Abstract
Background. Human ficolin 2 (encoded by FCN2) and mannose-binding lectin (encoded by MBL2) bind to specific pathogen-associated molecular patterns, activate the complement lectin cascade in a similar manner, and are associated with several infectious diseases. Our recently published study established certain FCN2 promoter variants and ficolin-2 serum levels as protective factors against schistosomiasis.
Methods. We used the Nigerian cohort from our recently published study, which included 163 Schistosoma haematobium–infected individuals and 183 matched healthy subjects, and investigated whether MBL deficiency and MBL2 polymorphisms are associated with schistosomiasis.
Results. MBL serum levels were significantly higher in controls and were associated with protection (P < .0001). The −550H minor allele was significantly associated with protection (P = .03), and the heterozygous genotypes −550HL were observed to confer protection (P = .03). The MBL2*HYPA haplotype was significantly associated with protection (P = .03), with significantly higher serum MBL levels in controls (P = .00073). The heterozygous 6-bp deletion in the promoter was observed to be a susceptibility factor in schistosomiasis (P = .03).
Conclusions. In agreement with findings from our recently published study, the findings reported here support the observation that MBL is also associated with protection in schistosomiasis.
Keywords: MBL2, genotypes, haplotypes, serum level, Schistosomiasis
Schistosomiasis is one of the neglected tropical diseases targeted for elimination by the World Health Organization and is caused by different species of the trematode genus Schistosoma. Of the 207 million estimated cases of schistosomiasis worldwide, 93% (192 million) occur in sub-Saharan Africa, with Nigeria recording the highest number of cases (29 million), followed by the United Republic of Tanzania (19 million) and the Democratic Republic of the Congo and Ghana (15 million each) [1]. Although various species cause schistosomiasis, Schistosoma haematobium is the most ubiquitous species in sub-Saharan Africa, contributes to urogenital schistosomiasis, and is associated with severe pathological conditions, such as hematuria, bladder cancer, and hydronephrosis [2–4]. S. haematobium infection represents a massive public health problem in Nigeria. It is endemic in many states of the federation, causing immense morbidity, as measured by disability-adjusted life-years, and represents a massive public health problem in Nigeria. The most-affected age group is school-aged children who are constantly in contact with cercariae-infected water [5]. Rapid reinfection [6], a limited supply of praziquantel, and the failure of the host immune system to mount parasite-specific immune responses add to the disease burden [7].
The prevalence of schistosomiasis within communities of endemicity may be influenced by several exposure-related factors, such as local environment and behavior, and by genetic factors related to individual susceptibility [8]. In schistosomiasis, studies have documented that recurrent infections in certain communities are subject to individual variability [9]. Schistosomes are complex multicellular helminthes with different developmental stages in the human host. S. haematobium in all developmental stages carries glycoconjugates that interact with innate immune recognition elements, such as mannose-binding lectin (MBL) and ficolins. Earlier studies have demonstrated that Schistosoma organisms exhibit different glycoproteins on their tegument [10], and carbohydrate moieties remain a potential target for MBL [11]. Moreover, in vitro studies have documented the complement-mediated killing of Schistosoma mansoni in all life stages of the parasite [12]. In addition, our previous studies have demonstrated that MBL competently binds to the sugar moieties of S. mansoni cercariae and adult worms in vitro and, with MBL-associated serine protease 1 (MASP1) and MASP2, that it is capable of interacting with the Schistosoma tegument, thereby activating the complement cascade [13].
MBL is a circulating innate immune recognition protein that is involved in innate immune defense against pathogens [14, 15]. In humans, the MBL encoded by MBL2 is located on chromosome 10. Three identified single-nucleotide polymorphisms (SNPs) in exon 1 of MBL2, at codons 52(MBL2*D), 54(MBL2*B), and 57(MBL2*C), interfere with the formation of higher MBL oligomers, leading to alterations in functional activity of the protein and their circulating levels [16, 17]. The haplotype of variant alleles is designated as O, whereas the haplotype of the common MBL2 allele is designated as A [18]. In addition, 2 strongly linked SNPs in the proximal promoter (L/H and X/Y), as well as a SNP in the 5′ untranslated region (UTR; P/Q), together are linked to 3 independent nonsynonymous SNPs (ie, B, C, and D) to form “secretor haplotypes,” which have been shown to partially account for alterations in complement activation and for decreased circulating levels of MBL [19]. In particular, a base substitution at −221 (G to C; promoter allele X) is associated with a lower MBL concentration in serum [11]. Studies have documented that these SNPs contribute to the circulating levels against the 7 common secretor haplotypes (ie, HYPA, HYPD, LXPA, LYPA, LYPB, LYQA, and LYQC) [11]. HYPA, LYQA, and LYPA are associated with high expression of MBL, whereas LXPA, HYPD, LYPB, and LYQC are associated with low expression of MBL [20]. These secretor haplotypes modulate the MBL concentration in healthy individuals, from levels that are undetectable to levels that are several thousand times greater than the mean level [14, 21]. There is increasing evidence that MBL2 polymorphisms are associated with infections in pediatric patients, severe acute respiratory syndrome, Cryptosporidium infection, human immunodeficiency virus (HIV) infection in children, infections in Polish neonates, visceral leishmaniasis, hepatitis B, malaria and placental malaria, leprosy, and rheumatoid arthritis [22–37].
Despite the documented interaction of S. mansoni with the MBL-MASP complex in vitro [38], there is no existing information on the association between functional MBL2 variants and serum MBL levels and schistosomiasis outcomes. We recently demonstrated that certain FCN2 promoter variants and ficolin-2 serum levels protected against schistosomiasis. Both ficolins and MBL are similar immune recognition proteins that can bind to carbohydrate sugars, such as N-acetylglucosamine, N-acetylgalactosamine, and glucose, of adult worms and cercariae [39]. Therefore, we hypothesized that MBL plays an analogous role in S. haematobium infection. In this study, we investigated the role of MBL2 polymorphisms and serum MBL levels in S. haematobium infection. We examined the possible contribution of functional MBL2 variants (2 strongly linked SNPs in the proximal promoter, a 6-bp deletion in the promoter, 1 SNP in the 5′ UTR, and 3 SNPs in exon 1) and investigated the relationship of genetic polymorphisms to circulating serum MBL levels in a Nigerian cohort.
