ABSTRACT
Background: During public health emergencies, the Military Health System experiences challenges similar to those across the U.S. public and private health systems. This study explored how 1 such event, the 2009/2010 influenza (H1N1) pandemic, impacted health care utilization and associated costs in the Military Health System. Methods: Data from the Military Data Repository were used to examine diagnoses, claims data, and dates of services with respect to military or civilian care during 2004–2009/2010 influenza seasons. Comparison analysis was conducted through two-tailed t-tests and regression models. Results: There was a significant increase in inpatient and outpatient health care utilization during the 2009/2010 H1N1 pandemic year, most markedly for emergency department visits. The 2009/2010 H1N1 pandemic cost the Department of Defense $100 million compared to influenza-related health care costs incurred in previous influenza seasons. Highest health care utilization costs were found in children less than age 5. The greatest cost burden was attributed to immunizations for active duty personnel delivered at military facilities. Conclusion: Annual trend analysis of costs and health care utilization would be helpful to plan and resource emerging influenza pandemics and to identify subgroups at greatest risk for contracting influenza.
“Influenza is something unique. It behaves epidemiologically in a way different from that of any other known infection.”
—Sir Christopher Howard Andrewes, Director of the World Influenza Center, World Health Organization, London (1948–1961).
INTRODUCTION
Public health emergencies have long been an area of concern for military health care systems because of the increased demand for health care services. Over the last decade, there have been several instances where outbreaks of infectious disease, as public health emergencies, have repeatedly challenged military policies for preparedness. In addition to localized outbreaks, international pandemics have become a focal concern because of their impact on available resources in both civilian and military health care systems. Since the 1918 influenza, the United States has helped mitigate the spread of disease during pandemics, but recent global epidemics have shifted the focus to strengthened preparedness for such public health emergencies.1
The growing number of emerging and re-emerging infectious diseases, like the severe acute respiratory syndrome-associated coronavirus in 2003 and the Influenza A virus subtype H1N1 pandemic in 2009, have highlighted the rapid progression of localized epidemics into global pandemics.2 Available treatment options with novel pathogens are typically limited during such global public health emergencies, thus necessitating greater reliance on emergency outpatient or inpatient supportive care. From a health systems management perspective, the large influx of patients being treated for either an unknown virulent etiology or supportive therapy can easily overburden health care facilities.
The U.S. Department of Defense (DoD) has long recognized potential threats posed by global pandemics to the readiness of combat forces, and the health and well-being of the nation they protect. The Military Health System (MHS), which maintains health care services for U.S. armed services personnel and their families, has extensive experience with influenza disease epidemics, such as the 1976 outbreak of H1N1 that was detected after the death of an Army recruit in Fort Dix, New Jersey.3 This outbreak resulted in a mass vaccination program across the United States and initiated a collaborative approach between CHAMPUS (now TRICARE, the system of health care plans for the U.S. Armed Forces and beneficiaries), the Centers for Disease Control and Prevention, and local/regional health departments. Twenty years after the Fort Dix incident, an outbreak of influenza A (H3N2) on a Navy ship led to the discovery of an antigenically distinct H3N2 influenza virus from the 1995/1996 seasonal vaccine administered to military personnel for a different vaccine strain.4 This outbreak on the USS Arkansas reached an incidence rate of 42%, infecting 232 of the ship's personnel. In addition to past outbreaks of influenza, threats of an avian influenza outbreak (avian influenza A, H5N1) surfaced in 2005, prompting the DoD to coordinate with the Department of Health and Human Services (DHHS) and the Department of Homeland Security to develop a national pandemic preparedness strategy.5 Other types of communicable diseases have similarly challenged military preparedness policies such as outbreaks of pertussis,6 occupational exposures to blood-borne pathogens or enteroviruses,7 and food-borne infectious diarrhea.8
Federal experiences identifying and controlling new strains of influenza are critical for military preparedness and the health care of DoD beneficiaries.9 As part of national pandemic preparedness, DoD policy now authorizes individual military base commanders to plan and coordinate response activities with local public health officials based on local declaration of public health emergencies.10 DoD also contributes to national pandemic control by assisting in diagnostic testing of laboratory samples and reporting of influenza prevalence data through the DoD Electronic Surveillance System for the Early Notification of Community-Based Epidemics, published online at the Force Health Protection Pandemic Influenza Watch Board.10,11
During the 2009 H1N1 pandemic, the World Health Organization reported 477,593 laboratory positive cases and 17,919 fatal cases from 214 countries.12 In the United States, the Centers for Disease Control and Prevention laboratory confirmed 2,117 fatal cases and 41,821 reported hospitalizations.13 Although laboratory-confirmed cases provide real-time case counts during a public health emergency, estimates are likely to be greater because of underreporting.
