However, urban development has also reduced the transmission of other diseases. Because tuberculosis10, 58, 59, 72, 73, 74 and HIV50, 75 transmission have already been documented elsewhere, these diseases, though of primary importance, are not discussed here.
When rural diseases turn urban
Several of the neglected tropical diseases that were once most common in rural, remote areas, are now frequently found in cities. Leishmaniasis is a growing health problem, and rapid urbanisation contributes to this increase.76 In several cities, the numbers have exploded: in Kabul, Afghanistan, cases of cutaneous leishmaniasis increased from 14 200 in 1994, to 65 000 in 2002, and in Ouagadougou, Burkina Faso, the incidence of cutaneous leishmaniasis increased from 28 cases in 1995, to 2375 in 2000.77 Visceral leishmaniasis has become an important issue in several Latin American cities including Teresina, Belo Horizonte, São Luis, and Salvador de Bahia in Brazil.78, 79 Several processes contributed to the urbanisation of this disease. First, rapid urban expansion might bring populations into contact with zoonotic cycles established in adjacent rural areas. For example, cutaneous leishmaniasis has established itself in the periphery of Manaus, Brazil, Bella Vista, Argentina, Marrakech, Morocco, and Khartoum, Sudan.80, 81, 82, 83 Second, migrations have probably contributed to the urbanisation of visceral leishmaniasis. In northeast Brazil, prolonged droughts have triggered massive population movements towards the outskirts of large cities. Rural migrants settled in shantytowns and brought chickens, pigs, and dogs with them, creating ideal conditions for the proliferation of sandflies and for the establishment of an urban transmission cycle.76 Similarly, the emergence of visceral leishmaniasis in Khartoum in 1988 likely resulted from the influx of people from western Upper Nile province, southern Sudan, who had fled the civil war in the south.84 Finally, poor sanitary conditions and changes in vector ecology also contributed substantially to the spread of visceral leishmaniasis, and high numbers of sandflies were recorded in several cities.35, 85, 90
Chagas disease, the American trypanosomiasis, caused by the protozoan parasite cruzi, affects 8 million to 10 million people every year.91 This disease is transmitted by triatomine bugs that hide in wall cracks and thatched roofs of rural households. Chagas disease has long been thought of as a disease of rural areas, but several reports suggest the existence of transmission foci in urban and periurban areas. In 1996, a seroepidemiological survey in Cochabamaba, Bolivia, found anti-T-cruzi antibodies in 12·5% of the inhabitants.40 Another survey showed that 22% of children from Cochabamba aged 5–13 years were seropositive for T-cruzi infection.92 In poor suburbs of Arequipa, Peru, of the 397 households surveyed, 194 (52%) were infested with triatomines, and 72 (19·3%) harboured insects that were infected with T cruzi.39 In urban settings, T cruzi can also be transmitted via blood transfusion or organ transplants. In Latin American cities between 1980 and 1989, 1·3–51·0% of blood units intended for transfusion were infected with T cruzi.93 Rural-to-urban migrants have probably played an important part in the establishment of Chagas disease in cities by transporting vectors from endemic rural areas to the peripheries of towns where they usually settle. Triatomine bugs were detected in Buenos Aires and San Juan, Argentina, in Heredia, Costa Rica, and in Cuernavaca, Mexico.94, 95, 96, 97 Vector proliferation is associated with poor socioeconomic conditions, poor housing, and the presence of domestic animals in and around houses.39 Other neglected tropical diseases have adapted to the urban environment. Among the 1·2 billion people at risk of lymphatic filariasis, about 29% live in urban settings.98 In poor neighbourhoods in Nigeria, Brazil, and India, mismanagement of waste water, absence of sewer systems, and accumulation of waste promote the proliferation of Wuchereria bancrofti vectors and increase biting rates.99, 100, 101, 102
The looming threat of explosive urban epidemics
The urban environment offers favourable grounds for the spread of epidemics, mainly because of high-population densities. Some diseases, such as dengue, have become permanently established in urban areas and cause regular epidemics, while others, like Ebola in Kikwit, Democratic Republic of Congo, in 1995, or Marburg haemorrhagic fever in Angola in 2005, might produce occasional, patchy outbreaks. Epidemic forms of certain diseases, such as chikungunya, might become restricted to the urban environment.103 In Africa, despite several decades of relative inactivity, outbreaks of yellow fever have occurred since the mid 1980s, sometimes involving tens of thousands of cases.104 Interruption of immunisation programmes, population movements, and urbanisation all partly account for the spread of this virus. In several endemic countries, rapid urban growth has resulted in non-immune populations being concentrated in overcrowded slums that are swarming with Aedes spp mosquitoes. Several densely-populated cities are near areas of enzootic activity, and the risk of large and uncontrollable outbreaks is looming.105 Since 2000, west Africa has had several urban epidemics: Abidjan, Côte d'Ivoire, in 2001 and 2008, Dakar and Touba, Senegal, in 2002, and Bobo-Dioulasso, Burkina Faso, in 2004.106, 107, 108 In South America, re-emergence of urban yellow fever might also occur in the near future, particularly in densely populated coastal regions where most of the population is not vaccinated.109 The 2008 re-emergence of yellow fever in Paraguay was almost an urban outbreak.
Dengue fever is mainly an urban disease that has been associated with sudden epidemics in tropical and subtropical regions. The geographical distribution of dengue has increased substantially in the past 30 years, and it is now endemic in more than 100 countries.110 About 50 million infections occur every year, including 400 000 cases of dengue haemorrhagic fever. The incidence of dengue has increased greatly in south Asian cities. In 2007, Indonesia reported 127 687 cases of dengue fever, 25 000 of which were in Jakarta.111 Epidemics of dengue fever and dengue haemorrhagic fever start in major cities and spread geographically outwards to rural areas.112 Low-herd immunity, high-population density, increased mobility, air travel, and ineffective control programmes are thought to have contributed to the re-emergence of the virus in south Asia. Unplanned urbanisation has also been central to the re-emergence of dengue fever in the Americas.113 The epicentre of the epidemic that affected Brazil between January, and April, 2008, was in Rio de Janeiro and resulted in more than 120 000 reported cases, including 647 cases of dengue haemorrhagic fever and 48 deaths.
