Abstract
We found that the sensitivities of 3 rapid influenza antigen tests for pandemic influenza A/H1N1 virus were low to moderate: BD Directigen EZ Flu A+B test (Becton Dickinson), 46.7%; BinaxNOW Influenza A&B (Inverness Medical), 38.3%; and QuickVue Influenza A+B Test (Quidel), 53.3%. A patient with influenza-like illness who has a negative rapid antigen test result should undergo further testing using reverse-transcription polymerase chain reaction.
On 17 April 2009, a novel triple-reassortant swine-origin influenza virus (pandemic A/H1N1) was identified by the Centers for Disease Control and Prevention (CDC) in 2 children living in adjacent counties in California [1]. By 12 June 2009, this virus had caused an estimated 29,669 cases of infection in 74 countries, including 145 deaths worldwide [2]. The World Health Organization raised the pandemic alert level to phase 6 on 11 June 2009.
Rapid diagnosis of influenza is important for initiation of antiviral therapy and implementation of infection control strategies. Reverse-transcriptase polymerase chain reaction (RT-PCR) is considered the reference test for diagnosis of influenza because of its high sensitivity and specificity as well as its rapid turnaround time. However, RT-PCR is expensive and requires trained expertise and batch testing, which delays reporting. Pandemic A/H1N1 RT-PCR is currently only available in designated reference or state laboratories, adding to the turnaround time. In addition, the large number of requests for RT-PCR testing has stretched resources, resulting in modified recommendations to test only severely ill persons or patients at risk of having serious complications [3].
Because other respiratory viruses frequently cocirculate with influenza viruses and can cause similar symptoms, diagnosing influenza on the basis of clinical presentation alone is difficult, with reported sensitivity ranging from 38% [4] to 79% [5]. Rapid influenza antigen tests (point-of-care tests) might prove useful, because they have a fast turnaround time (10–15 min) and require minimal training to perform. However, there are few data on the diagnostic accuracy of rapid influenza antigen tests for pandemic influenza A/H1N1 virus [6]. Soon after the onset of the pandemic influenza A/H1N1 outbreak, we received reports of poor performance of rapid influenza antigen tests. We report our findings of the clinical accuracy of 3 commonly used rapid influenza tests for diagnosis of pandemic A/H1N1 influenza.
Methods. During the period from 1 May 2009 through 2 June 2009, a convenience sample of 84 positive, nonduplicate nasopharyngeal specimens were tested using 3 different rapid antigen test kits: BD Directigen EZ Flu A+B test (Becton Dickinson), BinaxNOW Influenza A&B (Inverness Medical), and QuickVue Influenza A+B Test (Quidel). Testing was performed in accordance with the manufacturer's instructions, and each test result was interpreted by at least 2 of the study authors.
Nasopharyngeal specimens were collected from patients presenting with influenza-like illness using a sterile polyester nasopharyngeal swab and were transported to the microbiology laboratory in M4RT viral transport medium (Remel). Only specimens that were positive for respiratory viruses using the Luminex xTAG RVP (Luminex) were included. The Luminex xTAG RVP is a multiplex RT-PCR assay that allows for the simultaneous detection of 17 respiratory virus types/subtypes, including metapneumovirus, coronaviruses, influenza A virus subtypes H1 and H3, influenza B virus, parainfluenza virus types 1–4, respiratory syncytial virus, adenovirus, and rhinovirus. All specimens were refrigerated, and rapid antigen tests were performed ⩽48 h after specimen receipt. Specimens included 60 nasopharyngeal samples positive for pandemic influenza A/H1N1 virus, with results confirmed using the CDC's RT-PCR assay for pandemic influenza A/H1N1 virus. Control specimens included 24 nasopharyngeal specimens positive for other respiratory viruses, as follows: adenovirus (n=1), coronavirus (n=3), concurrent coronavirus and rhinovirus (n=1), metapneumovirus (n=4), rhinovirus (n=4), concurrent rhinovirus and parainfluenza virus (n=1), parainfluenza virus (n=7), and respiratory syncytial virus (n=3).
We calculated the sensitivity and specificity for each rapid antigen test. We determined the prevalence of pandemic A/H1N1 influenza over the study period; this was used to calculate the positive predictive value (PPV) and negative predictive value (NPV). Patient charts were reviewed, if available, for potential factors that may have been associated with rapid antigen test result; these included patient age, duration of symptoms before presentation, inpatient or emergency department versus outpatient status, and the median number of RT-PCR fluorescence intensity (MFI) units.
Data analysis was performed using SPSS, version 16.0 (SPSS). The Mann-Whitney U test was used for comparison of continuous variables, and χ2and McNemar tests were used for categorical independent and paired variables, respectively. P values <.05 were considered to be statistically significant. This study was approved by the institutional review board of Rush University Medical Center (Chicago, IL).
