Abstract
Purpose
Nurses are suffering from considerable work-related stress, which can result in disturbed sleep and depressive symptoms. Whereas, recovery experience can alleviate sleep disturbance and help maintain well-being in the working environment. The aim of this study was to examine whether recovery experiences play a mediating role in the relationship between sleep disturbance and depressive symptoms of female nurses in Chinese public hospitals.
Methods
From December 2017 to May 2018, the study with proportional sampling of cross-sectional design was carried out in the public tertiary hospitals from Shenyang of Liaoning Province in China. A total of 1500 female nurses who had been working for one or more years participated in this study. A structural equation model (SEM) was applied to test the assumption that recovery experiences might function as a mediator in the relationship between sleep disturbance and symptoms of depression.
Results
Sleep disturbance contributed most to the variance (32.9%) of depressive symptoms and had a significantly positive correlation with depressive symptoms (P<0.01) among nurses. Psychological detachment in recovery experience had a significantly positive correlation with sleep disturbance (P<0.01) and depressive symptoms (P<0.01). Whereas, relaxation, mastery experience, and control in recovery experience were significantly and negatively correlated with sleep disturbance (P<0.01) and depressive symptoms (P<0.01). Recovery experience served as a mediator between sleep disturbance and depressive symptoms (a * b = 0.066, BCa 95% CI: 0.045, 0.095).
Conclusion
Sleep disturbance was the predictor of depressive symptoms for female nurses. Moreover, recovery experience could combat the detrimental impacts of sleep disturbances on symptoms of depression. This study suggested that nurses might benefit from interventions on improving sleep quality to relieve depressive symptoms through mediating path of recovery experience.
Keywords: recovery experience, sleep disturbance, depressive symptoms, female nurses, public hospitals
Introduction
Depression has been predicted to rank as the second leading cause of disability, and one of the top ten sources of disease burden by the year of 2020.1 Nurses are susceptible to exposure to considerable work-related stressors which can increase the prevalence of depressive symptoms.2 Nurses are considered to be at high risk for the development of depressive symptoms.3,4 Given that female nurses are the indispensable health workforce in the healthcare system, which accounted for more than 98% of the nurse population.5 Furthermore, given sex differences in the prevalence of depression, female nurses are particularly vulnerable to perceive the symptoms of depression.6 Therefore, this study was conducted only in female nurses. There are a great deal of studies indicating that negative mental states such as depressive symptoms had a detrimental impact on the quality of care provided by nurses, and hence, affected patient’s medical treatment outcomes.3,7 Therefore, this study aims to evaluate the depressive symptoms among female nurses in China, which could help to understand their depressive symptoms and provide effective guidance for relieving depressive symptoms. Currently, the nurse to total population ratio in China (1:1750) is considerably lower when compared with that of developed countries (1:140–1:320) and most countries in the world (1:330).8,9 A large number of population-based health services need combined with insufficient nurse staffing result in heavy workloads for Chinese nurses, which likely aggravates the symptoms of depression.7 A recent study revealed that 40.8% of nurses exhibited depressive symptoms among 865 Chinese nurses.10 The depressive symptoms are more likely to occur among nurses than among the general population, which have become the major public health issues in most developed and developing countries.
There is considerable epidemiological evidence confirming that a positive correlation between sleep disturbance and depressive symptoms.11–13 Nurses are vulnerable to sleep disturbance owing to night shift work schedules, high workload, occupational stress, burnout, and a lack of social and family support.14,15 It has been reported in a recent study that 63.9% of Chinese nurses working in general hospital experienced disturbed sleep.16 Sleep disturbance is associated with depressive status17 and correlated with increased negative emotional state,18 which may in turn have significant influence on their mental status, further worsening depressive symptoms.19–21
Researchers have proposed to apply the Conservation of Resources (COR) theory into studies of work and stress in organizational circumstances22 and found that increase of resource is a critical component of the management of stress in organizations and successful prevention and can promote occupational well-being. Positive resources have been acknowledged to prevent the prevalence of mental disorders and enhance the physical health for employees by strengthening their psychological resources. Recovery experiences, as a new concept of positive resources that an individual can utilize when managing a stressful situation, is referred as “a process of change to restore resources such as self-esteem or vigour that may be depleted in unfavorable work environments” and can be mobilized to promote restoration of impaired mood when confronting with a stressful situation and return functioning systems to their pre-stressor state.23–26 Sonnentag and Frize argue that it is critical for employers to enhance recovery experience.25 Recovery experience may help nurses to combat negative emotions, reduce occupational fatigue and exhaustion, and relieve the symptoms of sleep disturbance through positive adjustment process of “psychological detachment, relaxation, mastery experiences and control” to manage the stressful situations in clinical settings, and ultimately may attenuate depressive symptoms.17,25,27–31
There has been a paucity of studies on the relationships among depressive symptoms, recovery experience, and sleep disturbance among female nurses in Chinese public hospitals. The aim of this study is to investigate female nurses’ depressive symptoms and examine the relationship between depressive symptoms, recovery experience, and sleep disturbance. And this study may help provide effective evidence of intervention on the decrease of depressive symptoms. It is of great significance for improving nurses’ mental health and quality of health services as well as enhancing the treatment outcomes for patients. The hypotheses of this study are 1. Greater severity of sleep disturbance would be predictive of higher depressive symptoms. 2. Recovery experience would have a direct impact on relieving depressive symptoms. 3. Recovery experience would mediate the relationship between sleep disturbance and depressive symptoms.