PATIENTS AND METHODS
Study Design and Sample Collection
We recruited 346 individuals blindly, irrespective of their infection status, from 2 communities in southwest Nigeria, Ilewo Orile (Abeokuta North) and Ore (Osogbo), in which there was a known history of S. haematobium infection. After parasitological and serological testing (for total anti-schistosome immunoglobulin G [IgG] antibodies), the cohort was divided into the following 3 groups: the case group (hereafter, the “SEP group”), the first control group (hereafter, the “SELP group”), and the second control group (hereafter, the “SELN group”).
The SEP group was composed of 163 individuals who tested positive for Schistosoma eggs. The ratio of males to females was 90 to 73; 99 (61%) were children, of whom 55 (34%) were males, and 44 (27%) were females. The mean age (±SD) was 17.1 ± 12.4 years (range, 4–70 years). Hematuria was detected in 90%, and the mean parasite count was 1595 parasites (range, 20–27 000 parasites).
The SELP group was composed of 119 individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (ELISA). The ratio of males to females was 58 to 61; 23 (19%) were children, of whom 10 (8%) were males, and 13 (11%) were females. The mean age (±SD) was 33.6 ± 18.8 years (range, 4–75 years). Hematuria was detected in 2.4%.
The SELN group was composed of 64 individuals who tested negative for Schistosoma antigens by ELISA and negative for Schistosoma eggs. The ratio of males to females was 40 to 24; 31 (48%) were children, of whom 23 (36%) were males, and 8 (13%) were females. The mean age (±SD) was 20.2 ± 17.2 years (range, 4–71 years). Hematuria was not detected in any subject.
All subjects were of Yoruba ethnicity. Additional parasitological data, serological data, and characteristics of this cohort are reported elsewhere [39].
About 10 mL of urine from all participants was collected into a sterile, labeled container and examined for the presence of S. haematobium eggs, and about 5 mL of blood was collected for serological assays and DNA extraction. Details about the study were provided in the local language to potential participants, and informed consent was obtained before recruitment into the study; for children, consent was obtained from parents and/or guardians. Ethics approval was obtained from the Ethical Committee of Ministry of Health, Abeokuta Ogun State, Nigeria.
Serological Assays
Serological assays were performed using a modified ELISA protocol to detect total anti-schistosome IgG antibodies, as previously described [40]. Serum levels of MBL were measured in patients and healthy control subjects, using an ELISA kit for human MBL (Hycult Biotech, Uden, the Netherlands).
MBL2 Genotyping
Genomic DNA was extracted using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany). The MBL2 promoter polymorphisms at −550G > C, −221G > C, and the 5′ UTR +4C > T and the exon 1 polymorphisms at codons 52C > T, 54G > A, and 57G > A were amplified by polymerase chain reaction (PCR), using primer pairs spanning from the promoter region through exon 1. The primers used were as follows: promoter, forward: 5′-GCCAGAAAGTAGAGAGGTATTTAGCAC-3′; internal primer exon 1, forward: 5′-CAGGTGTCTAGGCACAGATGAACC-3′; and exon 1, reverse: 5′-CCAACACGTACCTGGTTCCC-3′. In brief, 10 ng of genomic DNA was amplified in a 20-µL volume of reaction mixture containing 1× PCR buffer (20 mM Tris-HCl [pH 8.4], 50 mM KCl, and 1.5 mM of MgCl2), 0.125 mM of dNTPs, 0.25 mM of each primer, and 1 U Taq DNA polymerase (Qiagen, Hilden, Germany) on a PTC-200 Thermal cycler (MJ Research, United States). Thermal cycling parameters for amplification of both exon 1 and promoter regions were 94°C for 5 minutes (initial denaturation); 35 cycles of 30 seconds at 94°C (for denaturation), 30 seconds at 68°C (for annealing), 90 seconds at 72°C (for extension); and 120 second at 72°C (for final extension). PCR products were cleaned up by use of Exo-SAP-IT (USB, Affymetrix, United States), and 1 µL of the purified product was directly used as a template for sequencing, using the BigDye terminator v. 1.1 cycle sequencing kit (Applied Biosystems, United States) on an ABI 3130XL DNA sequencer, according to the manufacturers' instructions. Polymorphisms were identified by assembling the sequences with respective reference sequences (NG_008196.1), using CodonCode Aligner, version 4.0 (available at: http://www.codoncode.com/), and were reconfirmed visually from their respective electropherograms.
Statistical Analysis
Data were analyzed using Intercooled Stata, version 9.1, and the level of significance was set as a P value of < .05. A Kruskal-Wallis test was used to analyze the correlation of serum MBL levels to MBL2 variants. A 2-tailed Fischer exact test was performed to determine the differences in allele frequencies and genotype distributions. The Benjamini-Hochberg procedure was used for correction of P values involving multiple comparisons. Genotype or haplotype frequencies were analyzed by simple gene counting and the expectation-maximum algorithm, and the statistical significance of deviations from Hardy-Weinberg equilibrium was tested using the random-permutation procedure, as implemented in Arlequin software, version 3.5.1.2 (available at: http://cmpg.unibe.ch/software/arlequin3/). Linkage disequilibrium analysis was performed using Haploview, version 3.2.
RESULTS
MBL2 Gene Polymorphisms and S. haematobium Infection
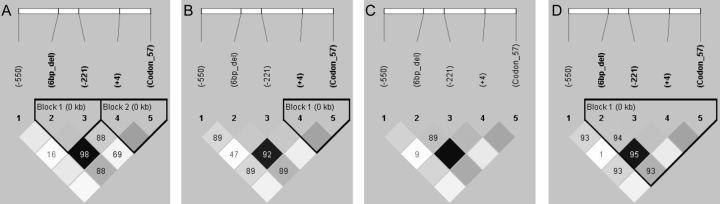
Both genotype and allele frequencies for all analyzed functional MBL2 SNPs in each respective group were in Hardy-Weinberg equilibrium. The distribution of MBL2 genotypes and allele(s) in the cohort are shown in Table 1. Linkage disequilibrium patterns of studied MBL2 variants, along with the observed 6-bp deletion in the SEP group, the SELP group, the SELN group, and the SELP and SELN groups combined are shown in Figure 1. The 6-bp deletion was in linkage disequilibrium with the promoter variant +4C/T (P/Q) in all studied subgroups.
