Abstract
Early recognition of patients who might potentially require ventilatory support is a key goal of critical care outreach programmes and an important skill for all hospital medical staff. Decisions about the initiation and timing of invasive ventilation can be difficult, and early discussion with critical care colleagues is essential. Appropriateness of invasive ventilatory support can also require advanced discussion with patients and families. In the past 10–15 years, the role of non-invasive ventilation (NIV) has expanded, not least in an attempt to minimize the complications inherent in invasive ventilation. Indeed, NIV is now considered first-line therapy in some conditions (chronic obstructive pulmonary disease, pulmonary oedema, mild to moderate hypoxaemic respiratory failure in immunocompromised patients), and a ‘trial of NIV’ is often considered in respiratory failure resulting from an increasingly wide range of causes. With NIV, the importance of the environment (setting, monitoring, experience of staff) and forward planning cannot be overemphasized. When used for other than the standard indications, NIV should be employed in a high-dependency or intensive care setting in patients for whom invasive ventilation would be considered.
Keywords: Intensive care, mechanical ventilation, non-invasive mechanical ventilation, respiratory failure
Key points.
-
•
NIV has numerous advantages over IMV, such as lower risks of, haemodynamic instability, nosocomial infections and ventilation induced lung injury. However, it is important to clarify that NIV is NOT a replacement in cases where IMV is primarily indicated
-
•
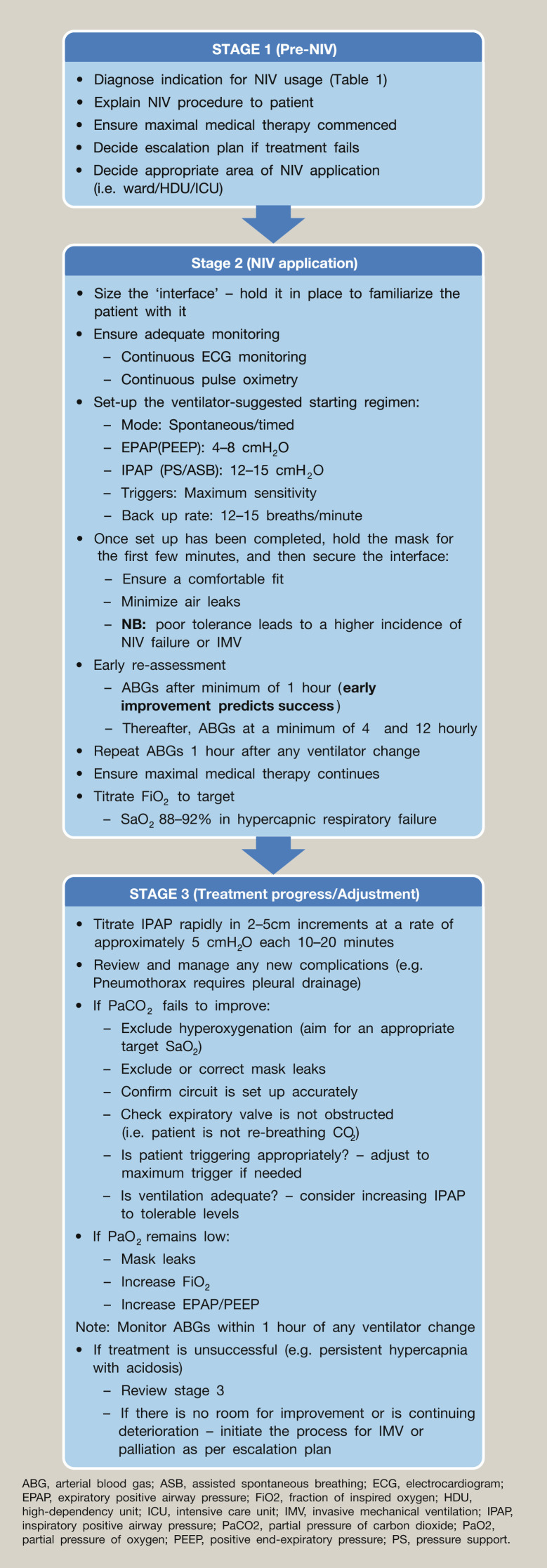
Tolerability and management of patients initiated on NIV requires an appropriate step by step process, to maximize the benefit and avoid treatment failure (see Figure 1)
-
•
NIV in acute type II respiratory failure in COPD patients is an established evidenced based therapy and in most cases is first line. Other clinical scenarios such as respiratory failure secondary to acute pulmonary oedema show good evidence for using NIV or CPAP. However, caution needs to be applied in using NIV for certain causes of respiratory failure (e.g. pneumonia)
-
•
Escalation plans in critically ill patients involving a decision and appropriateness of IMV, requires a thorough clinical assessment including an individuals baseline function, with early consultation and discussions between the senior physician, critical care team and patient/family.