Materials and Methods
Participants and Sampling
The study with proportional sampling of cross-sectional design was carried out from December 2017 to May 2018, in the public tertiary hospitals from Shenyang of Liaoning Province in China. Based on the geographic distribution of Shenyang, two hospitals from each region of eastern, western, southern, and northern part of Shenyang were randomly selected. In each hospital, 30% of the nurses were randomly selected. About 1500 female nurses with the ages of 18–65 years old who had been working for one or more years participated in this study. Questionnaires were self-administered on a mobile phone and pertained to demographic characteristics, sleep disturbance, recovery experiences, and depressive symptoms, lasting approximately 20 mins. Before the questionnaire was started, participants’ informed consent was obtained. A total of 1068 nurses took part in this study, resulting in an effective response rate of 71.2%.
Ethical Considerations
Each participant was well informed of the aims and contents of the questionnaire. The research was carried out in accordance with the Helsinki Declaration as revised in 1989, and the Ethics Committee of China Medical University approved the protocols of this study.
Instruments
Demographic Characteristics of the Participants
Demographic characteristics included the variables of age, educational level, marital status, and monthly income. “Marital status” was grouped into “married or cohabitating” and “others” including unmarried, separated, and divorced. “Educational level” was categorized into “junior college degree or lower” and “bachelor degree or higher”. “Monthly income” referred to “less than 3000 RMB” and “equal to or more than 3000 RMB”.
Sleep Disturbance
The PROMIS Sleep Disturbance Short Form with 8 items, was used to assess sleep disturbance.32 The respondents were asked to evaluate the severity of sleep disturbance in the past seven days with 5-point options for the scale. The original scores were summarized to obtain the total original score, which ranged from 8 to 40. Then, the original score was converted to a standardized T-score, with higher scores revealing more serious sleep disturbance.33 The Cronbach’s alpha of this scale was 0.91, which indicates that it has a good reliability. And previous study’s Cronbach’s alpha was 0.819.34
Recovery Experience
The Recovery Experience Questionnaire (REQ)25 was used to evaluate the levels of recovery experience. This scale consisted of 16 items, which was categorized into four dimensions of psychological detachment, relaxation, mastery experiences, and control. Each item on the measurement was rated on 5-point Likert scale (with the option of “never”, “rarely”, “sometimes”, “often”, and “always”) Higher scores indicate better recovery experience. The Cronbach’s alpha of overall REQ was 0.90, indicating REQ with a good reliability. The Cronbach’s alpha coefficients of psychological detachment, relaxation, mastery experiences, and control were 0.80, 0.87, 0.81, and 0.83, respectively. And previous study’s Cronbach’s alpha of overall REQ was 0.95.35
Depressive Symptoms
The Patient Health Questionnaire depression scale (PHQ-9) with a total of 9 items was employed to make an assessment of depressive symptoms, which had comparable sensitivity and specificity with many other depression scales.2,36 All the items are assessed on a four-point Likert scale with a range in total score from 0 to 27 and each item as “0” (not at all) to “3” (nearly every day). There was a summarized question in PHQ-9 scale: “How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?” The PHQ-9 has a good reliability, with the Cronbach’s alpha of 0.90 for this scale. And previous study’s Cronbach’s alpha was 0.88.37
Statistical Analysis
Statistical Package for Social Science Version 17.0 was applied to conduct the statistical analyses. T-tests and ANOVAs were used to compare the difference of depressive symptoms among categorical variables. The Spearman correlation was used to explore the correlations of sleep disturbance, recovery experience, and depressive symptoms. Hierarchical Multiple Regression (HMR) analysis was used to test the predictors and mediators of depressive symptoms. In order to examine the incremental contributions of the independent variables, they were entered, respectively, as follows: Step 1: demographic characteristics of the nurses; Step 2: sleep disturbance; Step 3: recovery experience. The contributions to the HMR models were tested with blocks of independent variables entered in later stages.2,38 The mediating effect of recovery experience between the relationship of sleep disturbance and depressive symptoms was confirmed with Structural Equation Model (SEM), which analyzed by Amos 17.0. The dependent variable was the depressive symptoms, with the sleep disturbance as the independent variable and recovery experience as the mediator in SEM, fitted with the SEM criteria (χ2/df < 5, GFI > 0.90, CFI > 0.90, RMSEA < 0.08, and TLI > 0.90). Bootstrapping was employed to examine the mediator (a*b product) of recovery experience between the relationship of sleep disturbance and depressive symptoms, with the estimate of 5000 samples. The bias-corrected and accelerated 95% confidence interval (BCa 95% CI) for a*b estimates were tested, with the statistical significance of a two-tailed probability value of less than 0.05.
