Abstract
The clinical exploitation of type I interferon (IFN) as an antiviral and antineoplastic agent is based on the properties originally attributed to this cytokine family, with schedules reflecting only their antiviral and antiproliferative activities. Nevertheless, type I IFN has emerged as a central activator of the innate immunity. As current schedules of treatment for chronic hepatitis C and for hematological and solid tumors, based on the continuous administration of recombinant type I IFN or pegylated formulations, disregard viral resistance, host genetic variants predicting treatment outcome and mechanisms of refractoriness, new administration schedules, the combination of type I IFN with new drugs and the increased monitoring of patients’ susceptibility to type I IFN are expected to provide a new life to this valuable cytokine.
Keywords: Interferon, Viral infection, Cancer, Interferon therapy, Resistance to interferon therapy
1. Introduction
In his book on the history of interferon (IFN), Toine Pieters affirms that IFN can be considered one of modern medicine's most famous and infamous drugs, the history of which has represented an example of therapeutic survival in the face of several cycles of promise and disappointment as a ‘miracle drug’. The therapeutic use of IFN has enhanced our understanding of how drug manufacturing and marketing has played a role in pushing the boundaries of research, from the post penicillin era to the genetics revolution in medicine [1]. It is worth noting that, despite the enormous efforts to produce natural and recombinant type I IFN, and the huge amount of research performed on its biology, the mechanisms of IFN action remain in part elusive and its exploitation in the clinic is still based on the knowledge of its biology from an earlier era. The questions also arise as to whether there is still room for a more appropriate use of type I IFN in infectious diseases and in cancer, and whether the volumes of new information about mechanism of action have been properly incorporated into clinical applications. Before specifically addressing the above issues, it is useful to briefly retrace the history of type I IFN as an anticancer and antiviral drug.
Hyped as a potential antiviral drug, the study of IFN from the very beginning attracted wide attention [2]. Because the efforts to molecularly define and purify IFN proteins remained fruitless for about 20 years, many scientists were openly skeptical about properties ascribed to IFN, including its very existence. Nevertheless, a method for production of IFN had been developed by culturing human leukocytes in Gresser's laboratory [3]. In addition, natural IFN was produced and partially purified at the Finland Red Cross by Cantell [4], for use in the first clinical trial in osteosarcoma patients [5], following the observations on type I IFN antitumor effects obtained in experimental models by Gresser et al. [6]. Many attempts were made to demonstrate the activity of natural IFN on other cancer types – those potentially associated with a viral origin – such as juvenile laryngeal papillomatosis, human condylomata acuminata, Hodgkin's disease, acute leukemia in children, multiple myeloma and others. Early results were considered encouraging but the treatment schedules required optimization and combination schemes required formulation for optimal effect [7].
With regard to true viral infections, the recognition that hepatitis B virus (HBV) may cause a chronic infection leading to cirrhosis and hepatocellular carcinoma suggested that virus-infected patients could be efficaciously treated with IFN. All the “IFN enthusiasts” remember the famous sentence “It is a pleasant surprise to learn that interferon may have an effect on an established chronic infection caused by a poorly understood but extremely important DNA virus” written in 1976 in New England Journal of Medicine by Ho after the discovery made by Greenberg and his colleagues on the ability of IFN to depress Dane-particle-associated DNA, DNA polymerase and core antigen in chronic active hepatitis [8], [9]. Based on these very preliminary “positive” results, IFN-based antiviral and antitumor therapies, quickly became more than a hope among the potential medical armamentarium against tumor and viral infections (Fig. 1, Fig. 2 ). However, it was only after the successful cloning of Type 1 IFN cDNA (the first cytokine ever cloned) and the identification of the IFN gene family that IFN research joined the mainstream of the scientific enterprise [10], [11], [12]. Specifically, Shigekazu Nagata and Sidney Pestka independently identified and expressed IFN alpha 2 in Escherichia coli; the protein was then rapidly purified with monoclonal antibodies and used for research and clinical trials [11], [13]. Thanks to the expression of the recombinant protein in yeast [14], pharmaceutical companies then produced these two types of recombinant IFN in substantial amounts for clinical use in oncology and infectious diseases. IFN alpha 2a and IFN alpha 2b were subsequently approved for the therapeutic treatment of hairy cell leukemia in [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142] (Fig. 1). IFN beta was also cloned, and produced in sufficient quantities for clinical use [15], [16] against tumors and viral diseases. IFN alpha 2a and 2b were registered in 1990 for the treatment of hepatitis C virus (HCV) infection; subsequently, IFN therapy for chronic HBV infection documented two complementary activities of IFN; in HBeAg-positive disease IFN may act as immunomodulatory agent while in HBeAg-negative disease IFN may function as a direct antiviral agent [17].
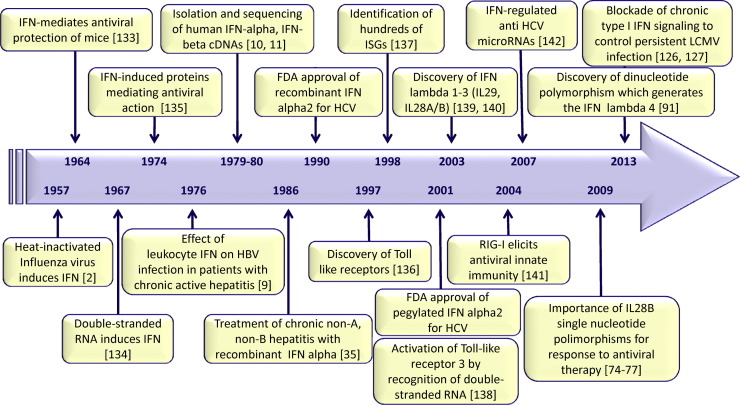
Fig. 1.
Timetable of the most relevant findings in the clinical exploitation of type I IFN in infectious diseases.
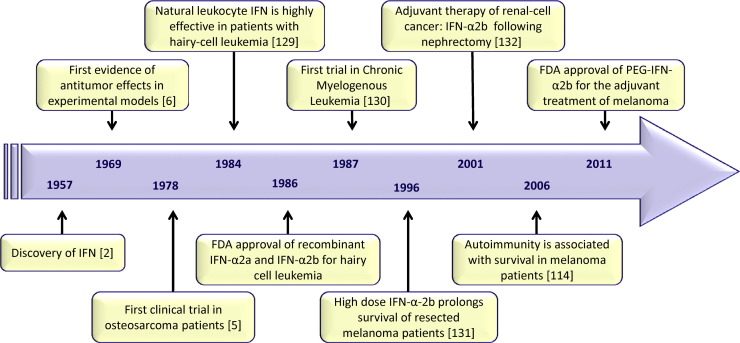
Fig. 2.
Timetable of the most relevant findings in the clinical exploitation of type I IFN in oncology.
IFNs have been the standard of care for certain diseases for more than a decade. It is opinion of the authors that during this period, there has not been an adequate effort made to address the actual mechanism of IFN action or to characterize the factors that could influence IFN treatment outcome. Hence our aim is to discuss some of these issues in the belief that they should be carefully addressed to fully appreciate the efficacy of IFNs as therapeutic agents.
2. Past and current use of IFN
The Type I IFN family in humans consists of 13 IFN alpha subtypes, plus IFN beta, IFN epsilon, IFN kappa, and IFN omega [18]. Most of the available IFN preparations used in clinical practice belong to the type I IFN family (Table 1 ). All type I IFN subtypes elicit antiviral, antiproliferative and immunomodulatory responses by binding to shared cell surface receptors. Interestingly, IFN alpha subtypes have different gene induction profiles and variable antiproliferative, antiviral and immunological properties [19], [20], [21]. However, only a few subtypes of type I IFN, namely IFN alpha 2a and 2b, have been used in therapeutic practice, and the remaining IFN subtypes represent an untapped reservoir of opportunity. The following section summarizes the most common applications of IFN alpha in oncology and virology.
Table 1.
Interferon (IFN) alpha formulations in clinical practice.
| Type of IFN | Brand name | Chemical modification | Structure | Company | Source | Recommendation |
|---|---|---|---|---|---|---|
| Lymphoblastoid IFN alpha N1 | Wellferon® | Not done | Mixture of natural human IFNs alpha subtypes | Glaxo Wellcome | Lymphoblastoid (Namalva) cells | Hairy cell leukemia, juvenile laryngeal papillomatosis, condylomata acuminata, chronic hepatitis B or C |
| Natural human leukocyte IFN alpha | Alfaferone® | Not done | Mixture of natural human IFNs alpha subtypes | Alfa Wassermann | Human leukocyte | Hairy cell leukemia, multiple myeloma, non-Hodgkin lymphoma, follicular lymphoma, chronic myelogenous leukemia, malignant melanoma, AIDS-related Kaposi's sarcoma, chronic hepatitis B or C |
| HuIFN alpha-Le | Multiferon® | Not done | Human leukocyte IFN alpha (IFN alfa-1, 2b, 8, 10, 14, 21) | Swedish Orphan International | Human leukocyte | Malignant melanoma; treatment of patients who initially respond to recombinant IFN-alpha, but for whom treatment subsequently fails, most likely as the result of neutralizing antibodies |
| IFN alpha 2b | Intron A® | Not done | 165 amino acids (19 kDa) Arginine at position 23, deletion at position 44 |
Schering-Plough | Trasformed E. coli | Chronic hepatitis B or C, hairy cell leukemia, follicular lymphoma, condylomata acuminata, AIDS-related Kaposi's sarcoma and malignant melanoma |
| IFN alpha 2a | Roferon-A® | Not done | 165 amino acids (19 kDa) Lysine at position 23, deletion at position 44 |
Hoffmann – La Roche Inc. | Trasformed E. coli | Chronic hepatitis B or C, hairy cell leukemia, chronic myelogenous leukemia |
| Consensus IFN (IFN alfacon-1) | Infergen® | ≈89% homology with IFN alpha and 30% homology with IFN beta | 166 amino acids (19.4 kDa) |
Kadmon Corporation | Trasformed E. coli | Chronic hepatitis C, hairy cell leukemia |
| Pegylated IFN alpha 2b | PegIntron® | 12 kDa linear pegylated molecule | 165 amino acids (19 kDa) |
Schering-Plough | Trasformed E. coli | Chronic hepatitis C |
| Pegylated IFN alpha 2a | Pegasys® | 40 kDa branched pegylated molecule | 165 amino acids (19 kDa) |
Hoffmann – La Roche Inc. | Trasformed E. coli | Chronic hepatitis B, chronic hepatitis C |
| Pegylated IFN alpha 2a | Reiferon Retard® – Egypt |
20 kDa linear pegylated molecule | 165 amino acids (19 kDa) |
Rhein-Minapharm | Trasformed Hansenula polymorpha | Chronic hepatitis C |
| Pegylated IFN alpha 2b | Sylatron™ | 31 kDa pegylated molecule | 165 amino acids (19 kDa) |
Schering Corporation | Trasformed E. coli | Melanoma after surgery |
2.1. Past and current use of IFN in oncology
After the first attempts to use IFN in osteosarcoma, many other tumors were tested for their sensitivity to IFN treatment, and among them, a number of sensitive tumors were identified (see Table 1). The first responsive malignancy was Hairy cell leukemia (HCL), in which IFN induced the reduction of cytopenia and the elimination of hairy cells from the blood, as well as the reduction of bone marrow fibrosis [22]. Although IFN is no longer considered a first-line therapy in HCL, it is still recommended for cytopenic patients to increase granulocyte levels, in order to mount a stronger anti-infective response to antibiotic or anti-fungal therapy.
