Abstract
Objective:
To describe the incidence and progression of radiographic and symptomatic hand osteoarthritis (rHOA and sxHOA) in a large community-based cohort.
Design:
Data were from the Johnston County OA Project (1999-2015, 12 ±1.2 years follow-up, age 45+). Participants had bilateral hand radiographs each visit, read for Kellgren-Lawrence grade (KLG) at 30 joints. We defined rHOA as KLG ≥2 in ≥1 joint. SxHOA was defined in a hand/joint with rHOA and self-reported symptoms or tenderness on exam. Incidence was assessed in those without, while progression was assessed in those with, baseline rHOA. Proportions or medians are reported; differences by sex and race were assessed using models appropriate for dichotomous or continuous definitions, additionally adjusted for age, education, BMI, and weight change.
Results:
Of 800 participants (68% women, 32% African American, mean age 60 years), 327 had baseline rHOA and were older, more often white and female, than those without rHOA (n=473). The incidence of HOA was high, for rHOA (60%) and for sxHOA (13%). Women were more likely than men to have incident HOA, particularly for DIP rOA (aOR 1.60 95% CI [1.03, 2.49]) and sxHOA (aOR 2.98 [1.50, 5.91]). Progressive HOA was more similar by sex, although thumb base rOA progressed more frequently in women than in men (aOR 2.56 [1.44, 4.55]). Particularly HOA incidence, but also progression, was more frequent among whites compared with African Americans.
Conclusion:
This study provides much needed information about the natural history of HOA, a common and frequently debilitating condition, in the general population.
Keywords: Hand osteoarthritis, radiographs, epidemiology
The presentation of osteoarthritis (OA) varies immensely – affecting adults of all ages and involving different joints throughout the body.1 Although hand osteoarthritis (HOA) is exceedingly common and will affect 4 in 10 people by age 852, this joint site is understudied in comparison to other sites, like the knee. HOA is a heterogeneous disease that presents as bony enlargement and deformities of various joints in the hand.3 Patients may experience pain, stiffness and decreased mobility, which can result in decreased grip strength and functionality of the hand.4 As such, HOA can lead to significant disability and increased healthcare utilization.5
To date, studies of HOA are limited – particularly with regard to incidence and progression of disease in longitudinal cohorts. Review of the literature reveals that prevalence estimates of HOA in adults vary depending on the population studied and definitions used to define the disease. HOA can be defined radiographically and/or symptomatically, and such definitions can affect frequency estimates.6 For example, the Framingham OA Study estimated the frequency of symptomatic HOA as 13% in men and 26% in women > 70 years of age, but only includes white individuals.7 As the US population is aging, these data suggest more people will be affected by HOA in the future highlighting the need for better understanding of the natural history of this common condition, including differences by sex and race.
The purpose of this study was to utilize recent longitudinal data to describe the incidence and progression of radiographic and symptomatic HOA (rHOA and sxHOA, respectively) in a large community-based cohort of African American and white men and women.
Participants and Methods
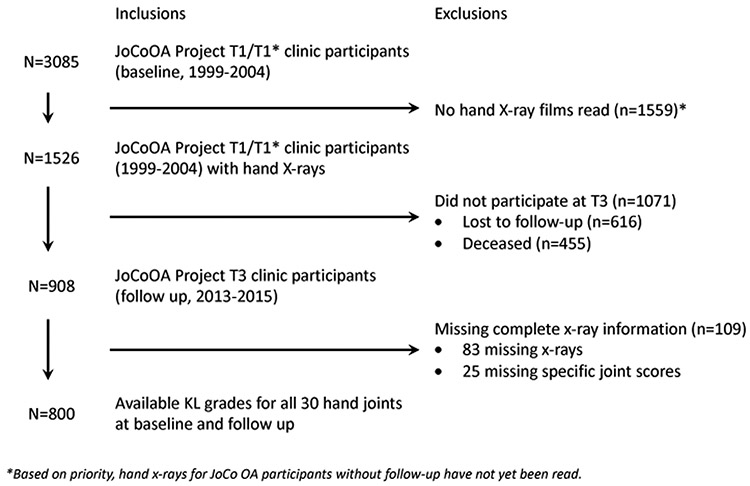
Data were obtained from adult participants (age ≥ 45 years) in the Johnston County Osteoarthritis Project (JoCo OA), an ongoing community-based prospective observational cohort study monitoring the occurrence and natural history of OA in Johnston County, North Carolina.8 JoCo OA enrolled non-institutionalized white and African American adults age 45 and older who resided in 6 townships in the county in a population-based manner (without regard for symptoms or diagnosis). All participants provide informed consent, answer standardized questionnaires and undergo an examination with trained staff, in addition to radiography of multiple joint sites. This analysis included all participants at the third JoCo OA follow up (n=909, collected 2013-15), and included data from all prior time points with hand data for these individuals (first follow-up: 1999-2003 or cohort enrichment: 2003-4, and second [combined] follow up: 2006-10). After exclusion of 109 participants due to missing radiographs over time (n=84) or missing any of the 30 specific joint scores over time (n=25), 800 participants were included in the complete case analysis (Figure 1).
