Abstract
Background
This study was performed to compare the clinical and radiographic outcomes of total knee arthroplasty (TKA) following high tibial osteotomy (HTO) versus primary TKA.
Methods
Relevant trials were identified via a search of Ovid, PubMed and the Cochrane Central Register of Controlled Trials from inception to 10 January 2019. A meta-analysis was performed to compare postoperative outcomes between revising HTO to TKA (RHTO) and primary TKA (PTKA) with respect to Knee Society Score (KSS), 10-year survival rate, operative time, flexion and extension angle, infection rate and radiographic results.
Results
Sixteen of 340 studies involving 103,552 adult patients (RHTO group, n = 3955; PTKA group, n = 99,597) were eligible for inclusion in the meta-analysis. Compared with primary TKA, revising HTO to TKA required longer operative time and had a higher infection rate (P < 0.05). The PTKA group had better flexion angle than the RHTO group (P < 0.05). There were no significant differences between the two groups in the KSS, extension angle, radiographic results and 10-year survival rate (P > 0.05).
Conclusion
Patients who undergo conversion of HTO to TKA have similar 10-year survival rate, KSS, extension angle and radiographic results as patients who undergo primary TKA. However, conversion of HTO to TKA required longer operative time and had a higher infection rate than performing primary TKA. Moreover, conversion of HTO to TKA is associated with poorer flexion angle than primary TKA.
Keywords: Knee osteoarthritis, High tibial osteotomy, Total knee arthroplasty, Meta-analysis
Background
Total knee arthroplasty (TKA) and high tibial osteotomy (HTO) are both used to treat osteoarthritis of the knee. High tibial osteotomy is a well-established technique for the treatment of medial osteoarthritis of the knee with varus malalignment, especially in young and active patients [1, 2]. Some knees may need a conversion to TKA because of failure such as the progression of osteoarthritis. However, the outcome of TKA after HTO remains uncertain. Some authors [3, 4] reported that the results of TKA following HTO were similar to those of primary TKA, whereas others [5–7] described worse results and a higher number of complications in cases previously treated by tibial osteotomy. Therefore, we performed a meta-analysis of clinical studies to answer the following question: Does a previous HTO influence the function or survival of a TKA?
Methods
Search strategy
The Cochrane Central Register of Controlled Trials, Ovid and PubMed databases were searched to identify relevant studies published in English from inception to 10 January 2019. The following search strategy was used to maximize search specificity and sensitivity: [(revision hto) OR (revised hto) OR (revised high tibial osteotomy) OR (revision high tibial osteotomy)] AND [(total knee) OR tka OR tkr], where “tkr” stands for total knee replacement.
Selection of studies
Three independent authors (X.D.S, J.W, and Z.S.) initially selected studies based on their titles and abstracts. Full papers were retrieved if a decision regarding study inclusion could not be made based on the titles and abstracts. The same three authors independently assessed each full paper to determine whether it met the inclusion criteria. Any disagreement was resolved by consensus; when a consensus could not be reached, the study was excluded.
Inclusion criteria
Cohort studies, case control studies, and randomized controlled trials were eligible for inclusion if they met the following criteria:
Comparison of the clinical outcomes of revised HTO versus primary TKA.
Mean follow-up duration of at least 2 years.
Evaluation of at least one of the following outcomes: Knee Society Score (KSS), 10-year survival rate, operative time, flexion and extension angles, infection rate, and radiographic results.
Sufficient data for extraction and pooling (i.e., reporting of the mean, standard deviation, and number of subjects for continuous outcomes, and reporting of the number of subjects for dichotomous outcomes).
Data extraction
Three reviewers (X.D.S. and J.W. and Z.S) independently performed data extraction using standardized data extraction forms. The general characteristics of each study were extracted [i.e., age, sex, body mass index (BMI), weight, follow-up, Knee Society Score (KSS), 10-year survival rate, operative time, flexion and extension angle, infection rate and radiographic results]. Any disagreement were resolved by consensus.
Statistical analysis
Dichotomous outcomes are expressed as the risk ratio (RR) with 95% confidence interval (CI), while continuous outcomes are expressed as the mean difference (MD) or Standard mean difference (SMD) with 95% CI. Heterogeneity is expressed as P and I2. This value of I2 ranges from 0% (complete consistency) to 100% (complete inconsistency). If the P value of the heterogeneity test was < 0.1 or I2 > 50%, a random-effects model was used in place of the fixed modality. Publication bias was tested using funnel plots. Forest plots were used to graphically present the results of individual studies and the respective pooled estimate of effect size. All statistical analyses were performed with Review Manager (version 5.3.0 for Windows; Cochrane Collaboration, Nordic Cochrane Centre, Copenhagen, Denmark).