Since then, IFN has been used primarily in hematologic malignancies such as chronic myelogenous leukemia, multiple myeloma, non-Hodgkin lymphomas, Kaposi's sarcoma in AIDS patients and mycosis fungoides. In all these malignancies, despite a clear in vitro effect on malignant cell proliferation and despite numerous clinical trials, its exact role in the management of disease remained uncertain. Continuous administration (about 3–6 million IU every other day), alone or in combination with other chemotherapeutic drugs, was considered the best treatment available in the induction as well as in the maintenance phase of treatment. In multiple myeloma, for example, among the patients who had an objective response to induction chemotherapy, those treated with IFN had a significantly longer duration of survival [23]. In contrast, with indolent non-Hodgkin lymphoma and follicular lymphoma, IFN treatment was not associated with an overall survival benefit, although it might prolong progression-free survival. Currently, the use of IFN competes with “new drugs”: thalidomide, lenalidomide and bortezomib are now successfully used in myeloma treatment; imatinib and tyrosine kinase inhibitors are the mainstay of treatment in chronic myelogenous leukemia, and IFN is rarely used in these malignancies. Despite evidence that addition of IFN to current protocols (CEOP-Bleo, CHOP, CVP, CHVP, MOPP) as maintenance therapy for follicular lymphoma improved progression-free survival, a net benefit for overall survival was less evident, and IFN was associated with significant toxicities that may have a major impact on the patient's quality of life [24]. In mantle cell lymphoma, rituximab in combination with CHOP or bendamustine have been carefully evaluated in clinical trials, while bortezomib (NFkB inhibitor) or lenalidomide are the approved agents [25]. Similarly, Kaposi's sarcoma and mycosis fungoides patients now have different treatment options in addition to IFN, but the relatively low number of cases actually reduces the quality of the analyses necessary to properly define a superior treatment regimen relative to other treatments [26], [27].
Renal cell carcinoma (RCC) and melanoma are two solid tumors that demonstrate some success with IFN therapy, although the armamentarium for the systemic therapy of these two tumors has undergone dramatic changes in recent years. In particular, cytokine-based therapy including IFN for RCC has been replaced by vascular-endothelial growth factor (VEGF) and mammalian target of rapamycin (mTOR) inhibitors. For low and intermediate risk disease, pazopanib, sunitinib or the combination of bevacizumab plus IFN are considered, whereas combinations of targeted agents (e.g. sunitinib combined with IFN) have generally been plagued by high grade toxicity. Therapy for malignant melanoma has been object of intense research to assess the efficacy of immunotherapeutic strategies; while no treatments have yet shown superior efficacy to IFN in the adjuvant phase, the efficacy of IFN treatment in this setting at low or high doses is still under debate. A number of trials are ongoing to assess whether IFN, associated with different vaccination strategies, reduces the risk of recurrence in resected metastatic melanoma patients [28], [29].
In conclusion, despite the multiple effects of IFN in a variety of malignancies that range from antiangiogenic [30] to potent immunomodulatory [31], differentiation-inducing [32], antiproliferative and proapoptotic [33], IFN is still administered following the schedule used in the first clinical trials, and its use has been superseded by new, more effective and less toxic drugs.
2.2. Past and current use of IFN as antiviral agent
There are currently several approved IFN formulations used to treat chronic viral infections (see Table 1 for the main indications). In addition to hepatitis B virus (HBV) and HCV infections, other chronic viral infections (such as herpes zoster, herpes simplex, cytomegalovirus, HIV, papillomavirus infections) have been effectively treated with both IFN alpha and IFN beta [34]. In parallel, prophylaxis and treatment of acute respiratory viral infections (such rhinovirus, influenza virus or coronavirus) have been evaluated; the introduction of effective antiviral compounds such as acyclovir and its analogs for herpesviruses or azidothymidine and protease inhibitors for HIV with greater therapeutic effect (and reduced side effects), rapidly reduced the commercial interest for IFNs as antivirals.
Evaluation of IFN treatment against all viral infections is an impossible task, thus our discussion is focused only on type I IFN in the treatment of HCV infection. Indeed, the use of IFNs as an anti-HCV agent is an excellent example of “a mix of partial successes and pending challenges”, and reflects the difficulties encountered in the therapeutic use of such a powerful biological weapon. The initial choice of IFN alpha as a potential treatment for chronic hepatitis C (CHC) in 1986 by Hoofnagle was rather empirical [35]. Since then, natural IFN or recombinant IFN alpha formulations were the only drugs available for the treatment of patients suffering from CHC but were associated to limited rates of sustained virological response (SVR), in the range of 12–16%. The addition of ribavirin (RBV) to recombinant IFN alpha increased the SVR rate to about 50%. In 2001, PEG-IFN alpha formulations, specifically PEG-IFN alpha 2a and PEG-IFN alpha 2b, in which inert polyethylene glycol was attached to conventional IFN molecules, were introduced into clinical practice, on the basis of a longer half-life (Fig. 2). The improvement in pharmacokinetic properties of standard IFN alpha preparations, led to a 40–50 SVR in patients infected with HCV genotype (GT) 1. It was therefore not surprising that, after the entry into the market of pegylated forms of IFN alpha (PEG-IFN), a number of companies developed modified IFN or novel IFN delivery systems in the hope of achieving improved pharmacokinetic and pharmacodynamic properties, more potent immunomodulatory effects, and better tolerability. The list of new IFN alpha preparations currently available is provided in Table 2 .
Table 2.
New interferon alpha formulations in clinical practice.
| Type of IFN | Brand name | Chemical modification | Structure | Company | Source | Recommendation |
|---|---|---|---|---|---|---|
| Albinterferon alpha 2b (Albuferon) | JOULFERON® Zalbin™ |
r-Human albumin modified IFN alpha 2b | 165 amino acids (19 kDa) | Human Genome Sciences Inc./Novartis International AG | Transformed Kluyveromyces | Chronic hepatitis C |
| IFN alpha 2b | Locteron® | PolyActive® technologya-based controlled-release recombinant formulation | 165 amino acids (19 kDa) | Biolex Therapeutics | Trasformed E. coli | Chronic hepatitis C |
| IFN alpha 2b | IFN alfa-2b XL | Medusa® technologyb-based recombinant formulation | 165 amino acids (19.4 kDa) | Flamel Technologies | Trasformed E. coli | Chronic hepatitis C |
| IFN alpha | Belerofon® | Single aa mutation that lowers sensitivity to protease-mediated degradation | N.A.c | Nautilus Biotech | N.A.c | Chronic hepatitis C |
| IFN alpha | Novaferon | Artificial design technology combining DNA-shuffling and High throughput screening | 82% sequence identity to IFN alpha 2b (19 kDa) | N.A. | N.A. | N.A |
Biodegradable polymeric drug delivery system.
Nanoparticles delivery system.
Not available.
More recently, the availability of several directly acting antiviral agents (DAAs) for HCV, mainly inhibitors of NS3, NS5A and NS5B viral proteins, has offered the possibility of IFN-free, anti-HCV treatment. Although moving to DAAs therapies will greatly increase SVR rate and offer new treatments for ineligible or non-responding HCV positive patients, the actual price of DAAs is exceedingly high and these new drugs are associated with development of drug resistance, thus calling into question the choice to abandon the “old and consolidated” therapeutic road. At the same time, new antiviral agents that boost host innate immunity or target specific cellular pathways (host-targeting antivirals (HTAs)), are also emerging as alternative anti-viral therapies [36]. Among them are Toll-like receptor (TLR)7, TLR9 (ANA773, GS-9620 and IMO-2125) and retinoic acid-inducible gene I (RIG-I) (e.g. 5′pppRNA) agonists and antimicroRNA122 (Miravirsen). All these strategies are linked with the IFN system, again emphasizing the critical role of IFN in orchestrating the innate immune response and the necessity to unravel the pleiotropic biological actions of IFN [36], [37], [38].
Type I IFN preparations remain a valid therapeutic option, due to their broad-spectrum of antiviral properties and their ready availability for the treatment of emerging zoonotic viral diseases, including those in which the time to vaccine availability precludes vaccination at the onset of an outbreak. Since the 2002–2003 severe acute respiratory syndrome coronavirus (SARS-COV) outbreak, several other examples illustrate the ability of IFN alpha/beta to inhibit the replication of new emerging viruses [e.g. Middle East Respiratory Syndrome coronavirus (MERS-COV), avian and pandemic H1N1influenza viruses [19], [39], [40], [41], [42], [43], [44]].
3. Factors affecting the response to type I IFN
The intense clinical research on the therapeutic use of type I IFN has not been paralleled by similar efforts in defining the determinants that confer cell sensitivity or refractoriness to it. More specifically, efforts to characterize the factors affecting IFN therapy outcome have not been comparable in oncology and virology, in large part because viral therapy is more suited to the complex relationships between host, virus and IFN response. Likewise, knowledge acquired in the virological field has not been fully exploited to explain the failure of IFN treatment in cancer patients.
