Abstract
Background
Five known human coronaviruses infect the human respiratory tract: HCoV-OC43, HCoV-229E, SARS-CoV, HCoV-NL63 and HCoV-HKU1.
Objectives
To evaluate the prevalence of HCoV-NL63 in hospitalized adult patients and to perform molecular characterization of Italian strains.
Study Design
HCoV-NL63 was sought by RT-PCR in 510 consecutive lower respiratory tract (LRT) samples, collected from 433 Central-Southern Italy patients over a 1-year period. Phylogenetic analysis was performed by partial sequencing of S and ORF1a. Additional S sequences from Northern Italy were included in the phylogenetic trees.
Results
HCoV-NL63 was detected in 10 patients (2.0%) with symptomatic respiratory diseases, mainly during winter. Phylogenetic analysis indicated a certain degree of heterogeneity in Italian isolates. The ORF1a gene clustering in phylogenetic trees did not match with that of the S gene.
Conclusions
As observed by others, HCoV-NL63 is often associated with another virus. Phylogenetic characterization of HCoV-NL63 circulating in Italy indicates that this virus circulates as a mixture of variant strains, as observed in other countries.
Abbreviations: CoV, coronavirus; SARS, severe acute respiratory syndrome; hCoV, human coronavirus; LRT, lower respiratory tract; S, spike; SP, sputum; BAL, bronchoalveolar lavage; EA, endotracheal aspirates; FLU, influenzavirus; hMPV, human metapneumovirus; AdV, adenovirus; PIV, parainfluenzavirus; RSV, respiratory syncytial virus; HRV, Human rhinoviruses; BP, bronchopneumonia; COPD, chronic obstructive pulmonary disease; CAP, community-acquired pneumonia; ARF, acute respiratory failure; RF, respiratory failure
Keywords: Human coronaviruses, HCoV-NL63, Lower respiratory tract infection, Phylogenetic analysis
1. Introduction
Coronaviruses (CoVs) are large, enveloped RNA viruses of both medical and veterinary importance. Five human CoVs (HCoVs) are known to infect the human respiratory tract: HCoV-OC43, HCoV-229E (Vabret et al., 2001), SARS-CoV (Peiris et al., 2003), HCoV-NL63 (Fouchier et al., 2004; van der Hoek et al., 2004) and HCoV-HKU1 (Woo et al., 2005).
HCoVs are divided into three distinct groups (van der Hoek et al., 2006; Virus taxonomy, VIIIth report of the ICTV): group 1, including HCoV-229E and HCoV-NL63; group 2, including HCoV-OC43, HCoV-HKU1 and SARS-CoV; group 3 CoVs, including mainly avian viruses.
HCoVs represent the second most frequent causes of common cold and upper respiratory tract infections, after rhinoviruses (Mäkelä et al., 1998). Particularly, HCoV-NL63 can be recovered from the lower respiratory tract (LRT) specimens of patients with pneumonia or LRT complications, mainly involving young infants, and immunocompromised persons (Gagneur et al., 2002, Garbino et al., 2006, Gerna et al., 2006, van der Hoek et al., 2006, Wu et al., 2008). HCoV-NL63 can be considered as a new important cause of respiratory illness, although the available data mainly refer to pediatric populations (Arden et al., 2005, Bastien et al., 2005b, Boivin et al., 2005, Chiu et al., 2005, Ebihara et al., 2005, Kuypers et al., 2007, Moës et al., 2005).
Based on phylogenetic analysis of different genome regions, several subtypes, currently co-circulating in the human population, have been identified in France, Canada, Australia, Belgium, Netherlands, Sweden, China and Korean (Arden et al., 2005, Bastien et al., 2005a, Chiu et al., 2005, Han et al., 2007, Koetz et al., 2006, Moës et al., 2005, Vabret et al., 2005, van der Hoek et al., 2004).
We investigated the prevalence of HCoV-NL63 in samples from the LRT of hospitalized adult patients. Molecular characterization was performed by sequencing a fragment of the spike (S) and of ORF1a genes.