-
•
Following intubation and IMV, low volume and low pressure ventilation (avoiding volutrauma), ‘permissive’ hypoxia and hypercapnia, are important ventilation strategies in combination with general intensive care management (e.g. sedation holds and early appropriate nutritional support)
Introduction
Indications for ventilation
Early identification of critically ill patients, before the occurrence of significant cardiorespiratory decompensation, is one of the major goals of critical care outreach programmes. Patients who require ventilatory support often develop a common pattern of physiological deterioration including:
-
•
increasing respiratory rate
-
•
an asynchronous respiratory pattern
-
•
a change in mentation and level of consciousness
-
•
frequent oxygen desaturation despite increasing oxygen concentration
-
•
hypercapnia and respiratory acidosis
-
•
circulatory problems, including hypotension and atrial dysrhythmias.
Modern ventilators
The modern ventilator is a complex, computer-driven tool, and a detailed description of its modes and use is beyond the scope of this article (see Further reading). In simple terms, it mixes air under pressure with variable oxygen concentrations to provide inspiration and expiration. Each ‘breath’ is characterized by three factors, which can be adjusted by the operator:
-
•
Trigger – the ventilator delivers a breath according to a timer that defines a specific set rate (ventilator-initiated/mandatory breaths), or as a result of the patient's own breathing efforts effecting a change in the pressure or flow in the ventilator circuit (patient-initiated/spontaneous breaths).
-
•
Target – the gas delivered to the lung is set to a specific limit of target flow rate (volume control) or pressure (pressure control, pressure support, bi-level).
-
•
Termination – the signal for the ventilator to finish inspiration and allow expiration (passive) is achieved by setting a specific volume (volume-cycled: volume control), setting a specific time (time-cycled: pressure control/bi-level) or following the reduction of inspiratory flow to a preset level (flow-cycled: pressure support).
Non-invasive ventilation (NIV)
NIV refers to the provision of respiratory support without direct tracheal intubation. This avoids some of the complications inherent with invasive ventilation, such as the need for sedation with risks of haemodynamic instability and subsequent risk of delirium, nosocomial infection, etc. There is increasing usage of NIV, and for some situations it is considered the first-choice mode of ventilatory support (Table 1 ). However, it may not be appropriate for all patients, particularly when used outside of the critical care setting (Table 2 ).
Table 1.
NIV-invasive ventilation to treat acute respiratory failure
| Recommendations based on levels of evidence Level 1 evidence Systematic reviews (with homogeneity) of RCTs and individual RCTs (with narrow CIs) Evidence of use (favourable)
Systematic reviews (with homogeneity) of cohort studies—individual cohort studies (including low-quality RCTs; e.g., <80% follow-up) Evidence of use (favourable)
Systematic reviews (with homogeneity) of case–control studies, individual case–control study Evidence of use (favourable)
Case series (and poor-quality cohort and case–control studies) Evidence of use (favourable)
|
CI, confidence interval; COPD, chronic obstructive pulmonary disease; RCT, randomized controlled trial.
Reprinted from Lancet, vol. 374; 250–259, 2009. Nava S, Hill N, Non-invasive ventilation in acute respiratory failure. With permission from Elsevier.
Table 2.
