Abstract
Early recognition of patients who might potentially require ventilatory support is a key goal of critical care outreach programs and an important skill for all hospital medical staff. Decisions about the initiation and timing of invasive ventilation can be difficult and early discussion with critical care colleagues is essential. Appropriateness of invasive ventilatory support may also be an issue requiring advanced discussion with patients and their families. In the past 10–15 years, the role of non-invasive ventilation (NIV) has expanded, not least in an attempt to minimize the complications inherent with invasive ventilation. As such, NIV is now considered first-line therapy in some conditions (chronic obstructive pulmonary disease, pulmonary oedema, mild-to-moderate hypoxaemic respiratory failure in immunocompromised patients), and a ‘trial of NIV’ is often considered in respiratory failure resulting from an increasingly wide range of causes. When using NIV, the importance of the environment (setting, monitoring and experience of staff) and forward planning cannot be overemphasized. When used for other than the standard indications, NIV should be employed in a high-dependency/intensive care setting only in patients for whom invasive ventilation would be considered.
Keywords: intensive care, mechanical ventilation, non-invasive mechanical ventilation, respiratory failure
Introduction
Indications for ventilation
Early identification of critically ill patients, before the occurrence of significant cardio-respiratory decompensation, is one of the major goals of critical care outreach programmes. Patients who require ventilatory support often develop a common pattern of physiological deterioration including:
-
•
increasing respiratory rate
-
•
asynchronous respiratory pattern
-
•
a change in mentation and level of consciousness
-
•
frequent oxygen desaturation despite increasing oxygen concentration
-
•
hypercapnia and respiratory acidosis
-
•
circulatory problems, including hypotension and atrial dysrhythmias.
Modern ventilators
The modern ventilator is a complex computer-driven tool and a detailed description of its modes and use are beyond the scope of this article (see Further reading). In simple terms, it mixes air under pressure with variable oxygen concentrations to provide inspiration and expiration, each ‘breath’ is characterized by three factors, which can be adjusted by the operator;
-
•
Trigger: the ventilator can deliver a breath according to a timer that defines a specific set rate (ventilator initiated/mandatory breaths), or as a result of the patient's own breathing efforts effecting a change in the pressure or flow in the ventilator circuit (patient-initiated/spontaneous breaths).
-
•
Target: the flow of air into the lung can be to a specific target flow rate (volume control) or pressure (pressure control; pressure support; bi-level)
-
•
Termination: the signal for the ventilator to finish inspiration and allow expiration (passive) may be the achievement of a specific volume (volume-cycled: volume control), after a specific time (time-cycled: pressure control/bi-level) or following the reduction of inspiratory flow to a preset level (flow-cycled: pressure support)
Non-invasive ventilation (NIV)
NIV refers to the provision of respiratory support without direct tracheal intubation. As such, it aims to avoid some of the complications inherent with invasive ventilation, such as the need for sedation with risks of haemodynamic instability and subsequent risk of delirium, nosocomial infection, etc.1 In a recent worldwide survey, use of NIV increased from 4% to 11% of all episodes of mechanical ventilation between 2001 and 2004 respectively, with even higher rates of use in some European countries.2 Indeed, for some situations it is considered the first-choice mode of ventilatory support (Table 1 : Evidence for use). However, it may not be appropriate for all patients, particularly as it is being used increasingly outside of the traditional critical care setting (Table 2 – Indications/Contraindications for NIV).
Table 1.
Recommendations for use of non-invasive ventilation to treat acute respiratory failure
| Recommendations based on levels of evidence21 Level 1 evidence Systematic reviews (with homogeneity) of RCTs and individual RCTs (with narrow CIs) Evidence of use (favourable)
Systematic reviews (with homogeneity) of cohort studies—individual cohort studies (including low-quality RCTs; eg, <80% follow-up) Evidence of use (favourable)
Systematic reviews (with homogeneity) of case–control studies, individual case–control study Evidence of use (favourable)
Case series (and poor-quality cohort and case–control studies) Evidence of use (favourable)
|
CI, confidence interval; COPD, chronic obstructive pulmonary disease; NIV, non-invasive ventilation; RCTs, randomized controlled trials. (Reprinted from Lancet, vol. 374; 250–259. Nava S, Hill N, Non-invasive ventilation in acute respiratory failure. With permission from Elsevier).