When urbanisation curtails transmission
There are several examples of urban growth triggering the decline of infectious diseases. Air and water pollution, which exist in many cities, can hinder vector proliferation. A study examining phlebotomine proliferation in Marrakech, showed that urbanisation generally decreased sandfly populations.114 Although most anopheline species do not tolerate polluted waters, some have adapted to contaminated waste water.115, 116, 117, 118, 119 Evidence for transmission of malaria has been found in most cities in sub-Saharan Africa, but levels of transmission are generally lower in urban areas than in rural areas.120, 121 Estimates predict that among the 0·6 billion people from Africa who are at risk of malaria, about 200 million are urban dwellers.122 In urban environments, anopheline vectors are less abundant and less likely to be infected with Plasmodium spp. Furthermore, urban dwellers experience reduced biting rates. Destruction of vector habitats, improved housing conditions, and improved access to preventive and curative measures all partly account for this decreased transmission. However, substantial variations in malaria transmission exist in different areas of the same city, thus reflecting disparities in environmental conditions and population dynamics.123 A survey done in Ouagadougou, Burkina Faso, showed that the prevalence of parasitaemia among school children varied between 24·1% in the centre, and 68·7% in peripheral areas.124 Urban transmission is usually remarkably focal and occurs in the vicinity of Anopheles spp breeding sites.125 In particular, urban farming might promote high densities of mosquitoes and increase transmission of malaria in specific areas.126, 127
Hepatitis A is another example of the positive effect that cities can have on transmission of infectious diseases. Hepatitis A is typically a disease of the poor, its prevalence being closely related to socioeconomic status, hygiene, and living conditions. In most low-income countries, exposure to hepatitis A virus is thought to be universal before age 10 years.128, 129, 130 However, in several countries, improvements in sanitation and public-health programmes have shifted the epidemiological pattern of hepatitis A viral infection, with exposure to the virus occurring at a later age.131, 132 This shift is particularly evident in urban areas, where improved socioeconomic status is generally accompanied by a decline in the prevalence of hepatitis A. For example, over the past 30 years, there has been a substantial decrease in hepatitis A infections in Singapore, and a 50% drop in the seroprevalence of hepatitis A antibodies since 1975.131 About 10 years ago, hepatitis A was viewed as an important health issue in Hong Kong, causing 67–83% of all notified cases of viral hepatitis.133 However, the number of notified cases showed a decrease of ten times since the 1990s, with 63 cases reported in 2005.134
Highly interconnected urban hubs: a catalyst to the spread of diseases
Global travel has changed substantially in the past 30 years, with ever-escalating speed, distance, and volume. According to the World Tourism Organization, international tourist arrivals increased from 25·3 million in 1950, to 924 million in 2008; an astounding increase of 36 times. Increased mobility has provided new opportunities for emerging diseases, such as for severe acute respiratory syndrome or chikungunya, particularly in cities, which constitute entry points for most travellers.135 Air travel and increased mobility have been central to the large and rapid outbreaks of chikungunya that occurred in cities of the Indian Ocean between 2005 and 2006. These epidemics involved genetically similar viruses, suggesting unique viral spreading, probably originating from southeast Africa.136 Urban epidemics can reach unprecedented scales and quickly become uncontrollable. The 2009 influenza A H1N1 pandemic shows how fast infections can spread worldwide. In African cities, where disease surveillance of human beings and animals is weak, movement is not effectively managed, and health-care systems are overtaxed by AIDS, tuberculosis, and malaria, the control of influenza viruses will be especially problematic.137
The changing epidemiology of diseases in the urban environment, combined with the increased global mobility of travellers and migrants, can also change the practice of physicians. Patients with unfamiliar diseases may consult physicians who are unaware of the existence of some imported diseases. With the arrival of migrants from Latin America, Chagas disease should be recognised and patients coming from endemic areas should be screened. Because cities are becoming major travel destinations, physicians should be informed about ongoing epidemics of yellow fever, the geographical expansion of dengue or chikungunya, and the existence of leishmaniasis or rabies in the cities visited by travellers. Additionally, the risks to visiting friends and relatives might change because of urbanisation, as shown by the reduction in malaria incidence in the UK.138 Prevention measures are summarised in the table . Furthermore, the rapid modernisation and advertising of large cities in emerging economies change how travellers perceive risks. Because most travellers are urban dwellers themselves, they tend to underestimate the risks related to the heterogeneity of cities. Large gatherings like the Olympic Games and the football World Cup now take place in countries such as China, South Africa, or Brazil. There are risks inherent to these events, such as the spread of diseases like measles or influenza; additionally, endemic diseases still persist, posing risks to travellers. This risk is particularly so if they combine a visit to rural areas in which conditions are very different from the better standards of the cities where events take place. The epidemiological transition in cities and the changes in the perception of risk by travellers visiting them oblige specialists in travel medicine to adjust their recommendations frequently.
Table.
Examples of preventive measures for diseases that have a modified epidemiology because of urban determinants
| Preventive measures for the community | Preventive measures for urban travellers | |
|---|---|---|
| Water-borne diseases | ||
| Bacterial dysentery, hepatitis A, cholera | Improvement of water supply, sanitation, and sewage systems | Food and water precautions Vaccination (hepatitis A and cholera) |
| Vector-borne diseases | ||
| Dengue; chikungunya | Promotion of actions to remove larval habitats of mosquito vectors | Protection against mosquito bites |
| Malaria | Elimination of mosquito breeding sites, use of mosquito nets, and indoor residual spraying with insecticides | Protection against mosquito bites Prophylactic drug |
| Leishmaniasis | According to the species: vector control, ±control of mammalian hosts | Protection against sandfly bites |
| Lymphatic filariasis | Elimination of mosquito breeding sites | Protection against mosquito bites |
| African trypanosomiasis | Reduction of the tsetse fly population Diagnosis and treatment of people who are infected |
Avoidance of affected regions Protection against tsetse fly bites |
| Chagas disease | Vector control (insecticide spraying) and housing improvement | Not sleeping in precarious dwellings Bednets |
| Yellow fever | Vector control Vaccination |
Vaccination Protection against mosquito bites |
| Plague | Improvement of waste management | Protection against flea bites |
| Leptospirosis | Improvement of sewerage systems and waste management | Avoidance of direct and indirect contact with animal urine |