Results
Demographic Characteristics of the Nurses
The Chinese female nurses’ demographic characteristics are illustrated in Table 1. The nurses’ average age was 32±8 years old. The majority (68.4%) of the nurses were married or cohabiting. Approximately 68.7% of the nurses were with the educational level of bachelor degree or higher, and nearly two-thirds (65.9%) of the nurses reported with a monthly income of 3000 RMB and more. Nearly seven in tenths (69.1%) of the Chinese female nurses suffered from depressive symptoms. Depressive symptoms were significantly worse in individuals with monthly income of less than 3000 RMB (Table 1).
Table 1.
Demographic Characteristic of Female Nurses (N = 1068)
| N (%) | Depressive Symptoms | |
|---|---|---|
| Age | ||
| ≤30 | 555(52.0) | 7.70±5.72 |
| >30 | 513(48.0) | 7.49±5.37 |
| Marital status | ||
| Married or cohabiting | 730(68.4) | 7.53±5.29 |
| Others | 338(31.6) | 7.75±6.08 |
| Educational level | ||
| Junior college or lower | 334(31.3) | 7.48±5.93 |
| Bachelor or higher | 734(68.7) | 7.66±5.38 |
| Monthly income | ||
| <3000 RMB | 364(34.1) | 8.38±5.65** |
| ≥3000 RMB | 704(65.9) | 7.20±5.46 |
Note: **P<0.01.
Correlations Among Sleep Disturbance, Recovery Experience, and Depressive Symptoms
As shown in Table 2, depressive symptoms were significantly linked with sleep disturbance and recovery experience. Sleep disturbance was positively correlated with depressive symptoms (P < 0.01). Psychological detachment in recovery experience had a significantly positive correlation with sleep disturbance (P<0.01) and depressive symptoms (P<0.01). Whereas, relaxation, mastery experience, and control in recovery experience were significantly and negatively correlated with sleep disturbance (P<0.01) and depressive symptoms (P<0.01).
Table 2.
The Correlation Among Sleep Disturbance, Recovery Experience, and Depressive Symptoms
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Depressive symptoms | 7.60 | 5.55 | 1 | |||||
| 2. Sleep disturbance | 49.67 | 9.76 | 0.579** | 1 | ||||
| 3. Psychological detachment | 7.84 | 3.22 | 0.115** | 0.127** | 1 | |||
| 4. Relaxation | 11.70 | 3.73 | −0.261** | −0.281** | 0.343** | 1 | ||
| 5. Mastery experiences | 12.16 | 3.49 | −0.283** | −0.263** | 0.247** | 0.658** | 1 | |
| 6. Control | 12.89 | 3.87 | −0.336** | −0.307** | 0.202** | 0.690** | 0.686** | 1 |
Note: **P < 0.01.
Regression Analysis of Sleep Disturbance, Recovery Experience, and Depressive Symptoms
The HMR results of depressive symptoms are depicted in Table 3. The final HMR model explained a total of 37.9% of the variance in depressive symptoms. According to the R2 change, sleep disturbance contributed most to the variance of the dependent variable (32.9%). Sleep disturbance, psychological detachment, mastery experiences, and control were strong predictors of depressive symptoms. In addition, depressive symptoms were positively associated with sleep disturbance and psychological detachment and negatively associated with mastery experiences and control.
Table 3.