3.1. General mechanisms of refractoriness to IFN
IFN activity is mediated by the binding to its receptor and the activation of the JAK–STAT signaling pathway, resulting in the induction of the expression of hundreds of IFN-stimulated genes (ISGs), as reviewed in [45]. All type I IFNs signal through a common heterodimeric receptor composed of a low- (IFNAR1) and a high-affinity (IFNAR2) subunit and, through an as yet non-completely elucidated mechanism, drive different biological signals [46]. When administered at high doses, IFNs are not devoid of toxic effects, indicating that their action must be fine-tuned through opposing enhancing and suppressive signals. Upon ligand engagement, the signaling complex is rapidly internalized by endocytosis and, subsequently ubiquitinated and degraded. Marijanovic et al. showed that while the surface half-life of IFNAR1 is 4 h in unstimulated cells, its half life is reduced to 1 h in cells stimulated with IFN alpha [47]. The non-responsive state of IFN-treated cells was shown to last up to 3 days [48], whereas after IFN removal, expression of IFNAR1 at the cell surface returned to nearly 100% control levels within 3 h [47]. The consequence of these observations is that continuous administration of high dose IFN or the pegylated formulations can determine an unwanted decrease of receptor expression at the cell surface, and represents one of the earliest activated mechanisms of refractoriness to IFN. Given that all effects of type I IFN on infected, malignant and immune cells are mediated by its receptor, modulation of IFNAR levels may be expected to play a dominant role in shaping the extent and the duration of the type I IFN response. Altogether, these observations argue that rational design of IFN-based therapies should carefully consider these aspects of IFN receptor biology, indicating that new strategies to stabilize IFNAR1 and inhibit its degradation are needed. Similarly, evaluation of the basal expression of the IFNAR complex and of its down-regulation following treatment should be a component of standard care in IFN-treated patients.
Mice repeatedly injected with murine IFN alpha were shown to become refractory to further stimulation within a few hours after the first injection [49]. Suppressor of cytokine signaling (SOCS) proteins, in particular SOCS1 and SOCS3, was shown to be important for the negative regulation of type I and type II IFN signaling, through the inhibition of STAT1 binding to IFNAR and suppression of JAK activity [50] respectively. Similarly, ubiquitin carboxy-terminal hydrolase 18 (USP18)/Ubiquitin protease 43 (UBP43) was shown to be required for induction of a long-lasting desensitized state [49]. Binding of UBP43 to IFNAR2 in vivo displaced JAK1 from IFNAR2 and led to the inhibition of the downstream phosphorylation cascade and other signaling events [51]. Of note, administration of PEG-IFN alpha 2b in patients with CHC was shown to activate the JAK/STAT pathway only during the first day following injection, and then rapidly induced SOCS1, SOCS3 and UBP43 expression, despite the fact that the serum concentrations of PEG-IFN alpha 2 remained high for the entire week. These observations argued that the superior antiviral efficacy of PEG-IFN alpha was not related to constitutive activation of IFN signaling pathways, but rather the induction of immune response-associated genes by PEG-IFN was the mechanism underlying increased efficacy [52].
Since the deficiency of either SOCS1 or UBP43 can amplify IFN antiviral and proinflammatory actions, both activities may represent promising therapeutic targets to improve the benefits of IFN treatment in cancer as well as in viral diseases. In this regard, UBP43 was identified as a poor prognostic marker of IFN alpha therapy in patients with chronic hepatitis C [53], and its in vitro silencing in human cells potentiated the antiviral activity of IFN [54]. Similarly, UBP43 levels were increased in several human tumors, including non-small cell lung cancer, and its silencing in mouse lung cancer cells rendered the cells less tumorigenic and more sensible to the growth-inhibitory and pro-apoptotic effects of IFN in vitro [55].
Several recent papers suggest a major role for different microRNAs (miR) in regulating the IFN response. In this regard, miR-155 broadly suppresses the expression of IFNAR–JAK–STAT pathway components in CD8+ T cells [56], while miR-221 suppresses SOCS1/SOCS3 functions, thus acting as enhancer of the JAK–STAT signaling [57]. Importantly, patients with hepatocellular carcinoma with reduced miR-26 expression in tumors displayed a significant improvement in overall survival after receiving adjuvant therapy with IFN alpha, indicating that miR-26 expression status can indeed help to stratify patients with respect to response to IFN therapy [58].
3.2. Resistance and variability to IFN alpha treatment in CHC patients
Since the beginning of IFN in therapy for CHC, it was evident that HCV infected subjects responded differently to IFN administration. Such a variability in responsiveness was totally unexpected on the basis of results obtained by in vitro experimentations, and this variability has stimulated intense efforts aimed at understanding the underlying mechanisms of resistance to IFN treatment, as well as characterizing predictive biomarkers that could be useful in identifying patients who were likely to respond to IFN treatment. It is important to emphasize that although many determinants of the IFN response have been identified, much work is still required to fully appreciate the potential of type I IFN action. Two variables that modulate the IFN response – viral and host determinants – will be discussed separately below.
3.2.1. Viral determinants
The highly variable response rate observed in HCV patients treated with IFN alpha depends on well-established viral factors such as viral load; patients with high pretreatment viral loads have poor long-term outcomes compared to patients with low viral loads, and an increased risk of treatment failure is observed against the most predominant HCV GT, GT1 (subtypes 1a and 1b). The HCV decay kinetics is also an important factor in estimating the effectiveness of antiviral therapy [59].
To fully appreciate the variability of the IFN response in HCV patients, it is also important to consider the polymorphism of the HCV genome. For instance, in 1995 Enomoto et al., found that a HCV GT1b virus with four or more amino acid substitutions in the NS5A 2209–2248 region, termed IFN-sensitivity-determining region (ISDR), prior to therapy was strongly correlated with the SVR to IFN alpha therapy in Japanese patients, and the number of amino acid substitutions was thought to be an independent predictor of IFN treatment success [60], [61]. These initial findings were further confirmed by other studies in Japanese patients [62], [63]. However, several reports from Europe and United States failed to show a correlation between ISDR mutations and IFN responsiveness [64]. Later it was established that the ISDR was necessary but not sufficient for the interaction between NS5A and the IFN induced PKR enzyme; an additional 26 amino acids, called PKR binding domain (PKRBD), distal to the ISDR was also required; the latter region was shown to hinder PKR dimerization and resulted in the repression of PKR function on the eIF-2alpha translation factor [64]. Indeed, mutations within the PKRBD of HCV GT1 have been associated with a long-term sustained response to IFN alpha and PEG-IFN alpha/RBV therapy [65], [66], [67].
Other regions of HCV, especially E2 (PKR/eIF-2alpha phosphorylation homology domain (PePHD)) or the NS5A region (V3 in the C-terminal portion) have been shown to contain specific sequences in different HCV genotypes that differentially affect the IFN response [64], [68], [69], [70]. Interestingly most of these HCV proteins can subvert the type I IFN response in vitro [18] but whether these HCV evasion strategies are active in vivo and influence the IFN treatment response are unclear. All the above considerations, together with the indication of a close association between HCV genetic variability and antiviral treatment outcome lead to an important general question – “Is the infection of specific HCV GTs and/or mutations in specific regions of the genome able to affect the endogenous production/action of IFNs and expression of ISGs, or does such a high variability simply reflect an authentic adaptation of HCV to the immune response including type I IFN expression and function”? Some attempts to answer these questions have been made but the issue remains largely unresolved [71], [72], [73].
3.2.2. Host determinants
Since the initial use of IFN for CHC therapy, it has been understood that different pre-treatment host factors (such as age, sex, body weight, insulin resistance, and liver fibrosis) significantly affect the virological response to IFN or PEG-IFN alpha-ribavirin therapy. The variability of IFN response however could not entirely be explained by the above-mentioned factors; recently, two single nucleotide polymorphisms (SNPs) rs12979860 (T/C) and rs8099917 (T/G), in the region of interleukin (IL) 28B/IFN lambda 3 on chromosome 19, have been definitively associated with spontaneous and IFN treatment-induced viral clearance in HCV infection [74], [75], [76], [77].
Together with the discovery of the above SNPs, it became clear that the concerted action of multiple ISGs must also be considered to fully understand the limits of IFN alpha treatment. Administration of IFN induces an up-regulation of ISGs in PBMC and the liver of HCV-infected individuals; the type, and especially the magnitude, of the IFN induced response differed between responder and non-responder HCV positive individuals [53], [78], [79], [80]. HCV infected patients who were less likely to respond to the IFN alpha therapy exhibited paradoxically a higher constitutive ISG expression compared to those that achieved a good response [53], [78], [80], [81], [82], [83]. Notably, the presence of high basal levels of ISGs was associated with a lack of increased expression after IFN administration [83], [84]. The molecular mechanism linking baseline ISG induction to IFN non-response remains currently unknown.
It has been proposed that the refractoriness to exogenous IFN could reflect the presence of high pretreatment levels of the UBP43 negative regulator and/or reflect that IFN transduction pathways are saturated [49], [80], [85]. The up-regulation of ISGs in liver-derived biopsies of chronically HCV infected patients is largely sustained by hepatocytes [86], although Kupffer cells can be a local source of IFN that promoted basal expression of ISG in hepatocytes of non-responders [87]. In addition, there is no significant correlation between serum or intrahepatic viral loads with ISG expression levels, suggesting that this response is ineffective in term of HCV replication control [80]. It is also not clear whether type I or III IFN is the driver of basal ISGs induction. In this regard, type I and III IFN differ in their kinetics of production and their level of ISG induction with a clearly detectable hierarchy [88], [89]; these pathways are severely impaired in liver-derived tissues of chronically HCV infected patients [86]. The lack of a specific signature of type I and III IFN in the liver of HCV positive subjects, characterized by the presence of high endogenous levels of ISGs, could be indicative of a severe impairment of early host defense pathways. In addition we speculate that pretreatment ISG response may reflect type I and III IFN produced in response of HCV replication, as well as an IFN-independent mechanism triggered by HCV; alternatively other pathways, for instance mitogen-activated protein kinase/extracellular-regulated kinase (MAPK/ERK) and the phosphoinositide-3 kinase (PI-3K), could be involved in the process. Another possibility is that the basal ISGs signature is induced by IFN beta rather than by IFN alpha subtypes, or reflects a deficient IFN gamma signal as observed in acute vs. chronic HCV infection [85]. In this regard, a unique IFN beta signaling axis mediated via the receptor IFNAR1 has been recently identified [90].
Several studies have demonstrated that the IL28B/IFN lambda 3 poor-response minor alleles (both the above rs120979860 and rs8099917) are associated with high basal levels of ISGs, providing compelling evidence for the involvement of a genetic predisposition [80]. It should also be mentioned that the very recent discovery of a dinucleotide polymorphism ss469415590 TT/ΔG upstream of IL28B/IFN lambda 3, which generates the novel IFN lambda 4 (variant allele, ΔG) protein, may reveal an alternative scenario to understand the functional architecture of type III IFN genomic regions and its influence on the outcome of HCV infection, and also to identify the relationship between endogenous ISG up-regulation and poor response to IFN alpha treatment [91]. As the IFN lambda 4 creating allele ΔG is correlated with the unfavorable rs12979860 allele T, ss469415590 TT was a better predictor of HCV clearance than rs12979860, and a role of ss469415590 TT in predicting response to anti-HCV therapy with or without IFN has been reported (for a review see [92]). Interestingly, carriers of the IFN lambda 4 creating ΔG allele were found to have significantly higher amounts of ISG mRNA than patients homozygous for the disruptive TT allele [93]. Moreover, by relating actual IFN lambda 4 transcription in carriers of the ΔG allele to ISG induction, HCV infected patients with measurable quantities of IFN lambda 4 mRNAs presented significantly stronger ISG induction than those without [93]. This observation may provide a possible explanation as to why HCV positive patients show ISG stimulation in their livers in the apparent absence of an induction of other IFN subtypes [93].
