Abstract
The involvement of insects in Reticuloendotheliosis virus (REV) transmission was examined by testing insects trapped at commercial farms and by controlled feeding experiments using mosquitoes, Culex pipiens L. and house flies, Musca domestica L. We established sensitive methods of REV detection, including reverse transcription-polymerase chain reaction (PCR) for REV-LTR and REV-gag genes, REV antigenemia measurements by enzyme-linked immunosorbent assay, and virus isolation in tissue cultures. A variety of blood-sucking species of insects were trapped at farms with infected poultry and tested, but none were positive. To rule out the possibility of PCR inhibition by insect RNA, spiking experiments were conducted and no interference was observed. Because Cx. pipiens mosquitoes were trapped frequently at farms, we performed feeding experiments with mosquito females fed on a REV-containing tissue culture medium and chicken blood mixture. Virus was detected in the mosquitoes up to 5 h postfeeding, compared with 96 h in the feeding mixture, indicating that Cx. pipiens can only harbor REV for a short period. House flies were suspected to be involved in the virus transmission because they frequently were trapped on positive farms. In contrast to mosquitoes, REV was harbored within the house fly digestive tract for up to 72 h and could infect chickens, as demonstrated by seroconversion and by detection of viral gag-sequence in the cloaca. The current study is supportive for the role of house flies as a mechanical vector of REV among poultry.
Keywords: Reticuloendotheliosis virus, mechanical transmission, mosquitoes, house flies, chickens
Reticuloendotheliosis virus (REV) is an exogenous C-type retrovirus that infects chickens, turkeys, and other species and causes immunosuppression and tumors. The virus transforms B and T cells (Witter 1997) and is transmitted both vertically and horizontally among gallinaceous birds (Purchase and Witter 1995, Witter 1997). The vertical mode of transmission from hen to chick occurs either via infection of the ovarian germ cells or contaminated oviduct. Horizontal transmission generally is the result of contamination of food or litter by infectious excretions from infected chickens or possibly by insects serving as mechanical vectors. This horizontal transmission occurs during the acute stages of infection (Peterson and Levine 1971, Yuasa et al. 1976, Bagust and Grimes 1979, Bagust et al. 1981, Witter et al. 1981, Witter and Johnson 1985).
Biting insects, such as mosquitoes, have been considered as mechanical vectors (Motha et al. 1984). REV was isolated during late summer and autumn from seven of 39 pools of mosquitoes, mainly Culex quinquefasciatus Say. That study also demonstrated a mechanical transmission between the viremic and sentinel chickens, probably by partially engorged insects. Viremic and sentinel chickens were housed in separate pens. Each week, an insect trap was set from dusk to dawn, and REV-positive insects were trapped from both groups. Interrupted feeding might have occurred resulting in the seroconversion of sentinel birds after being fed upon by partially fed females. Motha et al. (1984) also reported experimental transmission of REV between chickens by Culex annulirostris Skuse; however, transmission by fomites could not be excluded (Sincovic 1983). REV also has been isolated from Triatoma infestans Klug and Ornithodoros moubata Murray shortly after feeding on infected chickens (Thompson et al. 1968). Thompson et al. (1971) later showed that REV was stable for >48 h in several types of insects. However, efforts to culture REV in Aedes albopictus Skuse cells were unsuccessful (Rehacek et al. 1971). Collectively, these studies indicated that a mechanical mode of transmission by insects was possible. As proof of principal, McDaniel et al. (1962, 1964) previously implicated both Aedes aegypti (L.) and Culex pipiens L. in the transmission of chicken sarcomas caused by the Rous sarcoma retrovirus.
The hematophagous insects associated with chickens and turkeys in Israel has been surveyed (Braverman and Rubina 1976, Braverman et al. 2003). Based on references reviewed above and on additional accounts of transmission of nonarboviruses by insects, e.g., avian influenza (Lipkind et al. 1982) and lumpy skin disease (Yeruham et al. 1994, Chihota et al. 2001), our study was undertaken to ascertain the role of arthropods in the transmission of REV. Our study used a combination of new sensitive assays, including virus isolation in tissue culture, reverse transcriptionpolymerase chain reaction (RT-PCR) and REV antigen detection by enzyme-linked immunosorbent assay (ELISA). We provide information based on testing insects caught at farms with infected chickens and on experimental infection of both mosquitoes (Cx. pipiens) and house flies (M. domestica) by feeding on REV solutions. Recently, Calibeo-Hayes et al. (2003) implicated house flies in the mechanical transmission of the turkey Coronavirus.
