Highlights
-
•
SFTS viremia persists until week 3 from the day of symptom onset.
-
•
The concentrations of inflammatory cytokines are elevated in SFTS patients.
-
•
IFN-α, IL-10, and IP-10 are associated with the initial cytokine storm.
Keywords: Severe fever with thrombocytopenia syndrome virus, Viral load, Cytokines, Chemokines
Abstract
Background
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging infectious disease in China, Japan, and Korea, which is characterized by high fever, thrombocytopenia, and high mortality. It is hypothesized that a cytokine storm plays an important role in the pathophysiology of SFTS. However, limited data have been published on the detailed kinetics of the viral load and cytokine profiles throughout the course of this disease.
Objectives
We investigated the patterns of changes in cytokines and viral load in SFTS patients.
Study design
During the admission period of patients, RNA was extracted from plasma and quantified by reverse transcription polymerase chain reaction. In addition, cytokine bead arrays were performed for the 18 cytokines and chemokines selected for testing.
Results
The median time from admission to the negative conversion of SFTS viremia was 17.0 days. When censored patients were found to be negative for viral load at discharge, the median duration of viral shedding was 13.0 days (95% CI, 5.4–20.6). Interferon (IFN)-α, interleukin (IL)-10, and IFN-γ-induced protein (IP)-10 concentrations significantly increased in the early course of disease and then decreased during the hospital stay. However, the concentrations of tumor necrosis factor-α, IL-1β, IL-12p40, IL-13, IL-17A, Regulated on Activation and Normally T-cell Expressed and Secreted (RANTES), and vascular endothelial growth factor (VEGF) increased during the late course of disease. Initial IP-10 levels during hospital days 1–4 were the most significantly correlated with initial viral load (r = 0.88, P < .01).
Conclusion
SFTS viremia persisted until weeks 2–3 and was highly correlated with initial plasma IP-10 levels. In addition, IFN-α, IL-10, and IP-10 were associated with the initial cytokine storm in SFTS.
1. Background
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging infectious viral disease in China, Japan, and Korea. The SFTS virus (SFTSV) belongs to the genus Phlebovirus of the family Bunyavirus and was first identified by a group of Chinese medical researchers [1]. The major clinical signs and symptoms of SFTS are fever, abdominal pain, vomiting, nausea, thrombocytopenia, and leukocytopenia. Multiple organ failure can sometimes occur, with a mortality rate of 6–30% [[1], [2], [3]]. A previous study that used a pathogenic mouse model of SFTS reported that the viral RNA was detected and enriched primarily in the spleen during the acute phase of the disease. The study also suggested that because the virus was attached to the surface of the platelet and was detected in the cytosol of macrophages, macrophages may phagocytose SFTSV-attached platelets [4]. In an IFN-α/β knock-out mouse model, dendritic cells, megakaryocytes, monocytes, macrophages, neutrophils, and endothelial cells were not targeted by the virus; rather, reticular cells in the lymphoid tissues of the intestine and spleen were the major target cells [5]. In humans, however, the pathogenesis of the disease is poorly understood due to insufficient data.
2. Objectives
It has been hypothesized that the cytokine storm plays an important role in the pathophysiology of SFTS [[6], [7], [8], [9]]. However, limited data have been published on the detailed kinetics of viral load and cytokine profiles concerning the course of disease [3,10,11]. For this reason, we investigated the patterns of changes in cytokines and viral loads in SFTS patients during the course of disease.
3. Study design
3.1. Patients and clinical samples
From July 2015 to October 2016, we prospectively enrolled 11 patients with SFTS in Asan Medical Center. SFTSV infection was confirmed by using positive real-time reverse transcription polymerase chain reaction (RT-PCR) for the detection of viral RNA. Plasma samples were obtained from patients during their hospitalization period and placed in an EDTA-treated collection tube. Samples were immediately frozen at −80 °C until further analysis. Plasma samples from 10 healthy volunteers were analyzed as healthy controls for cytokine analysis. The study protocol was approved by the Institutional Review Board of Asan Medical Center.