Results
Search results
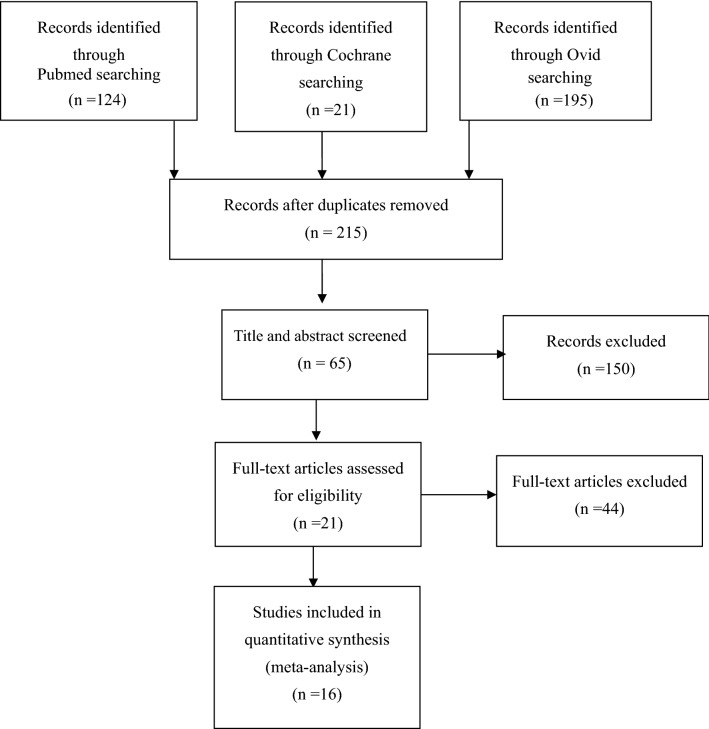
A flowchart of the studies considered for inclusion in our review is shown in Fig. 1. We identified 340 potential citations (124 from PubMed, 195 from Ovid, 21 from the Cochrane Library) comparing the clinical and radiographic outcomes of RHTO and PTKA. After reading the articles, Sixteen of the 340 citations were selected for the meta-analysis. The characteristics and data of these 16 studies [8–23] are shown in Tables 1 and 2.
Fig. 1.
Flow of study selection
Table 1.
Characteristics of included studies
| References | Technique of HTO | No. of patients | No. of knees | Age (years) | Female/male | BMI (kg/m2) | Mean time interval between HTO and TKA (months) | Follow-up (years) | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Amendola (2010) [8] | RHTO-C(19), RHTO-O(5) | 24 | 29 | 68.5 | 19/5 | NA | 100.7 | 8.1 | KSS, flexion angle, femorotibial angle |
| PTKA | 28 | 29 | 71 | NA | NA | – | 8.1 | ||
| Badawy (2015) [9] | RHTO | NA | 1399 | 69 | NA | NA | NA | > 10 | Infections, 10-year survival rate |
| PTKA | NA | 31077 | 71 | NA | NA | – | > 10 | ||
| Bae (2017) [10] | RHTO-C | 29 | 32 | 68.3 | 29/0 | 26.6 | 150 | 6.2 | KSS, flexion and extension angle, femorotibial angle, IS ratio |
| PTKA | 29 | 32 | 68.8 | 29/0 | 26.3 | – | 7.1 | ||
| Bergenudd (1997) [11] | RHTO | 14 | 14 | 70 | NA | NA | 96 | 4–9 | Flexion angle, infections, femorotibial angle, operative time |
| PTKA | 99 | 99 | 73 | NA | NA | – | 4–9 | ||
| Cross (2014) [12] | RHTO | 43 | 43 | 54.2 | 12/32 | 33.36 | 106.2 | 8.47 | KSS, infections, operative time |
| PTKA | 97 | 97 | 58.9 | 50/47 | 32.76 | – | 3.59 | ||
| Efe (2010) [13] | RHTO-C | 41 | 41 | 69 | 20/21 | NA | 86 | 6.8 | KSS, Infections, flexion and extension angle, IS ratio, operative time |
| PTKA | 41 | 41 | 73 | 24/17 | NA | – | 7.1 | ||
| El-Galaly (2018) [14] | RHTO | 1044 | 1044 | 62 | 448/596 | NA | NA | > 10 | Infections, 10-year survival rate |
| PTKA | 63762 | 63762 | 70 | 41142/22621 | NA | – | > 10 | ||
| Haddad (2000) [15] | RHTO-C(42), RHTO-D(8) | 42 | 50 | 65 | 26/16 | NA | 87.6 | 6.2 | KSS, femorotibial angle, infections |
| PTKA | 42 | 50 | 66 | 24/18 | NA | – | 6.2 | ||
| Haslam (2007) [16] | RHTO-C | 40 | 51 | 78 | 20/19 | NA | 58 | 12.6 | Infections |
| PTKA | 44 | 51 | 78 | 22/21 | NA | – | 12.6 | ||