Table 1.
Distribution of MBL2 Genotypes and Alleles Among Cases and Controls
| SNP Position | Genotype | Subjects, No. (%), by Study Group(s) |
SEP vs SELN |
SEP vs (SELP + SELN) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| SEP | SELP | SELN | SELP + SELN | OR (95% CI) | P a | OR (95% CI) | P a | ||
| (n = 163) | (n = 119) | (n = 64) | (n = 183) | ||||||
| rs11003125 (−550G/C) | |||||||||
| CC | LL | 149 (91.4) | 101 (84.9) | 51 (79.7) | 152 (83.1) | 2.7 (1.08–6.65) | .02 | 2.1 (1.06–4.59) | .03 |
| GC | HL | 13 (8) | 17 (14.3) | 13 (20.3) | 30 (16.4) | 0.34 (.13–.86) | .01 | 0.44 (.20–.91) | .03 |
| GG | HH | 1 (0.6) | 1 (0.8) | 0 | 1 (0.5) | … | NS | … | |
| C | L | 311 (95.4) | 219 (92) | 115 (89.8) | 334 (91.3) | … | … | ||
| G | H | 15 (4.6) | 19 (8) | 13 (10.2) | 32 (8.7) | 0.42 (.18–1.0) | .048 | 0.50 (.24–.98) | .03 |
| rs7096006 (−221G/C) | |||||||||
| GG | YY | 126 (77.3) | 98 (82.3) | 46 (71.9) | 144 (78.7) | … | … | ||
| GC | YX | 33 (20.2) | 19 (16) | 15 (23.4) | 34 (18.6) | … | … | ||
| CC | XX | 4 (2.5) | 2 (1.7) | 3 (4.7) | 5 (2.7) | … | NS | … | |
| G | Y | 285 (87.4) | 215 (90.3) | 107 (83.6) | 322 (88) | … | … | ||
| C | X | 41 (12.6) | 23 (9.7) | 21 (16.4) | 44 (12) | … | … | ||
| rs7095891 (+4C/T) | |||||||||
| CC | PP | 23 (14.1) | 15 (12.6) | 18 (28.1) | 33 (18.1) | 0.4 (.2–.9) | .02 | … | |
| CT | PQ | 94 (57.7) | 61 (51.3) | 24 (37.5) | 85 (46.4) | 2.27 (1.2–4.31) | .02 | … | |
| TT | 46 (28.2) | 43 (36.1) | 22 (34.4) | 65 (35.5) | … | NS | … | ||
| C | P | 140 (42.9) | 91 (38.2) | 60 (46.9) | 151 (41.3) | … | … | ||
| T | Q | 186 (57.1) | 147 (61.8) | 68 (53.1) | 215 (58.7) | … | NS | … | |
| MBL2* exon 1 (codon 57) | |||||||||
| GG | AA | 81 (49.7) | 56 (46.2) | 35 (54.7) | 91 (49.7) | … | … | ||
| GA | AO | 71 (43.6) | 50 (42.9) | 27 (42.2) | 77 (42.0) | … | … | ||
| AA | OO | 11 (6.7) | 13 (10.9) | 2 (3.1) | 15 (8.3) | … | NS | … | |
| G | A | 233 (71.5) | 162 (68.1) | 97 (75.8) | 259 (70.8) | … | … | ||
| A | O | 93 (28.5) | 76 (31.9) | 31 (24.2) | 107 (29.2) | … | … | ||
| 6-bp deletion (−338 to −332) | |||||||||
| wt/wt | 25 (15.3) | 17 (14.3) | 17 (26.6) | 34 (18.6) | … | NS | … | ||
| wt/del | 92 (56.5) | 56 (47) | 24 (37.5) | 80 (43.7) | 2.15 (1.1–4.09) | .03 | … | ||
| del/del | 46 (28.2) | 46 (38.7) | 23 (35.9) | 69 (37.7) | … | NS | … | ||
| wt | 142 (43.5) | 90 (37.8) | 58 (45.5) | 148 (40.4) | … | NS | … | ||
| del | 184 (56.5) | 148 (62.2) | 70 (54.5) | 218 (59.6) | … | … | |||
| Promoter (−221) + exon 1 | |||||||||
| YA/YA | 55 (33.7) | 43 (36.1) | 19 (29.7) | 62 (33.9) | … | … | |||
| YA/YO | 60 (36.8) | 42 (35.4) | 25 (39.1) | 67 (36.6) | … | … | |||
| YO/YO | 11 (6.7) | 13 (10.9) | 2 (3.1) | 15 (8.2) | … | … | |||
| XA/YA | 22 (13.5) | 11 (9.2) | 13 (20.3) | 24 (13.1) | … | NS | … | ||
| XA/YO | 11 (6.7) | 8 (6.7) | 2 (3.1) | 10 (5.5) | … | … | |||
| XA/XA | 4 (2.4) | 2 (1.7) | 3 (4.7) | 5 (2.7) | … | … | |||
Percentages may not sum to 100%, because of rounding errors. Study groups were as follows: the SEP group (cases) was composed of individuals who tested positive for Schistosoma eggs, the SELP group (controls) was composed of individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (ELISA), and the SELN group (controls) was composed of individuals who tested negative for Schistosoma antigens by ELISA and negative for Schistosoma eggs.
Abbreviations: CI, confidence interval; NS, not significant; OR, odds ratio.
a Adjusted by the Benjamini-Hochberg procedure.
Figure 1.
Linkage disequilibrium pattern of MBL2 variants in individuals who tested positive for Schistosoma eggs (the SEP group [cases]; A), individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (ELISA; the SELP group [controls]; B), individuals who tested negative for Schistosoma antigens by ELISA and negative for Schistosoma eggs (the SELN group [controls]; C), and the SELP and SELN groups combined (D). Empty squares indicate a high degree of linkage disequilibrium (D’ = 1). Numbers indicate the D’ value expressed as a percentile. The dense shading indicates the r2 value. The haplotype block is outlined by a solid line.