Figure 1.
Flow chart of participant inclusion in the current analysis
Sex, race, and age were from self-report at baseline. Educational attainment at baseline was categorized as completing less than a high school education vs at least a high school education. Body mass index (BMI) at baseline was computed from measured standing height (cm) and weight (kg) during the research clinic visit. Weight gain from baseline (T1) to second follow-up (T3) was defined as more than a 5% increase in BMI.
All participants had posteroanterior radiographs of the bilateral hands at each visit, read together in known time order9, 10 by an experienced musculoskeletal radiologist (JBR) using the Kellgren-Lawrence grading (KLG) system11 for all 30 joints (bilateral distal interphalangeal [DIP] 2-5; proximal interphalangeal [PIP] 2-5; metacarpophalangeal [MCP] 1-5; interphalangeal [IP] and carpometacarpal [CMC] of the thumb). The radiologist has previously demonstrated high reliability (kappa >0.7), detailed by joint in a prior paper.2 Erosive OA was not systematically assessed in this study, but noted only as a comment and appeared to be relatively uncommon in this sample (9 participants). Therefore, erosive OA was not analyzed separately, although these participants were included in the analyses for other outcomes.
There are many ways to define rHOA.12 For these analyses, we considered several definitions. First, rHOA overall was defined as a KLG of 2 or more in at least 1 of the 30 hand joints. Additionally, rOA by joint group (DIP, PIP, thumb IP, MCP, or CMC, involving at least one joint in the group) and rHOA affecting 2 or more joints was assessed. We also considered the number of joints affected by KLG of 2 or more and the sum score of KLG (0-4 at each joint) across all 30 joints (range 0-120). SxHOA was defined as the presence of symptoms defined in one of two ways with rOA in the same hand or specific joint site. First, self-reported pain, aching or stiffness in the entire hand was assessed using the answer to “On most days, do you have pain, aching, or stiffness in your hands” at baseline, which was modified at follow up to: “On most days of any one month in the last twelve months, did you have pain, aching, or stiffness in your hands?” at follow up, both with indicators for right or left hand. Second, tenderness to palpation at each of the 30 hand joints during the research exam was assessed (previously shown to be reliable, with agreement >0.9 for two trained readers1). We additionally considered the number of joints with sxHOA.
Two groups were defined: those with baseline rHOA (KLG of 2 or more in at least 1 of the 30 hand joints) and those without. Among those without baseline rHOA, we defined incident rHOA as newly meeting the above criteria in a hand or joint previously without rOA. Among those with baseline rHOA, progression was defined as an additional joint involved, either overall or in a given joint group for both rHOA and sxHOA. We again considered the overall number of rHOA joints and sxHOA joints as well as the total sum KLG for progression.
Incidence and progression were assessed over an average of 12 years involving a baseline (either first follow up: 1999-2004 or cohort enrichment: 2003-4) and two combined follow-up time-points (2006-2010 and 2013-2015). Descriptive statistics were shown as proportions for dichotomous variables and medians (interquartile range) for continuous variables.
Most incidence and progression differences between sex and race were assessed by modeling dichotomous definitions with logistic regression and producing adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) describing associations. For continuous definitions (consisting of skewed count distributions) either zero-inflated negative binomial, scaled negative binomial or scaled regression models were used to produce adjusted incidence density ratios (aIDR) or adjusted betas (β) and 95% CI describing associations. Models were adjusted for age, sex, race, education, BMI, weight gain of 5% or more, and HOA baseline values (for progression only).
