Abstract
Background
Mental ill-health in health professionals, including doctors, is a global and growing concern. The existing literature on interventions that offer support, advice and/or treatment to sick doctors has not yet been synthesised in a way that considers the complexity and heterogeneity of the interventions, and the many dimensions of the problem. We (1) reviewed interventions to tackle doctors’ and medical students’ mental ill-health and its impacts on the clinical workforce and patient care—drawing on diverse literature sources and engaging iteratively with diverse stakeholder perspectives—and (2) produced recommendations that support the tailoring, implementation, monitoring and evaluation of contextually sensitive strategies to tackle mental ill-health and its impacts.
Methods
Realist literature review consistent with the RAMESES quality and reporting standards. Sources for inclusion were identified through bibliographic database searches supplemented by purposive searches—resulting also from engagement with stakeholders. Data were extracted from included articles and subjected to realist analysis to identify (i) mechanisms causing mental ill-health in doctors and medical students and relevant contexts or circumstances when these mechanisms were likely to be ‘triggered’ and (ii) ‘guiding principles’ and features underpinning the interventions and recommendations discussed mostly in policy document, reviews and commentaries.
Results
One hundred seventy-nine records were included. Most were from the USA (45%) and were published since 2009 (74%). The analysis showed that doctors were more likely to experience mental ill-health when they felt isolated or unable to do their job and when they feared repercussions of help-seeking. Healthy staff were necessary for excellent patient care. Interventions emphasising relationships and belonging were more likely to promote wellbeing. Interventions creating a people-focussed working culture, balancing positive/negative performance and acknowledging positive/negative aspects of a medical career helped doctors to thrive. The way that interventions were implemented seemed critically important. Doctors and medical students needed to have confidence in an intervention for the intervention to be effective.
Conclusions
Successful interventions to tackle doctors’ and students’ mental ill-health are likely to be multidimensional and multilevel and involve multiple stakeholders. Evaluating and improving existing interventions is likely to be more effective than developing new ones. Our evidence synthesis provides a basis on which to do this.
Study registration
PROSPERO CRD42017069870. Research project webpage http://sites.exeter.ac.uk/cup/
Keywords: Wellbeing, Doctors, Physicians, Medical students, Mental ill-health, Burnout, Distress, Intervention, Stress management, Coping, Prevention, Organisational culture, Job satisfaction
Background
The mental ill-health of doctors is a global, increasingly pressing and intractable problem [1–4] affecting all medical specialties and career stages [5, 6]. Its consequences are significant and far-reaching, both within and beyond healthcare, and include poor quality or inequitable patient care [7, 8], absenteeism (doctors taking short or long-term sick leave), presenteeism (doctors working whilst unwell), poor workforce retention (doctors leaving the profession temporarily/permanently) and even suicide [9]. The processes leading to mental ill-health of doctors and medical students are also complex and multiple, encompassing individual, group, organisational, professional and socio-cultural dimensions. Examples of these dimensions comprise the demanding nature of the profession, the pressure to deliver excellent care with shrinking resources, loss of autonomy and erosion of professional values, and perceived stigma around mental illness [10].
Most research to date is undertaken within disciplinary silos and fails to consider simultaneously the many dimensions that may negatively affect doctors’ wellbeing [11–13]. Notably, the current emphasis on resilience places responsibility for good mental health with the individual doctor, but resilience training alone is not likely to solve such a complex and multidimensional issue and may even aggravate how doctors experience work-related pressures, potentially contributing to mental ill-health [14]. We found evidence of this from both systematic reviews and commentaries [11–13, 15].
Some positive signs are starting to surface. An important recent example is the 11th revision of the International Classification of Diseases (ICD-11) which classifies burnout as an occupational phenomenon rather than a medical condition.1 This classification challenges the emphasis on resilience and individual responsibility for burnout, highlighting the role (and therefore the responsibility) of the workplace. There is also a growing interest in a range of resources and initiatives that promote doctors’ and medical students’ wellbeing—at different levels, e.g. preventive, screening and therapeutic—both locally [16] and internationally [15].
However, more needs to be done to prevent further deterioration in the mental ill-health of doctors and medical students. In the United Kingdom (UK), the wellbeing-related results from the 2018 annual NHS staff survey are the worst in the last 5 years, with almost 40% of respondents indicating they had been unwell in the past 12 months because of work-related stress [17, 18].
In order to drive positive change, it is vital for research to take an approach consistent with understanding the complexity of the problem. Doing so requires an interdisciplinary perspective that can bridge different viewpoints and approaches [19, 20]. By using an interpretive, theory-driven approach to analysing data from diverse literature sources, realist reviews move beyond description to provide findings that explain how and why contexts can influence outcomes, taking account of the many dimensions (e.g. individual, organisational, socio-cultural) of the problem and the heterogeneity of approaches and interventions [21]. By undertaking a realist review and by working in a multidisciplinary research team, we have been able to find, analyse and synthesise research from across disciplinary and professional silos and engage stakeholders in understanding what our findings mean in practice for driving forward change in the system. This is the first ever realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce. Through this novel approach to analysis, we have been able to generate new insights which have allowed us to make different kinds of recommendations and interventional strategies than other types of research could do.
