Highlights
-
•
Coronaviruses employ versatile mechanisms to evade sensing of viral RNA.
-
•
Cap-methylation of viral RNA facilitates innate immune evasion.
-
•
There is increasing evidence that virus-encoded ribonucleases impact innate immune responses.
Abstract
An essential function of innate immunity is to distinguish self from non-self and receptors have evolved to specifically recognize viral components and initiate the expression of antiviral proteins to restrict viral replication. Coronaviruses are RNA viruses that replicate in the host cytoplasm and evade innate immune sensing in most cell types, either passively by hiding their viral signatures and limiting exposure to sensors or actively, by encoding viral antagonists to counteract the effects of interferons. Since many cytoplasmic viruses exploit similar mechanisms of innate immune evasion, mechanistic insight into the direct interplay between viral RNA, viral RNA-processing enzymes, cellular sensors and antiviral proteins will be highly relevant to develop novel antiviral targets and to restrict important animal and human infections.
Current Opinion in Microbiology 2014, 20:69–75
This review comes from a themed issue on Host–microbe interactions: viruses
Edited by Maria-Carla Saleh
For a complete overview see the Issue and the Editorial
Available online 5th June 2014
http://dx.doi.org/10.1016/j.mib.2014.05.005
1369-5274/© 2014 Elsevier Ltd. All rights reserved.
Introduction
Our immune system functions as a collaborative network of cells, lymphoid organs, cytokines and humoral factors, to combat infections caused by pathogenic agents such as bacteria, parasites and viruses [1]. The first line of host defence consists of innate immunity, which is evolutionary conserved, and has the main task to limit replication and spread of pathogens [2]. This response is then complemented by adaptive immunity, which develops more gradually and relies on lymphocytes that recognize antigenic structures on the surface of pathogens that managed to pass through the epithelium [1].
The emphasis of this present review lies on Coronaviruses (CoVs), which are positive-stranded RNA viruses of both veterinary and medical importance causing mainly respiratory and enteric diseases. Human CoV-infections usually present as mild respiratory tract disease (common cold) that may be more severe in elderly or immune-compromised individuals. However, the epidemic in 2002/03 caused by the severe acute respiratory syndrome-associated CoV (SARS-CoV) and the recently discovered Middle East Respiratory Syndrome coronavirus (MERS-CoV) demonstrate the zoonotic potential of CoVs and their ability to seriously impact human health [3, 4•, 5].
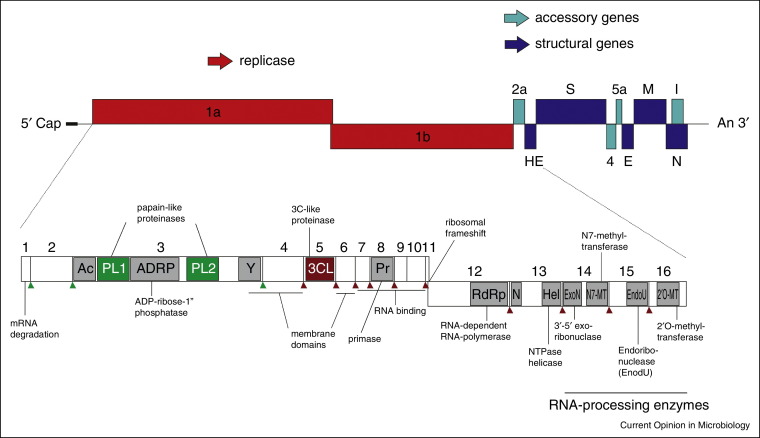
Coronavirus innate immune evasion
CoVs belong to the order Nidovirales and are characterized by a large single-stranded (ss) RNA genome of positive polarity and a complex replication cycle [3, 6••]. Upon entry into host cells the viral genome is uncoated and primary translation results in the synthesis of two large polyproteins pp1a and pp1ab that are co-translationally and post-translationally cleaved by viral proteases into 16 non-structural proteins (nsp 1–16) (Figure 1 ). These CoV nsps form the replication/transcription complex (RTC) that is responsible for the synthesis the viral RNA, the major CoV pathogen-associated molecular pattern (PAMP) recognized by host cell pathogen-recognition receptors (PRRs). Most PRRs responsible of sensing viruses are either located in the endosomes (e.g. Toll-like receptors; TLRs) [7] or in the cytosol (e.g. retinoic acid inducible gene I (RIG-I)-like receptors; RLRs) [8, 9], suggesting that viruses are primarily detected by the presence of their nucleic acids. Sensing of PAMPs by PRRs results in their activation and ultimate expression of numerous cytokines, including interferons (IFNs). IFNs in turn induce the expression of a broad array of IFN-stimulated genes (ISGs) to establish an antiviral state.