| Air-borne diseases | ||
| Tuberculosis | Early diagnosis and treatment of patients who are infectious Reduction of social situations that increase the risk of infection |
Avoidance of exposure to patients with known tuberculosis in crowded environments |
| Pneumonia | Reduction of atmospheric pollution | |
| Sexually transmitted diseases | ||
| HIV | Health education in the public and in schools Access to condoms and treatment |
Condoms Avoidance of use of unsterilised material (eg, for medical and dental procedures, or tattooing) and blood products |
Conclusion: opportunities for action
Urbanisation increasingly affects the epidemiological characteristics of infectious diseases. Depending on the pace, dynamics, and environment, urbanisation can either promote or hinder the spread of pathogens. In most developed cities, better living conditions, improvement of domestic hygiene, and targeted public-health interventions started the decline of infectious illnesses. In parallel, chronic diseases have progressed because of changes in lifestyle, population ageing, and improvement in the diagnostic capacities of health services. Several agglomerations in developing countries seem to be on track for this epidemiological transition.6, 7 However, uncontrolled urban growth has also resulted in large health inequities and in increases in the transmission of infectious diseases. In cities, numerous resources are present, and political power, money, and knowledge are concentrated. Urban centres offer incredible opportunities for disease surveillance, control, and prevention that are absent in rural areas. Well-planned strategies for vector control have enabled cities to eliminate malaria and dengue, and city-wide housing and sanitation programmes have shown spectacular effects.124, 139, 140 Additionally, higher levels of social cohesion, the presence of community-based organisations that mobilise populations and advocate for resources, and access to media and modern communication allow urban residents to have increased visibility and a stronger political voice than their rural counterparts.141
The improvement of local capacities to identify, control, and prevent communicable diseases that have the potential to spread widely is of international interest. Surveillance is of primary importance, and changes in public health strategies can have substantial consequences. In Singapore, the re-emergence of dengue is partly a result of decreased vector surveillance and a shift towards case detection in the late 1980s.140 Through use of the International Health Regulations, WHO has the mandate to help nations improve their surveillance and response capacities, with a substantial local, national, and international effect. Clearly a comprehensive global approach to disease surveillance, control, and prevention is increasingly needed.135 Conventional health strategies should be adapted according to the dynamics of urbanisation and to the distinctive epidemiological pattern of transmittable diseases in cities. Increased public spending on health and provision of technical assistance will certainly not suffice to curtail the urban expansion of communicable diseases. Rather, the solution is in sensible planning of the expansion of cities, and depends on policy interventions at the community, municipal, national, and worldwide level.142, 143
Whenever possible, local governments should incorporate health concerns into urban policies, such as economic promotion and community development. The Healthy Cities programme is a trans-sectoral approach that showed excellent results. In Marikina, Philippines, the combination of riverside clean-up campaigns, improvements in waste-management services, health education, and resettlement programmes resulted in a sharp decrease of dengue infections.141 In South Africa, the Cape Town Equity Gauge was established in 2002 in response to health inequities throughout the city. This collaborative initiative involved reallocation of health staff, health-promotion programmes in schools, and a pilot implementation of dry-sanitation toilets in informal settlements.144 Controlled and thoughtful urbanisation can produce substantive economic and health returns, both at the individual city level, and worldwide.142 Benefits include increased life expectancy, improved health during childhood and during peak earning years, safer travel, preparedness for worldwide outbreaks, and containment of epidemics. Urban health should therefore be viewed as an international and worldwide issue, and appropriate resources should be allocated to reduce inequities.
Search strategy and selection criteria
We identified references through searches of PubMed between January 1975 and November 2009. We used MeSH terms “Urban Health” or “urbanization” with disease-specific terms (ie, “diarrhoea”, “intestinal diseases, parasitic”, “respiratory tract infections”, “trypanosomiasis”, “schistosomiasis”, “leishmaniasis”, “HIV”, “sexually transmitted diseases”. Additional searches of PubMed and the Cochrane Library were done with the terms “urban”, “health”, “slums”, and “infectious diseases”, and references from pertinent reviews and articles were also used. Online searches were restricted to articles in English, French, and Spanish. Duplicates were removed and only studies of tropical countries were selected. Of about 350 relevant papers, about 150 were retained. Articles were selected on the basis of relevance and quality of the methodology. Finally, websites from international organisations and from UN agencies (eg, World Bank, UN-Habitat, WHO) were searched for relevant information and reports addressing issues related to urbanisation were analysed.
Acknowledgments
Acknowledgments
We thank Jean-Claude Bolay at Ecole Polytechnique Fédérale de Lausanne for valuable input and Cynthia White for proofreading the paper.
Contributors
EA and LG did the reference search. EA wrote the article and chose the pictures. LG drew the table. FC, BS, and LL proofread and edited the Review.
Conflicts of interest
We declare that we have no conflicts of interest.
References
- 1.UN World Urbanization prospects: the 2009 revision. March, 2010. http://esa.un.org/unpd/wup/index.htm (accessed Nov 18, 2010).
- 2.UN World Urbanization prospects: the 2007 revision. February, 2008. http://www.un.org/esa/population/publications/wup2007/2007WUP_Highlights_web.pdf (accessed Nov 18, 2010).
- 3.UN-HABITAT State of the world's cities 2010/2011: bridging the urban divide. 2008. http://www.unhabitat.org/pmss/listItemDetails.aspx?publicationID=2917 (accessed Nov 18, 2010).
- 4.Satterthwaite D. The transition to a predominantly urban world and its underpinnings. 2007. http://www.iied.org/pubs/pdfs/10550IIED.pdf (accessed Nov 18, 2010).
- 5.UN-HABITAT The state of African cities. 2008. http://www.unhabitat.org/pmss/listItemDetails.aspx?publicationID=2574 (accessed Nov 18, 2010).
- 6.UN-HABITAT The challenge of slums—global report on human settlements. 2003. http://www.unhabitat.org/pmss/listItemDetails.aspx?publicationID=1156 (accessed Nov 18, 2010).
- 7.Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002–2030. Ann Trop Med Parasitol. 2006;100:481–499. doi: 10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- 8.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 9.Harpham T, Tanner M. Features and determinants of urban health status. In: Harpham T, Tanner M, editors. Urban health in developing countries. Earthscan Publications Limited; London: 1995. pp. 35–47. [Google Scholar]
- 10.UN-HABITAT State of the world's cities 2006/2007. August, 2006. http://www.unhabitat.org/pmss/listItemDetails.aspx?publicationID=2101 (accessed Nov 18, 2010).