3.2. Quantification of viral RNA
The viral load of SFTSV was measured using one-step multiplex real-time RT-PCR. For detection, RNA was extracted from plasma samples using Qiagen RNeasy Mini Kit (Qiagen, Hilden, Germany). To detect SFTSV, segment S and M genes were quantified, and human beta actin gene was used as an internal control. The sequences of primers and probes used in this study were as follows: SF 5′-CGAGAGAGCTGGCCTATGAA-3′, SR 5′-TTCCCTGATGCCTTGACGAT-3′, SP 5′-FAM-TGTCTTTGCCCTGACTCGAGGCA-BHQ1-3′, MF 5′-ATGCTTGTCGTGAAGAAGGC-3′, MR 5′-CTAGACTTCCCACTGCCACA-3′, MP 5′-Cy5-ACTTTTGATGGATACGTAGGCTGGGGC-BHQ2-3′, BAF 5′-ACTAACACTGGCTCGTGTGA-3′, BAR 5′-CTTGGGATGGGGAGTCTGTT-3′, and BAP 5′-HEX-AGGCTGGTGTAAAGCGGCCTTGG-BHQ1-3′. The reaction mixture was prepared with the LightCycler Multiplex RNA Virus Master (Roche Diagnostics, Indianapolis, IN), and real-time RT-PCR was conducted using the LightCycler 96 System (Roche Diagnostics, Indianapolis, IN) according to the manufacturer’s instructions with slight modification. SFTSV RNA copy number was determined based on a standard curve made from Ct values of in vitro transcript RNA. The limit of quantitative PCR reaction was 4.3 copies/μL of plasma samples.
3.3. Measurement of plasma cytokines
We measured the 18 cytokine and chemokine levels in plasma samples of 11 patients and 10 healthy volunteers simultaneously by cytometric bead array based on microspheres for detecting cytokine/chemokine in accordance with the manufacturer’s instructions (BD Biosciences, San Jose, CA). We measured granulocyte colony-stimulating factor (G-CSF), granulocyte macrophage colony-stimulating factor (GM-CSF), interferon (IFN)-α, IFN-γ, tumor necrosis factor-α (TNF-α), interleukin (IL)-1β, IL-6, IL-8, IL-10, IL-12p40, IL-13, IL-17A, monocyte chemotactic protein (MCP)-1, macrophage inflammatory protein (MIP)-1α, MIP-1β, regulated on activation and normally T-cell expressed and secreted (RANTES), IFN-γ-induced protein (IP)-10, and vascular endothelial growth factor (VEGF). Data were acquired using the FACS CANTO II flow cytometer, FACSDiva software (BD Biosciences, San Jose, CA), and FlowJo software (FlowJo LLC, Ashland, OR).
3.4. Statistical analysis
Statistical analyses were performed using GraphPad Prism 5.01 (GraphPad Software, Inc., La Jolla, CA) and SPSS for Windows software package, version 23 (SPSS Inc., Chicago, IL). We classified disease progression as follows: hospital days 1–4, 5–10, 11–16, and 17–24. Statistical differences among periods were analyzed using the Kruskal–Wallis test. The viral load of the survivors and non-survivor were compared using the Mann–Whitney U test. The Spearman test was used to calculate the correlation coefficient between cytokine/chemokine levels and viral RNA load. The median time from admission to negative conversion of viremia was analyzed using Kaplan–Meier survival analysis. All tests of significance were two-tailed, and p values less than .05 were considered statistically significant.
4. Results
4.1. Clinical characteristics of the patients
A total of 11 patients with SFTS confirmed by SFTSV-specific RT-PCR testing of plasma specimens were enrolled in this study. Among these patients, eight were men, and the mean age (±standard deviation) of the group was 60 (±7) years. No underlying disease was present in three of the 11 SFTS patients. Four cases occurred in spring to summer, and seven cases occurred in fall. All patients had fever and thrombocytopenia, and seven patients showed an altered mental status. Ten patients survived and one died during the course of hospitalization. The detailed clinical characteristics of these patients are shown in Table 1 . The mean age (±standard deviation) of the 10 control subjects was 22.5 (±0.9) years, and 8 of 10 were male.
Table 1.