Materials and Methods
Insect Trapping in Commercial Chicken Farms.
Blacklight traps (DuToit 1944) were placed near the chicken flocks at six different sites at the Coastal Plain of Israel and were operated twice a week. The trapped insects were sorted by species and kept at –70°C until RNA extraction. All of the flocks sampled had been exposed to REV, because they were either REV antibody positive or REV was detected RT-PCR.
Virus.
The REV-S isolate used throughout originated from a 5-mo-old broiler breeder chicken flock. Infected chicken embryo fibroblast (CEF) infected tissue culture provided virus to feed the mosquitoes and house flies. The infectivity of the medium was determined by infecting CEF grown on coverslips. Virus was detected by indirect immunofluorescence (IF) by using monoclonal antibody 11A25 (received from Dr. L. Lee, Avian Disease and Oncology Laboratory, East Lansing, MI) (Davidson et al. 1997).
Feeding Experiments with Mosquitoes.
REV-S from infected tissue culture was mixed with whole chicken blood (1:0.75) (in the presence of 2% Versene as a anticoagulant) and was used to feed mosquitoes as described below. The colonized Cx. pipiens were started from larvae collected at Bet Dagan, Israel.
Mosquitoes were starved overnight and then fed through 1-d-old chick skin. Fifty mosquitoes were fed on one feeding device. At 0, 1, 3, 5, 24, 48, 72, and 96 h postfeeding, ≈25 fully engorged mosquitoes were sampled, observed under a binocular scope for blood content, and then frozen at -70°C until tested for virus. The blood-virus mixture was sampled at similar intervals to serve as control for the virus contained in the engorged mosquitoes. The REV content of mosquitoes was estimated by assaying 25 insects at each time point. The RNA from each sample of 25 insects was purified in one tube. To determine the virus stability in the insectary temperature and the effect of proteolytic enzymes on the chick skin, controls were analyzed at each time interval.
Feeding Experiments with House Flies.
Groups of 100 house flies were starved overnight and then fed on sugar cubes (1 cm3; 2.77 g) wet with 250 μl of REV-infected CEF medium (Braverman et al. 1999). The virus was titrated by seeding 10-fold dilutions on CEF, and the titer was 10–4 by IF assay. The house flies were examined for the virus at 0, 1, 3, 5, 8, 16, 24, 48, 72, and 96 h after feeding. At each time interval, RNA was prepared from whole flies (groups of four flies); outer fly body parts, i.e., legs and head (groups of five flies); dissected digestive tracts (from five flies); and feces collected from groups of five flies from nonabsorbent paper. Concurrently, REV RNA was extracted from the sugar cubes over the 96 h.
Experimental Infection of Chickens by Using REV-Fed House Flies.
Two experimental infections were performed with white Leghorn chickens. The 3.5-mo-old chickens were determined to be free of REV infection by PCR and serum antibodies to REV by ELISA (assay described below). The chickens were injected intramuscularly with 0.5 ml of REV-containing medium. In the first trial, three chickens were infected and three others served as control birds. In the second trial, two birds were infected in a similar, way and one bird was left as a control. The birds in the first trial were sampled at days 0, 7, and 14 postinoculation (p.i.), whereas in the second trial, the birds were sampled on days 1–4 p.i. The samples included blood in anticoagulant (2% EDTA), cloacal swabs, and feces. The feces served for feeding two groups of house flies, each comprised of 10 insects. For the viral genome amplification, the RNA from each group of fed house flies was extracted in two pools of five flies each.
Preparation of RNA and RT-PCR.
The insects were homogenized with a disposable pestle in 100 μl of Tris-EDTA buffer. They were processed in pools of various number, depending on their body size, i.e., 4-5 house flies, 10–25 mosquitoes, and up to 100 Culicoides. RNA was extracted with guanidinium thiocyanate by using TriReagentLS (Molecular Research Center, Inc., Cincinnati, OH) according to the manufacturer’s instructions. We developed the following procedure for amplification. The RNA was denatured at 90°C for 5 min and then reversed transcribed in a 20-μl reaction containing 3.3 μg of 6-mer random primer; dATP, dCTTP, dGTP, and dTTP, each at 200 μM; and 33 U of RNase inhibitor and 25 U Avian myeloblastosis virus reverse transcriptase (Promega, Madison, WI). The reaction was allowed to proceed for 10 min at 23°C, followed by incubation at 42°C for 30 min. The temperature was then raised to 98°C for 7 min, after which the sample was rapidly cooled to 4°C. For PCR, 3 μl of the reverse transcriptase (RT) product was used in the reaction described below.