| Karabatsos (2002) [17] | RHTO-C | 20 | 17 | 64 | 10/10 | NA | 100.8 | 5.2 | Infections, operative time |
| PTKA | 20 | 17 | 65 | 10/10 | NA | – | 4.7 | ||
| Kazakos (2008) [18] | RHTO-C | 32 | 38 | 67.2 | 24/8 | NA | 87.6 | 4.5 | KSS, flexion and extension angle, femorotibial angle, IS ratio, operative time |
| PTKA | 32 | 38 | 68.4 | 25/7 | NA | – | 4.5 | ||
| Meding (2011) [19] | RHTO-C | 39 | 19 | 66.9 | 12/27 | NA | 104.4 | 16.7 | KSS, flexion and extension angle, femorotibial angle |
| PTKA | 39 | 19 | 66.9 | 12/27 | NA | – | 16.6 | ||
| Niinimäki (2014) [20] | RHTO | NA | 1036 | 64.3 | NA | NA | NA | > 10 | Infections, 10-year survival rate |
| PTKA | NA | 4143 | 64.7 | NA | NA | – | > 10 | ||
| Nizard (1998) [21] | RHTO | 55 | 57 | 71.8 | NA | NA | 116.4 | 4.5 | KSS, IS ratio, infections |
| PTKA | NA | 57 | 70.5 | NA | NA | – | 4 | ||
| Saragaglia (2015) [22] | RHTO-O | 40 | 45 | 69 | 10/30 | 29.7 | NA | 3.9 | KSS, flexion angle, operative time |
| PTKA | 40 | 45 | 69 | 10/30 | 29 | – | 4.8 | ||
| Toksvig-Larsen (1998) [23] | RHTO | 40 | 40 | 69 | 26/14 | NA | 120 | 10 | Operative time |
| PTKA | 40 | 40 | 70 | 27/13 | NA | – | 10 |
No number, C closing, O opening, D dome, RHTO revising high tibial osteotomy to total knee arthroplasty, PTKA primary total knee arthroplasty, BMI body mass index, KSS Knee Society Score, IS ratio Insall–Salvat ratio, NA not available
Table 2.
The data of included studies
| References | KKS | KFS | 10-Survival rate | IS ratio | Femorotibial angle | Extension angle | Flexion angle | Operative time (min) | No of infections | |
|---|---|---|---|---|---|---|---|---|---|---|
| Amendola (2010) [8] | RHTO | 92.7 | 89.8 | – | – | 5.0° | – | 103° | – | – |
| PTKA | 91 | 84 | – | – | 4.0° | – | 100° | – | – | |
| Badawy (2015) [9] | RHTO | – | – | 92.6% | – | – | – | – | – | 10/1399 |
| PTKA | – | – | 93.8% | – | – | – | – | – | 289/31077 | |
| Bae (2017) [10] | RHTO | 90.6 | 88.8 | – | 1.13 | 6.0° | 0.2° | 129.2° | – | – |
| PTKA | 89.4 | 88.8 | – | 1.14 | 5.4° | 0.2° | 130.6° | – | – | |
| Bergenudd (1997) [11] | RHTO | – | – | – | – | 3° | – | 95° | 110 | 2/14 |
| PTKA | – | – | – | – | 3° | – | 95° | 113 | 5/99 | |
| Cross (2014) [12] | RHTO | 90 | 85 | – | – | – | – | – | – | 2/43 |
| PTKA | 86 | 85 | – | – | – | – | – | – | 2/97 | |
