Abstract
The reemergence of avian influenza (H5N1 infection) has heightened concern for a potential human influenza pandemic. Recommendations regarding preparation for a global avian influenza pandemic are available, and it is imperative that health care workers participate in preparedness planning and training. In developing countries, health care worker preparedness training should address the modes of avian influenza transmission and specify how to implement appropriate infection-control strategies to prevent and control the spread of avian influenza. We provide evidence for avian influenza transmission methods and identify prevention strategies relevant to infection control for hospitals in developing countries. Pandemic influenza preparedness plans must include health care administrative support, mechanisms to rapidly create temporary isolation facilities, systems to restrict access to exposed health care workers, and plans to involve specialists to screen and identify cases early, to provide for continuous monitoring to ensure adherence to optimal infection-control practices, and to provide regular feedback to health care workers
It is estimated that the next influenza pandemic will infect ∼20% of the world population. One in every 100 individuals with influenza is expected to be hospitalized, and 7 million people will potentially die within a few months [1,2–3]. The ongoing avian influenza (H5N1 infection) epidemic poses significant risks to both humans and animals [4,5,6–7]. The potential exists for cross-species transmission to humans and subsequent reassortment of avian and human influenza viruses in coinfected individuals [8]. Pandemic influenza planning and worldwide surveillance are key factors in mounting an effective global preparedness strategy for avian influenza [9]. Although recommendations for hospital infection control for avian influenza are available [10], adopting these recommendations has been an issue in developing countries. Because infection-control resources, including infrastructure and personal protective equipment (PPE), may vary considerably in different settings, hospital policy-makers in developing countries need to make decisions regarding the use of infection-control resources on the basis of disease prevalence, local priorities, personnel availability, and financial constraints. It is, therefore, important for health care workers (HCWs), who in many cases serve as first responders (i.e., may triage and evaluate an index case), to understand the dynamics of avian influenza transmission and to recognize the appropriate infection-control strategies recommended for the prevention and control of avian influenza.
?Evidence of Avian Influenza Transmission
Current evidence suggests that H5N1 viral infection occurs via bird-to-human transmission, possibly via environment-to-human transmission, and via limited, nonsustained human-to-human transmission [11]. To date, animal-to-human transmission is thought to be the predominant mode of avian influenza acquisition in humans [12, 13]. Risk factors include plucking and preparing ill birds, handling cocks for fighting events and tourism, playing with poultry, consumption of duck blood or undercooked poultry, and exposure to live poultry within 1 week prior to the onset of illness [11, 12]. Interestingly, interspecies transmission of avian influenza viruses has occurred in experimental settings from chickens to tigers, chickens to leopards, and chickens to domestic cats [14,15–16]. Human-to-human transmission of avian influenza has occurred via intimate contact without the use of barrier precautions but has not occurred from casual, social contact [17]. Serological studies of avian influenza among exposed HCWs, household contacts, and poultry cullers suggest that human-to-human transmission to date has been inefficient and that antibodies may develop in asymptomatic, exposed persons [13, 17,18,19,20–21]. Albeit rare, probable human-to-human transmission of H5N1 virus has been reported in several household clusters [8, 22].
Although it is unclear what role aerosols play in the natural transmission of avian influenza, it is important to keep in mind that the main goal of infection control is to minimize the risk of transmission of avian influenza within health care facilities. The recommendation to routinely use N95 respirators during an influenza pandemic is complicated by several factors. First, N95 respirators require fit testing. Once tested, any individual must use only the brand and size of respirator for which they have been certified. During a pandemic, it is likely that supplies of respirators may be limited, and supply chains may become disrupted. Therefore, it will be difficult to provide the appropriate size of respirator for each HCW. Also, the large number of N95 respirators marketed will make the stockpiling of appropriate numbers and sizes of respirators logistically difficult. The reproducibility of fit testing over time has been questioned [23], and prolonged use of N95 respirators has been shown to cause headaches [24] and facial discomfort [25] and may result in hypoxemia [26]. Poor compliance or incorrect use of an N95 respirator may negate any potential benefit that might be gained from their use. Therefore, pandemic influenza plans in developing countries might have to take these realities into consideration and use a more risk-based stratification approach to address droplet and contact precautions versus airborne and contact precautions.