- 11.Lienhardt C. From exposure to disease: the role of environmental factors in susceptibility to and development of tuberculosis. Epidemiol Rev. 2001;23:288–301. doi: 10.1093/oxfordjournals.epirev.a000807. [DOI] [PubMed] [Google Scholar]
- 12.Akhtar S, White F, Hasan R. Hyperendemic pulmonary tuberculosis in peri-urban areas of Karachi, Pakistan. BMC Public Health. 2007;7:70. doi: 10.1186/1471-2458-7-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bella H, de C Marshall TF, Omer AH, Vaughan JP. Migrant workers and schistosomiasis in the Gezira, Sudan. Trans R Soc Trop Med Hyg. 1980;74:36–39. doi: 10.1016/0035-9203(80)90008-5. [DOI] [PubMed] [Google Scholar]
- 14.Dabo A, Sow MY, Sangaré L. Transmission of schistosomiasis in an urban population and prevalence of intestinal helminthiasis in Bamako, Mali. Bull Soc Pathol Exot. 2003;96:187–190. (in French). [PubMed] [Google Scholar]
- 15.Sarda RK, Simonsen PE, Mahikwano LF. Urban transmission of urinary schistosomiasis in Dar es Salaam, Tanzania. Acta Trop. 1985;42:71–78. [PubMed] [Google Scholar]
- 16.Kabatereine NB, Kazibwe F, Kemijumbi J. Epidemiology of schistosomiasis in Kampala, Uganda. East Afr Med J. 1996;73:795–800. [PubMed] [Google Scholar]
- 17.Louis FJ, Bilenge CM, Simarro PP, Meso VK, Lucas P, Jannin J. Human African trypanosomiasis in an urban area: an emerging problem? Bull Soc Pathol Exot. 2003;96:205–208. (in French). [PubMed] [Google Scholar]
- 18.Huang YX, Manderson L. The social and economic context and determinants of Schistosomiasis japonica. Acta Trop. 2005;96:223–231. doi: 10.1016/j.actatropica.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Ximenes RA, Southgate B, Smith PG, Neto L Guimarães. Migration and urban schistosomiasis. The case of São Lourenço da Mata, northeast of Brazil. Rev Inst Med Trop Sao Paulo. 2000;42:209–217. doi: 10.1590/s0036-46652000000400006. [DOI] [PubMed] [Google Scholar]
- 20.Reyburn H, Rowland M, Mohsen M, Khan B, Davies C. The prolonged epidemic of anthroponotic cutaneous leishmaniasis in Kabul, Afghanistan: ‘bringing down the neighbourhood’. Trans R Soc Trop Med Hyg. 2003;97:170–176. doi: 10.1016/s0035-9203(03)90111-8. [DOI] [PubMed] [Google Scholar]
- 21.WHO, UNICEF Progress on drinking water and sanitation: special focus on sanitation. 2008. http://www.who.int/water_sanitation_health/monitoring/jmp2008.pdf (accessed Nov 18, 2010).
- 22.Guévart E, Noeske J, Solle J, Essomba Factors contributing to endemic cholera in Douala, Cameroon. Med Trop (Mars) 2006;66:283–291. (in French). [PubMed] [Google Scholar]
- 23.Agtini MD, Soeharno R, Lesmana M. The burden of diarrhoea, shigellosis, and cholera in North Jakarta, Indonesia: findings from 24 months surveillance. BMC Infect Dis. 2005;5:89. doi: 10.1186/1471-2334-5-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oninla SO, Owa JA, Onayade AA, Taiwo O. Intestinal helminthiases among rural and urban schoolchildren in south-western Nigeria. Ann Trop Med Parasitol. 2007;101:705–713. doi: 10.1179/136485907X241406. [DOI] [PubMed] [Google Scholar]
- 25.Ekpo UF, Odoemene SN, Mafiana CF, Sam-Wobo SO. Helminthiasis and hygiene conditions of schools in Ikenne, Ogun State, Nigeria. PLoS Negl Trop Dis. 2008;2:e146. doi: 10.1371/journal.pntd.0000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wagbatsoma VA, Aimiuwu U. Sanitary provision and helminthiasis among school children in Benin City, Nigeria. Niger Postgrad Med J. 2008;15:105–111. [PubMed] [Google Scholar]
- 27.Mehraj V, Hatcher J, Akhtar S, Rafique G, Beg MA. Prevalence and factors associated with intestinal parasitic infection among children in an urban slum of Karachi. PLoS ONE. 2008;3:e3680. doi: 10.1371/journal.pone.0003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Faria MT, Calderwood MS, Athanazio DA. Carriage of Leptospira interrogans among domestic rats from an urban setting highly endemic for leptospirosis in Brazil. Acta Trop. 2008;108:1–5. doi: 10.1016/j.actatropica.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De A, Varaiya A, Mathur M, Bhat M, Karande S, Yeolekar ME. An outbreak of leptospirosis in Mumbai. Indian J Med Microbiol. 2002;20:153–155. [PubMed] [Google Scholar]
- 30.Ko AI, Reis M Galvão, Dourado CM Ribeiro, Johnson WD, Jr, Riley LW. Urban epidemic of severe leptospirosis in Brazil. Salvador Leptospirosis Study Group. Lancet. 1999;354:820–825. doi: 10.1016/s0140-6736(99)80012-9. [DOI] [PubMed] [Google Scholar]
- 31.Hutton G, Haller L. Evaluation of the costs and benefits of water and sanitation improvements at the global level. 2004. http://www.who.int/water_sanitation_health/wsh0404.pdf (accessed Nov 18, 2010). [DOI] [PubMed]
- 32.SWITCH: managing water for the city of the future. http://www.switchurbanwater.eu/index.php (accessed Oct 8, 2010).
- 33.Moraes LR. Household solid waste bagging and collection and their health implications for children living in outlying urban settlements in Salvador, Bahia State, Brazil. Cad Saude Publica. 2007;23(suppl 4):S643–S649. doi: 10.1590/s0102-311x2007001600024. (in Portuguese). [DOI] [PubMed] [Google Scholar]
- 34.Rego RF, Barreto ML, Santos R, de Oliveira NF, Oliveira S. Rubbish index and diarrhoea in Salvador, Brazil. Trans R Soc Trop Med Hyg. 2007;101:722–729. doi: 10.1016/j.trstmh.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Costa CH, Werneck GL, Rodrigues L., Jr Household structure and urban services: neglected targets in the control of visceral leishmaniasis. Ann Trop Med Parasitol. 2005;99:229–236. doi: 10.1179/136485905X28018. [DOI] [PubMed] [Google Scholar]
- 36.Hayes JM, García-Rivera E, Flores-Reyna R. Risk factors for infection during a severe dengue outbreak in El Salvador in 2000. Am J Trop Med Hyg. 2003;69:629–633. [PubMed] [Google Scholar]
- 37.Ramos MM, Mohammed H, Zielinski-Gutierrez E. Epidemic dengue and dengue hemorrhagic fever at the Texas-Mexico border: results of a household-based seroepidemiologic survey, December 2005. Am J Trop Med Hyg. 2008;78:364–369. [PubMed] [Google Scholar]
- 38.Boisier P, Rahalison L, Rasolomaharo M. Epidemiologic features of four successive annual outbreaks of bubonic plague in Mahajanga, Madagascar. Emerg Infect Dis. 2002;8:311–316. doi: 10.3201/eid0803.010250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levy MZ, Bowman NM, Kawai V. Periurban Trypanosoma cruzi-infected Triatoma infestans, Arequipa, Peru. Emerg Infect Dis. 2006;12:1345–1352. doi: 10.3201/eid1209.051662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albarracin-Veizaga H, de Carvalho ME, Nascimento EM, Rodrigues VL, Casanova C, Barata JM. Chagas disease in an area of recent occupation in Cochabamba, Bolivia. Rev Saude Publica. 1999;33:230–236. doi: 10.1590/S0034-89101999000300003. [DOI] [PubMed] [Google Scholar]
- 41.Cattaneo MD, Galiani S, Gertler PJ, Martinez S, Titiunik R. Housing, health and happiness. April, 2007. http://www-wds.worldbank.org/external/default/WDSContentServer/IW3P/IB/2007/08/28/000158349_20070828131650/Rendered/PDF/wps421401update1.pdf (accessed Nov 18, 2010).