Figure 1.
Coronavirus genome organization. Schematic representation of the MHV genome and ORFs encoding for replicase (red boxes), structural (dark blue boxes) and accessory proteins (cyan boxes). Specific replicase domains and functions, including ExoN, N7-MTase, EndoU, and 2′O-MTase are depicted. Arrows represent polyprotein cleavage sites of papain-like proteinases (PL1 and PL2 proteinase; green) and chymotrypsin-like proteinase (3C-L proteinase; red).
Much of our current understanding concerning CoV-induced innate immune responses results from studies using mouse hepatitis virus (MHV) in the context of a murine model of infection. Upon MHV infection, plasmacytoid dendritic cells (pDCs) rapidly secrete high amounts of IFN-α mediated through TLR7 stimulation and constitutively expressed IFN-regulatory factor (IRF) 7 [10]. Considerably lower levels of type-I IFNs are produced by other cell types, such as macrophages, microglia and oligodendrocytes [11, 12, 13]. pDC-derived Type-I IFN is particularly important to protect cells that fail to raise a significant IFN-response during CoV-infections and thus secures their integrity and efficiently reduces virus replication and spread [14]. Remarkably, human CoVs (HCoVs) infection in human airway epithelial cells (HAEs), the primary target tissue at the entry port of respiratory pathogens, did not result in upregulation of IFNs or inflammatory cytokines, although these cells readily respond to exogenous type-I and type-III IFN [4•]. In line, SARS-CoV and MERS-CoV did not induce a pronounced IFN-response in polarized airway epithelial cells (Calu-3) [15, 16], in A549 cells (human alveolar adenocarcinoma cell line) and in human monocyte-derived macrophages [17]. Collectively, these data suggest that CoVs efficiently evade innate immune sensing in other cell types than pDCs, either passively, by hiding PAMPs, or actively, by encoding viral antagonists to counteract induction of IFN expression.
Mimicking cellular mRNAs
To distinguish host cell-derived from viral mRNAs, PPRs have evolved to specifically recognize foreign, or ‘non-self’, RNAs. The cap structure present at 5′-termini of eukaryotic mRNAs has a pivotal role in this context, as uncapped RNA bearing a 5′ triphosphate terminus, and RNA with a non-methylated or incompletely methylated cap structure are now considered as viral PAMPs. In addition, double-stranded (ds) RNA is a long known viral PAMP, since replication of RNA virus genomes involves so-called replicative intermediates consisting of dsRNA. The cytosolic RLRs RIG-I and melanoma-differentiation-associated protein 5 (MDA5) sense viral RNAs, however RIG-I preferentially senses short blunt-end or 5′ triphosphate RNAs [8, 9], while MDA5 recognizes cap0-structures (i.e. cap structures lacking ribose 2′O methylation) [18••] and long dsRNAs [8, 19]. Host cell mRNAs are usually not recognized by RLRs, since already in the nucleus their nascent 5′ triphosphate-end is co-transcriptionally modified to form a N7-methylated and 2′O-methylated 5′ cap structure [20••].
Many viruses that replicate in the cytoplasm have thus evolved mechanisms to provide a cap structure at the 5′ ends of their mRNAs in order to evade RLR recognition and to ensure eukaryotic translation. The acquisition of a cap structure is most efficiently done by either hijacking the cellular capping machinery, by snatching caps from cellular mRNAs or by encoding viral capping enzymes [20••]. CoV RNAs contain a 5′ cap structure [18••] and the CoV-RTC harbours capping enzymes such as a RNA-triphosphatase encoded by nsp13 [21], a N7-Methyltransferase (N7-MTase) residing in nsp14 [22] and a 2′O-MTase encoded by nsp16 [23].
