A significant decline in the number of applicants for infectious diseases fellowship positions has been noted in recent years. Most reduction is seen among international medical graduates. Reasons for the decline are speculated upon and possible solutions are offered.
Keywords: infectious diseases, fellowship, declining demand
Abstract
Recent match results from the National Resident Matching Program for the subspecialty of infectious diseases show an ongoing decline in the number of fellowship positions filled, and, more important, in the number of applicants, particularly from the pool of international medical graduates. The main reasons for this declining application rate are unclear; in the absence of hard data, we present our viewpoint on this issue. Difficulties in securing visas for permanent residency in the United States, perception of a limited job market, and the explosive growth in the number of hospitalist positions may be important contributing factors. Infectious Diseases Society of America members need to focus on medical students and medical residents in their formative years. We present potential solutions to this problem of declining interest in the field of infectious diseases.
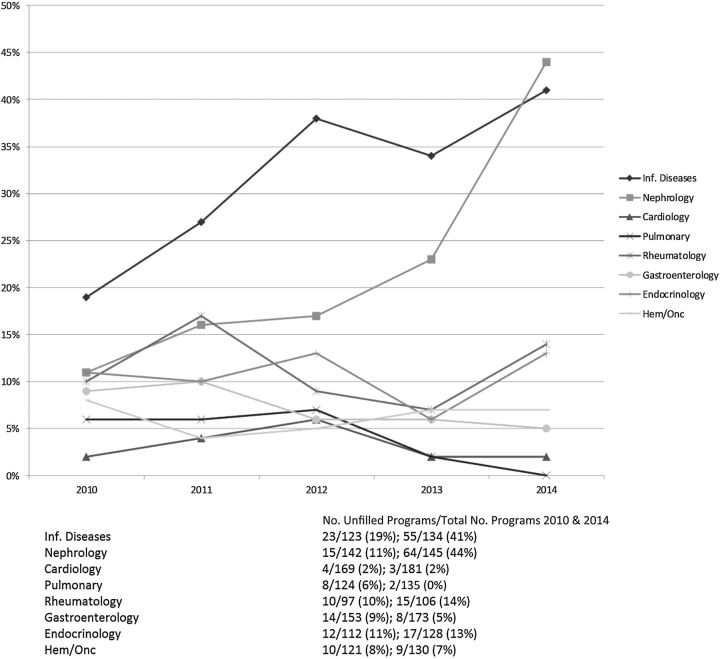
Recent match results from the National Resident Matching Program (NRMP) for the subspecialty of infectious diseases should raise concern for all infectious diseases subspecialists. For the adult infectious diseases fellowship training program cycle that began in July 2013, one-third of the accredited programs (45 of 134) failed to fill their positions; among the 334 positions offered, 64 (19%) were not filled (Figure 1). For the cycle starting in July 2014, 41% of infectious diseases fellowship programs did not fill all of their positions in the match, and of the 328 positions offered, 74 (23%) were not filled. These results are the result of the gradual decline in the number of medical residents applying to enter the subspecialty of infectious diseases and a small increase in the number of accredited programs and positions. Because of this, the ratio of the number of applicants to available infectious diseases fellowship positions declined to <1 for 2012 and 2013.
Figure 1.
Medical subspecialties: number of unfilled fellowship programs/total number of programs in 2010 and 2014.
Whereas the average number of US and Canadian medical graduates applying for infectious diseases fellowship positions has remained stable from 2009 through 2013 (14 applicants per program in 2009 vs 17 applicants per program in 2013), the number of international medical graduate applicants per program decreased markedly (51 applicants per program in 2009 to 33 in 2013). Thus, the reduction in the total number of applicants to infectious diseases training programs is almost entirely attributable to decreased applications from the cohort of international medical graduates.