Significant differences were observed either in genotypes or allelic distributions between the SEP group and both the SELN group alone and the SELP and SELN groups combined for the −550G/C variant. The homozygous variant LL (−550CC) genotype was observed more frequently in the SEP group, compared with the SELN group alone (odds ratio [OR], 2.7; 95% CI, 1.08–6.65; P = .02) and the SELP and SELN groups combined (OR, 2.1; 95% CI, 1.06–4.59; P = .03), suggesting that it is associated with an increased risk for S. haematobium infection (Table 1). The heterozygous genotype HL (−550GC) was observed less frequently in the SEP group, compared with the SELN group alone (OR, 0.34; 95% CI, .13–.86; P = .01) and the SELP and SELN groups combined (OR, 0.44; 95% CI, .20–.91; P = .03), suggesting that it might be protective against S. haematobium infection. The minor allele −550H was observed more frequently in the SELN group alone (OR, 0.42; 95% CI, .18–1.0; P = .048) and the SELP and SELN groups combined (OR, 0.5; 95% CI, .24–.98; P = .03), compared with the SEP group (Table 1). In exon 1, heterozygous genotype PQ (+4CT) was observed more frequently in the SEP group, compared with the SELN group (OR, 2.27; 95% CI, 1.2–4.31; P = .02). The homozygous genotype PP (+4CC) was observed less frequently in the SEP group, compared with the SELN group (OR, 0.4; 95% CI, .2–.9; P = .02). No significant differences in any other genotype distribution were observed when the SEP group was compared with the SELP group (data not shown). The heterozygous 6-bp deletion in the promoter region (−338 to −332) was more frequent in the SEP group, compared with the SELN group (OR, 2.15; 95% CI, 1.1–4.09; P = .01).
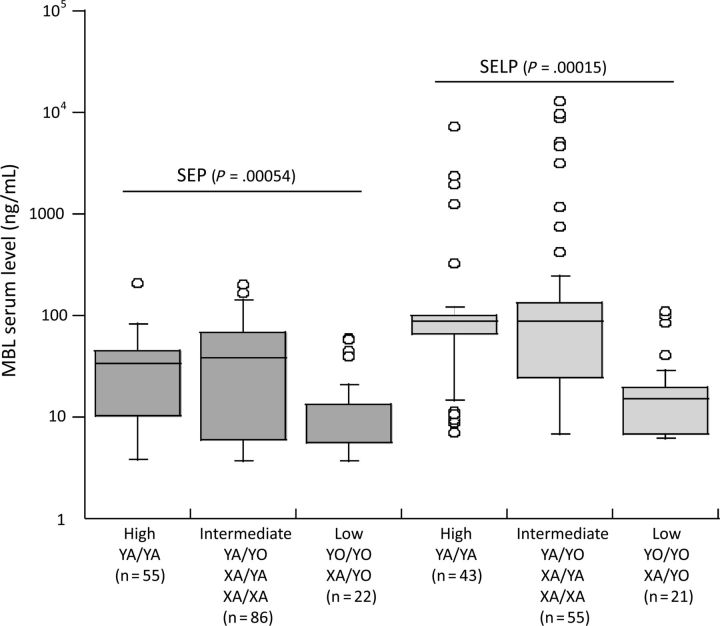
No significant differences were observed for other genotype comparisons between the cases and both control groups. We only observed variants at codon 57(MBL2*C), and no variants were observed at codons 52(MBL2*D) and 54(MBL2*B) in all the studied subgroups. When the combined genotypes for variant −221G/C and exon 1 (at codons 52[MBL2*D], 54[MBL2*B], and 57[MBL2*C]) were investigated for their influence in serum MBL levels (high MBL producers [YA/YA], intermediate producers [YA/YO, XA/XA, and XA/YA], and low producers [YO/YO, XA/YO, and XA/XO]), we observed no significant differences in comparisons between cases and controls (Table 1).
The reconstructed MBL2 haplotypes and the observed distribution in the Nigerian cohort are summarized in Table 2. We observed only 5 secretor haplotypes in our study. The MBL2 haplotypes were divided into those associated with high expression (LYPA + LYQA + HYPA) and those associated with low expression (LYQC + LXPA) of MBL. No significantly different distributions were observed (Table 2). The reconstructed haplotypes were marginally significantly different in comparisons between the SEP group and the SELN group alone (OR, 0.4; 95% CI, .18–1; P = .048) and the SELP and SELN groups combined (OR, 0.5; 95% CI, .25–98; P = .03), providing genetic clues about a possible factor of S. haematobium susceptibility (Table 2). No significant differences in haplotype distribution were observed between the SEP group and the SELP group (data not shown).
Table 2.
Distribution of MBL2 Haplotypes in Cases and Controls
| Haplotype | Haplotypes, No. (%), by Study Group(s) |
SEP vs SELN |
SEP vs (SELP + SELN) |
|||||
|---|---|---|---|---|---|---|---|---|
| SEP (n = 326) | SELP (n = 238) | SELN (n = 128) | SELP + SELN (n = 366) | OR (95% CI) | P a | OR (95% CI) | P a | |
| MBL2* LXPA | 41 (12.6) | 23 (9.7) | 21 (16.4) | 44 (12) | … | NS | … | NS |
| MBL2* LYQC | 93 (28.5) | 77 (32.3) | 31 (24.2) | 108 (29.5) | … | NS | … | NS |
| MBL2* LYQA | 93 (28.5) | 70 (29.4) | 37 (28.9) | 107 (29.3) | … | NS | … | NS |
| MBL2* HYPA | 15 (4.6) | 19 (8) | 13 (10.2) | 32 (8.7) | 0.4 (.18–1) | .048 | 0.5 (.25–.98) | .03 |
| MBL2* LYPA | 84 (25.8) | 49 (20.6) | 26 (20.3) | 75 (20.5) | … | NS | … | NS |
| Low expression of MBL2* | ||||||||
| LYQC + LXPA | 134 (41.1) | 100 (42) | 52 (40.6) | 152 (41.5) | … | NS | … | NS |
| High expression of MBL2* | ||||||||
| HYPA + LYQA + LYPA | 192 (58.9) | 138 (58) | 76 (59.4) | 214 (58.5) | … | NS | … | NS |
Percentages may not sum to 100%, because of rounding errors. Study groups were as follows: the SEP group (cases) was composed of individuals who tested positive for Schistosoma eggs, the SELP group (controls) was composed of individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (ELISA), and the SELN group (controls) was composed of individuals who tested negative for Schistosoma antigens by ELISA and negative for Schistosoma eggs.