Table 2.
Non-invasive ventilation: indications, contraindications and predictors for failure
|
Indications Clinical observation
| |
Gas exchange
| |
| Contraindications | Potential solution |
| Facial burns/trauma/recent facial upper airway surgery | Rarely role for NIV – invasive ventilation standard therapy |
| Vomiting | Treat cause, anti-emetics consider NG tube |
| Upper gastrointestinal surgery | Varies on type of surgery and also time from surgery |
| Copious respiratory secretions | Chest physiotherapy, adequate breaks off NIV (if possible) and treatment of infection – consider early IMV |
| Severe hypoxaemia | HDU/ICU setting – consider early IMV |
| Haemodynamically instability | HDU/ICU setting – consider early IMV |
| Severe co-morbidities | Clearly define role of NIV/IMV - palliative care may be more appropriate |
| Confusion/agitation | HDU/ICU setting – cautious and controlled pharmacological therapy and appropriate interface. Consider early IMV |
| Low Glasgow coma score | Those with a low Glasgow coma score (<8) due to hypercapnia, can have a good response to NIV: normally seen immediately. Do not instigate NIV when invasive ventilation is immediately indicated. |
| Unable to protect airway | Consider the above. Invasive ventilation likely |
| Bowel obstruction | NG tube drainage and/or surgery - consider early IMV |
| Respiratory arrest | No role for NIV; needs invasive ventilation |
|
Predictors of failure of NIV Hypercapnic respiratory failure
| |
ARDS, acute respiratory distress syndrome; HDU, high-dependency unit; ICU, intensive care unit; NG, nasogastric; NIV, non-invasive ventilation.
NIV today consists almost exclusively of the delivery of positive pressure ventilation via an external interface. There are six broad types of interface available, each with its own particular benefits and drawbacks (see Further reading):
-
•
total face masks (enclose mouth, nose eyes)
-
•
full face masks (enclose mouth and nose)
-
•
nasal mask (covers nose but not mouth)
-
•
mouthpieces (placed between lips and held in place by lip seal)
-
•
nasal pillows or plugs (inserted into nostrils)
-
•
helmet (covers the whole head/all or part of the neck – no contact with face).
NIV can be delivered using most modern ‘intensive care’ ventilators. For sicker patients this has several advantages (ability to deliver higher and precise concentrations of oxygen; separate inspiratory/expiratory limbs minimizing re-breathing of CO2; better monitoring/alarm features; and rapid access to invasive ventilation). Outside of the ICU, NIV is commonly applied using smaller, ‘simpler’ but increasingly sophisticated ‘non-invasive’ ventilators, which can provide a range of respiratory support modes. Pressure-cycled modes are generally preferred (accommodation of leaks), and breaths can be either patient-triggered (pressure support or bi-level positive airway pressure (BiPAP)), or initiated and controlled by the ventilator (pressure control). Indeed, both modes are often used synergistically to provide back up when triggering is poor or if patient respiratory rate is unreliable, and to cover potential apnoeic episodes.
Acute hypercapnic respiratory failure
Patients with acute hypercapnic respiratory acidosis secondary to an acute exacerbation of chronic obstructive pulmonary disease (COPD), represent the most extensively studied group, and the greatest evidence for benefit exists in COPD.3, 4, 5, 6 Numerous studies and meta-analyses have confirmed that use of NIV is associated with reduced risks of treatment failure (RR 0.48), lower intubation rates (RR 0.41) with lower incidence of nosocomial infections, and a reduction in mortality (RR 0.52) with subsequent reduced hospital length of stay and costs.7 These benefits have been shown predominantly in patients with mild-to-moderate hypercapnic respiratory failure (pH 7.30–7.34). As such, NIV should be considered first-line therapy for this patient group, and can be safely used in appropriately staffed and monitored environments outside of the ICU.4 This does not preclude the use of NIV in patients with more severe respiratory failure,8, 9, 10 and a pH as low as 7.20 may still be compatible with favourable outcomes. However, such patients should be managed in a high-dependency environment, to allow for rapid escalation to intubation and invasive ventilation if appropriate.