The DoD implemented a preparedness policy during this 2009 pandemic, including a stringent vaccination program and guidelines to providing health care during public health emergencies. Antiviral therapy and pandemic (H1N1) 2009 vaccination for active duty (AD) service members, including high risk beneficiaries, became a priority and this then served as the primary approach against this pandemic.10 TRICARE beneficiaries received the H1N1 vaccine under another program, one with the same vaccine accessibility provided to civilian populations but with prioritization for vulnerable beneficiary populations.14 With the implementation of the vaccination program during the peak of the pandemic, military treatment facilities (MTFs) had to cope with the influx of AD personnel and beneficiaries who were seen in emergency departments, inpatient wards, or outpatient clinics during the pandemic.
Here, we report on the results of a retrospective study to assess the impact of the 2009 H1N1 pandemic on the MHS with the overall goal of assessing and improving the effectiveness of pandemic preparedness in the DoD. This study examines the burden of disease caused by the 2009 H1N1 pandemic strain on the MHS with respect to health care utilization and associated costs and provides insight into DoD resource management of pandemics compared to previous nonpandemic influenza seasons.
METHODS
Data Source
We used the MHS Data Repository (MDR) to assess health care utilization, prescription claims, and estimated costs of H1N1 and influenza-like illnesses (ILIs). The MDR captured immunizations rendered to patients in a military health care setting only. Influenza immunization rendered in civilian settings were not tracked as non-AD beneficiaries may obtain immunization through multiple sources that may not be entered as MDR claims data (e.g., employment, free public health programs). Our analytical dataset consisted of outpatient encounters, inpatient stays, and medication records rendered through MTFs and civilian care, October 2004 through April 2010. We included encounter records if they had specific and nonspecific codes associated with ILI, influenza immunization, and associated treatments. Individuals with multiple influenza-related encounters were only counted once per season. Each record contained the month/year of the service encounter, the patient pseudoidentifier, sex, age, beneficiary category, branch of service, state of residence, and type of TRICARE enrollment plan (MTF Prime, Managed Care Support Contractor Prime, and non-Prime). The final dataset was aggregated to person-level records to enable characterization of the 2009 H1N1 influenza patient. Age was grouped by 0–4, 5–17, 18–24, 25–34, 35–44, 45–64, and 65 years or older. Beneficiary categories were AD, family members of AD, military retirees and family members of retirees <age 65, and military retirees and family members age 65 or older.
Cost data included costs associated with outpatient and emergency department visits, inpatient stays, influenza vaccine administration, and antiviral prescriptions rendered in the military and civilian settings from October 2004 to January 2010 (the last month when full cost data were available at the time of analysis). Costs also included $15.9 million spent by DoD to purchase H1N1 vaccine although this expenditure could not be allocated to the patient level. For each ILI service delivered from October 2004 through January 2010, we used the full cost associated with services delivered in MTFs (direct care); for services delivered by civilian providers (care purchased in the TRICARE network or from non-network providers), we tabulated the actual amounts paid by DoD using claim-level data.
Human Subject Protection
The study was reviewed by the TRICARE Management Activities Human Research Protection Program Oversight Office and determined to be exempt from full review by the DoD Institutional Review Board.