As HCV therapy is evolving rapidly from IFN-based to DAA-only regimens, the relevance of the endogenous IFN system for IFN-free therapy treatment outcome could be questioned. However, recently it has been demonstrated that HCV clearance achieved during IFN-free treatment with a DDAs regimen is accompanied by hepatic down-regulation of type II and III IFN, their receptors, and ISGs [94]. Furthermore, the ability to restore intrahepatic type I IFN signaling is associated with prolonged HCV suppression [94]. Altogether, the above findings together with the observation that RBV has been shown in vitro to up-regulate a narrow spectrum of ISGs [95], [96], highlight the importance of evaluating whether variability in the expression of components of the IFN system may affect the clinical outcome of IFN-free regimen in HCV patients.
3.3. Immunomodulatory properties of type I IFN
Although the immunoregulatory properties of type I IFN have been appreciated since the 1970s [97], [98], IFNs are still administered with schedules and modalities that reflect their antiviral and antiproliferative activities. Early studies in mouse tumor models demonstrated that the generation of a long-lasting antitumor response to type I IFN depended on host immune mechanisms [99], [100], in part reflecting the identification of type I IFN as a regulator of class I histocompatibility antigen expression [101]. IFNs are indeed important regulators of several components of the host immunity, with activities ranging from the stimulation of lymphocyte- and monocyte-mediated cytotoxicity [102], to the activation of macrophages, natural killer (NK) [103], CD8+ memory T cells [104] and dendritic cells (DC) [105], [106]. IFN alpha/beta, in fact, induces DC maturation, up-regulates their co-stimulatory activity and enhances their capacity to kill tumor cells and present or cross-present antigens [107]. IFN alpha also plays a key role in the polarization of T-helper cells toward a Th-1 subtype [108], in enhancing the primary antibody response to soluble antigens [109] and in deactivating the suppressive function of mice [110] and human regulatory T cells (Treg) [111], thus enhancing T helper cell functions and NK cell tumor cytotoxicity.
All the immunomodulatory activities of type I IFN and, in particular, the effects on the innate immune response and on immunological memory can account for its efficacy as a vaccine adjuvant, as demonstrated in an influenza infection model in mice [112], as well as in melanoma patients [28]. Recently, IFN was shown to have a pivotal role in rendering immunogenic the cell death induced by chemotherapies, thus supporting the participation of the immune system in their cytocidal activity [113]. The observed correlation between a favorable response to systemic administration of IFN alpha and the appearance of autoimmunity in metastatic melanoma patients, strongly corroborate the hypothesis that the induction of a host immunostimulatory mechanism is a critical factor predicting the antitumor efficacy of IFN [114]. Nevertheless, in the large majority of clinical studies, the effect of IFN administration on immune cells is not monitored and therefore an important part of its mechanism of action is disregarded, not allowing a mechanistic-based improvement of the therapeutic efficacy.
4. Conclusions and recommendations
IFNs and their receptors represent early elements in innate and adaptive immunity evolution and their physiological activity consists of stimulating immune defenses against the invasion of foreign pathological elements by a potent, but transient, action which is quickly extinguished by self-regulatory mechanisms. After the discovery of IFN, early studies focused only on two of its multiple properties, the antiviral and anti-proliferative activities. The identification of additional members of the IFN family, characterization of the complex properties of distinct IFN subtypes, and increasing knowledge of the regulation of the IFN response have all progressed rapidly in the realm of pre-clinical research, but have yet to be incorporated into the use of IFN in treatments for infectious disease or cancer. Clinically, IFN has been used at high doses, with the intent to maintain high concentrations in the body, through frequent injections or sustained release. The overall therapeutic results of such a strategy have been beneficial in some infectious or neoplastic diseases, but in other diseases, especially when used as a single agent, the value of IFN therapy has been limited, particularly in light of systemic toxicity. For example, high doses of IFN are effective in drastically reducing the viremia in HCV-infected patients after the first treatment cycle, but subsequently, virus loads rise and ribavirin is required for therapeutic efficacy. Furthermore, the beneficial effects of continuous exogenous IFN (i.e. after PEG-IFN) are hampered by the induction of different mechanisms of refractoriness – receptor internalization/degradation, rapid induction of UBP43 and SOCS negative regulators – thus limiting PEG-IFN activity, despite its persistence in serum [51]. Nevertheless, PEG-IFN alpha, with its favorable pharmacokinetics and pharmacodynamics, improves the outcome in CHC patients, although it is not clear that its activity is related to the acute induction of ISGs. Indeed, since its approval in the early 1990s for CHC, IFN alpha and PEG-IFN alpha has been used in HCV patients regardless of whether a pre-existing type I IFN signature could make the patient intrinsically resistant to IFN therapy, and may reflect an activated IFN transduction pathway, as in the case of chronic viral infection or continuous IFN administration [80], [115], [116]. The relationships between type I IFN production, ISG expression, host genetic determinants, virus variability and clearance of HCV are not understood for IFN alpha-based therapy; likewise the above properties of the IFN response may also be important in the new era of DAAs against HCV, since some evidence indicates that the introduction of DAAs into the IFN regimen may affect innate immune activation [94], [117]. It is thus questionable whether IFN alpha and/or DAAs can be used effectively without first assessing endogenous type I IFN activation. Indeed, IFN has known anti-fibrotic action and there is no proof that patients with advanced stage liver disease who clear viral infection with DAAs completely arrest liver disease progression [118].
In addition to the anti-angiogenic effects of high dose IFN, which lead to the reduction of tumor vasculature, most of the anti-tumor therapeutic effects of IFN are associated with immune modulation. A brief but intense production of type I IFN by plasmacytoid dendritic cells stimulates innate immunity [119] and, similarly induces the proliferation of memory CD4+ and CD8+ T cells [104] and activates NK cells [120]. In the physiology of the immune response, type I IFN plays a crucial but brief role, whereas continuous IFN production leads to pathological consequences as demonstrated in systemic lupus erythematosus [121]. These considerations should lead to a reconsideration of the scheduling of IFN treatment in favor of administration given at progressively delayed time intervals, to avoid the refractory mechanisms induced by IFN. Furthermore, IFN therapy should be directed to its target (vascular endothelium, monocytes/dendritic cells, T lymphocytes, tumor cells etc.), through targeted delivery strategies, which require lower doses and therefore produce less systemic side effects [122]. Also the pro-apoptotic and immuno-adjuvant activities of IFN should be combined with chemo- or radio-therapeutic treatment to increase the immunogenicity of dying tumor cells [113] and their up-take by dendritic cells [107]. Monitoring of immune cell activation should be considered in IFN treated patients for a mechanistic-based improvement of the therapeutic efficacy.
Based on the observations that genetic variability (i.e. SNPs in the IL28B/IFN lambda 3 and IFN lambda 4 on chromosome 19) rendered CHC patients prone to virus clearance after IFN treatment, IFN treatment should be personalized to consider genetic variations that may impact treatment of viral infections or cancer. Similarly, monitoring the known mechanisms of “resistance or escape” used by viruses and tumors, or developing drugs that reduce resistance, could improve IFN treatment effectiveness.
The observations that type I IFN response can be deleterious for the host in secondary bacterial or fungal infections, several autoimmune diseases, and certain chronic viral infections, should prompt us to reflect whether IFN alpha has been optimally used in clinical practice [123]. For instance the detrimental effects of type I IFN action are clearly demonstrable during lymphocytic choriomeningitis virus (LCMV), pathogenic simian immunodeficiency virus (SIV) and HIV infections where a direct causal link between type I IFN/ISGs expression and chronic immune activation and dysfunction has been reported [124], [125], [126], [127]. It is not surprising, then, that the possibility of therapeutically targeting either type I IFN or its production is now emerging as a new therapeutic strategy against viral diseases. However, recently it was demonstrated that blockade of the type I IFN receptor using type I IFN receptor antagonist after SIV infection of rhesus macaques diminished antiviral gene expression, increased SIV reservoir size and accelerated CD4+ T-cell depletion with progression to AIDS, despite decreased T-cell activation [128]. Thus, an elevated type I IFN signature can be deleterious in some chronic viral infections, further emphasizing the difficulties associated with in the in vivo manipulation of this complex biological system. All these observations demonstrate that the consequences of manipulation of IFN signaling are difficult to predict in vivo, and therapeutic intervention in patients should be conducted with caution, with careful consideration of the physiology of the IFN action.
Conflict of interest statement
None.
Acknowledgements
We thank Ms. Rosina Bellizzi for her excellent secretarial support and Mr. Gaetano Pezzicoli for his dedicated scientific assistance.
Biographies

Guido Antonelli is Full Professor of Virology at “Sapienza” University of Rome, Italy. He is Head of the Virology Section of the Department of Molecular Medicine at the same University and Head of the Department of “Diagnostic Medicine” at the “Policlinico Umberto I” University Hospital in Rome. He obtained his Ph.D. in “Medical Microbiology” at the University of Pisa, Italy in 1988. His initial research interests focused on the mechanism of action and production of interferons. During in that period, he worked in Ferdinando Dianzani's lab at the Sapienza University in Rome and as visiting scientist in Samuel Baron's Lab at the UTMB in Galveston, Texas (USA). Nowadays, his group's research interests lie primarily in the pathogenesis, control and diagnosis of viral infections (particularly HIV, HCV, HPV and respiratory viruses). For a number of years he has served as coeditor of peer-reviewed journals (including “Clinical Microbiology and Infection – CMI”/Wiley and “Journal of Global Antimicrobial Resistance – JGAR”/Elsevier).

Carolina Scagnolari graduated in Biological Sciences in 2000. After receiving her Ph.D. and Microbiology and Virology post graduated school degrees, in 2010, she joined the “Sapienza” University of Rome as Assistant Professor of Virology. Currently, she is the chief of antiviral innate immunity research Unit at the Department of Molecular Medicine. Scagnolari's career has been devoted to viral infectious diseases focusing principally on the role of type I and III interferons in the control of acute and chronic viral infections, mostly those caused by respiratory viruses, hepatitis C virus and HIV. She received the “Sivim” (2004) and “ICAR-CROI” (2014) awards, the special Jury Price CROI/2014 and several research grants from “Sapienza” University and Institutes of Pasteur International Network. She is author/co-author of about 63 papers appeared on international journals in the field of Virology and Immunology.