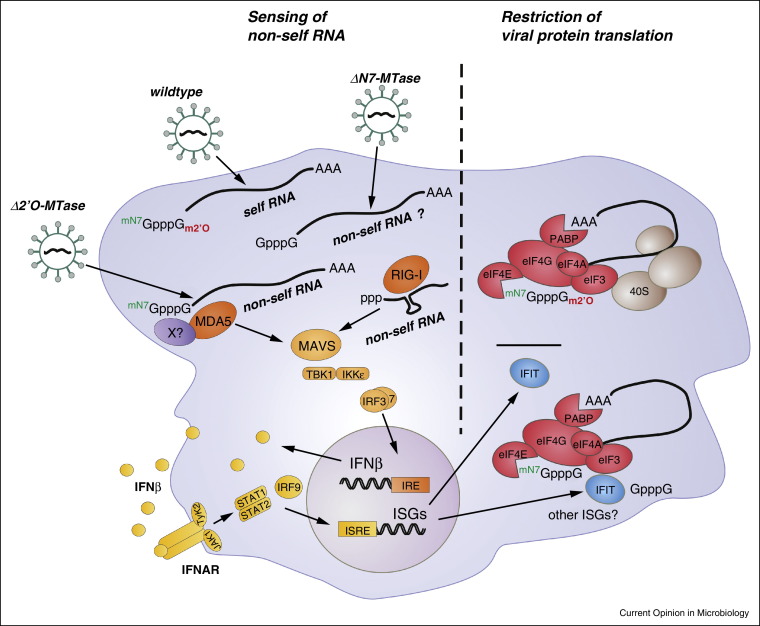
Detailed analyses including 2′O-MTase-deficient Coronaviruses, Flaviviruses and Poxviruses congruently demonstrated that 2′O-methylation of viral RNA increases virulence through evasion from innate immune responses (Figure 2 ). Recombinant 2′O-MTase-deficient MHV elicited an elevated type-I IFN-response in wildtype, but not in MDA5-deficient, macrophages, indicating that 2′O-methylation of viral RNA protects from recognition by MDA5 [18••]. Additionally, 2′O-MTase deficient viruses are more sensitive to the antiviral actions of IFN, suggesting that specific ISG(s) may explicitly restrict replication of viruses lacking 2′O-methylation [24]. Indeed, IFIT1 (IFN-induced-protein-with-tetratricopeptide-repeats-1) was shown to preferentially bind to cap0-RNA (i.e. lacking 2′O-methylation) and thereby impairs the attachment of eukaryotic initiation factors (eIFs) to the viral template, which will ultimately result in translation arrest [25••]. IFIT1 apparently has only marginal effects on replication and virulence of wildtype viruses [18••, 24, 25••]. However, replication of MHV-mutants, West-Nile-Virus-mutants, and vaccinia virus-mutants lacking 2′O-methylation was restricted in wildtype macrophages, but restored in IFIT1-deficient macrophages [18••, 24, 25••]. Interestingly, the ability of IFIT1 to restrict replication of West Nile Viruses lacking 2′O-methylation was highly cell-type specific and revealed that additional mechanisms independent of IFIT1 are involved in control of the infection [26].
Figure 2.
Host innate immune responses to coronaviral methyltransferase-deficient mutants. Sensing of non-self RNA: CoVs lacking 2′O-MTase-activity induce a MDA5-dependent expression of type-I IFN in macrophages, indicating the 2′O-methylation on viral RNAs provides a signature that classifies these RNAs as ‘self’ RNAs. Since direct binding of MDA5 to capped RNA lacking 2′O-methylation (i.e. cap0) could not yet been demonstrated, it remains possible that additional factor(s) (depicted as X) may facilitate MDA5 activation. Non-self RNAs are proposed as RNAs lacking 2′O-methylation (sensing by MDA5), N7-methylation and 2′O-methylation (sensing is currently not known) and RNA comprising 5′-ends with triphosphates (sensing by RIG-I). Restriction of viral protein translation: 2′O-MTase-deficient viruses are sensitive to the antiviral actions of IFN and the IFN-induced protein IFIT1 was shown to bind RNA lacking 2′O-methylation and causing a translation arrest. It is currently unknown how CoVs lacking the N7-MTase activity will affect viral replication and if a similar translational arrest may occur. IFIT1 was shown to efficiently bind non-methylated RNA (i.e. lacking N7-methylation and 2′O-methylation). It remains to be clarified if other IFIT proteins or ISG are required for translational arrest.
Biochemical analyses revealed that 2′O-MTases of CoVs and Flaviviruses specifically methylate N7-methylated RNA structures, suggesting that N7-methylation is a prerequisite for 2′O-methylation to occur, and thus, an inactive N7-MTase would prevent the 2′O-MTase from proceeding with methylation [27, 28]. It has been shown that WNVs lacking N7-methylation are non-replicative and that upon transfection of RNA encoding only weak N7-MTase activity, viruses with a number of compensatory mutations were rescued [29]. The coronaviral N7-MTase was only recently identified to reside in nsp14 [22, 27] and it is currently unknown how the inactivation of the CoV-N7-MTase will affect viral replication and innate immune recognition (Figure 2). It can only be hypothesized that non-methylated RNA will be preferentially recognized by IFIT1, resulting most likely in a translational arrest similar to RNA lacking 2′O-methylation [25••]. It has not yet been described if CoV-MTases also methylate internal nucleotides of nascent mRNAs as it is known for Flaviviruses [30] or if they employ a similar mechanism as demonstrated for the Marburg Virus (Filoviruses), where a multifunctional protein VP35 not only caps dsRNA-termini but also fully coats the backbone to physically protect the RNA from length-dependent sensing [31, 32].