Methods
Aim and objectives
The aim of our research was to improve understanding of how, why and in what contexts mental health services and support interventions can be designed in order to minimise the incidence of doctors’ and medical students’ mental ill-health. The main objectives were to:
Conduct a realist review on interventions to tackle doctors’ and medical students’ mental ill-health and its impacts on the clinical workforce and patient care, drawing on a wide range of literature sources and engaging iteratively with diverse stakeholder perspectives to produce actionable theory.
Produce recommendations that support the tailoring, implementation, monitoring and evaluation of contextually sensitive strategies to tackle mental ill-health and its impacts.
Review process
The realist review followed a detailed protocol which has previously been published [10]. In this section, we provide a brief overview of our detailed review protocol. Our realist review is based on Pawson’s five iterative stages: (1) locating existing theories, (2) searching for evidence, (3) selecting articles, (4) extracting and organising data and (5) synthesising the evidence and drawing conclusions [22]. The reporting and conduct of this review is consistent with the RAMESES publication standards and reporting for realist reviews respectively [23].
Step 1: Locating existing theories
In this first step of the review, we built the initial programme theory (a set of theoretical explanations or assumptions about how a particular programme, process or interventions is expected to work) [22]. We identified theories that helped to (i) understand the processes leading to mental ill-health in doctors and (ii) understand how interventions aiming to support doctors experiencing mental ill-health are supposed to work (and for whom), when they work, when they do not, why they are not effective and why they are not being used. We iteratively drew on informal iterative discussions, advice and feedback from key content experts representing multidisciplinary perspectives in our Stakeholder Group and an exploratory search of relevant literature.
Step 2: Searching for evidence
Our search was designed, piloted and conducted by an information specialist (SB) in consultation with the co-authors. Search terms were derived from the titles, abstracts and indexing terms of relevant studies already known to the review team from background reading and consultation with stakeholders. These ‘empirically derived’ search terms were supplemented with relevant synonyms selected in consultation with the review team. Several versions of the search strategy were tested in MEDLINE via Ovid by checking that the relevant pre-identified studies were returned and by refining the search terms to optimise the relative recall and precision of the search (i.e. maximising the retrieval of known relevant studies whilst minimising the retrieval of irrelevant studies). In the process of testing and refining the search, we identified additional relevant studies which we also made sure were retrieved in subsequent iterations of the search (see full search strategy in Additional file 1). In December 2017, the final search strategy was translated and run in a selection of medical and psychology bibliographic databases, including MEDLINE, MEDLINE In-Process and Other Non-indexed Citations and PsycINFO (all via Ovid) and ASSIA (via ProQuest). Search results were exported to Endnote (X8, Clarivate Analytics, Philadelphia, USA) and de-duplicated using the automated deduplication feature and manual checking. We did not apply a historical date limit to the database searches. We were particularly interested in the UK setting; therefore, we supplemented bibliographic database searches with forward citation searching of included studies that were set in the UK.
Step 3: Selecting articles
We included all sources that focussed on mental ill-health, absenteeism, presenteeism or workforce retention; all study designs; all healthcare settings; all studies that included medical doctors/medical students; descriptions of interventions or resources that focus on improving mental ill-health and minimising its impacts; and all mental health outcome measures, including absenteeism, presenteeism and workforce retention.
Using Endnote X8, DC screened the titles and abstracts of all articles resulting from the main and supplementary searches. A random 10% sample of the three sets of results were also screened independently for consistency of application of the inclusion criteria by CP (the second reviewer). Small inconsistencies were identified and resolved through discussion. DC then screened the full texts of the papers resulting from the first round of screening and classified them in categories based on their potential to contribute to programme theory.
The full text of a 10% sample of documents from the main search and a separate 10% sample of full texts from the supplementary searches were assessed and discussed between DC and CP to ensure that decisions for final inclusion and classification into categories have been made consistently. Small inconsistencies were identified that were resolved through discussion.
Step 4: Extracting and organising data
The analysis was driven by a realist logic of analysis [24]. We sought to interpret and explain mechanisms (e.g. the way in which individuals and groups respond to and reason about the resources, opportunities or challenges offered by a particular intervention) causing mental ill-health in doctors and medical students and to identify relevant contexts when these mechanisms were likely to be ‘triggered’. These contexts and mechanisms and the resultant outcomes became the way we expressed our causal claims—i.e. we developed and expressed our causal claims in the form of context-mechanism-outcome configurations (CMOcs).
Step 5: Synthesising the evidence and drawing conclusions
We compared and contrasted these CMOcs with the evolving programme theory, so as to understand the place of and relationships between each CMOc within the programme theory. As the review progressed, we iteratively refined the programme theory based on the analysis of data found within included sources, and by stakeholder feedback (see below). Our programme theory and the underpinning CMOcs enabled us to identify the interventions which were more likely to reduce or prevent mental ill-health in doctors, as well as important obstacles to the access and effectiveness of such interventions. We then developed guiding principles based on our programme theory, CMOcs and their related interventions.