Hospital Infection Control
The infection-control components of an avian influenza preparedness plan include: (1) basic infection-control measures, including hand hygiene; (2) use of PPE; (3) vaccination with seasonal influenza vaccines; (4) administration of prophylactic antiviral drugs; (5) surveillance and monitoring for HCW exposures; (6) evaluation of ill HCWs; (7) precautions for household and close contacts; and (8) limited visitation, if not quarantine, of ill patients. The rationale for most pandemic influenza preparedness plans are based on several assumptions: (1) it is unlikely that appropriate vaccines will be readily available in adequate supplies; (2) populations at high risk for complications may increase tremendously, given the high attack rate and mortality among adults aged 15–35 years seen in the 1918 pandemic [27]; and (3) containing illness among HCWs during an influenza pandemic will be challenging even if there is excellent compliance with infection-control practices.
In general, influenza attack rates during outbreaks among unvaccinated HCWs are reported to be as high as 59% [28]. Influenza attack rates often remain >10% among unvaccinated HCWs, even when there are excellent infection-control measures and behavioral compliance [29]. Viral shedding of influenza in adults can extend for 7 days after symptom onset and for weeks in infants and immunocompromised individuals. This makes environmental control of influenza even more difficult in health care facilities. Thus, the initial specific protection of HCWs will need to include available antiviral agents (e.g., oseltamivir and zanamivir) for chemoprophylaxis and treatment. A recently proposed university hospital—based preparedness plan has recommended the stockpiling of oseltamivir [29]. There are 4 potential strategies for using antiviral agents during an influenza outbreak [30, 31]: chemoprophylaxis for the entire influenza outbreak and season, postexposure chemoprophylaxis, treatment of ill patients, and a combination of chemoprophylaxis and treatment. Several studies support the use of prophylactic viral agents [31,32,33,34–35]. Furthermore, a model of the 1957–1958 Asian influenza pandemic predicted that 8 weeks of antiviral prophylaxis for close contacts of index case patients would have reduced the attack rate from 33% to 2% [36]. Thus, targeted prophylaxis for HCWs and patients would likely mean administering 6–8 weeks of prophylaxis to all vulnerable groups. Although attractive, this strategy is prohibitively expensive for most hospitals and other health care facilities in both developed and developing countries. Furthermore, widespread, long-term use of antiviral prophylaxis could promote antiviral resistance. An alternative strategy that focuses on the treatment of ill HCWs, with some targeted prophylaxis of heavily exposed HCWs, would be more financially feasible. This strategy would provide for treatment of those HCWs directly caring for patients with influenza during a pandemic. Recent studies have reported that neuraminidase inhibitors administered within 48 h of symptom onset decrease the duration of illness and viral shedding, the incidence of hospitalization, antibiotic use, and mortality [35, 37, 38]. Health care workers should be tracked and monitored for influenza-like illness (e.g., myalgia and fever). It is likely that such monitoring would identify most of the ill HCWs and, thus, allow timely administration of antiviral therapy. Despite these recommendations, health care facilities in developing countries may find it difficult to implement antiviral therapy because of the associated high cost.
Infection Control for Health care Facilities in Developing Countries
For preparedness planning in health care facilities in developing countries, some practical issues that are relevant to the adoption and modification of the above recommendations should be considered [39].