| Efe (2010) [13] | RHTO | 78.8 | 91 | – | 0.94 | – | 1.7° | 106° | 95 | 1/41 |
| PTKA | 78.2 | 87.8 | – | 0.90 | – | 0.2° | 115° | 90 | 2/41 | |
| El-Galaly (2018) [14] | RHTO | – | – | 91% | – | – | – | – | – | 21/1044 |
| PTKA | – | – | 94% | – | – | – | – | – | 707/63762 | |
| Haddad (2000) [15] | RHTO | 91 | 70 | – | – | – | 2° | 95° | – | 1/50 |
| PTKA | 89 | 66 | – | – | – | 0° | 103° | – | 2/50 | |
| Haslam (2007) [16] | RHTO | – | – | – | – | – | – | – | – | 3/51 |
| PTKA | – | – | – | – | – | – | – | – | 0/51 | |
| Karabatsos (2002) [17] | RHTO | – | – | – | – | – | – | – | 170 | 1/17 |
| PTKA | – | – | – | – | – | – | – | 118 | 0/17 | |
| Kazakos (2008) [18] | RHTO | 91.6 | 83 | – | 1.12 | 6.5° | 0.56° | 115.0° | 75 | – |
| PTKA | 92.0 | 84.4 | – | 1.24 | 5.4° | 0.64° | 119.1° | 50 | – | |
| Meding (2011) [19] | RHTO | 87.2 | 70.1 | – | – | 4.6° | − 0.1° | 110.6° | – | – |
| PTKA | 90.3 | 72.6 | – | – | 4.6° | − 0.3° | 112.6° | – | – | |
| Niinimäki (2014) [20] | RHTO | – | – | 91.8% | – | – | – | – | – | 14/1036 |
| PTKA | – | – | 94.5% | – | – | – | – | – | 31/4143 | |
| Nizard (1998) [21] | RHTO | 74.4 | 67.2 | – | 1.08 | – | – | – | – | 2/63 |
| PTKA | 80.9 | 64.1 | – | 1.1 | – | – | – | – | 0/63 | |
| Saragaglia (2015) [22] | RHTO | 87.5 | 96.5 | – | – | – | – | 117.5° | 73.5 | – |
| PTKA | 87.5 | 97 | – | – | – | – | 120.5° | 68.5 | – | |
| Toksvig-Larsen (1998) [23] | RHTO | – | – | – | – | – | – | – | 147 | – |
| PTKA | – | – | – | – | – | – | – | 134 | – |
No number, RHTO revising high tibial osteotomy to total knee arthroplasty, PTKA primary total knee arthroplasty, KKS Knee Society Knee Score, KFS Knee Society Function Score, IS ratio Insall–Salvat ratio
Meta-analysis results
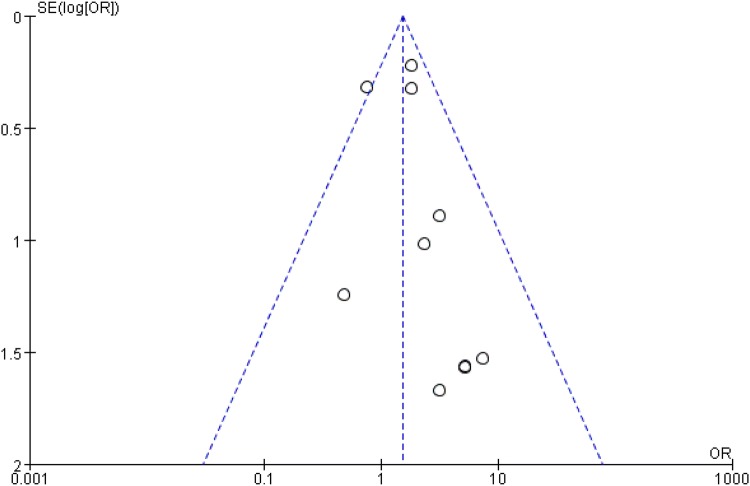
The meta-analysis included 16 studies [8–23], involving a total of 103,552 patients. The RHTO group included 3955 patients, while the PTKA group included 99,597 patients. A funnel plot based on the most frequently cited outcome was broadly symmetrical, indicating minimal publication bias (Fig. 2).
Fig. 2.
Funnel plot for infection rate
KSS
The KSS consists of the Knee Society Knee Score (KKS; 0–100) and the Knee Society Function Score (KFS; 0–100). There were no significant differences between these variables in the RHTO group versus the PTKA group (P > 0.05).