Results
Of the 800 included participants (Figure 1), 68% were women and 32% were African American (Table 1). The mean age of the sample was 59.6 (standard deviation ± 7.5) years, and the mean body mass index (BMI) was 31.0 ± 6.4 kg/m2. Those with baseline rHOA (n=327, 41% of the sample) tended to be older (63 ± 7 vs 57 ± 7 years) and were more often white (80% vs 61%) and women (72% vs 65%) than those without baseline rHOA (n=473, 59% of the sample). Socioeconomic status as represented by education level did not differ between groups, nor did the proportion experiencing weight gain over the course of the study (Table 1).
Table 1.
Descriptive characteristics of the sample overall and by baseline hand OA status
| Sample Characteristics |
Overall (n=800) | No baseline hand OA (n=473) |
Baseline hand OA (n=327) |
|---|---|---|---|
| mean (SD) or % | mean (SD) or % | mean (SD) or % | |
| Age, years | 59.6 (7.5) | 57.3 (6.6) | 63.1 (7.4) |
| Female, % | 68.0 | 65.3 | 71.9 |
| African American, % | 31.5 | 39.5 | 19.9 |
| <12 years education, % | 13.8 | 13.8 | 13.8 |
| Baseline body mass index, kg/m2 | 31.0 (6.4) | 31.6 (6.7) | 30.2 (5.9) |
| >5% weight gain from baseline to follow up, % | 32.6 | 33.4 | 31.5 |
Incident HOA
The frequencies of incident rHOA (≥1 or ≥2 joints), DIP rOA, PIP rOA, thumb IP rOA, and thumb base rOA were slightly higher among women, while men were more likely to have incident MCP rOA (Table 2). In adjusted models, women had statistically significantly greater odds of DIP rOA (aOR 1.60, 95% CI [1.03, 2.49]) and had, on average, 1.33 times the number of rHOA affected joints compared with men.
Table 2.
Proportions by hand OA incidence definition over ~ 12 (±1.2) year follow-up for those without baseline hand OA, by sex or race
| Hand OA incidence definition | Overall (n=473) |
Women (n=309) |
Men (n=164) |
Women vs Men* | White (n=286) |
African American (n=187) |
White vs AA* |
|---|---|---|---|---|---|---|---|
| % or median (interquartile range: Q1-Q3) |
effect (95% CI) | % or median (interquartile range: Q1-Q3) |
effect (95% CI) | ||||
| Radiographic HOA (≥1 joint(s)) | 59.4% | 60.5% | 57.3% | 1.26 (0.84, 1.90) | 65.0% | 50.8% | 2.26 (1.49, 3.43) |
| DIP (2nd – 5th) OA | 32.1% | 34.0% | 28.7% | 1.60 (1.03, 2.49) | 40.2% | 19.8% | 3.16 (1.97, 5.07) |
| PIP (2nd – 5th) OA | 20.1% | 21.4% | 17.7% | 1.24 (0.82, 1.87) | 22.7% | 16.0% | 1.17 (0.77, 1.77) |
| Thumb IP OA | 24.5% | 24.9% | 23.8% | 1.02 (0.64, 1.61) | 23.1% | 26.7% | 0.87 (0.55, 1.37) |
| MCP (1st – 5th) OA | 13.5% | 11.7% | 17.1% | 0.59 (0.34, 1.04) | 13.6% | 13.4% | 1.08 (0.60, 1.95) |
| Thumb base OA | 20.7% | 22.3% | 17.7% | 1.59 (0.96, 2.64) | 24.1% | 15.5% | 2.11 (1.24, 3.58) |
| Radiographic HOA (≥2 joint(s)) | 31.7% | 33.0% | 29.3% | 1.18 (0.78, 1.79) | 35.3% | 26.2% | 1.60 (1.05, 2.45) |
| Symptomatic HOA (≥1 joint(s)) | 12.9% | 15.9% | 7.3% | 2.98 (1.50, 5.91) | 17.1% | 6.4% | 4.29 (2.08, 8.86) |
| Number of radiographic HOA joints | 1 (0-3) | 1 (0-3) | 1 (0-2) | 1.33 (1.03, 1.72)1 | 1 (0-3) | 1 (0-2) | 2.00 (1.54, 2.61)1 |
| Number of symptomatic HOA joints | 0 (0-0) | 0 (0-0) | 0 (0-0) | 4.74 (2.08, 10.8)1 | 0 (0-0) | 0 (0-0) | 1.69 (0.41, 7.06)1 |
| Max=93 | Max=9 | Max=2 | Max=9 | Max=3 | |||
| Total sum KL score (30 joints) | At T3: | At T3: | At T3: | 0.99 (0.95, 1.03)2 | At T3: | At T3: | 1.00 (0.96, 1.04)2 |
| 11 (7-19) | 12 (8-19) | 11 (7-18) | 12 (8-20) | 11 (7-16) | |||
| Δ T3-T1: | Δ T3-T1: | Δ T3-T1: | Δ T3-T1: | Δ T3-T1: | |||
| 7 (4-12) | 7 (4-12) | 8 (4-11) | 8 (5-14) | 6 (3-9) |
Distal interphalangeal joint (DIP), Hand osteoarthritis (HOA), Interphalangeal joint (IP), Kellgren-Lawrence grade (KLG), Metacarpophalangeal joint (MCP), Osteoarthritis (OA), Proximal interphalangeal joint (PIP); Δ=change from T1 to T3 (baseline to follow up)
Effects shown are adjusted for baseline: age, sex, race, education, BMI, and weight gain—additionally adjusted for HOA baseline values for total sum KL score.
