Abstract
Adenoviral vectors are being developed as vaccines against infectious agents and tumour-associated antigens, because of their ability to induce cellular immunity. However, the protection afforded in animal models has not easily translated into primates and clinical trials, underlying the need for improving adenoviral vaccines-induced immunogenicity. A Toll-like receptor signalling molecule, TRAM, was assessed for its ability to modify the immune responses induced by an adenovirus-based vaccine. Different adenovirus vectors either expressing TRAM alone or co-expressing TRAM along with a model antigen were constructed. The modification of T-cell and antibody responses induced by TRAM was assessed in vivo in mice and in primates. Co-expression of TRAM and an antigen from adenoviruses increased the transgene-specific CD8+ T cell responses in mice. Similar effects were seen when a TRAM expressing virus was co-administered with the antigen-expressing adenovirus. However, in primate studies, co-administration of a TRAM expressing adenovirus with a vaccine expressing the ME-TRAP malaria antigen had no significant effect on the immune responses. While these results support the idea that modification of innate immune signalling by genetic vectors modifies immunogenicity, they also emphasise the difficulty in generalising results from rodents into primates, where the regulatory pathway may be different to that in mice.
Subject terms: Lymphocyte activation, Malaria
Introduction
The developing world urgently needs new vaccines for diseases such as malaria, HIV-AIDS and tuberculosis, which together kill over 5 million people every year1. Non-replicating recombinant viral vectors have been developed as promising new vaccine candidates. Adenovirus based vaccine vectors induce both innate and adaptive immune responses in mammalian hosts2–4. They continue to be developed because of their well-recognised ability to induce potent cellular as well as humoral responses against transgenic antigens from target pathogens. However, the protection afforded by such vaccines in animal models has not translated readily into primates5. Therefore, attempts are being made to increase their immunogenicity and efficacy by combining them with other vaccine formulations and heterologous booster doses, or by engineering the inserted transgenes.
The understanding of antigen presenting cells (APCs) suggests that early interactions with T lymphocytes have profound effects on immune activation6. The activation state of the APCs is a key factor in the activation of T-cell responses and is influenced by environmental signals, which include the sensing of pathogens through pattern-recognition receptors (PRRs)7. The downstream patterns of signalling from PRRs are increasingly understood, with four key intracellular activating adapters identified which are transducers of Toll like receptor signalling. These adapters couple receptors to the induction of proinflammatory cytokine signalling, and in some cases interferon signalling7. One of these, the TRIF-related adaptor molecule (TRAM), activates both interferon and proinflammatory pathways linked to Toll-like receptor (TLRs) 4 and 2, in response to stimuli including bacterial lipoproteins, LPS, and large DNA viruses8,9.
We have shown in vitro in mammalian cells that expression of TRAM from plasmids in transient transfection assays activates the cxcl2, lcn and ifnb (interferon b) promoters, which are canonical early and late pro-inflammatory pathway and interferon signalling pathways target genes, respectively10. When co-expressed with the TAK1 (MAP3K7) serine/threonine kinase, TRAM expression increases T-cell responses induced by DNA vaccination in vivo in mouse11. We hypothesized that the expression of TRAM from an adenovirus vector could alter the virus-dependant signalling cascade in vivo, modifying viral immunogenicity. We investigated immune responses elicited by adenovirus vaccine immunization, with and without TRAM expression, in both murine and non-human primate models.
Materials and Methods
Plasmids, recombinant adenoviruses and recombinant MVA vaccines
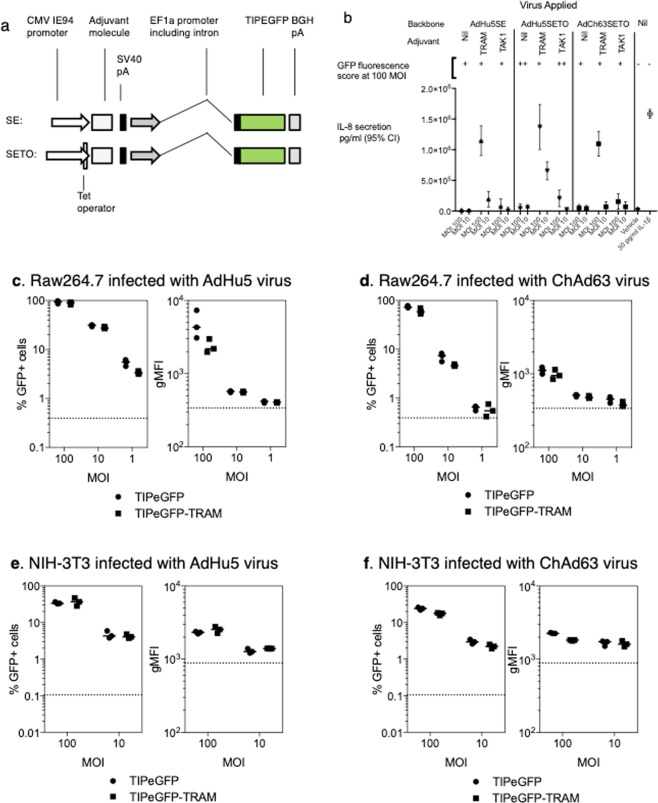
The synthetic multiepitope string (TIP, Tuberculosis-Immunodeficiency virus-Plasmodium epitope), containing CD8+ and CD4+ T cell epitopes from Plasmodium berghei, Mycobacterium tuberculosis and SIV, was described previously11. To generate recombinant adenoviruses expressing both the TIP antigen and an immune activator, a Gateway-compatible bicistronic entry vector was generated, derived from pENTR4 (Fisher) and the bicistronic expression vector previously described11 by a series of conventional cloning steps. To permit monitoring of antigen expression, the TIP antigen with a TIP antigen was fused in-frame to the N-terminus of GFP by PCR amplification and restriction cloning. One of the CMV IE94 promoters was replaced with the powerful human elongation factor 1α promoter (phEF1) from pEF-BOS12 to minimise repetitive sequences in the vector. phEF1 was used to drive antigen expression, while the CMV IE94 promoter was used to drive expression of mTRAM, and other inflammatory activator ORFs (Fig. 1a). In the experiments described here, two almost identical designs of this bicistronic expression cassette were used. One, designated the SE cassette, is described above. The SETO cassette differs from the SE cassette by addition of a Tetracycline-operator containing sequence flanking the CMV promoter TATA box (Fig. 1a) to limit CMV-driven expression in Tetracycline repressor containing cells13.
