Severe acute respiratory syndrome (SARS)-associated coronavirus (SARS-CoV) has been identified as the causal agent of SARS. Although not common, acute renal failure (ARF) in SARS patients usually has a catastrophic outcome, with a mortality rate of 77% [1]. The causes of ARF in association with SARS are unknown. An increase in creatine kinase (CK) may play a role [2]. We present two patients who met the definition of probable SARS.
Case 1
A 78-year-old man presented with fever and dyspnoea. SARS-CoV was detected using reverse transcription–polymerase chain reaction (RT–PCR) from his nasopharyngeal aspirate (NPA) and a search for serum IgG antibodies to the SARS-CoV was positive. On the 7th day, his IgG antibody titre against SARS-CoV was 1 : 200, and serum creatinine (SCre) was 1.3 mg/dl. On the 10th day, SCre increased to 1.9 mg/dl in spite of stable haemodynamics; serum myoglobin level was 271 ng/ml (normal <70 ng/ml) and CK was 138 U/l (normal <75 U/l). Serum cytokine level increased from day 5 to day 10; interleukin-6 (IL-6) from 2.9 to 12.5 pg/ml, (normal <9.7 pg/ml) and IL-8 from 19.2 to 110 pg/ml (normal <62 pg/ml), with no detectable circulating immunocomplexes.
The peak level of SCre was noted 12 days after fever onset, and the peak of IgG antibody titre of 1:1000 on day 16. The highest CK level was 5850 U/l and myoglobin was elevated to >10 000 ng/ml. In spite of vigorous treatment, the patient died on day 23 (Figure 1a).
Fig. 1.
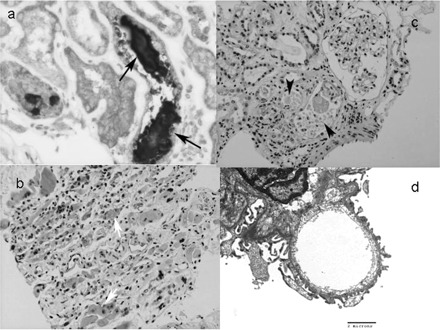
(a) The kidney from case 1. The renal tubule showed prominent cytoplasmic wasting pigment deposition with lymphocytes. The casts in the tubules (arrow) are positive for myoglobin (immunohistochemical stain, 200×). (b) The skeletal muscles from case 2. Myoid giant cells (white arrow) and interstitial ecstatic lymphovascular structures with inflammatory cell infiltration are evident (HE stain, 100×). (c) The kidney from case 2. There are several Mallory body-like casts (arrowhead) in dilated lumens with some sloughed and flattened renal tubular epithelial cells, indicating rhabdomyolysis and acute tubular necrosis. Interstitial infiltration of mononuclear cells is evident. There was a mild increase in mesangial cellularity and matrix (HE, 200×). (d) The glomerulus of case 2 (electron microscopy). Intact basement membrane surrounded by podocytes (×11 500). There was no immune complex deposition or virus particles.
Case 2
A 38-year-old woman was admitted to this hospital 7 days after the onset of diarrhoea, fever and chills. SARS-CoV from her NPA was identified using the results of RT–PCR. On admission, SCre was 0.8 mg/dl and CK was 21 U/l. SCre increased to 4.0 mg/dl on day 16 before the elevation of serum myoglobin (167 ng/ml) and CK (12834 U/l). Serum IL-6 increased from day 8 to day 16 (3.3 to 9.5 pg/ml), and there were also no detectable circulating IC1b immunocomplexes.
In spite of the marked elevation of CK on the 4 days following admission (up to 340 000 U/l), her SCre levels did not change significantly. Her lung function deteriorated gradually, and she died on day 30 of hospitalization (Figures 1b–d).
Discussion
SARS patients with rhabdomyolysis have a high incidence of bacterial infection, ARF and death [3]. Although direct muscle invasion by the virus is one of the possibilities suggested for virus-related rhabdomyolysis, the absence of viral particles in the muscles of our two patients does not support this mechanism.
ARF in these two patients cannot be accounted for by rhabdomyolysis alone, because the increase in SCre preceded the elevation of CK. Moreover, the elevation of CK in case 1 did not augment his SCre further, and in case 2 the decline of CK was associated with elevation of SCre. Instead, the frank rhabdomyolysis in these patients occurred when elevation of the cytokines and the presence of antibodies to the virus were marked.
Cytokines such as IL-6 and IL-8 induced by viral infections have been implicated as playing a pivotal role in renal failure. They increased in SARS whereas lymphocyte counts decreased [4], as our expression of cytokine dysregulation [5]. The elevated cytokines, together with lymphokines, lead to the adhesion of inflammatory cells to endothelium and other injury sites [6]. Several studies showed that impaired endothelium-dependent vasodilation is a prominent feature in patients with moderate renal impairment [7], and plasma cytokine levels could be useful in predicting mortality rates in critically ill patients with ARF.
Taken together, these findings suggest that in SARS, kidney injury, as well as lung injury, is related to immunopathological damage as a result of an exuberant host response, rather than uncontrolled viral replication.
Acknowledgments
This study was supported by The Ta-Tung Kidney Foundation.
Conflicts of interest statement. None declared.
References
- 1.Tsai HB, Huang JW, Chen KY et al Acute renal failure and renal replacement therapy in SARS patients. Presented at the Annual Committee on American Society of Nephrology, San Diego, November 12–17, 2003. [abstract]
- 2.Lee N, Hui D, Wu A et al A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348: 1986–1994 [DOI] [PubMed] [Google Scholar]
- 3.Tsai HB, Huang JW, Wu VC et al. Serum creatine phosphokinase predict the clinical outcome in SARS patients. Presented at the 20th Annual Committee on Taiwan Society of Nephrology, Taipei, December 13–14, 2003. [abstract]
- 4.Hsueh PR, Chen PJ, Hsiao CH et al Patient data, early SARS epidemic, Taiwan. Emerg Infect Dis 2004; 10: 489–493 [DOI] [PubMed] [Google Scholar]
- 5.Nicholls JM, Poon LL, Lee KC et al Lung pathology of fatal severe acute respiratory syndrome. Lancet 2003; 361: 1773–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Damle NK, Doyle LV, Bender JR, Bradley EC. Interleukin 2-activated human lymphocytes exhibit enhanced adhesion to normal vascular endothelial cells and cause their lysis. J Immunol 1987; 138: 1779–1785 [PubMed] [Google Scholar]
- 7.Annuk M, Lind L, Linde T, Fellstrom B. Impaired endothelium-dependent vasodilatation in renal failure in humans. Nephrol Dial Transplant 2001; 16: 302–306 [DOI] [PubMed] [Google Scholar]