- 42.Berkman L, Kawachi I. Social Epidemiology. Oxford University Press; New York: 2000. [Google Scholar]
- 43.Ompad DC, Galea S, Caiaffa WT, Vlahov D. Social determinants of the health of urban populations: methodologic considerations. J Urban Health. 2007;84(3 suppl):i42–i53. doi: 10.1007/s11524-007-9168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brockerhoff M, Brennan E. The poverty of cities in developing regions. Popul Dev Rev. 1998;24:75–114. [Google Scholar]
- 45.de Mattos Almeida MC, Caiaffa WT, Assuncao RM, Proietti FA. Spatial vulnerability to dengue in a Brazilian urban area during a 7-year surveillance. J Urban Health. 2007;84:334–345. doi: 10.1007/s11524-006-9154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siqueira JB, Martelli CM, Maciel IJ. Household survey of dengue infection in central Brazil: spatial point pattern analysis and risk factors assessment. Am J Trop Med Hyg. 2004;71:646–651. [PubMed] [Google Scholar]
- 47.Ximenes R, Southgate B, Smith PG, Neto L Guimarães. Socioeconomic determinants of schistosomiasis in an urban area in the Northeast of Brazil. Rev Panam Salud Publica. 2003;14:409–421. doi: 10.1590/s1020-49892003001100006. [DOI] [PubMed] [Google Scholar]
- 48.Reis RB, Ribeiro GS, Felzemburgh RD. Impact of environment and social gradient on leptospira infection in urban slums. PLoS Negl Trop Dis. 2008;2:e228. doi: 10.1371/journal.pntd.0000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Riley LW, Ko AI, Unger A, Reis MG. Slum health: diseases of neglected populations. BMC Int Health Hum Rights. 2007;7:2. doi: 10.1186/1472-698X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.UNAIDS AIDS epidemic update. December, 2006. http://data.unaids.org/pub/EpiReport/2006/2006_EpiUpdate_en.pdf (accessed Nov 18, 2010).
- 51.Khan MM, Kraemer A. Socio-economic factors explain differences in public health-related variables among women in Bangladesh: a cross-sectional study. BMC Public Health. 2008;8:254. doi: 10.1186/1471-2458-8-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kishk NA. Knowledge, attitudes and practices of women towards antenatal care: rural-urban comparison. J Egypt Public Health Assoc. 2002;77:479–498. [PubMed] [Google Scholar]
- 53.Gupta M, Thakur JS, Kumar R. Reproductive and child health inequities in Chandigarh Union Territory of India. J Urban Health. 2008;85:291–299. doi: 10.1007/s11524-007-9250-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fotso JC, Ezeh A, Oronje R. Provision and use of maternal health services among urban poor women in Kenya: what do we know and what can we do? J Urban Health. 2008;85:428–442. doi: 10.1007/s11524-008-9263-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fotso JC, Ezeh AC, Madise NJ, Ciera J. Progress towards the child mortality millennium development goal in urban sub-Saharan Africa: the dynamics of population growth, immunization, and access to clean water. BMC Public Health. 2007;7:218. doi: 10.1186/1471-2458-7-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meissner PE, Mandi G, Mockenhaupt FP. Marked differences in the prevalence of chloroquine resistance between urban and rural communities in Burkina Faso. Acta Trop. 2008;105:81–86. doi: 10.1016/j.actatropica.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 57.WHO Anti-tuberculosis drug resistance in the world: fourth global report. 2008. http://www.who.int/tb/publications/2008/drs_report4_26feb08.pdf (accessed Nov 18, 2010).
- 58.Almeida D, Rodrigues C, Udwadia ZF. Incidence of multidrug-resistant tuberculosis in urban and rural India and implications for prevention. Clin Infect Dis. 2003;36:e152–e154. doi: 10.1086/374931. [DOI] [PubMed] [Google Scholar]
- 59.Zaman K, Rahim Z, Yunus M. Drug resistance of Mycobacterium tuberculosis in selected urban and rural areas in Bangladesh. Scand J Infect Dis. 2005;37:21–26. doi: 10.1080/00365540410026095. [DOI] [PubMed] [Google Scholar]
- 60.Adler NE, Boyce T, Chesney MA. Socioeconomic status and health. The challenge of the gradient. Am Psychol. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 61.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 62.Råssjö EB, Kambugu F, Tumwesigye MN, Tenywa T, Darj E. Prevalence of sexually transmitted infections among adolescents in Kampala, Uganda, and theoretical models for improving syndromic management. J Adolesc Health. 2006;38:213–221. doi: 10.1016/j.jadohealth.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 63.Anderson AF, Qingsi Z, Hua X, Jianfeng B. China's floating population and the potential for HIV transmission: a social-behavioural perspective. AIDS Care. 2003;15:177–185. doi: 10.1080/0954012031000068326. [DOI] [PubMed] [Google Scholar]
- 64.He N, Detels R, Chen Z. Sexual behavior among employed male rural migrants in Shanghai, China. AIDS Educ Prev. 2006;18:176–186. doi: 10.1521/aeap.2006.18.2.176. [DOI] [PubMed] [Google Scholar]
- 65.Li L, Morrow M, Kermode M. Vulnerable but feeling safe: HIV risk among male rural-to-urban migrant workers in Chengdu, China. AIDS Care. 2007;19:1288–1295. doi: 10.1080/09540120701402855. [DOI] [PubMed] [Google Scholar]
- 66.Liu H, Li X, Stanton B. Risk factors for sexually transmitted disease among rural-to-urban migrants in China: implications for HIV/sexually transmitted disease prevention. AIDS Patient Care STDS. 2005;19:49–57. doi: 10.1089/apc.2005.19.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang X, Derlega VJ, Luo H. Migration, behaviour change and HIV/STD risks in China. AIDS Care. 2007;19:282–288. doi: 10.1080/09540120600909414. [DOI] [PubMed] [Google Scholar]
- 68.Auvert B, Buvé A, Ferry B. Ecological and individual level analysis of risk factors for HIV infection in four urban populations in sub-Saharan Africa with different levels of HIV infection. AIDS. 2001;15(suppl 4):S15–S30. doi: 10.1097/00002030-200108004-00003. [DOI] [PubMed] [Google Scholar]
- 69.Orubuloye O, Caldwell JC, Caldwell P. Men's sexual behaviour in urban and rural southwest Nigeria: its cultural, social and attitudinal context. Health Transit Rev. 1997;7(suppl):315–328. [PubMed] [Google Scholar]
- 70.Voeten HA, Egesah OB, Habbema JD. Sexual behavior is more risky in rural than in urban areas among young women in Nyanza province, Kenya. Sex Transm Dis. 2004;31:481–487. doi: 10.1097/01.olq.0000135989.14131.9d. [DOI] [PubMed] [Google Scholar]
- 71.Weiss RA, McMichael AJ. Social and environmental risk factors in the emergence of infectious diseases. Nat Med. 2004;10(12 suppl):S70–S76. doi: 10.1038/nm1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tornee S, Kaewkungwal J, Fungladda W, Silachamroon U, Akarasewi P, Sunakorn P. The association between environmental factors and tuberculosis infection among household contacts. Southeast Asian J Trop Med Public Health. 2005;36(suppl 4):221–224. [PubMed] [Google Scholar]
- 73.Tupasi TE, Radhakrishna S, Quelapio MI. Tuberculosis in the urban poor settlements in the Philippines. Int J Tuberc Lung Dis. 2000;4:4–11. [PubMed] [Google Scholar]
- 74.Kyobutungi C, Ziraba AK, Ezeh A, Yé Y. The burden of disease profile of residents of Nairobi's slums: results from a demographic surveillance system. Popul Health Metr. 2008;6:1. doi: 10.1186/1478-7954-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ambert C, Jassey K, Thomas L. Beyond sex and medicines: why getting the basics right is part of the response! HIV, Aids and urban development issues in sub-Saharan Africa. February, 2007. http://web.wits.ac.za/NR/rdonlyres/EAF81477-F895-44C3-9CDA-7BC981098936/0/B68.pdf (accessed Nov 18, 2010).