Results. The majority of patients with pandemic A/H1N1 influenza were children and young adults; the median age was 12.5 years (range, 7 months to 58 years). A total of 34 patients (57%) were assessed in the emergency department, and 26 patients (43%) were seen in physicians' offices. Twenty-two (65%) of 34 patients evaluated in the emergency department were subsequently hospitalized. Information for the duration of illness before presentation was available for 38 of 60 patients. The majority of patients (76%) presented ⩽3 days after developing symptoms influenza-like illness (mean interval, 2.8 days; range, 1–9 days). Control patients had a median age of 7 years (range, 4 months to 66 years); 14 control patients (58%) presented to the emergency department, and 10 (42%) were outpatients.
The analytic performance of the 3 rapid antigen tests, compared with that of the Luminex xTAG RVP are presented in Table 1. The overall respective sensitivity and specificity of the BD Directigen EZ Flu A+B test were 46.7% (28 of 60 specimens) and 100%; for the BinaxNOW Influenza A&B test, 38.3% (23 of 60 specimens) and 100%; and for the QuickVue Influenza A+B Test, 53.3% (32 of 60 specimens) and 100%. The QuickVue Influenza A+B Test was significantly more sensitive than the BinaxNOW Influenza A&B test (P<.01), but there was no significant difference between the other rapid antigen tests. During the study period, the overall prevalence of pandemic A/H1N1 virus was 17.9% (95% confidence interval, 8.24%-27.6%) among all specimens submitted for respiratory virus RT-PCR testing. On the basis of this prevalence, the calculated PPVs were 100% for all 3 tests, and the calculated NPVs were 89.6%, 88.2%, and 90.8% for BD Directigen EZ Flu A+B test, BinaxNOW Influenza A&B, and QuickVue Influenza A+B Test, respectively. Patient age and duration of symptoms prior to collection of the respiratory specimen did not correlate significantly with the results of rapid antigen tests (P>.05). A higher MFI unit with RT-PCR (which correlates with higher viral load) was significantly associated with positive results for all rapid antigen tests (P<.01) (Table 2).
Table 1.
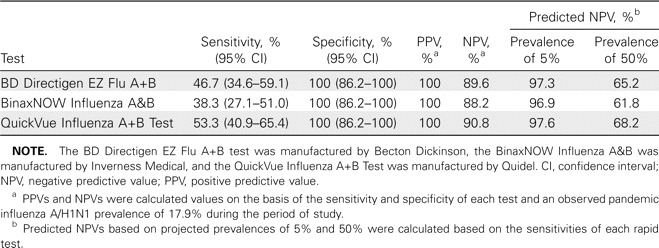
Analytic Performance of Rapid Influenza Antigen Tests, Compared with the Luminex xTAG RVP (Luminex) Reverse-Transcriptase Polymerase Chain Reaction
Table 2.
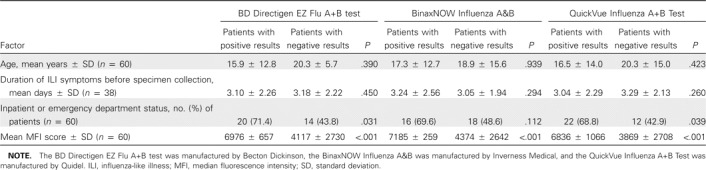
Summary of Variables Analyzed for Prediction of Rapid Antigen Test Results
Discussion. Rapid antigen tests are commonly used in many hospital laboratories, emergency departments, and doctors' offices. Most influenza rapid antigen tests are lateral flow chromatographic immunoassays in which patient samples are applied to a chromatographic strip that contains monoclonal antibodies against influenza A and B viruses. On-site diagnosis of influenza by point-of-care tests has been shown to limit antibiotic prescriptions, use of blood cultures, and chest radiography and ultimately to reduce patient costs [7]. However, rapid antigen tests have demonstrated a wide range of sensitivities for detection of seasonal influenza viruses, ranging from 69%-96% for the BD Directigen EZ Flu A+B test [8, 9], 64.9%-73% for the BinaxNOW Influenza A&B test [8, 10], and 19.7%-85% for the QuickVue Influenza A+B Test [11, 12].
We found that the 3 rapid antigen tests had low to modest sensitivities for diagnosis of pandemic influenza A/H1N1, although all tests demonstrated excellent specificity, with no cross-reactivity against other cocirculating respiratory viruses. Possible reasons for the low sensitivities in our study include the fact that the sample collection technique was not standardized and that specimens were refrigerated and only tested after completion of RT-PCR, which may have led to antigen degradation. However, we think that this is unlikely, because our findings are consistent with those of a similar study by Ginocchio et al [6] in which rapid antigen tests had a sensitivity of only 17.8% for pandemic influenza A/H1N1 virus, compared with the Luminex xTAG RVP. An alternative explanation may be related to differences in test sensitivity for detection of pandemic influenza A/H1N1 virus, compared with seasonal influenza viruses. In a study that used titered pandemic influenza A/H1N1 virus grown in cell cultures, rapid antigen tests required 1–1.5-log higher viral loads than did human seasonal virus for a positive result [13].
