Abstract
Background: Climate change is not only increasing ambient temperature but also accelerating the frequency, duration and intensity of extreme weather and climate events, such as heavy precipitation and droughts, and causing sea level rise, which can lead to population displacement. Climate change-related reductions in land productivity and habitability and in food and water security can also interact with demographic, economic and social factors to increase migration. In addition to migration, climate change has also implications for travel and the risk of disease. This article discusses the impact of climate change on migration and travel with implications for public health practice.
Methods: Literature review.
Results: Migrants may be at increased risk of communicable and non-communicable diseases, due to factors in their country of origin and their country of destination or conditions that they experience during migration. Although migration has not been a significant driver of communicable disease outbreaks to date, public health authorities need to ensure that effective screening and vaccination programmes for priority communicable diseases are in place.
Population growth coupled with socio-economic development is increasing travel and tourism, and advances in technology have increased global connectivity and reduced the time required to cover long distances. At the same time, as a result of climate change, many temperate regions, including high-income countries, are now suitable for vector-borne disease transmission. This is providing opportunities for importation of vectors and pathogens from endemic areas that can lead to cases or outbreaks of communicable diseases with which health professionals may be unfamiliar.
Conclusion: Health systems need to be prepared for the potential population health consequences of migration, travel and tourism and the impact of climate change on these. Integrated surveillance, early detection of cases and other public health interventions are critical to protect population health and prevent and control communicabledisease outbreaks.
Keywords: Climate change, travel, migration
Introduction
Travel medicine will increasingly see the health consequences of significant changes associated with global change, particularly climate change and socioeconomic development. Together these changes mean more opportunities for people to travel to pathogen-endemic countries and for pathogens to be imported to new locations, with the potential for unexpected communicable disease cases and outbreaks. Moreover, people who migrate or are displaced can also be at increased risk for chronic disease and mental health issues. Thus, travel medicine needs to take a broader perspective than just asking patients where they are going or where they have been, considering how the ongoing and projected shifts in the magnitude and pattern of disease could affect the health and well-being of individuals and populations. Modifications to the approaches used by health systems to manage adverse health outcomes are needed to ensure health care providers have the most up-to-date information.
Migration describes the movement of a person away from their usual residence whereas travel describes a person who passes from place to place, for any reason. Migration and travel have shaped the history of humanity and enriched societies economically, socially and culturally. Multiple and interacting factors drive migration in particular. Climate change, including increasing climate variability, can be one of these factors.
We discuss the potential impacts of climate change on migration and travel and the implications for travel medicine and public health practice. Following a brief review of climate change, we discuss the potential health implications of migration and travel and the way in which they are affected by climate change and provide suggestions for health systems to better manage the potential impact of climate change, migration and travel on population health.
Climate change
The Intergovernmental Panel on Climate Change Special Report on warming of 1.5°C concluded that human activities have caused ~1.0°C of global warming since pre-industrial times and that, if it continues to increase at the current rate, warming is likely to reach 1.5°C between 2030 and 2052.1 The Special Report concluded that climate change is increasing, and will continue to increase, land and ocean temperatures and the frequency, intensity and duration of heat waves in most land regions (high confidence). It also concluded that climate change will continue to increase the frequency and intensity of heavy precipitation events globally and the risk of drought in the Mediterranean region specifically (medium confidence). Climate change is a long-term process, but the extent to which individual weather events are influenced by climate change can increasingly be estimated.2,3
Migration
The greatest human migration started 60 000 or 70 000 years ago when Homo sapiens left Africa for other parts of the world4–7; a series of ‘mega-droughts’ may have contributed to this.6–8 Migration has continued since and has become a defining characteristic of our times, affecting every inhabited continent. Migrants may move internally, settle in neighbouring countries or move to other continents. Currently, Europe, North America and Oceania are the main destinations for migrants although, overall, Europe and Asia have received the greatest number of migrants in recent decades.9 Migration has political, social, economic, cultural, environmental and public health implications. Migrants generally contribute more in taxes and social contributions than they receive in benefits.10–13 But migration can also pose challenges, particularly when there is a rapid influx of large numbers of people.
The international importance of migration was recognized in 2015 by the United Nations General Assembly when the 2030 Agenda for Sustainable Development was adopted; 11 of the 17 Sustainable Development Goals (SDGs) directly or indirectly relate to migration14 (Table 1). In 2016, the United Nations General Assembly adopted the New York Declaration for Refugees and Migrants to support a comprehensive approach to migration. These international accords were also thematically linked to other major international agreements, including the Sendai Framework for Disaster Risk Reduction and the Paris Agreement under the United Nations Framework Convention on Climate Change.15,16
Table 1.
Migration, 2030 agenda for SDG and climate change
| SDG | Migrants | Climate Change |
|---|---|---|
| 1. No poverty | IDPs are often the poorest in their countries, as many had to leave belongings and work behind. Internal displacement also implies additional costs for host communities and aid providers. | Increases resilience to climate change |
| 2. Zero hunger | Internal displacement affects food security if food is no longer produced in regions of origin and resources are strained in areas of refuge. | Increases resilience to climate change |
| 3. Good health and well-being | IDPs’ physical and mental health is often affected by displacement. Health facilities may be strained in host areas; coverage and quality may diminish. | Increases resilience to climate change |
| 4. Quality education | Displaced children may be out of school for months or years. Children in host communities may suffer from lower quality of education if classrooms are overfilled. | Increases resilience to climate change |
| 5. Gender equality | Women tend to suffer most from lack of infrastructure in temporary settlements. Displacement can also increase gender-based violence. | Increases resilience to climate change |
| 6. Clean water and sanitation | Camps often provide limited access to water, sanitation and energy. Basic infrastructure in host communities may be overused and suffer shortages. | Increases resilience to climate change |
| 7. Affordable and clean energy | Lack of bio fuel can force out-migration. | Addresses some of the fundamental causes of climate change |
| 8. Decent work and economic growth | IDPs often leave their source of income behind and must find work in their host area, pressuring the local labour market. Reduced productivity, consumption, exports and taxes harm the economy. | Increases resilience to climate change |
| 9. Industry, innovation and infrastructure | Resilient infrastructure and sustainable industries may help limit the scale of disaster-induced displacement. | Addresses some of the fundamental causes of climate change |
| 10. Reduced inequalities | IDPs should be able to enjoy the same rights and opportunities as their compatriots but often suffer from inequality and discrimination. | Increases resilience to climate change |
| 11. Sustainable cities and communities | Urban systems can be stretched by the sudden and unplanned arrival of IDPs in cities. Informal settlements, urban poverty and further displacement risk can increase. Many countries are facing challenges to cope with urban displacement. | Addresses some of the fundamental causes of climate change |
| 12. Responsible consumption and production | Unsustainable use of natural resources, environmental degradation and climate change already push millions of people from their homes and will likely cause more displacement in the coming years. | Addresses some of the fundamental causes of climate change |
| 13. Climate action | NA | Take urgent action to combat climate change and its impacts |
| 14. Life below water | Sustainable management of marine ecosystems preserves local food sources. | Increases resilience to climate change |
| 15. Life on land | Sustainable management of terrestrial ecosystems preserves local food sources. | Increases resilience to climate change |
| 16. Peace, justice and strong institutions | Conflict and violence displaced 11.8 million people in 2017. Internal displacement can also facilitate the recruitment of IDPs by armed groups. | Increases resilience to climate change |
| 17. Partnerships for the goals | The scale and intensity of internal displacement can be reduced by dedicated policies, greater national accountability, increased participation and specific progress monitoring. | Increases resilience to climate change |
IDPs means internally displaced persons;
SDG means sustainable development goals.