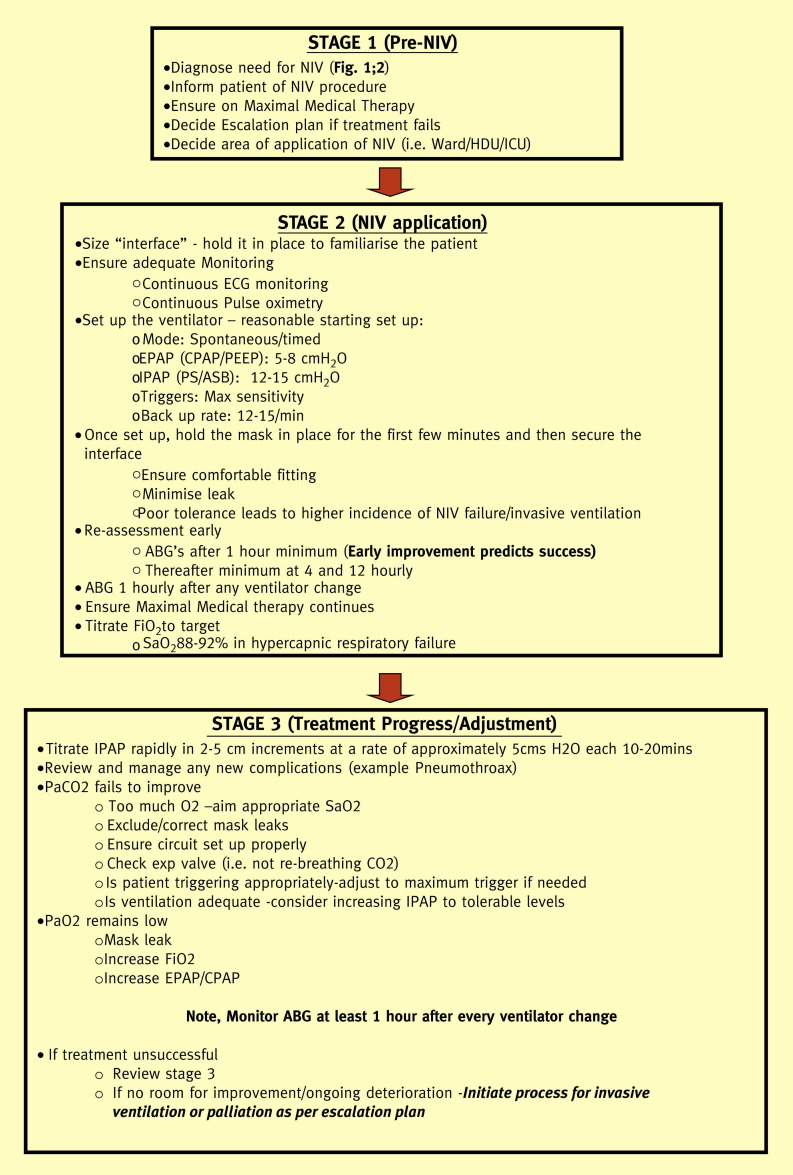
The importance of an established structure for effective NIV delivery cannot be overemphasized. Early initiation by experienced and skilled staff, appropriate environments and monitoring, and protocols to aid patient selection and subsequent decision making are key to the successful and safe application of NIV in all forms of respiratory failure11 (Figure 1 ).
Figure 1.
STAGE 1 (Pre-NIV), STAGE 2 (NIV application), STAGE 3 (Treatment progress/Adjustment).
Although treatment failure is uncommon in mild-to-moderate respiratory failure, it becomes increasingly frequent in sicker (lower pH and/or significant hypoxaemia) patients (Table 2). Common causes of NIV failure include interface leaks and patient asynchrony with the ventilator (Table 2). In experienced hands, such issues can be recognized early and rapidly remedied; if this is not possible, intubation and invasive ventilation will need to be considered.11, 12
The appropriateness of invasive ventilation in patients with COPD can be a contentious issue. However, recent evidence suggests more favourable outcomes than predicted, with stable or even improved quality of life in most patients.13 Decisions about the extent of future intervention should be made by a senior physician, taking into account factors such as functional status, previous pulmonary function tests, existing co-morbidities, body mass index, the need for long-term oxygen therapy and the patient's expressed wishes; ideally before the initiation of NIV. The outcome should be documented in the medical record and communicated to the patient/family as appropriate.