Other limitations of our study include the fact that we employed a known convenience sample of positive specimens. Because of the widespread interest regarding the clinical performance of rapid antigen tests for detection of pandemic influenza A/H1N1 virus, we used a convenience sample of positive specimens to allow for a quick yet relatively accurate assessment of these tests. In addition, all specimens were decoded, and both investigators performing the tests were blinded to the RT-PCR results. Finally, because the design of our study did not permit an accurate determination of the NPV and PPV, we calculated these values on the basis of the prevalence of novel influenza H1N1 during the study period. These values would clearly vary according to the prevalence of disease, and the PPV would be highest during the peak of an outbreak, with increased numbers of false-positive results when disease prevalence is low (Table 1).
Despite modest sensitivities, rapid influenza antigen testing could prove to be useful because of the tests' speed, portability, and ease of performance. Clinicians should be aware that patients presenting with an influenza-like illness and a negative rapid antigen test result should undergo further laboratory testing. However, a positive rapid antigen test result would allow presumptive diagnosis of novel influenza H1N1 virus infection and should lead to timely institution of infection control measures, treatment, and prophylaxis. Finally, as we approach the 2009–2010 winter season, it is desirable for manufacturers to develop sensitive rapid antigen kits that can also differentiate seasonal influenza A viruses from pandemic influenza A/H1N1 virus in view of their different antiviral susceptibilities.
Acknowledgments
Potential conflicts of interest. K.S. is on the speaker panel for Wyeth. S.V. and J.S.: no conflicts.
References
- 1.Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Influenza A(H1N1)—update 46. Available at http://www.who.int/csr/don/2009_06_12/en/index.html. Accessed 12 June 2009. [Google Scholar]
- 3.Chicago Department of Public Health. Health alert, swine influenza update 19. 8 June. 2009. Available at https://www.chicagohan.org. Accessed 9 June 2009. [Google Scholar]
- 4.Peltola V, Reunanen T, Ziegler T, Silvennoinen H, Heikkinen T. Accuracy of clinical diagnosis of influenza in outpatient children. Clin Infect Dis. 2005;41:1198–200. doi: 10.1086/444508. [DOI] [PubMed] [Google Scholar]
- 5.Monto AS, Gravenstein S, Elliott M, Colopy M, Schweinle J. Clinical signs and symptoms predicting influenza infection. Arch Intern Med. 2000;160:3243–7. doi: 10.1001/archinte.160.21.3243. [DOI] [PubMed] [Google Scholar]
- 6.Ginocchio CC, Zhang F, Manji R, et al. Evaluation of multiple test methods for the detection of the novel 2009 influenza A (H1N1) during the New York City outbreak. J Clin Virol. 2009;45:191–5. doi: 10.1016/j.jcv.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonner AB, Monroe KW, Talley LI, Klasner AE, Kimberlin DW. Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department: results of a randomized prospective controlled trial. Pediatrics. 2003;112:363–7. doi: 10.1542/peds.112.2.363. [DOI] [PubMed] [Google Scholar]
- 8.Hurt AC, Alexander R, Hibbert J, Deed N, Barr IG. Performance of six influenza rapid tests in detecting human influenza in clinical specimens. J Clin Virol. 2007;39:132–5. doi: 10.1016/j.jcv.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Chan KH, Maldeis N, Pope W, et al. Evaluation of the Directigen FluA+B test for rapid diagnosis of influenza virus type A and B infections. J Clin Microbiol. 2002;40:1675–80. doi: 10.1128/JCM.40.5.1675-1680.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fader RC. Comparison of the Binax NOW Flu A enzyme im mu no chro mato graph ic assay and R-Mix shell vial culture for the 2003–2004 influenza season. J Clin Microbiol. 2005;43:6133–5. doi: 10.1128/JCM.43.12.6133-6135.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agoritsas K, Mack K, Bonsu BK, Goodman D, Salamon D, Marcon MJ. Evaluation of the Quidel QuickVue test for detection of influenza A and B viruses in the pediatric emergency medicine setting by use of three specimen collection methods. J Clin Microbiol. 2006;44:2638–41. doi: 10.1128/JCM.02644-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uyeki TM, Prasad R, Vukotich C, et al. Low sensitivity of rapid diagnostic test for influenza. Clin Infect Dis. 2009;48:e89–92. doi: 10.1086/597828. [DOI] [PubMed] [Google Scholar]
- 13.Hurt AC, Baas C, Deng YM, Roberts S, Kelso A, Barr IG. Performance of influenza rapid point-of-care tests in the detection of swine lineage A (H1N1) influenza viruses. Influenza Other Respi Viruses. 2009;3:171–6. doi: 10.1111/j.1750-2659.2009.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