NIV: indications, contraindications and predictors of failure
|
Indications Clinical observation
| |
Gas exchange
| |
| Contraindications | Potential solution |
| Facial burns, trauma, recent facial upper airway surgery | Rarely a role for NIV – standard therapy is invasive ventilation |
| Vomiting | Treat cause, antiemetics, consider nasogastric tube |
| Upper gastrointestinal surgery | Varies with type of surgery and timing since surgery |
| Copious respiratory secretions | Chest physiotherapy, adequate breaks from NIV (if possible) and treatment of infection – consider early IMV |
| Severe hypoxaemia | HDU/ICU setting – consider early IMV |
| Haemodynamic instability | HDU/ICU setting – consider early IMV |
| Severe co-morbidities | Clearly define the role of NIV/IMV – palliative care may be more appropriate |
| Confusion/agitation | HDU/ICU setting – cautious and controlled pharmacological therapy and appropriate interface. Consider early IMV |
| Low Glasgow Coma Scale score | Patients with a low Glasgow Coma Scale score (<8) due to hypercapnia (particular in COPD), can have a good response to NIV, which is normally seen immediately Do not instigate NIV when invasive ventilation is immediately indicated |
| Unable to protect airway | Consider the above. IMV likely |
| Bowel obstruction | Nasogastric tube drainage and/or surgery – consider early IMV |
| Respiratory arrest | No role for NIV; needs IMV |
|
Predictors of failure of NIV Hypercapnic respiratory failure
| |
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; FiO2, fraction of inspired oxygen; HDU, high-dependency unit; IMV, invasive mechanical ventilation; PaCO2, partial pressure of carbon dioxide; PaO2, partial pressure of oxygen; SAPSII, simplified acute physiology score.
Modern NIV refers almost exclusively to the delivery of positive-pressure ventilation via an external interface. There are six broad types of interface, each with its own particular benefits and drawbacks (see Further reading):
-
•
total face masks (enclose the mouth, nose and eyes)
-
•
full face masks (enclose the mouth and nose)
-
•
nasal masks (cover the nose but not the mouth)
-
•
mouthpieces (placed between the lips and held in place by a lip seal)
-
•
nasal pillows or plugs (inserted into the nostrils)
-
•
helmets or hoods (cover the whole head and all or part of the neck, with no contact with the face).
NIV can be delivered using most modern ‘intensive care’ ventilators. For sicker patients, this has advantages (the ability to deliver higher and precise concentrations of oxygen; separate inspiratory and expiratory limbs minimizing the rebreathing of carbon dioxide; better monitoring and alarm features; rapid access to invasive ventilation). Outside the intensive care unit (ICU), NIV is commonly applied using smaller, portable and ‘simpler’ but increasingly sophisticated ‘non-invasive’ ventilators, which provide a range of respiratory support modes. Pressure-cycled modes are generally preferred (as they can accommodate leaks), and breaths can be either patient-triggered (pressure support or bi-level positive airway pressure), or initiated and controlled by the ventilator (pressure control). The two modes are often used synergistically to provide back-up when triggering is poor, the patient's respiratory rate is unreliable or potential apnoeic episodes need to be covered.
Acute hypercapnic respiratory failure
Patients with acute hypercapnic respiratory acidosis secondary to an acute exacerbation of chronic obstructive pulmonary disease (COPD) represent the most extensively studied group and the group showing the greatest evidence of benefit. Numerous studies and meta-analyses have confirmed that the use of NIV is associated with reduced risk of treatment failure (relative risk (RR) 0.48), lower intubation rates (RR 0.41) with a lower incidence of nosocomial infections, and a reduction in mortality (RR 0.52) with subsequent reduced length of hospital of stay and costs. These benefits have been shown predominantly in patients with mild to moderate hypercapnic respiratory failure (pH 7.30–7.34). NIV should therefore be considered first-line therapy for this group and can be safely used in appropriately staffed and monitored environments outside ICU. However, the use of NIV in patients with more severe respiratory failure1 can still be compatible with favourable outcomes. In such patients, treatment failure is higher, and thus a high-dependency environment should be considered to allow for rapid escalation to intubation and invasive ventilation if appropriate.
The importance of an established structure for effective NIV delivery cannot be overemphasized. Early initiation by experienced and skilled staff, appropriate environments and monitoring, and protocols to aid patient selection and subsequent decision-making are key to the successful and safe application of NIV in all forms of respiratory failure2 (Figure 1 ).
Figure 1.
Stage 1 (pre-NIV), Stage 2 (NIV application) and Stage 3 (treatment progress/adjustment) of NIV therapy.