Analysis
Demographics (number of cases by age group, gender, beneficiary category, branch of service, and TRICARE enrollment plan) for 2008/2009 influenza season and 2009/2010 pandemic season were examined using 2-tailed correlation analyses to identify differences between the two seasons. Cost data for the 2009/2010 H1N1 pandemic was derived by comparing the total ILI-related costs for the 2009/2010 influenza season to the ILI-related costs associated with the five preceding seasons. The expected costs were then compared with the actual costs for the 2009/2010 season to isolate the incremental cost of H1N1. The ILI-related costs excluded costs associated with services rendered outside a health care facility; costs borne by DHHS for H1N1 immunizations administered in civilian facilities; costs associated with lost productivity because of ILI; and costs of H1N1 surveillance, reporting, and response activities.
A series of linear regression models were then used to estimate the expected ILI costs during the 2009/2010 influenza season as if it had been a typical influenza season, and to ferret out those factors that contributed to costs. Eight regression models were specified, with separate models for military (direct) care and civilian (purchased) care as well as for four types of services: inpatient, outpatient nonpharmacy, outpatient pharmacy, and immunizations. The models controlled for the number of beneficiaries, age mix, beneficiary category, seasonality, and the underlying time trend. The time trend was modeled based on an explicit, independent variable that increased by one unit per month from October 2004 (month 1) through January 2010 (month 64). The model implicitly assumed that the underlying historical trend, controlling for the other independent variables, would continue. This underlying historical trend accounted for medical inflation and underlying trends in utilization per capita.
RESULTS
Frequency and Percentage of ILI
Of the 9,399,614 TRICARE beneficiaries in the May 2008 through April 2009 influenza season, 47,165 (0.5%) were diagnosed as having an ILI; of the 9,584,956 beneficiaries in the 2009/2010 influenza season, 176,281 (1.8%) were diagnosed as having an ILI. Within male and female groups, and within every age group, category of beneficiaries, branch of service, and type of TRICARE enrollment plan, 2-sided t-tests showed significantly higher rates of diagnosed ILI in the 2009/2010 pandemic season (p < 0.05). The subgroups with the highest rate increase between the 2008/2009 and 2009/2010 seasons are beneficiaries age 0 to 4 (1.2% vs. 4.4%) and those age 5 to 17 (1.1% vs. 4.4%), Managed Care Support Contractor Prime enrollees (1.1% vs. 3.6%), and family members of AD personnel (0.8% vs. 3.2%). Among AD personnel, the rate of diagnosed ILI increased between the 2008/2009 and 2009/2010 influenza seasons from 0.2% (n = 4,527 of 1,814,975) to 1.4% (n = 26,244 of 1,869,352).
Health Care Utilization
The total and mean per-patient number of outpatient visits, emergency department visits, inpatient stays, and antiviral prescription fills by each type of ILI service are shown in Table I. Relative to the preceding influenza season, utilization of 2009–2010 health care services for ILI increased at both military and civilian-contracted facilities, with the largest increases observed for emergency department visits (854.5% in military and 524.3% in civilian facilities). ILI office visits increased 532.1% and 324.6% at military and civilian facilities, respectively, whereas inpatient dispositions increased 513.0% and 284.2% at military and civilian facilities, respectively. In both military and civilian facilities, the mean number of inpatient days was significantly lower in the 2009/2010 influenza season relative to the prior influenza season (p = 0.003). Compared to the preceding influenza season, the use of oseltamivir and zanamivir increased by 313.2%, whereas use of other antiviral agents, amantadine and rimantadine, was somewhat reduced (84.6%), although no statistically significant change in the use of these other antivirals was found between the 2008/2009 and 2009/2010 seasons.
TABLE I.