DNA Preparation, Oligonucleotide Primers, and RT-PCR and PCR Conditions.
The presence of REV in the chicken was assayed by viral provirus amplification, because the virus integrates into the cellular genome as a DNA molecule, which is an obligatory replication state for a retrovirus. The DNA was prepared as described previously (Davidson et al. 1995). The primers R1 and R2 were used to amplify the proviral reticuloendotheliosis-long terminal repeat (REV-LTR) fragment (Aly et al. 1993) with an expected band size is 291 bp.
For the REV detection in both its RNA genomic and proviral form that is present in insects and avian cells, gag gene primers were used (Reiman and Werner 1996).
RT-PCR was performed using 0.5 μg of RNA in a volume of 20 μl. RT was obtained with 3.33 μg of 6-mer random primer (QIAGEN Operon, Alameda, CA), 1 mM dNTP, and 10 U of Super AMV (MGR, Tampa, FL). The mixture was incubated first at 23°C for 10 min and then at 45°C for 25 min, and finally inactivated at 98°C for 8 min. Resulting cDNA (3 μl) was used for amplification.
A 25-μl PCR reaction mixture contained 10 mM Tris-HCl (pH 8.5), 50 mM KCl, 1.5 mM MgCl2, dATP, dCTP, dGTP, and dTTP, each at 200 mM; primers (1.2 mM each); and 0.5 U of Taq polymerase (Advanced Biotechnologies, Inc., Surrey, United Kingdom). PCR cycling parameters were one cycle of 94°C for 1 min; 31 cycles of 94°C for 1 min, 55°C for 1 min, and 72°C for 1 min; followed by a final elongation at 72°C for 10 min (Davidson et al. 1995).
REV Antibody Determination by ELISA.
The assay was performed as described previously (Davidson et al. 1995). Sera were tested on two sections of the same plate, one coated with an REV antigen prepared from a lysate of REV-infected CEF, and the second coated with lysate of uninfected CEF. Sera were tested at a 1:400 dilution on both antigens, and an optical density difference >0.3 was considered positive. This difference in optical density (O.D.) represented a positive/negative ratio >2.
REV Detection in CEF Culture by Immunofluorescence.
Preparation and maintenance of CEF cultures and REV isolation were described previously (Davidson et al. 1997). Samples were inoculated onto CEF cultures and maintained for 6-7 d with media changed every second day. The virus was detected by IF staining as detailed elsewhere (Davidson et al. 1997).
REV Antigen Determination by ELISA.
REV antigen was detected by a sandwich ELISA. ELISA plates (Nunc-Immuno plate F96, Maxisorp 442404) were coated with a rabbit polyclonal REV antibody at a 1:500 dilution in carbonate-bicarbonate buffer. Control wells were coated with normal rabbit sera. The plates then were blocked with 3% bovine serum albumin for 1 h at 37°C. After washes, the insect homogenates were placed on both plates and allowed to adsorb for 18 h at 4°C, after which a chicken polyclonal antiserum to REV (1:400) was added. To obtain a specific reaction, we used a chicken serum with a high content of REV antibodies (REV antibody ELISA of ≈1.0 O.D.).
The next step consisted of an alkaline phosphatase conjugate of rabbit anti-chicken IgG (Sigma, St. Louis, MO), and the reaction was visualized by adding the p-nitrophenyl phosphatase to visualize the immunological sandwich. A threshold of a 0.35–0.4 O.D. was considered a significant difference, above which homogenates from engorged insects were considered positive.
Results
Trapping of Insects from Commercial Chicken Farms.
Insect collections surveyed the biting insect fauna and their REV infection rates at farms with chickens that were seropositive (Table 1). Although mosquitoes and many house flies were collected, none tested positive for REV.
Table 1.
Insects trapped near commercial chicken flocks on the Coastal Plain of Israel that tested negative for REV by PCR

To ascertain that the negative results were not due to the inhibitory effect of the insect RNA, several spiking experiments were performed by using the RNA of mosquitoes (Cx. pipiens), house flies, Culicoides schultzei gp midges, and Phlebotumus spp. sand flies.
Virus Detection in Mosquitoes Fed Blood-Virus Mixtures.