Health care administrative support. The level of occupational protection of HCWs in developing countries has not met the minimal standards of the US Occupational Health and Safety Administration. Despite the logistical and economic challenges, efforts to promote implementation of effective infection control and occupational health strategies are overdue, and a global need for such strategies is now recognized. Given the experience of severe acute respiratory syndrome (SARS) outbreaks, which occurred in both designated "SARS hospitals" and "non-SARS hospitals" [40,41–42], global preparedness plans should facilitate administrative, fiscal, and infrastructure support for routine occupational health and safety programs for HCWs, appropriate infection-control expertise, and infrastructure in health care settings, available PPE for HCWs, and epidemiological resources for the prevention and control of emerging infectious diseases. These expenditures should not be viewed as an increase in the cost of health care but as preventive health and safety measures that insure protection of HCWs and, ideally, provide an anticipated return on investment to the health care institution.
Development of practical surveillance strategies. Surveillance strategies should be developed in accordance with the current level of the influenza pandemic and the existing local infrastructure. Such strategies should be continuously monitored and modified. During the SARS outbreak in Hong Kong, there were very few private rooms in which to isolate patients. Some hospitals controlled the outbreak by having designated SARS teams and geographically separate wards for patient triage, patients with confirmed SARS cases, and patients without SARS [43]. During an avian influenza outbreak, some hospitals in Thailand performed surveillance for avian influenza among all patients who were admitted to the intensive care unit with severe community-acquired pneumonia [44, 45]. The estimated annual cost for avian influenza screening in a Thai hospital was $7375 [44]. These studies reported a low detection rate for avian influenza (3 cases among 5496 patients). Therefore, cost-effectiveness studies of screening programs, based on the level of local avian influenza activity, are warranted before this strategy can be adopted in areas where H5N1 infection is endemic.
Involvement of specialists. As in developed countries, health care providers with the least experience are often the first to evaluate patients with unrecognized emerging infectious diseases in developing countries [46, 47]. This may lead to delayed recognition of disease and missed opportunities to interrupt disease transmission [46, 47]. Several reports from developing countries emphasize the added value of specialists (e.g., infectious diseases, pulmonary, and emergency medicine specialists) in screening for suspected cases of emerging infectious diseases and early recognition of atypical cases in acute and ambulatory care settings [7, 21, 41, 48]. Given the difficulty of rapidly diagnosing avian influenza [49, 50], early involvement of specialists could promote the obtaining of adequate, lower respiratory tract specimens from an index patient before that patient receives antiviral medication. Although the value of infection control and health care epidemiology expertise has been formally recognized in North America and Europe [51–52], this is not the case in most acute-care facilities in developing countries.
Creation of a temporary isolation ward during an epidemic. Rapid creation of a temporary isolation ward using existing functional hospital units is readily applicable to clinical settings in developing countries. Such units should be divided into a clean zone, for changing into and out of street clothes and for recording the HCW's name and entry and exit times; an intermediate zone, for donning PPE that has been modified according to resource availability (e.g., scrubs and double-gloving); and a contaminated zone, for entering isolation areas [53]. Exhaust fans could be installed above windows in each room if isolation rooms with negative pressure ventilation are unavailable. At least 1 m of distance should be placed between patients to reduce the risk of cross-transmission through respiratory droplets. Although creation of a temporary isolation ward seems to be attractive during an epidemic, it is important to realize that the ward designated for temporary isolation should have separate entrance and exit pathways for HCWs and patients, and a one-way entrance and one-way exit should be designated for patients, to minimize problems involving cross-contamination (figure 1).
Figure 1.