Stakeholder group
We engaged with a stakeholder group throughout the lifecycle of the project, from the development of the project grant to dissemination. Consultations with stakeholder group members took place as part of 2-h meetings at regular intervals—every 2 months—throughout the project (which lasted 18 months). We arranged additional face-to-face meetings with some stakeholders who could not attend the main meetings, as well as using Skype, email exchanges and/or telephone conversations. The group was originally composed of 22 people, including patient representatives, clinicians, doctors-in-training and medical educators, and expanded to include policy makers and members of professional bodies such as the General Medical Council and Health Education England in the latter stages. The group provided content expertise, contributed to refinement of our programme theory and is currently involved in the dissemination of the project’s non-academic outputs [10]. The meetings usually started with a brief slide presentation by our project team to introduce stakeholders to the topic under discussion and realist review approach and to provide a quick update on progress with the review. We presented our findings under development to the group in the form of statements and visual prompts to obtain their feedback. Discussions were designed to be more open-ended in the early stages of the review, but focussed on particular aspects of our results as the project progressed. Later stakeholder groups focussed on actionable findings and dissemination of the study. Additional file 2 provides a list of the face-to-face meetings, including the number of participants and key topics discussed.
Results
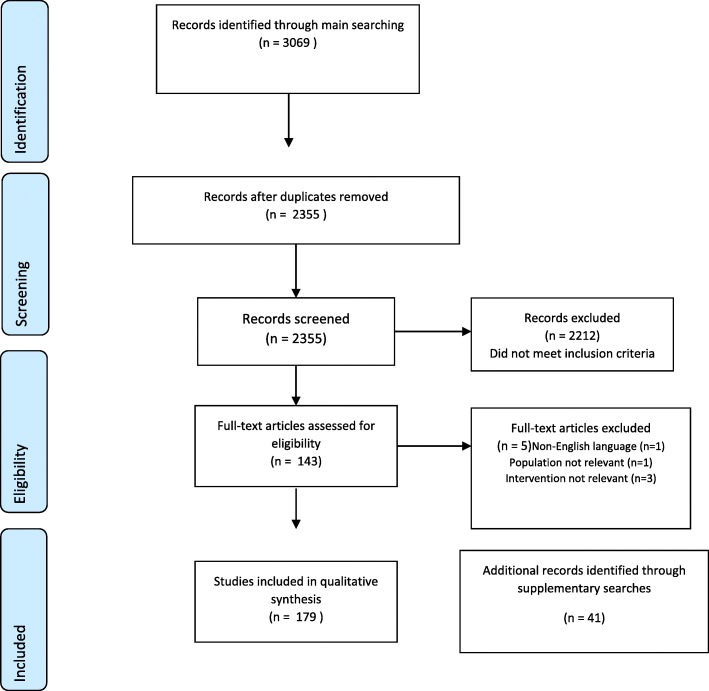
The main searches identified 3069 studies; 179 studies met the inclusion criteria and were included in the review (see Fig. 1 for a PRISMA flowchart and Additional file 3 for a table describing the included studies). Of the included studies, the country most represented was the USA (45%) (22.3% of the included studies were from the UK); 74% had been published in 2010 or more recently; most were research studies; 33% focussed on structural interventions (those that require changes in the organisation of doctors’ work environment, e.g. rotas), 21% focussed on individual interventions (those that target the individual doctor, e.g. mindfulness) and 46% considered both levels together. Most interventional studies were preventative, rather than considering treatment or screening. Less than a quarter of included studies (19%) provided cost information. Of these, costs in 5/179 (3%) were quantified, 24/179 (13%) contained unquantified narrative claims and 6/179 (3%) contained a mix of quantified costs and unquantified narrative claims. No included studies reported a health economic analysis. Finally, most studies referred to doctors or physicians in general, rather than focussing on specific specialties or career stages.
Fig. 1.
PRISMA diagram
Our realist analysis developed 19 CMOcs, structured around four main clusters: (1) processes leading to mental ill-health: isolation; (2) reducing mental ill-health: groups, belonging and relationality; (3) reducing mental ill-health: balance and timeliness; and (4) implementation methods: engendering trust. Table 1 provides a summary of the 19 CMOcs, which together make up the programme theory, organised in these four main clusters. The clusters are strongly intertwined, meaning that the likelihood of the success of an intervention strategy is enhanced by its alignment with all the four clusters. Examples of the citations that provide evidence for each CMOc are available in Additional file 4.
Table 1.