Figure 1.
TRAM-induced inflammatory signaling and adenovirus expression cassettes. (a) AdHu5 and ChAd63 adenoviruses were constructed by incorporating expression cassettes (illustrated) into the deleted E1 region. Two cassettes were studied, SE and SETO, the latter featuring repression of CMV promoter function during viral growth. All viruses expressed a model antigen (TIPEGFP) driven by the human EF1α promoter. (b) TRAM expression induces IL-8 response in vitro HeLa cells were either exposed to adenoviruses at an MOI of 10 or 100, or stimulated with IL1β, or exposed to vehicle (Optimem medium) for one hour. 36 hours after infection, antigen expression was assessed by microscopy and IL-8 secretion measured by EIA. (c–f) Co-expression of mouse TRAM does not increase the antigen transgene expression in mouse cell lines. Raw246.7 (c,d) or NIH-3t3 (e,f) cells were infected with the AdHu5 (a,e) or ChAd63 (d,f) at an MOI of 100, 10 or 1. Cells were harvested 24 hours later and the level of GFP expression measured by flow cytometry. Graphs represent the percentage of infected cells (GFP+) or the geometric mean fluorescence intensity (gMFI) of the GFP signal, each dot represents a replicate well with lines representing the median response.
SE and SETO expression cassettes were transferred from their plasmids of origin into the E1 locus of pAd/PL-DEST (Invitrogen), or the ChAd63 (chimpanzee adenovirus type 63) vector14 by in vitro recombination using LR clonase (Invitrogen). Control ChAd63 adenoviruses expressing blood-stage malaria antigens Pfm128 and PfAMA-1 or an irrelevant antigen (secreted alkaline phosphatase SEAP) were also used (hAd5-Pfm128, ChAd63-PfAMA-1 and ChAd63-SEAP). A monocistronic chimpanzee adenovirus serotypes serotype 63 (ChAd63) vector in which the complete human TRAM open reading frame was expressed by a CMV promoter was also created (ChAd63-TRAM), as previously described15. All adenoviruses were grown in human embryonic kidney 293 (HEK293) cells, purified by CsCl gradient ultracentrifugation, and dialyzed against 10 mM Tris (pH 7.4). Plasmid sequences were confirmed by Sanger sequencing, and are included in Supp. Data 1. In studies of both mouse and human TRAM, the entire unmodified open reading frame was expressed, including the myristoylation signal. The viruses were titered as described previously13 on HEK293 cells grown under standard conditions. Wells were scored positive or negative 10 days after infection using hexon immunostaining (Cell Biolabs Inc, San Diego, CA, USA), and infectious unit titers per milliliter were calculated with the Spearman-Karber method. A recombinant modified vaccinia virus Ankara (MVA) vector encoding ME-TRAP was also used, and was described previously16.
Viral bioactivity and antigen expression
To assess bioactivity of the viruses generated, HeLa cells were grown in DMEM containing 10% heat inactivated fetal bovine serum in 96 well plates to 80% confluency (~1 × 105 cells per well). Three treatments were compared: no stimulus, infection with various recombinant viruses, application of IL-1β. In all cases, media was aspirated and 100μl Optimem medium (Gibco) containing the stimulus was applied for one hour. For viral infection, medium contained virus at 10 and 100 MOI. For cytokine stimulation, media contained 30 pg/ml IL-1β (Calbiochem). GFP production was scored visually using an inverted fluorescence microscope 35 hours post infection. Thirty six hours post infection, supernatants were aspirated and IL-8 quantified in the supernatants (DY208, RnDSystem DuoSet).
To assess transgene expression quantitatively, Raw246.7 or NIH-3t3 cells, grown in DMEM containing 10% heat inactivated fetal bovine serum, were seeded (5 × 104 Raw246.7 and 2 × 104 NIH-3T3 cells per well) into 96-well flat bottom plates and left to adhere overnight. The following day, cells were infected with AdHu5-TIPEGFP (human adenovirus type 5, expressing fused to EGFP: enhanced green fluorescent protein) and ChAd63-TIPEGFP vectors, with and without TRAM, at increasing MOIs. 24 hours later, culture media was removed from each well and 30 µL of trypsin (TrypLE Express Enzyme, Life Technologies) added and incubated for 10–15 minutes, prior to resuspension of cells in 10% FCS in PBS and acquisition.