Abbreviations: CI, confidence interval; NS, not significant; OR, odds ratio.
a Adjusted by the Benjamini-Hochberg procedure.
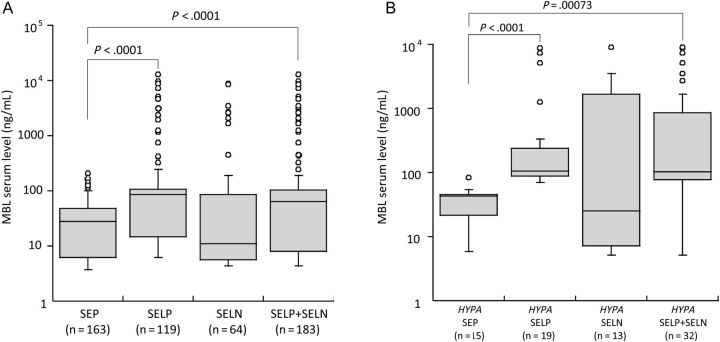
MBL Serum Levels and S. haematobium Infection
The serum MBL levels varied significantly between the SEP and SELP groups (P < .0001; Figure 2A). Also, the serum MBL levels were significantly higher in the SELP and SELN groups combined, compared with the SEP group (P < .0001; Figure 2A). The median MBL levels detected within groups were 27.6 ng/mL (range, 3.3–209 ng/mL) for the SEP group, 84.06 ng/mL (range, 6.13–13 122 ng/mL) for the SELP group, and 11.24 ng/mL (range, 4.38–8936 ng/mL) for the SELN group. Similar results from our recently published study demonstrated that higher serum ficolin-2 levels shield against schistosomiasis [39]. The serum MBL level of the reconstructed MBL2*HYPA haplotype for the SEP group was significantly lower than that for the SELP group alone (P < .0001) and the SELP and SELN groups combined (P < .0001; Figure 2B). We observed a significantly different distribution of serum MBL levels both in the SEP group and the SELP group among the investigated genotypes that were associated with differential serum MBL levels (Figure 3). In both observed distributions, the genotype YA/YA (high MBL producers) had an increased MBL levels, compared with the other genotypes in the studied population. No significant correlations were observed with the egg counts and serum levels (data not shown).
Figure 2.
A, Mannose-binding lectin (MBL) serum levels in individuals who tested positive for Schistosoma eggs (the SEP group [cases]), individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (ELISA; the SELP group [controls]), individuals who tested negative for Schistosoma antigens by ELISA and negative for Schistosoma eggs (the SELN group [controls]), and the SELP and SELN groups combined. B, MBL serum levels in individuals with HYPA haplotype in cases and controls.
Figure 3.
Mannose-binding lectin (MBL) serum levels according to combined genotypes of the −221 promoter region and exon 1 of MBL2 in individuals who tested positive for Schistosoma eggs (the SEP group) and individuals who tested positive for Schistosoma antigens by enzyme-linked immunosorbent assay (the SELP group). Genotypes were divided into high MBL-producing genotypes (YA/YA), intermediate MBL-producing genotypes (YA/YO, XA/YA, and XA/XA), and low MBL-producing genotypes (YO/YO and XA/YO).
DISCUSSION
To the best of our knowledge, this is the first study that investigated the role of MBL2 functional gene polymorphisms and MBL serum levels in schistosomiasis susceptibility. In our recent study, we demonstrated that FCN2 polymorphisms and ficolin-2 levels influence the outcome of schistosomiasis [39]. Similar to ficolins, MBL is an innate immune recognition protein that plays a vital role during the early phase of infection and pathogen recognition. Additionally, our studies have documented the involvement of MBL-activated complement in the response to Schistosoma antigens in vitro [13]. Therefore, in this study, we hypothesized that the sugar-rich surface of Schistosoma organisms is a good target for MBL and that single-locus substitutions in MBL2 resulting in variation in MBL production would eventually affect the disease outcome. In this study, we investigated the possible association of MBL serum levels and MBL2 variants in a case-control study, using 2 independent control groups. The classification of the control group is indispensable in Schistosoma-endemic areas, as it is difficult to differentiate individuals with and without a current infection.
MBL deficiency is associated with many diseases and protection against intracellular infections, such as tuberculosis, leprosy, and leishmaniasis [27, 32, 37, 41]. In our study, we observed that promoter genotypes (−550H/L) influence predisposition to schistosomiasis. The heterozygous genotype (−550HL) conferred protection against infection, whereas the homozygous genotype (−550LL) contributed to increased susceptibility. The results remained consistent when egg-positive patients (the SEP group) were compared to individuals in the SELN group, with or without individuals in the SELP group. The −550H minor allele in the studied population decreased the risk of Schistosoma infection. Our results imply that individuals who are heterozygous at promoter position −550H/L are less susceptible to infection. As observed in our study, earlier studies have documented the influence of −550H/L variants on the risk of HIV infection and AIDS progression in Italian children [34] and on prosthetic joint infection in Czech patients [42]. However, another study, which investigated the association of MBL2 variants with Bechet disease in a South Korean population, demonstrated that the patients had lower frequencies of the homozygous genotype (−550LL) [43]. This variation emphasizes that the clinical significance of the MBL2 variants may likely depend on the population and the disease context. We also observed that a noncoding SNP located +4 bp from the transcription start site (+4P/Q) was also observed to influence the predisposition to schistosomiasis, as determined by comparison of the SEP group to the SELN group. The individuals with major allele homozygous genotypes (+4PP) were less susceptible to infection than those in the SELN group, whereas the individuals with heterozygous genotypes (+4PQ) had a higher risk of infection than those in the SELN group. However, we did not observe significant associations with pooled values for the control groups.