The HMR Models of Depressive Symptoms
| MODEL1(B) | MODEL2(B) | MODEL3(B) | |
|---|---|---|---|
| BLOCK1 Demographic characteristics | |||
| Age | −0.034 | −0.023 | −0.031 |
| Marital status (Married or cohabiting vs Others) | 0.005 | −0.016 | −0.031 |
| Educational level (Junior college or lower vs Bachelor or higher) | −0.028 | −0.020 | −0.022 |
| Monthly income (<3000 RMB vs ≥3000 RMB) | 0.093** | 0.057* | 0.047 |
| BLOCK2 Sleep disturbance | 0.575** | 0.494** | |
| BLOCK3 Recovery experience | |||
| Psychological detachment | 0.102** | ||
| Relaxation | −0.012 | ||
| Mastery experiences | −0.071* | ||
| Control | −0.149** | ||
| R2 | 0.012 | 0.340 | 0.379 |
| ΔR2 | 0.012 | 0.329 | 0.039 |
Notes: *P < 0.05, **P < 0.01.
Mediator of Recovery Experience Between Sleep Disturbance and Depressive Symptoms
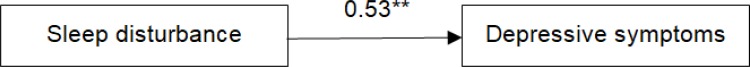
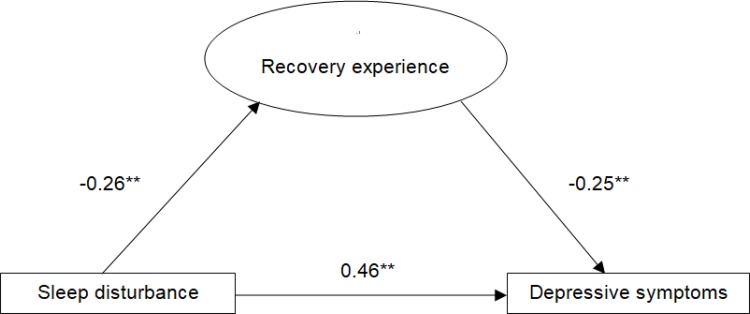
The path coefficients for the SEM analysis are shown in Table 4. The standardized solution for SEM is shown in Figures 1 and 2. As hypothesized, sleep disturbance had a significant direct influence on depressive symptoms (c = 0.53, P < 0.01). The SEM implied that sleep disturbance was positive associated with the dependent variable (β = 0.46, P < 0.001) and this model had good model fit indices (χ2/df < 5, RMSEA = 0.060, CFI = 0.967, GFI = 0.942, AGFI = 0.919, and TLI = 0.959) (Figure 1). Recovery experience tended to be significantly associated with depressive symptoms (β = −0.25, P < 0.001). Moreover, when recovery experience was modeled as a mediator (Figure 2), the path coefficient of sleep disturbance with depressive symptoms decreased significantly (c = 0.46, P < 0.01). The direct path coefficient of sleep disturbance on depressive symptoms was reduced or loss of statistical significance after adding the mediator of recovery experience, which indicated that the mediation effect was confirmed. The SEM also showed that recovery experience significantly mediated the association of sleep disturbance with depressive symptoms (a * b = 0.066, BCa 95% CI: 0.045, 0.095) (Figure 2), which confirmed that recovery experience acted as the mediator between sleep disturbance and depressive symptoms, with a goodness of model fit indices (χ2/df < 5, RMSEA = 0.060, CFI = 0.954, GFI = 0.924, AGFI = 0.901, and TLI = 0.946).
Table 4.
The Path Coefficients for the Structural Equation Model
| B | β | S.E. | C.R. | P | |||
|---|---|---|---|---|---|---|---|
| Recovery experience | ← | Sleep disturbance | −0.33 | −0.26 | 0.051 | −6.596 | *** |
| Depressive symptoms | ← | Recovery experience | −0.12 | −0.25 | 0.018 | −6.773 | *** |
| Depressive symptoms | ← | Sleep disturbance | 0.29 | 0.46 | 0.021 | 13.726 | *** |
Note: ***P < 0.001.
Abbreviations: B, the unstandardized path coefficient; β, the standardized path coefficient; S.E., the standard error; C.R., the critical ratio; P, the significance level.
Figure 1.
Standardized solutions for the structural equation model of sleep disturbance and depressive symptoms. **Indicating the coefficient of the path is significant.
Figure 2.
Standardized solutions for the structural equation model of recovery experience, sleep disturbance, and depressive symptoms. **Indicating the coefficient of the path is significant.