Immunizations
Mice were used in accordance with the UK Animals (Scientific Procedures) Act under project license number 30/2414 granted by the UK Home Office. The experimental protocols were approved by the Oxford University institutional Animal Welfare and Ethics Review Committee (AWERB), prior to getting licensing from the UK home Office. For induction of short-term anaesthesia, animals were either injected intraperitoneally (i.p.) with ketamine and Domitor® or anaesthetised using vaporised IsoFlo®. Female BALB/cOldHsd (BALB/c) or C57BL/6OldHsd (C57BL/6) mice (Harlan UK Limited) were immunised intradermally (i.d., into both ears) or intramuscularly (i.m., into each of the tibialis muscles of the hind limbs) with 50μl of vaccine in endotoxin-free phosphate-buffered saline (PBS). Groups of a minimum of four mice were used. The number was based around power calculations in which the variable under study (such as IFN-gamma secreting cell numbers) was log normally distributed with standard deviation of 10% of the mean, as based on previous data, and a 80% power to detect a 2.5 fold difference.
Male rhesus macaques (Macaca mulatta) aged between 4 ½ to 8 ½ years were housed at the National Primate Research Centre and cared for according to the regulations and guidelines of the University of Wisconsin Institutional Animal Care and Use Committee. The experimental protocol was reviewed and approved by the Wisconsin Institutional Animal Care and Use Committee (IACUC). Animals were anesthetized for all procedures and were returned after completion of the study into the colony for potential use in other studies or breeding programs. Male rhesus macaques were initially screened for neutralising antibodies against ChAd63 and background ELISpot responses to TRAP and ME peptides. Selection of 6 animals per group was based on ensuring an equal weight and age distribution as follows: negative control group 1 (ChAd63-ME TRAP) 8.8 kg (range 7.3–11.7 kg) and 5.9 years (range 5.3–7.3); group 2 (ChAd63-ME TRAP and 5x ChAd63-hTRAM) 8.5 kg (range 6.9–9.8) and 5.8 years (range 5.0–7.0); control group 3 (ChAd63-ME TRAP and 5x ChAd63-PfAMA-1) 8.2 kg (range 6.7–10.2) and 5.9 years (range 5.3–6.9). Animals received 1.5 × 108 iu of ChAd63-ME TRAP (8.9 × 109 vp) alone or mixed with 7.5 × 108 iu ChAd63-hTRAM (4.1 × 1010 vp) or 7.5 × 108 iu ChAd63-PfAMA-1 (7.2 × 1010 vp), in a total of 0.3 ml into the deltoid muscle at weeks 0 and 8. Blood samples were taken on the day of vaccination and at weeks 2, 4, 8, 10, 12, 16 after the first ChAd63 vaccination. All animals received 5 × 107 pfu MVA.ME TRAP at week 16 and blood samples were collected at weeks 17 (1 week post MVA), 19 and 23.
Ex vivo IFNγ ELISPOT
Mouse blood or mashed and filtered spleens were used for enumeration of antigen-specific IFNγ-producing T cells as described11. Nonhuman primate specific IFN-γ ELISPOT assays were performed as previously described17 using precoated ELISpotPLUS kits according to the manufacturer’s recommendation (Mabtech USA, Mariemont, OH, USA). All tests were performed in duplicate using pools of 20-mers at a final concentration of 5 μg/ml. Background values (mean of spots without peptide) were subtracted. A response was considered positive if the mean number of SFCs (spot forming cells) of duplicate sample wells exceeded background plus two standard deviations (STD) and was >50 SFC per 1 × 106 cells.
Ex vivo memory and intracellular cytokine staining
Frozen PBMC samples were thawed and rested for 6 hours at 37 °C in media containing 10U/ml of Benzonase (Novagen). Cells were then stimulated for a total of 16 hours with a single pool of TRAP peptides at 2 μg/ml final concentration, anti-CD28 APC (clone CD28.2, eBioscience), anti-CD49d (clone 9F10, eBioscience), anti-CD107a PECy5 (clone eBioH4.A3, eBioscience), Golgi-Stop and Golgi-Plug (BD Bioscience). Surface staining with CD95-bi (clone DX2, eBioscience) av-qDot565 (Invitrogen), CD4-APC H7 (clone L200, BD Bioscience), CD14 PE-Cy7 (clone M5E2, BioLegend), CD20 PE-Cy7 (clone 2H7, BioLegend) and live-dead Aqua was followed by fixation in 10% neutral buffered formalin (Sigma), prior to intracellular staining for CD3-PE (clone SP34–2, BD Bioscience), CD8 APC-H7 (clone RPA-T8, eBioscience) and IFN-γ FITC (clone 4 S.B3, BioLegend) in Perm-Wash Buffer (BD). All flow cytometry data were analysed using FlowJo (TreeStar) with cells gated based on size, doublet negative, CD3+ CD14/CD20−, and either CD4+CD8− or CD4−CD8+.
Evaluation of antibody responses
Antibodies to GFP were measured by ELISA. Briefly, 96 well Nunc-Immuno Maxisorp plates were coated for 1 hour at room temperature with recombinant GFP (Millipore) at a concentration of 2 μg/ml diluted in bi-carbonate buffer (Sigma Aldrich). After blocking with 1% BSA in 0.5% Tween-20 PBS, serum was incubated for 2 hours prior to detection of bound antibodies with alkaline phosphatase-conjugated goat anti-mouse IgG (whole molecule) (Sigma Aldrich) diluted 1:5000 and development with NPP substrate (Sigma Aldrich). Serum antibody endpoint titres were taken as the x-axis intercept of the dilution curve at an absorbance value 2x standard deviations greater than the OD405 for naïve mouse serum (typical cut-off OD405 for positive sera = 0.15). Serum from naïve mice were pooled and used as controls for all the ELISAs and were always below the level of detection.