Federica Moschella is a Post-doctoral researcher in Dr. Enrico Proietti's Applied biotherapy Unit of the Dept. of Hematology, Oncology and Molecular Medicine. She obtained a degree in Biological Sciences and a Ph.D. in Biochemistry and Molecular Biology from the University of Naples. She spent 3 years as a postdoctoral research fellow at Columbia Presbyterian Hospital, New York. Her research is mainly focused on unraveling the mechanisms that underlie the antitumor activity of combination strategies aimed at enhancing the efficacy of immunotherapy in cancer patients, with a particular emphasis on type I interferon-mediated mechanisms.
Enrico Proietti is research director and head of the Applied Biotherapy Unit in the Dept. of Hematology, Oncology and Molecular Medicine at Istituto Superiore di Sanità, Italy. He obtained his M.D. in 1978 and is board certified in clinical immunology and in clinical oncology. As visiting scientist he worked in Ion Gresser's laboratory in Villejuif, France, from 1989 to 1991. He worked for a long time on the anticancer and immuno-modulating activities of type I interferon, discovering its immunoadjuvant properties. Nowadays, the research of his group is focused on the clinical exploitation of new cancer vaccination modalities with particular interest in methods aimed at reducing cancer immune-suppression and potentiating antitumor immune responses.
References
- 1.Pieters T. Routledge; London and New York: 2005. Interferon: the science and selling of a miracle drug. [Google Scholar]
- 2.Isaacs A., Lindenmann J. Virus interference. I. The interferon. Proc R Soc Lond B Biol Sci. 1957;147:258–267. [PubMed] [Google Scholar]
- 3.Gresser I. Production of interferon by suspensions of human leucocytes. Proc Soc Exp Biol Med. 1961;108:799–803. doi: 10.3181/00379727-108-27072. [DOI] [PubMed] [Google Scholar]
- 4.Strander H., Cantell K. Production of interferon by human leukocytes in vitro. Ann Med Exp Biol Fenn. 1966;44:265–273. [PubMed] [Google Scholar]
- 5.Strander H., Adamson U., Aparisi T., Brostrom L.A., Cantell K., Einhorn S. Adjuvant interferon treatment of human osteosarcoma. Recent Results Cancer Res. 1978;68:40–44. doi: 10.1007/978-3-642-81332-0_7. [DOI] [PubMed] [Google Scholar]
- 6.Gresser I., Bourali C., Levy J.P., Fontaine-Brouty-Boye D., Thomas M.T. Increased survival in mice inoculated with tumor cells and treated with interferon preparations. Proc Natl Acad Sci U S A. 1969;63:51–57. doi: 10.1073/pnas.63.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strander H. The action of interferons on virus-associated human neoplasms. Cancer Surv. 1989;8:755–792. [PubMed] [Google Scholar]
- 8.Ho M. Editorial: interferon and hepatitis B virus. N Engl J Med. 1976;295:562–563. doi: 10.1056/NEJM197609022951009. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg H.B., Pollard R.B., Lutwick L.I., Gregory P.B., Robinson W.S., Merigan T.C. Effect of human leukocyte interferon on hepatitis B virus infection in patients with chronic active hepatitis. N Engl J Med. 1976;295:517–522. doi: 10.1056/NEJM197609022951001. [DOI] [PubMed] [Google Scholar]
- 10.Taniguchi T., Saka M., Fujii-Kuriyama Y., Muramatsu M., Kobayashi M., Sudo T. Construction and identification of a bacterial plasmid containing the human fibroblast interferon gene sequence. Proc Jpn Acad. 1979;55B:464–469. [Google Scholar]
- 11.Nagata S., Taira H., Hall A., Johnsrud L., Streuli M., Ecsodi J. Synthesis in E. coli of a polypeptide with human leukocyte interferon activity. Nature. 1980;284:316–320. doi: 10.1038/284316a0. [DOI] [PubMed] [Google Scholar]
- 12.Gray P.W., Goeddel D.V. Structure of the human immune interferon gene. Nature. 1982;298:859–863. doi: 10.1038/298859a0. [DOI] [PubMed] [Google Scholar]
- 13.Staehelin T., Hobbs D.S., Kung H., Lai C.Y., Pestka S. Purification and characterization of recombinant human leukocyte interferon (IFLrA) with monoclonal antibodies. J Biol Chem. 1981;256:9750–9754. [PubMed] [Google Scholar]
- 14.Hitzeman R.A., Leung D.W., Perry L.J., Kohr W.J., Levine H.L., Goeddel D.V. Secretion of human interferons by yeast. Science. 1983;219:620–625. doi: 10.1126/science.6186023. [DOI] [PubMed] [Google Scholar]
- 15.Derynck R., Content J., DeClercq E., Volckaert G., Tavernier J., Devos R. Isolation and structure of a human fibroblast interferon gene. Nature. 1980;285:542–547. doi: 10.1038/285542a0. [DOI] [PubMed] [Google Scholar]
- 16.Goeddel D.V., Shepard H.M., Yelverton E., Leung D., Crea R., Sloma A. Synthesis of human fibroblast interferon by E. coli. Nucleic Acids Res. 1980;8:4057–4074. doi: 10.1093/nar/8.18.4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcellin P., Lau G.K., Bonino F., Farci P., Hadziyannis S., Jin R. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–1217. doi: 10.1056/NEJMoa040431. [DOI] [PubMed] [Google Scholar]
- 18.Scagnolari C., Antonelli G. Antiviral activity of the interferon alpha family: biological and pharmacological aspects of the treatment of chronic hepatitis C. Expert Opin Biol Ther. 2013;13:693–711. doi: 10.1517/14712598.2013.764409. [DOI] [PubMed] [Google Scholar]
- 19.Scagnolari C., Trombetti S., Solda A., Selvaggi C., Monteleone K., Spano L. Pandemic 2009 H1N1 influenza virus is resistant to the antiviral activity of several interferon alpha subtypes. J Interferon Cytokine Res. 2011;31:475–479. doi: 10.1089/jir.2010.0125. [DOI] [PubMed] [Google Scholar]
- 20.Scagnolari C., Trombetti S., Selvaggi C., Carbone T., Monteleone K., Spano L. In vitro sensitivity of human metapneumovirus to type I interferons. Viral Immunol. 2011;24:159–164. doi: 10.1089/vim.2010.0073. [DOI] [PubMed] [Google Scholar]
- 21.Gibbert K., Schlaak J.F., Yang D., Dittmer U. IFN-alpha subtypes: distinct biological activities in anti-viral therapy. Br J Pharmacol. 2013;168:1048–1058. doi: 10.1111/bph.12010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maevis V., Mey U., Schmidt-Wolf G., Schmidt-Wolf I.G. Hairy cell leukemia: short review, today's recommendations and outlook. Blood Cancer J. 2014;4:e184. doi: 10.1038/bcj.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mandelli F., Avvisati G., Amadori S., Boccadoro M., Gernone A., Lauta V.M. Maintenance treatment with recombinant interferon alfa-2b in patients with multiple myeloma responding to conventional induction chemotherapy. N Engl J Med. 1990;322:1430–1434. doi: 10.1056/NEJM199005173222005. [DOI] [PubMed] [Google Scholar]
- 24.Baldo P., Rupolo M., Compagnoni A., Lazzarini R., Bearz A., Cannizzaro R. Interferon-alpha for maintenance of follicular lymphoma. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD004629.pub2. CD004629. [DOI] [PubMed] [Google Scholar]
- 25.Vose J.M. Mantle cell lymphoma: 2013 update on diagnosis, risk-stratification, and clinical management. Am J Hematol. 2013;88:1082–1088. doi: 10.1002/ajh.23615. [DOI] [PubMed] [Google Scholar]
- 26.Regnier-Rosencher E., Guillot B., Dupin N. Treatments for classic Kaposi sarcoma: a systematic review of the literature. J Am Acad Dermatol. 2013;68:313–331. doi: 10.1016/j.jaad.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Humme D., Nast A., Erdmann R., Vandersee S., Beyer M. Systematic review of combination therapies for mycosis fungoides. Cancer Treat Rev. 2014;40:927–933. doi: 10.1016/j.ctrv.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 28.Di Pucchio T., Pilla L., Capone I., Ferrantini M., Montefiore E., Urbani F. Immunization of stage IV melanoma patients with Melan-A/MART-1 and gp100 peptides plus IFN-alpha results in the activation of specific CD8(+) T cells and monocyte/dendritic cell precursors. Cancer Res. 2006;66:4943–4951. doi: 10.1158/0008-5472.CAN-05-3396. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell M.S., Abrams J., Thompson J.A., Kashani-Sabet M., DeConti R.C., Hwu W.J. Randomized trial of an allogeneic melanoma lysate vaccine with low-dose interferon Alfa-2b compared with high-dose interferon Alfa-2b for Resected stage III cutaneous melanoma. J Clin Oncol. 2007;25:2078–2085. doi: 10.1200/JCO.2006.10.1709. [DOI] [PubMed] [Google Scholar]
- 30.Fidler I.J. Regulation of neoplastic angiogenesis. J Natl Cancer Inst Monogr. 2001:10–14. doi: 10.1093/oxfordjournals.jncimonographs.a024251. [DOI] [PubMed] [Google Scholar]
- 31.Rizza P., Moretti F., Belardelli F. Recent advances on the immunomodulatory effects of IFN-alpha: implications for cancer immunotherapy and autoimmunity. Autoimmunity. 2010;43:204–209. doi: 10.3109/08916930903510880. [DOI] [PubMed] [Google Scholar]
- 32.Rossi G.B., Albertini R., Battistini A., Coccia E.M., Romeo G., Fiorucci G. Interferons and the differentiation of friend cells. Ann N Y Acad Sci. 1989;567:253–258. doi: 10.1111/j.1749-6632.1989.tb16476.x. [DOI] [PubMed] [Google Scholar]
- 33.Kotredes K.P., Gamero A.M. Interferons as inducers of apoptosis in malignant cells. J Interferon Cytokine Res. 2013;33:162–170. doi: 10.1089/jir.2012.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borden E.C., Sen G.C., Uze G., Silverman R.H., Ransohoff R.M., Foster G.R. Interferons at age 50: past, current and future impact on biomedicine. Nat Rev Drug Discov. 2007;6:975–990. doi: 10.1038/nrd2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoofnagle J.H., Mullen K.D., Jones D.B., Rustgi V., Di Bisceglie A., Peters M. Treatment of chronic non-A, non-B hepatitis with recombinant human alpha interferon. A preliminary report. N Engl J Med. 1986;315:1575–1578. doi: 10.1056/NEJM198612183152503. [DOI] [PubMed] [Google Scholar]