Logit models for categorical definitions producing adjusted odds ratios (aOR)
zero inflated negative binomial models for continuous definitions producing adjusted incidence density ratios (aIDR)
scaled negative binomial model for continuous definitions producing adjusted incidence density ratios (aIDR)
Incident sxHOA was significantly more likely in women (16% vs 7%), who also had more joints with sxHOA (but not rHOA) compared with men. Both differences were statistically significant in adjusted models, where women had nearly 3 times the odds of developing sxHOA and had 4.7 times more joints affected with sxHOA than men. The overall KLG sum score across all joints was similar by sex.
All definitions of rHOA and sxHOA were more common in white compared with African American participants, particularly for rHOA (≥1 joint), DIP OA, and thumb base OA (Table 2), all of which were at least twice as likely among whites in adjusted models. SxHOA was more than twice as frequent in white compared to African American participants (17% vs 6%), with an adjusted odds ratio over 4. The number of joints affected by rHOA or sxHOA, and the overall KLG sum, were also higher in white participants, although the adjusted IDR was only significant for number of joints with rHOA (aIDR 2.00 [1.54, 2.61]).
Progression of HOA
Progressive rHOA was seen at similar frequencies between men and women, except for MCP rOA, which more commonly progressed in men (58% vs 39%), and thumb base rOA, which progressed more often in women (61% vs 41%, Table 3). Only thumb base OA was statistically significant in adjusted models, where women had 2.5 times the odds of progression compared with men. Progressive rHOA and sxHOA were slightly but not statistically significantly more common in women compared with men. Women also had more joints involved with rHOA and sxHOA over time, although this was not significant in adjusted models.
Table 3.
Proportion by hand OA progression definition over ~ 12 (±1.2) year follow-up for those with baseline hand OA, by sex or race
| Hand OA progression definition |
Overall (n=327) |
Women (n=235) |
Men (n=92) |
Women vs Men* | White (n=262) |
African American (n=65) |
White vs AA* |
|---|---|---|---|---|---|---|---|
| % or median (interquartile range: Q1-Q3) |
effect (95% CI) | % or median (interquartile range: Q1-Q3) |
effect (95% CI) | ||||
| Radiographic HOA (additional in ≥1 joint(s)) | 94.2% | 94.0% | 94.6% | 0.70 (0.22, 2.22) | 95.4% | 89.2% | 1.15 (0.38, 3.45) |
| DIP (2nd – 5th) OA | n=306 | n=218 | n=88 | 1.26 (0.67, 2.37) | n=242 | n=64 | 1.39 (0.70, 2.76) |
| 77.8% | 79.4% | 73.9% | 81.0% | 65.6% | |||
| PIP (2nd – 5th) OA | n=318 | n=228 | n=90 | 1.38 (0.80, 2.37) | n=254 | n=64 | 0.94 (0.51, 1.76) |
| 63.5% | 66.2% | 56.7% | 65.0% | 57.8% | |||
| Thumb IP OA | n=286 | n=205 | n=81 | 0.80 (0.46, 1.37) | n=228 | n=58 | 1.30 (0.71, 2.40) |
| 56.3% | 54.2% | 61.7% | 57.9% | 50.0% | |||
| MCP (1st – 5th) OA | 44.0% | 38.7% | 57.6% | 0.61 (0.36, 1.05) | 44.7% | 41.5% | 0.96 (0.52, 1.77) |
| Thumb base OA | n=274 | n=193 | n=81 | 2.56 (1.44, 4.55) | n=215 | n=59 | 3.39 (1.74, 6.60) |
| 54.7% | 60.6% | 40.7% | 60.5% | 33.9% | |||
| Radiographic HOA (additional ≥2 joint(s)) | 80.4% | 81.3% | 78.3% | 1.11 (0.59, 2.10) | 82.4% | 72.3% | 1.08 (0.53, 2.18) |
| Symptomatic HOA (additional ≥1 joint(s)) | 31.0% | 31.9% | 28.6% | 1.25 (0.72, 2.16) | 32.4% | 25.0% | 1.96 (1.01, 3.83) |
| Number of radiographic HOA joints | At T3: | At T3: | At T3: | 1.17 (0.99, 1.39)1 | At T3: | At T3: | 1.12 (0.92, 1.36)1 |