Antibody responses to TRAP were measured using a luciferase immunoprecipitation system (LIPS) as previously described18. Briefly, serum samples were incubated for 1 hour with a cell lysate from 293 cells transfected with a TRAP-rLuc expression plasmid, prior to incubation with Protein A/G UltraLink Resin beads (ThermoScientific) in MultiScreen HTS membrane Barex plates (Millipore) for 1 hour. Unbound lysate and antibodies were removed by washing the plates prior to quantification of bound rLuc activity using Renilla luciferase assay system (Promega) and a Varioskan Flash luminometer (Thermo). Antibody levels are expressed as a fold increase from the pre-vaccination timepoint.
Statistical analysis
GraphPad Prism version 5.0 was used to perform two-way ANOVA testing when multiple doses or routes were tested.
Results
TRAM expression from a bi-cistronic adenovirus vector increases IL-8 production in vitro
Bi-cistronic AdHu5 vectors and ChAd63 vectors encoding a model transgene of interest (containing malaria and TB epitopes, fused to EGFP), driven by a human EF1α (hEF1α) promoter, were constructed including cassettes allowing inflammatory signalling components to be expressed under the control of a CMV promoter (Fig. 1a), while the antigen was driven by an hEF1α promoter, a strong mammalian promoter12.
Infection of HeLa cells by these vectors showed that TRAM-expressing vectors consistently caused the release of IL-8, a chemokine chosen for bioactivity monitoring (Fig. 1b). Significant increased in IL-8 concentrations were not observed with control viruses that did not express TRAM relative to mock infection (Fig. 1b). The increase with TRAM expressing viruses was much larger than that observed with vectors expressing another inflammatory activator, TAK111. That the pro-inflammatory response was not observed in cells infected with control viruses, in which the only difference is the absence of the TRAM gene, or with a vector containing a different transgene (TAK1), provides evidence of the transgene-specific modification of the signalling response in the cells. A GFP was used in this system to confirm that the insertion of the TRAM gene in the adenovirus vector did not modify the amount of antigen expressed, an important control to confirm that the pro-inflammatory effect was due to the transgene itself rather than to an indirect effect. Antigen expression, assessed using GFP fluorescence, was similar in three infected cell lines: HeLa (Fig. 1b), NIH-3T3 and RAW264.7 (Fig. 2) irrespective of the presence of TRAM in the virus. We have however not tagged the TRAM molecule in the transgene design out of concern that any epitope tag might alter the intra-cellular activity of TRAM, thus preventing the possibility to measure directly the increase of TRAM molecules within the cells with this method.
Figure 2.
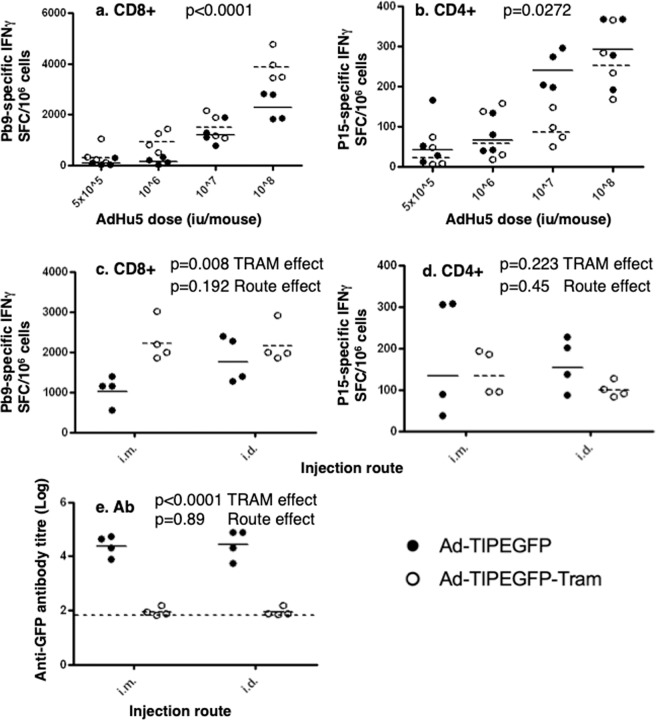
Co-expression of TRAM in AdHu5-TIPEGFP vector impacts on the transgene-specific immune responses. Groups of BALB/c mice were immunized i.m. at day 0 with AdHu5-TIPEGFP (SE) (black dots, black lines in all graphs) or with AdHu5-TIPEGFP-tram (SE) vectors (open circles, dotted lines in all graphs), at the doses indicated (a,b), or at 4 × 108 iu/mouse (c–e). Specific CD8+ T cell responses to Pb9 peptide (a,c) or CD4+ responses to P15 peptide (b,d) were measured by IFN-γ ELIspot at week 2. Antibody titres against GFP protein were measured at the same time point (e) and the long dotted lines represent the detection limit of the assay. Each dot represents one mouse and the short lines represent the geometric means per group. P values are indicated (2-way ANOVA).
Co-expression of TRAM with antigen in AdHu5 bicistronic vector increases CD8+ and decreases antibody responses to the transgene in mice
To assess whether the co-expression of TRAM was associated with a modification of AdHu5-TIP EGFP-induced immunogenicity in vivo, groups of BALB/c mice were immunized with the mTRAM encoding virus and compared the immune responses with the non-adjuvanted counterpart under different conditions. Insertion of the murine Tram gene increased the CD8+ T cell responses to the Pb9 epitope (Fig. 2a, two way ANOVA, p < 0.0001 for the TRAM effect), while it did only marginally increased CD4+ T cell responses (Fig. 2b, p = 0.0272 for the TRAM effect, observed at one dose only). This effect was not restricted to the intramuscular route: The increase of CD8+ T cell response was detected both i.m. and i.d. (Fig. 2c, two way ANOVA, p = 0.008 for the TRAM effect), and its magnitude was not route-dependant (p = 0.192 for the route effect). The CD4+ T cells responses did not differ significantly by TRAM or by the route of AdHu5 injection at that dose (Fig. 2d. p = 0.223 and p = 0.45 respectively). TRAM expression also markedly reduced the antibody response to the transgene, as measured by the reduction of GFP-specific antibody titres induced by the TRAM-expressing virus with both immunization routes (Fig. 2e, two-way ANOVA, p < 0.0001 for the TRAM effect, p = 0.89 for the route effect).