Ribonucleases remove RNA-PAMPs?
Efficient removal of RNA-PAMPs prevents the activation of the innate immune system and is thus facilitating successful replication in the host cell. Infections by Arenaviruses, including the Lassa fever virus (LASV), are characterized by a potent mechanism of immune suppression, which is partially mediated by the 3′-to-5′ exoribonuclease (ExoN) which is encoded in the LASV nucleoprotein and structurally very similar to members of the DEDDh family of ExoNs [33]. The LASV-ExoN specifically digests viral dsRNAs and consequently removes RNA PAMPs which otherwise would activate cellular receptors and trigger an IFN-response [31, 33, 34].
Coronaviruses also encode a 3′-to-5′ ExoN of the DEDDh superfamily within the N-terminal part of nsp14. The enzyme hydrolyses ssRNAs and dsRNAs, and excises single nucleotide mismatches at the 3′-end of dsRNAs [35•]. Replacement of catalytic residues in the ExoN domain of MHV and SARS-CoV resulted in viable mutants. However, mutations accumulated throughout their genomes albeit without any obvious fitness costs [36], indicating that ExoN functions as an unique RNA-proofreading enzyme and thereby confers very high replication fidelity, which is required for stable propagation of large viral RNA genomes exceeding 20 kb [6••, 37]. Obviously, RNase-activities are expected to be very target-specific and tightly regulated to prevent unwanted cleavage of viral or cellular RNAs. It has been shown that DNA, ribose-2′O-methylated RNA substrates [38], diribonucleotide, triribonucleotide or longer unpaired ribonucleotide stretches as well as 3′-modified RNAs [35•] are resistant to ExoN-mediated cleavage. Furthermore, CoV-nsp10 has been described to allosterically regulate the 2′O-MTase activity [27, 39] and interestingly, also stimulate the CoV-ExoN activity [35•]. This suggests an important regulatory role of nsp10 in immune suppression through its dual impact on ExoN and 2′O-MTase [35•], proposing that the ExoN is not only involved in RNA-proofreading but also in the escape of host innate immunity. As IFN-induction is efficiently inhibited during CoV-infection, a role of ExoN in degrading RNA-PAMPs might be indeed conceivable and would complement known IFN-antagonistic activities during CoV-infection.
The second ribonuclease of CoVs, an endoribonuclease (EndoU) is encoded by nsp15 and was until recently considered a Nidovirus-specific feature. However, the discovery of an insect-born Nidovirus and the re-evaluation of invertebrate Ronivirus genomes revealed that they lack an EndoU domain, indicating that the utilization of an EndoU domain is restricted to vertebrate Nidoviruses [6••]. The CoV-EndoU domain is structurally very conserved but exhibits only moderate sequence conservation [40, 41]. It hydrolyses ssRNA and dsRNA substrates, preferably 3′ of uridylates [41, 42] and cleaves similar as XendoU and RNase A, as the reaction products possess 2′,3′-cyclic phosphate ends [42]. Ectopic expression studies demonstrated that CoV-nsp15 is not only co-localized with the RTC, but also distributed throughout the cytoplasm [40], thus an additional function besides its involvement in viral replication has been proposed [43]. Overexpression studies in the absence of CoV-infection suggested a role of the SARS-CoV EndoU as a robust IFN-antagonist [44] and it seems plausible that CoVs might use the RNase activity of nsp15 to digest RNA-PAMPs and thus avoid activation of the innate immune system, similar as described for the Pestivirus ribonuclease activity of the structural protein Erns [45•, 46]. However it should be kept in mind that during virus infection, Arterivirus and CoV EndoUs co-localize mainly with the RTC, and it still remains to be determined if the proposed mechanism of immune evasion is actually taking place at Arterivirus and CoV RTCs. Further it remains elusive if the EndoU substrate is RNA of viral or cellular origin, and under which circumstances the utilization of an EndoU is required, as the enzyme is absent in invertebrate Nidoviruses [6••].
Shielding dsRNA from innate immune sensors
A hallmark of CoV replication is the induction of ER-derived double membrane vesicles (DMVs) that are part of a reticulovesicular network in the host cytoplasm. Particular proteins involved in replication (nsp3, nsp5, nsp8) are found predominantly at the outer membrane of DMVs [47], whereas dsRNA was mostly detected within the inner lumen of the vesicles [48, 49]. Interestingly, no connection of the DMV lumen to the cytoplasm could be identified so far. Thus, assuming that the dsRNA within CoV-induced DMVs is of viral origin, it remains enigmatic how viral mRNAs may leave the vesicles and become accessible for translation. It furthermore raises the question if dsRNA within DMVs represents replicative intermediates [47] or rather dead-end products that are shielded from innate immune sensing by cytoplasmic receptors. It thus remains to be determined if DMVs are the actual site of RNA synthesis and additionally, how transcripts are transported to the sites of assembly. Moreover, given the assumption that dsRNA may simply represent potent PAMPs that are hidden from innate sensors, it would be crucial to evaluate the strength of the IFN-response in the absence of DMVs and also, which receptors may play a role in this context.