Summary of the CMOcs (programme theory)
| (1) Processes leading to mental ill-health in doctors: isolation | |
| CMOc 1: Underdeveloped workforce planning | In a workplace in which basic support structures to enable doctors to do their job are not in place (C), doctors may feel they must make up for the deficiencies of the organisation for patients and colleagues (M). This may contribute to a toxic working culture in which overwork and its negative consequences are normalised (O). |
| CMOc 2: Normalisation of high workload | When high workload and its negative consequences (e.g. distress, burnout) are normalised (C), overworked or sick doctors may feel they are letting down their colleagues and patients (M). This can contribute to presenteeism (O) and associated negative consequences on mental health (O1) and workforce retention (O2). |
| CMOc 3: Loss of autonomy | When doctors experience lack of autonomy over their work (C1), and some aspects of their work as less meaningful (C2), they may feel dissatisfied with their job (e.g. because they are unable to do the job they were trained for) (M). This can make doctors more vulnerable to stress and mental ill-health, irrespective of workload (O). |
| CMOc 4: Stigma towards vulnerability | In a professional culture where mental ill-health and vulnerability may be seen as unprofessional (C), doctors (and medical students) may feel ashamed (M1) or afraid (M2) of not living up to their professional identity if they experience mental ill-health (or other difficulties at work). This can lead doctors (and medical students) to adopt strategies which involve hiding their difficulties from themselves and colleagues (O). |
| CMOc 5: Hiding vulnerability | Where there is mental health support available for doctors (C1), doctors, who understand the system and that confidentiality is difficult to achieve (C2), may fear that seeking support could jeopardise their career (M) and so they may hide their distress rather than seek support (O). |
| CMOc 6: Isolation | When doctors work in physical and emotional isolation (C), they are likely to feel less supported by their colleagues and/or their employing organisation (M1) and/or mistrust of these groups (M2). This can make doctors more vulnerable to work-related pressure and mental ill-health (O). |
| (2) Reducing mental ill-health: groups, belonging and relationality | |
| CMOc 7: Positive and meaningful workplace relations | Positive and meaningful workplace relations (C) can foster a sense of belonging between colleagues and towards the medical profession (M). This can lead to an increased capacity to work under pressure (O) |
| CMOc 8: Functional working groups | Working in functional groups (C) can make doctors feel more supported (M1) and more at ease with vulnerability (M2). This can normalise vulnerability (O1) and reduce the stigma around mental ill-health (O2) |
| CMOc 9: Balancing quality and quantity of time at work | When doctors (for different reasons) have less connectedness and meaning at work (C), they may feel they can only find fulfilment outside work (M1), making it less likely that their condition will improve (O). |
| CMOc 10: Limits of groups | Sick doctors (and medical students) with particularly delicate circumstances (C) may not feel safe to share their problems (M1) and/or may not identify with the other group members (M2). This can result in a dysfunctional group (O1) and intensification of mental ill-health in doctors (O2). |
| CMOc 11: ‘Organic’ spaces to connect | If there are protected times and psychologically safe spaces for students/doctors to congregate within the confines of the work environment (C), students/doctors are likely to bond over whatever is most important to them at that time (M). This may improve connectedness (O). |
| (3) Reducing mental ill-health: balance and timeliness | |
| CMOc 12: Recognising both positive and negative performance | Where supervision and feedback recognise both positive and negative performance and promote doctors’ (and students’) learning from both of these (C), doctors (and students) may feel more fairly treated (M1) and more inclined to value their colleagues and employing organisation (M2), potentially leading to more connectedness and engagement at work (O1), and a more supportive work culture (O2). |
| CMOc 13: Balancing prevention of metal ill-health with promotion of wellbeing | In a work environment that actively demonstrates the importance of the balance between health and wellbeing with fighting stress and mental ill-health (C), doctors (and students) are more likely to feel that caring about their own wellbeing is legitimate (M1) and less afraid to acknowledge vulnerability (M2). This can contribute to a de-stigmatisation of mental ill-health and vulnerability (O). |
| CMOc 14: Acknowledging the positive and negative aspects of the profession | Where both the positive and negative aspects of a medical career are recognised (C), doctors (and medical students) may feel less inadequate and helpless when they or their colleagues experience stress or mental ill-health (M). This may lead to increased capacity to deal with work pressure (O1) and to recognition and acceptance of vulnerability (O2). |
| CMOc 15: Timely support | Timely support when doctors (and students) are particularly vulnerable (e.g. after a suicide attempt, death of a colleague, addiction) (C) may represent their only source of hope (M) and reduce the intensity of mental ill-health and its related outcomes, including suicide (O). |
| (4) Implementation methods: engendering trust | |
| CMOc 16: Endorsement | Doctors are less likely to engage with an intervention (O) if it is not endorsed by the employing organisation and senior leadership (C) because they may then lack trust in it (M1) and may also feel frustrated (M2) if they cannot access it due to work constraints. |
| CMOc 17: Expertise | If those delivering interventions do not have specific training to address the needs of sick doctors (C), the recipients may be less likely to trust the intervention (M) and the intervention may be ineffective (O1) and/or harmful (O2) or not accessed at all (O3). |
| CMOc 18: Engagement | If doctors (and students) are involved in the development and implementation of interventions (C), the recipients are more likely to trust (M1) and feel ownership (M2) of the intervention. As a result, it is more likely to be used (O1) and to be effective (O2). |
| CMOc 19: Evaluation | If the outcomes of interventions and the wellbeing of the workforce are regularly reviewed and monitored (C1), and commitment to act upon the outcome of these regular review exercises is shown (C2, and CMOc 16), then doctors may feel more supported (M) and engage with efforts to tailor these interventions (O1). This may also lead to greater awareness about vulnerability and wellbeing in the workplace (O2). |
Processes leading to mental ill-health: isolation
Our analysis revealed that doctors (and medical students) are more likely to experience mental ill-health when they feel isolated, when they feel unable to do the job they were trained for and when they fear the repercussions of seeking help and support (CMOcs 1–6). These processes blend organisational and work culture factors. The main organisational ones are resources and workload, work structure, workforce planning and governance (CMOcs 1–3). The main factors relating to work culture are medical culture and identity, and in particular the ideas of invulnerability, perfectionism and stigma around mental ill-health within the medical profession (CMOcs 4–6). Considerations of biographical aspects, related to individual psychological predisposition to mental ill-health, personal contexts and/or traumatic events outside of work, were often strongly intertwined with the dimensions described above.