Mosquitoes fed on whole blood mixed with REV were assayed in pools of 25 at 0, 1, 3, 5, 14, 48, 72, and 96 h postfeeding. Pools were tested by CEF tissue culture followed by IF assay and for REV antigen by ELISA. REV also was detected using primers for the gag gene to detect the viral RNA and primers for the LTR gene to detect the proviral DNA that originated from the integrated viral genome in the infected tissue culture cells (Table 2). Controls, including the blood used to dilute the REV-containing tissue culture medium, insects before feeding, and insects that engorged on blood without virus were negative by all tests. REV-containing tissue culture medium was positive by all tests, and the feeding mixture (REV-containing tissue culture medium and blood) was positive for REV antigens and virus isolation in tissue culture for the entire 96 h. Because mosquito midgut differs from tissue culture medium in proteolytic enzyme content, engorged mosquitoes were ELISA positive for 5 h, compared with at least 96 h for the blood mixture. REV could be detected in tissue culture for 24 h from the beginning of feeding. REV could be detected for 24 h in engorged mosquitoes, compared with at least 96 h in tissue cultures. The proviral RNA was amplified for 96 h from the feeding mixture, but it was not detected in the RNA purified from the engorged mosquitoes. The gag primers detected the viral RNA in the feeding mixture also for 96 h, but not from the engorged insects. By using the whole engorged insect homogenates, REV-LTR and gag were amplified from the feeding mixture for 24 h and from fed mosquitoes for 5 h. These data show that REV RNA was present continuously in the feeding mixture, but after the mosquitoes imbibed the mixture, virus remained viable for a limited time in the midgut.
Table 2.
Summary of experimental feeding of mosquitoes on REV–blood mixtures

Virus Detection in House Flies Fed on Sugar Impregnated with REV.
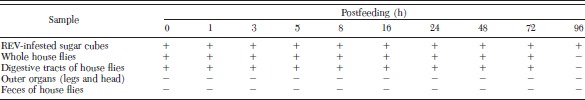
House flies were observed for feeding on the sugar cubes wetted with REV-containing tissue culture medium. REV RNA was detected from the sugar cubes for 96 h (Table 3). RNA purified from whole house flies and from the digestive tracts of fed house flies were positive for REV up to 72 h postfeeding. In contrast, the outer anatomy and feces were RT-PCR negative at all times. REV virus was ingested by the house flies, and they are a potential virus carrier. House flies that fed on sugar cubes wetted with liquid that did not contained REV remained negative (not shown).
Table 3.
Detection of REV in house flies fed on sugar cubes containing REV in CEF culture medium
Transmission of REV to Chickens by Infected House Flies.
To assess the ability of house flies to transmit the viral infection to chickens, one group of chickens was infected experimentally with REV and exposed to house flies, whereas others were not infected and served as negative controls. Possible contacts between the birds and house flies might occur through feces, other body secretions, and open wounds. Birds also eat the flies and their larvae. REV presence was verified by RT-PCR by using the gag and LTR primers and RNA prepared from cloaca swabs and blood, respectively. House flies then were exposed separately to the feces produced by each group of chickens. Table 4 shows the results of the first experiment, indicating the successful infection of the chickens, as determined by the cloaca excretion of REV at 7 d postinfection and the formation of REV antibodies at 14 d p.i. However, the infection was transient and could not be detected at 14 d p.i. In that experiment, house flies were brought into contact with the infected chickens from days 10–14 pi, and the virus could not be detected in the house flies that were in contact with the feces of the REV-infected chickens.
Table 4.
Infection of chickens by virus-infected house flies

In the second experiment, the chickens were infected with REV in a similar manner, but the house flies were fed with feces of the REV-infected birds within 24 h postinfection. Ten house flies were fed at each time point. The house flies that were fed on feces taken at 1 d p.i. were negative, but all flies that were fed on feces of the infected chickens at 2 and 3 d p.i. were REV-PCR positive. These results indicated that virus was shed on day 2 p.i., and it could be transferred to the flies that were in contact with these chickens.
Discussion
We evaluated the suspected insect vectors of REV and added our knowledge of their impact on the poultry health. Positive insects were not found near REV antibody-positive flocks, indicating that the virus load or infection rates were too low to be transmitted mechanically by these insects. It seems, therefore, that under conditions of natural infection in commercial flocks, the insects may not be a major risk factor for infection with REV. However, in previous studies hematophagous arthropods have been implicated in the horizontal dissemination of REV in commercial flocks (Motha et al. 1984; Thompson et al. 1968, 1971) because REV was detected and monitored in Israel in previous years (Davidson and Malkinson 1997), we sought to study the possible involvement of insects in several controlled experiments.