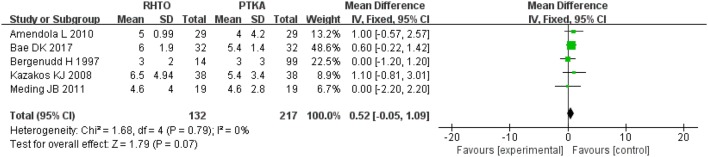
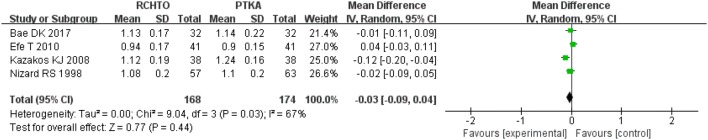
Radiographic results
The radiographic results consist of femorotibial angle and IS ratio, and are summarized in Table 2. No significant differences were observed between the RHTO group and the PTKA group in terms of femorotibial angle and IS ratio (P > 0.05) (Figs. 3, 4).
Fig. 3.
Forest plot for femorotibial angle
Fig. 4.
Forest plot for IS ratio
Flexion and extension angle
The MD of the flexion and extension angle for TKA with HTO were − 2.92 (P = 0.006; 95% CI − 4.98 to − 0.86) and 0.66 (P = 0.11; 95% CI − 0.15 to 1.46), respectively. These results imply that flexion angle was better in the PTKA group than RHTO group, but the extension angle between the two groups was no significant differences.
Operative time and infection rate
Six studies involving 475 patients provided data on operative time. The operative time used for the RHTO group was significantly longer than that used for the PKA group (SMD = 1.10; 95% CI 0.20–2.00; P = 0.02).
Ten studies involving 103,158 patients provided data on infections. There was a significantly higher infection rate in the RHTO group than in the PTKA group (RR = 1.51; P = 0.005; 95% CI 1.14–2.02).
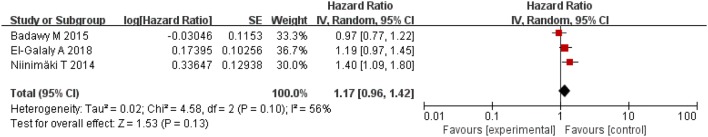
Survival rate
Three studies involving 102,461 patients provided data on 10-year survival rate. No significant differences were found between the two groups (P > 0.05) (Fig. 5).
Fig. 5.
Forest plot for survival rate
Discussion
The most important finding of the present meta-analysis was that there were no significant differences between the RHTO group and the PTKA group regarding the KSS, extension angle, radiographic results, and 10-year survival rate. However, the PTKA group showed better outcomes than the RHTO group in terms of the flexion angle, operative time, and infection rate.
The KSS is often used to evaluate the ability to perform walking and stair-climbing activities.. Bae et al. [10] and Meding et al. [19] reported that the mean KSS did not significantly differ between the RHTO group and the PTKA group, whereas Efe et al. [13] found that the KSS was significantly better in the PTKA group than the RHTO group. The present meta-analysis revealed that the KSS was similar in the RHTO and the PTKA groups. The function of the knee is also assessed based on the range of motion (ROM) of the joint. In the present meta-analysis, the RHTO group had a smaller flexion angle than the PTKA group, which is in accordance with the findings of other studies [12, 13, 15]. Furthermore, extension angle did not significantly differ between the two groups. However, Miner et al. [24] revealed that ROM is much less important than the overall results, and Ripanti et al. [25] reported that previous HTO has no adverse effect on the outcome and functional results of the subsequent TKA.
HTO can result in a coronal deformity of the tibial plateau [26]. Lee et al. [27] found loss of correction in the operated limb occurred in open-wedge osteotomy, especially in the bilateral open-wedge osteotomy. Some studies [8, 11, 19] reported that the femorotibial angle after TKA following HTO did not significantly differ from that after primary TKA. Furthermore, some studies found that the patellar height was altered after HTO [6, 28]. Bae et al. [10] and Efe et al. [13] reported that the IS ratio did not significantly differ between the RHTO and PTKA groups; however, Kazakos et al. [18] reported the opposite. The present meta-analysis revealed that the mean femorotibial angle and IS ratio did not differ significantly between the two groups. The patellar height and femorotibial angle should be considered in preoperative planning. As the deformity can be corrected intra-articularly at the time of the TKA, it is essential to assess the postoperative alignment on radiography.