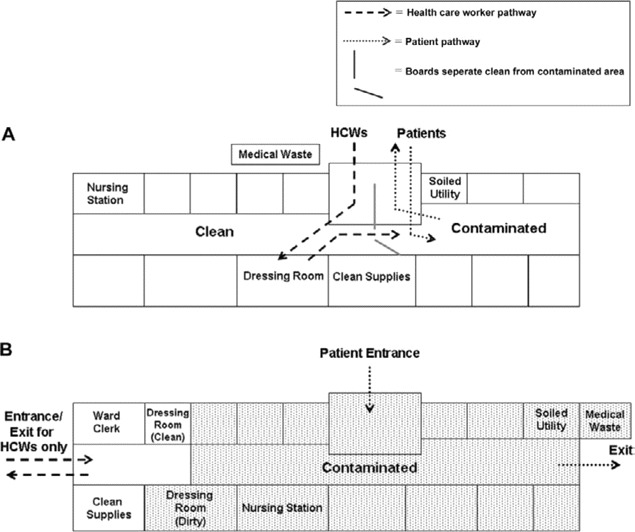
Potential cross-contamination of the isolation unit (A). This issue could be minimized by using separate entrance and exit pathways for health care workers (HCWs) and patients and by creating a one-way entrance and one-way exit for patients (B). Dressing room (clean), room where HCWs put on personal protective equipment; dressing room (dirty), room where HCWs remove contaminated personal protective equipment after leaving the contaminated zone.
Improvement of existing infection-control practices. As is the case with any set of practices, infection-control practices may be difficult to orchestrate without effective communication that clearly outlines the objectives for these practices. This point was emphasized in recent reports of increased rates of methicillin-resistant Staphylococcus aureus acquisition in Hong Kong and Singapore during the SARS outbreak [54, 55]. These studies suggested that rates of methicillin-resistant S. aureus transmission increased when HCWs adopted the nonstandard practice of wearing gloves and gowns all of the time. Several infection-control practices, such as proper hand hygiene and the correct use of PPE, may need to be highly monitored, with feedback provided to HCWs in a timely manner, to optimize appropriate infection-control practices and to reduce the risk of disease transmission.
Conclusions
Avian influenza is a likely candidate for the next influenza pandemic. Given the global experience from the SARS epidemics, it is reasonable to suspect that health care facilities may serve as the nidus for large-scale community outbreaks. Health care facilities in developing countries will benefit from adopting or modifying their strategic pandemic influenza plan and identifying local expertise to optimize control of outbreaks at their earliest stages.
Acknowledgments
Financial support. National Center and Genetic Engineering and Biotechnology, National Science and Technology Development Agency (BT-B-01-MG-13-5019) and Thai Research Fund (to A.A.).
Potential conflicts of interest. D.K.W. is a consultant for and has received research support from 3M Healthcare and is a consultant for Enturia. A.A. and V.J.F.: no conflicts.
References
- 1.Kilbourne ED. Inluneza pandemics of the 20th century. Emerg Infect Dis. 2006;12:9–14. doi: 10.3201/eid1201.051254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meltzer MI, Cox NJ, Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis. 1999;5:659–71. doi: 10.3201/eid0505.990507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meltzer MI. Presentation at the WHO consultation on priority public health interventions before and during the influenza pandemic. Geneva: 2004. Available at: http://www.who.int/csr/disease/avian_influenza/consultation/en/. Accessed 4 July 2007. [PubMed] [Google Scholar]
- 4.Abbott A, Pearson H. Fear of human pandemic grows as bird flu sweeps through Asia. Nature. 2004;427:472–3. doi: 10.1038/427472a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chotpitayasunondh T, Ungchusak K, Hanshaoworakul W, et al. Human disease from influenza A (H5N1), Thailand, 2004. Emerg Infect Dis. 2005;11:201–9. doi: 10.3201/eid1102.041061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tran TH, Nguyen TL, Nguyen TD, et al. Avian influenza A (H5N1) in 10 patients in Vietnam. N Engl J Med. 2004;350:1179–88. doi: 10.1056/NEJMoa040419. [DOI] [PubMed] [Google Scholar]