- 36.Baugh J.M., Garcia-Rivera J.A., Gallay P.A. Host-targeting agents in the treatment of hepatitis C: a beginning and an end. Antiviral Res. 2013;100:555–561. doi: 10.1016/j.antiviral.2013.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Janssen H.L., Reesink H.W., Lawitz E.J., Zeuzem S., Rodriguez-Torres M., Patel K. Treatment of HCV infection by targeting microRNA. N Engl J Med. 2013;368:1685–1694. doi: 10.1056/NEJMoa1209026. [DOI] [PubMed] [Google Scholar]
- 38.Goulet M.L., Olagnier D., Xu Z., Paz S., Belgnaoui S.M., Lafferty E.I. Systems analysis of a RIG-I agonist inducing broad spectrum inhibition of virus infectivity. PLoS Pathog. 2013;9:e1003298. doi: 10.1371/journal.ppat.1003298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cinatl J., Morgenstern B., Bauer G., Chandra P., Rabenau H., Doerr H.W. Treatment of SARS with human interferons. Lancet. 2003;362:293–294. doi: 10.1016/S0140-6736(03)13973-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scagnolari C., Vicenzi E., Bellomi F., Stillitano M.G., Pinna D., Poli G. Increased sensitivity of SARS-coronavirus to a combination of human type I and type II interferons. Antivir Ther. 2004;9:1003–1011. [PubMed] [Google Scholar]
- 41.Osterlund P., Pirhonen J., Ikonen N., Ronkko E., Strengell M., Makela S.M. Pandemic H1N1 2009 influenza A virus induces weak cytokine responses in human macrophages and dendritic cells and is highly sensitive to the antiviral actions of interferons. J Virol. 2010;84:1414–1422. doi: 10.1128/JVI.01619-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ngunjiri J.M., Mohni K.N., Sekellick M.J., Schultz-Cherry S., Webster R.G., Marcus P.I. Lethal H5N1 influenza viruses are not resistant to interferon action in human, simian, porcine or chicken cells. Nat Med. 2012;18:1456–1457. doi: 10.1038/nm.2879. [DOI] [PubMed] [Google Scholar]
- 43.Falzarano D., de Wit E., Rasmussen A.L., Feldmann F., Okumura A., Scott D.P. Treatment with interferon-alpha2b and ribavirin improves outcome in MERS-CoV-infected rhesus macaques. Nat Med. 2013;19:1313–1317. doi: 10.1038/nm.3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Omrani A.S., Saad M.M., Baig K., Bahloul A., Abdul-Matin M., Alaidaroos A.Y. Ribavirin and interferon alfa-2a for severe Middle East respiratory syndrome coronavirus infection: a retrospective cohort study. Lancet Infect Dis. 2014 doi: 10.1016/S1473-3099(14)70920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ivashkiv L.B., Donlin L.T. Regulation of type I interferon responses. Nat Rev Immunol. 2014;14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Weerd N.A., Nguyen T. The interferons and their receptors – distribution and regulation. Immunol Cell Biol. 2012;90:483–491. doi: 10.1038/icb.2012.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marijanovic Z., Ragimbeau J., Kumar K.G., Fuchs S.Y., Pellegrini S. TYK2 activity promotes ligand-induced IFNAR1 proteolysis. Biochem J. 2006;397:31–38. doi: 10.1042/BJ20060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larner A.C., Chaudhuri A., Darnell J.E., Jr. Transcriptional induction by interferon. New protein(s) determine the extent and length of the induction. J Biol Chem. 1986;261:453–459. [PubMed] [Google Scholar]
- 49.Sarasin-Filipowicz M., Wang X., Yan M., Duong F.H., Poli V., Hilton D.J. Alpha interferon induces long-lasting refractoriness of JAK–STAT signaling in the mouse liver through induction of USP18/UBP43. Mol Cell Biol. 2009;29:4841–4851. doi: 10.1128/MCB.00224-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fenner J.E., Starr R., Cornish A.L., Zhang J.G., Metcalf D., Schreiber R.D. Suppressor of cytokine signaling 1 regulates the immune response to infection by a unique inhibition of type I interferon activity. Nat Immunol. 2006;7:33–39. doi: 10.1038/ni1287. [DOI] [PubMed] [Google Scholar]
- 51.Malakhova O.A., Kim K.I., Luo J.K., Zou W., Kumar K.G., Fuchs S.Y. UBP43 is a novel regulator of interferon signaling independent of its ISG15 isopeptidase activity. EMBO J. 2006;25:2358–2367. doi: 10.1038/sj.emboj.7601149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dill M.T., Makowska Z., Trincucci G., Gruber A.J., Vogt J.E., Filipowicz M. Pegylated IFN-alpha regulates hepatic gene expression through transient Jak/STAT activation. J Clin Invest. 2014;124:1568–1581. doi: 10.1172/JCI70408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen L., Borozan I., Feld J., Sun J., Tannis L.L., Coltescu C. Hepatic gene expression discriminates responders and nonresponders in treatment of chronic hepatitis C viral infection. Gastroenterology. 2005;128:1437–1444. doi: 10.1053/j.gastro.2005.01.059. [DOI] [PubMed] [Google Scholar]
- 54.Randall G., Chen L., Panis M., Fischer A.K., Lindenbach B.D., Sun J. Silencing of USP18 potentiates the antiviral activity of interferon against hepatitis C virus infection. Gastroenterology. 2006;131:1584–1591. doi: 10.1053/j.gastro.2006.08.043. [DOI] [PubMed] [Google Scholar]
- 55.Guo Y., Chinyengetere F., Dolinko A.V., Lopez-Aguiar A., Lu Y., Galimberti F. Evidence for the ubiquitin protease UBP43 as an antineoplastic target. Mol Cancer Ther. 2012;11:1968–1977. doi: 10.1158/1535-7163.MCT-12-0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gracias D.T., Stelekati E., Hope J.L., Boesteanu A.C., Doering T.A., Norton J. The microRNA miR-155 controls CD8(+) T cell responses by regulating interferon signaling. Nat Immunol. 2013;14:593–602. doi: 10.1038/ni.2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xu G., Yang F., Ding C.L., Wang J., Zhao P., Wang W. MiR-221 accentuates IFNs anti-HCV effect by downregulating SOCS1 and SOCS3. Virology. 2014;462–463:343–350. doi: 10.1016/j.virol.2014.06.024. [DOI] [PubMed] [Google Scholar]
- 58.Ji J., Shi J., Budhu A., Yu Z., Forgues M., Roessler S. MicroRNA expression, survival, and response to interferon in liver cancer. N Engl J Med. 2009;361:1437–1447. doi: 10.1056/NEJMoa0901282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pawlotsky J.M. Treatment of hepatitis C: how will we use viral kinetics, response-guided therapy? Curr Gastroenterol Rep. 2013;15:309. doi: 10.1007/s11894-012-0309-x. [DOI] [PubMed] [Google Scholar]
- 60.Enomoto N., Sakuma I., Asahina Y., Kurosaki M., Murakami T., Yamamoto C. Comparison of full-length sequences of interferon-sensitive and resistant hepatitis C virus 1b. Sensitivity to interferon is conferred by amino acid substitutions in the NS5A region. J Clin Invest. 1995;96:224–230. doi: 10.1172/JCI118025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Enomoto N., Sakuma I., Asahina Y., Kurosaki M., Murakami T., Yamamoto C. Mutations in the nonstructural protein 5A gene and response to interferon in patients with chronic hepatitis C virus 1b infection. N Engl J Med. 1996;334:77–81. doi: 10.1056/NEJM199601113340203. [DOI] [PubMed] [Google Scholar]
- 62.Kurosaki M., Enomoto N., Murakami T., Sakuma I., Asahina Y., Yamamoto C. Analysis of genotypes and amino acid residues 2209 to 2248 of the NS5A region of hepatitis C virus in relation to the response to interferon-beta therapy. Hepatology. 1997;25:750–753. doi: 10.1002/hep.510250343. [DOI] [PubMed] [Google Scholar]
- 63.Komatsu H., Fujisawa T., Inui A., Miyagawa Y., Onoue M. Mutations in the nonstructural protein 5A gene and response to interferon therapy in young patients with chronic hepatitis C virus 1b infection. J Med Virol. 1997;53:361–365. [PubMed] [Google Scholar]
- 64.Hofmann W.P., Zeuzem S., Sarrazin C. Hepatitis C virus-related resistance mechanisms to interferon alpha-based antiviral therapy. J Clin Virol. 2005;32:86–91. doi: 10.1016/j.jcv.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 65.Berg T., Mas Marques A., Hohne M., Wiedenmann B., Hopf U., Schreier E. Mutations in the E2-PePHD and NS5A region of hepatitis C virus type 1 and the dynamics of hepatitis C viremia decline during interferon alfa treatment. Hepatology. 2000;32:1386–1395. doi: 10.1053/jhep.2000.20527. [DOI] [PubMed] [Google Scholar]
- 66.Macquillan G.C., Niu X., Speers D., English S., Garas G., Harnett G.B. Does sequencing the PKRBD of hepatitis C virus NS5A predict therapeutic response to combination therapy in an Australian population. J Gastroenterol Hepatol. 2004;19:551–557. doi: 10.1111/j.1440-1746.2003.03319.x. [DOI] [PubMed] [Google Scholar]
- 67.Munoz de Rueda P., Casado J., Paton R., Quintero D., Palacios A., Gila A. Mutations in E2-PePHD, NS5A-PKRBD, NS5A-ISDR, and NS5A-V3 of hepatitis C virus genotype 1 and their relationships to pegylated interferon-ribavirin treatment responses. J Virol. 2008;82:6644–6653. doi: 10.1128/JVI.02231-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gerotto M., Dal Pero F., Pontisso P., Noventa F., Gatta A., Alberti A. Two PKR inhibitor HCV proteins correlate with early but not sustained response to interferon. Gastroenterology. 2000;119:1649–1655. doi: 10.1053/gast.2000.20230. [DOI] [PubMed] [Google Scholar]
- 69.Maekawa S., Enomoto N. Viral factors influencing the response to the combination therapy of peginterferon plus ribavirin in chronic hepatitis C. J Gastroenterol. 2009;44:1009–1015. doi: 10.1007/s00535-009-0126-7. [DOI] [PubMed] [Google Scholar]