Previous studies have revealed that HTO results in satisfactory clinical outcomes. Furthermore, the HTO located at the metaphyseal areas had a significantly higher percentage of bone healing regardless of open- and closed-wedge osteotomies [29]. However, osteoarthritis progression may occur with a long term follow-up, and requiring conversion to TKA [30–32]. In addition, a systematic review and meta-analysis [33] found the HTO with concurrent cartilage procedures such as marrow stimulation procedure, mesenchymal stem cell transplantation, and injection were performed, but the concurrent procedures would produce little beneficial effect regarding clinical and radiological outcomes compared with HTO alone. In the included studies, the mean time interval between HTO and TKA ranged from 58 to 150 months (Table 1), which suggests that HTO is still a successful and reliable treatment method for unicompartmental knee osteoarthritis. However, previous studies have shown conflicting results regarding the survival rate after TKA following HTO versus that after primary TKA [34–36]. Several related studies with adequate sample sizes have been recently published, but the conclusions were still inconsistent. These studies estimated the survival rate using the Kaplan–Meier analysis and performed Cox regression analysis adjusted for age and sex. The present meta-analysis of the pooled 10-year survival rate data from the 102,461 patients evaluated in these included studies suggests that previous HTO should not be considered a factor related to a worse survival rate.
Conversion TKA after HTO may be more technically demanding than primary TKA due to the difficulty of the surgical approach, the ligamentous imbalance, and the anatomical distortion of the proximal tibial metaphysis [17, 37]. Bastos et al. [28] reported that incidence of additional procedures were required for the surgical approach because of the difficult patellar eversion in conversion TKA after HTO. Nagamine et al. [38] reported that a tibial offset stem may be required to solve the problem of translational and meta-diaphyseal mismatch of the tibia. Therefore, the longer operative time required for TKA following HTO is probably due to the increased surgical difficulty compared with primary TKA. Moreover, some studies [39, 40] reported that prolonged operative times were associated with an increased risk of surgical site infection, and related studies have also shown an increased risk of infection in patients undergoing TKA after prior knee surgery [41, 42]. The present meta-analysis revealed a higher infection rate in the RHTO group than in the PTKA group, which is in accordance with previous studies. This increased infection rate may be caused by the longer operative time and previous history of internal fixation.
The limitations of the present meta-analysis are the lack of adjustments for BMI or weight, the variation in the types of prostheses used, and the retrospective study design.
Conclusion
Patients who undergo conversion of HTO to TKA have similar 10-year survival rate, KSS, extension angle and radiographic results as patients who undergo primary TKA. However, conversion of HTO to TKA required longer operative time and had a higher infection rate than performing primary TKA. Moreover, conversion of HTO to TKA is associated with poorer flexion angle than primary TKA.
Funding
This work was supported by Health Commission of Weifang City (wfwsjk-2019-159).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xuedong Sun, Email: hisxd1118@sina.com.
Jun Wang, Email: hisxd@sina.com.
Zheng Su, Email: asue1006@sina.com.