Adopted from http://www.internal-displacement.org/global-report/grid2018/.
The drivers of migration are complex and include political, economic, social, cultural and environmental factors (Figure 1). These same factors can determine whether migration is permanent or temporary. The drivers of migration can be grouped into five categories17–19:
1) Push factors that force people to migrate including war, unemployment, food scarcity, over-population or prosecution.
2) Pull factors that attract people to a new destination including work and educational opportunities, political or religious freedom.
3) Network drivers that facilitate the migration process such family ties, social support, kinship, safety and feasibility of transport.
4) National policies that allow or prohibit migration.
5) Personal aspirations and motivations.
Figure 1.
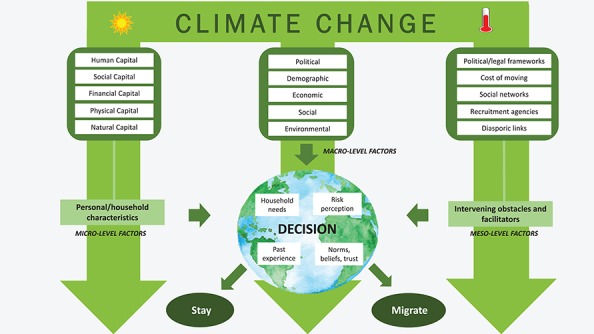
Conceptual framework of climate change and other drivers of migration.27,30,34
These drivers are often interconnected and situation specific (Figure 1). They can also interact with climate change, which can itself be a trigger for migration (Figure 2).20,21 Although environmental drivers do not appear to have been the most significant contributor to international migration to date,22,23 migration in response to the consequences of climate change can be a pragmatic adaption strategy that balances the risks of staying and the risks of moving.20,24–27 For example, for the Tonga-speaking people in Southern Zambia, migration is an adaptation strategy to climate variability when the availability of water affects both agricultural production and livestock survival.28 Additional warming of 0.5°C is projected to further exacerbate climate-related drivers of migration; studies suggest that an increase in extreme weather and climate events and disasters associated with climate change could trigger an increase in migration.29–32
Figure 2.
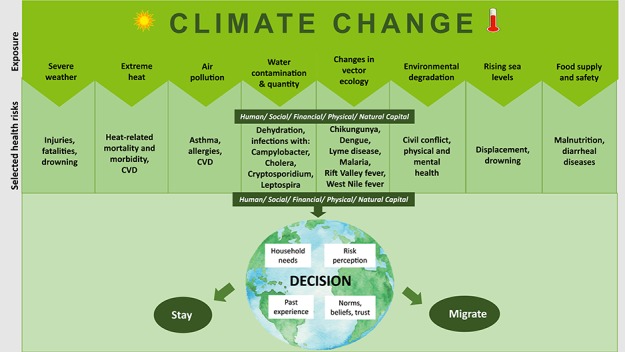
Conceptual framework of health impacts from climate change as drivers of migration.27,30,34
Climate change impacts on migration and health
The complex and multiple drivers of migration mean that it is difficult to attribute specific migrations to climate change (Figures 1 and 2). As a result, projections of migration associated with climate change vary widely, ranging from 50 million to 200 million, with these numbers based on extrapolations.27,33 In 2018, a World Bank report on the impact of climate change on migration estimated that by 2050—in just three regions—climate change could force more than 143 million people to move within their countries.34Table 2 summarizes the World Bank findings from three case studies in sub-Saharan Africa (Ethiopia), South Asia (Bangladesh) and Latin America (Mexico).
Table 2.
Climate migration for Ethiopia, Bangladesh and Mexico in 205034
| Ethiopia | Bangladesh | Mexico | |
|---|---|---|---|
| Population in 2050 compared with 2020 | Increases to 159 million from 103 million (in SSP2) or 184 million from 105 million (in SSP4)a | Increases to 196 million from 166 million (in SSP2) or 177 million from 164 million (in SSP4)a | Increases to 149 million from 126 million (in SSP2) or 136 million from 125 million (in SSP4)a |
| Number of climate migrants by 2050 | Highest in more climate-friendly scenario, with average projection of 1.5 millionb | Highest in pessimistic reference scenario, with average projection of 13.3 million | Highest in pessimistic reference scenario, with average projection of 1.7 million |
| Internal climate-related migration | Southern highlands Ahmar Mountains in the east | Main stem of the Ganges River basin in the west | Central plateau near Mexico City and east of Puebla Smaller hotspots farther south in Oaxaca State and on the northern coast of Baja California south of Tijuana |
| Climate out-migration hotspots | Northern highlands Addis Ababa | Dhaka and river delta south of the city Eastern coast near Chittagong Northeast | Along Gulf of Mexico, especially Veracruz and Tabasco States, in southern state of Chiapas and on Pacific coast, especially Guerrero State Scattered in the arid north |
| Climate migration in/out of rural livelihood zones | In-migration: pastoral and rangelands, semi-natural and wild areas; out-migration: rainfed croplands | In-migration: rainfed croplands; out-migration: rice-growing areas | In-migration: pastoral and rangelands; out-migration: rainfed croplands |
SSP2 means moderate development; SSP4, unequal development.
aThe moderate development SSP2 scenario for Bangladesh and Mexico yield larger populations than the unequal development SSP4 scenario because both are middle-income countries. Only low-income countries show marked increases in population under SPP4.
bThe higher number of climate migrants under the more climate-friendly scenario in Ethiopia is in part driven by the regional climate models, which project lower water availability by 2050 in general compared with the other two scenarios (pessimistic reference and more inclusive development scenarios), which are coupled with higher emissions.
Evidence for the possible role of climate change on migration comes from different sources (Figure 1 and 2). These include studies of the extent to which `temperature and precipitation’ are associated with out-migration. For example, in recent decades, temperature had a statistically significant effect on out-migration from agriculture-dependent countries.35 There is a nexus between climate change and migration in that temperature and precipitation are positively associated with migration: a 1°C increase in average temperature in the sending country is associated with a 1.9% increase in bilateral migration flows; an additional millimeter of average annual precipitation is associated with an increase in migration of 0.5%.36 Another study suggests that an increase in precipitation anomalies from the long-term mean may also be associated with an increase in out-migration.37 Under a moderate climate change scenario, if global mean temperature rises by 2°C, tropical populations would have to move considerable distances in order find places where temperatures are similar to those in places they currently live in and to preserve their annual mean temperatures.38
`Extreme weather events’ linked to climate change, such as heat waves, droughts, storms, floods and wildfires, cause short-term population displacement (Figure 2). In 2017, disasters—most of which were related to extreme weather—displaced 18.8 million people in 135 countries (Figure 3).9 In 2018, California experienced the most destructive wildfire season on record with more than 81,000 people being evacuated from their homes.39 A number of factors led to these fires, including accumulated natural fuel and compounding atmospheric conditions that were linked to climate change.40 Based on the experience of other events in the USA, some people will eventually return to their communities, but others will permanently relocate. For example, following Hurricane Katrina, it was estimated that between 37% and 54% of the population returned,41 with young adults being more likely to have moved further away.41,42 In 1992, after Hurricane Andrew in Florida, 76% of displaced residents relocated within the same county, 18% moved within the state and 6% moved out of state.43
Figure 3.