Acute pulmonary oedema
The use of NIV (including continuous positive airway pressure (CPAP)) to treat respiratory failure secondary to acute pulmonary oedema is widespread.14, 15, 16, 17 Several meta-analyses have established benefit, including decreased intubation rate (CPAP/bi-level) and mortality (CPAP) compared to standard medical therapy.18 However, these findings were not borne out in a recent randomized control trial,19 even though physiological improvements occurred earlier in the NIV arms (CPAP/bi-level). The low rate of intubation (<3%), and the potential for crossover between the study arms may have limited the ability to document improvements with NIV. The European Cardiology Task Force20 for diagnosis and treatment of cardiogenic pulmonary oedema recommends NIV/CPAP as first-line treatments in addition to standard medical therapy when respiratory failure is present.
Hypoxaemic respiratory failure
There is conflicting evidence for the use of NIV in hypoxaemic respiratory failure.21, 22, 23, 24 A recent meta-analysis where NIV in addition to standard therapy was compared to standard therapy alone, in hypoxaemic respiratory failure not related to pulmonary oedema, reported improvements in intubation rate, mortality and hospital length of stay with the use of NIV.22 However the literature in this area is hampered by marked heterogeneity between the study populations in both cause and severity of respiratory failure – in particular the frequency of pre-existing COPD. Therefore, although some studies suggest benefit, routine use of NIV in severe pneumonia or acute respiratory distress syndrome (ARDS) cannot be recommended. However, in immunocompromised patients, studies have shown early NIV use to be beneficial in the management of hypoxic respiratory failure, particular in patients with solid organ transplantation, haematological malignancies and HIV infection.25, 26, 27 NIV should be considered in such patients, preferably in a high-dependency/ICU environment with rapid access to invasive ventilation and multi-organ support.
NIV in weaning from invasive ventilation
In an attempt to limit exposure to the risks of invasive mechanical ventilation, NIV is being used increasingly to promote earlier extubation and prevent re-intubation. Present evidence suggests it is most likely to be beneficial in COPD patients, medical patients with multiple morbidities who are likely to fail on extubation and those with hypercapnia during spontaneous breathing trials.28
NIV in other conditions
With increasing expertize in its use, it is not surprising that clinicians have been keen to exploit the potential benefits of NIV over invasive ventilation in other29, 30 forms of respiratory compromise (Table 1). It is important to recognize that in some conditions the literature represents small series from experienced centres and the importance of the environment and forward planning cannot be overemphasized. In these circumstances we would recommend that NIV should be employed in an intensive care setting only if invasive ventilation would be considered for the patient.
Invasive ventilation
Invasive mechanical ventilation requires access to the trachea, most commonly via an endotracheal tube, and represents the commonest reason for admission to the ICU. Large multinational surveys confirm the common indications for invasive ventilation to be:2
-
•
coma 16%
-
•
COPD 13%
-
•
ARDS 11%
-
•
heart failure 11%
-
•
pneumonia 11%
-
•
sepsis 11%
-
•
trauma 11%
-
•
postoperative complications 11%
-
•
neuromuscular disorders 5%.
Initiation of ventilation in the critically ill
Decisions about the initiation and timing of invasive ventilation can be difficult and early discussion with critical care colleagues is essential. Appropriateness of ventilatory support may also be an issue requiring advanced discussion with patients and families. Once a decision to intubate has been made, the transition from an awake and self-ventilating patient to controlled invasive ventilation can be very difficult in the critically ill. Most patients will have evidence of developing or established organ dysfunction, particularly cardiovascular dysfunction (ischaemic heart disease, sepsis), and commonly such patients are hypovolaemic. Both anaesthetic induction agents and positive pressure ventilation (which decreases venous return) produce cardiovascular depression and peri-intubation hypotension is common. In addition, cessation of spontaneous ventilation can lead to very rapid desaturation in such patients, due to their marginal respiratory reserve and circulatory problems. Such consequences need to be anticipated: large-volume cannulae should be in place; access to plasma expanders and inotropes should be immediately available; and following induction of anaesthesia the airway must be rapidly secured by an experienced member of the critical care team – ideally in an appropriately equipped area of the hospital.