In our studied population, we only observed the MBL2*C genotype (codon 57). No significant associations were observed in the distribution of genotypes (MBL2*C independently and with the combined promoter-220 + exon 1) that influences the serum MBL levels. This observed MBL2*C genotype was documented to be the most frequent African MBL2 variant [31], and studies have reported that the MBL2*C variant is associated with placental malaria and malaria in African children [31, 44]. A heterozygous 6-bp deletion (wt/del) in the promoter region was observed to confer increased risk to schistosomiasis in comparisons between the SEP group and the SELN group. These results are in accordance with those of another study, which demonstrated that the 6-bp deletion at position −328 was correlated with HIV type 1 infection [34]. The reconstruction of haplotypes is important to revealing how different combinations of functional polymorphic alleles can interact to modulate their individual effects. Moreover, many studies have shown the effect of MBL2 haplotypes in disease association studies [32, 35, 43]. Stratification of our cohort on the basis of MBL2 haplotype showed that the MBL2*HYPA haplotype was significantly lower in the case group than in controls, elucidating the fact that individuals with these haplotypes had a lower risk of schistosomiasis. Similar results on the influence of MBL2*HYPA haplotypes has been demonstrated in Bechet disease, in pediatric patients with common infectious diseases, and in patients with colon cancer [23, 43, 45].
Investigation of the MBL serum level further confirms the important role of MBL in schistosomiasis. MBL serum levels varied significantly between cases and controls. A significant difference was found between the SEP group and both the SELP group alone and the SELP and SELN groups combined. MBL serum levels were significantly higher in the control groups, compared with the case group, showing that high levels of MBL may have a protective role in reducing the susceptibility to S. haematobium infection and adding further support the view that MBL plays a role in first-line defense against this pathogen. The MBL2*HYPA haplotypes that contributed to a decreased risk of schistosomiasis were also correlated significantly to MBL serum levels. The control groups (the SELP group alone and the SELP and SELN groups combined) had significantly higher MBL serum levels, compared with the case group. MBL2 polymorphisms related to higher MBL levels in serum were associated with decreased susceptibility to respiratory tract infection in children [46] and to SARS coronavirus infection, compared with controls [22]. The role of MBL as a first line of defense in infectious and noninfectious diseases has been documented in many clinical settings. Comparable results from our study were reported in individuals infected with the intestinal protozoan parasite Cryptosporidium, in which MBL2 polymorphisms and haplotypes that were associated with deficient serum MBL levels increased the susceptibility to infection [30]. On the contrary, MBL2 polymorphisms were also reported to play a dual role in leprosy [32]: the wild-type haplotype was shown to increase susceptibility to the disease per se, and defective haplotypes were shown to confer protection against lepromatous and borderline leprosy. Therefore, depending on the type of disease, MBL deficiency may increase susceptibility to intestinal parasite infections, as in cryptosporidium and schistosomiasis, or may be protective against intracellular pathogens, such as Mycobacterium leprae [32]. In our study, a normal MBL level was found to decrease the susceptibility to S. haematobium infection.
In our earlier study, we observed that ficolin-2 gene polymorphisms and ficolin-2 serum level play an important role in the susceptibility to S. haematobium infection [39]. Both MBL and l-ficolin have similar structural templates comprising collagen-like and ligand binding domains that binds specifically to pathogen-associated molecular patterns on the pathogen surface. In association with the MBL-associated serine proteases (MASP1 and MASP2), MBL and l-ficolin initiate the complement lectin cascade, leading to clearance of pathogens by opsonization [47, 48]. A previous study showed that the surfaces of both S. mansoni cercariae and adult worms were recognized specifically by the MBL-MASP complex, suggesting that an interaction between MBL and the parasite results in activation of complement in vitro [13]. Lectin-binding studies of Schistosoma organisms have revealed many different glycoproteins on the surface of the parasite, regardless of life cycle stage and sex [38, 49], and it was shown MBL interacts with these sugar residues on the parasite surface, triggering the host immune response [13, 50]. We clearly observed in this study that higher MBL levels and ficolin-2 levels [39] were predictive of protection from S. haematobium infection.
The study shows that there is still a high prevalence of S. haematobium infection in Nigeria, with children bearing the highest burden. Overall, we demonstrated that MBL2 variants and serum MBL levels are associated with protection against S. haematobium infection. This study, in line with our previous study of ficolins, may provide vital insights about the possible role of MBL, a vital innate immune component of the complement system that regulates Schistosoma infection and may lay the foundation for a testable immunological intervention to control and contain the disease in human populations.
Notes
Acknowledgments.We thank Abass Busari of State Hospital Ijaye, Abeokuta; Sanusi Tawakalitu, Olaolu Abdulazeez, and Adedokun Samuel, of Ladoke Akintola University of Technology, Osogbo, for the technical support; the staff of the Schistosomiasis Control Unit, Ministry of Health, Abeokuta, and the community members, for their participation in the study; Silvelia Grummes, for technical help; and Timo Grau, for help with sequencing.