- 7.Apisarnthanarak A, Kitphati R, Thongphubeth K, et al. Atypical avian influenza (H5N1) Emerg Infect Dis. 2004;10:1321–4. doi: 10.3201/eid1007.040415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ungchusak K, Auewarakul P, Dowell SF, et al. Probable person-to-person transmission of avian influenza A (H5N1) N Engl J Med. 2005;352:333–40. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 9.Cox NJ, Tamblyn SE, Tam T. Influenza pandemic planning. Vaccine. 2003;21:1801–3. doi: 10.1016/s0264-410x(03)00076-8. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. WHO global influenza preparedness plan. Available at: http://www.who.int.libproxy.lib.unc.edu/csr/resources/publications/influenza/GIP_2005_5Eweb.pdf. Accessed 2 May 2007. [Google Scholar]
- 11.Beigel JH, Farrar J, Han AM, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–85. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 12.Mounts AW, Kwong H, Izurieta HS, et al. Case-control study of risk factors for avian influenza A (H5N1) disease, Hong Kong, 1997. J Infect Dis. 1999;180:505–8. doi: 10.1086/314903. [DOI] [PubMed] [Google Scholar]
- 13.Bridges CB, Lim W, Hu-Primmer J, et al. Risk of influenza A (H5N1) infection among poultry workers, Hong Kong, 1997–1998. J Infect Dis. 2002;185:1005–10. doi: 10.1086/340044. [DOI] [PubMed] [Google Scholar]
- 14.Keawcharoen J, Oraveerakul K, Kuiken T, et al. Avian influenza H5N1 in tigers and leopards. Emerg Infect Dis. 2004;10:2189–91. doi: 10.3201/eid1012.040759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thanawongnuwech R, Amonsin A, Tantilertcharoen R, et al. Probable tiger-to-tiger transmission of avian influenza H5N1. Emerg Infect Dis. 2005;11:699–701. doi: 10.3201/eid1105.050007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuiken T, Rimmelzwaan G, van Riel D, et al. Avian H5N1 influenza in cats. Science. 2004;306:241–0000. doi: 10.1126/science.1102287. [DOI] [PubMed] [Google Scholar]
- 17.Katz JM, Lim W, Bridges CB, et al. Antibody response in individuals infected with avian influenza A (H5N1) viruses and detection of anti-H5 antibody among household and social contacts. J Infect Dis. 1999;180:1763–80. doi: 10.1086/315137. [DOI] [PubMed] [Google Scholar]
- 18.Buxton Bridges C, Katz JM, Seto WH, et al. Risk of influenza A (H5N1) infection among health care workers exposed to patients with influenza A (H5N1), Hong Kong. J Infect Dis. 2000;181:344–8. doi: 10.1086/315213. [DOI] [PubMed] [Google Scholar]
- 19.Liem NT, Lim W. World Health Organization International Avian Influenza Investigation Team, Vietnam. Lack of H5N1 avian influenza transmission to hospital employees, Hanoi, 2004. Emerg Infect Dis. 2005;11:210–5. doi: 10.3201/eid1102.041075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schultsz C, Dong VC, Chau NV, et al. Avian influenza H5N1 and healthcare workers. Emerg Infect Dis. 2005;11:1158–9. doi: 10.3201/eid1107.050070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Apisarnthanarak A, Erb S, Stephenson I, et al. Seroprevalence of anti-H5 antibody among Thai health care workers after exposure to Avian influenza (H5N1) in a tertiary care center. Clin Infect Dis. 2005;40:e16–8. doi: 10.1086/427034. [DOI] [PubMed] [Google Scholar]
- 22.Kandun IN, Wibisono H, Sedyaningsih ER, et al. Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med. 2006;355:2186–94. doi: 10.1056/NEJMoa060930. [DOI] [PubMed] [Google Scholar]
- 23.Coffey CC, Lawrence RB, Campbell DL, Zhuang Z, Calvert CA, Jensen PA. Fitting characteristics of eighteen N95 filtering-facepiece respirators. J Occup Environ Hyg. 2004;1:262–71. doi: 10.1080/15459620490433799. [DOI] [PubMed] [Google Scholar]