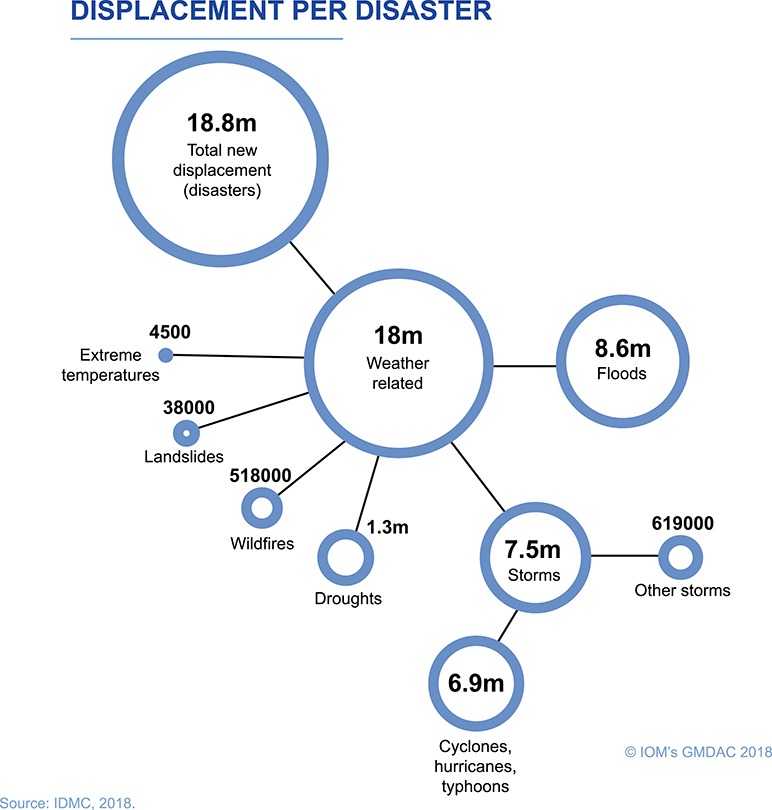
Internal displacement by environmental disasters in 2017.9
In some cases, extreme weather events can cause longer-term migration. For example, an increase in the frequency and intensity of droughts in Tanzania has killed livestock and forced the Maasai people to migrate from rural to urban settings, with documented implications for their mental health.44 Similarly, prior to the Syrian migrant crisis in 2015, the Fertile Crescent was affected by a severe and sustained drought associated with anthropogenic increases in greenhouse gas emissions45 and this, combined with unsustainable agricultural and environmental practices, contributed to internal migration, political instability and conflict and eventually to an exodus of one million migrants to Europe.46
`River flooding and erosion’ has adversely affected agriculture in Bangladesh and resulted in population migration to India (Figure 2).47 Climate change models project an increased frequency and likelihood of severe storms, with implications for sea level and flooding, in the Ganges–Brahmaputra–Meghna delta, and this is likely to displace a large number of people.48 In Pakistan, the adverse economic impact of heat waves on agricultural and non-agricultural activity has increased out-migration.49 In contrast, flooding in Pakistan was not associated with significantly increased migration, possibly due to the larger scale of the response by relief agencies to floods compared with heat waves.49 In other regions, food scarcity due to flooding has contributed to internal migration. In 2018 in Mali, flooding destroyed fields, damaged grain stores and impeded livestock production and, as a result, an estimated 4.6 million people are food insecure and 77 000 internally displaced.
`Gradual changes’ due to climate change, such as changing rainfall patterns, rise in sea level, increased salinization and decreased soil fertility, can also be a driver for migration (Figure 2).
Climate change impacts on migration: implications for public health practice
Migration has implications for health and public health practice.50,51 Migrants can be exposed to health risks in their country of origin and country of destination (Figure 2)52; they may be particularly at risk during their journey, due to lack of shelter, exposure to harsh climatic conditions, heat and over-crowded, inadequate transit and detention centres.53 Public health interventions need to target migrants in all of these settings, and especially during migration, in order to minimize associated health risks (Figure 2).
Sudden displacement because of a disaster or other event can be very stressful and manifest in post-traumatic stress disorders, depression or anxiety that can continue for months or even years.54 Other factors that can affect the mental health of migrants include family separation, acculturation, job insecurity, restricted mobility, dangerous border crossings, stigmatization and marginalization.55 Stress is associated with higher rates of depression and anxiety disorders in the short term and with cardiovascular disease in the longer term.56–58
Epidemic intelligence data from the European Centre for Disease Prevention and Control (ECDC) suggests that migration is a relatively infrequent driver of communicable disease threat events in Europe, compared with travel and tourism.59,60 There was no evidence during the 2015 migrant crisis in Europe that migrants posed a risk to European Union citizens from communicable diseases,61 and despite the barriers to accessing immunization that migrants experience, the contribution of migrants to the current measles outbreaks in Europe is minimal.62 However, migrants may be at increased risk of communicable disease due to exposure or conditions during migration and in the country of destination (Table 3).29,61,63,64–67 For example, there is evidence that tuberculosis transmission occurs on migration routes to Europe, including during long-term stays in refugee camps.68 Overcrowded and inadequate refugee camps, detention centres and housing can spread vectors (e.g. lice and fleas) that transmit diseases such as relapsing fever, trench fever and epidemic or murine typhus.61 Poor and overcrowded living conditions can also increase the risk of respiratory diseases, such as seasonal influenza.69 Migrants living in overcrowded conditions with poor sanitation may also be at risk of cholera outbreaks.70 Overcrowding, poor sanitation and limited access to health services can also facilitate the emergence of antimicrobial resistance (AMR) among migrants, particularly refugees and asylum seekers.71
Table 3.
Summary of evidence-based statements for screening and vaccination for communicable diseases among newly arrived migrants within the EU/EEA
| Infectious disease | Evidence-based statement |
|---|---|
| Active TB | Offer active TB screening using CXR soon after arrival for migrant populations from high-TB incidence countries. Those with an abnormal CXR should be referred for assessment of active TB and have a sputum culture for Mycobacterium tuberculosis. |
| LTBI | Offer LTBI screening using a TST or an IGRA soon after arrival for all migrant populations from high-TB-incidence countries and link to care and treatment where indicated. |
| HIV | Offer HIV screening to migrants who have lived in communities with high HIV prevalence (≥1%). If HIV positive, link to care and treatment as per clinical guidelines. Offer testing for HIV to all adolescents and adult migrants at high risk for exposure to HIV. If HIV positive, link to care and treatment as per clinical guidelines. |
| Hepatitis B | Offer screening and treatment for hepatitis B (HBsAg and anti-HBc, anti-HBs) to migrants from intermediate/high prevalence countries (≥2% to ≥5% HBsAg.) Offer hepatitis B vaccination series to all migrant children and adolescents from intermediate/high prevalence countries (≥2% to ≥5% HBsAg) who do not have evidence of vaccination or immunity. |
| Hepatitis C | Offer hepatitis C screening to detect Hepatitis C Virus antibodies to migrant populations from HCV-endemic countries (≥2%) and subsequent RNA testing to those found to have antibodies. Those found to be Hepatitis C Virus RNA positive should be linked to care and treatment. |
| Schistosomiasis | Offer serological screening and treatment (for those found to be positive) to all migrants from countries of high endemicity in sub-Saharan Africa and focal areas of transmission in Asia, South America and North Africa. |
| Strongyloidiasis | Offer serological screening and treatment (for those found to be positive) for strongyloidiasis to all migrants from countries of high endemicity in Asia, Africa, the Middle East, Oceania and Latin America. |
| Vaccine-preventable diseases | Offer vaccination against MMR to all migrant children and adolescents without immunization records as a priority. Offer vaccination to all migrant adults without immunization records with either one dose of MMR or in accordance with the MMR immunization schedule of the host country. Offer vaccination against diphtheria, tetanus, pertussis, polio and HiBa (DTaP-IPV-Hib) to all migrant children and adolescents without immunization records as a priority. Offer vaccination to all adult migrants without immunization records in accordance with the immunization schedule of the host country. If this is not possible, adult migrants should be given a primary series of diphtheria, tetanus and polio vaccines. See Table 5 for details. |
CXR means chest X-ray; LTBI, latent TB infection; TST, tuberculin skin test; IGRA, interferon-gamma release assay; MMR, measles/mumps/rubella.