Co-expression of TRAM on the same virus as the transgene is not required to modify the transgene-specific immune responses
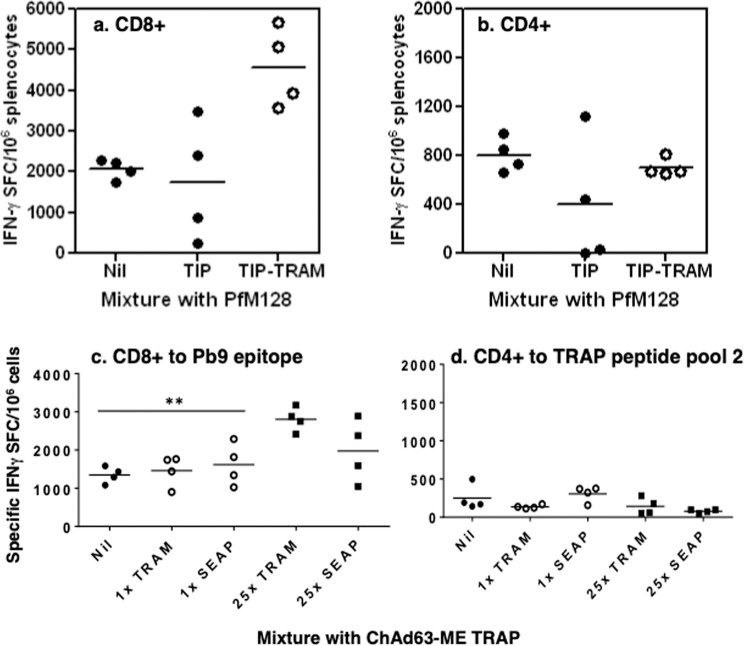
Expression of molecules from the TLR pathway in DNA vectors can adjuvant the CD8+ T cell immune response to a transgene delivered by another, co-administered plasmid11, the so-called ‘trans’ setting. To investigate whether this effect is observed with adenovirus-based vaccines, groups of C57BL/6 mice were immunized with AdHu5-Pfm128, which encodes a malaria blood stage antigen, mixed with either AdHu5-TIP-EGFP or AdHu5-TIP-EGFP-mTRAM. C57BL/6 mice were selected for this assessment because in this strain of mice CD4+ and CD8+ T cell epitopes are present in Pfm128 that are not contained in the TIP-EGFP antigen19, so Pfm128 immunogenicity could be monitored without immune competition with the TIP-EGFP antigen. Two weeks after immunization, an ELISPOT assay with peptides corresponding to known Pfm128 CD8+ and CD4+ T cell epitopes was performed. The mTRAM-encoding virus significantly increased the CD8+ (Fig. 3a, p = 0.0073), but not the CD4+, T cell response to Pfm128 (Fig. 3b), a pattern of responses seen in previous experiments (Fig. 2).
Figure 3.
Effect of murine and human TRAM in mice by co-injection. Expression of murine TRAM impacts on the CD8+ immune response elicited by a co-injected vector. (a,b) Groups of C57BL/6 mice were immunized i.m. at day 0 with 108vp AdHu5-Pfm128 alone (black dots, referred as Nil in the X axis) or mixed with AdHu5-TIPEGFP (black dots, referred as TIP in the X axis) or with AdHu5-TIPEGFP-tram vectors (open dots, referred as TIP-TRAM), at 107 iu/mouse. Specific CD8+ T cell responses (a) and CD4+ responses (b) were measured by IFN-γ ELIspot at week 2. Each dot represents one mouse and the short lines represent the geometric means per group. Effect of human TRAM-encoding ChAd63 in mouse by co-injection (c,d). Groups of mice were immunized i.m. at day 0 with ChAd63-ME TRAP alone or was mixed with ChAd63-hTRAM, expressing human TRAM, at a 1:1 or 1:25 ratio. (c,d) A control group included ChAd63-ME TRAP mixed with similar ratios of an adenovirus encoding an irrelevant antigen (secreted alkaline phosphatase, ChAd63-SEAP). Specific CD8+ T cell responses (c) and CD4+ responses (d) were measured by IFN-γ ELIspot at week 2. Each dot represents one mouse and the short lines represent the geometric means per group. Only the group that received 25x TRAM had a response significantly superior to the group that received ChAd63-ME TRAP with no adjuvant (nil).
Adjuvant effect of human TRAM-encoding adenovirus in ChAd63 vector in mouse
To confirm these findings, a monocistronic chimpanzee adenovirus serotypes serotype 63 vector (ChAd63) was generated, in which the complete human TRAM open reading frame was expressed by a CMV promoter (ChAd63-TRAM). No antigen was encoded in this ‘adjuvant’ virus. It was mixed with a ChAd63 vector encoding the liver-stage malaria antigen ME-TRAP (ChAd63-ME TRAP), and antigen chosen because, when delivered by ChAd63 as part of prime boost regimen, ME-TRAM induces modest protection against malaria in field trials20. It also includes the pb9 epitope included in the TIPEGFP constructs.