- 24.Lim C, Seet RC, Lee KH, Wilder-Smith EP, Chuah BY, Ong BK. Headaches and the N95 face-mask amongst healthcare workers. Acta Neurol Scand. 2006;113:199–202. doi: 10.1111/j.1600-0404.2005.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Tokura H, Guo YP, et al. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Arch Occup Environ Health. 2005;78:501–9. doi: 10.1007/s00420-004-0584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kao TW, Huang KC, Huang YL, Tsai TJ, Hsieh BS, Wu MS. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004;103:624–8. [PubMed] [Google Scholar]
- 27.Tuabenberger JK, Reid AH, Fanning TG. Capturing a killer flu virus. Sci Am. 2005;292:48–57. [PubMed] [Google Scholar]
- 28.Salgado CD, Farr BM, Hall KK, Hayden FG. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–55. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 29.Cinti S, Chenoweth C, Monto AS. Preparing for pandemic influenza: should hospitals stockpile oseltamivir? Infect Control Hosp Epidemiol. 2005;26:852–4. doi: 10.1086/502507. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization (WHO) Geneva. Switzerland: WHO; 2004. WHO guidelines on the use of vaccines and antivirals during influenza pandemics: global health security—epidemic alert and response; pp. 1–11. [Google Scholar]
- 31.Ward P, Small I, Smith J, Suter P, Dutkowski R. Oseltamivir (Tamiflu) and its potential for use in the event of an influenza pandemic. J Antimicrob Chemother. 2005;55(Suppl 1):i5–21. doi: 10.1093/jac/dki018. [DOI] [PubMed] [Google Scholar]
- 32.Brady MT, Sears SD, Pacini DL, et al. Safety and prophylactic efficacy of low-dose rimantadine in adults during an influenza A epidemic. Antimicrob Agents Chemother. 1990;34:1633–6. doi: 10.1128/aac.34.9.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shilling M, Povinelli L, Krause P. Efficacy of zanamivir for chemoprophylaxis of nursing home influenza outbreaks. Vaccine. 1998;16:1771–4. doi: 10.1016/s0264-410x(98)00141-8. [DOI] [PubMed] [Google Scholar]
- 34.Hayden FG, Atmar RL, Schilling M, et al. Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza. N Engl J Med. 1999;341:1336–43. doi: 10.1056/NEJM199910283411802. [DOI] [PubMed] [Google Scholar]
- 35.Bowles SK, Lee W, Simor AE, et al. Use of oseltamivir during influenza outbreaks in Ontario nursing homes, 1999–2000. J Am Geriatr Soc. 2002;50:608–16. doi: 10.1046/j.1532-5415.2002.50153.x. [DOI] [PubMed] [Google Scholar]
- 36.Longini IM, Jr, Halloran ME, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159:623–33. doi: 10.1093/aje/kwh092. [DOI] [PubMed] [Google Scholar]
- 37.Kaiser L, Wat C, Mills T, Mahoney P, Ward P, Hayden F. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med. 2003;163:1667–72. doi: 10.1001/archinte.163.14.1667. [DOI] [PubMed] [Google Scholar]
- 38.Whitley RJ, Hayden FG, Reisinger KS, et al. Oral oseltamivir treatment of influenza in children. Pediatr Infect Dis J. 2001;20:127–33. doi: 10.1097/00006454-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Apisarnthanarak A, Mundy LM. Infection control for emerging infectious diseases in developing countries and resource-limited settings. Infect Control Hosp Epidemiol. 2006;27:885–7. doi: 10.1086/505924. [DOI] [PubMed] [Google Scholar]