Virus was detected in mosquitoes for up to 5 h postblood feeding, but it was detected in the feeding mixture up to 96 h. Rapid inactivation of REV in engorged mosquitoes seems to be related to digestion of the virus in the midgut, indicating probably that these insects lack receptors for viral attachment and midgut infection. Mosquitoes may harbor REV for short time periods and could transmit REV mechanically for short periods if a bloodmeal is shared between infected and uninfected birds. These data and that no REV was detected in the trapped insects indicate that mosquitoes in particular, and probably other insects, are not infected with REV, and certainly the virus is not replicating in the insects, but is transmitted mechanically.
This is the first study where house flies were implicated in the context of REV horizontal transmission. REV was present within house fly digestive tract for 4 d. Chickens might be exposed to REV carried by the flies through eating them or by contact with open wounds on their bodies. To demonstrate the feasibility of the house flies to serve as an insect carrier of REV, we performed an experimental cycle of REV transmission from chickens to flies and back to other chickens. Because we showed the transmission of the virus from infected chicken to the house flies, the partial cycle was achieved, thus contributing to the knowledge on the avenues of REV horizontal spread in commercial flocks.
Acknowledgements
We are grateful to A. Ginzburg-Chizov for help throughout the experiments.
References Cited
- Aly M. M., Smith E. J., Fadly A. M. 1993. Detection of reticuloendotheliosis virus infection using the polymerase chain reaction. Avian Pathol. 22: 543–554. [DOI] [PubMed] [Google Scholar]
- Bagust T. J., Grimes T. M. 1979. Experimental infection of chickens with an Australian strain of reticuloendotheliosis virus. 2. Serological responses and pathogenesis. Avian Pathol. 8: 375–389. [DOI] [PubMed] [Google Scholar]
- Bagust T. J., Grimes T. M., Ratnamohan N. 1981. Experimental infection of chickens with an Australian strain of reticuloendotheliosis virus. 3. Persistent infection and transmission by the adult hen. Avian Pathol. 10: 375–385. [DOI] [PubMed] [Google Scholar]
- Braverman Y., Rubina M. 1976. Light trapping of biting insects in poultry houses in Israel. Isr. J. Zool. 25: 95–101. [Google Scholar]
- Braverman Y., Chizov-Ginzburg A., Saran A., Winkler M. 1999. The role of house flies (Musca domestica) in harboring Corynebacterium pseudotuberculosis in dairy herds in Israel. Rev. Sci. Tech. Off. Int. Epiz. 18: 681–690. [DOI] [PubMed] [Google Scholar]
- Braverman Y., Davidson I., Chizov-Ginzburg A., Chastel C. 2003. Detection of Israel turkey meningoencephalitis virus from mosquito (Diptera: Culicidae) and Culicoides (Diptera: Ceratopogonidae) species and its survival in Culex pipiens and Phlebotomus papatasi (Diptera: Phlebotomidae). J. Med. Entomol. 40: 518–521. [DOI] [PubMed] [Google Scholar]
- Calibeo-Hayes D., Denning S. S., Stringham S. M., Guy J. S., Smith L. G., Wes Watson D. 2003. Mechanical transmission of turkey coronavirus by domestic house flies (Musca domestica Linnaeaus). Avian Dis. 47: 149–153. [DOI] [PubMed] [Google Scholar]
- Chihota C. M., Rennie L. F., Kitching R. P., Mellor P. S. 2001. Mechanical transmission of lumpy skin disease virus by Aedes aegypti (Diptera: Culicidae). Epidemiol. Infect. 126: 317–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson I., Malkinson M. 1996. A non-radioactive method for identifying env and LTR genes using psoralen-biotin labelled probes. J. Virol. Methods 59: 113–119. [DOI] [PubMed] [Google Scholar]
- Davidson I., Malkinson M. 1997. Epidemiology and control of reticuloendotheliosis in Israel, pp. 7–75. InProceedings of the AVMP/AAAP Annual Meeting, Avian Tumor viruses Symposium, 21 July 1997, Reno, NV. [Google Scholar]