Descriptions of individual ventilatory strategies are beyond the scope of this chapter. However, over the past 10–20 years there has been increasing recognition that invasive ventilation, although lifesaving, can be associated with significant complications, such as nosocomial pneumonia, critical illness neuromyopathy syndromes and barotrauma (pneumothoraces); and ventilation itself may be associated with propagation of underlying lung injury and subsequent worsening of multi-organ failure.31, 32 The landmark NIH ARDS network trial33 confirmed that in patients with acute lung injury, the use of a reduced tidal volume (6 ml/kg) and avoidance of high airway pressures (<30 cmH2O) were associated with improved mortality (31% vs. 39.8% (NNT≈11)) when compared with a conventional ventilatory approach. Although it is not without controversy,34 this and subsequent studies form the basis for management of patients with hypoxaemic respiratory failure. Although individual patients differ, key concepts include:
Ventilator-specific strategies
-
•
Low tidal volume (6 ml/kg ideal bodyweight) and avoidance of high inspiratory pressures (P plat < 30) to minimize the risk of volutrauma33
-
•
Reduced oxygenation targets (SaO2 88–95%; pO2 7.5–10.5) – ‘permissive hypoxia’
-
•
Acceptance of mild–moderate respiratory acidosis – ‘permissive hypercapnia’
-
•
Greater use of positive end-expiratory pressure (PEEP), particularly in more severe hypoxaemia35 (NB: PEEP should be used cautiously and may be contraindicated in obstructive airways disease)
-
•
Early use of neuromuscular blockade in severe cases36
General strategies
-
•
Avoidance of excessive fluid administration
-
•
Minimizing sedation once acute insult has settled – daily sedation holds (interruption of sedation), use of sedation scores37
-
•
Daily trials of spontaneous breathing and protocolized weaning once initial insult has resolved38
-
•
Early and appropriate nutritional support
-
•
Deep vein thrombosis prophylaxis
-
•
Stress ulcer prophylaxis
More recently, attention has turned to the use of extracorporeal support in patients with extreme gas exchange abnormalities. In the recent CESAR study,39 transfer to a centre capable of delivering extracorporeal membrane oxygenation (ECMO) was associated with improved outcome (death or disability) at 6 months. This study and the high-profile success of ECMO in the H1N140 influenza pandemic has resulted in a resurgence of interest in this technique. Simpler forms of extracorporeal support exist where hypercapnia is the predominant problem.41 The development of these and other specialist techniques, along with a recognized volume–outcome relationship for mechanical ventilation,42 has promoted the concept of advanced respiratory support centres to manage the sickest patients.
Longer term, there is an increased recognition that survivors of critical illness can be left with significant physical, mental and psychological sequelae43 and early rehabilitation and ICU follow-up programmes have evolved to address these issues.
References
- 1.Tobin M.J. 2nd edn. McGraw Hill; 2006. Principles and practice of mechanical ventilation. [Google Scholar]
- 2.Esteban A., Ferguson N.D., Meade M.O. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008;177:170–177. doi: 10.1164/rccm.200706-893OC. [DOI] [PubMed] [Google Scholar]
- 3.Roberts C.M., Brown J.L., Reinhardt A.K. Non-invasive ventilation in chronic obstructive pulmonary disease: management of acute type 2 respiratory failure. Clin Med. 2008;8:517–521. doi: 10.7861/clinmedicine.8-5-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plant P.K., Owen J.L., Elliott M.W. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355:1931–1935. doi: 10.1016/s0140-6736(00)02323-0. [DOI] [PubMed] [Google Scholar]
- 5.Sinuff T.K.S. Clinical practice guideline for the use of noninvasive positive pressure ventilation in COPD patients with acute respiratory failure. J Crit Care. 2004;19:82–91. doi: 10.1016/j.jcrc.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Lightowler J.V., Wedzicha J.A., Elliott M.W., Ram F.S.F. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: cochrane systematic review and meta-analysis. Br Med J. 2003;326:185. doi: 10.1136/bmj.326.7382.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ram F.S.F., Picot J., Lightowler J., Wedzicha J.A. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2004 doi: 10.1002/14651858.CD004104.pub3. CD004104. [DOI] [PubMed] [Google Scholar]
- 8.Conti G., Antonelli M., Navalesi P. Noninvasive vs. conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trial. Intensive Care Med. 2002;28:1701–1707. doi: 10.1007/s00134-002-1478-0. [DOI] [PubMed] [Google Scholar]
- 9.Brochard L., Mancebo J., Wysocki M. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease — NEJM. New Eng J Med. 1995;333:817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 10.Crummy F., Buchan C., Miller B., Toghill J., Naughton M.T. The use of noninvasive mechanical ventilation in COPD with severe hypercapnic acidosis. Respir Med. 2007;101:53–61. doi: 10.1016/j.rmed.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 11.NIPPV – NIV in Acute Respiratory Failure Guideline. http://www.brit-thoracic.org.uk/guidelines/nippv-?-niv-in-acute-respiratory-failure-guideline.aspx (accessed 5 Jan 2012).