- 40.Tambyah PA, Singh KS, Kabib AG. SARS: understanding the coronavirus: accuracy of WHO criteria was similar in a "non-SARS" hospital in Singapore. BMJ. 2003;327:620–0000. doi: 10.1136/bmj.327.7415.620-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ooi SB, Tambyah PA. Transmission of severe acute respiratory syndrome in an emergency department. Am J Med. 2004;116:486–9. doi: 10.1016/j.amjmed.2003.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1977–85. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 43.Ho PL, Tang XP, Seto WH. SARS: hospital infection control and admission strategies. Respirology. 2003;8(Suppl):41–5. doi: 10.1046/j.1440-1843.2003.00523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Apisarnthanarak A, Puthavathana P, Kitphati R, et al. Avian influenza H5N1 screening of intensive care unit patients with community-acquired pneumonia. Emerg Infect Dis. 2006;12:1766–9. doi: 10.3201/eid1211.060443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Olsen SJ, Ungchusak K, Birmingham M, Bresee J, Dowell SF, Chunsuttiwat S. Surveillance for avian influenza in human beings in Thailand. Lancet Infect Dis. 2006;6:757–8. doi: 10.1016/S1473-3099(06)70639-9. [DOI] [PubMed] [Google Scholar]
- 46.Centers for Disease Control Prevention. Severe acute respiratory syndrome-Singapore 2003. MMWR Morb Mortal Wkly Rep. 2003;52:405–11. [PubMed] [Google Scholar]
- 47.Ho KY, Singh KS, Habib AG, et al. Mild illness associated with severe acute respiratory syndrome coronavirus infection: lessons from a prospective seroepidemiologic study of health-care workers in a teaching hospital in Singapore. J Infect Dis. 2004;189:642–7. doi: 10.1086/381558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fisher DA, Lim TK, Lim YT, Singh KS, Tambyah PA. Atypical presentation of SARS. Lancet. 2003;361:1740–0000. doi: 10.1016/S0140-6736(03)13336-3. [DOI] [PubMed] [Google Scholar]
- 49.Oner AF, Bay A, Arslan S, et al. Avian influenza A (H5N1) infection in eastern Turkey in 2006. N Engl J Med. 2006;355:2179–85. doi: 10.1056/NEJMoa060601. [DOI] [PubMed] [Google Scholar]
- 50.Apisarnthanarak A, Kitphati R, Mundy LM. Difficulty in the rapid diagnosis of avian influenza A infection: Thailand experience. Clin Infect Dis. 2007;44:1252–3. doi: 10.1086/513584. [DOI] [PubMed] [Google Scholar]
- 51.Scheckler WE, Brimhall D, Buck AS, et al. Requirements for infrastructure and essential activities of infection control and epidemiology in hospitals: a consensus panel report. Society for Healthcare Epidemiology of America. Infect Control Hosp Epidemiol. 1998;19:194–24. doi: 10.1086/647779. [DOI] [PubMed] [Google Scholar]
- 52.Horan-Murphy E, Barnard B, Chenoweth C, et al. APIC/CHICA-Canada infection control and epidemiology: professional and practice standards. Association for Professionals in Infection Control and Epidemiology and the Community and Hospital Infection Control Association-Canada. Am J Infect Control. 1999;27:47–51. doi: 10.1016/s0196-6553(99)70073-8. [DOI] [PubMed] [Google Scholar]
- 53.Fung CP, Hsieh TL, Tan KH, et al. Rapid creation of a temporary isolation ward for patients with severe acute respiratory syndrome in Taiwan. Infect Control Hosp Epidemiol. 2004;25:1026–32. doi: 10.1086/502339. [DOI] [PubMed] [Google Scholar]
- 54.Yap FH, Gomersall CD, Fung KS, et al. Increase in methicillin-resistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin Infect Dis. 2004;39:511–6. doi: 10.1086/422641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chai LY, Ng TM, Habib AG, Singh K, Kumarasinghe G, Tambyah PA. Paradoxical increase in methicillin-resistant Staphylococcus aureus acquisition rates despite barrier precautions and increased hand washing compliance during an outbreak of severe acute respiratory syndrome. Clin Infect Dis. 2005;40:632–3. doi: 10.1086/427150. [DOI] [PMC free article] [PubMed] [Google Scholar]