2. Methods
A total of 510 consecutive LRT samples, including 329 sputums (SP), 165 endotracheal aspirates (EA) and 16 bronchoalveolar lavages (BAL), were collected from 433 adult patients, admitted to three Italian hospitals, during April 2004–May 2005.
All specimens were screened with a molecular panel for detecting 12 respiratory viruses. Of the 510 samples tested, 220 (43.1%) were positive for one respiratory virus and 33 (6.5%) were positive for more than one virus. The detailed prevalence for each of these pathogens is published elsewhere (Minosse et al., 2008).
HCoV-NL63 was detected by nested RT-PCR, targeting a 237 bp fragment of the ORF1b (van der Hoek et al., 2004). As a positive control, a clinical sample positive for HCoV-NL63 by RT-PCR and confirmed by sequence analysis, was used. As negative controls, water and a nasopharyngeal swab from an individual without respiratory symptoms were used in each analytical session. The sensitivity of our RT-PCR protocol, established by probit analysis of serial replicate dilutions of a plasmid containing the RT-PCR amplicon as the insert, was 1 copy/reaction, corresponding to 42 copies/ml of the starting sample. The RT-PCR assay was validated through participation in an external quality assessment (QCMD 2006 Rhinovirus & Coronavirus RNA EQA Pilot Study, Glasgow, UK), where HCoV-NL63 was detected in all positive samples included in the panel.
For phylogenetic analysis, two different genomic regions were amplified and sequenced: a 523 bp fragment of S gene and a 525 bp fragment of ORF1a, by using primers previously described (Bastien et al., 2005a, Vabret et al., 2005).
3. Results
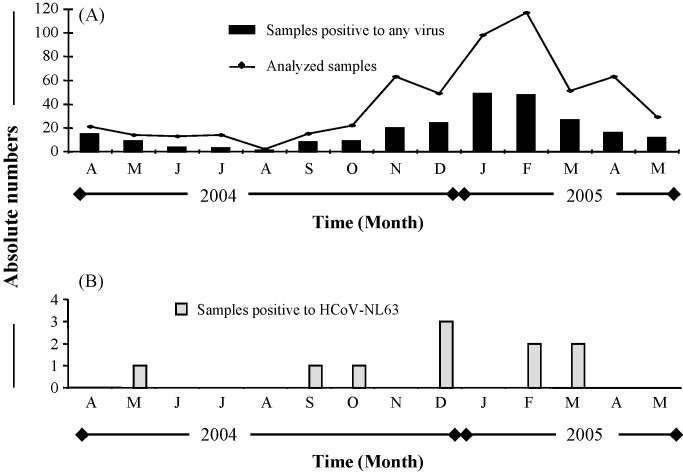
The age of the 433 patients included in the study ranged from 15 to 93 years, mean (±S.D.): 56.3 (18.2) years, median (IQR): 57.0 (41.0–72.0) years. Temporal distribution of samples collected over the 1-year study period is shown in Fig. 1 . HCoV-NL63 was detected in 10 (2.0%) of 510 samples. Of the 10 positive samples, 3 were co-infected with human rhinovirus (HRV) and 1 with adenovirus (see Table 1 ). Demographic and clinical characteristics of positive cases are reported in Table 1. The overall frequency of HCoV-NL63 infected patients was equally distributed between genders. The age of HCoV-NL63 positive patients ranged from 29 to 85 years (mean ± S.D. was 60.1 [18.3] years; median IQR was 64.5 [41.5–76.0] years). All patients were symptomatic, and had clinically relevant respiratory diseases, including bronchopneumonia, chronic obstructive pulmonary disease, community-acquired pneumonia, and acute respiratory failure. Three patients were in the intensive care unit and needed mechanical ventilation; two patients were immunosuppressed, due to solid organ tumour or HIV infection.
Fig. 1.
Monthly distribution of positivity to respiratory viruses and to HCoV-NL63 during the period April 2004–May 2005. (A) Solid line: number of analyzed samples; bars: samples positive to any of 12 tested viruses. (B) Bars: samples positive to HCoV-NL63.
Table 1.