Financial support. This work was funded by an institutional internal grant, the Alexander von Humboldt Foundation (to O. O.), the Egyptian Ministry of Higher Education (to E. A. O.), and the Vietnamese government (scholarship to H. v. T.).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis. 2006;6:411–25. doi: 10.1016/S1473-3099(06)70521-7. [DOI] [PubMed] [Google Scholar]
- 2.Prevention and control of schistosomiasis and soil-transmitted helminthiasis. World Health Organ Tech Rep Ser. 2002;912:1–57. [PubMed] [Google Scholar]
- 3.Akinwale OP, Oliveira GC, Ajayi MB, Akande DO, Oyebadejo S, Okereke KC. Squamous cell abnormalities in exfoliated cells from the urine of Schistosoma haematobium-infected adults in a rural fishing community in Nigeria. World Health Popul. 2008;10:18–22. doi: 10.12927/whp.2008.19581. [DOI] [PubMed] [Google Scholar]
- 4.van der Werf MJ, de Vlas SJ, Brooker S, et al. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86:125–39. doi: 10.1016/s0001-706x(03)00029-9. [DOI] [PubMed] [Google Scholar]
- 5.Mafe MA, Appelt B, Adewale B, et al. Effectiveness of different approaches to mass delivery of praziquantel among school-aged children in rural communities in Nigeria. Acta Trop. 2005;93:181–90. doi: 10.1016/j.actatropica.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Uneke CJ. Soil transmitted helminth infections and schistosomiasis in school age children in sub-Saharan Africa: efficacy of chemotherapeutic intervention since World Health Assembly Resolution 2001. Tanzan J Health Res. 2010;12:86–99. doi: 10.4314/thrb.v12i1.56366. [DOI] [PubMed] [Google Scholar]
- 7.Yazdanbakhsh M, Sacks DL. Why does immunity to parasites take so long to develop? Nat Rev Immunol. 2010;10:80–1. doi: 10.1038/nri2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinot de MA, Fulford AJ, Kabatereine NB, Ouma JH, Booth M, Dunne DW. Analysis of complex patterns of human exposure and immunity to Schistosoma mansoni: the influence of age, sex, ethnicity and IgE. PLoS Negl Trop Dis. 2010;4:1–10. doi: 10.1371/journal.pntd.0000820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dessein AJ, Couissinier P, Demeure C, et al. Environmental, genetic and immunological factors in human resistance to Schistosoma mansoni. Immunol Invest. 1992;21:423–53. doi: 10.3109/08820139209069383. [DOI] [PubMed] [Google Scholar]
- 10.Hayunga EG, Sumner MP. Expression of lectin-binding surface glycoproteins during the development of Schistosoma mansoni schistosomula. J Parasitol. 1986;72:913–20. [PubMed] [Google Scholar]
- 11.Dommett RM, Klein N, Turner MW. Mannose-binding lectin in innate immunity: past, present and future. Tissue Antigens. 2006;68:193–209. doi: 10.1111/j.1399-0039.2006.00649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasmussen KR, Kemp WM. Schistosoma mansoni: interactions of adult parasites with the complement system. Parasite Immunol. 1987;9:235–48. doi: 10.1111/j.1365-3024.1987.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 13.Klabunde J, Berger J, Jensenius JC, et al. Schistosoma mansoni: adhesion of mannan-binding lectin to surface glycoproteins of cercariae and adult worms. Exp Parasitol. 2000;95:231–9. doi: 10.1006/expr.2000.4539. [DOI] [PubMed] [Google Scholar]
- 14.Ip WK, Takahashi K, Ezekowitz RA, Stuart LM. Mannose-binding lectin and innate immunity. Immunol Rev. 2009;230:9–21. doi: 10.1111/j.1600-065X.2009.00789.x. [DOI] [PubMed] [Google Scholar]
- 15.Kilpatrick DC. Introduction to mannan-binding lectin. Biochem Soc Trans. 2003;31(Pt 4):745–7. doi: 10.1042/bst0310745. [DOI] [PubMed] [Google Scholar]
- 16.Garred P, Larsen F, Madsen HO, Koch C. Mannose-binding lectin deficiency—revisited. Mol Immunol. 2003;40:73–84. doi: 10.1016/s0161-5890(03)00104-4. [DOI] [PubMed] [Google Scholar]
- 17.Garred P, Larsen F, Seyfarth J, Fujita R, Madsen HO. Mannose-binding lectin and its genetic variants. Genes Immun. 2006;7:85–94. doi: 10.1038/sj.gene.6364283. [DOI] [PubMed] [Google Scholar]
- 18.Velavan TP, Boldt AB, Tomiuk J, et al. Variant alleles of the mannose binding lectin 2 gene (MBL2) confer heterozygote advantage within Crohn's families. Scand J Gastroenterol. 2010;45:1129–30. doi: 10.3109/00365521.2010.485324. [DOI] [PubMed] [Google Scholar]
- 19.Madsen HO, Garred P, Thiel S, et al. Interplay between promoter and structural gene variants control basal serum level of mannan-binding protein. J Immunol. 1995;155:3013–20. [PubMed] [Google Scholar]
- 20.Madsen HO, Satz ML, Hogh B, Svejgaard A, Garred P. Different molecular events result in low protein levels of mannan-binding lectin in populations from southeast Africa and South America. J Immunol. 1998;161:3169–75. [PubMed] [Google Scholar]
- 21.Ezekowitz RA, Day LE, Herman GA. A human mannose-binding protein is an acute-phase reactant that shares sequence homology with other vertebrate lectins. J Exp Med. 1988;167:1034–46. doi: 10.1084/jem.167.3.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang H, Zhou G, Zhi L, et al. Association between mannose-binding lectin gene polymorphisms and susceptibility to severe acute respiratory syndrome coronavirus infection. J Infect Dis. 2005;192:1355–61. doi: 10.1086/491479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tao R, Hua CZ, Hu YZ, Shang SQ. Genetic polymorphisms and serum levels of mannose-binding lectin in Chinese pediatric patients with common infectious diseases. Int J Infect Dis. 2012;16:e403–7. doi: 10.1016/j.ijid.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 24.Swierzko AS, Atkinson AP, Cedzynski M, et al. Two factors of the lectin pathway of complement, l-ficolin and mannan-binding lectin, and their associations with prematurity, low birthweight and infections in a large cohort of Polish neonates. Mol Immunol. 2009;46:551–8. doi: 10.1016/j.molimm.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 25.Summerfield JA, Ryder S, Sumiya M, et al. Mannose binding protein gene mutations associated with unusual and severe infections in adults. Lancet. 1995;345:886–9. doi: 10.1016/s0140-6736(95)90009-8. [DOI] [PubMed] [Google Scholar]