Source: ECDC. Public health guidance on screening and vaccination for infectious diseases in newly arrived migrants within the EU/EEA. https://ecdc.europa.eu/sites/portal/files/documents/Public%20health%20guidance%20on%20screening%20and%20vaccination%20of%20migrants%20in%20the%20EU%20EEA.pdf.
Vaccination against Hib is only recommended to children up to five years of age.
Migrants may be at increased risk of communicable disease in their country of destination due to factors including lack of vaccination, low socioeconomic status and poor living conditions and limited access to health care (Table 3).69 Recent evidence from the European Union (EU) and the European Economic Area (EEA), based on CD4 cell counts and HIV-RNA trajectories from seroconversion also suggests that migrants may be at risk of HIV transmission in their country of destination; two-thirds of a sample of HIV-positive migrants from sub-Saharan Africa, Latin America and the Caribbean acquired their HIV infection in the country of destination.72
Essential public health measures include ensuring adequate living conditions, access to health care in refugee camps, detention centres, screening for communicable diseases and assessment of vaccination status on arrival in countries of destination (Table 4). Available evidence shows that it is cost-effective to screen child, adolescent and adult migrants for active and latent tuberculosis, HIV, hepatitis C, hepatitis B, strongyloidiasis and schistosomiasis (Table 3).73 Targeted HIV prevention, testing and treatment programmes are also required in countries where migrants are at risk of HIV acquisition after arrival. There is also a clear benefit from ensuring that migrants are included in vaccination programmes and providing catch-up vaccinations where needed (Table 5). Particular attention should be given to vulnerable children, women and the elderly, who might also suffer from non-communicable diseases, such as cardiovascular diseases, diabetes, cancer, chronic lung diseases, mental health74 and trauma. Sudden migration can result in complications from non-communicable diseases if treatment and care are discontinued or if access to medications is interrupted. These conditions can cause a life-threatening deterioration and acutely exacerbate pre-existing conditions in the event of sudden migration (Table 6).
Table 4.
| Clinical presentation | Differential diagnosis to consider |
|---|---|
| Fever | Typhoid fever Malaria Louse-borne diseases Visceral leishmaniasis Amoebic abscess Arboviruses |
| Respiratory symptoms | Tuberculosis Influenza |
| Gastrointestinal symptoms | Cholera Typhoid fever Shigellosis Amoebic colitis Helminthiasis: ascaris, whipworm and hookworm |
| Sores | Scabies Cutaneous leishmaniasis Cutaneous diphtheria |
| Skin rash | Measles Rubella Louse-borne diseases |
| Meningitis or other neurological symptoms | Rabies Invasive bacterial diseases (Neisseria meningitidis, Haemophilus influenza type b and Streptococci pneumoniae) Polio Dengue and other arboviruses |
This list identifies diseases to be considered in addition to the more common causes of the clinical presentations among resident EU populations.
Table 5.
Vaccinations to be offered to migrants in the absence of documented evidence of prior vaccination within the EU/EEA64
| Disease/age group | Children and adolescents (<18 years) | Adults (>18 years) |
|---|---|---|
| Priority vaccinations | ||
| MMR | Administer to individuals ≥9 months of age. Two doses of MMRa should be administered at least 1 month apart but preferably longer according to national guidelines. Measles vaccine provided before 12 months of age does not induce protection in all and should be repeated after 12 months of age. | Administer one or two doses of MMR to all individuals, according to national guidelines.a |
| Diphtheria, tetanus, pertussis, polio and Hib | Administer to individuals ≥2months, three doses of DTaP-IPV-Hib (Hib-component only for children <6 years unless other country-specific recommendations) containing vaccines at least 1 month apart, followed by a booster dose according to national guidelines. Pentavalent and hexavalent combination vaccines are authorized up to 6 years of age. | Administer to all adults, three doses of TdaPIPV-containing vaccinesb according to national guidelines. |
| To be considered | ||
| Hepatitis B | Administer to individuals ≥2 months, three doses according to national guidelines.c Administer to new-born infants of HBsAg-positive mothers within 24 hours of birth, according to national guidelines. | Administer to all adults, with or without previous screening, according to national guidelines. |
| Meningococcal disease | National guidelines for meningococcal vaccines against serogroups A, B, C, W135 and Y should be followed, unless the epidemiological situation suggests otherwise. | |
| Pneumococcal disease | Administer to individuals ≥2 months with one to three doses of conjugate vaccine at least 1 month apart, according to national guidelines. | Administer to individuals ≥65 years, according to national guidelines. |
| Varicella | National guidelines should be followed unless the epidemiological situation suggests otherwise. If used, administer to individuals ≥11 months of age, two doses of varicella at least 1 month apart, but preferably longer. | National guidelines should be followed unless the epidemiological situation suggests otherwise. Consider vaccinating non-immune non-pregnant women of childbearing age. |
| Influenza | National guidelines should be followed unless the epidemiological situation suggests otherwise. Consider vaccinating risk groups over 6 months of age ahead of and during influenza season. | National guidelines should be followed unless the epidemiological situation suggests otherwise. Consider vaccinating risk groups, including pregnant women, ahead of and during influenza season. |
| Tuberculosis | Administer BCG according to national guidelines. Re-vaccination with BCG is not recommended. | BCG is generally not recommended for adults, unless specific reasons suggest otherwise. |
MMR means measles/mumps/rubella;
EU means European Union;
EEA means European Economic Area.
aMMR vaccine is contra-indicated in immunocompromised individuals and during pregnancy. Pregnancy should be avoided for one month after MMR vaccination.
bIf there is a vaccine shortage administer at least one dose of vaccine containing a cellular pertussis component.
cTesting for hepatitis B virus infection (HBsAg) could be done before the vaccine is administered.
Table 6.
Impact of sudden migration on the health of people with non-communicable diseases
| Impact of sudden migration | Examples of health consequences |
|---|---|
| Physical injuries | Factors such as secondary infections and poor control of glycaemia compromise management of acute traumatic injuries |
| Forced displacement | Loss of access to medication or devices, loss of prescriptions, lack of access to health care services leading to prolongation of disruption of treatment |
| Degradation of living conditions | Loss of shelter, shortages of water and regular food supplies and lack of income add to physical and psychological strain |
| Interruption of care | Due to destruction of health infrastructure, disruption of medical supplies and the absence of health care providers who have been killed, injured or are unable to return to work |
| Interruption of power supplies or safe water | Life-threatening consequences, especially for people with end-stage renal failure who require dialysis |
Travel and tourism
Travel, including for business and tourism, has increased dramatically in recent decades. Globally, in 2017, commercial airlines carried more than 4 billion passengers; this is projected to have risen to 4.4 billion in 2018 and to continue to increase in the coming years.75 Air travel contributes to greenhouse gas emissions and, hence, to climate change.