ChAd63-TRAM was mixed with ChAd63-METRAP at 1:1 (antigen:adjuvant) or 1:25 (antigen:adjuvant) ratio, and injected into groups of mice. A control group included ChAd63-ME-TRAP mixed with similar ratios of an adenovirus encoding an irrelevant molecule (secreted alkaline phosphatase, ChAd63-SEAP), instead of the TRAM adjuvant. IFN-γ responses to the murine epitope Pb9, contained in ME-TRAP, showed that at a 1:1 ratio, human TRAM-encoding adenovirus did not increase the Pb9-specific response in mouse, while an increase was observed when ChAd63-hTRAM was in excess (1:25, Fig. 3c, p < 0.01 as compared with the group receiving no adjuvant (nil)). Mixing with ChAd63-SEAP did not significantly alter the Pb9 response induced by co-administered ChAd63-ME TRAP at any of the ratios studied. As expected, this mixture did not increase the CD4+ T cell responses (Fig. 3d).
Adjuvant effect of human TRAM-encoding adenovirus in Rhesus macaques
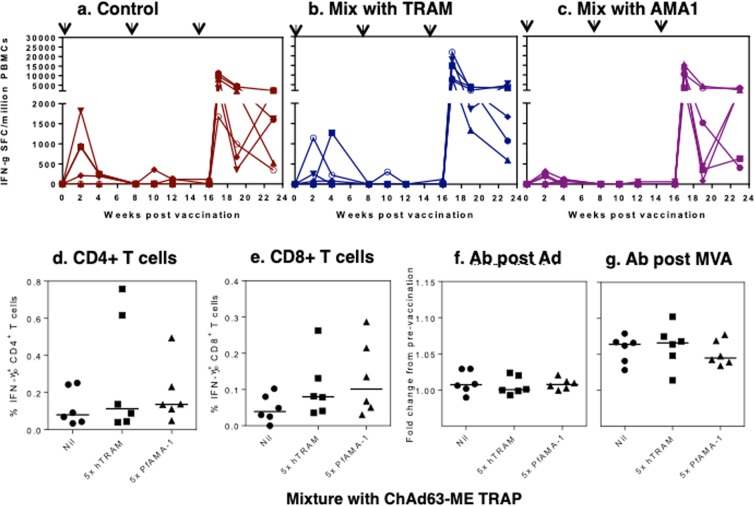
The adjuvant effect of human TRAM-expressing vector was investigated in a non-human primate using the mixture approach described above. To this end, three groups of six Rhesus macaques were immunized with ChAd63-ME TRAP alone, or mixed with 5x ChAd63-hTRAM, or with 5x ChAd63-PfAMA1, encoding a blood-stage malaria antigen used as a control.
After a first injection, the TRAP-specific IFNγ ELISPOT responses peaked at week 2 or 4 and ranged from 0 to 1825 SFC/million PBMCs, with 4/6 animals responding in the control and the hTRAM-adjuvanted groups, versus 5/6 in the PfAMA1 group (Fig. 4a–c). No significant difference of the TRAP-specific response was observed, and in all animals, responses had declined to below detection level at week 8 (Fig. 4a–c). A second ChAd63 injection failed to boost the primary responses, as the number of IFNγ-producing cells decreased to below 400 SFU/million PBMC in responding animals (2/6 in the control and hTRAM groups, 1/6 in the PfAMA1 group, Fig. 4a–c). All animals were boosted at week 16 with MVA-ME TRAP. Strong TRAP-specific IFNγ responses were elicited in all animals one week post MVA injection, ranging from 1675 to 21890 SFC/million PBMCs. No significant difference was observed between the groups (Fig. 4a–c).
Figure 4.
Effect of human TRAM-encoding adenovirus in Rhesus macaques. Three groups of six Rhesus macaques were immunized with ChAd63-ME TRAP alone (a), or mixed with 5x ChAd63-hTRAM (b), or with 5x ChAd63-PfAMA1 (c), at weeks 0 and 8. The individual TRAP-specific IFNγ responses were measured by ELISPOT at several time points as indicated. Each line represents one animal. TRAP specific IFN-γ production was measured after adenovirus vaccination (data not shown) and one week post MVA boost by intracellular cytokine staining. Graphs represent the frequency of IFN-γ+ CD4+ T cells (d) or IFN-γ+ CD8+ T cells (e) in each group with each animal displayed as a single point and lines representing the median group response. Antibodies to TRAP were measured by LIPs with the graphs representing the fold increase in TRAP responses between the pre-vaccination timepoint and 4 weeks post adenovirus prime (f) and 3 weeks post-MVA boost (g). Each animal is represented by a single point with lines representing the median response per group.
To determine the phenotype of the TRAP specific T cell response, PBMCs were restimulated overnight with TRAP peptides and IFN-γ production measured by intracellular cytokine staining. No significant difference between groups was observed for the low IFN-γ+ CD4+ or IFN-γ+ CD8+ T cells responses measured two weeks after adenovirus administration (data not shown). After the MVA boost, slightly higher frequencies of TRAP specific CD4+ T cells (Fig. 4d) were observed compared to CD8+ T cells (Fig. 4e), however there was again no significant difference in the frequency of IFN-γ+ CD4+ or CD8+ T cells between the groups. In addition, there was no significant difference in either the frequency or proportion of T effector, T effector memory or T central memory cells between the three groups (data not shown). TRAP antibodies were measured pre-vaccination, at week 4 post first adenovirus injection and 3 weeks post-MVA boost. While increases in TRAP specific responses were observed after vaccination, mainly after MVA boost (indicated by a greater than 1 fold increase Fig. 4f,g), no significant difference between the three groups of macaques at these two time points was observed. In conclusion, strong TRAP specific immune responses were observed in all vaccinated animals with the peak response observed one week post-MVA boost. Vaccination induced TRAP specific IFN-γ+ CD4+ and IFN-γ+ CD8+ T cells and TRAP specific antibodies, yet neither enhancement of the CD8+ response nor decrease of the antibody response by co-vaccination with ChAd63 expressing TRAM was observed.