In the February 2013 Infectious Diseases Society of America (IDSA) News, recent IDSA President David Relman called for prompt action, pointing out that infectious diseases was the only internal medicine subspecialty for which there were more fellowship positions available than the number of applicants [1]. Indeed, the current decline is most striking for the subspecialties of infectious diseases and nephrology, whereas the other subspecialities remain highly competitive. As nephrology and infectious diseases are both hospital-based and nonprocedural in nature, the factors underlying the decline may be somewhat similar. A recent American Society of Nephrology survey identified 3 reasons for the declining interest: perceived suboptimal lifestyle of a nephrologist; relatively inadequate compensation; and the perception that the specialty is too difficult to master (personal communication, Noreen Rossi, MD, Fellowship Program Director, Nephrology, Wayne State University).
The processes for applicants in all medical sub-specialties that are accredited through the American College of Graduate Medical Education (ACGME) involve two steps. The first step is through the Electronic Residency Application Service (ERAS) which is a program of the American Association of Medical Colleges [2]. Until 2012, the ERAS application and process including interviews for subspecialties of Internal Medicine occurred in the fall and winter, usually during the residents’ second training year. The match process is the second step. The match results, until recently, were announced by the NRMP in the spring for candidates starting fellowship the following year, ie. 13–14 months before the beginning of fellowship. In order to allow resident applicants more time to experience electives and improve their applications for subspecialty fellowships, the match was moved to 7 months prior to starting fellowship starting in December 2010.
The match was created in large part to help residents have equal access to positions and to obtain a position without undue pressure to decide during an interview if they wish to join a program. This system has worked well since 1994 and has only been an issue now that there are fewer applicants. The NRMP mandates that 75% of all programs with available positions in a given year register for the match and that 75% of available positions within the specialty be registered with the NRMP [3]. The pressure to fill openings has now caused some program directors to offer positions outside the match. This practice forces programs remaining in the match to draw from a smaller group of applicants; therefore, they have a higher chance of not filling. Programs that do not fill are often subject to administrative scrutiny for possible reduction in positions, creating significant pressure to fill the program. After an unsuccessful match, program directors and other faculty members spend extra time in recruitment during the “scramble.”
If the number of unfilled positions grows, there are potential implications on the interest level in pursuing a career in adult infectious diseases among high-quality internal medicine trainees. The ability to produce a workforce of the “best and brightest” infectious diseases physicians in the future is weakened as the overall numbers entering into the field decrease. In the 2013 match, only 5% of applicants to adult infectious diseases programs remained unmatched compared with 11%–48% for other internal medicine subspecialties. Ensuring an appropriate balance between the number of fellowship positions and suitable candidates is vital to maintaining excellence in our field. Why the declining interest, particularly among international medical graduates? Although there are no studies to evaluate this decline, we provide some explanations and possible solutions for reversal of this trend.
FACTORS CONTRIBUTING TO DECLINING INTEREST (“CHALLENGES”)
To better understand the training satisfaction and job prospects in infectious diseases, the IDSA Program Directors' Committee (TPDC) conducted a survey among 2009–2011 graduates of infectious diseases and presented the results on 19 October 2011 at the program directors' national meeting during the IDSA Annual Meeting held in Boston. There were 421 responses. Overall, 28% obtained positions that were not entirely related to the management of infectious diseases and 42% felt that their compensation was inadequate. Among 2011 graduates, 35% had positions that were not entirely related to infectious diseases, and job satisfaction was much less in that group.
The creation of a new physician specialty, the “hospitalist,” and the increasing difficulty to obtain permanent visas for non-US physicians have, in our opinion, significantly swayed international medical graduates away from the field of infectious diseases. The increasing number of hospitalists in US hospitals has created new opportunities for internal medicine graduates. In 2010, it was estimated that there were >30 000 hospitalists in the United States; many graduates are choosing this field, attracted by both the financial and lifestyle benefits afforded to those choosing this subspeciality [4]. From a recent survey of 40 000 new physicians conducted in September 2011, the median starting salary for hospitalists was $165 000 compared with $158 000 for infectious diseases physicians [5]. Hospitalists are not required to have additional years of subspecialty training and often are paid higher wages than a board-certified infectious diseases physician, work in shifts with extended periods of time off, and have no outpatient overhead or responsibilities. This is appealing to many young physicians who are frequently burdened with large debt and growing families, especially at a time of uncertainty over the effects of healthcare payment reform. The effect of the rapid growth of the hospitalist on candidates applying for the infectious diseases match has not been formally evaluated. However, there is a temporal association between the increase in this field and the reduction in the number of international graduates applying to adult infectious diseases programs. A recent survey of internal medicine resident graduates from 2009 to 2011 demonstrated that international graduates had a decreased interest in all subspecialty medicine and an increased interest in hospitalist medicine as a career plan from the first to the third postgraduate year [6].