Baseline clinical characteristics of the 11 patients with SFTS.
| SFTS (n = 11) | |
|---|---|
| Age mean years ± SD | 60 ± 7 |
| Male sex | 8 (73) |
| Season (months) | |
| Spring–summer (3–8) | 4 (36) |
| Fall (9–11) | 7 (64) |
| Eschar | 3 (27) |
| Clinical characteristics | |
| Fever | 11 (100) |
| Skin rash | 0 (0) |
| Headache | 5 (45) |
| Altered mental status | 7 (64) |
| Underlying disease | |
| Previous healthy | 3 (27) |
| Diabetes | 2 (18) |
| Solid tumor | 0 |
| Chronic liver disease | 0 |
| Chronic kidney disease | 0 |
| Immunosuppressive condition | 0 |
| Leukocytosis (WBC > 10,000/mm3) | 0 |
| Leukopenia (WBC < 4000/mm3) | 10 (91) |
| Thrombocytopenia (platelet, <150 × 103/mm3) | 11 (100) |
| Normal CRP (≤1.0 mg/dL) | 10 (91) |
| Renal dysfunction | 4 (36) |
| Clinical course | |
| ICU admission | 6 (55) |
| In-hospital mortality | 1 (9) |
| Treatment | |
| Doxycycline | 9 (82) |
| Ribavirin | 8 (73) |
Abbreviations: WBC, white blood cell; CRP, C-reactive protein; ICU, intensive care unit; SFTS, severe fever with thrombocytopenia syndrome; SD, standard deviation. Note: Data are no. (%) of patients, unless otherwise indicated.
4.2. Viral load kinetics
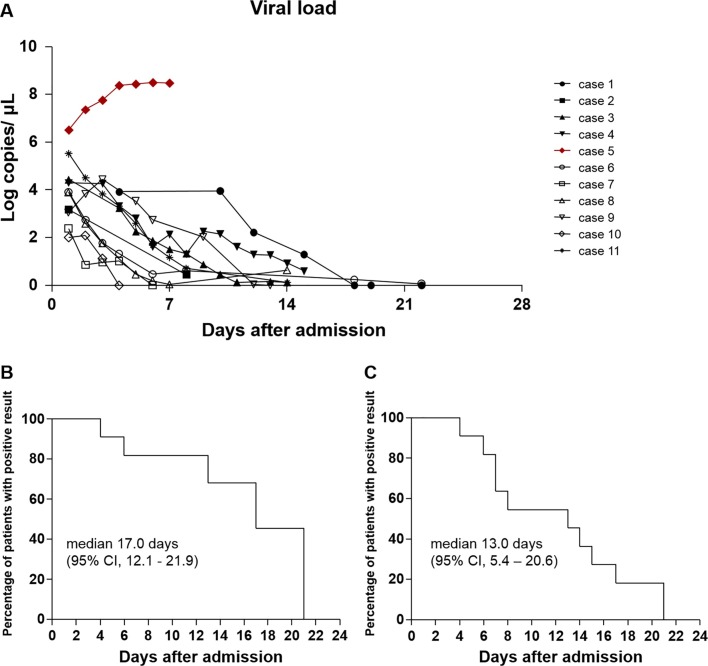
The detailed viral load kinetics of each patient are shown in Fig. 1 A. The initial viral load was measured at the day of admission in plasma specimens from 10 patients, including nine survivors and one non-survivor. In the nine survivors, the mean initial viral load was 3.70 log copies/μL (±1.03), and the viral RNA level gradually decreased over the course of disease. However, the initial viral load was 6.51 log copies/μL, and it increased up to the time of death in the non-survivor (Supplementary Fig. 1A). There was a significant difference in the plasma viral RNA level at admission between the survivors and non-survivor (P < .01, Supplementary Fig. 1B). The median time to the negative conversion of the RT-PCR result for SFTSV from the day of admission was 17.0 (95% CI, 12.1–21.9) days (Fig. 1B). If censored patients who did not show negative RT-PCR results were considered negative for viral load at discharge, the median duration of viremia was 13.0 (95% CI, 5.4–20.6) days (Fig. 1C). In addition, the median time to negative RT-PCR result for SFTSV from symptom onset was 26.0 (95% CI, 20.4–31.6) days, and when the censored patients were considered negative for viral load at discharge, the median duration of viremia was 20.0 (95% CI, 13.7–26.3) days (Supplemental Fig. 2A–C).