Total and Per-Patient Health Care Utilization for 2008/2009 and 2009/2010 Influenza Seasons by Type and Location of Service
| May 2008–April 2009 Influenza Season | May 2009–April 2010 Influenza Season | Percentage increase* (e/b) (%) | p-value** | |||||
|---|---|---|---|---|---|---|---|---|
| No. of Patients (a) | Total (b) | Mean per patient (c) | No. of Patients (d) | Total (e) | Mean per patient (f) | |||
| Military Facilities | ||||||||
| Office Visits | 6,237 | 6,798 | 1.09 | 31,733 | 36,172 | 1.14 | 532.1 | <0.05 |
| Emergency Department Visits | 1,994 | 2,058 | 1.03 | 17,001 | 17,582 | 1.03 | 854.5 | 0.576 |
| Inpatient Dispositions | 202 | 205 | 1.01 | 1,020 | 1,049 | 1.03 | 513.0 | 0.162 |
| Inpatient Bed Days | 202 | 1,111 | 5.50 | 1,020 | 3,699 | 3.63 | 333.1 | 0.003 |
| Civilian Facilities | ||||||||
| Office Visits | 28,295 | 33,082 | 1.17 | 85,911 | 107,397 | 1.25 | 324.6 | <0.05 |
| Emergency Department Visits | 5,573 | 6,074 | 1.09 | 27,642 | 31,845 | 1.15 | 524.3 | <0.05 |
| Inpatient Admissions | 955 | 1,012 | 1.06 | 2,526 | 2,877 | 1.14 | 284.2 | <0.05 |
| Inpatient Bed Days | 955 | 8,039 | 8.42 | 2,526 | 17,139 | 6.79 | 213.2 | 0.003 |
| Antiviral Prescriptions | ||||||||
| Recommended Antivirals | 87,368 | 107,889 | 1.23 | 276,892 | 337,939 | 1.22 | 313.2 | 0.004 |
| Other Antiviral Therapy | 4,016 | 8,083 | 2.01 | 3,266 | 6,838 | 2.09 | 84.6 | 0.797 |
Percentage increase in influenza-related services in 2009/2010 season relative to the 2008/2009 season.
Statistical significance difference in 2008/2009 season and 2009/2010 season, 2-sided t-test.
H1N1 Cost Impact
Tables II and III show the HI1N1 cost impact by age group and type/source of care, respectively. For the estimated $84 million H1N1 impact that could be allocated to the patient level (Table II), 61% of the cost increase was attributable to care rendered to beneficiaries aged 0 to 24 years, whereas 72% of the cost increase was due to care rendered to AD service members and their family members. Table III indicates where the total of $156.7M was spent on ILI from July 2009 to January 2010. This total was approximately $100M more than projected for these months during a normal influenza season. Table III includes $15.9M for DoD-purchased H1N1 vaccine that could not be allocated in the patient-level cost data. Treatment costs accounted for 58% of the $100M overall cost impact, whereas immunization-related costs, including the DoD purchase of vaccine, accounted for 42%.
TABLE II.
H1N1 Cost Impact July 2009 to January 2010 by Age Group and Beneficiary Category (Dollars in Millions)
| Cost of Influenza Treatment and Immunizations | |||||
|---|---|---|---|---|---|
| Actual Costs ($) | Expected Cost (Normal Influenza) ($) | Cost Increase Because of H1N1 ($) | Percentage Increase Because of H1N1 (%) | Percentage Share of H1N1 Cost (%) | |
| Age | |||||
| 0–4 | 25.2 | 11.4 | 13.8 | 122 | 17 |
| 5–17 | 32.1 | 6.8 | 25.3 | 374 | 30 |
| 18–24 | 22.2 | 10.2 | 12.1 | 118 | 14 |
| 25–44 | 30.2 | 11.7 | 18.5 | 159 | 22 |
| 45–64 | 21.0 | 10.0 | 10.9 | 109 | 13 |
| Non-AD Family Members 65+ | 6.1 | 4.8 | 1.3 | 26 | 2 |
| Unknown Age | 3.9 | 2.2 | 1.8 | 80 | 2 |
| Total* | 140.7 | 57.0 | 83.7 | 147 | 100 |
| Beneficiary Category | |||||
| AD | 34.5 | 14.4 | 20.0 | 139 | 24 |
| AD Family | 60.3 | 20.2 | 40.1 | 198 | 48 |
| Non-AD family member < age 65 | 39.9 | 17.6 | 22.3 | 127 | 27 |
| Non-AD family member age 65+ | 6.1 | 4.8 | 1.3 | 26 | 2 |
| Total* | 140.7 | 57.0 | 83.7 | 147 | 100 |
Total actual cost and the increase attributed to H1N1 does not include $15.9M spent by DoD to purchase H1N1 vaccine, as this cost could not be allocated to the patient-level data. This additional cost is included in Table III.