Although treatment failure is uncommon in mild to moderate respiratory failure, it becomes increasingly frequent in sicker (lower pH and/or significant hypoxaemia) patients (Table 2). Common causes of NIV failure include interface leaks and patient asynchrony with the ventilator (Table 2). In experienced hands, such issues can be recognized early and rapidly remedied; if this is not possible, intubation and invasive ventilation should be considered.2
The appropriateness of invasive ventilation in patients with COPD can be contentious. However, evidence suggests more favourable outcomes than previously predicted, with stable or even improved quality of life for most patients. Decisions about the extent of future intervention should be made by a senior physician, ideally before the initiation of NIV, taking into account factors such as functional status, previous pulmonary function tests, co-morbidities, body mass index, need for long-term oxygen therapy and the patient's expressed wishes. The outcome should be documented in the medical record and communicated to the patient and family as appropriate.
Acute pulmonary oedema
The use of NIV, including continuous positive pressure (CPAP), is advocated as effective first-line treatment for respiratory failure secondary to cardiogenic pulmonary oedema, with an improvement in physiological parameters, reduced intubation rates (RR 0.53) and lower hospital mortality (RR 0.6).3 It should be noted that the true mortality benefit of using NIV or CPAP in these patient groups is still questioned, with positive data only derived from smaller trials.
Hypoxaemic respiratory failure
There is conflicting evidence for the use of NIV in hypoxaemic respiratory failure. Although some studies report improvements in intubation rate, mortality and length of hospital stay with NIV, this is not universal. Differences may be partly due to marked heterogeneity between the study populations in both cause and severity of respiratory failure, in particular in the frequency of pre-existing COPD, for which benefits are very clear. As such, the routine use of NIV in severe pneumonia or acute respiratory distress syndrome (ARDS) is not recommended outside critical care facilities. Although early studies have shown early NIV initiation to be beneficial in the management of hypoxic respiratory failure in immunocompromised patients, this has not been borne out in a recent large multicentre study (IVNIctus4). Again, we would advocate that this is best undertaken in a high-dependency or intensive care environment with rapid access to invasive ventilation and multiorgan support.
NIV in weaning from invasive ventilation
NIV is being increasingly used to promote earlier extubation, prevent reintubation and thus limit exposure to the risks of invasive mechanical ventilation. These benefits are more likely in COPD patients, medical patients with multiple morbidities and those with hypercapnia during spontaneous breathing trials.
NIV in other conditions
With increasing expertise in its usage, clinicians have been keen to exploit the potential benefits of NIV over invasive ventilation in other forms of respiratory compromise (Table 1). However, it is important to recognize that, for some conditions, the literature represents small case series from experienced centres, so the importance of the environment and forward planning is again emphasized. In these circumstances, we recommend that NIV should only be applied in an intensive care setting if invasive mechanical ventilation would be undertaken if NIV treatment failed.
Invasive ventilation
Invasive mechanical ventilation requires access to the trachea, most commonly via an endotracheal tube, and represents the most common reason for admission to ICU. Large multinational surveys confirm the common indications for invasive ventilation to be:
-
•
coma 16%
-
•
COPD 13%
-
•
ARDS 11%
-
•
heart failure 11%
-
•
pneumonia 11%
-
•
sepsis 11%
-
•
trauma 11%
-
•
postoperative complications 11%
-
•
neuromuscular disorders 5%.
Initiation of ventilation in the critically ill
Decisions about the initiation and timing of invasive ventilation can be difficult, and early discussion with critical care colleagues is essential. Appropriateness of ventilatory support can also require advanced discussion with patients and families.
Once a decision to intubate has been made, the transition from an awake and self-ventilating patient to controlled invasive ventilation can be very challenging in critically ill individuals. Most patients will have evidence of developing or established organ dysfunction, particularly cardiovascular dysfunction (ischaemic heart disease, sepsis), and such patients are commonly hypovolaemic. Both anaesthetic induction agents and positive-pressure ventilation (which decreases venous return) produce cardiovascular depression, and peri-intubation hypotension is common. In addition, cessation of spontaneous ventilation can lead to very rapid desaturation in such patients because of their marginal respiratory reserve and circulatory problems. These consequences must be anticipated and require early involvement of an experienced member of the critical care team, ideally in an appropriately equipped area of the hospital.