Fig. 1.
Viral load kinetics and Kaplan–Meier curves for the negative conversion of SFTS patients. (A) The lines represent the viral RNA concentration of each patient from the day of admission. Percentage of patients with positive RT-PCR results after the day of admission (B) and percentage of patients with positive RT-PCR results after the day of admission when censored patients were considered as negative for viral RNA at discharge (C).
4.3. Cytokine analysis
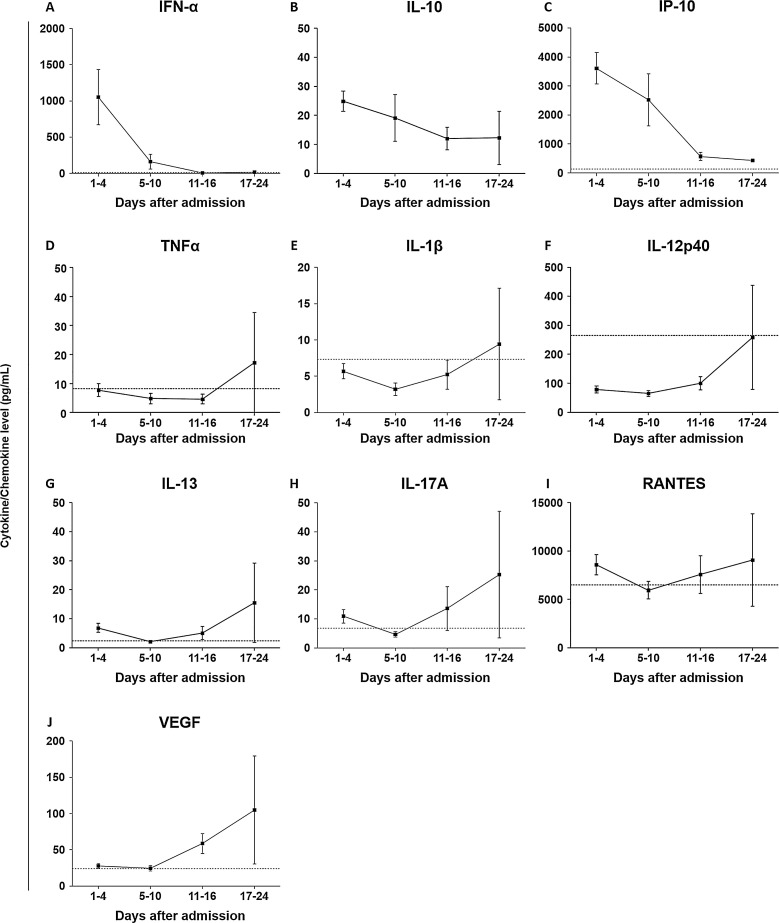
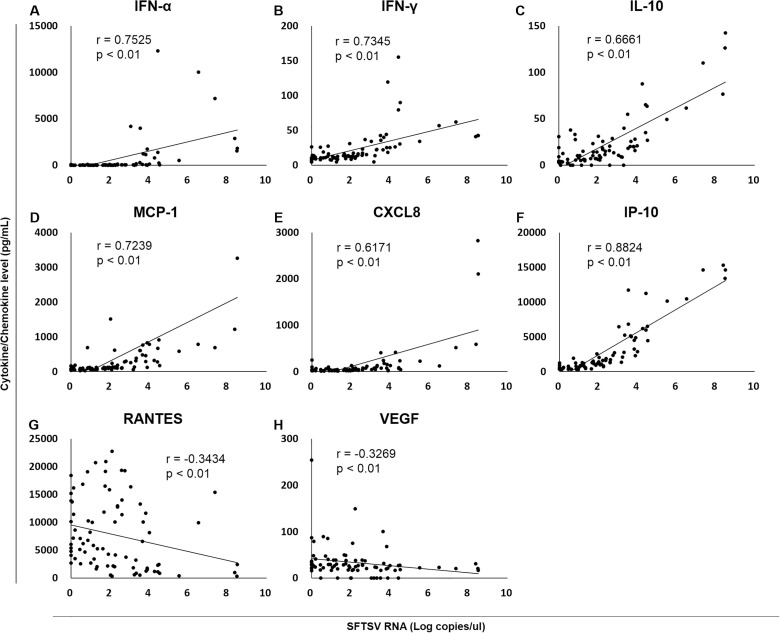
A total of 81 plasma specimens from 11 patients with SFTS and 10 plasma specimens from 10 healthy volunteers were available for 18-plex cytokine bead array analysis. G-CSF, IFN-α, IL-6, IL-10, MCP-1, MIP-1α, CXCL8, and IP-10 levels were higher in the SFTS group than in the healthy control group during the entire course of hospitalization (Supplementary Fig. 3). The levels of IFN-α, IL-10, and IP-10 increased during the early course of disease and decreased during the late course of disease (Fig. 2 ). By contrast, the concentrations of TNF-α, IL-1β, IL-12p40, IL-13, IL-17A, RANTES, and VEGF in plasma tended to increase during the late course of disease (Fig. 2). We also analyzed the relationships between cytokine or chemokine levels and the viral RNA load. IFN-α, IFN-γ, IL-10, MCP-1, CXCL8, and IP-10 levels were found to significantly correlate with viral load (r > 0.6, P < .01), whereas RANTES and VEGF showed inverse correlations with viral load (r < −0.3, P < .01) (Fig. 3 ). More details are provided in Supplementary Fig. 4.
Fig. 2.
Cytokine and chemokine levels during the course of the disease. (A–C) The levels of IFN-α, IL-10, and IP-10 increased during the early course of disease and decreased subsequently. (D–J) The concentrations of TNF-α, IL-1β, IL-12p40, IL-13, IL-17A, RANTES, and VEGF in plasma tended to increase during the late course of disease.
Fig. 3.
The relationship between cytokine and chemokine levels and levels of viral RNA in the plasma. (A–F) IFN-α, IFN-γ, IL-10, MCP-1, CXCL8, and IP-10 levels were significantly correlated with viral load. (G, H) RANTES and VEGF showed inverse correlations with viral load.
5. Discussion