Discussion
In this study, the adjuvant effect of a signalling pathway molecule on a co-administered antigen previously observed with DNA immunization was investigated in the context of viral vector immunization. A modest (1.5 to 2 fold) increase of CD8+ T cell responses was observed in mice immunized with TRAM expressing adenovirus vaccines, concomitant with a marked decrease of antibody responses. In mice, the effect was observed in experiments where the murine tram gene was inserted in the same vector as the antigen, or when the antigen and TRAM (murine or human) were encoded by different vectors mixed together prior to injection. The effect was observed with the human serotype 5 as well as with the chimpanzee serotype 63 adenoviruses described above. In rhesus macaques however, there was no evidence of any adjuvant effect induced by a vector encoding human TRAM on the immune response elicited by a co-administered adenovirus, under the conditions studied. Difficulties translating murine adjuvants into primates was observed previously with 4-1BBL21.
The adjuvant effect was restricted to increase of CD8+ responses, while a decrease of antibody responses was observed in mouse. Such effect was previously observed with a Venezuelan equine encephalitis virus adenovirus vaccine: when IFN-alpha was co-expressed with the antigen, a reduction of transgene-specific antibody responses was observed22. Thus, in vivo interferon induction induced by TRAM7–9 may explain some of the effects observed.
The immune modulation induced by TRAM seen in mice was not observed in primates. The regime tested in primates used an adjuvant virus administered in a molar excess relative to the antigen expressing virus. The ratio of adjuvant to antigen expressing virus was lower than that at which significantly enhanced immunogenicity was observed in mice, but was chosen because it was considered to be a more realistic candidate for manufacturing and human use, compared with regimes with higher ratios of adjuvant to antigen (such as that used in Fig. 3a). It is possible that the mixture used was not optimal in primates.
Induction of immune responses is dependent on complex pathways, and therefore immune modulation by modification of intracellular signalling pathway may differ between species. In particular, a splice variant of TRAM, TAG, acts as a negative regulator of the TLR4 signalling pathway in primates23. This molecule competes with TRAM for the recruitment of TRIF, and is not found in mice, and such regulation could explain the difference of TRAM-adjuvant effect between mice and non-human primates. Therefore, it is unlikely that any modification aiming at increasing the expression of TRAM from an adenovirus vector would result in a suitable adjuvant system in human, because of the negative regulation system. However, a combination with another stimulation may overcome the negative regulation: TRAM is a membrane-anchored molecule, containing a TIR-domain adaptor that induces the MyD88-dependent signaling pathway, and ultimately activates NF-kB. We hypothesized that over-expression of TRAM could mediate intracellular signal activation, that would result in enhanced immune responses. The intracellular signal activation may be enhanced in the presence of TLR stimulation. Therefore, combining a TRAM expressing vector with TLR stimulating small molecule may enhance the adjuvant properties and vaccination efficacy. This is an area for further research.
Altogether, these results support the concept that modification of viral vector immunogenicity by modifying virally induced innate immune signalling profiles, but emphasise the difficulty of doing so in a cross-species manner. Adjuvanting viral vector induced responses in primates can be achieved by altering antigenic structure: oligomerization of several antigens with molecules such as C4bp variants19,24. In addition, fusion of antigens to MHC class II invariant chain also induced increased T-cell responses in mice and in non-human primates25. Such structural modifications of antigens may have more consistent effects between species than modulation of signalling pathways.
Supplementary information
Acknowledgements
This work was funded by a grant from the Foundation for the National Institutes of Health through the Grand Challenges in Global Health Initiative of the Gates Foundation, with additional support from the Wellcome Trust. Non-human primate studies were supported by National Center for Research Resources (NCRR) grant # P51 RR000167, and were conducted at a facility constructed with support from grants RR15459 and RR020141. The authors wish to acknowledge the expert contribution of Dr Matthew G. Cottingham, and the expert help provided by the Animal Services Unit, and the Immunology Services Unit of the Wisconsin National Primate Research Center, in particular D. Watkins and E. Rakasz. CR is supported by the NIHR Biomedical Research Centre, Oxford. CR, SGC and AVSH are Jenner Institute Investigators and AVSH is a Wellcome Trust and NIHR Senior Investigator. The funding sources had no involvement in study design; collection, analysis and interpretation of data, in the writing of the report and in the decision to submit the article for publication.
Author contributions
C.R., A.S., K.C.S., S.G., A.V.S.H. and D.W. contributed to the conception and design of the study, analysis and interpretation of data. C.R., A.S., K.C.S., J.H., J.F. and D.W. performed the experiments and acquisition of data. C.R., A.S., M.B., A.V.S.H. and D.W. contributed to analysis and interpretation of data, and drafting the article or revising it critically for important intellectual content. All authors have approved the final article.
Competing interests
A.V.S.H. and S.G.C. are names as co-inventors on patents related to recombinant viral vectors for malaria and other indications.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Christine S. Rollier and Alexandra J. Spencer.
Supplementary information
is available for this paper at 10.1038/s41598-020-61730-8.