Significance and perspectives
CoVs raised considerable concerns as zoonotic pathogens. However, they have long been known as important animal pathogens and our knowledge on molecular details of their replication strategy has significantly increased during the past decades. CoVs have evolved versatile mechanisms to counteract host innate immune responses, including mimicking cellular mRNAs, engagement of virus-encoded ribonucleases, and shielding of dsRNA from innate immune sensing. There are a number of parallels described for other viruses, suggesting that those mechanisms target evolutionary conserved innate immune pathways. Nevertheless, mechanistic details of CoV innate immune evasion are still sparse. It will be important in future studies to address the overarching theme ‘how, where and when CoV-RNA is sensed during infection’. For example, it is important to clarify where exactly CoV-RNA synthesis takes place and which role(s) CoV-induced DMVs play in the context of viral replication and innate immune evasion. How and where do cytosolic PRRs access CoV-RNA and which mechanisms for self–non-self distinction of RNA exist. Important consideration are (i) when and where during the infection do viral RNA and PRRs interact, (ii) is there a particular sensing complex assisting RLRs to assess molecular signatures, such as 2′O-methylation, in order to distinguish self from non-self RNA, and (iii) is there a particular sensing complex to detect ‘mis-localized’ RNA, for example viral RNA outside DMVs. A better understanding of these basic questions will be crucial to design novel strategies of antiviral intervention that will be applicable to a wide spectrum of virus-induced diseases in animals and humans.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Acknowledgements
This work was supported by the Swiss National Science Foundation (310030_149784) and the Deutsche Forschungsgemeinschaft (SPP 1596 “Ecology and species barriers in emerging viral diseases”).
References
- 1.Parkin J., Cohen B. An overview of the immune system. Lancet. 2001;357:1777–1789. doi: 10.1016/S0140-6736(00)04904-7. [DOI] [PubMed] [Google Scholar]
- 2.Kawai T., Akira S. TLR signaling. Cell Death Differ. 2006;13:816–825. doi: 10.1038/sj.cdd.4401850. [DOI] [PubMed] [Google Scholar]
- 3.Perlman S., Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. 2009;7:439–450. doi: 10.1038/nrmicro2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4•.Kindler E., Jónsdóttir H.R., Muth D., Hamming O.J., Hartmann R., Rodriguez R., Geffers R., Fouchier R.A.M., Drosten C., Müller M.A. Efficient replication of the novel human betacoronavirus EMC on primary human epithelium highlights its zoonotic potential. MBio. 2013;4 doi: 10.1128/mBio.00611-12. [DOI] [PMC free article] [PubMed] [Google Scholar]; This work describes that the novel MERS-CoV induces only marginal innate immune responses in primary airway epithelia cells.
- 5.Zaki A., van Boheemen S., Bestebroer T., Osterhaus A.D.M., Fouchier R.A.M. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 6••.Nga P.T., Parquet M., del C., Lauber C., Parida M., Nabeshima T., Yu F., Thuy N.T., Inoue S., Ito T., Okamoto K. Discovery of the first insect Nidovirus, a missing evolutionary link in the emergence of the largest RNA virus genomes. PLoS Pathog. 2011;7:e1002215. doi: 10.1371/journal.ppat.1002215. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study revealed that invertebrate Nidoviruses lack the EndoU domain. This raises the question if the EndoU domain may not be required in invertebrate hosts to counteract innate immune responses.