Discussion
This study, as far as our knowledge goes, is the first attempt to explore the mediating role of recovery experience on the association between sleep disturbance and depressive symptoms among Chinese female nurses. The results of this study revealed that Chinese female nurses frequently suffered from depressive symptoms (69.1%), which appears to be higher compared with Chinese physicians (46.9%),39 Chinese nurses (61.7%), and South Korean nurses (38%).3,40 The Chinese female nurses might be vulnerable to the detrimental effects of sleep disturbance on symptoms of depression. It has also been revealed that sleep disturbance was the strongest predictor of depressive symptoms and their association was partially mediated by recovery experiences. Significant associations have been observed between recovery experiences such as psychological detachment, mastery experiences, and control and depressive symptoms. Moreover, recovery experiences were found to mediate the effect of sleep disturbance on depressive symptoms. This research implied that recovery experience could alleviate the detrimental impacts of sleep disturbance on the prevalence of depressive symptoms for Chinese female nurses which supported the contention that positive resources such as recovery experiences could replenish the individuals’ vigor and energy and improve health and well-being.22
Notably, it was found that sleep disturbance had the strongest relationship to depressive symptoms, which confirmed the findings of prior research.19–21 Sleep disturbance, including interference occurring in the process of calming indispensable for adequate sleep, might lead to the cognitive slowing, poor memory, slow reactions, irritability, and ultimately is more likely to result in depressive symptoms.16 Sleep disturbance might also result in the disruption of circadian regulation, development of a negative emotional state, and reduction of social activities, which subsequently gives rise to increased risk of depressive symptoms.18 Longitudinal studies have demonstrated the link between sleep disturbance and higher likelihood of developing depression.11–13 This study indicated that the higher the sleep disturbance, the more severe the depressive symptoms among the nurses, which confirmed the finding of prior research that the deterioration of sleep quality was highly correlated with depressive symptoms.12,13 Therefore, intervention on sleep disturbance for the nurses is of great significance in alleviating their prevalence of depressive symptoms.
Furthermore, sleep disturbance not only had a direct effect on depressive symptoms but also had an indirect effect of sleep disturbance on depressive symptoms through the mediating path of recovery experience. As for the positive psychological resource, recovery experience, which includes psychological detachment, mastery experiences, and control, was also a significant predictor of depressive symptoms and played a partial mediating role in the relationship between sleep disturbances and depressive symptoms. This study indicated that recovery experience combated the adverse effect of sleep disturbance on depressive symptoms among nurses in China. Several studies have shown that recovery experience appeared to be protective against sleep problems and decrease the likelihood that depressive symptoms will arise.29–31 This is consisting with the research on the recovery experience which yielded various findings on the health of employers and has been found to alleviate occupational stress and help maintain the well-being in the working environment.26 Recovery experience could help female nurses to recover from their impaired emotions, replenish their vitality, and assist in participating in relaxation activities and relieving detrimental effects caused by stressors in the working environment,22–26 as well as improving sleep quality and ultimately decrease the risk of depressive symptoms.29–31 and hence, their physical and mental health and well-beings would be elevated.22 This study indicated that improving the resource of recovery experience could help the nurses to combat with sleep disturbance and attenuate the harmful effects of sleep disturbance on depressive symptoms. In the present study, a positive association has also been found between psychological detachment and depressive symptoms, whereas negative associations have been revealed between both mastery and control experiences and depressive symptoms. Psychological detachment can be viewed as the experience of an individual detaching from the environment in which he or she works.41 That indicates the individuals avoid thinking about work-related issues during off-work time, with not only the soma getting away from the work but also the psycho temporally switching off the work.42 Psychological detachment can promote well-being and work engagement of workers,43,44 and their emotion resources are no longer taxed and would be more positive with it.22 Notably, this study found that psychological detachment was positively associated with depressive symptoms, which was contrary to the existing literature revealing that psychological detachment acted as the protecting role for the well-being.43,44 The possible reason is that when the nurses are confronted with high demands at work, they may be more likely to constantly think about their job in order to find the solutions to the problems originating from job demands.29 They cannot completely get away from work physically and mentally,29,42 as a result, psychological detachment cannot be realized. Moreover, Shimazu’s research indicated that being a workaholic would inhibit psychological detachment in the off-job domain.45 Therefore, these nurses may be afflicted with sleep problems caused by lack of psychological detachment, and ultimately resulting in prevalence of depressive symptoms. Besides, mastery experiences refer to the challenging activities outside of work that can stimulate interests in acquiring knowledge and give rise to a sense of accomplishment.25 Although taking part in these activities requires effort and energy, mastery experiences could provide opportunities and challenges for female nurses to recover from job-related strains and replenish positive resources which may contribute to health and well-being improvement,25 and this would help female nurses protect against the sleep disturbance and could stop the progression of depressive symptoms. Additionally, the individuals with control can decide the degree of what to do, when and how to do.25 At the same time, it can be used as a positive resource to improve recovery from work. Sonnentag and Fritz indicated that mastery experiences and control had been demonstrated to have negative associations with emotional exhaustion,25 they might help alleviate sleep disturbance, thus, resulting in the protection from depressive symptoms. Meanwhile, Sonnentag indicated that control had negative correlation with depressive symptoms.25 Therefore, control could alleviate the negative effects of sleep disturbance on depressive symptoms. Psychological and educational implications are debated in the light of the results of this study, proposing interventions on the recovery promotion especially on the management of psychological detachment and enhancement of mastery experiences and control are necessary to ameliorate the effect of sleep disturbance on depressive symptoms among female nurses in China.