Viral kinetic data in SFTS patients in the course of disease is essential for understanding its pathophysiology, monitoring of potential experimental treatment’s efficacy, prediction of disease progression, and transmission of SFTS. However, there are limited data on the detailed viral kinetics of patients with SFTS [10,11]. Yang et al. reported that viral load reached the maximum at day 6 from the onset of symptoms and then gradually decreased with a negative conversion of RT-PCR in about half of patients tested on day 18 after symptom onset [10]. Wen et al. demonstrated that 50% of the SFTS patients they reviewed were SFTSV positive according to RT-PCR within the first 2 weeks after symptom onset [11]. Our current data, which showed that the median time to negative conversion of the RT-PCR result for SFTSV from symptom onset was 26 days, are slightly different from those of previous studies [10,11]. A possible reason for this discrepancy may be methodological differences in the real-time RT-PCR. Another possible explanation could be a difference in the severity of the disease between the studies. Further studies on viral load kinetics that stratify the disease severity with minimal methodological variation are thus needed.
Among the cytokines and chemokines tested in our present analysis, the levels of IFN-α, IL-10, and IP-10 in plasma specimens were the highest during the early course of disease and decreased to the same level as those in healthy volunteers. In addition, the SFTS viral load had a positive correlation with the levels of IFN-α, IFN-γ, IL-10, IP-10, MCP-1, and CXCL8 and inverse relationships with RANTES and VEGF. Virus-infected cells release type I IFN, such as IFN-α, causing nearby cells to heighten their anti-viral defenses. In addition, the fact that IFNAR-deficient mice are highly susceptible to SFTSV suggests the importance of IFN-α in the resistance to SFTSV infection [5]. Our finding that IFN-α was high during the early stage of SFTS is consistent with the findings of a previous study [12], which indicated that IFN-α might be involved in a cytokine storm rather than being under the control of SFTSV. Proinflammatory cytokines such as IL-6 and chemokines such as IP-10, CXCL8, and MCP-1 were elevated during the acute phase of SFTS, which supports the cytokine storm theory.