At the same time, the effects of climate change on tourism assets, such as biodiversity, coral reefs, glaciers and cultural heritage, are leading to an increase in `last chance’ travel to destinations before they are further degraded.76–78 For example, in the southern hemisphere, sea level is projected to rise by 30–150 cm by the end of this century, submerging much of the Maldives.79 In northern latitudes, climate change is already having an adverse impact on the winter tourism industry in Lapland and may make it impossible to maintain its snow-covered winter wonderland in future.80 In many ski resorts, artificial snowmaking, which has high energy costs, is increasingly being used to supplement natural snow, to improve reliability and to extend the season.
Climate change impacts on travel and health
Climate change can be a factor in creating conditions suitable for vector-borne disease transmission. Importation of pathogens from endemic areas can then result in the subsequent spread of these diseases under suitable climatic conditions. Extended seasonal transmission seasons due to climate change can also increase the window of opportunity of pathogen importation.
Climatic suitability, including lower and upper temperature thresholds, affects the growth, abundance and survival of mosquito vectors such as Aedes aegypti and Aedes albopictus that can transmit dengue, Zika and chikungunya. In Europe, a warmer climate appears to be associated with more frequent outbreaks of dengue and chikungunya81 and climatic conditions are projected to become more suitable for onward transmission of the chikungunya pathogen.82 Climate change may have contributed to the explosive spread of Zika in Brazil.83 The epidemic was preceded by `record warmest’ climatic conditions, accompanied by a severe drought.84 The utilization of home water storage containers during the drought might have provided breeding sites for Aedes mosquitoes and increased exposure to mosquitoes. Virus importation into a susceptible population could then have triggered the epidemic.83
Precipitation, another important environmental factor affected by climate change, also influences the availability of conditions suitable for mosquito vectors. For example, heavy rainfall increases the abundance of A. albopictus and, hence, the risk of transmission of dengue and chikungunya.85 Climate change can increase the risk of other vector-borne diseases, including tick-borne and rodent-borne infections,85 and can also influence the range, seasonality and incidence of water-borne diseases such as cholera.86,87
Global air travel may facilitate the spread of `resistant pathogens’. For example, it is thought to have facilitated the rapid dissemination of methicillin-resistant Staphylococcus aureus from the UK and North America across Europe and then to Asia.88 Vancomycin-resistant enterococci and Klebsiella pneumoniae carbapenemase-producing K. pneumoniae followed a similar trajectory.88 The burden of antibiotic resistance in destination countries can also be exacerbated by climate change, because an increase in ambient temperature is associated with a significant increase in antibiotic resistance for common pathogens, including K. pneumoniae and S. aureus.89 It is hypothesized that temperature accelerates horizontal transfer of resistance genes or the uptake of genetic material. Ambient temperature may also facilitate environmental growth of resistant strains and enhance transmission from food, agriculture and environmental sources.89
Climate change impacts on travel: implications for public health practice
Air travel can facilitate the spread of communicable diseases around the globe. Passenger volume has been identified as a significant driver of the importation of viremic passengers.90,91 Flights directly connect millions of passengers between Europe and Asia, Africa, North America and South America, with many of these locations ‘hot spots’ for the emergence of communicable diseases.92 A disease outbreak in one part of the world can quickly spread to another part via air travel.59,60 For example, in-flight transmission of severe acute respiratory syndrome (SARS) in 2003 resulted in the rapid spread of SARS-associated coronavirus (SARS-CoV) around the world.93 International air travellers departing from Mexico in 2009 unknowingly carried and disseminated the novel influenza virus A(H1N1)v around the world.94 Similarly, air transport networks contributed to the spread of Middle East Respiratory Syndrome from Saudi Arabia in 2012, chikungunya dispersion in the Americas in 2013, Ebola from West Africa in 2014 and Zika spread in the Americas in 2015.95–98
More specifically, air travel can increase the risk of importation of pathogens from endemic areas into regions with competent mosquito vectors and suitable climatic and environmental conditions for vector-borne diseases.90 Dengue, a mosquito-borne viral disease, is a significant public health concern, threatening almost half of the world’s population.99 Transmission occurs largely in tropical and sub-tropical regions, but outbreaks have occurred in Europe around the Mediterranean where A. albopictus is present.100 Infected air passengers from endemic areas can arrive in Europe during their viremic period, be bitten by local mosquito vectors and transmit the dengue virus locally and trigger an outbreak due to a warming climate.81 Other means of transport are also implicated in the spread of disease-causing pathogens. For example, ballast from cargo ships played a role in moving pathogenic Vibrios to new locations that were environmentally and climatically suitable, even in northern latitudes.101 Travel and tourism can also facilitate the importation of pathogens from developed countries with low vaccination coverage, to developing countries with high rates of susceptible individuals due to lack of health care access.102,103
Responding to the public health challenges associated with travel and climate change requires robust national surveillance systems, including effective tracking of vector location and disease importation.104 Integrated surveillance of invasive and endemic mosquito species is crucial for effective prevention and control of vector-borne diseases.104 Early detection of outbreaks can be aided by seasonal surveillance in areas where competent vectors are active and in close proximity to airports with a large influx of passengers from endemic areas.90 For example, the risk of dengue importation can be described by a model that relates air travellers from dengue-affected areas to dengue importation.90 This approach can delineate in space and time where the risk is the highest, and target seasonal surveillance to high-risk areas, for early case detection and intervention.
An important consideration when projecting risk of disease transmission associated with climate change and travel is that the timing of risks may be under-estimated, i.e. transmission may occur sooner than models suggest. For example, the modelled future environmental suitability of A. aegypti in the contiguous USA in the period 2061–2080 projects potential suitability in southern areas of mid-western states, such as Illinois, Indiana and Ohio.105 However, breeding colonies of A. aegypti were found in Ontario in southern Canada in 2017, indicating that the risk of transmission of diseases such as dengue fever and Zika may occur earlier than the projections suggest.106
The importation and spread of tropical pathogens in temperate regions due to climate change is another aspect to consider for public health practice. It is a potential threat to the safety of the blood supply and, hence, of blood transfusions, particularly with respect to pathogens for which there are no diagnostic tests.107–111 Expansion of areas with an increased risk of communicable diseases due to climate change also increases the risk of blood bank contamination with communicable pathogens as a higher number of prospective blood donors are exposed to potential infections for a longer period, e.g. if climate change alters the length of the annual mosquito activity season.107 Moreover, the asymptomatic phase of many infections, even if it is relatively short, increases the potential for transmission by transfusion.112 Climate change projections of the probability of infection should therefore be used for preparedness activities. In addition, certain pathogens, such as the West Nile virus, can persist in stored blood components and subsequently cause infection through intravenous application. Pathogen reduction technology that inactivates pathogens in donated blood is a strategy that could be used for pre-emptive risk reduction.108
Conclusion
The world is warmer today than in pre-industrial times, and warming is projected to continue. The frequency, duration and intensity of extreme weather events have increased, with implications for migration in particular. Global warming is associated with migration from farming communities and from small islands and coastal areas. Evidence of climate change impacts on migration in other settings is less clear. The combined impact of travel and climate change can favour the importation, establishment and spread of tropical diseases in temperate regions.
These developments require public health action, including targeted and culturally appropriate interventions and novel technologies, to prevent and control emerging health threats associated with the interaction between climate change, migration and travel. It calls for training of health care professionals to provide appropriate health care (prevention, screening, and treatment) for migrants and for risk assessment of diseases among travellers/tourists. Adequate living conditions, screening and vaccination programmes, and medical interventions for migrants can prevent outbreaks of communicable diseases and the spread of resistant pathogens. Assessment and interventions also need to encompass chronic conditions, mental health and trauma due to migration. Targeted HIV prevention, testing and treatment programmes are also required in countries where migrants are at risk of HIV acquisition after arrival.