Female nurses might benefit from the intervention on recovery experience in order to relieve negative effects caused by stressors at work, alleviate sleep disturbance, and ultimately reduce the risk of depressive symptoms. Future study should focus on the randomized control trials on recovery experience enhancement to examine its effectiveness and application in the management of health workforce.
Limitations
Although a large number of female nurses with a high response rate (71.2%) indicated that this study’s population has great representativeness, which can increase the universality of our research conclusions, the cross-sectional study bears the limitation that the mechanism cannot be examined between sleep disturbance, recovery experience, and depressive symptoms. Additionally, depressive symptoms and sleep disturbance are the complex constructs, in which a good number of potentially confounding data and variables have not been captured in this study. And this study was only conducted in Shenyang, China, which may not allow for the generalizability of the results among nurses in other areas.
Conclusion
This study revealed 69.1% of female nurses in China were subject to depressive symptoms and also provided new evidence on strong predictive role of sleep disturbance for depressive symptoms. Moreover, recovery experience was found to combat the detrimental effects of sleep disturbances on depressive symptoms through the meditational path of increasing the resources of psychological detachment, mastery experience, and control. The findings of this study suggest that efforts to reduce depressive symptoms among nurses might be fruitful through sleep disturbance interventions and recovery skills training.
Acknowledgments
The authors thank Professor Fritz, who authorizes the scale of The Recovery Experience Questionnaire.
Abbreviations
SEM, Structural Equation Model; COR, Conservation of Resources; REQ, Recovery Experience Questionnaire; PHQ-9, Patient Health Questionnaire depression scale; HMR, Hierarchical Multiple Regression.
Data Sharing Statement
Data supporting the findings presented in the current study will be available from the corresponding author upon request.
Ethics and Consent Statement
The study was approved by the Ethical Research Committee of China Medical University. The study was performed in accordance with the Helsinki Declaration as revised in 1989. All of the subjects completed an informed consent form, and their data were anonymized.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Murray CJ, Lopez AD. Evidence-based health policy—lessons from the global burden of disease study. Science. 1996;274(5288):740–743. doi: 10.1126/science.274.5288.740 [DOI] [PubMed] [Google Scholar]
- 2.He SC, Wu S, Wang C, et al. Interaction between job stress and the BDNF Val66Met polymorphism affects depressive symptoms in chinese healthcare workers. J Affect Disord. 2018;236:157–163. doi: 10.1016/j.jad.2018.04.089 [DOI] [PubMed] [Google Scholar]
- 3.Gao YQ, Pan BC, Sun W, Wu H, Wang JN, Wang L. Depressive symptoms among chinese nurses prevalence and the associated factors. J Adv Nurs. 2012;68(5):1166–1175. doi: 10.1111/j.1365-2648.2011.05832.x [DOI] [PubMed] [Google Scholar]
- 4.Thun E, Bjorvatn B, Torsheim T, Moen BE, Magerøy N, Pallesen S. Night work and symptoms of anxiety and depression among nurses: a longitudinal study. Work Stress. 2014;28(4):376–386. doi: 10.1080/02678373.2014.969362 [DOI] [Google Scholar]
- 5.Liu J, Fan DY. An analysis of the current situation of male nurses in china and the countermeasures. Sci Tech Inf Gansu. 2015;44(04):53-54+14. [Google Scholar]
- 6.Neitzke, Alex B. An illness of power: gender and the social causes of depression. Culture, Med, Psychiatry. 2016;40(1):59–73. doi: 10.1007/s11013-015-9466-3 [DOI] [PubMed] [Google Scholar]
- 7.Hao J, Wu D, Liu L, Li X, Wu H. Association between work-family conflict and depressive symptoms among Chinese female nurses: the mediating and moderating role of psychological capital. Int J Environ Res Public Health. 2015;12(6):6682–6699. doi: 10.3390/ijerph120606682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu H, Chi TS, Chen L, Wang L, Jin YP. Occupational stress among hospital nurses: cross-sectional survey. J Adv Nurs. 2010;66(3):627–634. doi: 10.1111/j.1365-2648.2009.05203.x [DOI] [PubMed] [Google Scholar]