IL-10 exhibits suppressive effects on the expression of class II major histocompatibility complex and B7 costimulatory molecules on the surface of monocytes and macrophages, resulting in the inhibition of proinflammatory cytokine release in various infections [13]. However, IL-10 may play an important role in the amplification of humoral responses by inducing activated B cells to secrete large amounts of IgG, IgA, and IgM [14]. Previous studies on other viral hemorrhagic fevers have reported that IL-10 levels significantly increase in the acute phase of Crimean–Congo hemorrhagic fever, Ebola, and dengue fever [[15], [16], [17]]. In addition, a previous study on SFTS demonstrated that IL-10 is increased in SFTS patients [12]. Therefore, this consistent finding of high IL-10 levels in the acute stages of viral hemorrhagic fever highlights the importance of the balance between IL-10-mediated T cell inhibition and B cell activation. Therefore, further studies are needed in this area.
In our current study, the IFN-γ level decreased, and IL-13 and IL-17A levels were elevated in the late course of disease. Because IL-13 and IL-17A are representative cytokines of the Th2 and Th17 subsets of CD4+ T cells, the chemokine profiles during disease course might contribute to shaping T cell immunity toward Th2 and Th17 responses. In addition, we found that VEGF was released from activated platelets and tumor cells that increased in the late stages of SFTS. Other studies on acute bunyavirus infection, Hantavirus, and Crimean–Congo hemorrhagic fever virus have reported that the binding of VEGF to its receptor contributes to vascular hyper-permeability, resulting in effusions [18,19]. Interestingly, we also detected an increased RANTES level in the late stages of SFTS, reminiscent of a previous study in which we reported its marked elevation also in the late stage of survivors with Middle East respiratory syndrome (MERS) [20]. Previous studies have similarly reported increased concentrations of RANTES in survivors of Ebola viral disease [21]. Because RANTES can recruit and activate T cells, T cell activation may play an important role in recovery from Ebola, MERS, and SFTS.
We compared the concentrations of cytokines in plasma and viral RNA titer, and IFN-α, IFN-γ, IL-10, MCP-1, CXCL8, and IP-10 had positive correlations during the course of the disease. The levels of those cytokines and viral concentrations were most correlated at days 5–10 of admission. This correlation was maintained while the viral RNA was detected but disappeared as the virus became undetectable, which suggests that SFTSV infection induced the expression of these inflammatory cytokines. These findings are consistent with previous reports showing that concentrations of MCP-1, CXCL8, IL-10, IFN-γ, and IP-10 are correlated with the viral load of SFTSV [3,9,12]. However, the plasma levels of TNF-α in patients with SFTS were varied among the studies. In two such reports [6,7], the TNF-α level of SFTS patients was higher than that in healthy controls and showed higher concentrations in severe cases compared with non-severe cases. On the other hand, some other studies have reported no significant differences in TNF-α concentration between the plasma samples of severe and non-severe cases [12,22]. Therefore, further studies are needed to understand the relationship among viral load, disease severity, and various cytokines in patients with SFTS.
Of note, there were several limitations to our current study. First, there was only one non-survivor; thus, it was not possible to identify prognostic factors associated with mortality. Second, we did not examine the responses of antibodies and T cells. To investigate the adaptive immune response against SFTSV, it might be helpful to measure titers and the neutralizing function of SFTSV-specific antibodies and identify profiles of immune cells during the course of the infection.
In conclusion, our data on the kinetics of cytokines in the plasma of patients with SFTS might provide us with insights into the pathogenesis of SFTS. The viral shedding kinetics from blood in patients with SFTS might provide guidance on the duration of treatment and isolation.
Conflicts of interest
There are no potential conflicts of interest for any authors.
Acknowledgements
This study was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea [grant number HI15C2774].
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jcv.2018.01.017.