An additional factor that may affect international medical residents' decision to pursue a career in infectious diseases is the US visa (J-1 or H-1) requirement when deciding postresidency career plans. In recent years, federal regulations have been tightened for non-US physicians to obtain the H-1 visa that leads to permanent residency in the United States. Fellowship training programs are increasingly reluctant to incur the costs associated with visa sponsorship, thus limiting residents' opportunities for fellowship positions. Trainees with H-1 visas have a 6-year window to complete their training and apply for permanent residency (green card) status; completing 5 years of training (3 years of residency and 2 years of fellowship) restricts the time available to apply for a green card. For internal medicine residents with a J-1 visa, because few J-1–sponsored jobs exist for subspecialists, most enter the field of general internal medicine. Moreover, the recent change in dates of the match (from June of second year of residency to December of third year) leaves unmatched candidates little time to secure a J-1–sponsored job. Hence, visa-related issues are likely a large factor in the decreasing number of fellowship applicants among international graduates. This trend has disproportionately affected the infectious diseases subspecialty—the percentage of decline, from 2010 to 2014, among the international students applying for an infectious diseases match was 38%, compared with an overall decline of only 3.7% to all internal medicine fellowships. The exact reasons for this disproportionate decrease are unclear.
In addition to issues such as reimbursement, lifestyle, and visa, there is also a concern of job availability for the graduating infectious diseases fellows. This issue was previously addressed in 2 editorials from another era [7, 8]. In a 1987 editorial, saturation of the job market was felt to be “imminent” and would likely “last much longer in the field of infectious diseases than in subspecialties that are older” [8]. Hence, the trainees may feel that job opportunities in infectious diseases are decreasing, particularly with improved control and relatively straightforward management of human immunodeficiency virus (HIV)/AIDS. In 2 more recent articles, the expanding roles of infectious diseases physicians were summarized [9, 10]. Infection control/hospital epidemiology, antibiotic stewardship, treatment of sepsis, and outpatient antibiotic therapy have been cited as additional areas of responsibilities that help avoid saturating the infectious diseases job market. Certainly, the expanding population of HIV-infected individuals due to the advances in anti-HIV therapy has contributed to the steady growth of infectious diseases jobs over the last 2 decades. Importantly, with the newer anti–hepatitis C drugs and the increase in the immunosuppressed population, the role of infectious diseases physicians in the prevention/management of infections will likely increase while we witness decreasing national trends in hospitalization rates and length of stay as well as decrease in reimbursement for consultants.
POSSIBLE SOLUTIONS (“OPPORTUNITIES”)
At the program directors’ national meeting held on 16 October 2012 in San Diego, California, the IDSA TPDC reported a survey of the fellowship program directors regarding why they felt residents chose to apply to infectious diseases programs. Among 83 respondents, program directors felt that availability of a mentor in the field of infectious diseases, exposure to ambulatory management of HIV, and clinical experience abroad were the strongest drivers for residents to seek fellowship training. IDSA is currently funding a formal study to better understand those factors that influence Internal Medicine residents' subspecialty career choices in general, and specifically for Infectious Diseases. The results may provide some insight into ways to enhance interest in the specialty among trainees.
Some possible solutions provided by the authors are summarized in Table 1. As the main target for potential fellowship applicants will increasingly be US graduates, the process of promoting our field needs to begin in preclinical years of medical school. This will be particularly important as the number of US medical school graduates is expected to grow. It is time to review, update, and expand the syllabi for infectious diseases in medical school curricula. Given the issue of the urgency of global antimicrobial resistance, the medical school deans may be convinced to give increased time for infectious diseases. Increasing knowledge and experience among medical students in areas of global health, HIV infection, antibiotic stewardship, and diagnostic microbiology would hopefully increase the pool of future applicants. Opportunities for students to spend time at medical schools in developing countries is likely to further their interest in the field of infectious diseases and global health. Mentorship for student research among medical school faculty through programs such as the Medical Scholars Program (sponsored by the IDSA) is critical.