- Davidson I., Borowsky A., Perl S., Malkinson M. 1995. Use of the PCR for the diagnosis of natural infection of chickens and turkeys with Marek’s disease virus and reticuloendotheliosis virus. Avian Pathol. 24: 69–94. [DOI] [PubMed] [Google Scholar]
- Davidson I., Alphandary R., Novoseler M., Malkinson M. 1997. Replication of non-defective reticuloendotheliosis viruses in the avian embryo assayed by PCR and immunofluorescence. Avian Pathol. 26: 579–593. [DOI] [PubMed] [Google Scholar]
- DuToit R. M. 1944. The transmission of bluetongue and horse-sickness by Culicoides. Onderstepoort J. Vet. Sci. Anim. Ind. 19: 7–16. [Google Scholar]
- Lipkind M., Braverman Y., Frish K., Shimanter E. 1982. Preliminary studies on the replication of influenza virus in mosquitoes. InThe 7th Symposium of Veterinary Medicine, Faculty of Agriculture, Hebrew University of Jerusalem, Rehovot, 10 February, Refuah Veterinarith, Israel. [Google Scholar]
- McDaniel L. S., McDaniel I. N., Schute H. L. 1962. Laboratory transmission of Rous sarcoma virus by Aedes aegypti. Avian Dis. 127–132. [Google Scholar]
- McDaniel L. S., McDaniel I. N., Schute H. L. 1964. Persistence of Rous sarcoma virus in the mosquito Culex pipiens pipiens. J. Am. Vet. Res. 25: 262–263. [PubMed] [Google Scholar]
- Motha M. X., Egerton J. R., Sweeney A. W. 1984. Some evidence of mechanical transmission of reticuloendotheliosis virus by mosquitoes. Avian Dis. 28: 858–867. [PubMed] [Google Scholar]
- Sincovic B. 1983. Studies of the epizootiology of reticuloendotheliosis virus infection in commercial Australian chicken flocks. InProceedings of the 22nd World Veterinary Congress, Perth, Australia. [Google Scholar]
- Thompson K. D., Fischer R. G., Luecke D. H. 1968. Determination of the viremic period of avian reticuloendotheliosis virus (strain T) in chicks and virus viability in Triatoma infestans (KLUG) (Hemiptera: Reduviidae). Avian Dis. 12: 354–360. [PubMed] [Google Scholar]
- Thompson K. D., Fischer R. G., Luecke D. H. 1971. Quantitative infectivity studies of avian reticuloendotheliosis virus (strain T) in certain hematophagous arthropods. J. Med. Entomol. 8: 486–490. [DOI] [PubMed] [Google Scholar]
- Peterson D. A., Levine S. A. 1971. Avian reticuloendotheliosis (strain T). IV. Infectivity and transmissibility in day-old cockerels. Avian Dis. 15: 874–883. [PubMed] [Google Scholar]
- Purchase H. G., Witter R. L. 1995. The reticuloendotheliosis viruses. Curr. Top. Microbiol. Immunol. 71: 103–124. [DOI] [PubMed] [Google Scholar]
- Rehacek J., Dolan T., Thompson K. D., Fischer R. G., Rahecek Z., Johnson H. 1971. Cultivation of oncogenic viruses in mosquito cells in vitro. Curr. Top. Microbiol. Immunol. 55: 161–164. [DOI] [PubMed] [Google Scholar]
- Reiman I., Werner O. 1996. Use of the polymerase chain reaction for the detection of reticuloendotheliosis virus in Marek’s disease vaccines and chicken tissues. J. Vet. Med. B. 43: 75–84. [DOI] [PubMed] [Google Scholar]
- Witter R. L. 1997. Reticuloendotheliosis, pp. 467–484. InCalnek B. W., Barnes H. J., Beard C. W., Yoder H. W., Jr. [eds.], Diseases of poultry, 9th ed. Iowa State University Press, Ames, IA. [Google Scholar]
- Witter R. L., Johnson D. C. 1985. Epidemiology of reticuloendotheliosis virus in broiler breeder flocks. Avian Dis. 29: 1140–1154. [PubMed] [Google Scholar]
- Witter R. L., Smith R. J., Crittenden L. B. 1981. Tolerance, virus shedding and neoplasia in chickens infected with nondefective reticuloendotheliosis virus. Avian Dis. 25: 374–394. [PubMed] [Google Scholar]
- Yeruham I., Nir O., Braverman Y., Davidson M., Greinstein H., Haymovitch M., Zamir O. 1994. Observation on mode of spread of lumpy skin disease in Israeli dairy herds. Vet. Rec. 137: 91–93. [DOI] [PubMed] [Google Scholar]
- Yuasa N., Yoshida I., Taniguchi T. 1976. Isolation of a reticuloendotheliosis virus from chickens inoculated with Marek’s disease vaccine. Natl. Inst. Anim. Health Q 16: 141–151. [PubMed] [Google Scholar]