Effective national surveillance systems that include tracking of vector location and disease importation can inform targeted prevention and control interventions. Novel approaches including modelling the arrival of air passengers into environmentally and climatically receptive areas, to improve assessment of the risk of importation of pathogens from endemic areas, and assessment of climatic suitability, can inform seasonal surveillance or active case finding. Specific measures may be required to ensure blood safety, including pathogen reduction technology, where there is a risk of the importation and spread of tropical pathogens in temperate regions.
Author statements
The authors report no financial interests or connections, direct or indirect or other situations that might raise the question of bias in the work reported or the conclusions, implications or opinions stated—including pertinent commercial or other sources of funding for the individual author(s) or for the associated department(s) or organization(s), personal relationships or direct academic competition.
Author Contributions
J.C.S. wrote the first draft of the paper. Both authors approved the final paper.
Acknowledgements
We would like to thank the editor and the three anonymous reviewers for detailed and constructive feedback on the manuscript. We also appreciated the insightful comments and suggestions from Teymur Noori, Pontus Naucler and Senia Rosales-Klintz at ECDC. The views and opinions expressed herein are the authors’ own and do not necessarily state or reflect those of ECDC. ECDC is not responsible for the data and information collation and analysis and cannot be held liable for conclusions or opinions drawn. We should like to thank Wei-Yee Leong from the Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore for her help with the figures.
Conflicts of interest: None declared.
References
- 1. IPCC Global warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty In: IPCC, 2018: Summary for Policymakers. 2018,https://www.ipcc.ch/sr15/ (17 April 2019, date last accessed).
- 2. Ebi KL, Ogden NH, Semenza JC et al. Detecting and attributing health burdens to climate change. Environ Health Perspect 2017; 125:085004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Weather Attribution 2018https://www.worldweatherattribution.org. (17 April 2019, date last accessed).
- 4. Stringer C. Human evolution: out of Ethiopia. Nature 2003; 423:692–3, 5. [DOI] [PubMed] [Google Scholar]
- 5. Liu H, Prugnolle F, Manica A et al. A geographically explicit genetic model of worldwide human-settlement history. Am J Hum Genet 2006; 79:230–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Menocal PB, Stringer C. Human migration: climate and the peopling of the world. Nature 2016; 538:49–50. [DOI] [PubMed] [Google Scholar]
- 7. Timmermann A, Friedrich T. Late Pleistocene climate drivers of early human migration. Nature 2016; 538:92–5. [DOI] [PubMed] [Google Scholar]
- 8. Rito T, Richards MB, Fernandes V et al. The first modern human dispersals across Africa. PloS One 2013; 8:e80031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Internal Displacement Monitoring Centre (IDMC) Global Report on Internal Displacement. 2018, http://www.internal-displacement.org/global-report/grid2018/ (17 April 2019, date last accessed).
- 10. Organisation for Economic Co-operation and Development (OECD) Is Migration Good for the Economy? Migration Policy Debates 2014. https://www.oecd.org/migration/OECD%20Migration%20Policy%20Debates%20Numero%202.pdf (17 April 2019, date last accessed).
- 11. Growth Analysis The Effects of Immigration on Economic Growth—a Literature Study. 2018. http://www.tillvaxtanalys.se/in-english/publications/pm/pm/2018-04-26-the-effects-of-immigration-on--economic-growth---a-literature-study.html (17 April 2019, date last accessed).
- 12. International Organization for Migration (IOM) World Migration Report. 2018. http://publications.iom.int/system/files/pdf/wmr_2018_en.pdf (17 April 2019, date last accessed).
- 13. Organisation for Economic Co-operation and Development (OECD) Is Migration Good for the Economy? 2014. https://www.oecd.org/migration/OECD%20Migration%20Policy%20Debates%20Numero%202.pdf (17 April 2019, date last accessed).
- 14. Assembly UNUG Sustainable Development Goals (SDGs). 2015. https://sustainabledevelopment.un.org/?menu=1300 (17 April 2019, date last accessed).
- 15. Aitsi-Selmi AMV. Protecting the health and well-being of populations from disasters: health and health care in the Sendai framework for disaster risk reduction 2015–2030. Prehosp Disaster Med 2016; 31:74–8. [DOI] [PubMed] [Google Scholar]
- 16. UNFCCC The Paris Agreement CN7352016TREATIES-XXVII7d (Depositary Notification) PARIS, 12 DECEMBER 2015 2015.
- 17. Black RK D, Schmidt-Verkerk K. Migration and climate change: towards an integrated assessment of sensitivity. Environ Plan 2007; 43:431–50. [Google Scholar]
- 18. Massey D. (ed). Theory of Migration. Orlando, FL, USA: University of Central Florida, 2015. [Google Scholar]
- 19. Weir T, Dovey L, Orcherton D. Social and cultural issues raised by climate change in Pacific Island countries: an overview. Reg Environ Chang 2017; 17:1017–28. [Google Scholar]
- 20. Black R, Bennett SR, Thomas SM et al. Climate change: migration as adaptation. Nature 2011; 478:447–9. [DOI] [PubMed] [Google Scholar]
- 21. Stephenson J, Newman K, Mayhew S. Population dynamics and climate change: what are the links? J Public Health (Oxf) 2010; 32:150–6. [DOI] [PubMed] [Google Scholar]
- 22. Brzoska M, Frölich C. Climate change, migration and violent conflict: vulnerabilities, pathways, and adaptation strategies. Migration Dev 2015; 5:190–210. [Google Scholar]
- 23. Reuveny R. Climate change-induced migration and violent conflict. Polit Geogr 2007; 26:656–73. [Google Scholar]
- 24. Tacoli C. Crisis or adaptation? Migration and climate change in the context of high mobility. Environ Urban 2009; 21:513–25. [Google Scholar]
- 25. de Sherbinin A, Castro M, Gemenne F et al. Climate change. Preparing for resettlement associated with climate change. Science (New York, NY) 2011; 334:456–7. [DOI] [PubMed] [Google Scholar]
- 26. Adger WNP JM, Barnett J, Dabelko GD et al. (eds). Human Security. Cambridge, UK: Cambridge University Press, 2015. [Google Scholar]
- 27. The Government Office for Science Foresight: Migration and Global Environmental Change. 2018. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/287717/11-1116-migration-and-global-environmental-change.pdf (17 April 2019, date last accessed).
- 28. Simatele D, Simatele M. Migration as an adaptive strategy to climate variability: a study of the Tonga-speaking people of southern Zambia. Disasters 2015; 39:762–81. [DOI] [PubMed] [Google Scholar]
- 29. McMichael C, Barnett J, McMichael AJ. An ill wind? Climate change, migration, and health. Environ Health Perspect 2012; 120:646–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schwerdtle P, Bowen K, McMichael C. The health impacts of climate-related migration. BMC Med 2017; 16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Burrows K, Kinney PL. Exploring the climate change, migration and conflict nexus. Int J Environ Res Public Health 2016; 13:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schutte S, Gemenne F, Zaman M et al. Connecting planetary health, climate change, and migration. Lancet Planet Health 2018;2:e58–e9. [DOI] [PubMed] [Google Scholar]
- 33. Myers N. Environmental refugees: an emergent security issue In: Documents from the 13th Economic Forum, Proceedings of the 13th Meeting of the Organization for Security and Co-operation in Europe (OSCE) Economic Forum, Session III (Environment and Migration). Czech Republic: Prague, 2005. [Google Scholar]
- 34. Kumari Rigaud K, de Sherbinin A, Jones B et al. Groundswell: Preparing for Internal Climate Migration. Washington, DC: The World Bank, 2018. [Google Scholar]
- 35. Cai R, Feng S, Oppenheimer M et al. Climate variability and international migration: the importance of the agricultural linkage. J Environ Econ Manag 2016; 79:135–51. [Google Scholar]
- 36. Backhaus A, Martinez-Zarzoso I, Muris C. Do climate variations explain bilateral migration? A gravity model analysis. IZA J Migration 2015; 4:3. [Google Scholar]
- 37. Coniglio ND, Pesce G. Climate variability and international migration: an empirical analysis. Environ Dev Econ 2018; 20:434–68. [Google Scholar]
- 38. Hsiang SM, Sobel AH. Potentially extreme population displacement and concentration in the tropics under non-extreme warming. Sci Rep 2016; 6:25697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thomas Fuller KJ, Dougherty C. California fires only add to acute housing crisis. The New York Times 2018; 15:2018. [Google Scholar]
- 40. Radke J, Biging GS, Roberts K. Assessing extreme weather-related vulnerability and identifying resilience options for California's interdependent transportation fuel sector. August 2018.