Reducing mental ill-health: groups, belonging and relationality
Our analysis also showed that interventions that emphasise relationships and belonging (for example with colleagues, to a healthcare team or the profession) are more likely to promote wellbeing and improve workplace cultures (CMOcs 7–11). The sense of belonging and connectedness, fostered by positive and meaningful workplace relations, can lead to an increased capacity to work under pressure (CMOc 7), can lead to an increased sense of meaning at work (CMOc 9) and can also contribute to normalise vulnerability and mental ill-health (CMOc 8). It is beyond the scope of this review to provide details of what is needed for initiatives to foster effective relationality, but, as suggested by some of our included sources (e.g. [25]) and research in psychology of health [26], relationships that are not imposed via mandatory activities and occur more spontaneously are particularly positive—for example, where the work environment provides protected time and safe spaces for student/doctors to congregate (CMOc 11). Our analysis also suggested that there are some limitations to group approaches and one-to-one support approaches are sometimes preferable, for example when there are significant confidentiality issues, when the individual is under investigation, or after the death of a colleague (CMOc 10).
Reducing mental ill-health: balance and timeliness
Our analysis highlighted that interventions that create a people-focussed working culture which recognises that the health and wellbeing of staff is important both as a value in itself and as a necessary precondition to excellent patient care, promotes doctors and medical students learning from both positive and negative performance and acknowledges both the rewarding and stressful aspects of a medical career can help doctors to thrive at work and deal with work pressures (CMOCs 12–15).
It is common for pressured healthcare services to focus more on workforce mistakes, errors and negative patient outcomes and less on positive practice and performance [27, 28]. However, promoting supervision and feedback that recognise both positive and negative performance and encourage doctors and students to learn from both can lead to more connectedness and engagement in the workplace and to a more supportive work culture (CMOc 12). Similarly, a work culture that promotes health and wellbeing alongside focussing on fighting mental ill-health can contribute to the normalisation and de-stigmatisation of mental ill-health (CMOc 13). Acknowledging both rewarding and stressful aspects of the medical profession can also help to achieve the same outcomes as it may make students and doctors feel less inadequate when they or their colleagues experience mental ill-health or difficulties at work (CMOc 14).
The timeliness of support, especially when doctors or students are particularly vulnerable (e.g. in relation to traumatic events such as a suicide attempt, addiction and sickness absence), may reduce mental ill-health outcomes, including suicide (CMOc 15).
Implementation methods: engendering trust
Our analysis suggests that for an intervention to be successful, it is important to consider not only its content but also how such intervention is implemented: the how is as important as the what. Doctors (and medical students) need to have confidence in an intervention, and those delivering it, for the intervention to be effective (CMOCs 16–19). Interventions are more likely to work if they are endorsed by the senior level of the organisation involved (CMOc 16), those delivering them have adequate training to address the needs of sick doctors’ and students’ (CMOc 17), doctors (and students) are engaged in their design (CMOc 18) and the outcomes of such interventions are regularly reviewed and effectively acted upon (CMOc 19).
Discussion
The aim of our realist review was to improve understanding of how, why and in what contexts mental health services and support interventions can be designed in order to minimise the incidence of doctors’ and medical students’ mental ill-health. Our review identified three important processes leading to mental ill-health: significant and complex workload, organisational management and the professional culture of medicine.
Working relationships, with other doctors and healthcare staff as well as with the organisation, explained a key part of how mental ill-health could be prevented and reduced. Whilst not operating in a linear fashion, meaningful workplace relations and functional working groups are likely to enable the protective mechanisms of a sense of belonging and an ease with vulnerability to function. Moreover, the, often implicit, vision set by healthcare organisations and professional bodies about what a medical career entails and how different clinicians are expected to behave could have important implications for mental ill-health. Constructive workplace feedback on performance, an organisation’s demonstrable valuing of employees’ health and wellbeing and a professional culture that recognises both the rewarding and stressful aspects of a medical career could provide the context for doctors (and students) to contribute to and benefit from an upward cycle of interacting mechanisms such as legitimating their own wellbeing, acknowledging vulnerability, preventing feelings of inadequacy and valuing colleagues. Finally, when doctors and students are affected negatively by significant life events, the provision of timely support in the workplace is crucial for hope to play a role in recovery.
Whilst interventions that target individual doctors and students (e.g. to prevent mental ill-health or ameliorate it once established) may address parts of the processes leading to mental ill-health, interventions that address multiple organisational and professional issues simultaneously are more likely to be successful.