References
- 1.Habata T, Uematsu K, Hattori K, et al. High tibial osteotomy that does not cause recurrence of varus deformity for medial gonarthrosis. Knee Surg Sports Traumatol Arthrosc. 2006;14:962–967. doi: 10.1007/s00167-006-0077-y. [DOI] [PubMed] [Google Scholar]
- 2.Lobenhoffer P. Importance of osteotomy around to the knee for medial gonarthritis: indications, technique and results. Orthopade. 2014;43:425–431. doi: 10.1007/s00132-013-2189-7. [DOI] [PubMed] [Google Scholar]
- 3.Amendola A, Rorabeck CH, Bourne RB, et al. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty. 1989;4(Suppl):S11–S17. doi: 10.1016/s0883-5403(89)80002-6. [DOI] [PubMed] [Google Scholar]
- 4.Staeheli JW, Cass JR, Morrey B. Condylar total knee arthroplasty after failed proximal tibial osteotomy. J Bone Joint Surg Am. 1987;69(1):28–31. [PubMed] [Google Scholar]
- 5.Katz MM, Hungerford DS, Krackow KA, et al. Results of knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1987;69(2):225–233. [PubMed] [Google Scholar]
- 6.Windsor RE, Insall JN, Vince KG. Technical Considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am. 1988;70(4):547–555. [PubMed] [Google Scholar]
- 7.Tungall JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34(2):255–261. doi: 10.1007/s00264-009-0819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amendola L, Fosco M, Cenni E, Tigani D. Knee joint arthroplasty after tibial osteotomy. Int Orthop. 2010;34(2):289–295. doi: 10.1007/s00264-009-0894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badawy M, Fenstad AM, Indrekvam K, et al. The risk of revision in total knee arthroplasty is not affected by previous high tibial osteotomy. Acta Orthop. 2015;86(6):734–739. doi: 10.3109/17453674.2015.1060402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bae DK, Song SJ, Park CH, et al. Comparison of mid-term results between conversion total knee arthroplasties following closed wedge high tibial osteotomy and primary total knee arthroplasties: a matched pair study including patellar symptom and position. J Orthop Sci. 2017;22(3):495–500. doi: 10.1016/j.jos.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 11.Bergenudd H, Sahlström A, Sanzén L. Total knee arthroplasty after failed proximal tibial valgus osteotomy. J Arthroplast. 1997;12(6):635–638. doi: 10.1016/s0883-5403(97)90135-2. [DOI] [PubMed] [Google Scholar]
- 12.Cross MB, Yi PY, Moric M. Revising an HTO or UKA to TKA: is it more like a primary TKA or a revision TKA? J Arthroplast. 2014;29(9 Suppl):229–231. doi: 10.1016/j.arth.2014.03.053. [DOI] [PubMed] [Google Scholar]
- 13.Efe T, Heyse TJ, Boese C, et al. TKA following high tibial osteotomy versus primary TKA—a matched pair analysis. BMC Musculoskelet Disord. 2010;11:207. doi: 10.1186/1471-2474-11-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Galaly A, Nielsen PT, Jensen SL, et al. Prior high tibial osteotomy does not affect the survival of total knee arthroplasties: results from the Danish Knee Arthroplasty Registry. J Arthroplast. 2018;33(7):2131–2135. doi: 10.1016/j.arth.2018.02.076. [DOI] [PubMed] [Google Scholar]
- 15.Haddad FS, Bentley G. Total knee arthroplasty after high tibial osteotomy: a medium-term review. J Arthroplast. 2000;15(5):597–603. doi: 10.1054/arth.2000.6621. [DOI] [PubMed] [Google Scholar]
- 16.Haslam P, Armstrong M, Geutjens G, et al. Total knee arthroplasty after failed high tibial osteotomy long-term follow-up of matched groups. J Arthroplast. 2007;22(2):245–250. doi: 10.1016/j.arth.2006.01.031. [DOI] [PubMed] [Google Scholar]
- 17.Karabatsos B, Mahomed NN, Maistrelli GL. Functional outcome of total knee arthroplasty after high tibial osteotomy. Can J Surg. 2002;45(2):116–119. [PMC free article] [PubMed] [Google Scholar]
- 18.Kazakos KJ, Chatzipapas C, Verettas D, et al. Mid-term results of total knee arthroplasty after high tibial osteotomy. Arch Orthop Trauma Surg. 2008;128(2):167–173. doi: 10.1007/s00402-007-0488-3. [DOI] [PubMed] [Google Scholar]
- 19.Meding JB, Wing JT, Ritter MA. Does high tibial osteotomy affect the success or survival of a total knee replacement? Clin Orthop Relat Res. 2011;469(7):1991–1994. doi: 10.1007/s11999-011-1810-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niinimäki T, Eskelinen A, Ohtonen P, et al. Total knee arthroplasty after high tibial osteotomy: a registry-based case–control study of 1,036 knees. Arch Orthop Trauma Surg. 2014;134(1):73–77. doi: 10.1007/s00402-013-1897-0. [DOI] [PubMed] [Google Scholar]