Demografic and clinical characteristics of patients with HCoV-NL63 infection
| Patient | Age | Sex | Sample date | Specimen* | Symptoms | Respiratory diagnosis** | Immunosoppression | Mechanical ventilation |
|---|---|---|---|---|---|---|---|---|
| R1 | 40 | – | 22 02 05 | SP | Fever, dyspnea, productive cough | BP | Yes (HIV, stage B2) | No |
| R2 | 80 | M | 14 02 05 | SP | Dyspnea, productive cough | COPD | No | |
| R3a | 53 | F | 5 03 05 | SP | Fever | BP | No | |
| R4 | 62 | F | 19 05 04 | SP | Dyspnea, chill, productive cough | COPD | No | |
| R5 | 67 | M | 18 03 05 | SP | Dyspnea, productive cough | COPD, pulmonary emphysema | No | |
| R6b | 70 | M | 27 07 04 | EA | Dyspnea, headache | CAP, ARF, COPD | Yes (solid tumour) | Yes |
| R7 | 29 | M | 18 10 04 | EA | Dyspnea | ARF | Yes | |
| R8 | 43 | F | 14 12 04 | SP | Fever | BP | No | |
| R9b | 72 | F | 17 12 04 | SP | Fever, dyspnea, productive cough | RF, COPD | No | |
| R10b | 85 | M | 27 12 04 | EA | Fever, dyspnea, productive cough | ARF, acute pulmonary oedema, | Yes |
SP, sputum; EA, endotracheal aspirate.
BP, Bronchopneumonia; COPD, Chronic Obstructive Pulmonary Disease; CAP, community-acquired pneumonia; ARF, acute respiratory failure; RF, respiratory failure.
Positive for AdV.
Positive for HRV.
Only 5 of 10 positive samples had sufficient material to allow for genetic characterization. Sequence analysis of the S and ORF1a gene fragments showed 97–99% similarity to the prototype HCoV-NL63 1988 and 2003 Netherland isolates (GenBank accession numbers: AY567487, AY518894). As expected, the phylogenetic tree built on ORF1a contained two clusters: 4 out of the 5 of Italian isolates were included in cluster 1, while one isolate (R3) had the characteristics of an outlier (Fig. 2 ). The phylogenetic analysis of S gene nucleotide sequences is shown in Fig. 3 . Besides the 5 patients described in Fig. 2 (indicated as Southern-Central Italy), 7 additional patients identified in Pavia (indicated as Northern Italy) had S gene sequence data available, and were included in this analysis, together with 12 French isolates and 2 prototype isolates whose sequences were available in GenBank. From this tree it was not possible to identify any cluster with bootstrap values >80. However, one of the Italian isolates (PV5) was included in a subcluster with the French isolate AY994247 (bootstrap values = 78; Fig. 3), that was proposed to be an outlier by Vabret et al. (2005).
Fig. 2.
Phylogenetic analysis of the partial ORF1a nucleotide sequences of HCoV-NL63 isolates from Southern-Central Italy. A region spanning nt position 5844 to 6169 of the reference strain AY518894 was analyzed. Italian isolates are in bold character. The nucleotide sequences of 2 prototype HCoV-NL63 sequences available in GenBank (AY567487 and AY518894, indicated as HCoV-NL63 1988 and HCoV-NL 2003, respectively) were included in the analysis. HCoV-229E was used as an outgroup. Bootstrap analysis with 500 replicates was performed to assess the significance of the nodes; values greater than 80% were considered significant. The ORF1a nucleotide sequences from the 5 strains of HCoV-NL63 from Southern-Central Italy have been lodged in the GenBank sequence database under accession no. EU030684, EU030685, EU125188 to EU1250190.
Fig. 3.
Phylogenetic analysis of the S gene nucleotide sequences of HCoV-NL63 isolates from Southern-Central and Northern Italy. A region spanning nt position 22567 to 23039 of the reference strain AY518894 was analyzed. Italian isolates are in bold character. The nucleotide sequences of 2 prototype HCoV-NL63 sequences available in GenBank (AY567487 and AY518894, indicated as HCoV-NL63 1988 and HCoV-NL 2003, respectively) were included in the analysis. HCoV-229E was used as an outgroup. Bootstrap analysis with 500 replicates was performed to assess the significance of the nodes; values greater than 80% were considered significant. The S nucleotide sequences from the 5 strains of HCoV-NL63 from Southern-Central Italy have been lodged in the GenBank sequence database under accession no. EU025124 to EU025128.