By undertaking a realist review, we have been able to find, analyse and synthesise data from across disciplinary silos and ‘sense check’ our findings against feedback from various perspectives. Our multidisciplinary research team worked closely with a large, diverse group of individuals in the stakeholder group and sense-making groups and ‘translated’ the findings through these interactions. This was in contrast to much of the research into doctors’ mental ill-health identified through our review, which tended to be limited to quite specific perspectives occurring in disciplinary silos [11–13, 15]. An important limit of this approach is the lack of consideration of the organisational and structural contexts that may have a detrimental effect on doctors’ wellbeing. There are however commentators who have argued that interventions should also focus on organisational support and systemic factors contributing to mental ill-health, rather than on individual doctors [9, 29, 30]—some have advocated for a shift from ‘individual’ to ‘organisational resilience’ [13]. Our study corroborates this multidimensional approach.
The key limitation of our research, in common with all literature-based research methods, is that the findings are only as good as the literature available to synthesise. Most studies about individual- and work-related factors related to doctors’ mental ill-health are of a cross-sectional design; however, it is still epistemologically possible to make causal claims based on such data, especially by combining data of various types, as in a realist review [21, 24]. In this review, most of the literature came from the USA, with a smaller component from the UK, which made the interpretation of the relevance of the data from included sources to the UK healthcare setting more challenging. We were assisted through the methodological challenges related to the transferability of our findings to a UK setting by our stakeholder group.
Conclusions
Drawing on our analysis and engagement with key stakeholders, we articulated recommendations and implementation principles about intervention strategy design and development for different audiences (Table 2). Whilst these recommendations and principles are presented separately to aid comprehension, the interdependency of these levels should be acknowledged in intervention strategy design and development. For example, doctors may not be able to prioritise relationships at work if there are no organisational structures to support this. To maximise the impact of our review and help those refining/designing interventional strategies to tackle doctors’ mental ill-health, we also developed 10 ‘Care Under Pressure’ principles, by which existing interventions might be refined, which draw out the interdependence of the different levels (Table 3).
Table 2.
Key recommendations and principles for refining/developing strategies to reduce mental ill-health
| Key recommendations and principles for refining/designing strategies to reduce mental ill-health in doctors | |
| For policy makers | Policies that aim to secure the future of the NHS workforce must foster a supportive work culture in which individuals can thrive. Policies and interventions that target the individual in the absence of a supportive work culture are unlikely to succeed. CMOCs 1–3, 7–9, 12–14, 16, 19. |
| For employers | Ensure influential nominated Board-level responsibility for the wellbeing of staff. This should include regular immersion in practice settings, as well as regular reports on progress against key performance indicators (e.g. absenteeism might be detected by sickness absence, rota gaps and vacant posts; presenteeism might be detected by complaints and errors; workforce retention might be detected by staff turnover; general staff wellbeing might be detected via annual staff surveys, markers of overwork and occupational health referrals). CMOCs 12–13, 16–19. |
| For team leaders | Actively look out for behaviours that may be potentially stigmatising and encourage help-seeking. In performance reviews, emphasise the positive as well as the negative and ensure the doctor knows their hard work in often challenging circumstances is valued. Make clear that prioritising own health is important for patient care. CMOCs 12–15. |
| For doctors | Recognise when you are working under pressure and, even when your workload is high, prioritise your relationships at work. CMOCs 7–11. |
| For other healthcare team members | Recognise that the whole team may, at times, be providing care under pressure. Try to normalise discussions of struggle in the context of challenging work. CMOCs 7, 8, 11–13. |
| For patients | Know that doctors and other health professionals are usually doing the best job they can in difficult circumstances. A thank you when things go well will always be appreciated! CMOCs 4, 5, 7, 12. |
| For researchers | Use research syntheses and stakeholder involvement to target your research to the areas of greatest need. Research of all kinds will be needed to develop theory and interventions, and design appropriate outcome measures, approaches to evaluation and implementation, in relation to doctors’ mental ill-health. CMOCs 1–19. |
| For those refining/designing interventions | Adopt our 10 Care Under Pressure principles (see below). CMOCs 1–19. |
Table 3.
Principles for use for those refining/designing interventional strategies to tackle doctors’ mental ill-health
| 10 Care Under Pressure principles, for use by those refining/designing interventional strategies to tackle doctor mental ill-health | |
| 1. Be clear about who the intervention is for (given the continuum from full health, to ‘under pressure’, to mental ill-health). | |
| 2. Give options by signposting to a range of interventions (e.g. a ‘one stop shop’ of local, regional and national resources). | |
| 3. Ensure that information about the intervention is readily and rapidly available. | |
| 4. Ensure that interventions are accessible to someone who works long and inflexible hours. | |
| 5. At the initial enquiry stage, invest time in building trust and normalising stigma and struggle. | |
| 6. Provide interventions in groups whenever possible, to prioritise connectedness, relationships and belonging. | |
| 7. Ensure interventions for individuals are endorsed by or embedded in the workplace, where possible. | |
| 8. Encourage and empower individuals to tackle low-level everyday hassles at work, to free up capacity to deal with bigger issues. | |
| 9. Emphasise that prioritising and investing in physical and mental health is essential for optimal patient care. | |
| 10. Evaluate and improve the intervention regularly, using data such as numbers and types of attendee, programme adherence and user perceptions. |
To support and bring to life our recommendations and principles, we have developed, with our stakeholders and with two artists and a film maker, a series of graphic illustrations and videos (see Fig. 2 for an example of cartoon about self-care and presenteeism2). These have been designed to surface the issues that underpin some of the recommendations and principles—making them more human and accessible.