TABLE III.
MHS H1N1 Cost Impact of $100M for July 2009 to January 2010 by Type and Source of Care (Dollars in Millions)
| Actual Costs ($) | Expected Costs ($)* | Cost Increase Because of H1N1 ($) | Percentage Increase Because of H1N1 (%) | Percentage Share of H1N1 Cost (%) | |
|---|---|---|---|---|---|
| Military Care Inpatient | 10.7 | 3.2 | 7.5 | 237 | 8 |
| Civilian Care (Purchased) Inpatient | 23.7 | 4.2 | 19.5 | 462 | 20 |
| Military Care Outpatient | 10.1 | 1.0 | 9.2 | 922 | 9 |
| Civilian Care (Purchased) Outpatient | 19.1 | 3.6 | 15.4 | 424 | 15 |
| Military Care Pharmacy | 3.8 | 1.0 | 2.9 | 291 | 3 |
| Civilian Care (Purchased) Pharmacy | 4.4 | 1.0 | 3.5 | 367 | 4 |
| Subtotal Treatment | 71.9 | 14.0 | 57.9 | 415 | 58 |
| Military Care Immunizations | 64.7 | 32.4 | 32.3 | 100 | 32 |
| Civilian Care (Purchased) Immunizations | 20.1 | 10.7 | 9.4 | 88 | 9 |
| Subtotal, Immunizations | 84.8 | 43.1 | 41.7 | 97 | 42 |
| Subtotal, Military Care | 89.4 | 37.5 | 51.8 | 138 | 52 |
| Subtotal, Civilian Care (Purchased) | 67.3 | 19.5 | 47.8 | 245 | 48 |
| Total | 156.7 | 57.0 | 99.6 | 175 | 100 |
Expected costs are based on 2004–2008/2009 influenza seasons.
The regression models showed that there was a high cost burden for civilian inpatient hospitalization and civilian outpatient services across the period of analysis. The highest health care utilization costs were found for children ages 5 to 17. The overall greatest cost burden, however, was incurred for immunizations delivered at MTFs.
The estimated costs from the regression models and the actual costs for each influenza season by month between October 2004 and January 2010 are presented in Figure 1. As shown, there is a slight increase in ILI-related costs between the 2004/2005 and 2008/2009 influenza seasons, then a dramatic increase for the 2009/2010 season.
FIGURE 1.
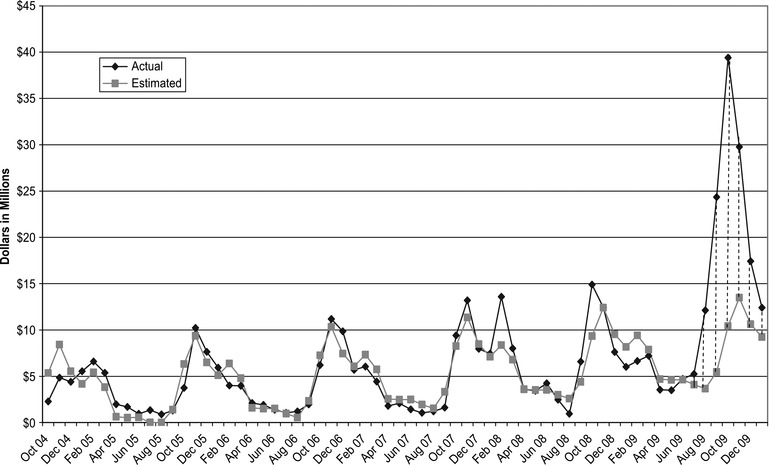
Actual and estimated costs associated with treatment and immunization for past five influenza seasons, October 2004 to January 2009.