- 41. Fussell E. The long term recovery of New Orleans' population after hurricane Katrina. Am Behav Sci 2015; 59:1231–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sastry N, Gregory J. The location of displaced New Orleans residents in the year after hurricane Katrina. Demography 2014; 51:753–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Smith SK, McCarty C. Demographic effects of natural disasters: a case study of hurricane Andrew. Demography 1996; 33:265–75. [PubMed] [Google Scholar]
- 44. Heaney AK, Winter SJ. Climate-driven migration: an exploratory case study of Maasai health perceptions and help-seeking behaviors. Int J Public Health 2016; 61:641–9. [DOI] [PubMed] [Google Scholar]
- 45. Kelley CP, Mohtadi S, Cane MA et al. Climate change in the Fertile Crescent and implications of the recent Syrian drought. Proc Natl Acad Sci U S A 2015; 112:3241–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. United Nations High Commissioner for Refugees (UNHCR) Operational Portal. Refugee Situations. Mediterranean Situation. 2018. https://data2.unhcr.org/en/situations/mediterranean (17 April 2019, date last accessed).
- 47. Banjeree L. Effect of flood on agricultural wages in Bangladesh: an empirical analysis. World Dev 2007; 35:1989–2009. [Google Scholar]
- 48. Kay S, Caesar J, Wolf J et al. Modelling the increased frequency of extreme sea levels in the Ganges-Brahmaputra-Meghna delta due to sea level rise and other effects of climate change. Environ Sci: Processes Impacts 2015; 17:1311–22. [DOI] [PubMed] [Google Scholar]
- 49. Mueller V, Gray C, Kosec K. Heat stress increases long-term human migration in rural Pakistan. Nat Clim Chang 2014; 4:182–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Greenaway C, Castelli F. Infectious diseases at different stages of migration: an expert review. J Travel Med 2019; 26. doi: 10.1093/jtm/taz007. [DOI] [PubMed] [Google Scholar]
- 51. Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med 2017; 24. doi: 10.1093/jtm/tax016. [DOI] [PubMed] [Google Scholar]
- 52. Schwerdtle PN, Bowen K, McMichael C et al. Human mobility and health in a warming world. J Travel Med 2019; 26. doi: 10.1093/jtm/tay160. [DOI] [PubMed] [Google Scholar]
- 53. Keim SM, Mays MZ, Parks B et al. Estimating the incidence of heat-related deaths among immigrants in Pima County, Arizona. J Immigr Minor Health 2006; 8:185–91. [DOI] [PubMed] [Google Scholar]
- 54. Edmondson D, Gamboa C, Cohen A et al. Association of posttraumatic stress disorder and depression with all-cause and cardiovascular disease mortality and hospitalization among hurricane Katrina survivors with end-stage renal disease. Am J Public Health 2013; 103:e130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tuggle AC, Cohen JH, Crews DE. Stress, migration, and allostatic load: a model based on Mexican migrants in Columbus, Ohio. J Physiol Anthropol 2018; 37:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychol Health Med 2013; 18:627–44. [DOI] [PubMed] [Google Scholar]
- 57. Sagud M, Jaksic N, Vuksan-Cusa B et al. Cardiovascular disease risk factors in patients with posttraumatic stress disorder (PTSD): a narrative review. Psychiatr Danub 2017; 29:421–30. [DOI] [PubMed] [Google Scholar]
- 58. Albert MA, Durazo EM, Slopen N et al. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: rationale, design, and baseline characteristics. Am Heart J 2017; 192:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Semenza JC, Lindgren E, Balkanyi L et al. Determinants and drivers of infectious disease threat events in Europe. Emerg Infect Dis 2016; 22:581–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Semenza JC, Rocklov J, Penttinen P et al. Observed and projected drivers of emerging infectious diseases in Europe. Ann N Y Acad Sci 2016; 1382:73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Semenza JC, Carrillo-Santisteve P, Zeller H et al. Public health needs of migrants, refugees and asylum seekers in Europe, 2015: infectious disease aspects. Eur J Public Health 2016; 26:372–3. [DOI] [PubMed] [Google Scholar]
- 62. Heywood AE. Measles: a re-emerging problem in migrants and travellers. J Travel Med 2018; 25. [DOI] [PubMed] [Google Scholar]
- 63. McMichael C. Climate change-related migration and infectious disease. Virulence 2015; 6:548–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. ECDC Infectious diseases of specific relevance to newly-arrived migrants in the EU/EEA 2015. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/Infectious-diseases-of-specific-relevance-to-newly-arrived-migrants-in-EU-EEA.pdf.
- 65. Fakoya I, Alvarez-del Arco D, Woode-Owusu M et al. A systematic review of post-migration acquisition of HIV among migrants from countries with generalised HIV epidemics living in Europe: mplications for effectively managing HIV prevention programmes and policy. BMC Public Health 2015; 15:561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Rice BD, Elford J, Yin Z et al. A new method to assign country of HIV infection among heterosexuals born abroad and diagnosed with HIV. AIDS (London, England) 2012; 26:1961–6. [DOI] [PubMed] [Google Scholar]
- 67. Desgrees-du-Lou A, Pannetier J, Ravalihasy A et al. Sub-Saharan African migrants living with HIV acquired after migration, France, ANRS PARCOURS study, 2012 to 2013. Euro Surveill 2015; 20. doi: 10.2807/1560-7917.ES.2015.20.46.30065. [DOI] [PubMed] [Google Scholar]
- 68. Jajou R, de Neeling A, Rasmussen EM et al. A predominant variable-number tandem-repeat cluster of mycobacterium tuberculosis isolates among asylum seekers in the Netherlands and Denmark, deciphered by whole-genome sequencing. J Clin Microbiol 2018; 56. doi: 10.1128/JCM.01100-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ejebe IH, Zhang X, Rangel MG et al. Seasonal influenza vaccination among Mexican migrants traveling through the Mexico-US border region. Prev Med 2015; 71:57–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Swaddiwudhipong W, Ngamsaithong C, Peanumlom P et al. An outbreak of cholera among migrants living in a Thai-Myanmar border area. J Med Assoc Thai 2008; 91:1433–40. [PubMed] [Google Scholar]
- 71. Nellums LB, Thompson H, Holmes A et al. Antimicrobial resistance among migrants in Europe: a systematic review and meta-analysis. Lancet Infect Dis 2018; 18:796–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Alvarez-Del Arco D, Fakoya I, Thomadakis C et al. High levels of postmigration HIV acquisition within nine European countries. AIDS (London, England) 2017; 31:1979–88. [DOI] [PubMed] [Google Scholar]
- 73. European Centre for Disease Prevention and Control ECDC Issues Migrant Screening and Vaccination Guidance. 2018. https://ecdc.europa.eu/en/news-events/ecdc-issues-migrant-screening-and-vaccination-guidance (17 April 2019, date last accessed).