| 9 (4-14) | 9 (5-15) | 8 (4-12) | 10 (5-15) | 6 (3-10) | |||
| ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | |||
| 5 (2-8) | 6 (3-9) | 5 (2-7) | 6 (3-8) | 4 (2-8) | |||
| Number of symptomatic HOA joints | At T3: | At T3: | At T3: | 0.23 (−0.34, 0.81)2 | At T3: | At T3: | 0.46 (−0.21, 1.12)2 |
| 0 (0-1) | 0 (0-2) | 0 (0-1) | 0 (0-1) | 0 (0-0) | |||
| ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | |||
| 0 (0-1) | 0 (0-1) | 0 (0-0) | 0 (0-1) | 0 (0-0) | |||
| Total sum KL score (30 joints) | At T3: | At T3: | At T3: | 1.09 (0.97, 1.24)1 | At T3: | At T3: | 1.09 (0.94, 1.26)1 |
| 34 (21-45) | 35 (22-47) | 32.5 (19-42) | 35 (23-47) | 27 (17-37) | |||
| ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | ΔT3-T1: | |||
| 16 (9-22) | 16 (10-23) | 14.5 (8.5-20.5) | 17 (10-22) | 13 (8-18) |
Distal interphalangeal joint (DIP), Hand osteoarthritis (HOA), Interphalangeal joint (IP), Kellgren-Lawrence grade (KLG), Metacarpophalangeal joint (MCP), Osteoarthritis (OA), Proximal interphalangeal joint (PIP); Δ=change from T1 to T3 (baseline to follow up)
Effects shown are adjusted for baseline: age, sex, race, education, BMI, weight gain, and HOA baseline values.
Logit models for categorical definitions producing adjusted odds ratios (aOR)
scaled negative binomial model for continuous definitions producing adjusted incidence density ratios (aIDR)
scaled regression models for the number of symptomatic HOA joints producing adjusted betas.
All measures of HOA progression were higher among whites compared with African Americans, although most were modestly so (Table 3). Thumb base rOA progression was significantly more frequent among white compared with African American participants (61% vs 34%), as was sxHOA progression (32% vs 25%, respectively); both remained significant in adjusted models. Additionally, the number of joints affected and the change in number of joints involved were slightly higher among whites compared with African Americans, although not statistically significant after adjustment.
Discussion
HOA remains understudied in comparison to other common sites of OA, like the hip and knee. While several studies have described the prevalence of hand OA in various populations, there have been surprisingly few analyses of the incidence and progression of OA in longitudinal, community-based cohorts. An understanding of the natural history of this common and often debilitating condition is essential to informing further study, including the development of new interventions. In this longitudinal, community-based cohort including African American and white men and women, we found high frequencies of new disease over an average of 12 years, particularly for rHOA (60%) but also for sxHOA (13%). For most joint sites, compared with men, women were somewhat more likely to have incident HOA, although the opposite was true at the MCP. The differences by race were more apparent, with white participants experiencing much higher frequencies of incident HOA by most definitions. HOA progression was similarly common, with rHOA progression occurring in the majority of the sample and sxHOA in about two out of every five (41%). Differences by sex were similar for progression and for incidence, while differences by race were somewhat less pronounced. Of note, more than 1/4 of the sample, regardless of subgroup, had progressive sxHOA with at least one additional joint involved over the follow-up period (28% of African Americans, 35% of men, 43% of whites and 44% of women), emphasizing the burden of this condition.