- 9.Jiang Y, Shen N, Yan RG. Analysis and advice of nursing human resources in China. J Nurs. 2004; Admin. 4,19–21 In Chinese. [Google Scholar]
- 10.Dai C, Qiu H, Huang Q, et al. The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatr Dis Treat. 2019;15:435–440. doi: 10.2147/NDT.S190689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32(9):664–670. doi: 10.1002/da.2015.32.issue-9 [DOI] [PubMed] [Google Scholar]
- 12.Ehlers CL, Frank E, Kupfer DJ. Social Zeitgebers and biological rhythms. a unified approach to understanding the etiology of depression. Arch Gen Psychiatry. 1988;45(10):948–952. doi: 10.1001/archpsyc.1988.01800340076012 [DOI] [PubMed] [Google Scholar]
- 13.Baglioni C, Battagliese G, Feige B. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–19. doi: 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 14.Klein M, Wobbe-Ribinski S, Buchholz A, Nienhaus A, Schablon A. Nurse-work instability and incidence of sick leave – results of a prospective study of nurses aged over 40. J Occup Med Toxicol. 2018;13(1):31. doi: 10.1186/s12995-018-0212-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gershon RR, Stone PW, Zeltser M, Faucett J, MacDavitt K, Chou SS. Organizational climate and nurse health outcomes in the United States: a systematic review. Ind Health. 2007;45(5):622–636. doi: 10.2486/indhealth.45.622 [DOI] [PubMed] [Google Scholar]
- 16.Dong H, Zhang Q, Sun Z, Sang F, Xu Y. Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry. 2017;17(1):241. doi: 10.1186/s12888-017-1402-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry. 2017;78(7):882–888. doi: 10.4088/JCP.15m10206 [DOI] [PubMed] [Google Scholar]
- 18.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–708. doi: 10.1016/j.jpsychires.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Duffy JF, De Castillero ER. Do sleep disturbances mediate the association between work-family conflict and depressive symptoms among nurses? A cross-sectional study. J Psychiatr Ment Health Nurs. 2017;24(8):620–628. doi: 10.1111/jpm.2017.24.issue-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernando AT, Samaranayake CB, Blank CJ, Roberts G, Arroll B. Sleep disorders among high school students in New Zealand. J Prim Health Care. 2013;5(4):276–282. doi: 10.1071/HC13276 [DOI] [PubMed] [Google Scholar]
- 21.Cheung T, Yip P. Depression, anxiety and symptoms of stress among Hong Kong nurses: a cross-sectional study. Int J Environ Res Public Health. 2015;12(9):11072–11100. doi: 10.3390/ijerph120911072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hobfoll SE. Conservation of resources. A new attempt at conceptualizing stress. Am Psychol. 1989;44(3):513–524. doi: 10.1037/0003-066X.44.3.513 [DOI] [PubMed] [Google Scholar]
- 23.Poulsen MG, Poulsen AA, Khan A, Poulsen EE, Khan SR. Recovery experience and burnout in cancer workers in Queensland. Eur J Oncol Nurs. 2015;19(1):23–28. doi: 10.1016/j.ejon.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 24.Meijman TF, Mulder G. Psychological aspects of workload In: Drenth PJD, Thierry H, de Wolff CJ, editors. Handbook of Work and Organizational Psychology: Vol. 2. Work Psychology. Hove: PsychologyPress; 1998:5–33. [Google Scholar]
- 25.Sonnentag S, Fritz C. The recovery experience questionnaire: development and validation of a measure for assessing recuperation and unwinding from work. J Occup Health Psychol. 2007;12(3):204–221. doi: 10.1037/1076-8998.12.3.204 [DOI] [PubMed] [Google Scholar]
- 26.He L, Zhang CL, Yang T, Lan YJ. Relationship between occupational stress, recovery experience, and physiological health of nurses in a municipal grade A tertiary hospital. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2017;35(6):425–428. doi: 10.3760/cma.j.issn.1001-9391.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 27.Hahn VC, Binnewies C, Sonnentag S, Mojza EJ. Learning how to recover from job stress: effects of a recovery training program on recovery, recovery-related self-efficacy, and well-being. J Occupy Health Psychol. 2011;16(2):202–216. doi: 10.1037/a0022169 [DOI] [PubMed] [Google Scholar]