Descriptions of individual ventilatory strategies are beyond the scope of this chapter. However, over the past 10–20 years there has been increasing recognition that, although it is life-saving, invasive ventilation is associated with significant complications, such as nosocomial pneumonia, delirium and critical illness neuromyopathy; it can be associated with propagation of underlying lung injury and subsequent worsening of multiorgan failure. Recent studies examining both ventilator-specific and general management strategies have concentrated on mitigating these potential harmful effects to form the basis for the management of patients with hypoxaemic respiratory failure. Although individual patients differ, key concepts are outlined below.
Ventilator-specific strategies
-
•
Low tidal volume (6 ml/kg ideal bodyweight) and avoidance of high inspiratory pressures (P plat <30) to minimize the risk of volutrauma.
-
•
Reduced arterial oxygenation saturation (SaO2) targets 88–95% and reduced partial pressure of arterial oxygen (PaO2) 7.5–10.5 kPa – ‘permissive hypoxia’.
-
•
Acceptance of mild to moderate respiratory acidosis – ‘permissive hypercapnia’.
-
•
Greater use of positive end-expiratory pressure (PEEP), particularly in more severe hypoxaemia (Note that PEEP should be used cautiously and may be contraindicated in expiratory airflow limitation, i.e. COPD.)
-
•
Early use of neuromuscular blockade in severe cases.
-
•
Prone positioning in severe cases.
General strategies
-
•
Avoidance of excessive fluid administration.
-
•
Minimizing sedation once the acute insult has settled – daily sedation holds (interruptions of sedation), use of sedation scores.
-
•
Daily trials of spontaneous breathing and protocolized weaning once the initial insult has resolved.5
-
•
Early and appropriate nutritional support.
-
•
Prophylaxis against venous thromboembolism.
-
•
Stress ulcer prophylaxis.
-
•
Rehabilitation during and following critical illness (as per National Institute for Health and Care Excellence guidelines).
More recently, attention has turned to the use of extracorporeal support in patients with extreme abnormalities of gas exchange. The CESAR (Conventional Ventilation or ECMO for Severe Adult Respiratory Failure) study, in which transfer to a centre capable of delivering extracorporeal membrane oxygenation (ECMO) was associated with improved outcome (death, disability) at 6 months, and the high-profile success of ECMO in the H1N1 influenza pandemic, has resulted in a resurgence of interest in this technique. Simpler forms of extracorporeal support exist for when hypercapnia is the predominant problem. Studies are ongoing to establish whether such therapies have a role in further mitigating the injurious effects of invasive ventilation in patients with ARDS, avoiding invasive ventilation in patients with COPD failing NIV and weaning patients from longer term mechanical ventilation. The development of these and other specialist techniques has promoted the establishment of advanced respiratory support centres to manage the sickest patients in many countries, including the UK.
Key references
- 1.Crummy F., Buchan C., Miller B., Toghill J., Naughton M.T. The use of noninvasive mechanical ventilation in COPD with severe hypercapnic acidosis. Respir Med. 2007;101:53–61. doi: 10.1016/j.rmed.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Nava S., Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–259. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vital F.M., Saconato H., Ladeira M.T. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2013 May 31;5:CD005351. doi: 10.1002/14651858.CD005351.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Lemiale V., Resche-Rigon M., Azoulay E., Study Group for Respiratory Intensive Care in Malignancies Groupe de Recherche en Reanimation Respiratoire du patient d'Onco-Hematologie Early non-invasive ventilation for acute respiratory failure in immunocompromised patients (IVNIctus): study protocol for a multicenter randomized controlled trial. Trials. 2014;15:372. doi: 10.1186/1745-6215-15-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blackwood B., Alderdice F., Burns K., Cardwell C., Lavery G., O'Halloran P. Use of weaning protocols for reducing duration of mechanical ventilation in critically ill adult patients: cochrane systematic review and meta-analysis. Br Med J. 2011;342:c7237. doi: 10.1136/bmj.c7237. [DOI] [PMC free article] [PubMed] [Google Scholar]