References
- 1.Hotez PJ, Bottazzi ME, Strych U. New Vaccines for the World’s Poorest People. Annu. Rev. Med. 2016;67:405–417. doi: 10.1146/annurev-med-051214-024241. [DOI] [PubMed] [Google Scholar]
- 2.Tatsis N, Ertl HC. Adenoviruses as vaccine vectors. Mol. therapy: J. Am. Soc. Gene Ther. 2004;10:616–629. doi: 10.1016/j.ymthe.2004.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ewer KJ, et al. Viral vectors as vaccine platforms: from immunogenicity to impact. Curr. Opin. immunology. 2016;41:47–54. doi: 10.1016/j.coi.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Lopez-Camacho C, et al. Rational Zika vaccine design via the modulation of antigen membrane anchors in chimpanzee adenoviral vectors. Nat. Commun. 2018;9:2441. doi: 10.1038/s41467-018-04859-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rollier CS, Reyes-Sandoval A, Cottingham MG, Ewer K, Hill AV. Viral vectors as vaccine platforms: deployment in sight. Curr. Opin. immunology. 2011;23:377–382. doi: 10.1016/j.coi.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Alpan O, Bachelder E, Isil E, Arnheiter H, Matzinger P. ‘Educated’ dendritic cells act as messengers from memory to naive T helper cells. Nat. Immunol. 2004;5:615–622. doi: 10.1038/ni1077. [DOI] [PubMed] [Google Scholar]
- 7.Newton, K. & Dixit, V. M. Signaling in innate immunity and inflammation. Cold Spring Harbor perspectives in biology4, 10.1101/cshperspect.a006049 (2012). [DOI] [PMC free article] [PubMed]
- 8.Stack J, et al. TRAM is required for TLR2 endosomal signaling to type I IFN induction. J. immunology. 2014;193:6090–6102. doi: 10.4049/jimmunol.1401605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nilsen NJ, et al. A role for the adaptor proteins TRAM and TRIF in toll-like receptor 2 signaling. J. Biol. Chem. 2015;290:3209–3222. doi: 10.1074/jbc.M114.593426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wyllie DH, et al. Identification of 34 novel proinflammatory proteins in a genome-wide macrophage functional screen. PLoS one. 2012;7:e42388. doi: 10.1371/journal.pone.0042388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larsen KC, et al. Expression of tak1 and tram induces synergistic pro-inflammatory signalling and adjuvants DNA vaccines. Vaccine. 2009;27:5589–5598. doi: 10.1016/j.vaccine.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 12.Mizushima S, Nagata S. pEF-BOS, a powerful mammalian expression vector. Nucleic acids Res. 1990;18:5322. doi: 10.1093/nar/18.17.5322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cottingham MG, et al. Preventing spontaneous genetic rearrangements in the transgene cassettes of adenovirus vectors. Biotechnol. Bioeng. 2012;109:719–728. doi: 10.1002/bit.24342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodgson SH, et al. Evaluation of the efficacy of ChAd63-MVA vectored vaccines expressing circumsporozoite protein and ME-TRAP against controlled human malaria infection in malaria-naive individuals. J. Infect. Dis. 2015;211:1076–1086. doi: 10.1093/infdis/jiu579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chartier C, et al. Efficient generation of recombinant adenovirus vectors by homologous recombination in Escherichia coli. J. virology. 1996;70:4805–4810. doi: 10.1128/JVI.70.7.4805-4810.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McConkey SJ, et al. Enhanced T-cell immunogenicity of plasmid DNA vaccines boosted by recombinant modified vaccinia virus Ankara in humans. Nat. Med. 2003;9:729–735. doi: 10.1038/nm881. [DOI] [PubMed] [Google Scholar]
- 17.Wilson NA, et al. Vaccine-induced cellular immune responses reduce plasma viral concentrations after repeated low-dose challenge with pathogenic simian immunodeficiency virus SIVmac239. J. virology. 2006;80:5875–5885. doi: 10.1128/jvi.00171-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burbelo PD, Lebovitz EE, Notkins AL. Luciferase immunoprecipitation systems for measuring antibodies in autoimmune and infectious diseases. Transl. research: J. laboratory Clin. Med. 2015;165:325–335. doi: 10.1016/j.trsl.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forbes EK, et al. T cell responses induced by adenoviral vectored vaccines can be adjuvanted by fusion of antigen to the oligomerization domain of C4b-binding protein. PLoS one. 2012;7:e44943. doi: 10.1371/journal.pone.0044943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogwang C, et al. Prime-boost vaccination with chimpanzee adenovirus and modified vaccinia Ankara encoding TRAP provides partial protection against Plasmodium falciparum infection in Kenyan adults. Sci. Transl. Med. 2015;7:286re285. doi: 10.1126/scitranslmed.aaa2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spencer AJ, et al. 4-1BBL enhances CD8+ T cell responses induced by vectored vaccines in mice but fails to improve immunogenicity in rhesus macaques. PLoS one. 2014;9:e105520. doi: 10.1371/journal.pone.0105520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Brien L, et al. Alpha interferon as an adenovirus-vectored vaccine adjuvant and antiviral in Venezuelan equine encephalitis virus infection. J. Gen. Virol. 2009;90:874–882. doi: 10.1099/vir.0.006833-0. [DOI] [PubMed] [Google Scholar]
- 23.Palsson-McDermott EM, et al. TAG, a splice variant of the adaptor TRAM, negatively regulates the adaptor MyD88-independent TLR4 pathway. Nat. Immunol. 2009;10:579–586. doi: 10.1038/ni.1727. [DOI] [PubMed] [Google Scholar]
- 24.Spencer AJ, et al. Fusion of the Mycobacterium tuberculosis antigen 85A to an oligomerization domain enhances its immunogenicity in both mice and non-human primates. PLoS one. 2012;7:e33555. doi: 10.1371/journal.pone.0033555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer AJ, et al. Enhanced vaccine-induced CD8+ T cell responses to malaria antigen ME-TRAP by fusion to MHC class ii invariant chain. PLoS one. 2014;9:e100538. doi: 10.1371/journal.pone.0100538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.