- 28.Chen MG, Zhang J. Effect of recovery training on nurses′ sleep quality and work engagement. J Nurs Sci. 2019;34(06):44–47. [Google Scholar]
- 29.Shimazu A, Sonnentag S, Kubota K, Kawakami N. Validation of the japanese version of the recovery experience questionnaire. J Occup Health. 2012;54(3):196–205. doi: 10.1539/joh.11-0220-OA [DOI] [PubMed] [Google Scholar]
- 30.Fritz C, Yankelevich M, Zarubin A, Barger P. Happy, healthy and productive: the role of detachment from work during nonwork time. J Appl Psychol. 2010;95(5):977–983. doi: 10.1037/a0019462 [DOI] [PubMed] [Google Scholar]
- 31.Schwarz UVT. Inability to withdraw from work as related to poor next-day recovery and fatigue among women. Appl Psychol-Int Rev. 2011;60(3):377–396. doi: 10.1111/j.1464-0597.2011.00440.x [DOI] [Google Scholar]
- 32.Yu L, Buyssem DJ, Germain A, et al. Development of short forms from the PROMIS sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2011;10(1):6–24. doi: 10.1080/15402002.2012.636266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hanish AE, Lin-Dyken DC, Han JC. PROMIS sleep disturbance and sleep-related impairment in adolescents: examining psychometrics using self-report and actigraphy. Nurs Res. 2017;66(3):246–251. doi: 10.1097/NNR.0000000000000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deng JL. Study of Short Sleep Disorders (SDSF) in evaluating the effects of IMRT on sleep in patients with nasopharyngeal carcinoma. Guangxi Medical University; 2017. Available from: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201901&filename=1018156650.nh&uid=WEEvREcwSlJHSldRa1FhcEFLUmVhMFUybkNOdVd6STNhMVZBWGFaeWtRQT0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4IQMovwHtwkF4VYPoHbKxJw!!&v=MTAzMjFGMjZGcks5R05mSnI1RWJQSVI4ZVgxTHV4WVM3RGgxVDNxVHJXTTFGckNVUjdxZlpPZG1GeS9sVWI3TVY=. Accessed March 23, 2020. [Google Scholar]
- 35.Ding J, Jia Y, Zhao J, Ma R, Yang X. Optimizing quality of life among Chinese physicians: the positive effects of resilience and recovery experience. Qual Life Res. 2020. doi: 10.1007/s11136-020-02414-8 [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dadfar M, Kalibatseva Z, Lester D. Reliability and validity of the Farsi version of the patient health questionnaire-9 (PHQ-9) with iranian psychiatric outpatients. Trends Psychiatry Psychother. 2018;40(2):144–151. doi: 10.1590/2237-6089-2017-0116 [DOI] [PubMed] [Google Scholar]
- 38.Hong F, Zhang RR. The relationship between job requirements and employees’ occupational well-being: multiple mediating role of recovery experience. Manage Administration. 2017;7:33–36. [Google Scholar]
- 39.Jia H, Yu J, Xv MY, Guo CC, Li MY, Lan L. Depression/anxiety status of general hospital doctors and its correlation with doctor-patient tension. World Latest Med Inf. 2019;19(27):171-172+179. [Google Scholar]
- 40.Yoon SL, Kim JH. Job-related stress, emotional labor, and depressive symptoms among korean nurses. J Nurs Scholarsh. 2013;45(2):169–176. doi: 10.1111/jnu.12018 [DOI] [PubMed] [Google Scholar]
- 41.Etzion D, Eden D, Lapidot Y. Relief from job stressors and burnout: reserve service as a respite. J Appl Psychol. 1998;83(4):577–585. doi: 10.1037/0021-9010.83.4.577 [DOI] [PubMed] [Google Scholar]
- 42.Sonnentag S, Bayer UV. Switching off mentally: predictors and consequences of psychological detachment from work during off-job time. J Occup Health Psychol. 2005;10(4):393–414. doi: 10.1037/1076-8998.10.4.393 [DOI] [PubMed] [Google Scholar]
- 43.De Jonge J, Spoor E, Sonnentag S, Dormann C, van den Tooren M. “Take a break?!” Off-job recovery, job demands, and job resources as predictors of health, active learning, and creativity. Eur J Work Organ Psychol. 2012;21(3):321–348. doi: 10.1080/1359432X.2011.576009 [DOI] [Google Scholar]
- 44.Sonnentag S, Binnewies C, Mojza EJ. Staying well and engaged when demands are high: the role of psychological detachment. J Appl Psychol. 2010;95(5):965–976. doi: 10.1037/a0020032 [DOI] [PubMed] [Google Scholar]
- 45.Shimazu A, Jonge JD, Kubota K, Kawakami N. Psychological detachment from work during off-job time: predictive role of work and non-work factors in Japanese employees. Ind Health. 2014;52(2):141–146. doi: 10.2486/indhealth.2013-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]