Table 1.
Possible Solutions to Shortage of Applicants for Infectious Diseases Fellowship
1. Improve medical school curriculum (years 1 and 2)
|
2. Improve infectious diseases experience among internal medicine residents
|
3. State infectious diseases societies
|
4. IDSA involvement
|
Abbreviation: IDSA, Infectious Diseases Society of America.
Program directors of internal medicine need to be made aware of the declining interest in infectious diseases among residents, and their assistance needs to be sought to implement appropriate strategies. The infectious diseases faculty (practitioners) need to work toward a mandatory rotation in infectious diseases for all internal medicine residents. Infectious diseases faculty must become increasingly involved in personal and professional mentoring of all residents, in fostering research, and in the development of the internal medicine residency curriculum for infection control, antibiotic stewardship, and HIV continuity care. Patient safety and quality improvement are areas that provide rich opportunities for clinical research, and infectious diseases clinicians can play a major leadership role attracting residents to participate in research in such areas. The infectious diseases faculty need to identify potential candidates during the formative period of residency and nurture such individuals. Exposing junior residents to ambulatory infectious diseases and HIV clinics may serve well in many institutions. The decreased presence of infectious diseases faculty within many internal medicine residency programs needs remediation. Encouraging residents to present their research in local or state infectious diseases society meetings is an inexpensive method to promote lifelong interest in infectious diseases. Although there are limited resources to train medical residents abroad, the use of teleconferences with partner institutions overseas can be used to create interest, particularly in tropical medicine.
Currently, the IDSA offers nominal registration fees for medical students and residents to attend the IDWeek and gives the Kass Award to provide stipends to students and residents presenting their research findings at the IDWeek. In 2012, 173 residents and 121 medical students attended the IDWeek, and 4 Kass Awards were given. For IDWeek 2013, the program directors’ committee hosted a session on careers in infectious diseases that was directed toward medical students and residents. In addition, research presentations from medical students and residents were presented as the “Posters in the Park” session wherein many program directors and infectious diseases faculty interacted with these individuals to enhance the positive experience. Whether these efforts contribute to an increased number of fellowship program applicants needs careful assessment.
Importantly, the issue of better physician reimbursement is critical and needs to be dealt with. Recent published evidence suggests that early intervention by infectious diseases subspecialists is associated with decreased mortality and lower healthcare costs [11, 12]. Improved patient outcome and reducing healthcare costs are attention-getters, and such data need to be maximally utilized by the IDSA leadership during discussions of appropriate compensation for infectious diseases specialists. Based on a survey of nearly 22 000 US physicians across 25 subspecialties, Medscape recently released an Infectious Disease Physician Compensation Report 2014 [13]. Forty percent of the infectious diseases subspecialists earned $150 000–$200 000 per year, while another 40% earned >$200 000 per year. Infectious diseases physicians ranked 25th out of the 25 specialties surveyed.
ACGME currently permits up to 25% of infectious diseases fellowship positions over a 5-year period to be filled by United States Medical Licensing Examination-certified graduates from approved non-US residency programs. This allowance gives the fellowship program directors a unique opportunity to bring superior candidates from overseas to be trained, then return to their country to serve as role models in the practice of infectious diseases. A small number of US-based fellowship positions are funded by other countries so that their candidates return to practice clinical/academic infectious diseases. Although there is no established mechanism to develop these academic and financial relationships, further work to grow the US infectious diseases fellowships as a “global resource” should be pursued in the common interest of developing a well-trained global infectious diseases community with good practice standards. Existing infectious diseases fellowship positions can also be used to train physicians for work overseas. Whereas traditionally, US-trained physicians who sought international jobs worked in resource-limited countries, the economic growth of many countries has resulted in substantial improvements in healthcare in countries where subspecialty training is sparse. Thus, US infectious diseases fellowships may also prove to be helpful for training a global workforce.