The phylogenetic analysis of the predicted amino acid sequences for the analyzed S and ORF1a gene fragments was consistent with that based on nucleotide sequences (not shown).
4. Discussion
Generally, HCoV-229E and HCoV-OC43 cause disease much like the common cold, but they have also been associated with more severe LRT conditions, especially in weakened patients (Kuypers et al., 2007, Pene et al., 2003, Vabret et al., 2001). The spectrum of clinical symptoms associated with HCoV-NL63 infection still needs to be determined.
In this study, we detected HCoV-NL63 in 2.0% of hospital-based adult patients with LRT diseases. This frequency is consistent with prevalence data from previous studies, ranging from 1.0% to 9.3% (Arden et al., 2005, Bastien et al., 2005a, Bastien et al., 2005b, Chiu et al., 2005, Ebihara et al., 2005, Kaiser et al., 2005, Kuypers et al., 2007, Moës et al., 2005, Suzuki et al., 2005, Vabret et al., 2005, van der Hoek et al., 2005). Due to the lack of matched healthy subjects for comparison, it is not possible to attribute any causal role to HCoV-NL63 in LRT diseases. Nevertheless, the following points can be derived from our results: (a) HCoV-NL63 was detected in LRT secretions of a small number of adult patients with clinically overt LRT disease; however, it is not possible to rule out that the virus detected could actually derive from contamination by upper respiratory tract secretions; (b) HCoV-NL63 is often combined with other respiratory viruses, in agreement with previous data (van der Hoek et al., 2006); in fact, 3 out 10 HCoV-NL63 positive samples were co-infected with HRV and 1 with adenovirus; these findings raise the possibility that HCoV-NL63 may be only a bystander virus present in people with LRT disease due to other causative agents, rather than directly being involved in the disease aetiology; in addition, our numbers are too low to draw any conclusion on the role of immunosuppression on prevalence and clinical presentation of HCoV-NL63 infection; (c) temporal distribution of HCoV-NL63 positive samples (Fig. 1) is consistent with winter seasonality of the infection, as previously reported (Arden et al., 2005, Bastien et al., 2005a, Ebihara et al., 2005, Moës et al., 2005, Vabret et al., 2005, van der Hoek et al., 2005).
Recent reports indicate that HCoV-NL63 has a worldwide distribution. Sequence data from Australia, Japan, Canada, France, Belgium, and the Netherlands indicate that this virus circulates as a mixture of variants, without a specific geographical segregation (van der Hoek et al., 2006). In fact, RNA viruses have an enormous potential to generate genetic diversity due to their high mutation rates. As a consequence, HCoV-NL63, like other RNA viruses, may exist as a dynamic distribution of closely related variants.
This report shows the phylogenetic characterization of HCoV-NL63 circulating in Italy. The results, based on two different genomic regions (a portion of the S gene and of ORF1a), shows a certain degree of heterogeneity in Italian isolates, suggesting that different subtypes may be currently co-circulating, as observed in other countries (France, Netherlands, Australia, Canada, and Belgium), without the emergence of geographically distinct clusters (Moës et al., 2005, Vabret et al., 2005, van der Hoek et al., 2006).
In agreement with literature data, the clustering based on the ORF1a gene does not match with that of the S gene. As suggested in other reports, recombination occurring between different HCoV-NL63 isolates may account for this finding (Pyrc et al., 2007, Moës et al., 2005, van der Hoek et al., 2006).
Acknowledgments
This work was supported in part by grants from the Italian Ministry of Health (Fondi Ricerca Corrente, Ricerca Finalizzata, and “Fondi per la creazione di un polo centralizzato per la crioconservazione”) to INMI “L. Spallanzani”, and RF [grant 89282(05)/A] and RC (grant 80557) to Fondazione IRCCS “Policlinico San Matteo”. Neither funding source influenced the design, conduct or reporting of this study.
We acknowledge the enthusiastic contribution of M. Visca and M. Cava, who assisted in clinical investigation and collaborated with sample and data collection.