- 76.Desjeux P. The increase in risk factors for leishmaniasis worldwide. Trans R Soc Trop Med Hyg. 2001;95:239–243. doi: 10.1016/s0035-9203(01)90223-8. [DOI] [PubMed] [Google Scholar]
- 77.Desjeux P. Leishmaniasis: current situation and new perspectives. Comp Immunol Microbiol Infect Dis. 2004;27:305–318. doi: 10.1016/j.cimid.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 78.Costa CH, Pereira HF, Araújo MV. Visceral leishmaniasis epidemic in the State of Piauí, Brazil, 1980–1986. Rev Saude Publica. 1990;24:361–372. doi: 10.1590/s0034-89101990000500003. (in Portuguese). [DOI] [PubMed] [Google Scholar]
- 79.Oliveira CD, Assunção RM, Reis IA, Proietti FA. Spatial distribution of human and canine visceral leishmaniasis in Belo Horizonte, Minas Gerais State, Brasil, 1994–1997. Cad Saude Publica. 2001;17:1231–1239. doi: 10.1590/s0102-311x2001000500023. [DOI] [PubMed] [Google Scholar]
- 80.Moroccan Ministry of Health. Programme de lutte contre les leishmanioses. Préfecture de Marrakech. 2004. Plan d'Action Préfectoral 2005. Rabat: Morocco.
- 81.Barrett TV, Senra MS. Leishmaniasis in Manaus, Brazil. Parasitol Today. 1989;5:255–257. doi: 10.1016/0169-4758(89)90258-5. [DOI] [PubMed] [Google Scholar]
- 82.el-Safi SH, Peters W. Studies on the leishmaniases in the Sudan. 1. Epidemic of cutaneous leishmaniasis in Khartoum. Trans R Soc Trop Med Hyg. 1991;85:44–47. doi: 10.1016/0035-9203(91)90151-n. [DOI] [PubMed] [Google Scholar]
- 83.Salomón OD, Sosa-Estani S, Ramos K. Tegumentary leishmaniasis outbreak in Bella Vista City, Corrientes, Argentina during 2003. Mem Inst Oswaldo Cruz. 2006;101:767–774. doi: 10.1590/s0074-02762006000700010. [DOI] [PubMed] [Google Scholar]
- 84.de Beer P, el Harith A, Deng LL, Semiao-Santos SJ, Chantal B, van Grootheest M. A killing disease epidemic among displaced Sudanese population identified as visceral leishmaniasis. Am J Trop Med Hyg. 1991;44:283–289. doi: 10.4269/ajtmh.1991.44.283. [DOI] [PubMed] [Google Scholar]
- 85.Costa CH. Characterization and speculations on the urbanization of visceral leishmaniasis in Brazil. Cad Saude Publica. 2008;24:2959–2963. doi: 10.1590/s0102-311x2008001200027. [DOI] [PubMed] [Google Scholar]
- 90.Silva EA, Andreotti R, Dias ES, Barros JC, Brazuna JC. Detection of Leishmania DNA in phlebotomines captured in Campo Grande, Mato Grosso do Sul, Brazil. Exp Parasitol. 2008;119:343–348. doi: 10.1016/j.exppara.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 91.Remme JHF, Feenstra P, Lever PR. Tropical diseases targeted for elimination: Chagas disease, lymphatic filariasis, onchocerciasis, and leprosy. In: Jamison DT, Breman JG, Measham AR, editors. Disease control priorities in developing countries. The World Bank and Oxford University Press; New York: 2006. pp. 433–449.http://www.who.int/management/referralhospitals.pdf (accessed Nov 18, 2010). [Google Scholar]
- 92.Medrano-Mercado N, Ugarte-Fernandez R, Butrón V. Urban transmission of Chagas disease in Cochabamba, Bolivia. Mem Inst Oswaldo Cruz. 2008;103:423–430. doi: 10.1590/s0074-02762008000500003. [DOI] [PubMed] [Google Scholar]
- 93.Schmuñis GA. Trypanosoma cruzi, the etiologic agent of Chagas' disease: status in the blood supply in endemic and nonendemic countries. Transfusion. 1991;31:547–557. doi: 10.1046/j.1537-2995.1991.31691306255.x. [DOI] [PubMed] [Google Scholar]
- 94.Gajate P, Pietrokovsky S, Abramo Orrego L, et al. Triatoma infestans in Greater Buenos Aires, Argentina. Mem Inst Oswaldo Cruz 200; 96: 473–77. [DOI] [PubMed]
- 95.Vallvé SL, Rojo H, Wisnivesky-Colli C. Urban ecology of Triatoma infestans in San Juan, Argentina. Mem Inst Oswaldo Cruz. 1996;91:405–408. doi: 10.1590/s0074-02761996000400003. [DOI] [PubMed] [Google Scholar]
- 96.Zeledon R, Calvo N, Montenegro VM, Lorosa ES, Arevalo C. A survey on Triatoma dimidiata in an urban area of the province of Heredia, Costa Rica. Mem Inst Oswaldo Cruz. 2005;100:507–512. doi: 10.1590/s0074-02762005000600002. [DOI] [PubMed] [Google Scholar]
- 97.Ramsey JM, Alvear AL, Ordoñez R. Risk factors associated with house infestation by the Chagas disease vector Triatoma pallidipennis in Cuernavaca metropolitan area, Mexico. Med Vet Entomol. 2005;19:219–228. doi: 10.1111/j.0269-283X.2005.00563.x. [DOI] [PubMed] [Google Scholar]
- 98.Erlanger TE, Keiser J, De Castro M Caldas. Effect of water resource development and management on lymphatic filariasis, and estimates of populations at risk. Am J Trop Med Hyg. 2005;73:523–533. [PubMed] [Google Scholar]
- 99.Maciel A, Rocha A, Marzochi KB. Epidemiological study of bancroftian filariasis in Recife, northeastern Brazil. Mem Inst Oswaldo Cruz. 1996;91:449–455. doi: 10.1590/s0074-02761996000400011. [DOI] [PubMed] [Google Scholar]
- 100.Medeiros Z, Alves A, Brito JA. The present situation regarding lymphatic filariasis in Cabo de Santo Agostinho, Pernambuco, Northeast Brazil. Rev Inst Med Trop Sao Paulo. 2006;48:263–267. doi: 10.1590/s0036-46652006000500005. [DOI] [PubMed] [Google Scholar]