- 12.Nava S., Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–259. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wildman M.J., Sanderson C.F.B., Groves J. Survival and quality of life for patients with COPD or asthma admitted to intensive care in a UK multicentre cohort: the COPD and Asthma Outcome Study (CAOS) Thorax. 2009;64:128–132. doi: 10.1136/thx.2007.091249. [DOI] [PubMed] [Google Scholar]
- 14.Crane S.D., Elliott M.W., Gilligan P., Richards K., Gray A.J. Randomised controlled comparison of continuous positive airways pressure, bilevel non-invasive ventilation, and standard treatment in emergency department patients with acute cardiogenic pulmonary oedema. Emerg Med J. 2004;21:155–161. doi: 10.1136/emj.2003.005413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellone A., Vettorello M., Monari A., Cortellaro F., Coen D. Noninvasive pressure support ventilation vs. continuous positive airway pressure in acute hypercapnic pulmonary edema. Intensive Care Med. 2005;31:807–811. doi: 10.1007/s00134-005-2649-6. [DOI] [PubMed] [Google Scholar]
- 16.Masip J., Betbesé A.J., Páez J. Non-invasive pressure support ventilation versus conventional oxygen therapy in acute cardiogenic pulmonary oedema: a randomised trial. Lancet. 2000;356:2126–2132. doi: 10.1016/s0140-6736(00)03492-9. [DOI] [PubMed] [Google Scholar]
- 17.Mehta S., Al-Hashim A.H., Keenan S.P. Noninvasive ventilation in patients with acute cardiogenic pulmonary edema. Respir Care. 2009;54:186–195. discussion 195–7. [PubMed] [Google Scholar]
- 18.Peter J.V., Moran J.L., Phillips-Hughes J., Graham P., Bersten A.D. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367:1155–1163. doi: 10.1016/S0140-6736(06)68506-1. [DOI] [PubMed] [Google Scholar]
- 19.Gray A., Goodacre S., Newby D.E., Masson M., Sampson F., Nicholl J. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008;359:142–151. doi: 10.1056/NEJMoa0707992. [DOI] [PubMed] [Google Scholar]
- 20.Nieminen M.S., Böhm M., Cowie M.R. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the task force on acute heart failure of the European Society of Cardiology. Eur Heart J. 2005;26:384–416. doi: 10.1093/eurheartj/ehi044. [DOI] [PubMed] [Google Scholar]
- 21.Hess D.R. The evidence for noninvasive positive-pressure ventilation in the care of patients in acute respiratory failure: a systematic review of the literature. Respir Care. 2004;49:810–829. [PubMed] [Google Scholar]
- 22.Keenan S.P., Sinuff T., Cook D.J., Hill N.S. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med. 2004;32:2516–2523. doi: 10.1097/01.ccm.0000148011.51681.e2. [DOI] [PubMed] [Google Scholar]
- 23.Rana S., Jenad H., Gay P.C., Buck C.F., Hubmayr R.D., Gajic O. Failure of non-invasive ventilation in patients with acute lung injury: observational cohort study. Critical Care. 2006;10:R79. doi: 10.1186/cc4923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrer M., Esquinas A., Leon M., Gonzalez G., Alarcon A., Torres A. 2003. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. [DOI] [PubMed] [Google Scholar]
- 25.Antonelli M., Conti G., Bufi M., Costa M.G., Lappa A., Gasparetto A. Noninvasive ventilation for treatment undergoing solid organ transplantation. J Am Med Assoc. 2000;283:235–241. doi: 10.1001/jama.283.2.235. [DOI] [PubMed] [Google Scholar]
- 26.Gilles Hilbert M.D., Didier Gruson M.D., Fréderic Vargas M.D. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Eng J Med. 2001;344:481–487. doi: 10.1056/NEJM200102153440703. [DOI] [PubMed] [Google Scholar]