References
- Arden K.E., Nissen M.D., Sloots T.P., Mackay I.M. New human coronavirus, HCoV-NL63, associated with severe lower respiratory tract disease in Australia. J Med Virol. 2005;75(March (3)):455–462. doi: 10.1002/jmv.20288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien N., Anderson K., Hart L., Van Caeseele P., Brandt K., Milley D. Human coronavirus NL63 infection in Canada. J Infect Dis. 2005;191(February 15 (4)):503–506. doi: 10.1086/426869. [Epub 2005 January 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien N., Robinson J.L., Tse A., Lee B.E., Hart L., Li Y. Human coronavirus NL-63 infections in children: a 1-year study. J Clin Microbiol. 2005;43(September (9)):4567–4573. doi: 10.1128/JCM.43.9.4567-4573.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin G., Baz M., Côté S., Gilca R., Deffrasnes C., Leblanc E. Infections by human coronavirus-NL in hospitalized children. Pediatr Infect Dis J. 2005;24(December (12)):1045–1048. doi: 10.1097/01.inf.0000183743.68569.c7. [DOI] [PubMed] [Google Scholar]
- Chiu S.S., Chan K.H., Chu K.W., Kwan S.W., Guan Y., Poon L.L. Human coronavirus NL63 infection and other coronavirus infections in children hospitalized with acute respiratory disease in Hong Kong, China. Clin Infect Dis. 2005;40(January 15 (12)):1721–1729. doi: 10.1086/430301. [Epub 2005 May 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara T., Endo R., Ma X., Ishiguro N., Kikuta H. Detection of human coronavirus NL63 in young children with bronchiolitis. J Med Virol. 2005;75(March (3)):463–465. doi: 10.1002/jmv.20289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauquet CM, editor. Virus taxonomy VIIIth report of the International Committee on taxonomy of viruses.
- Fouchier R.A., Hartwig N.G., Bestebroer T.M., Niemeyer B., de Jong J.C., Simon J.H., Osterhaus A.D. A previously undescribed coronavirus associated with respiratory disease in humans. Proc Natl Acad Sci USA. 2004;101(April 20 (16)):6212–6216. doi: 10.1073/pnas.0400762101. [Epub 2004 April 8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneur A., Sizun J., Vallet S., Legr M.C., Picard B., Talbot P.J. Coronavirus-related nosocomial viral respiratory infections in a neonatal and paediatric intensive care unit: a prospective study. J Hosp Infect. 2002;51(May (1)):59–64. doi: 10.1053/jhin.2002.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbino J., Crespo S., Aubert J.D., Rochat T., Ninet B., Deffernez C. A prospective hospital-based study of the clinical impact of non-severe acute respiratory syndrome (Non-SARS)-related human coronavirus infection. Clin Infect Dis. 2006;43(October 15 (8)):1009–1015. doi: 10.1086/507898. [Epub 2006 September 13] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerna G., Campanini G., Rovida F., Percivalle E., Sarasini A., Marchi A. Genetic variability of human coronavirus OC43-, 229E-, and NL63-like strains and their association with lower respiratory tract infections of hospitalized infants and immunocompromised patients. J Med Virol. 2006;78(July (7)):938–949. doi: 10.1002/jmv.20645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han T.H., Chung J.Y., Kim S.W., Hwang E.S. Human Coronavirus-NL63 infections in Korean children, 2004–2006. J Clin Virol. 2007;38(January (1)):27–31. doi: 10.1016/j.jcv.2006.10.009. [Epub 2006 November 29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser L., Regamey N., Roiha H., Deffernez C., Frey U. Human coronavirus NL63 associated with lower respiratory tract symptoms in early life. Pediatr Infect Dis J. 2005;24(November (11)):1015–1017. doi: 10.1097/01.inf.0000183773.80217.12. [DOI] [PubMed] [Google Scholar]