- 7.O’Neill L.A., Golenbock D., Bowie A.G. The history of Toll-like receptors — redefining innate immunity. Nat Rev Immunol. 2013;13:453–460. doi: 10.1038/nri3446. [DOI] [PubMed] [Google Scholar]
- 8.Kato H., Takeuchi O., Mikamo-Satoh E., Hirai R., Kawai T., Matsushita K., Hiiragi A., Dermody T.S., Fujita T., Akira S. Length-dependent recognition of double-stranded ribonucleic acids by retinoic acid-inducible gene-I and melanoma differentiation-associated gene 5. J Exp Med. 2008;205:1601–1610. doi: 10.1084/jem.20080091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y., Ludwig J., Schuberth C., Goldeck M., Schlee M., Li H., Juranek S., Sheng G., Micura R., Tuschl T. Structural and functional insights into pattern recognition by the innate immune receptor RIG-I. Nat Struct Mol Biol. 2010;17:781–787. doi: 10.1038/nsmb.1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cervantes-Barragan L., Züst R., Weber F., Spiegel M., Lang K.S., Akira S., Thiel V., Ludewig B. Control of coronavirus infection through plasmacytoid dendritic-cell-derived type I interferon. Blood. 2007;109:1131–1137. doi: 10.1182/blood-2006-05-023770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roth-Cross J.K., Bender S.J., Weiss S.R. Murine coronavirus mouse hepatitis virus is recognized by MDA5 and induces type I interferon in brain macrophages/microglia. J Virol. 2008;82:9829–9838. doi: 10.1128/JVI.01199-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J., Liu Y., Zhang X. Murine coronavirus induces type I interferon in oligodendrocytes through recognition by RIG-I and MDA5. J Virol. 2010;84:6472–6482. doi: 10.1128/JVI.00016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou H., Perlman S. Mouse hepatitis virus does not induce Beta interferon synthesis and does not inhibit its induction by double-stranded RNA. J Virol. 2007;81:568–574. doi: 10.1128/JVI.01512-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cervantes-Barragán L., Kalinke U., Züst R., König M., Reizis B., López-Macías C., Thiel V., Ludewig B. Type I IFN-mediated protection of macrophages and dendritic cells secures control of murine coronavirus infection. J Immunol. 2009;182:1099–1106. doi: 10.4049/jimmunol.182.2.1099. [DOI] [PubMed] [Google Scholar]
- 15.Lau S.K., Lau C.C., Chan K.-H., Li C.P., Chen H., Jin D.-Y., Chan J.F., Woo P.C., Yuen K.-Y. Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by the novel Middle East respiratory syndrome coronavirus: implications for pathogenesis and treatment. J Gen Virol. 2013;94:2679–2690. doi: 10.1099/vir.0.055533-0. [DOI] [PubMed] [Google Scholar]
- 16.Zielecki F., Weber M., Eickmann M., Spiegelberg L., Zaki A.M., Matrosovich M., Becker S., Weber F. Human cell tropism and innate immune system interactions of human respiratory coronavirus EMC compared to those of severe acute respiratory syndrome coronavirus. J Virol. 2013;87:5300–5304. doi: 10.1128/JVI.03496-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou J., Chu H., Li C., Wong B.H.-Y., Cheng Z.-S., Poon V.K.-M., Sun T., Lau C.C.-Y., Wong K.K.-Y., Chan J.Y.-W. Active replication of middle east respiratory syndrome coronavirus replication and aberrant induction of inflammatory cytokines and chemokines in human macrophages: implications for pathogenesis. J Infect Dis. 2013;43:1–12. doi: 10.1093/infdis/jit504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18••.Zuest R., Cervantes-Barragan L., Habjan M., Maier R., Neuman B.W., Ziebuhr J., Szretter K.J., Baker S.C., Barchet W., Diamond M.S. Ribose 2′-O-methylation provides a molecular signature for the distinction of self and non-self mRNA dependent on the RNA sensor Mda5. Nat Immunol. 2011;12:137–143. doi: 10.1038/ni.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates that Coronaviruses lacking 2′O-MTase activity induce elevated levels of type-I IFN dependent on the RLR Mda5.
- 19.Pichlmair A., Schulz O., Tan C.-P., Rehwinkel J., Kato H., Takeuchi O., Akira S., Way M., Schiavo G., Reis e Sousa C. Activation of MDA5 requires higher-order RNA structures generated during virus infection. J Virol. 2009;83:10761–10769. doi: 10.1128/JVI.00770-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20••.Decroly E., Ferron F., Lescar J., Canard B. Conventional and unconventional mechanisms for capping viral mRNA. Nat Rev Microbiol. 2011;10:51–65. doi: 10.1038/nrmicro2675. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review article provides a comprehensive overview on viral strategies to cap their RNA 5′-ends.