Appendix A. Supplementary data
The following are Supplementary data to this article:
Viral loads in plasma samples from survivors and a non-survivor. (A) Viral load kinetics of 10 survivors (blue) and one non-survivor (red). (B) The initial viral load (hospital day 1–4) in the survivors was significantly lower than that in the non-survivor.
Viral load kinetics and Kaplan–Meier curves for the negative conversion of patients from symptom onset. (A) The lines represent the viral RNA concentration of each patient from the day of symptom onset. Percentage of patients with positive RT-PCR results after the day of symptom onset (B) and percentage of patients with positive RT-PCR results after the day of symptom onset when censored patients were considered as negative for viral RNA at discharge (C).
Detailed kinetics of cytokines and chemokines over the course of the disease.
Detailed relationships between cytokine and chemokine levels and viral RNA load in the plasma viral load.
References
- 1.Yu X.J., Liang M.F., Zhang S.Y., Liu Y., Li J.D., Sun Y.L. Fever with thrombocytopenica associated with a novel bunyavirus in China. N. Engl. J. Med. 2011;364(16):1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ding F., Zhang W., Wang L., Hu W., Sores Magalhaes R.J., Sun H. Epidemiologic features of severe fever with thrombocytopenia syndrome in China, 2011–2012. Clin. Infect. Dis. 2013;56(11):1682–1683. doi: 10.1093/cid/cit100. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Y.Z., He Y.W., Dai Y.A., Xiong Y., Zheng H., Zhou D.J. Hemorrhagic fever caused by a novel Bunyavirus in China: pathogenesis and correlates of fatal outcome. Clin. Infect. Dis. 2012;54(4):527–533. doi: 10.1093/cid/cir804. [DOI] [PubMed] [Google Scholar]
- 4.Jin C., Liang M., Ning J., Gu W., Jiang H., Wu W. Pathogenesis of emerging severe fever with thrombocytopenia syndrome virus in C57/BL6 mouse model. Proc. Natl. Acad. Sci. U. S. A. 2012;109(25):10053–10058. doi: 10.1073/pnas.1120246109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y., Wu B., Paessler S., Walker D.H., Tesh R.B., Yu X.J. The pathogenesis of severe fever with thrombocytopenia syndrome virus infection in alpha/beta interferon knockout mice: insights into the pathologic mechanisms of a new viral hemorrhagic fever. J. Virol. 2014;88(3):1781–1786. doi: 10.1128/JVI.02277-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng B., Zhang S., Geng Y., Zhang Y., Wang Y., Yao W. Cytokine and chemokine levels in patients with severe fever with thrombocytopenia syndrome virus. PLoS One. 2012;7(7):e41365. doi: 10.1371/journal.pone.0041365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ding Y.P., Liang M.F., Ye J.B., Liu Q.H., Xiong C.H., Long B. Prognostic value of clinical and immunological markers in acute phase of SFTS virus infection. Clin. Microbiol. Infect. 2014;20(11):870–878. doi: 10.1111/1469-0691.12636. [DOI] [PubMed] [Google Scholar]
- 8.Sun L., Hu Y., Niyonsaba A., Tong Q., Lu L., Li H. Detection and vealuation of immunofunction of patients with severe fever with thrombocytopenia syndrome. Clin. Exp. Med. 2014;14(4):389–395. doi: 10.1007/s10238-013-0259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun Y., Jin C., Zhan F., Wang X., Liang M., Zhang Q. Host cytokine storm is associated with disease severity of severe fever with thrombocytopenia syndrome. J. Infect. Dis. 2012;206(7):1085–1094. doi: 10.1093/infdis/jis452. [DOI] [PubMed] [Google Scholar]