There are a few large cohort studies to which we can compare our findings. Haugen, et al13, using data from the Framingham OA Study (FOA, collected 1992-5 and 2002-5), reported 9-year cumulative incidence for similar definitions of HOA that were overall lower than those reported here (e.g., rHOA approximately 34%, PIP 5%, although thumb base OA was comparable at 17% in men and 21% in women). However, the pattern of sex differences was similar between the two studies. For progression over 9 years, the overall frequencies were fairly similar to the current report (e.g., rHOA progression in >90%), although DIP progression was slightly lower among women in the JoCo OA than in the FOA (74% vs. 78%, respectively) but higher in men, (72% in JoCo OA vs. 59% in FOA). Additionally, PIP and MCP progression were more common in JoCo OA compared with FOA. Thumb base OA progression was more frequent in FOA (<50% in JoCo OA, >60% in FOA), again with similar patterns by sex. Among individuals with hand pain but without baseline rHOA in the Clinical Assessment Studies of the Hand study14, the KLG sum (for 20 joints; no MCP) increased by 9 in women and 7 in men over 7 years, not dissimilar to the increase of 12 and 11 in the current analysis over 12 years (although the latter sum was for 30 joints). In the Genetics, Arthrosis and Progression study15, a family study of multiple joint OA, the pattern of progression was similar to the present study, with HOA progression most frequent in the DIPs, then CMC, PIP/IP and MCPs. In a few smaller studies in more specific populations, progression has been shown to be a common occurrence, although often modest in severity16-18. Of course, these are very different populations and utilized somewhat different methodologies so are not directly comparable. The fact that there are not more studies, and that there are none in diverse populations (all of the above studies were among whites), highlights the need for additional work in this area.
We have previously reported on the cross-sectional frequency of multiple joint OA phenotypes, including HOA, by race and sex in the JoCo OA.19, 20 We found that, compared to whites, African Americans were less likely to have phenotypes that included rHOA20 or sxHOA19, although they were more likely to have phenotypes involving one or more large joints. Additionally, the lifetime risk of sxHOA was lower among African Americans compared with whites in this cohort (29.2% vs. 41.4%).2 A large cross-sectional study in young (age 42-53) African American and white women nearly two decades ago found a similar prevalence of hand OA by race, although MCP OA was more common among African American (12%) compared with white (3%) women; African American women were also more likely to have both hand and knee OA (8% vs 2% of white women)21. Unfortunately, we are not aware of any other community-based studies including African Americans that are available for comparison, and the mechanisms behind these differences are not known.
Limitations of this work include small numbers in some categories which precluded more detailed modeling. As in most large cohorts, we have relatively infrequent assessments of symptoms, and are not able to model detailed fluctuations in symptoms over time. We focused on incidence and progression and did not separately analyze improvements in symptoms over time. However, the strengths, including the large overall sample size, the unique biracial cohort including both men and women, and the community-based nature of the cohort, make this an important contribution to the HOA literature.
In this large, longitudinal, community-based cohort inclusive of African American and white men and women, we found overall high frequencies of both incidence and progression of HOA over an average of 12 years of follow up. Although common across the board, the frequencies of incident and progressive HOA by a variety of definitions were generally higher in women compared with men and among whites compared with African Americans; differences were overall more marked for definitions of incidence than for progression. Additional studies are needed to understand potential mechanisms for the identified differences (e.g., occupational, genetic, nutritional, biomechanical, or other factors).
Acknowledgments:
We would like to thank the staff and participants in the Johnston County Osteoarthritis Project, without whom this work would not be possible.
Role of the funding source:
This work is funded in part by: CDC U01 DP006266 and DP003206, NIH/NIAMS P60 AR049465 and AR064166. The funding agencies had no role in the design, analysis, or interpretation of data, nor in the writing of the manuscript or the decision to submit it for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interest statement:
None of the authors has any competing interests in relation to this work.