- 21.Ivanov K.A., Thiel V., Dobbe J.C., Van Der Meer Y., Snijder E.J., Ziebuhr J. Multiple enzymatic activities associated with severe acute respiratory syndrome coronavirus helicase. J Virol. 2004;78:5619–5632. doi: 10.1128/JVI.78.11.5619-5632.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Y., Cai H., Pan J., Xiang N., Tien P., Ahola T., Guo D. Functional screen reveals SARS coronavirus nonstructural protein nsp14 as a novel cap N7 methyltransferase. Proc Natl Acad Sci. 2009;106:3484–3489. doi: 10.1073/pnas.0808790106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Y., Su C., Ke M., Jin X., Xu L., Zhang Z., Wu A., Sun Y., Yang Z., Tien P. Biochemical and structural insights into the mechanisms of SARS coronavirus RNA ribose 2′-O-methylation by nsp16/nsp10 protein complex. PLoS Pathog. 2011;7:e1002294. doi: 10.1371/journal.ppat.1002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daffis S., Szretter K.J., Schriewer J., Li J., Youn S., Errett J., Lin T.-Y., Schneller S., Zust R., Dong H. 2′-O methylation of the viral mRNA cap evades host restriction by IFIT family members. Nature. 2010;468:452–456. doi: 10.1038/nature09489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25••.Habjan M., Hubel P., Lacerda L., Benda C., Holze C., Eberl C.H., Mann A., Kindler E., Gil-Cruz C., Ziebuhr J. Sequestration by IFIT1 impairs translation of 2′O-unmethylated capped RNA. PLoS Pathog. 2013;9:e1003663. doi: 10.1371/journal.ppat.1003663. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides first evidence that IFIT proteins can efficiently bind RNAs containing non-methylated cap structures lacking 2′O-methylation and N7-methylation.
- 26.Szretter K.J., Daniels B.P., Cho H., Gainey M.D., Yokoyama W.M., Gale M., Virgin H.W., Klein R.S., Sen G.C., Diamond M.S. 2′-O methylation of the viral mRNA cap by West Nile virus evades ifit1-dependent and -independent mechanisms of host restriction in vivo. PLoS Pathog. 2012;8:452–456. doi: 10.1371/journal.ppat.1002698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouvet M., Debarnot C., Imbert I., Selisko B., Snijder E.J., Canard B., Decroly E. In Vitro reconstitution of SARS-Coronavirus mRNA cap methylation. PLoS Pathog. 2010;6:e1000863. doi: 10.1371/journal.ppat.1000863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chung K.Y., Dong H., Theodore A., Shi P.-Y., Lescar J., Pheng S., Yan K. Higher catalytic efficiency of N-7-methylation is responsible for processive N-7 and 2′-O methyltransferase activity in dengue virus. Virology. 2010;402:52–60. doi: 10.1016/j.virol.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 29.Zhang B., Dong H., Zhou Y., Shi P.-Y. Genetic interactions among the West Nile virus methyltransferase, the RNA-dependent RNA polymerase, and the 5′ stem-loop of genomic RNA. J Virol. 2008;82:7047–7058. doi: 10.1128/JVI.00654-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dong H., Chang D.C., Ho M., Hua C., Lim S.P., Chionh Y.H., Hia F., Lee Y.H., Kukkaro P., Lok S. 2′-O methylation of internal adenosine by flavivirus NS5 methyltransferase. PLoS Pathog. 2012;8:e1002642. doi: 10.1371/journal.ppat.1002642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hastie K.M., Bale S., Kimberlin C.R., Ollmann E. Hiding the evidence: two strategies for innate immune evasion by hemorrhagic fever viruses. Curr Opin Microbiol. 2013;2:151–156. doi: 10.1016/j.coviro.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bale S., Julien J.-P., Bornholdt Z., Kimberlin C.R., Halfmann P., Zandonatti M., Kunert J., Kroon G.J., Kawaoka Y., MacRae I.J. Marburg virus VP35 can both fully coat the backbone and cap the ends of dsRNA for interferon antagonism. PLoS Pathog. 2012;8:e1002916. doi: 10.1371/journal.ppat.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qi X., Lan S., Wang W., Mc Lay Schelde L., Dong H., Wallat G.D., Ly H., Liang Y., Dong C. Cap binding and immune evasion revealed by Lassa nucleoprotein structure. Nature. 2010;468:779–783. doi: 10.1038/nature09605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang X., Huang Q., Wang W., Dong H., Ly H., Liang Y., Dong C. Structures of arenaviral nucleoproteins with triphosphate dsRNA reveal a unique mechanism of immune suppression. J Biol Chem. 2013;288:16949–16959. doi: 10.1074/jbc.M112.420521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35•.Bouvet M., Imbert I., Subissi L., Gluais L., Canard B., Decroly E. RNA 3′-end mismatch excision by the severe acute respiratory syndrome coronavirus nonstructural protein nsp10/nsp14 exoribonuclease complex. Proc Natl Acad Sci. 2012;109:9372–9377. doi: 10.1073/pnas.1201130109. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates that the CoV exonuclease can excise 3′-end mismatches, suggesting that it can act as RNA proofreading enzyme. Furthermore, nsp10 appears to have a pivotal role in regulating nsp14 and nsp16 activities.