- Koetz A., Nilsson P., Lindén M., van der Hoek L., Ripa T. Detection of human coronavirus NL63, human metapneumovirus and respiratory syncytial virus in children with respiratory tract infections in south-west Sweden. Clin Microbiol Infect. 2006;12(November (11)):1089–1096. doi: 10.1111/j.1469-0691.2006.01506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuypers J., Martin E.T., Heugel J., Wright N., Morrow R., Englund J.A. Clinical disease in children associated with newly described coronavirus subtypes. Pediatrics. 2007;119(January (1)):e70–e76. doi: 10.1542/peds.2006-1406. [Epub 2006 November 27] [DOI] [PubMed] [Google Scholar]
- Mäkelä M.J., Puhakka T., Ruuskanen O., Leinonen M., Saikku P., Kimpimäki M. Viruses and bacteria in the etiology of the common cold. J Clin Microbiol. 1998;36(February (2)):539–542. doi: 10.1128/jcm.36.2.539-542.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minosse C., Selleri M., Zaniratti M.S., Cappiello G., Longo R., Schifano E. Frequency of detection of respiratory viruses in the lower respiratory tract of hospitalized adults. J Clin Virol. 2008;(March 13) doi: 10.1016/j.jcv.2008.01.012. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moës E., Vijgen L., Keyaerts E., Zlateva K., Li S., Maes P. A novel pancoronavirus RT-PCR assay: frequent detection of human coronavirus NL63 in children hospitalized with respiratory tract infections in Belgium. BMC Infect Dis. 2005;5(February (1) 1):6. doi: 10.1186/1471-2334-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris J.S. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361(April 19 (9366)):1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pene F., Merlat A., Vabret A., Rozenberg F., Buzyn A., Dreyfus F. Coronavirus 229E-related pneumonia in immunocompromised patients. Clin Infect Dis. 2003;37(October 1 (7)):929–932. doi: 10.1086/377612. [Epub 2003 September 8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyrc K., Berkhout B., van der Hoek L. The novel human coronaviruses NL63 and HKU1. J Virol. 2007;81(April (7)):3051–3057. doi: 10.1128/JVI.01466-06. [Epub 2006 November 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki A., Okamoto M., Ohmi A., Watanabe O., Miyabayashi S., Nishimura H. Detection of human coronavirus-NL63 in children in Japan. Pediatr Infect Dis J. 2005;24(July (7)):645–646. doi: 10.1097/01.inf.0000168846.71517.ee. [DOI] [PubMed] [Google Scholar]
- Vabret A., Mouthon F., Mourez T., Gouarin S., Petitjean J., Freymuth F. Direct diagnosis of human respiratory coronaviruses 229E and OC43 by the polymerase chain reaction. J Virol Methods. 2001;97(September (1–2)):59–66. doi: 10.1016/S0166-0934(01)00343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vabret A., Mourez T., Dina J., van der Hoek L., Gouarin S., Petitjean J. Human coronavirus NL63, France. Emerg Infect Dis. 2005;11(August (8)):1225–1229. doi: 10.3201/eid1108.050110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Hoek L., Pyrc K., Jebbink M.F., Vermeulen-Oost W., Berkhout R.J., Wolthers K.C. Identification of a new human coronavirus. Nat Med. 2004;10(April (4)):368–373. doi: 10.1038/nm1024. [Epub 2004 March 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Hoek L., Sure K., Ihorst G., Stang A., Pyrc K., Jebbink M.F. Croup is associated with the novel coronavirus NL63. PLoS Med. 2005;2(August (8)):e240. doi: 10.1371/journal.pmed.0020240. [Epub 2005 August 23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Hoek L., Pyrc K., Berkhout B. Human coronavirus NL63, a new respiratory virus. FEMS Microbiol Rev. 2006;30(September (5)):760–773. doi: 10.1111/j.1574-6976.2006.00032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo P.C., Lau S.K., Chu C.M., Chan K.H., Tsoi H.W., Huang Y. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol. 2005;79(January (2)):884–895. doi: 10.1128/JVI.79.2.884-895.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P.S., Chang L.Y., Berkhout B., van der Hoek L., Lu C.Y., Kao C.L. Clinical manifestations of human coronavirus NL63 infection in children in Taiwan. Eur J Pediatr. 2008;167(January (1)):75–80. doi: 10.1007/s00431-007-0429-8. [Epub 2007 February 13] [DOI] [PMC free article] [PubMed] [Google Scholar]