- 21.Nizard RS, Cardinne L, Bizot P, et al. Total knee replacement after failed tibial osteotomy results of a matched-pair study. J Arthroplast. 1998;13(8):847–853. doi: 10.1016/s0883-5403(98)90188-7. [DOI] [PubMed] [Google Scholar]
- 22.Saragaglia D, Massfelder J, Refaie R, et al. Computer-assisted total knee replacement after medial opening wedge high tibial osteotomy: medium-term results in a series of ninety cases. Int Orthop. 2016;40(1):35–40. doi: 10.1007/s00264-015-2791-x. [DOI] [PubMed] [Google Scholar]
- 23.Toksvig-Larsen S, Magyar G, Onsten I, et al. Fixation of the tibial component of total knee arthroplasty after high tibial osteotomy: a matched radiostereometric study. J Bone Joint Surg Br. 1998;80(2):295–297. doi: 10.1302/0301-620x.80b2.8153. [DOI] [PubMed] [Google Scholar]
- 24.Miner AL, Lingard EA, Wright EA, et al. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplast. 2003;18(3):286–294. doi: 10.1054/arth.2003.50046. [DOI] [PubMed] [Google Scholar]
- 25.Ripanti S, Marin S, Romani G, et al. Total knee arthroplasty following high tibial osteotomy. J Bone Joint Surg Br. 2012;94:SUPP XXV 195. [Google Scholar]
- 26.Farfalli LA, Farfalli GL, Aponte-Tinao LA. Complications in total knee arthroplasty after high tibial osteotomy. Orthopedics. 2012;35:e464–e468. doi: 10.3928/01477447-20120327-21. [DOI] [PubMed] [Google Scholar]
- 27.Lee OS, Kwon O, Lee YS. Comparison of the outcome between unilateral and bilateral open wedge high tibial osteotomy in the bilateral varus knees. Arch Orthop Trauma Surg. 2018;138(3):307–316. doi: 10.1007/s00402-017-2848-y. [DOI] [PubMed] [Google Scholar]
- 28.Bastos Filho R, Magnussen RA, Duthon V. Total knee arthroplasty after high tibial osteotomy: a comparison of opening and closing wedge osteotomy. Int Orthop. 2013;37(3):427–431. doi: 10.1007/s00264-012-1765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simon MH, Grünwald L, Schenke M, et al. Corrective osteotomies of femur and tibia: which factors influence bone healing? Arch Orthop Trauma Surg. 2019 doi: 10.1007/s00402-019-03217-4. [DOI] [PubMed] [Google Scholar]
- 30.Aglietti P, Buzzi R, Vena LM, et al. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003;16(1):21–26. [PubMed] [Google Scholar]
- 31.Coventry MB, Illstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty cases. Bone Joint Surg Am. 1993;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Yasuda K, Majima T, Tsuchida T, et al. A 10- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res. 1992;282:186–195. [PubMed] [Google Scholar]
- 33.Lee OS, Ahn S, Ahn JH, et al. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2018;138(2):227–236. doi: 10.1007/s00402-017-2826-4. [DOI] [PubMed] [Google Scholar]
- 34.Pearse AJ, Hooper GJ, Rothwell AG, et al. Osteotomy and unicompartmental knee arthroplasty converted to total knee arthroplasty: data from the New Zealand joint registry. J Arthroplast. 2012;27:1827–1831. doi: 10.1016/j.arth.2012.05.031. [DOI] [PubMed] [Google Scholar]
- 35.Parvizi J, Hanssen A, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Jt Surg Am. 2004;86:474–479. doi: 10.2106/00004623-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Treuter S, Schuh A, Hönle W, et al. Long-term results of total knee arthroplasty following high tibial osteotomy according to Wagner. Int Orthop. 2012;36:761–764. doi: 10.1007/s00264-011-1373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bae DK, Song SJ, Yoon KH. Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop. 2010;34:283–287. doi: 10.1007/s00264-009-0749-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagamine R, Inoue S, Miura H, et al. Femoral shaft bowing influences the correction angle for high tibial osteotomy. J Orthop Sci. 2007;12:214–218. doi: 10.1007/s00776-007-1112-7. [DOI] [PubMed] [Google Scholar]
- 39.Pugely AJ, Martin CT, Gao Y, et al. The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplast. 2015;30(9 Suppl):47–50. doi: 10.1016/j.arth.2015.01.063. [DOI] [PubMed] [Google Scholar]
- 40.George J, Mahmood B, Sultan AA, et al. How fast should a total knee arthroplasty be performed? An analysis of 140,199 surgeries. J Arthroplast. 2018;33(8):2616–2622. doi: 10.1016/j.arth.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 41.Berbari EF, Hanssen AD, Duffy MC, et al. Risk factors for prosthetic joint infection: case–control study. Clin Infect Dis. 1998;27:1247–1254. doi: 10.1086/514991. [DOI] [PubMed] [Google Scholar]
- 42.Oiestad BE, Engebretsen L, Storheim K, et al. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]