- 26.Song LH, Binh VQ, Duy DN, et al. Mannose-binding lectin gene polymorphisms and hepatitis B virus infection in Vietnamese patients. Mutat Res. 2003;522:119–25. doi: 10.1016/s0027-5107(02)00284-1. [DOI] [PubMed] [Google Scholar]
- 27.Santos IK, Costa CH, Krieger H, et al. Mannan-binding lectin enhances susceptibility to visceral leishmaniasis. Infect Immun. 2001;69:5212–5. doi: 10.1128/IAI.69.8.5212-5215.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martiny FL, Veit TD, Brenol CV, et al. Mannose-binding lectin gene polymorphisms in Brazilian patients with rheumatoid arthritis. J Rheumatol. 2012;39:6–9. doi: 10.3899/jrheum.110052. [DOI] [PubMed] [Google Scholar]
- 29.Luty AJ, Kun JF, Kremsner PG. Mannose-binding lectin plasma levels and gene polymorphisms in Plasmodium falciparum malaria. J Infect Dis. 1998;178:1221–4. doi: 10.1086/515690. [DOI] [PubMed] [Google Scholar]
- 30.Kelly P, Jack DL, Naeem A, et al. Mannose-binding lectin is a component of innate mucosal defense against Cryptosporidium parvum in AIDS. Gastroenterology. 2000;119:1236–42. doi: 10.1053/gast.2000.19573. [DOI] [PubMed] [Google Scholar]
- 31.Holmberg V, Onkamo P, Lahtela E, et al. Mutations of complement lectin pathway genes MBL2 and MASP2 associated with placental malaria. Malar J. 2012;11:61. doi: 10.1186/1475-2875-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Messias-Reason IJ, Boldt AB, Moraes Braga AC, et al. The association between mannan-binding lectin gene polymorphism and clinical leprosy: new insight into an old paradigm. J Infect Dis. 2007;196:1379–85. doi: 10.1086/521627. [DOI] [PubMed] [Google Scholar]
- 33.Cedzynski M, Swierzko AS, Kilpatrick DC. Factors of the lectin pathway of complement activation and their clinical associations in neonates. J Biomed Biotechnol. 2012;2012:363246. doi: 10.1155/2012/363246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boniotto M, Crovella S, Pirulli D, et al. Polymorphisms in the MBL2 promoter correlated with risk of HIV-1 vertical transmission and AIDS progression. Genes Immun. 2000;1:346–8. doi: 10.1038/sj.gene.6363685. [DOI] [PubMed] [Google Scholar]
- 35.Boldt AB, Messias-Reason IJ, Lell B, et al. Haplotype specific-sequencing reveals MBL2 association with asymptomatic Plasmodium falciparum infection. Malar J. 2009;8:97. doi: 10.1186/1475-2875-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boldt AB, Luty A, Grobusch MP, et al. Association of a new mannose-binding lectin variant with severe malaria in Gabonese children. Genes Immun. 2006;7:393–400. doi: 10.1038/sj.gene.6364312. [DOI] [PubMed] [Google Scholar]
- 37.Alonso DP, Ferreira AF, Ribolla PE, et al. Genotypes of the mannan-binding lectin gene and susceptibility to visceral leishmaniasis and clinical complications. J Infect Dis. 2007;195:1212–7. doi: 10.1086/512683. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt J. Glycans with N-acetyllactosamine type 2-like residues covering adult Schistosoma mansoni, and glycomimesis as a putative mechanism of immune evasion. Parasitology. 1995;111(Pt 3):325–36. doi: 10.1017/s0031182000081877. [DOI] [PubMed] [Google Scholar]
- 39.Ouf EA, Ojurongbe O, Akindele AA, et al. Ficolin-2 levels and FCN2 genetic polymorphisms as a susceptibility factor in schistosomiasis. J Infect Dis. 2012;206:562–70. doi: 10.1093/infdis/jis396. [DOI] [PubMed] [Google Scholar]
- 40.Knobloch J, Delgado E. Immunodiagnosis of cysticercosis: standardization of ELISA and its application to field conditions. Trop Med Parasitol. 1985;36:157–9. [PubMed] [Google Scholar]
- 41.Cosar H, Ozkinay F, Onay H, et al. Low levels of mannose-binding lectin confers protection against tuberculosis in Turkish children. Eur J Clin Microbiol Infect Dis. 2008;27:1165–9. doi: 10.1007/s10096-008-0573-8. [DOI] [PubMed] [Google Scholar]
- 42.Navratilova Z, Gallo J, Mrazek F, Lostak J, Petrek M. MBL2 gene variation affecting serum MBL is associated with prosthetic joint infection in Czech patients after total joint arthroplasty. Tissue Antigens. 2012;80:444–51. doi: 10.1111/tan.12001. [DOI] [PubMed] [Google Scholar]
- 43.Park KS, Min K, Nam JH, Bang D, Lee ES, Lee S. Association of HYPA haplotype in the mannose-binding lectin gene-2 with Behcet's disease. Tissue Antigens. 2005;65:260–5. doi: 10.1111/j.1399-0039.2005.00363.x. [DOI] [PubMed] [Google Scholar]
- 44.Holmberg V, Schuster F, Dietz E, et al. Mannose-binding lectin variant associated with severe malaria in young African children. Microbes Infect. 2008;10:342–8. doi: 10.1016/j.micinf.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 45.Zanetti KA, Haznadar M, Welsh JA, et al. 3′-UTR and functional secretor haplotypes in mannose-binding lectin 2 are associated with increased colon cancer risk in African Americans. Cancer Res. 2012;72:1467–77. doi: 10.1158/0008-5472.CAN-11-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koch A, Melbye M, Sorensen P, et al. Acute respiratory tract infections and mannose-binding lectin insufficiency in small children. Ugeskr Laeger. 2002;164:5635–40. [PubMed] [Google Scholar]
- 47.Dunkelberger JR, Song WC. Complement and its role in innate and adaptive immune responses. Cell Res. 2010;20:34–50. doi: 10.1038/cr.2009.139. [DOI] [PubMed] [Google Scholar]
- 48.Kilpatrick DC, Chalmers JD. Human L-ficolin (ficolin-2) and its clinical significance. J Biomed Biotechnol. 2012;2012:138797. doi: 10.1155/2012/138797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu X, Stack RJ, Rao N, Caulfield JP. Schistosoma mansoni: fractionation and characterization of the glycocalyx and glycogen-like material from cercariae. Exp Parasitol. 1994;79:399–409. doi: 10.1006/expr.1994.1102. [DOI] [PubMed] [Google Scholar]
- 50.Hokke CH, Yazdanbakhsh M. Schistosome glycans and innate immunity. Parasite Immunol. 2005;27:257–64. doi: 10.1111/j.1365-3024.2005.00781.x. [DOI] [PubMed] [Google Scholar]