Fig. 2.
Example of Care Under Pressure creative output: a cartoon about self-care and presenteeism drawn by our collaborator Dr. Ian Williams—for more cartoons and information, please visit http://sites.exeter.ac.uk/cup/cartoons/
A significant number of interventions are described in the peer-reviewed and grey literature, but many fall short of meeting the ‘10 Care Under Principles’ that we have developed through this research. Therefore, evaluating and improving existing interventions is likely to be more effective than developing new ones. The role of undergraduate medical education in forming doctors’ professional culture is important for the way it can develop healthy or unhealthy attitudes and behaviours in relation to coping and disclosure. If supportive working cultures can be created and sustained, medical schools could provide an early opportunity to proactively emphasise the importance of looking after one’s own health, to normalise discussions of struggle when work is challenging, to recognise the positive and negative aspects of medical careers and to promote an understanding of how and when to seek help.
Future research can build on our realist review to evaluate and refine interventional strategies that have been already implemented, or design, implement and evaluate new ones. For example, the Royal College of Surgeons and Health Education England are piloting a ‘modern firm’, one of whose main objectives is to make trainees ‘feel more valued while also recognising the needs of senior doctors: specifically their own need for training and for time to train and support their junior colleagues’ [31]. Such evaluations might use a realist evaluation approach or a complex intervention trial approach.
Supplementary information
Additional file 1. Search 1: Interventions to reduce mental ill health.
Additional file 2. Table describing the stakeholder group meetings.
Additional file 3. Table describing the included studies.
Additional file 4. Examples of the citations that provide evidence for each CMOc.
Acknowledgements
We would like to express our gratitude to the members of our stakeholder group, those who took part in the policy workshop, and others who offered their perspective through individual meetings for their significant contributions to the programme theory and actionable findings emerging from the review. These included (alphabetically by first name) Alex Aylward, Alex Blohm, Andrew Tressider, Andy Grant, Clare Gerada, Daisy Robinson, Derek Gallen, Diana Frost, Fady Awad, Ian Fussell, Jackye Hayden, Jill Maben, Jodie Blackadder, Julie Harvey, Katrina Wyatt, Kirsten Leslie, Laura Hill, Linda Gask, Luna Dolezal, Lynn Monrouxe, Lynn Tatnell, Mark Tarrant, Nadine Dyar, Nicola Brennan, Paul Dieppe, Peta Foxall, Richard Jones, Robert Lewis, Ruth Riley, Sarah Huline-Dickens, Theresa Hewitt-Moran and Vik Mohan. We would also like to thank the members of our steering group (alphabetically by first name): Barbara Jones, Dave Richards (Chair) and Nigel Reed, for their excellent advice and guidance throughout. The two artist collaborators are Ian Williams, GP and comics artist, and Matilda Tristram, animator, illustrator and writer; and the film maker is Phil Gurr, Owner/Director at Digitalcut and Exeter Web Video. Finally, we would like to thank Marilyn Evans for her administrative support.
Abbreviations
- CMOcs
Context-Mechanism-Outcome configurations
- ICD
International Classification of Diseases
Authors’ contributions
KM and MP conceptualised the study with input from SB, CP, DC, MJ and GW. DC wrote the first draft of this manuscript. SB, CP, KM, MP and GW critically contributed to and refined this manuscript. SB, CP, DC, KM, MP, MJ and GW read and approved the final manuscript.
Funding
This project is funded by the National Institute for Health Research (NIHR) HS&DR (project number 16/53/12) and supported by the NIHR Collaboration for Leadership in Applied Health Research and Care South West Peninsula. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Availability of data and materials
The authors will share the secondary data identified by this research.
Ethics approval and consent to participate
Secondary research. Ethical approval is not required.
Consent for publication
Not applicable.
Competing interests
Geoff Wong is the Joint Deputy Chair of the National Institute for Health Research Health Technology Assessment Programme Prioritisation Committee Panel A (Out of hospital). Mark Pearson is a member of the NIHR Health Services & Delivery Research (HS&DR) Funding Committee. The other authors declare that they have no competing interests.
Footnotes
For more information, please visit http://sites.exeter.ac.uk/cup/.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12916-020-01532-x.