- 74. Abbott A. The mental-health crisis among migrants. Nature 2016; 538:158–60. [DOI] [PubMed] [Google Scholar]
- 75. Glaesser D, Kester J, Paulose H et al. Global travel patterns: an overview. J Travel Med 2017; 24. [DOI] [PubMed] [Google Scholar]
- 76. Lemelin R, Dawson J, Stewart EJ (eds). Last Chance Tourism: Adapting Tourism Opportunities in a Changing World. Abingdon, Oxon, UK: Routledge, 2012. [Google Scholar]
- 77. AE P-MK, KE MN. Last chance tourism and the great barrier reef. J Sustain Tour 2017; 25:397–415. [Google Scholar]
- 78. Emma J, Stewart JW, Espiner S et al. Implications of climate change for glacier tourism. Tourism Geographies 2016; 18:377–98. [Google Scholar]
- 79. Hussain M, Mumtaz S. Climate change and managing water crisis: Pakistan's perspective. Rev Environ Health 2014; 29:71–7. [DOI] [PubMed] [Google Scholar]
- 80. Tervo-Kankare K, Hall CM, Saarinen J. Christmas tourists’ perceptions to climate change in Rovaniemi, Finland. Tourism Geographies 2013; 15:292–317. [Google Scholar]
- 81. Lillepold K, Rocklov J, Liu-Helmersson J et al. More arboviral disease outbreaks in continental Europe due to the warming climate? J Travel Med 2019. doi: 10.1093/jtm/taz017. [DOI] [PubMed] [Google Scholar]
- 82. Tjaden NB, Suk JE, Fischer D et al. Modelling the effects of global climate change on chikungunya transmission in the 21(st) century. Sci Rep 2017; 7:3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Paz S, Semenza JC. El Nino and climate change--contributing factors in the dispersal of Zika virus in the Americas? Lancet (London, England) 2016; 387:745. [DOI] [PubMed] [Google Scholar]
- 84. Munoz AG, Thomson MC, Goddard L et al. Analyzing climate variations at multiple timescales can guide Zika virus response measures. GigaScience 2016; 5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Semenza JC, Suk JE. Vector-borne diseases and climate change: a European perspective. FEMS Microbiol Lett 2018; 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Koelle K, Rodo X, Pascual M et al. Refractory periods and climate forcing in cholera dynamics. Nature 2005; 436:696–700. [DOI] [PubMed] [Google Scholar]
- 87. Walker JT. The influence of climate change on waterborne disease and legionella: a review. Perspect Public Health 2018; 138:282–6. [DOI] [PubMed] [Google Scholar]
- 88. Molton JS, Tambyah PA, Ang BS et al. The global spread of healthcare-associated multidrug-resistant bacteria: a perspective from Asia. Clin Infect Dis 2013; 56:1310–8. [DOI] [PubMed] [Google Scholar]
- 89. MacFadden DR, McGough SF, Fisman D et al. Antibiotic resistance increases with local temperature. Nat Clim Chang 2018; 8:510–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Semenza JC, Sudre B, Miniota J et al. International dispersal of dengue through air travel: importation risk for Europe. PLoS Negl Trop Dis 2014; 8:e3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Tatem AJ, Hay SI, Rogers DJ. Global traffic and disease vector dispersal. Proc Natl Acad Sci U S A 2006; 103:6242–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Jones KE, Patel NG, Levy MA et al. Global trends in emerging infectious diseases. Nature 2008; 451:990–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Olsen SJ, Chang HL, Cheung TY et al. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med 2003; 349:2416–22. [DOI] [PubMed] [Google Scholar]
- 94. Khan K, Arino J, Hu W et al. Spread of a novel influenza a (H1N1) virus via global airline transportation. N Engl J Med 2009; 361:212–4. [DOI] [PubMed] [Google Scholar]
- 95. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet (London, England) 2015; 386:995–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Dixon MG, Schafer IJ. Ebola viral disease outbreak--West Africa, 2014. MMWR Morb Mortal Wkly Rep 2014; 63:548–51. [PMC free article] [PubMed] [Google Scholar]
- 97. Yactayo S, Staples JE, Millot V et al. Epidemiology of chikungunya in the Americas. J Infect Dis 2016; 214:S441–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Faria NR, Azevedo R, Kraemer MUG et al. Zika virus in the Americas: early epidemiological and genetic findings. Science (New York, NY) 2016; 352:345–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Simmons CP, Farrar JJ, Nguyen vV et al. Dengue. N Engl J Med 2012; 366:1423–32. [DOI] [PubMed] [Google Scholar]
- 100. European Centre for Disease Prevention and Control Aedes Albopictus—Current Known Distribution: June 2018. 2018. https://ecdc.europa.eu/en/publications-data/aedes-albopictus-current-known-distribution-june-2018 (17 April 2019, date last accessed).
- 101. Ng C, Goh SG, Saeidi N et al. Occurrence of vibrio species, beta-lactam resistant vibrio species, and indicator bacteria in ballast and port waters of a tropical harbor. Sci Total Environ 2018; 610–611:651–6. [DOI] [PubMed] [Google Scholar]
- 102. Alla A, Waku-Kouomou D, Benjouad A et al. Rapid diversification of measles virus genotypes circulating in Morocco during 2004-2005 epidemics. J Med Virol 2006; 78:1465–72. [DOI] [PubMed] [Google Scholar]
- 103. Tra My PV, Rabaa MA, Vinh H et al. The emergence of rotavirus G12 and the prevalence of enteric viruses in hospitalized pediatric diarrheal patients in southern Vietnam. Am J Trop Med Hyg 2011; 85:768–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Semenza JC, Zeller H. Integrated surveillance for prevention and control of emerging vector-borne diseases in Europe. Euro Surveill 2014; 19 pii: 20757. [DOI] [PubMed] [Google Scholar]
- 105. Monaghan AJ, Sampson KM, Steinhoff DF et al. The potential impacts of 21st century climatic and population changes on human exposure to the virus vector mosquito Aedes aegypti. Clim Change 2018; 146:487–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Windsor-Essex County Health Unit Aedes aegypti Mosquito. 2018. https://www.wechu.org/z-health-topics/aedes-aegypti-mosquito.
- 107. Semenza JC, Tran A, Espinosa L et al. Climate change projections of West Nile virus infections in Europe: implications for blood safety practices. Environ Health 2016; 15:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Semenza JC, Domanović D. Blood supply under threat. Nat Clim Chang 2013; 3:432–5. [Google Scholar]
- 109. Dodd RY, Leiby DA. Emerging infectious threats to the blood supply. Annu Rev Med 2004; 55:191–207. [DOI] [PubMed] [Google Scholar]
- 110. Alter HJ, Stramer SL, Dodd RY. Emerging infectious diseases that threaten the blood supply. Sem Hematol 2007; 44:32–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Stramer SL. Current perspectives in transfusion-transmitted infectious diseases: emerging and re-emerging infections. ISBT science series 2014; 9:30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Stramer SL, Hollinger FB, Katz LM et al. Emerging infectious disease agents and their potential threat to transfusion safety. Transfusion 2009; 49:1S–29S. [DOI] [PubMed] [Google Scholar]