- 36.Eckerle L.D., Becker M.M., Halpin R.a., Li K., Venter E., Lu X., Scherbakova S., Graham R.L., Baric R.S., Stockwell T.B. Infidelity of SARS-CoV Nsp14-exonuclease mutant virus replication is revealed by complete genome sequencing. PLoS Pathog. 2010;6:e1000896. doi: 10.1371/journal.ppat.1000896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lauber C., Goeman J.J., Parquet M.D.C., Nga P.T., Snijder E.J., Morita K., Gorbalenya A.E. The footprint of genome architecture in the largest genome expansion in RNA viruses. PLoS Pathog. 2013;9:e1003500. doi: 10.1371/journal.ppat.1003500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Minskaia E., Hertzig T., Gorbalenya A.E., Campanacci V., Cambillau C., Canard B., Ziebuhr J. Discovery of an RNA virus 3′->5′ exoribonuclease that is critically involved in coronavirus RNA synthesis. Proc Natl Acad Sci. 2006;103:5108–5113. doi: 10.1073/pnas.0508200103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Decroly E., Debarnot C., Ferron F., Bouvet M., Coutard B., Imbert I., Gluais L., Papageorgiou N., Sharff A., Bricogne G. Crystal structure and functional analysis of the SARS-coronavirus RNA cap 2′O methyltransferase nsp10/nsp16 complex. PLoS Pathog. 2011;7:e1002059. doi: 10.1371/journal.ppat.1002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cao J., Xuming Z. Comparative in vivo analysis of the Nsp15 Endoribonuclease of murine, porcine and severe acute respiratory syndrome Coronaviruses. Virus Res. 2012;167:247–258. doi: 10.1016/j.virusres.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kang H., Bhardwaj K., Li Y., Palaninathan S., Sacchettini J., Guarino L., Leibowitz J.L., Kao C.C. Biochemical and genetic analyses of murine hepatitis virus Nsp15 endoribonuclease. J Virol. 2007;81:13587–13597. doi: 10.1128/JVI.00547-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhardwaj K., Sun J., Holzenburg A., Guarino L.a, Kao C.C. RNA recognition and cleavage by the SARS coronavirus endoribonuclease. J Mol Biol. 2006;361:243–256. doi: 10.1016/j.jmb.2006.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shi X., Wang L., Li X., Zhang G., Guo J., Zhao D., Chai S., Deng R. Endoribonuclease activities of porcine reproductive and respiratory syndrome virus nsp11 was essential for nsp11 to inhibit IFN-β induction. Mol Immunol. 2011;48:1568–1572. doi: 10.1016/j.molimm.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frieman M., Ratia K., Johnston R.E., Mesecar D., Baric R.S., Signaling N.-B., Mesecar A.D. Severe acute respiratory syndrome coronavirus papain-like protease ubiquitin-like domain and catalytic domain regulate antagonism of IRF3 and NF-κB signaling. J Virol. 2009;83:6689–6705. doi: 10.1128/JVI.02220-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45•.Python S., Gerber M., Suter R., Ruggli N., Summerfield A. Efficient sensing of infected cells in absence of virus particles by plasmacytoid dendritic cells is blocked by the viral ribonuclease E(rns.) PLoS Pathog. 2013;9:e1003412. doi: 10.1371/journal.ppat.1003412. [DOI] [PMC free article] [PubMed] [Google Scholar]; This work suggests a role of a viral endoribonuclease in removing RNA-PAMPs.
- 46.Magkouras I., Mätzener P., Rümenapf T., Peterhans E., Schweizer M. RNase-dependent inhibition of extracellular, but not intracellular, dsRNA-induced interferon synthesis by Erns of pestiviruses. J Gen Virol. 2008;89:2501–2506. doi: 10.1099/vir.0.2008/003749-0. [DOI] [PubMed] [Google Scholar]
- 47.Knoops K., Kikkert M., Van Den Worm S.H.E., Zevenhoven-Dobbe J.C., van der Meer Y., Koster A.J., Mommaas a.M., Snijder E.J. SARS-coronavirus replication is supported by a reticulovesicular network of modified endoplasmic reticulum. PLoS Biol. 2008;6:e226. doi: 10.1371/journal.pbio.0060226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Snijder E.J., van der Meer Y., Zevenhoven-Dobbe J., Onderwater J.J.M., van der Meulen J., Koerten H.K., Mommaas a.M. Ultrastructure and origin of membrane vesicles associated with the severe acute respiratory syndrome coronavirus replication complex. J Virol. 2006;80:5927–5940. doi: 10.1128/JVI.02501-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brockway S.M., Clay C.T., Lu X.T., Denison M.R. Characterization of the expression intracellular localization, and replication complex association of the putative mouse hepatitis virus RNA-dependent RNA polymerase. J Virol. 2003;77:10515–10527. doi: 10.1128/JVI.77.19.10515-10527.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]