- 70.El-Shamy A., Shoji I., El-Akel W., Bilasy S.E., Deng L., El-Raziky M. NS5A sequence heterogeneity of hepatitis C virus genotype 4a predicts clinical outcome of pegylated-interferon-ribavirin therapy in Egyptian patients. J Clin Microbiol. 2012;50:3886–3892. doi: 10.1128/JCM.02109-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bellecave P., Sarasin-Filipowicz M., Donze O., Kennel A., Gouttenoire J., Meylan E. Cleavage of mitochondrial antiviral signaling protein in the liver of patients with chronic hepatitis C correlates with a reduced activation of the endogenous interferon system. Hepatology. 2010;51:1127–1136. doi: 10.1002/hep.23426. [DOI] [PubMed] [Google Scholar]
- 72.Akuta N., Suzuki F., Hirakawa M., Kawamura Y., Yatsuji H., Sezaki H. Amino acid substitution in hepatitis C virus core region and genetic variation near the interleukin 28B gene predict viral response to telaprevir with peginterferon and ribavirin. Hepatology. 2010;52:421–429. doi: 10.1002/hep.23690. [DOI] [PubMed] [Google Scholar]
- 73.Maekawa S., Sakamoto M., Miura M., Kadokura M., Sueki R., Komase K. Comprehensive analysis for viral elements and interleukin-28B polymorphisms in response to pegylated interferon plus ribavirin therapy in hepatitis C virus 1B infection. Hepatology. 2012;56:1611–1621. doi: 10.1002/hep.25826. [DOI] [PubMed] [Google Scholar]
- 74.Ge D., Fellay J., Thompson A.J., Simon J.S., Shianna K.V., Urban T.J. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461:399–401. doi: 10.1038/nature08309. [DOI] [PubMed] [Google Scholar]
- 75.Thomas D.L., Thio C.L., Martin M.P., Qi Y., Ge D., O’Huigin C. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature. 2009;461:798–801. doi: 10.1038/nature08463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Suppiah V., Moldovan M., Ahlenstiel G., Berg T., Weltman M., Abate M.L. IL28B is associated with response to chronic hepatitis C interferon-alpha and ribavirin therapy. Nat Genet. 2009;41:1100–1104. doi: 10.1038/ng.447. [DOI] [PubMed] [Google Scholar]
- 77.Tanaka Y., Nishida N., Sugiyama M., Kurosaki M., Matsuura K., Sakamoto N. Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet. 2009;41:1105–1109. doi: 10.1038/ng.449. [DOI] [PubMed] [Google Scholar]
- 78.Antonelli G., Simeoni E., Turriziani O., Tesoro R., Redaelli A., Roffi L. Correlation of interferon-induced expression of MxA mRNA in peripheral blood mononuclear cells with the response of patients with chronic active hepatitis C to IFN-alpha therapy. J Interferon Cytokine Res. 1999;19:243–251. doi: 10.1089/107999099314171. [DOI] [PubMed] [Google Scholar]
- 79.Ji X., Cheung R., Cooper S., Li Q., Greenberg H.B., He X.S. Interferon alfa regulated gene expression in patients initiating interferon treatment for chronic hepatitis C. Hepatology. 2003;37:610–621. doi: 10.1053/jhep.2003.50105. [DOI] [PubMed] [Google Scholar]
- 80.Heim M.H. 25 years of interferon-based treatment of chronic hepatitis C: an epoch coming to an end. Nat Rev Immunol. 2013;13:535–542. doi: 10.1038/nri3463. [DOI] [PubMed] [Google Scholar]
- 81.Giannelli G., Guadagnino G., Dentico P., Antonelli G., Antonaci S. MxA and PKR expression in chronic hepatitis C. J Interferon Cytokine Res. 2004;24:659–663. doi: 10.1089/jir.2004.24.659. [DOI] [PubMed] [Google Scholar]
- 82.Bellecave P., Moradpour D. A fresh look at interferon-alpha signaling and treatment outcomes in chronic hepatitis C. Hepatology. 2008;48:1330–1333. doi: 10.1002/hep.22571. [DOI] [PubMed] [Google Scholar]
- 83.Sarasin-Filipowicz M., Oakeley E.J., Duong F.H., Christen V., Terracciano L., Filipowicz W. Interferon signaling and treatment outcome in chronic hepatitis C. Proc Natl Acad Sci U S A. 2008;105:7034–7039. doi: 10.1073/pnas.0707882105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scagnolari C., Bellomi F., Trombetti S., Casato M., Carlesimo M., Bagnato F. Expression of biomarkers of interferon type I in patients suffering from chronic diseases. Clin Exp Immunol. 2007;147:270–276. doi: 10.1111/j.1365-2249.2006.03280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dill M.T., Makowska Z., Duong F.H., Merkofer F., Filipowicz M., Baumert T.F. Interferon-gamma-stimulated genes, but not USP18, are expressed in livers of patients with acute hepatitis C. Gastroenterology. 2012;143:777–786. doi: 10.1053/j.gastro.2012.05.044. e1–6. [DOI] [PubMed] [Google Scholar]
- 86.Jouan L., Chatel-Chaix L., Melancon P., Rodrigue-Gervais I.G., Raymond V.A., Selliah S. Targeted impairment of innate antiviral responses in the liver of chronic hepatitis C patients. J Hepatol. 2012;56:70–77. doi: 10.1016/j.jhep.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 87.Lau D.T., Negash A., Chen J., Crochet N., Sinha M., Zhang Y. Innate immune tolerance and the role of kupffer cells in differential responses to interferon therapy among patients with HCV genotype 1 infection. Gastroenterology. 2013;144:402–413. doi: 10.1053/j.gastro.2012.10.044. e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bolen C.R., Ding S., Robek M.D., Kleinstein S.H. Dynamic expression profiling of type I and type III interferon-stimulated hepatocytes reveals a stable hierarchy of gene expression. Hepatology. 2014;59:1262–1272. doi: 10.1002/hep.26657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Olagnier D., Hiscott J. Type I and type III interferon-induced immune response: it's a matter of kinetics and magnitude. Hepatology. 2014;59:1225–1228. doi: 10.1002/hep.26959. [DOI] [PubMed] [Google Scholar]
- 90.de Weerd N.A., Vivian J.P., Nguyen T.K., Mangan N.E., Gould J.A., Braniff S.J. Structural basis of a unique interferon-beta signaling axis mediated via the receptor IFNAR1. Nat Immunol. 2013;14:901–907. doi: 10.1038/ni.2667. [DOI] [PubMed] [Google Scholar]
- 91.Prokunina-Olsson L., Muchmore B., Tang W., Pfeiffer R.M., Park H., Dickensheets H. A variant upstream of IFNL3 (IL28B) creating a new interferon gene IFNL4 is associated with impaired clearance of hepatitis C virus. Nat Genet. 2013;45:164–171. doi: 10.1038/ng.2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Riva E., Scagnolari C., Turriziani O., Antonelli G. Hepatitis C virus and interferon type III (interferon lambda 3/interleukin 28B and interferon lambda 4): genetic basis of susceptibility to infection and response to antiviral treatment. Clin Microbiol Infect. 2014 doi: 10.1111/1469-0691.12797. [DOI] [PubMed] [Google Scholar]
- 93.Amanzada A., Kopp W., Spengler U., Ramadori G., Mihm S. Interferon-lambda4 (IFNL4) transcript expression in human liver tissue samples. PLOS ONE. 2013;8:e84026. doi: 10.1371/journal.pone.0084026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Meissner E.G., Wu D., Osinusi A., Bon D., Virtaneva K., Sturdevant D. Endogenous intrahepatic IFNs and association with IFN-free HCV treatment outcome. J Clin Invest. 2014;124:3352–3363. doi: 10.1172/JCI75938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Thomas E., Feld J.J., Li Q., Hu Z., Fried M.W., Liang T.J. Ribavirin potentiates interferon action by augmenting interferon-stimulated gene induction in hepatitis C virus cell culture models. Hepatology. 2011;53:32–41. doi: 10.1002/hep.23985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tokumoto Y., Hiasa Y., Uesugi K., Watanabe T., Mashiba T., Abe M. Ribavirin regulates hepatitis C virus replication through enhancing interferon-stimulated genes and interleukin 8. J Infect Dis. 2012;205:1121–1130. doi: 10.1093/infdis/jis025. [DOI] [PubMed] [Google Scholar]
- 97.Gresser I., Tovey M.G. Antitumor effects of interferon. Biochim Biophys Acta. 1978;516:231–247. doi: 10.1016/0304-419x(78)90009-4. [DOI] [PubMed] [Google Scholar]
- 98.Belardelli F., Gresser I., Maury C., Maunoury M.T. Antitumor effects of interferon in mice injected with interferon-sensitive and interferon-resistant Friend leukemia cells. II. Role of host mechanisms. Int J Cancer. 1982;30:821–825. doi: 10.1002/ijc.2910300622. [DOI] [PubMed] [Google Scholar]
- 99.Belardelli F., Ferrantini M., Proietti E., Kirkwood J.M. Interferon-alpha in tumor immunity and immunotherapy. Cytokine Growth Factor Rev. 2002;13:119–134. doi: 10.1016/s1359-6101(01)00022-3. [DOI] [PubMed] [Google Scholar]
- 100.Moschella F., Proietti E., Capone I., Belardelli F. Combination strategies for enhancing the efficacy of immunotherapy in cancer patients. Ann N Y Acad Sci. 2010;1194:169–178. doi: 10.1111/j.1749-6632.2010.05464.x. [DOI] [PubMed] [Google Scholar]
- 101.Nissen M.H., Plesner T., Larsen J.K., Olesen B.K., Ernst P. Enhanced expression in vivo of HLA-ABC antigens and beta 2-microglobulin on human lymphoid cells induced by human interferon-alpha in patients with lung cancer. Enhanced expression of class I major histocompatibility antigens prior to treatment. Clin Exp Immunol. 1985;59:327–335. [PMC free article] [PubMed] [Google Scholar]
- 102.Webb D.S., Gerrard T.L. IFN-alpha and IFN-gamma can affect both monocytes and tumor cells to modulate monocyte-mediated cytotoxicity. J Immunol. 1990;144:3643–3648. [PubMed] [Google Scholar]
- 103.Trinchieri G., Santoli D. Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells. Enhancement of human natural killer cell activity by interferon and antagonistic inhibition of susceptibility of target cells to lysis. J Exp Med. 1978;147:1314–1333. doi: 10.1084/jem.147.5.1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tough D.F., Borrow P., Sprent J. Induction of bystander T cell proliferation by viruses and type I interferon in vivo. Science. 1996;272:1947–1950. doi: 10.1126/science.272.5270.1947. [DOI] [PubMed] [Google Scholar]