- 101.Sharma S, Sharma M, Rathaur S. Bancroftian filariasis in the Varanasi region of north India: an epidemiological study. Ann Trop Med Parasitol. 1999;93:379–387. doi: 10.1080/00034989958375. [DOI] [PubMed] [Google Scholar]
- 102.Terranella A, Eigiege A, Gontor I. Urban lymphatic filariasis in central Nigeria. Ann Trop Med Parasitol. 2006;100:163–172. doi: 10.1179/136485906X86266. [DOI] [PubMed] [Google Scholar]
- 103.Pialoux G, Gaüzère BA, Jauréguiberry S, Strobel M. Chikungunya, an epidemic arbovirosis. Lancet Infect Dis. 2007;7:319–327. doi: 10.1016/S1473-3099(07)70107-X. [DOI] [PubMed] [Google Scholar]
- 104.Robertson SE, Hull BP, Tomori O, Bele O, LeDuc JW, Esteves K. Yellow fever: a decade of reemergence. JAMA. 1996;276:1157–1162. [PubMed] [Google Scholar]
- 105.WHO Yellow fever in Africa and South America, 2006. Wkly Epidemiol Rec. 2008;83:60–76. [PubMed] [Google Scholar]
- 106.Akoua-Koffi C, Ekra KD, Kone AB. Detection and management of the yellow fever epidemic in the Ivory Coast, 2001. Med Trop (Mars) 2002;62:305–309. [PubMed] [Google Scholar]
- 107.WHO Yellow fever, Senegal (update) Wkly Epidemiol Rec. 2002;77:373–374. [PubMed] [Google Scholar]
- 108.WHO The yellow fever situation in Africa and South America in 2004. Wkly Epidemiol Rec. 2005;80:250–256. [PubMed] [Google Scholar]
- 109.Monath TP. Facing up to re-emergence of urban yellow fever. Lancet. 1999;353:1541. doi: 10.1016/S0140-6736(99)00155-5. [DOI] [PubMed] [Google Scholar]
- 110.WHO Dengue/dengue haemorrhagic fever. Wkly Epidemiol Rec. 2000;75:193–196. [PubMed] [Google Scholar]
- 111.WHO Situation update of dengue in the South East Asia Region. 2007. http://www.searo.who.int/LinkFiles/Dengue_Dengue_update_SEA_2010.pdf (accessed Nov 18, 2010).
- 112.Cummings DA, Irizarry RA, Huang NE. Travelling waves in the occurrence of dengue haemorrhagic fever in Thailand. Nature. 2004;427:344–347. doi: 10.1038/nature02225. [DOI] [PubMed] [Google Scholar]
- 113.Pinheiro FP, Corber SJ. Global situation of dengue and dengue haemorrhagic fever, and its emergence in the Americas. World Health Stat Q. 1997;50:161–169. [PubMed] [Google Scholar]
- 114.Boussaa S, Pesson B, Boumezzough A. Phlebotomine sandflies (Diptera: Psychodidae) of Marrakech city, Morocco. Ann Trop Med Parasitol. 2007;101:715–724. doi: 10.1179/136485907X241398. [DOI] [PubMed] [Google Scholar]
- 115.Trape JF, Zoulani A. Malaria and urbanization in central Africa: the example of Brazzaville. Part II: results of entomological surveys and epidemiological analysis. Trans R Soc Trop Med Hyg. 1987;81(suppl 2):10–18. doi: 10.1016/0035-9203(87)90472-x. [DOI] [PubMed] [Google Scholar]
- 116.Barbazan P, Baldet T, Darriet F, Escaffre H, Djoda DH, Hougard JM. Impact of treatments with Bacillus sphaericus on Anopheles populations and the transmission of malaria in Maroua, a large city in a savannah region of Cameroon. J Am Mosq Control Assoc. 1998;14:33–39. [PubMed] [Google Scholar]
- 117.Awolola TS, Oduola AO, Obansa JB, Chukwurar NJ, Unyimadu JP. Anopheles gambiae s.s. breeding in polluted water bodies in urban Lagos, southwestern Nigeria. J Vector Borne Dis. 2007;44:241–244. [PubMed] [Google Scholar]
- 118.Batra CP, Adak T, Sharma VP, Mittal PK. Impact of urbanization on bionomics of An. culicifacies and An. stephensi in Delhi. Indian J Malariol. 2001;38:61–75. [PubMed] [Google Scholar]
- 119.Sattler MA, Mtasiwa D, Kiama M. Habitat characterization and spatial distribution of Anopheles sp. mosquito larvae in Dar es Salaam (Tanzania) during an extended dry period. Malar J. 2005;4:4. doi: 10.1186/1475-2875-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Robert V, Macintyre K, Keating J. Malaria transmission in urban sub-Saharan Africa. Am J Trop Med Hyg. 2003;68:169–176. [PubMed] [Google Scholar]
- 121.Hay SI, Guerra CA, Tatem AJ, Atkinson PM, Snow RW. Urbanization, malaria transmission and disease burden in Africa. Nat Rev Microbiol. 2005;3:81–90. doi: 10.1038/nrmicro1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Keiser J, Utzinger J, de Castro M Caldas, Smith TA, Tanner M, Singer BH. Urbanization in sub-saharan Africa and implication for malaria control. Am J Trop Med Hyg. 2004;71(2 suppl):118–127. [PubMed] [Google Scholar]
- 123.Clark TD, Greenhouse B, Njama-Meya D. Factors determining the heterogeneity of malaria incidence in children in Kampala, Uganda. J Infect Dis. 2008;198:393–400. doi: 10.1086/589778. [DOI] [PubMed] [Google Scholar]
- 124.Wang SJ, Lengeler C, Smith TA. Rapid urban malaria appraisal (RUMA) I: epidemiology of urban malaria in Ouagadougou. Malar J. 2005;4:43. doi: 10.1186/1475-2875-4-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Staedke SG, Nottingham EW, Cox J, Kamya MR, Rosenthal PJ, Dorsey G. Short report: proximity to mosquito breeding sites as a risk factor for clinical malaria episodes in an urban cohort of Ugandan children. Am J Trop Med Hyg. 2003;69:244–246. [PubMed] [Google Scholar]
- 126.Matthys B, Vounatsou P, Raso G. Urban farming and malaria risk factors in a medium-sized town in Cote d'Ivoire. Am J Trop Med Hyg. 2006;75:1223–1231. [PubMed] [Google Scholar]