DISCUSSION
In 2009/2010, the MHS realized an estimated $100 million increase in ILI-related costs compared to prior influenza seasons. The DoD experience with the 2009/2010 H1N1 pandemic is remarkably similar to experiences found in the nation as a whole, at least among populations with access to health care. Our findings closely mirror those based on U.S. civilian populations, i.e., heavy reliance on emergency departments15 and high rates of ILI among beneficiaries less than age 18.16 The increased rates of health care utilization and costs observed in the DoD pediatric population is particularly concerning, given a new report that concludes that the nation's capacity to care for pediatric populations during the 2009/2010 influenza season was marginally adequate; had the 2009/2010 H1N1 pandemic been more virulent, tertiary pediatric facilities would have been overwhelmed.17 Further, in contrast to our findings, the U.S. civilian population saw a heavier burden of ILI among young adults.18 Most young adults included in our DoD population were AD personnel, who, unlike their civilian counterparts, were required to be vaccinated for H1N1.
Based on our findings and those based on civilian reports,19 we recommend that DoD, as well as the local communities where MTFs reside, develops specialized preparedness procedures for pediatric populations in anticipation of future influenza pandemics or epidemics. One strategy, based on estimated models when immunization resources are scarce and the influenza incidence is declining, is to consider immunizing school-age children as well as high-risk adults.20 Although DoD has clear requirements for vaccinating AD personnel, there are no such directives for vaccinating family members. Another strategy is to consider closing elementary schools on DoD installations, the length of closure dependent on pandemic severity as modeled elsewhere using civilian schools.21 In addition, to assist fiscal and resource planning, we recommend time trends that compare rates and costs to previous influenza seasons be conducted annually for each MTF. Finally, we recommend that future study be directed to evaluating effective models of triaging individuals who present with ILI symptoms, particularly for those presenting in emergency departments.
Our study has several limitations. Our inclusion of nonspecific vaccine administration codes in the MDR may have captured vaccines unrelated to influenza. Only vaccines administered in the health care setting are captured in the MDR, but some immunizations are administered to service members in the field; thus, total vaccine-related costs for DoD are underestimated in our study. Cost allocation data, particularly for care rendered in the military hospitals, were not specific to immunization clinics or different types of immunizations. Immunizations or treatment for ILI may have occurred as part of a broader health care visit, and ILI costs may not have been identified. Moreover, our cost estimation methodology may not have generated an accurate estimate for all events because we only had cost data through January 2010. To some extent, comparison with prior influenza seasons mitigates the impact of this limitation, assuming that health care practices persisted across the 2004–2009 influenza seasons. Yet another limitation, out of concern for patient privacy, is that we did not conduct analysis at the MTF level. Therefore, we neither examined the prevalence of H1N1 cases, health care utilization, or costs by individual MTFs nor consider MTF facility size, the number of available beds, and size of outpatient clinics in relation to the number of cases received at a particular facility. Finally, while the cost of care provided in civilian settings is directly calculated from government payments/costs at a claim level, military care costs are reported in aggregate (by clinic) and then fitted and allocated to the detail “visit” level; hence, military care costs are inexact comparisons to civilian costs.
CONCLUSIONS
The focus of this study was to examine the impact of the 2009 H1N1 pandemic on the MHS and inform military commanders and policy makers about the burden of a public health emergency on health care systems used by DoD beneficiaries. This information should assist in review of DoD's response to this most recent pandemic and help strategize for preparedness response to similar events. In particular, review and evaluation of strategies that address our capacity to care for the DoD pediatric population during an influenza pandemic is warranted, as is the need to manage increased demand on emergency departments during such events.
Footnotes
Parts of this manuscript were included in an oral presentation, “H1N1 Preparedness and Recent Lessons Learned,” at the 2011 Military Health System Conference, National Harbor, MD, January 2011.
REFERENCES
- 1. Middaugh JP. Pandemic influenza preparedness and community resiliency. JAMA 2008; 299(5): 566–8. [DOI] [PubMed] [Google Scholar]
- 2. Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003; 348(20): 1953–66. [DOI] [PubMed] [Google Scholar]
- 3. Hodder RA, Gaydos JC, Allen RG, Top FH Jr, Nowosiwsky T, Russell PK. Swine influenza A at Fort Dix, New Jersey (January–February 1976). Extent of spread and duration of the outbreak. J Infect Dis 1977; 136: S369–75. [DOI] [PubMed] [Google Scholar]
- 4. Earhart KC, Beadle C, Miller LK, et al. Outbreak of influenza in highly vaccinated crew of U.S. Navy ship. Emerg Infect Dis 2001; 7(3): 463–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The National Strategy for Pandemic Influenza, Implementation Plan (NSPIIP), Homeland Security Council, May 2006. Available athttp://georgewbush-whitehouse.archives.gov/homeland/pandemic-influenza.html; accessed July 24, 2012.