For institutions interested in starting new infectious diseases fellowship programs, strong caution must be offered by the infectious diseases physician community. Also, infectious diseases program directors need to take a cautious approach to increasing the number of fellowship positions. From 2009 to 2013, whereas there was a 19.2% reduction in the number of applicants to infectious diseases through ERAS, there was a 9.1% increase in the number of fellowship positions. Departments of medicine and divisions of infectious diseases must seriously weigh the potential academic value added by increasing infectious diseases fellowship positions against the decreasing number of applicants.
So, is the subspecialty of infectious diseases nearing its demise? Firmly, no. Our field is endlessly captivating; the ever-increasing threat of antibiotic resistance around the globe, discovery of new emerging pathogens (eg, Mimivirus, Emmonsia, Bradyrhizobium, Middle East respiratory syndrome coronavirus), continuing experience with epidemics (eg, fungal meningitis after contaminated steroid use), and the unfolding story of the microbiome and its potential applications are just a few examples of proof of our exciting, vibrant, and kinetic field. The field of infectious diseases uniquely lends itself to multiple career paths. Identifying the exact reasons for the declining number of applications and an increase in involvement by infectious diseases subspecialists in the education/training of medical students and residents are priority measures. The time to act is now.
Notes
Acknowledgments. We acknowledge the Infectious Diseases Society of America Program Directors' Committee, as many of the ideas presented were stimulated by the discussion within the group.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.IDSA news. 2013. Available at: http://news.idsociety.org/idsa/issues/2013-02-28/email.html .
- 2. Association of the American Medical Colleges. Available at: https://www.aamc.org/services/eras . Accessed 14 February 2013.
- 3. National Resident Resident Matching Program, Results and Data: Specialties Matching Service 2014 Appointment Year. National Resident Matching Program, Washington, DC, 2014.
- 4.American Hospital Association. Annual survey of the American Hospital Association. Chicago, IL: American Hospital Association.; 2010. [Google Scholar]
- 5.Profiles. The online database of graduating physicians. Available at: www.profilesdatabase.com. Accessed 14 February 2013.
- 6.West CP, Dupras DM. General internal medicine vs. subspecialty career plans among internal medicine residents. JAMA. 2012;308:2241–7. doi: 10.1001/jama.2012.47535. [DOI] [PubMed] [Google Scholar]
- 7.Petersdorf RL. Whither infectious diseases? Memories, manpower and money. J Infect Dis. 1986;153:189–95. doi: 10.1093/infdis/153.2.189. [DOI] [PubMed] [Google Scholar]
- 8.Kaye D, Abrutyn E. Infectious diseases fellowship training: another viewpoint. Rev Infect Dis. 1987;9:388–91. doi: 10.1093/clinids/9.2.388. [DOI] [PubMed] [Google Scholar]
- 9.Petrak RM, Sexton DJ, Butera ML, et al. The value of an infectious diseases specialist. Clin Infect Dis. 2003;36:1013–7. doi: 10.1086/374245. [DOI] [PubMed] [Google Scholar]
- 10.McQuillen DP, Petrak RM, Wasserman RB, Nahass RG, Scull JA, Martinelli LP. The value of infectious diseases specialists: non-patient care activities. Clin Infect Dis. 2008;47:1051–63. doi: 10.1086/592067. [DOI] [PubMed] [Google Scholar]
- 11.Schmitt S, McQuillen DP, Nahass R, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis. 2014;58:22–8. doi: 10.1093/cid/cit610. [DOI] [PubMed] [Google Scholar]
- 12.Hamandi B, Husain S, Humar A, et al. Impact of infectious disease consultation on the clinical and economic outcomes of solid organ transplant recipients admitted for infectious complications. Clin Infect Dis. 2014;59:1074–82. doi: 10.1093/cid/ciu522. [DOI] [PubMed] [Google Scholar]
- 13.Peckham C. Medscape HIV/ID specialist compensation report. Available at: http://www.medscape.com/features/slideshow/compensation/2014/hiv. Accessed 30 August 2014. [Google Scholar]