References
- 1.Gullo TR, Golightly YM, Cleveland RJ, Renner JB, Callahan LF, Jordan JM, et al. Defining multiple joint osteoarthritis, its frequency and impact in a community-based cohort. Semin Arthritis Rheum 2019;48:950–957. doi: 10.1016/j.semarthrit.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qin J, Barbour KE, Murphy LB, Nelson AE, Schwartz TA, Helmick CG, et al. Lifetime Risk of Symptomatic Hand Osteoarthritis: The Johnston County Osteoarthritis Project. Arthritis Rheumatol 2017;69:1204–1212. doi: 10.1002/art.40097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis 2009;68:8–17. doi: 10.1136/ard.2007.084772. [DOI] [PubMed] [Google Scholar]
- 4.Michon M, Maheu E, Berenbaum F. Assessing health-related quality of life in hand osteoarthritis: a literature review. Ann Rheum Dis 2011;70:921–928. doi: 10.1136/ard.2010.131151. [DOI] [PubMed] [Google Scholar]
- 5.Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum 1995;38:1134–1141. [DOI] [PubMed] [Google Scholar]
- 6.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage 2011;19:1270–1285. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Niu J, Kelly-Hayes M, Chaisson CE, Aliabadi P, Felson DT. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: The Framingham Study. Am J Epidemiol 2002;156:1021–1027. [DOI] [PubMed] [Google Scholar]
- 8.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol 2007;34:172–180. [PubMed] [Google Scholar]
- 9.Felson DT, Nevitt MC. Blinding images to sequence in osteoarthritis: evidence from other diseases. Osteoarthritis Cartilage 2009;17:281–283. doi: 10.1016/j.joca.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gensburger D, Roux JP, Arlot M, Sornay-Rendu E, Ravaud P, Chapurlat R. Influence of blinding sequence of radiographs on the reproducibility and sensitivity to change of joint space width measurement in knee osteoarthritis. Arthritis Care Res (Hoboken) 2010;62:1699–1705. doi: 10.1002/acr.20311. [DOI] [PubMed] [Google Scholar]
- 11.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marshall M, Dziedzic KS, van der Windt DA, Hay EM. A systematic search and narrative review of radiographic definitions of hand osteoarthritis in population-based studies. Osteoarthritis Cartilage 2008;16:219–226. doi: 10.1016/j.joca.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Haugen IK, Englund M, Aliabadi P, Niu J, Clancy M, Kvien TK, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis 2011;70:1581–1586. doi: 10.1136/ard.2011.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marshall M, Peat G, Nicholls E, Myers HL, Mamas MA, van der Windt DA. Metabolic risk factors and the incidence and progression of radiographic hand osteoarthritis: a population-based cohort study. Scand J Rheumatol 2019;48:52–63. doi: 10.1080/03009742.2018.1459831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bijsterbosch J, Meulenbelt I, Watt I, Rosendaal FR, Huizinga TW, Kloppenburg M. Clustering of hand osteoarthritis progression and its relationship to progression of osteoarthritis at the knee. Ann Rheum Dis 2014;73:567–572. doi: 10.1136/annrheumdis-2012-202461. [DOI] [PubMed] [Google Scholar]
- 16.Paradowski PT, Lohmander LS, Englund M. Natural history of radiographic features of hand osteoarthritis over 10 years. Osteoarthritis Cartilage 2010;18:917–922. doi: 10.1016/j.joca.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Balblanc JC, Mathieu P, Mathieu L, Tron AM, Conrozier T, Piperno M, et al. Progression of digital osteoarthritis: a sequential scintigraphic and radiographic study. Osteoarthritis Cartilage 1995;3:181–186. doi: 10.1016/s1063-4584(05)80052-4. [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Hart DJ, Dacre JE, Huskisson EC, Spector TD. The progression of radiological hand osteoarthritis over ten years: a clinical follow-up study. Osteoarthritis Cartilage 1994;2:247–252. doi: 10.1016/s1063-4584(05)80076-7. [DOI] [PubMed] [Google Scholar]
- 19.Nelson AE, Golightly YM, Renner JB, Schwartz TA, Kraus VB, Helmick CG, et al. Brief report: differences in multijoint symptomatic osteoarthritis phenotypes by race and sex: the Johnston County Osteoarthritis Project. Arthritis Rheum 2013;65:373–377. doi: 10.1002/art.37775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson AE, Renner JB, Schwartz TA, Kraus VB, Helmick CG, Jordan JM. Differences in multijoint radiographic osteoarthritis phenotypes among African Americans and Caucasians: The Johnston County Osteoarthritis project. Arthritis Rheum 2011;63:3843–3852. doi: 10.1002/art.30610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sowers M, Lachance L, Hochberg M, Jamadar D. Radiographically defined osteoarthritis of the hand and knee in young and middle-aged African American and Caucasian women. Osteoarthritis Cartilage 2000;8:69–77. doi: 10.1053/joca.1999.0273. [DOI] [PubMed] [Google Scholar]