- 6. Armed Forces Health Surveillance Center (AFHSC) Pertussis diagnoses among service members and other beneficiaries of the U.S. Military Health System, January 2005–June 2012. MSMR 2012; 19(8): 14–7. [PubMed] [Google Scholar]
- 7. Armed Forces Health Surveillance Center (AFHSC) Viral meningitis, active and reserve components, U.S. Armed Forces, 2002–2011. MSMR 2012; 19(8): 2–6. [PubMed] [Google Scholar]
- 8. Kasper MR, Lescano AG, Lucas C, et al. Diarrhea outbreak during U.S. military training in El Salvador. PLoS One 2012; 7(7): e40404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eick-Cost AA, Tastad KJ, Guerrero AC, et al. Effectiveness of seasonal influenza vaccines against influenza-associated illnesses among US military personnel in 2010–11: a case-control approach. PLoS One 2012; 7(7): e41435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Department of Defense Instruction Number 6200.03. Public Health Emergency Management Within the Department of Defense. June 1, 2012 USD (P&R). Available athttp://www.dtic.mil/whs/directives/corres/pdf/620003p.pdf; accessed July 24, 2012.
- 11. Department of Defense Pandemic Influenza Watchboard. January 2011. Available athttp://fhp.osd.mil/aiWatchboard; accessed April 25, 2013.
- 12. World Health Organization Pandemic (H1N1) 2009-update 98. April 2010. Available athttp://www.who.int/csr/don/2010_04_30a/en/index.html; accessed July 24, 2012.
- 13. Centers for Disease Control 2009 H1N1 Flu U.S. Situation Update. April 30, 2010. Available athttp://www.cdc.gov/h1n1flu/updates/us/043010.htm; accessed July 24, 2012.
- 14. Peters KM. Defense officials prepare for H1N1 flu. August 26, 2009. Available athttp://www.govexec.com/defense/2009/08/defense-officials-prepare-for-h1n1-flu/29843/; accessed July 24, 2012.
- 15. Plagianos MG, Wu WY, McCullough C, Paladini M, Lurio J, Buck MD. Syndromic surveillance during pandemic (H1N1) 2009 outbreak, New York, New York, USA. Emerg Infect Dis 2011; 17(9): 1724–6. Available at 10.3201/eid1709.101357; accessed April 25, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jain S, Kamimoto L, Bramley AM, et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April–June 2009. N Engl J Med 2009; 361(20): 1935–44. [DOI] [PubMed] [Google Scholar]
- 17. Sills MR, Hall M, Fieldston ES, et al. Inpatient capacity at children's hospitals during pandemic (H1N1) 2009 outbreak, United States. Emerg Infect Dis 2011; 17(9): 1685–91. Available at 10.3201/eid1709.101950; accessed April 25, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reed C, Angulo FJ, Swerdlow DL, et al. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April–July 2009. Emerg Infect Dis 2009; 17(12): 2004–7. Available athttp://wwwnc.cdc.gov/eid/article/15/12/09-1413.htm; accessed April 25, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Department of Health and Human Services An HHS Retrospective on the 2009 H1N1 Influenza Pandemic to Advance All Hazards Preparedness. Available athttp://www.phe.gov/Preparedness/mcm/h1n1-retrospective/Documents/h1n1-retrospective.pdf, accessed January 11, 2013, 2013.
- 20. Goldstein E, Wallinga J, Lipsitch M. Vaccine allocation in a declining epidemic. J R Soc Interface 2012; 9(76): 2798–803. Available atrsif.royalsocietypublishing.org; accessed January 11, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Araz OM, Damien P, Paltiel DA, et al. Simulating school closure policies for cost effective pandemic decision making. BMC Public Health 2012; 12: 449 Available athttp://www.biomedcentral.com/content/pdf/1471-2458-12-449.pdf; accessed April 25, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]