- 27.Confalonieri M., Calderini E., Terraciano S. Noninvasive ventilation for treating acute respiratory failure in AIDS patients with Pneumocystis carinii pneumonia. Intensive Care Med. 2002;28:1233–1238. doi: 10.1007/s00134-002-1395-2. [DOI] [PubMed] [Google Scholar]
- 28.Burns K.E.A., Adhikari N.K.J., Keenan S.P., Meade M. Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. Br Med J. 2009;338:b1574–b1582. doi: 10.1136/bmj.b1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ram F.S.F., Wellington S., Rowe B.H., Wedzicha J.A. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev. 2005;126 doi: 10.1002/14651858.CD004360.pub3. CD004360. [DOI] [PubMed] [Google Scholar]
- 30.Murase K., Tomii K., Chin K. The use of non-invasive ventilation for life-threatening asthma attacks: changes in the need for intubation. Respirology. 2010;15:714–720. doi: 10.1111/j.1440-1843.2010.01766.x. [DOI] [PubMed] [Google Scholar]
- 31.Lionetti V., Recchia F.A., Ranieri V.M. Overview of ventilator-induced lung injury mechanisms. Curr Opin Crit Care. 2005;11:82–86. doi: 10.1097/00075198-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Dos Santos C.C., Slutsky A.S. Cellular responses to mechanical Stress: invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol. 2000;89:1645. doi: 10.1152/jappl.2000.89.4.1645. [DOI] [PubMed] [Google Scholar]
- 33.England T.N. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 34.Steinbrook R. How best to ventilate? Trial design and patient safety in studies of the acute respiratory distress syndrome. N Engl J Med. 2003;348:1393–1401. doi: 10.1056/NEJMhpr030349. [DOI] [PubMed] [Google Scholar]
- 35.Briel M., Meade M., Mercat A. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. J Am Med Assoc. 2010;303:865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 36.Papazian L., Forel J.-M., Gacouin A. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 37.Girard T.D., Kress J.P., Fuchs B.D. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): a randomised controlled trial. Lancet. 2008;371:126–134. doi: 10.1016/S0140-6736(08)60105-1. [DOI] [PubMed] [Google Scholar]
- 38.Blackwood B., Alderdice F., Burns K., Cardwell C., Lavery G., O'Halloran P. Use of weaning protocols for reducing duration of mechanical ventilation in critically ill adult patients: cochrane systematic review and meta-analysis. Br Med J. 2011;342:c7237. doi: 10.1136/bmj.c7237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peek G.J., Mugford M., Tiruvoipati R. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 40.Investigators* TA and NZEMO (ANZ EI. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. J Am Med Assoc. 2009;302:1888–1895. doi: 10.1001/jama.2009.1535. [DOI] [PubMed] [Google Scholar]
- 41.The Novalung® iLA membrane ventilator: technical aspects. http://www.ctsnet.org/portals/thoracic/newtechnology/article-9.html.
- 42.Kahn J.M., Goss C.H., Heagerty P.J., Kramer A.A., O’Brien C.R., Rubenfeld G.D. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006;355:41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- 43.Herridge M.S., Cheung A.M., Tansey C.M. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;1:812. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
Further reading
- 44.NIPPV – NIV in Acute Respiratory Failure Guideline. http://www.brit-thoracic.org.uk/guidelines/nippv-?-niv-in-acute-respiratory-failure-guideline.aspx.