- 105.Paquette R.L., Hsu N.C., Kiertscher S.M., Park A.N., Tran L., Roth M.D. Interferon-alpha and granulocyte-macrophage colony-stimulating factor differentiate peripheral blood monocytes into potent antigen-presenting cells. J Leukoc Biol. 1998;64:358–367. doi: 10.1002/jlb.64.3.358. [DOI] [PubMed] [Google Scholar]
- 106.Santini S.M., Lapenta C., Logozzi M., Parlato S., Spada M., Di Pucchio T. Type I interferon as a powerful adjuvant for monocyte-derived dendritic cell development and activity in vitro and in Hu-PBL-SCID mice. J Exp Med. 2000;191:1777–1788. doi: 10.1084/jem.191.10.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Moschella F., Bisikirska B., Maffei A., Papadopoulos K.P., Skerrett D., Liu Z. Gene expression profiling and functional activity of human dendritic cells induced with IFN-alpha-2b: implications for cancer immunotherapy. Clin Cancer Res. 2003;9:2022–2031. [PubMed] [Google Scholar]
- 108.Brinkmann V., Geiger T., Alkan S., Heusser C.H. Interferon alpha increases the frequency of interferon gamma-producing human CD4+ T cells. J Exp Med. 1993;178:1655–1663. doi: 10.1084/jem.178.5.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Le Bon A., Schiavoni G., D’Agostino G., Gresser I., Belardelli F., Tough D.F. Type I interferons potently enhance humoral immunity and can promote isotype switching by stimulating dendritic cells in vivo. Immunity. 2001;14:461–470. doi: 10.1016/s1074-7613(01)00126-1. [DOI] [PubMed] [Google Scholar]
- 110.Pace L., Vitale S., Dettori B., Palombi C., La Sorsa V., Belardelli F. APC activation by IFN-alpha decreases regulatory T cell and enhances Th cell functions. J Immunol. 2010;184:5969–5979. doi: 10.4049/jimmunol.0900526. [DOI] [PubMed] [Google Scholar]
- 111.Bacher N., Raker V., Hofmann C., Graulich E., Schwenk M., Baumgrass R. Interferon-alpha suppresses cAMP to disarm human regulatory T cells. Cancer Res. 2013;73:5647–5656. doi: 10.1158/0008-5472.CAN-12-3788. [DOI] [PubMed] [Google Scholar]
- 112.Bracci L., Canini I., Venditti M., Spada M., Puzelli S., Donatelli I. Type I IFN as a vaccine adjuvant for both systemic and mucosal vaccination against influenza virus. Vaccine. 2006;24(Suppl. 2):56–57. doi: 10.1016/j.vaccine.2005.01.121. [DOI] [PubMed] [Google Scholar]
- 113.Sistigu A., Yamazaki T., Vacchelli E., Chaba K., Enot D.P., Adam J. Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nat Med. 2014;20:1301–1309. doi: 10.1038/nm.3708. [DOI] [PubMed] [Google Scholar]
- 114.Gogas H., Ioannovich J., Dafni U., Stavropoulou-Giokas C., Frangia K., Tsoutsos D. Prognostic significance of autoimmunity during treatment of melanoma with interferon. N Engl J Med. 2006;354:709–718. doi: 10.1056/NEJMoa053007. [DOI] [PubMed] [Google Scholar]
- 115.Naveau S., Emilie D., Borotto E., Portier A., Lazizi Y., Giraud V. Interleukin-1 receptor antagonist plasma concentration is specifically increased by alpha-2A-interferon treatment. J Hepatol. 1997;27:272–275. doi: 10.1016/s0168-8278(97)80171-7. [DOI] [PubMed] [Google Scholar]
- 116.Cotler S.J., Craft T., Ferris M., Morrisey M., McCone J., Reddy K.R. Induction of IL-1Ra in resistant and responsive hepatitis C patients following treatment with IFN-con1. J Interferon Cytokine Res. 2002;22:549–554. doi: 10.1089/10799900252982025. [DOI] [PubMed] [Google Scholar]
- 117.Malone D.F., Falconer K., Weiland O., Sandberg J.K. The dynamic relationship between innate immune biomarkers and interferon-based treatment effects and outcome in hepatitis C virus infection is altered by telaprevir. PLOS ONE. 2014;9:e105665. doi: 10.1371/journal.pone.0105665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ippolito G., Capobianchi M.R., Lanini S., Antonelli G. Is hepatitis C virus eradication around the corner only 25 years after its discovery? Int J Antimicrob Agents. 2014 doi: 10.1016/j.ijantimicag.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 119.Banchereau J., Briere F., Caux C., Davoust J., Lebecque S., Liu Y.J. Immunobiology of dendritic cells. Annu Rev Immunol. 2000;18:767–811. doi: 10.1146/annurev.immunol.18.1.767. [DOI] [PubMed] [Google Scholar]
- 120.Lee C.K., Rao D.T., Gertner R., Gimeno R., Frey A.B., Levy D.E. Distinct requirements for IFNs and STAT1 in NK cell function. J Immunol. 2000;165:3571–3577. doi: 10.4049/jimmunol.165.7.3571. [DOI] [PubMed] [Google Scholar]
- 121.Banchereau J., Pascual V. Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity. 2006;25:383–392. doi: 10.1016/j.immuni.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 122.Garcin G., Paul F., Staufenbiel M., Bordat Y., Van der Heyden J., Wilmes S. High efficiency cell-specific targeting of cytokine activity. Nat Commun. 2014;5:3016. doi: 10.1038/ncomms4016. [DOI] [PubMed] [Google Scholar]
- 123.Trinchieri G. Type I interferon: friend or foe? J Exp Med. 2010;207:2053–2063. doi: 10.1084/jem.20101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bosinger S.E., Sodora D.L., Silvestri G. Generalized immune activation and innate immune responses in simian immunodeficiency virus infection. Curr Opin HIV AIDS. 2011;6:411–418. doi: 10.1097/COH.0b013e3283499cf6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hughes R., Towers G., Noursadeghi M. Innate immune interferon responses to human immunodeficiency virus-1 infection. Rev Med Virol. 2012;22:257–266. doi: 10.1002/rmv.1708. [DOI] [PubMed] [Google Scholar]
- 126.Teijaro J.R., Ng C., Lee A.M., Sullivan B.M., Sheehan K.C., Welch M. Persistent LCMV infection is controlled by blockade of type I interferon signaling. Science. 2013;340:207–211. doi: 10.1126/science.1235214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wilson E.B., Yamada D.H., Elsaesser H., Herskovitz J., Deng J., Cheng G. Blockade of chronic type I interferon signaling to control persistent LCMV infection. Science. 2013;340:202–207. doi: 10.1126/science.1235208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sandler N.G., Bosinger S.E., Estes J.D., Zhu R.T., Tharp G.K., Boritz E. Type I interferon responses in rhesus macaques prevent SIV infection and slow disease progression. Nature. 2014;511:601–605. doi: 10.1038/nature13554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Quesada J.R., Reuben J., Manning J.T., Hersh E.M., Gutterman J.U. Alpha interferon for induction of remission in hairy-cell leukemia. N Engl J Med. 1984;310:15–18. doi: 10.1056/NEJM198401053100104. [DOI] [PubMed] [Google Scholar]
- 130.Talpaz M., Kantarjian H.M., McCredie K.B., Keating M.J., Trujillo J., Gutterman J. Clinical investigation of human alpha interferon in chronic myelogenous leukemia. Blood. 1987;69:1280–1288. [PubMed] [Google Scholar]
- 131.Kirkwood J.M., Strawderman M.H., Ernstoff M.S., Smith T.J., Borden E.C., Blum R.H. Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J Clin Oncol. 1996;14:7–17. doi: 10.1200/JCO.1996.14.1.7. [DOI] [PubMed] [Google Scholar]
- 132.Flanigan R.C., Salmon S.E., Blumenstein B.A., Bearman S.I., Roy V., McGrath P.C. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med. 2001;345:1655–1659. doi: 10.1056/NEJMoa003013. [DOI] [PubMed] [Google Scholar]
- 133.Ho M. Interferon-like viral inhibitor in rabbits after intravenous administration of endotoxin. Science. 1964;146:1472–1474. doi: 10.1126/science.146.3650.1472. [DOI] [PubMed] [Google Scholar]
- 134.Field A.K., Tytell A.A., Lampson G.P., Hilleman M.R. Inducers of interferon and host resistance. II. Multistranded synthetic polynucleotide complexes. Proc Natl Acad Sci U S A. 1967;58:1004–1010. doi: 10.1073/pnas.58.3.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kerr I.M., Brown R.E., Ball L.A. Increased sensitivity of cell-free protein synthesis to double-stranded RNA after interferon treatment. Nature. 1974;250:57–59. doi: 10.1038/250057a0. [DOI] [PubMed] [Google Scholar]
- 136.Medzhitov R., Preston-Hurlburt P., Janeway C.A., Jr. A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature. 1997;388:394–397. doi: 10.1038/41131. [DOI] [PubMed] [Google Scholar]
- 137.Der S.D., Zhou A., Williams B.R., Silverman R.H. Identification of genes differentially regulated by interferon alpha, beta, or gamma using oligonucleotide arrays. Proc Natl Acad Sci U S A. 1998;95:15623–15628. doi: 10.1073/pnas.95.26.15623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Alexopoulou L., Holt A.C., Medzhitov R., Flavell R.A. Recognition of double-stranded RNA and activation of NF-kappaB by Toll-like receptor 3. Nature. 2001;413:732–738. doi: 10.1038/35099560. [DOI] [PubMed] [Google Scholar]
- 139.Kotenko S.V., Gallagher G., Baurin V.V., Lewis-Antes A., Shen M., Shah N.K. IFN-lambdas mediate antiviral protection through a distinct class II cytokine receptor complex. Nat Immunol. 2003;4:69–77. doi: 10.1038/ni875. [DOI] [PubMed] [Google Scholar]
- 140.Sheppard P., Kindsvogel W., Xu W., Henderson K., Schlutsmeyer S., Whitmore T.E. IL-28, IL-29 and their class II cytokine receptor IL-28R. Nat Immunol. 2003;4:63–68. doi: 10.1038/ni873. [DOI] [PubMed] [Google Scholar]
- 141.Yoneyama M., Kikuchi M., Natsukawa T., Shinobu N., Imaizumi T., Miyagishi M. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat Immunol. 2004;5:730–737. doi: 10.1038/ni1087. [DOI] [PubMed] [Google Scholar]
- 142.Pedersen I.M., Cheng G., Wieland S., Volinia S., Croce C.M., Chisari F.V. Interferon modulation of cellular microRNAs as an antiviral mechanism. Nature. 2007;449:919–922. doi: 10.1038/nature06205. [DOI] [PMC free article] [PubMed] [Google Scholar]