- 10.Yang Z.D., Hu J.G., Lu Q.B., Guo C.T., Cui N., Peng W. The prospective evaluation of viral loads in patients with severe fever with thrombocytopenia syndrome. J. Clin. Virol. 2016;78:123–128. doi: 10.1016/j.jcv.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Wen H.L., Zhao L., Zhai S., Chi Y., Cui F., Wang D. Severe fever with thrombocytopenia syndrome, Shandong Province, China, 2011. Emerg. Infect. Dis. 2014;20(1):1–5. doi: 10.3201/eid2001.120532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu M.M., Lei X.Y., Yu H., Zhang J.Z., Yu X.J. Correlation of cytokine level with the severity of severe fever with thrombocytopenia syndrome. Virol. J. 2017;14(1):6. doi: 10.1186/s12985-016-0677-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Couper K.N., Blount D.G., Riley E.M. IL-10: the master regulator of immunity to infection. J. Immunol. 2008;180(9):5771–5777. doi: 10.4049/jimmunol.180.9.5771. [DOI] [PubMed] [Google Scholar]
- 14.Rousset F., Garcia E., Defrance T., Péronne C., Vezzio N., Hsu D.H. Interleukin 10 is a potent growth and differentiation factor for activated human B lymphocytes. Proc. Natl. Acad. Sci. U. S. A. 1992;89(5):1890–1893. doi: 10.1073/pnas.89.5.1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Green S., Vaughn D.W., Kalayanarooj S., Nimmannitya S., Suntayakorn S., Nisalak A. Elevated plasma interleukin-10 levels in acute dengue correlate with disease severity. J. Med. Virol. 1999;59(3):329–334. [PubMed] [Google Scholar]
- 16.Papa A., Tsergouli K., Caglayik D.Y., Bino S., Como N., Uyar Y. Cytokines as biomarkers of Crimean-Congo hemorrhagic fever. J. Med. Virol. 2016;88(1):21–27. doi: 10.1002/jmv.24312. [DOI] [PubMed] [Google Scholar]
- 17.Villinger F., Rollin P.E., Brar S.S., Chikkala N.F., Winter J., Sundstrom J.B. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J. Infect. Dis. 1999;179(Suppl. 1):S188–91. doi: 10.1086/514283. [DOI] [PubMed] [Google Scholar]
- 18.Ozturk B., Kuscu F., Tutuncu E., Sencan I., Gurbuz Y., Tuzun H. Evaluation of the association of serum levels of hyaluronic acid, sICAM-1, sVCAM-1, and VEGF-A with mortality and prognosis in patients with Crimean-Congo hemorrhagic fever. J. Clin. Virol. 2010;47(2):115–119. doi: 10.1016/j.jcv.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Srikiatkhachorn A., Spiropoulou C.F. Vascular events in viral hemorrhagic fevers: a comparative study of dengue and hantaviruses. Cell Tissue Res. 2014;355(3):621–633. doi: 10.1007/s00441-014-1841-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hong K.H., Choi J.P., Hong S.H., Lee J., Kwon J.S., Kim S.M. Predictors of mortality in Middle East respiratory syndrome (MERS) Thorax. 2017 doi: 10.1136/thoraxjnl-2016-209313. [DOI] [PubMed] [Google Scholar]
- 21.McElroy A.K., Erickson B.R., Flietstra T.D., Rollin P.E., Nichol S.T., Towner J.S. Biomarker correlates of survival in pediatric patients with Ebola virus diseases. Emerg. Infect. Dis. 2014;20(10):1683–1690. doi: 10.3201/eid2010.140430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J., Han Y., Xing Y., Li S., Kong L., Zhang Y. Concurrent measurement of dynamic changes in viral load, serum enzymes, T cell subsets, and cytokines in patients with severe fever with thrombocytopenia syndrome. PLoS One. 2014;9(3):e91679. doi: 10.1371/journal.pone.0091679. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Viral loads in plasma samples from survivors and a non-survivor. (A) Viral load kinetics of 10 survivors (blue) and one non-survivor (red). (B) The initial viral load (hospital day 1–4) in the survivors was significantly lower than that in the non-survivor.
Viral load kinetics and Kaplan–Meier curves for the negative conversion of patients from symptom onset. (A) The lines represent the viral RNA concentration of each patient from the day of symptom onset. Percentage of patients with positive RT-PCR results after the day of symptom onset (B) and percentage of patients with positive RT-PCR results after the day of symptom onset when censored patients were considered as negative for viral RNA at discharge (C).
Detailed kinetics of cytokines and chemokines over the course of the disease.
Detailed relationships between cytokine and chemokine levels and viral RNA load in the plasma viral load.