- 127.Klinkenberg E, McCall PJ, Hastings IM, Wilson MD, Amerasinghe FP, Donnelly MJ. Malaria and irrigated crops, Accra, Ghana. Emerg Infect Dis. 2005;11:1290–1293. doi: 10.3201/eid1108.041095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Craig PG, Bryan JP, Miller RE. The prevalence of hepatitis A, B and C infection among different ethnic groups in Belize. Am J Trop Med Hyg. 1993;49:430–434. doi: 10.4269/ajtmh.1993.49.430. [DOI] [PubMed] [Google Scholar]
- 129.Poovorawan Y, Chatchatee P, Chongsrisawat V. Epidemiology and prophylaxis of viral hepatitis: a global perspective. J Gastroenterol Hepatol. 2002;17(suppl):S155–S166. doi: 10.1046/j.1440-1746.17.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 130.Villarejos VM, Provost PJ, Ittensohn OL, McLean AA, Hilleman MR. Seroepidemiologic investigations of human hepatitis caused by A, B, and a possible third virus. Proc Soc Exp Biol Med. 1976;152:524–528. doi: 10.3181/00379727-152-39432. [DOI] [PubMed] [Google Scholar]
- 131.Barzaga BN. Hepatitis A shifting epidemiology in South-East Asia and China. Vaccine. 2000;18(suppl 1):S61–S64. doi: 10.1016/s0264-410x(99)00467-3. [DOI] [PubMed] [Google Scholar]
- 132.Tanaka J. Hepatitis A shifting epidemiology in Latin America. Vaccine. 2000;18(suppl 1):S57–S60. doi: 10.1016/s0264-410x(99)00466-1. [DOI] [PubMed] [Google Scholar]
- 133.Lai JY. Hepatitis A and E in Hong Kong. Hong Kong Med J. 1997;3:79–82. [PubMed] [Google Scholar]
- 134.Department of Health Department of Health annual report 1005/2006. http://www.dh.gov.hk/english/pub_rec/pub_rec_ar/pub_rec_arpis_0506_html_ar.html (accessed Nov 18, 2010).
- 135.Hufnagel L, Brockmann D, Geisel T. Forecast and control of epidemics in a globalized world. Proc Natl Acad Sci USA. 2004;101:15124–15129. doi: 10.1073/pnas.0308344101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Charrel RN, de Lamballerie X, Raoult D. Chikungunya outbreaks—the globalization of vectorborne diseases. N Engl J Med. 2007;356:769–771. doi: 10.1056/NEJMp078013. [DOI] [PubMed] [Google Scholar]
- 137.Fasina FO, Bisschop SP, Webster RG. Avian influenza H5N1 in Africa: an epidemiological twist. Lancet Infect Dis. 2007;7:696–697. doi: 10.1016/S1473-3099(07)70244-X. [DOI] [PubMed] [Google Scholar]
- 138.Behrens RH, Carroll B, Smith V, Alexander N. Declining incidence of malaria imported into the UK from West Africa. Malar J. 2008;7:235. doi: 10.1186/1475-2875-7-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Elkhalifa SM, Mustafan IO, Wais M, Malik EM. Malaria control in an urban area: a success story from Khartoum, 1995–2004. East Mediterr Health J. 2008;14:206–215. [PubMed] [Google Scholar]
- 140.Ooi EE, Goh KT, Gubler DK. Dengue prevention and 35 years of vector control in Singapore. Emerg Infect Dis. 2006;12:887–893. doi: 10.3201/10.3201/eid1206.051210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.WHO Kobe Centre Our cities, our health, our future: acting on social determinants for health equity in urban settings. July, 2007. http://www.who.int/social_determinants/resources/knus_report_16jul07.pdf (accessed Nov 18, 2010).
- 142.Yusuf S, Nabeshima K, Ha W. Income and health in cities: the messages from stylized facts. J Urban Health. 2007;8(3 suppl):i35–i41. doi: 10.1007/s11524-007-9186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Szreter S. The importance of social intervention in Britain's mortality decline c1850–1914; a re-interpretation of the role of public health. Soc Hist Med. 1988;1:1–37. [Google Scholar]
- 144.Scott V, Stern R, Sanders D, Reagon G, Mathews V. Research to action to address inequities: the experience of the Cape Town Equity Gauge. Int J Equity Health. 2008;7:6. doi: 10.1186/1475-9276-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Uncited reference
- 86.França-Silva JC, Barata RA, Costa RT. Importance of Lutzomyia longipalpis in the dynamics of transmission of canine visceral leishmaniasis in the endemic area of Porteirinha Municipality, Minas Gerais, Brazil. Vet Parasitol. 2005;131:213–220. doi: 10.1016/j.vetpar.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 87.Oliveira AG, Galati EA, de Oliveira O. Abundance of Lutzomyia longipalpis (Diptera: Psychodidae: Phlebotominae) and urban transmission of visceral leishmaniasis in Campo Grande, state of Mato Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz. 2006;101:869–874. doi: 10.1590/s0074-02762006000800008. [DOI] [PubMed] [Google Scholar]
- 88.Rojas E, Scorza JV, Morales G, Morales C, Barazarte R, Torres A. Diversity and species composition of sand flies (Diptera: Psychodidae) in a Venezuelan urban focus of cutaneous leishmaniasis. J Am Mosq Control Assoc. 2004;20:189–194. [PubMed] [Google Scholar]
- 89.Salomón OD, Orellano PW. Lutzomyia longipalpis in Clorinda, Formosa province, an area of potential visceral leishmaniasis transmission in Argentina. Mem Inst Oswaldo Cruz. 2005;100:475–476. doi: 10.1590/s0074-02762005000500005. [DOI] [PubMed] [Google Scholar]