References
- 1.Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358:j3360. doi: 10.1136/bmj.j3360. [DOI] [PubMed] [Google Scholar]
- 2.Cozens JF. Stress in health professionals: psychological and organisational causes and interventions. 1999. [Google Scholar]
- 3.The Lancet Physician burnout: the need to rehumanise health systems. Lancet. 2019;394(10209):1591. doi: 10.1016/S0140-6736(19)32669-8. [DOI] [PubMed] [Google Scholar]
- 4.The Lancet Physician burnout: a global crisis. Lancet. 2019;394(10193):93. doi: 10.1016/S0140-6736(19)31573-9. [DOI] [PubMed] [Google Scholar]
- 5.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kemp S, Hu W, Bishop J, Forrest K, Hudson JN, Wilson I, et al. Medical student wellbeing - a consensus statement from Australia and New Zealand. BMC Med Educ. 2019;19(1):69. doi: 10.1186/s12909-019-1505-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elton C. Doctors can’t care for patients if the system doesn’t care for them—an essay by Caroline Elton. BMJ. 2019;364:l968. doi: 10.1136/bmj.l968. [DOI] [PubMed] [Google Scholar]
- 9.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 10.Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, et al. ‘Care Under Pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open. 2018;8:e021273. 10.1136/bmjopen-2017-021273. [DOI] [PMC free article] [PubMed]
- 11.Wilkinson E. UK NHS staff: stressed, exhausted, burnt out. Lancet. 2015;385(9971):841–2. [DOI] [PubMed]
- 12.Balme E, Gerada C, Page L. Doctors need to be supported, not trained in resilience. BMJ. 2015;351:h4709.
- 13.Cheshire A, Ridge D, Hughes J, Peters D, Panagioti M, Simon C, et al. Influences on GP coping and resilience: a qualitative study in primary care. Br J Gen Pract. 2017;67(659):e428–e436. 10.3399/bjgp17X690893. [DOI] [PMC free article] [PubMed]
- 14.Gerada C. The wounded healer—why we need to rethink how we support doctors. BMJ. 2015;351:h3526. doi: 10.1136/bmj.h3526. [DOI] [Google Scholar]
- 15.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 16.Robinson F. Why I . . . launched a lunch club for trainees. BMJ. 2019;365:l2377. doi: 10.1136/bmj.l2377. [DOI] [PubMed] [Google Scholar]
- 17.Rimmer A. Staff stress levels reflect rising pressure on NHS, says NHS leaders. BMJ. 2018;360:k1074. doi: 10.1136/bmj.k1074. [DOI] [PubMed] [Google Scholar]
- 18.Thornton J. NHS staff survey: just 29% of organisations take health and wellbeing seriously. BMJ. 2019;364:l924. doi: 10.1136/bmj.l924. [DOI] [PubMed] [Google Scholar]
- 19.Carrieri D. “Care Under Pressure”: how can we achieve wellbeing at work for doctors? TheBMJOpinion https://blogs.bmj.com/bmj/2019/02/01/care-under-pressure-how-can-we-achieve-wellbeing-at-work-for-doctors/2019.
- 20.Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift: BioMed Central. 2018;16:95. 10.1186/s12916-018-1089-4. [DOI] [PMC free article] [PubMed]
- 21.Pawson R, Tilley N, Tilley N. Realistic evaluation: sage. 1997. [Google Scholar]
- 22.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist synthesis: an introduction. ESRC research methods programme. Manchester: University of Manchester; 2004. [Google Scholar]
- 23.Wong G, Greenhalgh T, Westhorp G, Pawson R. Health Services and Delivery Research. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses - Evolving Standards) project. Southampton: NIHR Journals Library Copyright (c) Queen's Printer and Controller of HMSO 2014; 2014. [PubMed] [Google Scholar]
- 24.Pawson R. Evidence-based policy: a realist perspective. Thousand Oaks: Sage; 2006.
- 25.McNeill KG, Kerr A, Mavor KI. Identity and norms: the role of group membership in medical student wellbeing. Perspect Med Educ. 2014;3(2):101–112. doi: 10.1007/s40037-013-0102-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haslam C, Jetten J, Cruwys T, Dingle G, Haslam A. The new psychology of health: unlocking the social cure. London: Routledge; 2018.
- 27.Cawsey MJ, Ross M, Ghafoor A, et al. Implementation of Learning from Excellence initiative in a neonatal intensive care unit Archives of Disease in Childhood - Fetal and Neonatal Edition. 2018;103:F293. [DOI] [PubMed]
- 28.Haizlip J, May N, Schorling J, Williams A, Plews-Ogan M. Perspective: the negativity bias, medical education, and the culture of academic medicine: why culture change is hard. Acad Med. 2012;87(9):1205–1209. doi: 10.1097/ACM.0b013e3182628f03. [DOI] [PubMed] [Google Scholar]
- 29.Gerada C. Clare Gerada: dissecting resilience. BMJ. 2018;363:k4974. doi: 10.1136/bmj.k4974. [DOI] [PubMed] [Google Scholar]
- 30.Spiers J, Buszewicz M, Chew-Graham CA, Gerada C, Kessler D, Leggett N, et al. Barriers, facilitators, and survival strategies for GPs seeking treatment for distress: a qualitative study. Br J Gen Pract. 2017;67(663):e700–e7e8. doi: 10.3399/bjgp17X692573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Godlee F. The modern firm. BMJ. 2019;365:l4173. doi: 10.1136/bmj.l4173. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search 1: Interventions to reduce mental ill health.
Additional file 2. Table describing the stakeholder group meetings.
Additional file 3. Table describing the included studies.
Additional file 4. Examples of the citations that provide evidence for each CMOc.
Data Availability Statement
The authors will share the secondary data identified by this research.